Abstract
The precise mechanisms of pathology in severe COVID-19 remains elusive. Current evidence suggests that inflammatory mediators are responsible for the manifestation of clinical symptoms that precedes a fatal response to infection. This review examines the nature of platelet activating factor and emphasizes the similarities between the physiological effects of platelet activating factor and the clinical complications of severe COVID-19.
Keywords: platelet activating factor, COVID-19, thrombosis
Introduction
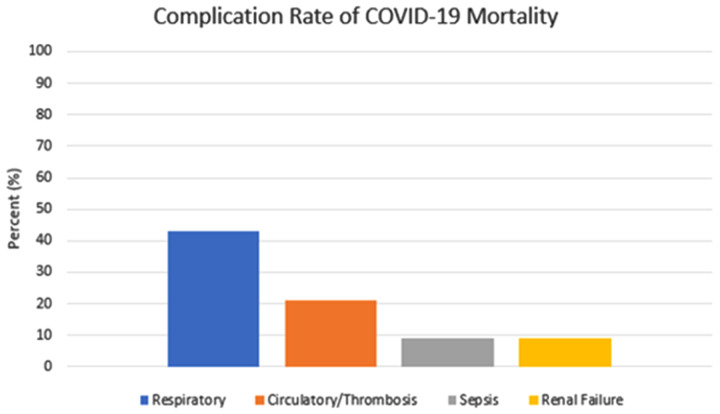
The novel SARS-CoV-2 virus has created a worldwide pandemic which has claimed over four million lives globally. 1 The severity of COVID-19 remains a key predictor for the risk of morbidity and mortality.2,3 Despite ongoing research, scientists have yet to unlock the precise mechanisms of pathology that leads to the high rate of mortality seen in severe COVID-19. Efforts to understand the causes of morbidity and mortality in severe COVID-19 are plagued by the inability to pinpoint clear mechanistic interrelations among potential pathological mechanisms and organ systems impacted by the SARS-CoV-2 virus. Morbidity and mortality associated with COVID-19 has been attributed to a wide range of physiological effects and critical events that involves multiple organ systems and has bewildered clinicians that are fighting to curtail the rate of fatality (Figure 1). 4 COVID-19 mortality has been directly linked to a myriad of sequelae including pneumonia, respiratory distress, hemodynamic instability, thrombotic events, cardiovascular disease, acute renal insufficiency, and other multi-organ failures.3,4 Aside from COVID-19 infection itself, a commonality among the various causes of morbidity and mortality has not been identified. Moreover, anecdotal evidence suggests a high variation of symptomatic presentation and severity of disease in the general population whereby some individuals remain asymptomatic while others will develop a fatal response.
Figure 1.
Rate of Complications Contributing to Mortality in COVID-19 (as of November 2020). 4
The purpose of this article is to introduce platelet activating factor (PAF) as a biomolecular entity with a potential role in the physiological processes which dictate a severe response to COVID-19. PAF exists as a potent phospholipid mediator that is highly involved in many complex biological processes. As PAF has not commanded the same level of attention as other biochemical mediators and pathways, it is easy to overlook the role that PAF may have as a contributor to pathogenesis. However, there is growing interest and ongoing research into PAF as an important mediator of normal physiological function. Conversely, dysfunction or dysregulation of PAF pathways can result in pathogenic effects.
The Biological Role of Platelet Activating Factor
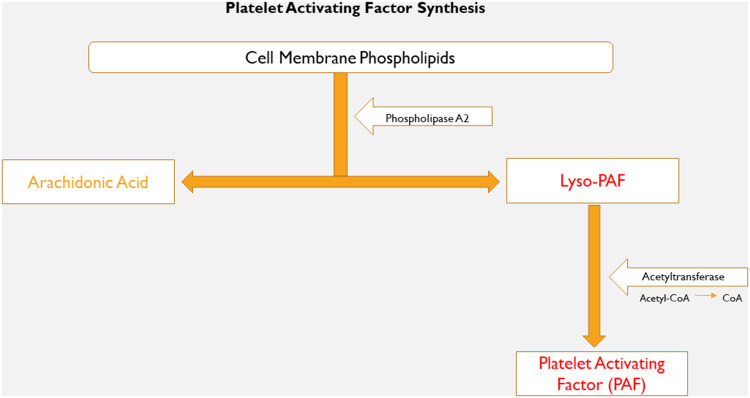
The synthesis of PAF is not unique to any particular cell line and production occurs within multiple cell families which includes inflammatory cells, mast cells, endothelial cells, platelets, and some organ tissues.5,6 The physiological effect of PAF is typically localized to the region of synthesis, and activity is dependent on the precise cellular group(s) involved. PAF synthesis begins when cellular membrane phospholipids are catalyzed by the enzyme phospholipase A2 into Lyso-PAF, the intermediary predecessor to PAF.5,6 Acetyl-CoA acetyltransferase is a thiolase enzyme that preforms the rate-limiting step to complete the conversion of Lyso-PAF into PAF (Figure 2).5,6
Figure 2.
Intracellular biosynthesis of platelet activating factor.
Endogenously, PAF is an agonist at platelet activating factor receptor sites expressed on the surface of leukocytes, endothelial cells, platelets, and a host of other cell types. PAF promotes chemotaxis of leukocytes and is a potent mediator of inflammation, particularly in response to microbial or viral infectious processes.5,6 PAF is also an important contributor to the physiological response of allergy and anaphylactic reactions in the presence of allergens and allergic stimuli. Synthesis of PAF within platelet cells promotes platelet aggregation and clot formation as activation of the G protein-coupled platelet activating factor receptor signals intracellular integrin αIIbβ3, thromboxane A2 synthesis, and promotes binding of fibrinogen. 6 Researchers have also examined the role of PAF in the support of brain function, glycogen degradation, and reproductive integrity.5,6 PAF production by endothelial cells, which comprises the inner lining of the vasculature, results in either vasoconstriction or vasodilation, the extent of which is dependent on the affected vascular bed and the presence of leukocyte infiltration. The downstream effect of platelet activating factor receptor activation is mediated by diverse intracellular signaling pathways and alterations in mRNA transcription. 6 Termination of PAF activity occurs when PAF is recycled back into Lyso-PAF by acetylhydrolases for subsequent incorporation back into the cell membrane as phospholipids.5,6
Platelet Activating Factor Pathogenesis
Although PAF promotes a natural inflammatory response to allergens and infectious processes, researchers have hypothesized that PAF-mediated physiological actions could become pathogenic in the presence of excessive activity or dysregulation. The presence of inflammation and leukocytes stimulates the PAF production cycle. 6 The risk of pathogenicity arises when PAF synthesis or termination cycles are altered as a result of disease or individual genetic variation in physiology. As PAF promotes localized inflammation, it becomes a “beacon” for further recruitment of granulocytes, monocytes, and macrophages. The migration of leukocytes to the affected area further perpetuates the PAF synthesis cycle, creating a surge which can overwhelm innate regulatory mechanisms designed to inhibit PAF. 6
Infection or allergic stimuli are potent catalysts of PAF mediated increases in vascular permeability that induces localized swelling, edema, hypotension, and cytokine release. 6 Pathogenicity can occur when these responses are exaggerated in vital organ systems. Such examples include the respiratory system where vascular permeability promotes pulmonary edema and infiltration thereby compromising pulmonary function. Similar to hemodynamic instability that occurs in situations of sepsis or anaphylaxis, reflexive vascular response to PAF signaling may lead to the development of hypotensive shock. However, the detrimental effects of PAF are not restricted or confined to the vasculature. Other mechanisms of pathogenicity explored include atherogenesis, gastrointestinal ulceration, pancreatitis, renal impairment, inflammatory skin, and autoimmune disorders.5,6
PAF in Acute Respiratory Distress Syndrome
One of the earliest clinically recognized manifestations of COVID-19 was severe pneumonia leading to Acute Respiratory Distress Syndrome (ARDS) requiring mechanical ventilation. 4 Data from a study conducted by Feng et al. cited the prevalence of severe pneumonia in COVID-19 at 10 % and noted that this may be an underestimation when compared to previously published studies. 7 The prevalence of clinically milder pneumonia is expected to be considerably higher than what was reported by Feng et al. who had only examined the rate of severe pneumonia. While the role of PAF in ARDS secondary to COVID-19 remains unexplored, numerous studies have investigated the role of PAF as an instigator of acute lung injury and ARDS in the context of bacterial sepsis.8,9 In vitro experiments have shown that exogenously administered PAF increases vascular permeability and pulmonary edema in animal models. 9 Moreover, the inhibition of PAF activity reduces the development of pulmonary edema in similar animal models. 9 The implications of these findings for human patients remains to be determined.
Previous studies have also examined the nature of PAF acetylhydrolase deficiency and its relationship to asthmatic symptoms. 10 As previously discussed, acetylhydrolase is an enzyme tasked with terminating the action of PAF by recycling PAF back into its intermediary precursor, Lyso-PAF. Masao et al. and colleagues examined PAF acetylhydrolase deficiency in Japanese children as a result of autosomal recessive heredity and determined that the prevalence of serum PAF acetylhydrolase deficiency was significantly higher in those individuals who experienced severe asthma symptoms. 10 In addition, PAF has also been shown to promote bronchoconstriction, mucus secretion, and inflammation of bronchi in asthmatic patients.10,11 The severity of asthmatic symptoms may also be influenced by commonplace anti-inflammatory medications, many of which are available for over-the-counter purchase. It has been suggested that the use of systemic non-steroidal anti-inflammatory drugs (NSAIDs) could exacerbate asthma symptoms as inhibition of cyclooxygenase enzymes shifts arachidonic acid down the parallel lipoxygenase pathway that results in the synthesis of leukotrienes responsible for bronchial inflammation and asthmatic symptoms.12,13 Although there was early speculation that systemic NSAIDs could worsen the outcomes of severe COVID-19, further research has since disproved this hypothesis. 14 The role of inflammatory cytokines in COVID-19 morbidity and mortality remains a significant topic of research.
PAF in Acute Cardiovascular Events and Thrombosis
Patients with COVID-19 have a high incidence of both arterial and venous thrombotic complications. In a large New York City health system, thrombotic events occurred in 16% of hospitalized COVID-19 patients. 15 The all-cause mortality in the described population was 24.5% and was higher in those with thrombotic events (43.2% vs 21.0%; P < 0.001). 15 Other studies have estimated rates of thrombotic events as high as 49% in severe COVID-19. 16 Thrombotic events, in these studies, included a wide range of diagnoses including acute coronary syndrome, deep vein thrombosis, pulmonary embolism, and cerebrovascular events.16,17 Although most of the initial research in COVID-19 associated thrombosis focused on the existence of an underlying hypercoagulable state, there is increasing evidence to suggest the presence of endothelial damage and vascular injury as essential contributors to the activation of the coagulation cascade.16,17 We have previously discussed the action of PAF as a provocateur of vascular permeability, microvascular leakage, and progression of atherosclerosis in the vasculature. Insult to the vascular system intensifies when sustained vascular injury is accompanied by recruitment of leukocytes, platelets, and mast cells to the damaged site which further potentiates the activation of PAF. 18 The net result is a nocuous medley of platelet reactivity, aggregation, and release of pro-inflammatory vascular cytokines that promotes the construction of atherosclerotic plaques. 18 Interleukin-1β, a potent inflammatory cytokine produced by activated platelets, is abundant in platelet-fibrin thrombi and substantiates a potential link between inflammatory mediators and thrombosis. 6 Furthermore, PAF derives its nomenclature from earlier human and animal experiments that identified PAF as a potent mediator of platelet aggregation in vitro.19,20 When human platelet-rich plasma is exposed to PAF in vitro, researchers have observed concentration dependent reversible and irreversible platelet aggregation. 19 In vivo, studies have demonstrated that exogenously administered PAF antagonists suppresses platelet activation and aggregation in rabbit and canine models. 21 Researchers have also postulated that PAF can increase reactive nitrogen and oxygen species which incites vascular permeability. 18 Moreover, certain reactive nitrogen species may inhibit acetylhydrolases and enhance the activity of PAF under conditions of oxidative stress. 18 Preliminary research has reported that COVID-19 patients who were taking low-dose aspirin, an irreversible inhibitor of platelet aggregation, were at reduced risk for placement of mechanical ventilation, or transfer to intensive care units. 22 Data from studies conducted in China demonstrated that mean plasma concentration of PAF levels in patients with coronary heart disease reached 49.7 pg/ml, which was higher than the 23.8 pg/ml observed in controls. 18 More research is needed to discern whether thrombosis in COVID-19 is a unilateral process attributed solely to a hypercoagulable state or whether those thrombotic events involves a myriad of processes that includes platelet aggregation. Hottz et al. observed increased platelet activation and platelet-monocyte aggregate activity in patients with severe COVID-19 compared to milder cases. Their conclusions were based on amplification in the surface expression of P-selectin and CD63, markers indicating platelet activation, and confirmed by measuring plasma levels of thromboxane B2. 23 There continues to be heightened interest in the role of PAF as a mechanism of thrombosis in primary acute coronary syndrome. Subsequently, PAF emerges as an intriguing mechanism that may be linked to the incidence of coronary events and thrombosis seen with severe COVID-19.
PAF in Hemodynamic Instability
Another notable symptom of severe COVID-19 is hemodynamic instability and the presence of hypotensive shock reminiscent of sepsis or anaphylactic reactions. In septic or anaphylactic shock, a cascade of inflammatory mediators increases vascular permeability and vasodilation leading to hypotension and hypoperfusion of vital organs. 24 Furthermore, compensatory mechanisms designed to maintain hemodynamic stability can amplify myocardial strain, thereby provoking a coronary event as the imbalance between oxygen availability and oxygen requirements widens. Research has suggested that PAF serves a pivotal role in the clinical presentation of anaphylaxis. Vadas et al. found that serum levels of PAF in anaphylactic individuals reached 805 ± 595 pg/ml, concentrations far higher than the 23.8 pg/ml reported in controls. 25 The higher levels of serum PAF were also found to be directly correlated with increased severity of anaphylactic response. 25 The elimination of PAF receptors results in diminished anaphylactic reactions in genetically modified animal models. 26 In vitro, rupatadine is a second-generation antihistamine with demonstrated anti-PAF activity, that appears to block cytokine production and degranulation in select types of mast cells. 26 Contrarily, these inhibitory effects were not seen in antihistamines without anti-PAF activity. 26 These findings have led to interest in PAF inhibitors as a potential treatment for allergy mediated symptoms such as allergic rhinitis and chronic urticaria. 27 An expansion of this concept is that progressive mast cell activity in direct response to the presence of PAF has been examined as a highly plausible pathway in the pathophysiology of anaphylactic shock.25,28 Mechanisms of mast cell degranulation become more intriguing relative to COVID-19 morbidity when we consider that initial mast cell activation and PAF synthesis at focal sites can rapidly evolve into an amplification loop that triggers mast cell degranulation at more distal sites (ie, pulmonary structures) as some researchers have suggested. 28 Hemodynamic compromise may be at least partly a consequence of unbridled vasodilation and increased capillary permeability provoked by mast cell degranulation and inflammatory cytokines. 25
PAF in Multi-Organ Failure
Morbidity and mortality associated with severe COVID-19 has also been characterized by vital organ failure, or in some instances, multiple-organ failure.29,30 The diversity of organ systems involved has perplexed both scientists and medical personnel alike. Acute renal dysfunction has been a reported sequelae in 3 to 9% of COVID-19 infections. 31 The presence of acute kidney injury is also associated with poor prognostic outcomes and increased mortality rate. 2 Previous research in human patients has shown that both serum and urine PAF levels are elevated under conditions of corresponding acute renal failure. 32 Mariano et al. reported that plasma PAF levels collected from patients with acute renal failure in the setting of sepsis were significantly higher than PAF levels seen in controls on the first day of observation (244.4 ± 105.1 pg/ml vs 6.6 ± 4.7 pg/ml; P < 0.05). 32 Mariano et al. collected additional data over four consecutive days and concluded that PAF levels in septic patients with acute renal failure were similarly elevated each of the four days when compared to controls. 32 Other investigators have demonstrated that activation of PAF receptors in renal tissue increases kidney inflammation and fibrosis in animal models. 33
The association between PAF and systemic inflammatory response syndrome (SIRS) in the setting of acute pancreatitis has been previously recognized. 34 The release of proinflammatory cytokines, anti-inflammatory cytokines, and tumor necrosis factor α mediates the development of SIRS and systemic multi-organ failure in acute pancreatitis. 34 This “inflammatory soup” also includes PAF which establishes a link between PAF and the manifestation of SIRS in pancreatic disease. 34 However, Johnson et al. failed to demonstrate that antagonism of PAF activity reduces morbidity or prevents multi-organ failure in individuals hospitalized with acute pancreatitis. 34 The connection between PAF and SIRS is intriguing none the less.
It is widely accepted that diabetes is an independent risk factor for the development of sepsis and SIRS. 34 International studies have confirmed that diabetes is also a significant risk factor of mortality in severe COVID-19. Available data suggests that diabetes (type I or type II), with the latter being most prominent, is present in approximately one-third of mortality cases associated with COVID-19.35,36 If diabetes does increase either the incidence of SIRS, or sets into motion another inflammatory cascade that ultimately leads to multi-organ failure with severe COVID-19, then the potential role of PAF as a progenitor of COVID-19 morbidity and mortality becomes more tangible.
Similarities of Symptomatic Presentations Between Severe COVID-19 and Dengue
Early detection of COVID-19 infection is vital to both the timeliness of treatment initiation for individual patients as well as contact tracing to reduce spread of infection within the general population. Efforts to distinguish the earlier non-specific clinical stages of COVID-19 from other diseases has been a priority from the beginning of the pandemic, especially in geographical regions with a higher prevalence rate of other viral illnesses that exhibit similar symptoms to COVID-19 and can undermine COVID-19 early detection efforts. Such research has led to a direct comparison between the symptomatic presentation found in COVID-19 to symptoms that are seen in dengue, a mosquito-borne viral illness that can result in fatal hemorrhagic fever. 37 Henrina et al. reported that COVID-19 and dengue share a remarkable resemblance in clinical presentation, particularly when examining the earlier stages of COVID-19. 37 The presence of fever is the most common symptom shared between COVID-19 and dengue. 37 The symptomatic similarities between COVID −19 and dengue do not end there and expand to include headache and myalgias. 37 Manifestation of pulmonary symptoms which includes cough or respiratory distress can occur in both COVID-19 and dengue as well. 37 Nausea, vomiting, abdominal pain, diarrhea, and acute liver injury comprise the list of gastrointestinal symptoms akin to either syndrome. 37 Although less common, individuals infected by COVID-19 or dengue virus may also experience the precipitous appearance of a cutaneous rash. 37 Applied laboratory analysis of serum samples collected from individuals infected by COVID-19 or dengue virus have also demonstrated similar abnormalities in hematologic indexes. Thrombocytopenia, leukopenia, and elevated D-dimer as identified by hematologic panels can be present in both COVID-19 and dengue. 37 The similarities of clinical presentation between COVID-19 and dengue is so pronounced that it can be difficult to distinguish between these two pathologies, particularly in the early stages of infection, and has resulted in COVID-19 cases that were initially misdiagnosed as dengue. 37
The telltale signs of severe dengue infections are thrombocytopenia, hemorrhage, increased vascular permeability, shock, and excessive cytokine activity. 38 Evidence from animal models has shown that deletion of PAF receptor genes and administration of PAF receptor antagonists results in lower severity of disease following exposure to dengue virus. 38 These findings appear to support at least a partial role of PAF in the pathogenesis of dengue infections. Sousa et al. noted that in murine models, deletion or inhibition of PAF activity reduced the production of inflammatory cytokines and tumor necrosis factor α. 38 If there truly exists a communal inflammatory pathway resulting in the manifestation of similar clinical presentation in both COVID-19 and dengue, then it is plausible that PAF plays a significant role in the pathogenesis of COVID-19 as well.
Discussion
COVID-19 can present with a myriad of clinical symptoms. There is significant overlap between the clinical manifestations of COVID-19 and other well-established clinical syndromes such as allergy and anaphylactic reactions, thrombotic events, and viral illnesses like dengue. Our existing knowledge regarding the latter syndromes suggests the potential role of PAF in COVID-19 as a mediator within the inflammatory cascade which promotes the development of inflammation, thrombosis, and hemodynamic compromise (Table 1). As we identify key similarities in pathogenesis between COVID-19 and other disease states to affirm the role of PAF in COVID-19, we can apply the same principles of speculative comparison to treatments with proven efficacy in medical conditions of which we have familiarity and experience. In the case of severe allergy, anaphylaxis, and septic shock, the administration of corticosteroids has been demonstrated to improve disease outcomes. 39 Available evidence suggests that corticosteroids can also improve outcomes in severe COVID-19 disease igniting the acceptance of corticosteroids as a viable treatment modality for severe COVID-19. 40 A review of the PAF synthesis pathway and corticosteroid pharmacodynamics reveals that corticosteroids inhibit the activity of phospholipase A2, an enzyme responsible for the conversion of cell membrane phospholipids to Lyso-PAF, the progenitor of PAF, and thereby reducing downstream production of PAF itself. 41 If PAF indeed activates physiological pathways that contribute to the pathogenic effects of COVID-19, it is conceivable that pharmacological agents which directly inhibit the activity of PAF, or modulate the cycle of PAF synthesis and degradation may reduce morbidity and mortality associated with COVID-19.42–45 This speculative concept is shared by others.46,47 Moreover, scientists continue to explore whether pharmacological agents that demonstrate PAF inhibition, such as rupatadine, are viable treatments for COVID-19.47,48
Table 1.
Categorization of pathology that contributes to morbidity and mortality in severe COVID-19 with a direct comparison to the known physiological effects of Platelet Activating Factor in human or animal models.
| COVID-19 Complication Category | Physiological Effects of Platelet Activating Factor | References |
|---|---|---|
| Acute Respiratory Syndrome/Pneumonia | Increase of vascular permeability in lung tissues resulting in pulmonary edema.8,9 PAF promotes bronchoconstriction, mucus secretion, and bronchial inflammation in asthmatic individuals.10-13 | [10] Miwa M., Miyake T., Yamanaka T., et al.: Characterization of serum platelet-activating factor (PAF) acetylhydrolase. Correlation between deficiency of serum PAF acetylhydrolase and respiratory symptoms in asthmatic children. J Clin Invest. 1988;82(6):1983 to 1991. [11] Hsieh K.H., Ng C.K.: Increased plasma platelet-activating factor in children with acute asthmatic attacks and decreased in vivo and in vitro production of platelet-activating factor after immunotherapy. J Allergy Clin Immunol. 199; Feb;91(2):650 to 7. [12] Kowalski M.L, Agache I., Bavbek S., et al.: Diagnosis and management of NSAID-Exacerbated Respiratory Disease (N-ERD)-a EAACI position paper. Allergy 2019; Jan;74(1):28 to 39. [13] Busse W.W.: Leukotrienes and inflammation. Am J Respir Crit Care Med. 1998; Jun;157(6 Pt 1):S210 to 3. |
| Thrombosis | Signals platelet reactivity and aggregation that results in construction of atherosclerotic plaques. Promotes vascular inflammation and remodeling.16-21 | [16] Hajra A., Mathai S.V., Ball S., et al.: Management of Thrombotic Complications in COVID-19: An Update. Drugs 2020;80(15):1553 to 1562. [17] Piazza G., Campia U., Hurwitz S., et al.: Registry of Arterial and Venous Thromboembolic Complications in Patients With COVID-19. J Am Coll Cardiol. 2020; Nov 3;76(18):2060 to 2072. [18] Palur Ramakrishnan A.V., Varghese T.P., Vanapalli S., et al.: Platelet activating factor: A potential biomarker in acute coronary syndrome? Cardiovasc Ther. 2017; Feb;35(1):64 to 70. [19] Marcus A.J., Safier L.B., Ullman H.L., et al.; Effects of acetyl glyceryl ether phosphorylcholine on human platelet function in vitro. Blood. 1981; 58 (5): 1027 to 1031. [20] Cazenave J.P., Benveniste J., Mustard J.F.: Aggregation of rabbit platelets by platelet-activating factor is independent of the release reaction and the arachidonate pathway and inhibited by membrane-active drugs. Lab Invest. 1979 Sep;41(3):275 to 285. [21] Golino P., Ambrosio G., Ragni M., et al.: Short-term and long-term role of platelet activating factor as a mediator of in vivo platelet aggregation. Circulation. 1993 Sep;88(3):1205 to 1214. |
| Hemodynamic Instability/Septic Shock | In response to infection or allergic stimuli, PAF stimulates degranulation of mast cells and recruitment of inflammatory mediators. The net result is increased vascular permeability and vasodilation that can lead to hypotensive shock.25,26 | [25] Vadas P., Gold M., Perelman B., et al.: Platelet-activating factor, PAF acetylhydrolase, and severe anaphylaxis. N Engl J Med. 2008; Jan 3;358(1):28 to 35. [26] Munoz-Cano R.M., Casas-Saucedo R., Valero Santiago A., et al.: Platelet-Activating Factor (PAF) in Allergic Rhinitis: Clinical and Therapeutic Implications. J Clin Med. 2019; Aug 29;8(9):1338. |
| Multi-Organ Failure/SIRS | Promotes inflammation and fibrosis in renal tissue.31,33 PAF serum levels elevated under conditions of acute kidney failure. 32 PAF represents an element of the inflammatory cascade that leads to the development of SIRS.28-30 | [28] Kajiwara N., Sasaki T., Bradding P., et al.: Activation of human mast cells through the platelet-activating factor receptor. J Allergy Clin Immunol. 2010; May;125(5):1137 to 1145. [29] Mokhtari T., Hassani F., Ghaffari N., et al.: COVID-19 and multiorgan failure: A narrative review on potential mechanisms. J Mol Histol. 2020;51(6):613 to 628. [30] Zaim S., Chong J.H., Sankaranarayanan V., et al.: COVID-19 and Multiorgan Response. Curr Probl Cardiol. 2020;45(8):100618. [31] Raza A., Estepa A., Chan V., et al.: Acute Renal Failure in Critically Ill COVID-19 Patients With a Focus on the Role of Renal Replacement Therapy: A Review of What We Know So Far. Cureus. 2020;12(6):e8429. Published 2020; Jun 3. [32] Mariano F., Guida G., Donati D., et al.: Production of platelet-activating factor in patients with sepsis-associated acute renal failure. Nephrology Dialysis Transplantation. 1999; May;14(5): 1150 to 1157. [33] Correa-Costa M., Andrade-Oliveira V., Braga T.T., et al.: Activation of platelet-activating factor receptor exacerbates renal inflammation and promotes fibrosis. Lab Invest. 2014; Apr;94(4):455 to 66. |
Abbreviations: PAF, Platelet Activating Factor; SIRS, Systemic Inflammatory Response Syndrome
Conclusion
Our understanding of COVID-19 remains limited and the pathologic mechanisms which contribute to disease development are likely multi-factorial and complex. PAF represents a potential pathophysiologic mechanism for severe COVID-19 due to its prominent role in signaling of inflammatory and thrombotic pathways. Even if PAF does indeed play a role in the pathogenesis of severe COVID-19, it is unlikely that it is a sole player in the cascade of events that leads to the culmination of the clinically varied and complex presentation of COVID-19. Additional research is needed to validate both the relationship between PAF and COVID-19 as well as the extent to which PAF may increase morbidity and mortality in severe COVID-19.
Acknowledgements
MK, VD, and FM are all employees of the Minneapolis VA Healthcare System. This material is based upon work supported by the Department of Veterans Affairs (specifically the Veterans Health Administration).
Author biography
Dr. Mark Klein is a Staff Physician at the Minneapolis VA Healthcare System and Associate Professor at the University of Minnesota.
Vinh Dao is a pharmacist in the Pain Center at the Minneapolis VA Healthcare System.
Dr. Fatima Khan is a Staff Physician at the Minneapolis VA Healthcare System and Assistant Professor at the University of Minnesota.
Footnotes
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest Statement: The Author(s) declare(s) that there is no conflict of interest
Ethics and Patient Consent: This is a review article. Our institution does not require ethics approval for a review article. Patient consent is not applicable to this article.
Author Contributions: F.K., V.D., and M.K. came up with the concept for the manuscript. V.D. did the initial literature search, and F.K. and M.K. confirmed the appropriateness of the sources. All authors wrote the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iDs: Mark Klein https://orcid.org/0000-0003-3457-6879
References
- 1.Corona Virus Resource Center. Global Deaths Data. John Hopkins University of Medicine; 2021. Available at https://coronavirus.jhu.edu. [Google Scholar]
- 2.Jehi L, Ji X, Milinovich A, et al. Development and validation of a model for individualized prediction of hospitalization risk in 4,536 patients with COVID-19. PLoS One. 2020;15(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berlin DA, Gulick RM, Martinez FJ. Severe covid-19. N Engl J Med. 2020;383(25):2451–2460. [DOI] [PubMed] [Google Scholar]
- 4.Center for Disease Control and Prevention, National Center for Health Statistics (2020), Provisional Death Counts for Coronavirus Disease 2019 (COVID-19), Weekly Updates by Select Demographic and Geographic Characteristics, Atlanta, GA. Available at https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm.
- 5.Prescott SM, Zimmerman GA, McIntyre TM, et al. Platelet-Activating factor and related lipid mediators annual review of biochemistry. Annu Rev Biochem. 2000;69(1):419-445. [DOI] [PubMed] [Google Scholar]
- 6.Zimmerman GA, McIntyre TM, Prescott SM, et al. The platelet-activating factor signaling system and its regulators in syndromes of inflammation and thrombosis. Crit Care Med. 2002;30(5 Suppl):S294-S301. [DOI] [PubMed] [Google Scholar]
- 7.Feng Z, Yu Q, Yao S, et al. Early prediction of disease progression in COVID-19 pneumonia patients with chest CT and clinical characteristics. Nat Commun. 2020;11(1):4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Makristathis A, Stauffer F, Feistauer SM, et al. Bacteria induce release of platelet-activating factor (PAF) from polymorphonuclear neutrophil granulocytes: possible role for PAF in pathogenesis of experimentally induced bacterial pneumonia. Infect Immun. 1993;61(5):1996-2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clavijo LC, Carter MB, Matheson PJ, et al. Platelet-activating factor and bacteremia-induced pulmonary hypertension. J Surg Res. 2000;88(2):173-180. [DOI] [PubMed] [Google Scholar]
- 10.Miwa M, Miyake T, Yamanaka T, et al. Characterization of serum platelet-activating factor (PAF) acetylhydrolase. Correlation between deficiency of serum PAF acetylhydrolase and respiratory symptoms in asthmatic children. J Clin Invest. 1988;82(6):1983-1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsieh KH, Ng CK. Increased plasma platelet-activating factor in children with acute asthmatic attacks and decreased in vivo and in vitro production of platelet-activating factor after immunotherapy. J Allergy Clin Immunol. 199;91(2):650-657. [DOI] [PubMed] [Google Scholar]
- 12.Kowalski ML, Agache I, Bavbek S, et al. Diagnosis and management of NSAID-exacerbated respiratory disease (N-ERD)-a EAACI position paper. Allergy. 2019;74(1):28-39. [DOI] [PubMed] [Google Scholar]
- 13.Busse WW. Leukotrienes and inflammation. Am J Respir Crit Care Med. 1998;157(6 Pt 1):S210-S213. [PubMed] [Google Scholar]
- 14.Moore N, Carleton B, Blin P, et al. Does ibuprofen worsen COVID-19? Drug Saf. 2020;43(7):611-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bilaloglu S, Aphinyanaphongs Y, Jones S, et al. Thrombosis in hospitalized patients With COVID-19 in a New York city health system. JAMA. 2020;324(8):799-801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hajra A, Mathai SV, Ball S, et al. Management of thrombotic complications in COVID-19: an update. Drugs. 2020;80(15):1553-1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piazza G, Campia U, Hurwitz S, et al. Registry of arterial and venous thromboembolic complications in patients With COVID-19. J Am Coll Cardiol. 2020;76(18):2060-2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palur Ramakrishnan AV, Varghese TP, Vanapalli S, et al. Platelet activating factor: a potential biomarker in acute coronary syndrome? Cardiovasc Ther. 2017;35(1):64-70. [DOI] [PubMed] [Google Scholar]
- 19.Marcus AJ, Safier LB, Ullman HL, et al. Effects of acetyl glyceryl ether phosphorylcholine on human platelet function in vitro. Blood. 1981;58(5):1027-1031. [PubMed] [Google Scholar]
- 20.Cazenave JP, Benveniste J, Mustard JF. Aggregation of rabbit platelets by platelet-activating factor is independent of the release reaction and the arachidonate pathway and inhibited by membrane-active drugs. Lab Invest. 1979;41(3):275-285. [PubMed] [Google Scholar]
- 21.Golino P, Ambrosio G, Ragni M, et al. Short-term and long-term role of platelet activating factor as a mediator of in vivo platelet aggregation. Circulation. 1993;88(3):1205-1214. [DOI] [PubMed] [Google Scholar]
- 22.Chow JH, Khanna AK, Kethireddy S, et al. Aspirin Use is associated with decreased mechanical ventilation, ICU admission, and In-hospital mortality in hospitalized patients with COVID-19. Anesth Analg. 2020;132(4):930-941. [DOI] [PubMed] [Google Scholar]
- 23.Hottz ED, Azevedo-Quintanilha IG, Palhinha L, et al. Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood. 2020;136(11):1330-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beltran-Garcia J, Osca-Verdegal R, Pallardo FV, et al. Sepsis and coronavirus disease 2019: common features and anti-inflammatory therapeutic approaches. Crit Care Med. 2020;48(12):1841-1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vadas P, Gold M, Perelman B, et al. Platelet-activating factor, PAF acetylhydrolase, and severe anaphylaxis. N Engl J Med. 2008;358(1):28-35. [DOI] [PubMed] [Google Scholar]
- 26.Munoz-Cano RM, Casas-Saucedo R, Valero Santiago A, et al. Platelet-Activating factor (PAF) in allergic rhinitis: clinical and therapeutic implications. J Clin Med. 2019;8(9):1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Palgan K, Bartuzi Z. Platelet activating factor in allergies. Int J Immunopathol Pharmacol. 2015;28(4):584-589. [DOI] [PubMed] [Google Scholar]
- 28.Kajiwara N, Sasaki T, Bradding P, et al. Activation of human mast cells through the platelet-activating factor receptor. J Allergy Clin Immunol. 2010;125(5):1137-1145. [DOI] [PubMed] [Google Scholar]
- 29.Mokhtari T, Hassani F, Ghaffari N, et al. COVID-19 and multiorgan failure: a narrative review on potential mechanisms. J Mol Histol. 2020;51(6):613-628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zaim S, Chong JH, Sankaranarayanan V, et al. COVID-19 and multiorgan response. Curr Probl Cardiol. 2020;45(8):100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raza A, Estepa A, Chan V, et al. Acute renal failure in critically Ill COVID-19 patients With a focus on the role of renal replacement therapy: a review of what We know So Far. Cureus. 2020;12(6):e8429. Published 2020; Jun 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mariano F, Guida G, Donati D, et al. Production of platelet-activating factor in patients with sepsis-associated acute renal failure. Nephrol Dial Transplant. 1999;14(5):1150-1157. [DOI] [PubMed] [Google Scholar]
- 33.Correa-Costa M, Andrade-Oliveira V, Braga TT, et al. Activation of platelet-activating factor receptor exacerbates renal inflammation and promotes fibrosis. Lab Invest. 2014;94(4):455-466. [DOI] [PubMed] [Google Scholar]
- 34.Johnson CD, Kingsnorth AN, Imrie CW, et al. Double blind, randomised, placebo controlled study of a platelet activating factor antagonist, lexipafant, in the treatment and prevention of organ failure in predicted severe acute pancreatitis. Gut. 2001;48(1):62-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ganesan SK, Venkatratnam P, Mahendra J, et al. Increased mortality of COVID-19 infected diabetes patients: role of furin proteases. Int J Obes. 2020;44(12):2486-2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barron E, Bakhai C, Kar P, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in england: a whole-population study. Lancet Diabetes Endocrinol. 2020;8(10):813-822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henrina J, Putra ICS, Lawrensia S, et al. Coronavirus disease of 2019: a mimicker of dengue infection? SN Compr Clin Med. 2020:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Souza DG, Fagundes CT, Sousa LP, et al. Essential role of platelet-activating factor receptor in the pathogenesis of dengue virus infection. Proc Natl Acad Sci U S A. 2009;106(33):14138-14143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lian XJ, Huang DZ, Cao YS, et al. Reevaluating the role of corticosteroids in septic shock: an updated meta-analysis of randomized controlled trials. Biomed Res Int. 2019:3175047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Prescott HC, Rice TW. Corticosteroids in COVID-19 ARDS: evidence and hope during the pandemic. JAMA. 2020;324(13):1292-1295. [DOI] [PubMed] [Google Scholar]
- 41.Ericson-Neilsen W, Kaye AD. Steroids: pharmacology, complications, and practice delivery issues. Ochsner J. 2014;14(2):203-207. [PMC free article] [PubMed] [Google Scholar]
- 42.Shamizadeh S, Brockow K, Ring J. Rupatadine: efficacy and safety of a non-sedating antihistamine with PAF-antagonist effects. Allergo J Int. 2014;23(3):87-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sudhakara Rao M, Dwarakanatha Reddy D, Murthy PS. Rupatadine: pharmacological profile and its use in the treatment of allergic rhinitis. Indian J Otolaryngol Head Neck Surg. 2009;61(4):320-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Papakonstantinou V, Lagopati N, Tsilibary EC, et al. A review on platelet activating factor inhibitors: could a New class of potent metal-based anti-inflammatory drugs induce anticancer properties? Bioinorg Chem Appl. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peplow PV. Regulation of platelet-activating factor (PAF) activity in human diseases by phospholipase A2 inhibitors, PAF acetylhydrolases, PAF receptor antagonists and free radical scavengers. Prostaglandins Leukot Essent Fatty Acids. 1999;61(2):65-82. [DOI] [PubMed] [Google Scholar]
- 46.Demopoulos CA. Is platelet-activating factor (PAF) a missing link for elucidating the mechanism of action of the coronavirus SARS-CoV-2 and explaining the Side effects-complications of COVID-19 disease? Preprints. 2020:2020060253 [Google Scholar]
- 47.Demopoulos CA, Antonopoulou S, Theoharides TC. COVID-19, microthromboses, inflammation, and platelet activating factor. Biofactors. 2020;42(10):1850-1852. [DOI] [PubMed] [Google Scholar]
- 48.Theoharides TC, Antonopoulou S, Demopoulos CA. Coronavirus 2019, microthromboses, and platelet activating factor. Clin Ther. 2020;42(10):1850-1852. [DOI] [PMC free article] [PubMed] [Google Scholar]