Abstract
Background:
The treatment strategy for pediatric anterior cruciate ligament (ACL) tears, especially in patients with open physes, remains controversial.
Purpose:
To assess clinical outcomes and postoperative complications after all-epiphyseal double-bundle ACL (DB-ACL) reconstruction for patients with open physes.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Included were 102 patients aged ≤15 years who underwent ACL reconstruction at a single institution and had a minimum of 2 years of follow-up. Of these patients, 18 had undergone all-epiphyseal DB-ACL reconstruction (mean age, 12.4 ± 1.2 year) and 84 had undergone conventional DB-ACL reconstruction (mean age, 14.1 ± 0.9 year). The outcomes of the all-epiphyseal group were compared with those of the conventional group. Objective clinical outcomes included KT-1000 arthrometer measurements of side-to-side difference in anterior tibial translation, Lachman test grade, and pivot-shift test grade. Radiographic angular deformity (defined as >3° of the side-to-side difference in femorotibial angle) and incidence of second ACL injury were also compared.
Results:
The postoperative side-to-side difference in laxity significantly improved from 6.1 ± 2.4 to 0.6 ± 0.9 mm in the all-epiphyseal group (P = .001), and postoperative laxity was similar to that of the conventional group (0.4 ± 0.8 mm; P = .518). A Lachman grade 1 positive result was observed in 20% of the all-epiphyseal group and 3% of the conventional group (P = .042), and a pivot-shift grade 1 positive result was observed in 22% of the all-epiphyseal group and 4% of the conventional group (P = .074). A total of 4 patients (26.7%) in the all-epiphyseal group and 4 (6.1%) in the conventional group demonstrated angular deformity (P = .035). The incidence of postoperative ipsilateral ACL tear was 16.7% in the all-epiphyseal group and 23.8% in the conventional group (P = .757). The incidence of contralateral ACL tear was 11.1% in the all-epiphyseal group and 14.3% in the conventional group (P ≥ .999).
Conclusion:
All-epiphyseal DB-ACL reconstruction for skeletally immature patients achieved satisfactory clinical outcomes compared with conventional DB-ACL reconstruction. The incidence of ipsilateral graft rupture was relatively high in both groups. The all-epiphyseal group had a significantly higher incidence of angular deformity.
Keywords: all-epiphyseal technique, anterior cruciate ligament reconstruction, double-bundle reconstruction, pediatric
The incidence of anterior cruciate ligament (ACL) reconstruction among the pediatric population has been increasing in recent years. 3,9 The treatment strategy for pediatric ACL tears, especially in patients with open physes, remains controversial. There are various nonsurgical or surgical treatment options, and, if surgical treatment is selected, choices of timing, surgical procedure, and graft type. Although it has been reported that about 90% of skeletally immature patients were able to return to sports after nonoperative treatment, 22% underwent ACL reconstruction during the follow-up period and 38% had to decrease their level of sport. 25 Some reports have demonstrated inferior clinical outcomes after nonoperative treatment owing to secondary meniscal or cartilage injury. 20,24,26,28,32,43,48
Several surgical ACL reconstruction procedures have been established for patients with an open physis, including the physeal-sparing technique, 2,7,15,18,20 partial transphyseal technique, 22 and complete transphyseal technique. 17,21 One of the major issues in pediatric ACL reconstruction is growth disturbance or angular deformity. A systematic review comparing the physeal-sparing and transphyseal techniques concluded that there was no difference in incidence of growth disturbance. 31 In contrast, a recent clinical study revealed that physeal violation leads to a high rate of growth disturbance in patients where longer growth remains. 4 Theoretically, surgeons should be able to avoid these complications with the physeal-sparing technique; however, this has not always been the case. 5,7,31
In previous reports regarding the physeal-sparing technique, most surgical procedures comprised a single-bundle (SB) reconstruction using the iliotibial band, 15,16,44 hamstring tendon (HT), 2,4,7,17,21,27 or quadriceps tendon. 41,47 It was reported that the ACL femoral insertion is oval shaped, 37 and the tibial insertion is C-shaped. 42 To mimic these ACL insertions, a double-bundle (DB) reconstruction using HT has been developed and has demonstrated good clinical outcomes among skeletally mature patients. 38 A recent meta-analysis comparing clinical outcomes between SB and DB-ACL reconstruction in adults concluded that subjective knee evaluations, KT-1000 arthrometer laxity measurements, and proprioception were quite similar and that the number of positive pivot-shift test results was significantly lower in the DB-ACL reconstruction group. 12 A biomechanical study reported that DB-ACL reconstruction was able to restore both the anteromedial bundle (AMB) and the posterolateral bundle (PLB), which may produce better knee kinematics, especially during rotatory loads. 51
The biomechanical advantages of the DB technique may also apply to skeletally immature patients. Koizumi et al 18 performed DB-ACL reconstruction for patients with open physes in which the AMB was placed in an over-the-top position and the PLB was placed in an anatomic position with a bone tunnel. This physeal-sparing technique showed good clinical outcomes, similar to those obtained with adult patients; however, the AMB was a nonanatomic reconstruction. The optimal procedure for pediatric ACL reconstruction is still controversial.
To both minimize the risk of complications and reproduce anatomic insertion, we believe it is desirable to perform all-epiphyseal DB-ACL reconstruction, in which the apertures of both the AMB and PLB are created within anatomic insertions and the bone tunnels are within the epiphysis. The purpose of this study was to assess clinical outcomes and postoperative complications after anatomic all-epiphyseal DB-ACL reconstruction for patients with open physes. It was hypothesized that, compared with conventional DB-ACL reconstruction, all-epiphyseal DB-ACL reconstruction would provide satisfactory clinical outcomes, including knee stability and subjective knee function, without serious complications.
Methods
Patients and Treatment Strategy for Pediatric Patients
The study design was approved by the ethics committee of our institution, and all patients, or their parents, provided informed consent. A retrospective analysis of prospectively collected data was conducted. There were 959 ACL surgical procedures at our center between April 2009 and March 2018. Among these, 18 patients received primary all-epiphyseal DB-ACL reconstruction (all-epiphyseal group) and had a minimum of 24 months of follow-up.
Our treatment strategy included implementing delayed ACL reconstruction after skeletal maturity (physis closing) for patients with an open physis and without concomitant injuries, including to the meniscus and cartilage. A strict restriction on activity was applied during the waiting period to prevent the occurrence of secondary injuries such as meniscal or cartilage injury as much as possible. For patients with an open physis who had a concomitant injury at the time of ACL injury, patients with a new concomitant injury during the surgery waiting period, or patients hoping for an early return to sports, an all-epiphyseal DB-ACL reconstruction using an HT autograft was implemented. 13 If the central physis closure occurred on both the distal femur and the proximal tibia (dropout sign), 30,39 or complete closure was observed on magnetic resonance imaging, conventional (transphyseal) DB-ACL reconstruction using an HT graft or rectangular tunnel bone–patellar tendon–bone (BTB) ACL reconstruction was implemented. 38
Surgical Technique
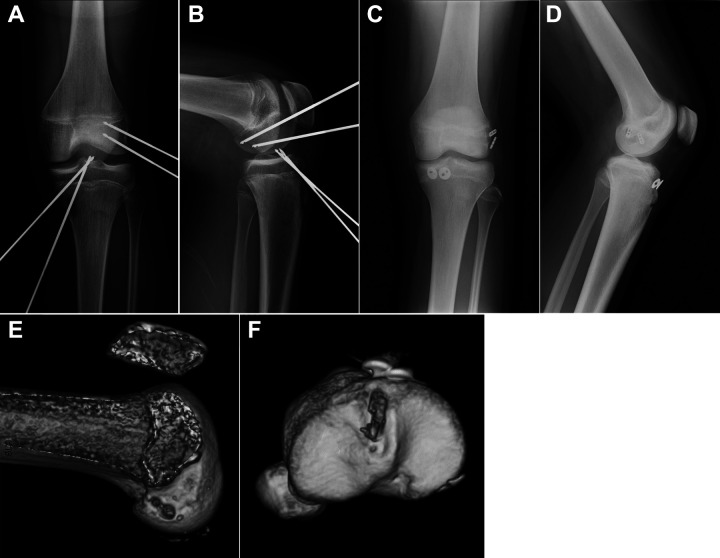
In the all-epiphyseal DB-ACL reconstruction, 13 a semitendinosus tendon (ST) was initially harvested; the harvested ST was cut in half, and the distal and proximal halves were used for the AMB and PLB, respectively. A small longitudinal skin incision was made above the lateral epicondyle of the femur, and the iliotibial band was incised along the line of the fibers. Femoral anteromedial (AM) and posterolateral (PL) guide pins were then inserted into the anatomical footprint using an outside-in Small Angle Footprint Femoral ACL Guide (AR-1510FRS; Arthrex) while avoiding epiphyseal injury. Subsequently, tibial guide pins were inserted into the tibial footprint using a tibial guide (Small Angle Pin Tip Tibial Marking Hook ACL Guide; AR-1510GTS; Arthrex) while avoiding epiphyseal injury. The location of the 4 pins was confirmed by intraoperative radiographs (Figure 1).
Figure 1.
All-epiphyseal double-bundle anterior cruciate ligament reconstruction. Intraoperative radiographs: (A) anteroposterior and (B) lateral view. Postoperative radiographs: (C) anteroposterior and (D) lateral view. Three-dimensional computed tomography images: (E) medial view of femoral tunnels and (F) upper view of tibial tunnels.
The femoral sockets were created using a retrograde reamer (Short FlipCutter II; AR-1204AS; Arthrex) in an order corresponding to the PL and AM tunnels. The length of the femoral socket was approximately 20 mm. The tibial guide pins were overdrilled from the tibial cortex side using a cannulated reamer. In this series, the average diameter of the femoral and tibial tunnel was 5.4 ± 0.4 mm (range, 5.0-6.0 mm) and 5.8 ± 0.4 mm (range, 5.0-6.0 mm), respectively, in the AMB and 5.4 ± 0.6 mm (range 4.5-6.0 mm) and 5.5 ± 0.5 mm (range, 5.0-6.0 mm), respectively, in the PLB.
The PLB graft was introduced into the joint from the tibial tunnel to the femoral socket, followed by the AMB graft. The femoral side of the graft was fixed by a cortical suspensory device. On the tibial side, the PLB graft was first fixed by tying it over a tibial disc, which was positioned proximal to the tibial physis, followed by the AMB graft in the same manner. The PLB and AMB were fixed while the knee was maintained at 20° of flexion (Figure 1). In all procedures, the senior author (Y.I.) performed or directly supervised the ACL reconstruction and repair or partial resection for concomitant meniscal injury.
Postoperative Rehabilitation
Patients were permitted crutch-assisted partial body weightbearing ambulation with knee brace along with range-of-motion (ROM) and isometric muscle strength exercises from the day after surgery. Full weightbearing was allowed depending on whether there was postoperative knee pain. Jogging was permitted after 3 months, sports-specific training from after 6 to 9 months, and return to sport after 9 to 12 months. All patients performed postoperative rehabilitation according to the same protocol.
Clinical Assessments
Demographic data, including age at the time of surgery, sex, height, body weight, body mass index, time from injury to surgery, concomitant meniscal and cartilage injury in intraoperative arthroscopic findings, and type of graft, were examined retrospectively from medical records.
Objective clinical outcomes included knee ROM, side-to-side difference in anterior tibial translation measured using a KT-1000 arthrometer (MEDmetric Corp), and grade of Lachman and pivot-shift tests before and 24 months after surgery. Patients' subjective outcomes were evaluated using the Knee Injury and Osteoarthritis and Outcome Score (KOOS) at final follow-up. 34,35
Recovery of muscle strength of the knee extensor and flexor was evaluated preoperatively and at 3, 6, 9, 12, and 24 months after surgery: isokinetic peak torque (angular velocity of 60°/s) was measured using a Biodex system 4 dynamometer (Biodex Corp) and normalized by dividing the value of the involved side by that of the uninvolved side.
In the radiographic evaluation, the femorotibial angle (FTA) in an anteroposterior (AP) view was measured on both the involved and uninvolved sides. A single observer (S.S.) performed radiographic measurements at a single timepoint. The amount of change in FTA (the varus and valgus angle were represented with positive and negative values, respectively) from before surgery to final follow-up was calculated. In addition, the incidence of postoperative angular deformity, which was assumed to be greater than 3° of the side-to-side difference in FTA, 5,10,40 was examined. The number of second ACL injuries (ipsilateral graft rupture and/or contralateral injury) occurring during the follow-up period was also recorded.
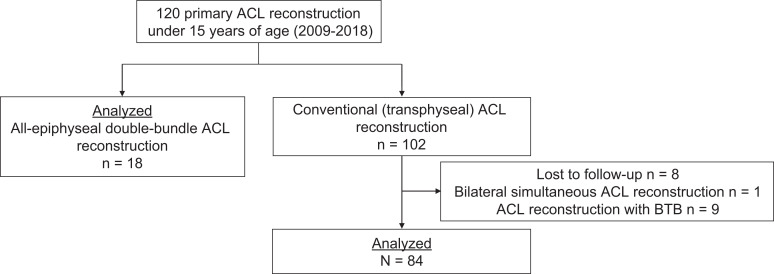
To compare the clinical outcomes of all-epiphyseal DB-ACL reconstruction with conventional DB-ACL reconstruction for skeletally mature patients, a control group was defined as patients under 15 years of age who underwent transphyseal DB-ACL reconstruction using HT autograft during the study period. During the analysis period, 102 patients received conventional ACL reconstruction. Eight patients who could not be followed for 24 months after surgery, 1 patient who suffered a bilateral ACL tear and received simultaneous bilateral ACL reconstruction, and 9 patients who were reconstructed using BTB graft were excluded from the control group. Ultimately, 84 patients were included in the control group (conventional group) (Figure 2 and Table 1).
Figure 2.
Study flowchart. ACL, anterior cruciate ligament, BTB, bone–patellar tendon–bone .
Table 1.
Demographic Data of Study Patients a
| All-Epiphyseal (n = 18) |
Conventional (n = 84) |
P | |
|---|---|---|---|
| Age at the time of surgery, y | 12.4 ± 1.2 | 14.1 ± 0.9 | <.001 |
| Sex, n (%) | |||
| Female | 10 (56) | 75 (89) | .002 |
| Male | 8 (44) | 9 (11) | |
| Height, cm | 160.4 ± 8.0 | 160.0 ± 5.8 | .792 |
| Weight, kg | 52.2 ± 13.0 | 55.2 ± 6.6 | .371 |
| Body mass index, kg/m2 | 20.0 ± 3.4 | 21.6 ± 2.5 | .059 |
| Time from injury to surgery, weeks | 17.8 ± 32.3 | 9.9 ± 14.3 | .353 |
| Follow-up period, months | 41.6 ± 20.1 | 38.2 ± 20.1 | .530 |
| Meniscus injury, n (%) | .948 | ||
| LM | 7 (39) | 29 (46) | |
| MM | 2 (11) | 13 (21) | |
| LM and MM | 4 (22) | 21 (33) | |
| Cartilage injury, n | 0 | 0 | |
| Surgical time, min | 71.5 ± 9.1 | 64.4 ± 15.3 | .061 |
a Data are reported as mean ± SD unless otherwise indicated. Bold P values indicate statistically significant difference between groups (P < .05). LM, lateral meniscus; MM, medial meniscus.
Statistical Analysis
Variable normality was determined using the Shapiro-Wilk test. Clinical assessments, including knee ROM and side-to-side difference in anterior tibial translation pre- and postsurgery, were compared using the Wilcoxon test. The distribution of Lachman test and pivot-shift test grades was compared by chi-square test. Muscle strength recovery was analyzed by 1-way analysis of variance (ANOVA) and Tukey post hoc analysis.
The number of concomitant meniscal injuries, the incidence of postoperative radiographic angular deformity, and second ACL injury were compared with the chi-square test. Muscle strength recovery was compared for time effect and surgical procedure effect by 2-way ANOVA; P < .05 was considered statistically significant. To achieve 80% statistical power with an α of .05 in demonstrating moderate effect size (ρ = 0.5), power analysis revealed that a minimum of 26 and 119 patients in the all-epiphyseal and conventional group, respectively, would be required to detect any differences in clinical outcomes of knee stability. In this study, the power was 0.697 with an α of .05 demonstrating medium effect size (P = .5). All statistical analyses were performed with Statistical Package for the Social Sciences (Version 27.0; SPSS Inc).
Results
At 24 months after surgery, knee extension and flexion ROM was 2.9° ± 4.3° and 149.6° ± 3.6°, respectively, in the all-epiphyseal group and 1.4° ± 3.7° and 148.8° ± 3.2°, respectively, in the conventional group. The KT-1000 arthrometer side-to-side difference improved significantly from 6.1 ± 2.4 to 0.6 ± 0.9 mm in the all-epiphyseal group (P = .001), and from 5.7 ± 2.2 to 0.4 ± 0.8 mm in the conventional group (P < .001). There was no significant difference between groups at 24 months after surgery (P = .518). No cases in the all-epiphyseal group showed grade 2 or 3 in the Lachman test and pivot-shift test at 24 months after surgery. However, the frequency of a grade 1 Lachman was significantly higher in the all-epiphyseal group (P = .042). The postoperative grade 1 pivot shift was more common in the all-epiphyseal group than in the conventional group (22% versus 4%, respectively) but did not reach significance (P = .074) (Table 2). In the KOOS assessment, there was no significant difference on any subscale (Table 3).
Table 2.
Results of Lachman Test and Pivot-Shift Test a
| All-Epiphyseal | Conventional | Pb | |||
|---|---|---|---|---|---|
| Preop | 24 Mo Postop | Preop | 24 Mo Postop | ||
| Lachman test | .042 | ||||
| Grade 0 | 0 (0) | 12 (80) | 0 (0) | 64 (97) | |
| Grade 1 | 0 (0) | 3 (20) | 0 (0) | 2 (3) | |
| Grade 2 | 6 (33) | 0 (0) | 36 (43) | 0 (0) | |
| Grade 3 | 12 (67) | 0 (0) | 48 (57) | 0 (0) | |
| Pivot-shift test | .074 | ||||
| Grade 0 | 0 (0) | 12 (78) | 0 (0) | 63 (96) | |
| Grade 1 | 0 (0) | 3 (22) | 17 (20) | 3 (4) | |
| Grade 2 | 8 (44) | 0 (0) | 44 (53) | 0 (0) | |
| Grade 3 | 10 (56) | 0 (0) | 23 (27) | 0 (0) | |
a Data are presented as No. of patients (%). Postop, postoperatively; preop, preoperatively.
bP value comparing results between groups at 24 months postoperatively.
Table 3.
Results of KOOS Assessment at Final Follow-up a
| KOOS Subscale | All-Epiphyseal | Conventional | P |
|---|---|---|---|
| Pain | 97.0 ± 3.8 | 96.8 ± 4.9 | .883 |
| Symptoms | 93.5 ± 8.6 | 92.5 ± 8.9 | .730 |
| ADL | 99.6 ± 1.0 | 98.9 ± 2.9 | .191 |
| Sport/recreation | 97.3 ± 4.1 | 94.2 ± 8.5 | .107 |
| QOL | 92.6 ± 8.8 | 89.1 ± 9.6 | .265 |
a ADL, activities of daily living; KOOS, Knee Injury and Osteoarthritis and Outcome Score; QOL, quality of life.
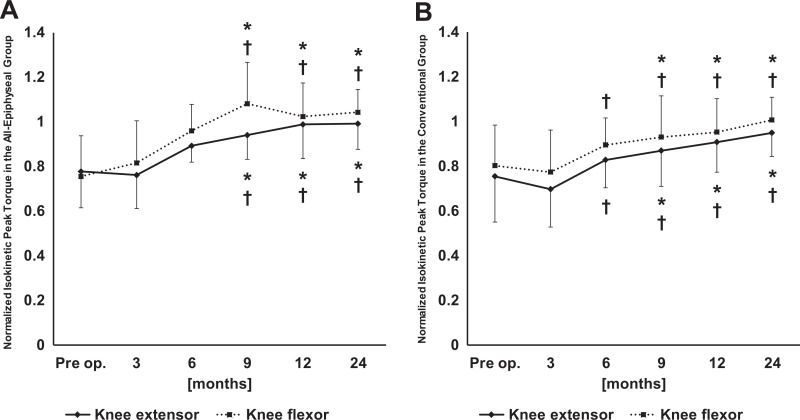
In the all-epiphyseal group, knee extensor and flexor strength increased significantly over time (P < .001 for both ) (Figure 3). At 24 months after surgery, there was no significant difference in normalized knee extensor (0.99 ± 0.11 in all-epiphyseal and 0.95 ± 0.10 in conventional group) and flexor strength (1.04 ± 0.10 in all-epiphyseal and 1.01 ± 0.12 in conventional group) between groups (P = .433 and P = .240, respectively).
Figure 3.
Recovery in the normalized isokinetic peak torque of the knee extensor and flexor in the (A) all-epiphyseal and (B) conventional group. *P < .05 when comparing with preoperatively (Pre op.); † P < .05 when comparing with 3 months after surgery.
In the radiographic assessment, there were no significant differences in the amount of change in FTA at final follow-up between the all-epiphyseal (−1.6° ± 3.1° on the involved side and −1.6° ± 1.6° on the uninvolved side) and conventional (−1.0° ± 1.9° on the involved side and 0.2° ± 1.5° on the uninvolved side) groups (P = .516 and P = .068, respectively). The postoperative angular deformity (>3° of side-to-side difference in FTA) was observed in 4 of 15 patients (26.7%) in the all-epiphyseal group and 4 of 66 patients (6.1%) in the conventional group; there was a significant difference between the 2 groups (P = .035) (Table 4). There were no symptomatic cases, and no cases required additional surgery for lower limb deformity during follow-up periods.
Table 4.
Details of Patients Who Demonstrated Radiographic Angular Deformity a
| Patient | Age, y | Sex | BMI, kg/m2 | Time From Injury to Surgery, wk | Preoperative Status of Epiphyseal Line | Surgical Procedure | Concomitant Surgery | Side-to-Side Difference in FTA,°b |
|---|---|---|---|---|---|---|---|---|
| 1 | 11 | Female | 17.2 | 3 | Open | All-epiphyseal | None | −8 |
| 2 | 13 | Male | 18.3 | 5 | Open | All-epiphyseal | None | 5 |
| 3 | 14 | Male | 22.3 | 5 | Open | All-epiphyseal | MM repair | 4 |
| 4 | 14 | Male | 20.6 | 141 | Open | All-epiphyseal | MM and LM repair | −6 |
| 5 | 12 | Female | 23.4 | 12 | Central physis close | Conventional | None | −4 |
| 6 | 14 | Male | 19.8 | 4 | Central physis close | Conventional | MM repair | 4 |
| 7 | 15 | Female | 22.8 | 2 | Close | Conventional | None | 5 |
| 8 | 15 | Female | 23.9 | 48 | Close | Conventional | MM repair | 4 |
a BMI, body mass index; FTA, femorotibial angle; LM lateral meniscus; MM, medial meniscus.
b Healthy side minus injured side.
In the all-epiphyseal group, 3 ipsilateral graft ruptures (16.7%; 10.0 ± 1.6 months after surgery) and 2 contralateral ACL injuries (11.1%; 30.0 ± 18.0 months after surgery) occurred during the follow-up period. In the conventional group, 20 ipsilateral graft ruptures (23.8%; 21.9 ± 14.3 months after surgery) and 12 contralateral ACL injuries (14.3%; 31.0 ± 14.0 after surgery) occurred during the follow-up period. There was no significant difference between groups in the incidence of ipsilateral graft rupture (P = .757) and contralateral ACL injury (P ≥ .999).
Discussion
The most important finding of this study was that an equivalent clinical outcome, including in subjective knee score and incidence of second ACL injury, was obtained between all-epiphyseal and conventional techniques of DB-ACL reconstruction. However, a higher incidence of residual laxity and postoperative angular deformity was observed in all-epiphyseal DB-ACL reconstructions when compared with conventional ACL reconstructions.
Most ACL reconstruction techniques for pediatric patients with open physes reported previously were SB reconstructions using soft tissue graft. 2,15,22 It is well-known that the native ACL has 2 bundles with different functions. 11,36,45,50 Previous anatomic studies have demonstrated that the femoral insertion is oval shaped 37 and the tibial insertion is C-shaped. 42 It may be difficult to reproduce the shape of such insertions using single round tunnel reconstruction or the over-the-top technique. Although a recent meta-analysis concluded that there was no significant difference in knee functional score, AP stability, or retear rate between DB and SB-ACL reconstruction, rotational stability was superior in DB-ACL reconstruction. 12 Therefore, our institution has a strategy of performing DB-ACL reconstruction as much as possible, even in patients with open physes.
Koizumi et al 18 suggested physeal-sparing DB-ACL reconstruction for pediatric patients. In their technique, the AMB was reconstructed by the over-the-top technique and the PLB was reconstructed by the all-epiphyseal technique. Although the clinical outcome was similar to that of ACL reconstructions in adults, positive results from a postoperative Lachman test and pivot-shift test were observed in 13% and 20% of patients, respectively. 18 In our study, 20% and 22% of patients in the all-epiphyseal group showed postoperative grade 1 positive results from the Lachman and pivot-shift tests. Although a significant difference between the 2 groups was observed only in the Lachman test, considering the number and percentage of distribution, the all-epiphyseal technique might be inferior to the conventional technique in both the Lachman and the pivot-shift test.
The reasons that residual knee instability remains at a higher rate in the all-epiphyseal technique may be multifactorial and might include the technical difficulty of this technique, the direction of bone tunnel (graft bending angle), smaller sized grafts, or patients with high activity. Equivalent outcomes were obtained in both groups regarding subjective knee function and muscle strength recovery; however, the possibility of residual knee instability after surgery should be noted by the orthopaedic surgeon before performing ACL reconstruction for patients with open physes, and informed consent should be given by patients and parents.
One possible reason for the high incidence of postoperative positive Lachman or pivot-shift test results in the all-epiphyseal group may be that the all-epiphyseal group had a longer waiting period for surgery. In our department, the treatment strategy for patients with an open physis without concomitant injury is delayed reconstruction. It has been reported that AP instability or rotational instability increases with time from injury. 23,29,46 In addition, it has been reported that greater preoperative laxity is associated with a risk of postoperative pivot shift. 52 Since the number of patients in the all-epiphyseal group in this study was small, it was difficult to examine the effect of preoperative chronicity on postoperative results.
Critical issues in pediatric ACL reconstruction include postoperative growth disturbance or angular deformity. The risk of these complications can be minimized, but they are difficult to avoid completely, even in the physeal-sparing technique, which does not damage the epiphyseal line. 33 Although a systematic review comparing transphyseal and physeal-sparing techniques for pediatric patients concluded that there was no difference in the incidence of growth disturbance, the incidences of leg-length discrepancy and angular deformity were 0.81% and 0.61% in the transphyseal technique, and 1.2% and 0% in the physeal-sparing technique, respectively. 31 In a systematic review of 39 cases of patients with open physes who had a growth disturbance after ACL reconstruction, Collins et al 5 reported that the most common surgical technique causing growth disturbance on both the femur and the tibia was the transphyseal technique. However, although it was believed that the physeal-sparing technique had a low risk of postoperative complications, 25% of patients with angular malformation and 47% of patients with leg-length discrepancy had undergone ACL reconstruction with the physeal-sparing technique. Therefore, there might be underreporting of growth disturbance after ACL reconstruction in skeletally immature patients. In addition, Chambers et al 4 suggested a high incidence of postoperative growth disturbance among patients with >5 years of growth remaining.
The findings of the current study did not indicate a definitive conclusion; however, they revealed that angular deformity might not be completely avoided even in the all-epiphyseal technique. It seemed that various factors, such as high activity and invasion of immature bone, are involved. In our institution, postoperative computed tomography was performed in all cases to confirm the association between the location of the bone tunnel and the epiphyseal line. No cases were found in which the epiphyseal line was damaged in computed tomography; however, the possibility that the epiphyseal line was damaged by intraoperative procedures cannot be denied. The distal femoral physis might have been damaged in patients who had valgus deformity, and the proximal tibial physis might have been damaged in the patients who had varus deformity. In addition, it was considered that the long waiting period for surgery and cartilage degeneration due to meniscal tear might affect the angular deformity.
Furthermore, this study showed a relatively high incidence of angular deformity in the conventional group compared with previous reports. 31 Although the reason for this high incidence rate remains unclear, the status of the epiphyseal line on preoperative magnetic resonance imaging scans was centrally closed (not completely closed) in 2 of 4 patients in the control group. Central physis closure and complete closure of the epiphyseal line were observed in 39% and 61% patients of the control group in this study. Conventional DB-ACL reconstruction was performed on cases of central physis closure in our institution. However, there may be individual differences in growth remaining among these patients. In the future, it will be necessary to verify the safety of the transphyseal technique for such cases.
In this study, the incidence rate of graft rupture and contralateral ACL injury during the follow-up period was 16.7% and 11.1% in the all-epiphyseal group and 23.8% and 14.3% in the control group, respectively. Wong et al 49 conducted a meta-analysis of complications after pediatric ACL reconstruction and concluded that patients with rerupture require surgery at much higher rates than those with growth disturbance. Dekker et al 8 reported second-injury rates among patients younger than 18 years. In the minimum 2-year follow-up, the incidence of graft rupture was 19% and that of contralateral ACL injury was 13%. Regarding the second-injury rate after the all-epiphyseal technique, it was reported that the 4-year cumulative rates of graft rupture and contralateral ACL rupture were 18.2% and 6.63%, respectively. 14 Cordasco et al 6 performed SB-ACL reconstruction using the all-epiphyseal technique, partial transphyseal technique, and complete technique with each of the 3 groups divided according to skeletal age (mean age: 12, 14.3, and 16.2 years, respectively). The all-epiphyseal group showed a revision rate of 6%, which was significantly higher than that of the transphyseal group (20%).
Although there are differences in retear rate depending on the literature, competition level, or age, our results regarding the incidence rate of second injury were higher than that of previous reports. Regarding the incidence of postoperative retear, this study could not find any superiority in all-epiphyseal DB-ACL reconstruction compared with previously reported procedures or conventional DB-ACL reconstruction for skeletally mature patients. It has been reported that pediatric and adolescent patients are at increased risk for retear and contralateral injury compared with adults. 1,8 Pediatric patients of a younger age might have had a high second-injury rate because of their long competition period after surgery, or high activity, as evidenced by postoperative KOOS in our study. These results suggest the importance of reinjury prevention in this specific age group.
There were some limitations of this study. First, this study included a relatively limited number of patients in the all-epiphyseal group. This is because ACL tear in pediatric patients with wide open physes is relatively rare, and our treatment strategy is to perform ACL reconstruction after epiphyseal closure as much as possible. Inevitably, the number of cases who are reconstructed by the all-epiphyseal technique is limited in our institution. The power was insufficient in this study, and only limited results were obtained in comparison with other surgical procedures and other age groups. It was also not possible to derive superiority in comparison with other surgical procedures or other age groups. In this study, if the epiphyseal line was not closed at the time of occurrence of a new meniscal tear during the waiting period for surgery, all-epiphyseal DB-ACL reconstruction was performed, and these patients were included in the all-epiphyseal group. In addition, patients who were injured before the epiphyseal line was closed and were able to wait for surgery without concomitant injury were included in the conventional-repair control group. Since the duration of the waiting period for surgery may affect postoperative outcomes, it seems necessary to increase the number of cases and conduct a more detailed investigation in the future.
A second limitation was that the effect of the waiting period for surgery or concomitant injuries on postoperative outcomes, including knee stability or the incidence of postoperative retear in the all-epiphyseal group, was unclear. The chronicity of ACL tears is reported to correlate with meniscal tear, cartilage injury, 19,28 or increasing knee instability. 23,29,46 In the future, it will be crucial to examine this in detail in a sufficient number of cases. Third, leg-length discrepancy could not be evaluated because a plain long leg view radiograph was not taken in all cases. Although no patients complained about subjective symptoms of leg-length discrepancy, it was possible that radiographic leg-length discrepancy might have been present.
Conclusion
All-epiphyseal DB-ACL reconstruction for skeletally immature patients achieved satisfactory clinical outcomes in terms of subjective knee functional score and muscle strength recovery in comparison with conventional reconstruction. The incidence of ipsilateral graft rupture was relatively high in both groups with no significant difference between groups. Postoperative knee stability tended to be inferior, and the incidence of angular deformity was significantly higher in the all-epiphyseal group.
Footnotes
Final revision submitted July 4, 2021; accepted July 19, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Hirosaki University Graduate School of Medicine.
References
- 1. Abram SGF, Judge A, Beard DJ, Price AJ. Rates of adverse outcomes and revision surgery after anterior cruciate ligament reconstruction: a study of 104,255 procedures using the National Hospital Episode Statistics Database for England, UK. Am J Sports Med. 2019;47:2533–2542. doi: 10.1177/0363546519861393 [DOI] [PubMed] [Google Scholar]
- 2. Anderson AF. Transepiphyseal replacement of the anterior cruciate ligament using quadruple hamstring grafts in skeletally immature patients. J Bone Joint Surg Am. 2004;86(suppl 1):201–209. doi: 10.2106/00004623-200409001-00010 [DOI] [PubMed] [Google Scholar]
- 3. Beck NA, Lawrence JT, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139(3):e20161 877. doi: 10.1542/peds.2016-1877 [DOI] [PubMed] [Google Scholar]
- 4. Chambers CC, Monroe EJ, Allen CR, Pandya NK. Partial transphyseal anterior cruciate ligament reconstruction: clinical, functional, and radiographic outcomes. Am J Sports Med. 2019;47:1353–1360. doi: 10.1177/0363546519836423 [DOI] [PubMed] [Google Scholar]
- 5. Collins MJ, Arns TA, Leroux T, et al. Growth abnormalities following anterior cruciate ligament reconstruction in the skeletally immature patient: a systematic review. Arthroscopy. 2016;32:1714–1723. doi: 10.1016/j.arthro.2016.02.025 [DOI] [PubMed] [Google Scholar]
- 6. Cordasco FA, Black SR, Price M, et al. Return to sport and reoperation rates in patients under the age of 20 after primary anterior cruciate ligament reconstruction: risk profile comparing 3 patient groups predicated upon skeletal age. Am J Sports Med. 2019;47:628–639. doi: 10.1177/0363546518819217 [DOI] [PubMed] [Google Scholar]
- 7. Cordasco FA, Mayer SW, Green DW. All-inside, all-epiphyseal anterior cruciate ligament reconstruction in skeletally immature athletes: return to sport, incidence of second surgery, and 2-year clinical outcomes. Am J Sports Med. 2017;45:856–863. doi: 10.1177/0363546516677723 [DOI] [PubMed] [Google Scholar]
- 8. Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99:897–904. doi: 10.2106/jbjs.16.00758 [DOI] [PubMed] [Google Scholar]
- 9. Dodwell ER, LaMont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42:675–680. doi: 10.1177/0363546513518412 [DOI] [PubMed] [Google Scholar]
- 10. Frosch KH, Stengel D, Brodhun T, et al. Outcomes and risks of operative treatment of rupture of the anterior cruciate ligament in children and adolescents. Arthroscopy. 2010;26:1539–1550. doi: 10.1016/j.arthro.2010.04.077 [DOI] [PubMed] [Google Scholar]
- 11. Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint: anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;(106):216–231. doi: 10.1097/00003086-197501000-00033 [DOI] [PubMed] [Google Scholar]
- 12. Ishibashi Y, Adachi N, Koga H, et al. Erratum to “Guideline Japanese Orthopaedic Association 2019 guidelines for anterior cruciate ligament injuries” (3rd edition) [Journal of Orthopaedic Science, 25(Jan 2020) 6—. J Orthop Sci. 2020:S0949-2658(20): 30177–9. doi: 10.1016/j.jos.2020.07.001 [DOI] [PubMed] [Google Scholar]
- 13. Ishibashi Y, Sasaki S, Sasaki E, Kimura Y, Yamamoto Y, Tsuda E. All-epiphyseal double-bundle anterior cruciate ligament reconstruction for skeletally immature patients. Arthrosc Tech. 2020;9(12):e1993–e2000. doi: 10.1016/j.eats.2020.08.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kay J, Memon M, Marx RG, Peterson D, Simunovic N, Ayeni OR. Over 90% of children and adolescents return to sport after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26:1019–1036. doi: 10.1007/s00167-018-4830-9 [DOI] [PubMed] [Google Scholar]
- 15. Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am. 2005;87:2371–2379. doi: 10.2106/00004623-200511000-00001 [DOI] [PubMed] [Google Scholar]
- 16. Kocher MS, Heyworth BE, Fabricant PD, Tepolt FA, Micheli LJ. Outcomes of physeal-sparing ACL reconstruction with iliotibial band autograft in skeletally immature prepubescent children. J Bone Joint Surg Am. 2018;100:1087–1094. doi: 10.2106/jbjs.17.01327 [DOI] [PubMed] [Google Scholar]
- 17. Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89:2632–2639. doi: 10.2106/jbjs.f.01560 [DOI] [PubMed] [Google Scholar]
- 18. Koizumi H, Kimura M, Kamimura T, Hagiwara K, Takagishi K. The outcomes after anterior cruciate ligament reconstruction in adolescents with open physes. Knee Surg Sports Traumatol Arthrosc. 2013;21:950–956. doi: 10.1007/s00167-012-2051-1 [DOI] [PubMed] [Google Scholar]
- 19. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582–2587. doi: 10.1177/0363546511420818 [DOI] [PubMed] [Google Scholar]
- 20. Lawrence JT, Bowers AL, Belding J, Cody SR, Ganley TJ. All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Clin Orthop Relat Res. 2010;468:1971–1977. doi: 10.1007/s11999-010-1255-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liddle AD, Imbuldeniya AM, Hunt DM. Transphyseal reconstruction of the anterior cruciate ligament in prepubescent children. J Bone Joint Surg Br. 2008;90:1317–1322. doi: 10.1302/0301-620x.90b10.21168 [DOI] [PubMed] [Google Scholar]
- 22. Lipscomb AB, Anderson AF. Tears of the anterior cruciate ligament in adolescents. J Bone Joint Surg Am. 1986;68:19–28. doi: 10.2106/00004623-198668010-00004 [PubMed] [Google Scholar]
- 23. Mishima S, Takahashi S, Kondo S, Ishiguro N. Anterior tibial subluxation in anterior cruciate ligament-deficient knees: quantification using magnetic resonance imaging. Arthroscopy. 2005;21:1193–1196. doi: 10.1016/j.arthro.2005.07.008 [DOI] [PubMed] [Google Scholar]
- 24. Mizuta H, Kubota K, Shiraishi M, Otsuka Y, Nagamoto N, Takagi K. The conservative treatment of complete tears of the anterior cruciate ligament in skeletally immature patients. J Bone Joint Surg Br. 1995;77:890–894. doi: 10.1302/0301-620x.77b6.7593101 [PubMed] [Google Scholar]
- 25. Moksnes H, Engebretsen L, Eitzen I, Risberg MA. Functional outcomes following a non-operative treatment algorithm for anterior cruciate ligament injuries in skeletally immature children 12 years and younger. A prospective cohort with 2 years follow-up. Br J Sports Med. 2013;47:488–494. doi: 10.1136/bjsports-2012-092066 [DOI] [PubMed] [Google Scholar]
- 26. Moksnes H, Engebretsen L, Risberg MA. Prevalence and incidence of new meniscus and cartilage injuries after a nonoperative treatment algorithm for ACL tears in skeletally immature children: a prospective MRI study. Am J Sports Med. 2013;41:1771–1779. doi: 10.1177/0363546513491092 [DOI] [PubMed] [Google Scholar]
- 27. Nawabi DH, Jones KJ, Lurie B, Potter HG, Green DW, Cordasco FA. All-inside, physeal-sparing anterior cruciate ligament reconstruction does not significantly compromise the physis in skeletally immature athletes: a postoperative physeal magnetic resonance imaging analysis. Am J Sports Med. 2014;42:2933–2940. doi: 10.1177/0363546514552994 [DOI] [PubMed] [Google Scholar]
- 28. Newman JT, Carry PM, Terhune EB, et al. Factors predictive of concomitant injuries among children and adolescents undergoing anterior cruciate ligament surgery. Am J Sports Med. 2015;43:282–288. doi: 10.1177/0363546514562168 [DOI] [PubMed] [Google Scholar]
- 29. Nishida K, Matsushita T, Hoshino Y, et al. The influences of chronicity and meniscal injuries on pivot shift in anterior cruciate ligament-deficient knees: quantitative evaluation using an electromagnetic measurement system. Arthroscopy. 2020;36:1398–1406. doi: 10.1016/j.arthro.2020.01.018 [DOI] [PubMed] [Google Scholar]
- 30. Pennock AT, Bomar JD, Manning JD. The creation and validation of a knee bone age atlas utilizing MRI. J Bone Joint Surg Am. 2018;100:e20. doi: 10.2106/jbjs.17.00693 [DOI] [PubMed] [Google Scholar]
- 31. Pierce TP, Issa K, Festa A, Scillia AJ, McInerney VK. Pediatric anterior cruciate ligament reconstruction: a systematic review of transphyseal versus physeal-sparing techniques. Am J Sports Med. 2017;45:488–494. doi: 10.1177/0363546516638079 [DOI] [PubMed] [Google Scholar]
- 32. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42:2769–2776. doi: 10.1177/0363546513510889 [DOI] [PubMed] [Google Scholar]
- 33. Robert HE, Casin C. Valgus and flexion deformity after reconstruction of the anterior cruciate ligament in a skeletally immature patient. Knee Surg Sports Traumatol Arthrosc. 2010;18:1369–1373. doi: 10.1007/s00167-009-0988-5 [DOI] [PubMed] [Google Scholar]
- 34. Roos EM, Roos HP, Ekdahl C, Lohmander LS. Knee injury and Osteoarthritis Outcome Score (KOOS)—validation of a Swedish version. Scand J Med Sci Sports. 1998;8:439–448. doi: 10.1111/j.1600-0838.1998.tb00465.x [DOI] [PubMed] [Google Scholar]
- 35. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88 [DOI] [PubMed] [Google Scholar]
- 36. Sakane M, Livesay GA, Fox RJ, Rudy TW, Runco TJ, Woo SY. Relative contribution of the ACL, MCL, and bony contact to the anterior stability of the knee. Knee Surg Sports Traumatol Arthrosc. 1999;7:93–97. doi: 10.1007/s001670050128 [DOI] [PubMed] [Google Scholar]
- 37. Sasaki N, Ishibashi Y, Tsuda E, et al. The femoral insertion of the anterior cruciate ligament: discrepancy between macroscopic and histological observations. Arthroscopy. 2012;28:1135–1146. doi: 10.1016/j.arthro.2011.12.021 [DOI] [PubMed] [Google Scholar]
- 38. Sasaki S, Tsuda E, Hiraga Y, et al. Prospective randomized study of objective and subjective clinical results between double-bundle and single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:855–864. doi: 10.1177/0363546515624471 [DOI] [PubMed] [Google Scholar]
- 39. Sasaki T, Ishibashi Y, Okamura Y, Toh S, Sasaki T. MRI evaluation of growth plate closure rate and pattern in the normal knee joint. J Knee Surg. 2002;15:72–76. [PubMed] [Google Scholar]
- 40. Seil R, Robert H. VKB-Plastik bei offenen Wachstumsfugen. Arthroskopie. 2005;18:48–52. doi: 10.1007/s00142-004-0288-5 [Google Scholar]
- 41. Shea KG, Burlile JF, Richmond CG, et al. Quadriceps tendon graft anatomy in the skeletally immature patient. Orthop J Sports Med. 2019;7:2325967119856578. doi: 10.1177/2325967119856578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Siebold R, Schuhmacher P, Fernandez F, et al. Flat midsubstance of the anterior cruciate ligament with tibial “C”-shaped insertion site. Knee Surg Sports Traumatol Arthrosc. 2015;23:3136–3142. doi: 10.1007/s00167-014-3058-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Streich NA, Barié A, Gotterbarm T, Keil M, Schmitt H. Transphyseal reconstruction of the anterior cruciate ligament in prepubescent athletes. Knee Surg Sports Traumatol Arthrosc. 2010;18:1481–1486. doi: 10.1007/s00167-010-1057-9 [DOI] [PubMed] [Google Scholar]
- 44. Sugimoto D, Whited AJ, Brodeur JJ, et al. Long-term follow-up of skeletally immature patients with physeal-sparing combined extra-/intra-articular iliotibial band anterior cruciate ligament reconstruction: a 3-dimensional motion analysis. Am J Sports Med. 2020;48:1900–1906. doi: 10.1177/0363546520927399 [DOI] [PubMed] [Google Scholar]
- 45. Takai S, Woo SL, Livesay GA, Adams DJ, Fu FH. Determination of the in situ loads on the human anterior cruciate ligament. J Orthop Res. 1993;11:686–695. doi: 10.1002/jor.1100110511 [DOI] [PubMed] [Google Scholar]
- 46. Tanaka Y, Kita K, Takao R, et al. Chronicity of anterior cruciate ligament deficiency, part 1: effects on the tibiofemoral relationship before and immediately after anatomic ACL reconstruction with autologous hamstring grafts. Orthop J Sports Med. 2018;6:2325967117750813. doi: 10.1177/2325967117750813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Todd DC, Ghasem AD, Xerogeanes JW. Height, weight, and age predict quadriceps tendon length and thickness in skeletally immature patients. Am J Sports Med. 2015;43:945–952. doi: 10.1177/0363546515570620 [DOI] [PubMed] [Google Scholar]
- 48. Vavken P, Murray MM. Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy. 2011;27:704–716. doi: 10.1016/j.arthro.2010.11.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wong SE, Feeley BT, Pandya NK. Complications after pediatric ACL reconstruction: a meta-analysis. J Pediatr Orthop. 2019;39:e566–e571. doi: 10.1097/BPO.0000000000001075 [DOI] [PubMed] [Google Scholar]
- 50. Xerogeanes JW, Takeda Y, Livesay GA, et al. Effect of knee flexion on the in situ force distribution in the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 1995;3:9–13. doi: 10.1007/bf01553518 [DOI] [PubMed] [Google Scholar]
- 51. Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660–666. doi: 10.1177/03635465020300050501 [DOI] [PubMed] [Google Scholar]
- 52. Yamamoto Y, Tsuda E, Maeda S, et al. Greater laxity in the anterior cruciate ligament-injured knee carries a higher risk of postreconstruction pivot shift: intraoperative measurements with a navigation system. Am J Sports Med. 2018;46:2859–2864. doi: 10.1177/0363546518793854 [DOI] [PubMed] [Google Scholar]