Abstract
Background:
There is no consensus how to determine the varus laxity due to the LCL injury using the ultrasonography. There is a risk of lateral collateral ligament injury during or after arthroscopic extensor carpi radialis brevis release for tennis elbow. The equator of the radial head has been suggested as a landmark for the safe zone to not increase this risk; however, the safe zone from the intra-articular space has not been established.
Hypothesis:
Increased elbow varus laxity due to lateral collateral ligament–capsular complex (LCL-cc) injury could be assessed reliably via ultrasound.
Study Design:
Descriptive laboratory study.
Methods:
Eight cadaveric elbows were evaluated using a custom-made machine allowing passive elbow flexion under gravity varus stress. The radiocapitellar joint (RCJ) space was measured via ultrasound at 30° and 90° of flexion during 4 stages: intact elbow (stage 0), release of the anterior one-third of the LCL-cc (stage 1), release of the anterior two-thirds (stage 2), and release of the entire LCL-cc (stage 3). Two observers conducted the measurements separately, and the mean RCJ space in the 3 LCL-cc injury models (stages 1-3) at both flexion angles was compared with that of the intact elbow (stage 0). We also compared the measurements at 30° versus 90° of flexion.
Results:
At 30° of elbow flexion, the RCJ space increased 2 mm between stages 0 and 2 (95% confidence interval [CI], 1-3 mm; P < .01) and 4 mm between stages 0 and 3 (95% CI, 2-5 mm; P < .01). At 90° of elbow flexion, the RCJ space increased 1 mm between stages 0 and 2 (95% CI, 1-2 mm; P < .01) and 2 mm between stages 0 and 3 (95% CI, 2-3 mm; P < .01).
Conclusion:
Elbow varus laxity under gravity stress can be reliably assessed via ultrasound by measuring the RCJ space.
Clinical Relevance:
Because ultrasonographic measurement of the RCJ space can distinguish the increasing varus laxity seen with release of two-thirds or more of the LCL-cc, the anterior one-third of the LCL-cc, based on the diameter of the radial head, can be considered the safe zone in arthroscopic extensor carpi radialis brevis release for tennis elbow.
Keywords: lateral collateral ligament, elbow, varus laxity, diagnostic ultrasound, biomechanics
Extensor carpi radialis brevis (ECRB) release has been a reliable procedure to manage lateral epicondylitis by eliminating the pathologic tissue around the ECRB origin. Arthroscopic ECRB release reduces the surgical scar and offers the advantage of detecting associated intra-articular pathologies, such as synovial plicae or degenerative tissue. 4,12,19 However, this procedure can risk injury to the lateral collateral ligament (LCL)–capsular complex (LCL-cc) since the LCL-cc and the most proximal part of the ECRB are parallel and overlap along their proximal insertion. 8,13,23 In addition, if a partial injury to the LCL-cc occurs during arthroscopic ECRB release, the remaining structure might theoretically attenuate over time, given the repetitive gravity varus loading stress that occurs in the elbow with most activities of daily living.
Dynamic fluoroscopic examination traditionally has been used as the imaging modality of choice to determine elbow laxity. 17,21 However, there is still a paucity of data on the method for creating the varus stress and the position of the forearm and the elbow during dynamic fluoroscopy. Sonographic assessment for posterolateral rotatory stress was previously studied by Camp et al 7 using measurement of the posterolateral ulnohumeral distance at rest and during manual stress at 4 stages of increasing instability. Studies 9,10 have documented the ability of ultrasound to image the soft tissue and bony structures about the lateral elbow, as well as to assist in the diagnosis and management of lateral elbow disorders affecting the common extensor tendons and the radiocapitellar joint (RCJ). Although previous studies 10,24,25 have reported on the ultrasonographic evaluation of the lateral elbow ligaments in cadavers and healthy volunteers, the ability of ultrasound to detect varus laxity under gravity stress after LCL injury has not been investigated formally.
The purposes of this study were to determine (1) whether elbow varus laxity as evidenced by widening of the RCJ space can be assessed reliably via ultrasound and (2) whether ultrasound can distinguish between the intact elbow and that with mild or severe elbow varus laxity attributed to LCL-cc injury. We hypothesized that the RCJ space could be measured reliably via ultrasound and that the extent of RCJ widening would increase with the severity of the LCL-cc injury, becoming more apparent at 30° than at 90° of elbow flexion.
Methods
Included in this study were 8 fresh-frozen cadaveric upper limbs (4 right and 4 left) from the fingertip to the mid-humerus. Specimens were donated to the anatomy program of our institute. The mean ± standard deviation age of the 8 specimens was 84 ± 10 years. None of the specimens had a flexion contracture >10°, a pronation-supination rotation arc <140°, or radiologic evidence of arthritis or deformity. Any specimen with ligament insufficiency was excluded (detected by performing the posterolateral rotatory drawer test 15 or after direct visualization of the ligaments). Any intra-articular loose bodies were removed. Any specimen with any obvious bony deformity that limited the range of motion or normal articular contact was excluded. Any specimen with cartilage erosion to the subchondral bone (Outerbridge grade 4) was also excluded, but we did not discard specimens exhibiting shallow erosion with fibrillation or fissuring (Outerbridge grades 2-3) with normal joint contact. This study was performed with the approval of our institutional Biospecimen Subcommittee.
Specimen Preparation
The specimens were thawed at room temperature overnight. The skin and subcutaneous fat were removed from the mid-humerus to 5 cm distal to the elbow joint. The biceps, brachialis, and triceps muscle bellies were removed, while their tendon insertions were preserved. The common flexor and extensor humeral origins were preserved. For this experiment, the LCL-cc was defined as the LCL, the annular ligament, and the lateral capsule, and the anterior and posterior boundaries of the LCL-cc were defined as the anterior and posterior margins of the radial head. The capsule anterior to the radial head was excised, with care taken not to injure the LCL-cc. A medial column humeral osteotomy was made to open the joint (Figure 1A).
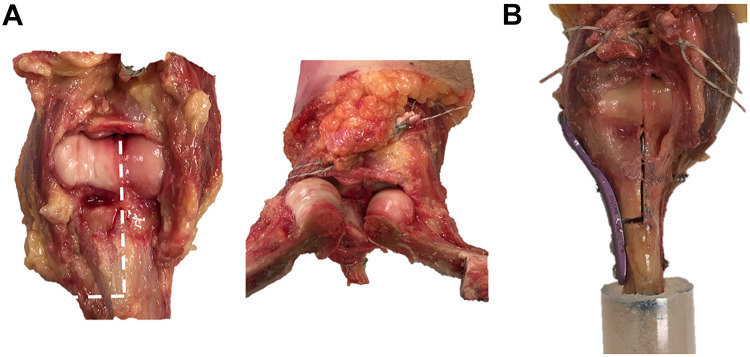
Figure 1.
(A) A medial column humeral osteotomy was made to open the radiocapitellar joint. (B) Before cutting, we fixed the distal humerus using an anatomic distal humerus plate with 4 screws along the medial cortex of the distal humerus. The proximal humeral end of the specimen was then potted into a cylindrical fiberglass sleeve in parallel to its long axis using polyurethane resin. Images reproduced with permission from the Mayo Foundation for Medical Education and Research. All rights reserved.
Before cutting, we prefixed the distal humerus using an anatomic distal humerus plate (Acumed Medial Column Plate) with 4 screws (1 AO 3.5-mm cancellous screw for intercondylar fixation and 3 AO 3.5-mm cortical screws for distal humerus fixation; Arbeitsgemeinschaft für Osteosynthesefragen) along the medial cortex of the distal humerus (Figure 1B). The proximal humeral end of the specimen was then potted into a cylindrical fiberglass sleeve in parallel to its long axis using polyurethane resin (Smooth-Cast 65D; Techno-Industrial Products) (Figure 1B) to affix the specimen onto the testing machine (Figure 2).
Figure 2.
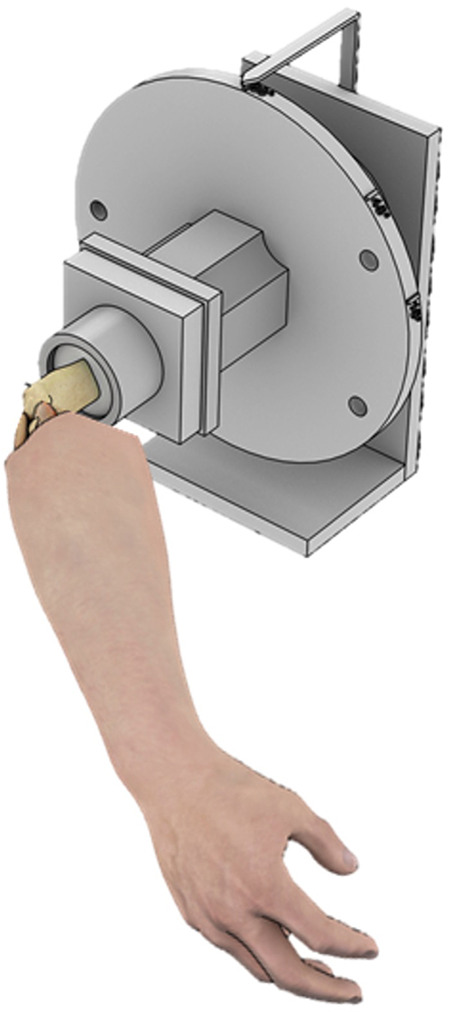
The humerus was held by a chuck in the center of a wheel that could be rotated to control the humeral rotation at 90°. Image reproduced with permission from the Mayo Foundation for Medical Education and Research. All rights reserved.
Specimen Mounting and Sequential Injury Model
Specimens were mounted in a custom apparatus to mimic elbow flexion with the shoulder at 90° of forward flexion and 90° of internal rotation. In other words, the humerus was horizontal with the lateral epicondyle upward and the transcondylar axis perpendicular to the floor such that the elbow was under a constant varus gravitational torque (Figure 2). The forearm was placed in pronation and confirmed to remain there under the influence of gravity throughout the stages of testing.
The RCJ space was measured, as described in the next section, with the elbow at 30° and 90° of flexion (position confirmed using a handheld goniometer) before and after creating the LCL-cc injury model. The overlying common extensor tendon was separated from the LCL-cc by bluntly dissecting between the two from anterior to posterior at the level of the RCJ. The LCL-cc was cut in 3 stages: anterior one-third of the LCL-cc (stage 1), anterior two-thirds of the LCL-cc (stage 2), and entire LCL-cc (stage 3). To calculate each cut of the LCL-cc, the anterior-posterior diameter of the radial head was measured using a digital caliper (with the forearm temporarily in neutral rotation) and divided into thirds (Figure 3). Intact (stage 0) measurements were obtained before separating the common extensor tendon and underlying LCL-cc as defined earlier.
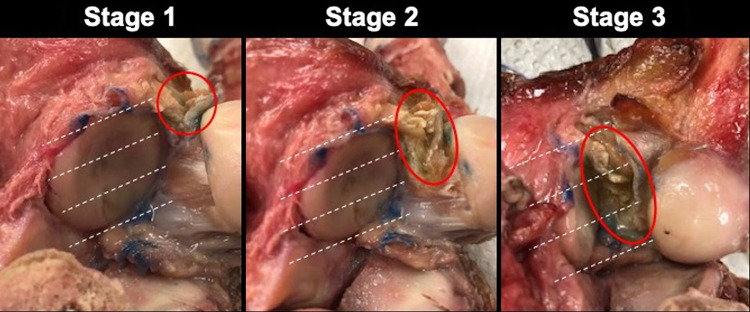
Figure 3.
Sequential lateral collateral ligament–capsular complex (LCL-cc) injury model. The LCL-cc was cut in 3 stages: anterior one-third (stage 1), anterior two-thirds (stage 2), and entire complex (stage 3). To calculate each cut of the LCL-cc for each stage (circled in red), the anterior-posterior diameter of the radial head was measured using a digital caliper (with the forearm temporarily in neutral rotation) and divided into thirds (white dotted lines). Images reproduced with permission from the Mayo Foundation for Medical Education and Research. All rights reserved.
Joint Space Measurement
The sonographic measurements were obtained by 2 orthopaedic surgeons (J.M.K. and D.R.) using an ultrasound machine and linear array transducer (12-5 MHz; SonoSite M-Turbo). The ultrasound transducer was centered in the coronal plane, perpendicular to the radial head, at the midpoint of the RCJ to provide the most distinct bony articular margins (Figure 4). The basic principle of the sonographic measurement used in this study was based on a previously published sonographic technique. 7
Figure 4.
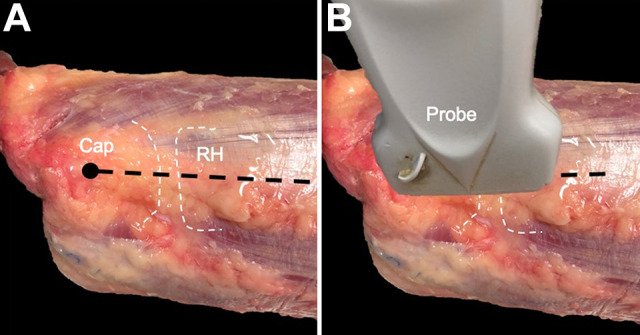
(A) White dotted lines indicate the outlines of the capitellum (Cap) and radial head (RH); the black dot, the most prominent point of the lateral epicondyle; and the black dashed line, the center of the radiocapitellar joint. (B) The ultrasound transducer was positioned to provide the most distinct bony margins of the radiocapitellar joint by bridging the ultrasound probe from the lateral epicondyle to the center of the radial head and by orienting the ultrasound probe approximately parallel to the long axis of the radius. Images reproduced with permission from the Mayo Foundation for Medical Education and Research. All rights reserved.
The RCJ space was measured in millimeters using the electronic calipers on the ultrasound machine. While maintaining the ultrasound probe as parallel as possible to the lateral-most edge of the radial head, the observers measured the distance from the most proximal point on the radial head closest to the ultrasound probe straight across proximally (in the horizontal plane of the image frame) to the nearest point on the capitellum (distance between lines B and C in Figure 5). The reference points used for RCJ gap measurement were left at the discretion of each observer. However, each observer used the same reference points for RCJ gap measurement during every experimental stage of LCL disruption in each specimen. For each specimen, the 2 observers measured the joint gap a minimum of 3 times at each experimental stage. Based on these measurements, a mean gap distance for each specimen was calculated at each stage for each observer. To maintain observer objectivity, the observers performed the measurements independently, with prior discussion of only the principles of what must be measured (ie, the RCJ space) and without discussing the methodology specifics.
Figure 5.
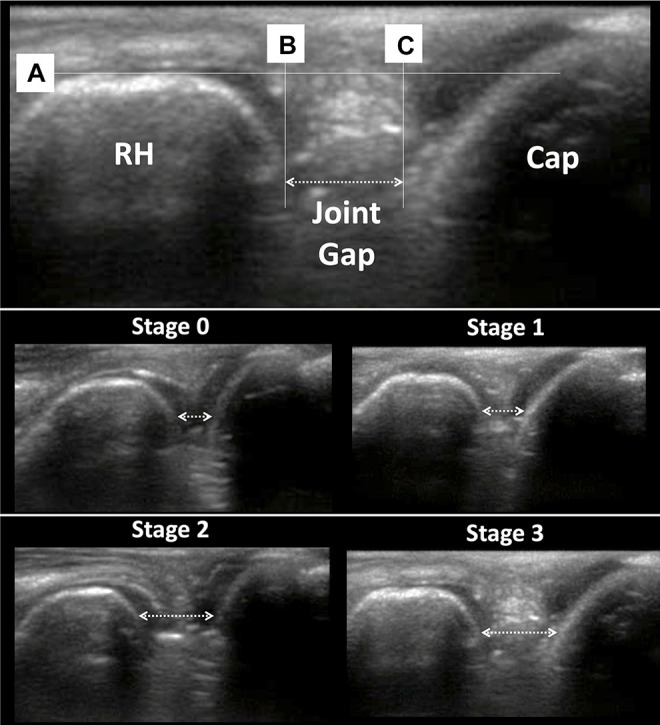
Measurement of the radiocapitellar joint space. Using a line parallel to the lateral border of the radial head (line A) as a reference, we defined the radiocapitellar joint space as the distance between a line perpendicular to A crossing the proximal edge of the radial head (line B) and a line parallel to B crossing the distal edge of capitellum (line C). This measurement was performed for each experimental condition tested: intact (stage 0), release of the anterior one-third of the lateral collateral ligament–capsular complex (stage 1), release of the anterior two-thirds (stage 2), and release of the entire complex (stage 3). Cap, capitellum; RH, radial head.
Statistical Analysis
All data, unless otherwise stated, are presented as means and 95% confidence intervals (CIs). All measurements were rounded to the nearest millimeter, and means and 95% CIs were also rounded to the nearest millimeter for effectiveness of communication and clinical relevance. The interobserver reliability of the RCJ space measurements was assessed using a 2-way mixed-effects, absolute-agreement, average-measures intraclass correlation coefficient to assess the agreement between observers. Measurement error was estimated using the standard error of measurement. The interobserver agreement in the change in RCJ space between consecutive stages of LCL disruption was assessed using a Bland-Altman analysis for repeated measures.
The data for stages 1 to 3 of the LCL-cc injury model were compared with the data for the intact elbow (stage 0) at each angle of elbow flexion (30° and 90°). Also, we compared the data collected at 30° of flexion with the data collected at 90° of flexion to assess whether differences between the 3 stages and the intact elbow varied as a function of the elbow flexion angle. The data were modeled using analysis of variance. All data were analyzed using 1- or 2-factor repeated-measures analysis of variance with post hoc comparisons using the Dunnett test or least-squares means and contrasts with Bonferroni corrections where appropriate. P values <.05 were considered to be significant. For example, based on Bonferroni p-value correction for multiple comparisons, P < .016 was considered to be significant for assessing increases in the radiocapitellar joint (RCJ) space between stage 0 (baseline) and each stage of sequential cutting of the lateral collateral ligament–capsular complex (stages 1-3). Statistical analysis was performed using JMP (Version 14; SAS Institute) and MedCalc Statistical Software (Version 19.6.4; MedCalc Software Ltd).
A power analysis revealed that with a sample size of 8, we had at least an 80% chance of detecting a statistical significance of 1.0 standard deviation between our experimental groups at P < .05. Power calculations were performed using G*Power Version 3.1 (Heinrich Heine Universität Düsseldorf).
Results
The interobserver reliability of the RCJ space measurements was good to excellent (intraclass correlation coefficient, 0.87; 95% CI, 0.79-0.92), and reliability was not affected by the elbow flexion angle (Table 1); therefore, data are presented as the average of the 2 observers. The standard error of the measurements between observers was 0.9 mm. The Bland-Altman analysis showed that there was no systematic bias (mean interobserver difference, 0 mm) between the observers in the measurements of the change in RCJ space between consecutive stages of LCL disruption (Figure 6).
Table 1.
Interobserver Reliability for RCJ Space Measurements a
| RCJ Space Measurement | ICC (95% CI) |
|---|---|
| All measurements | 0.87 (0.79-0.92) |
| At 30° of elbow flexion | 0.85 (0.70-0.92) |
| At 90° of elbow flexion | 0.91 (0.82-0.96) |
a ICC, intraclass correlation coefficient; RCJ, radiocapitellar joint.
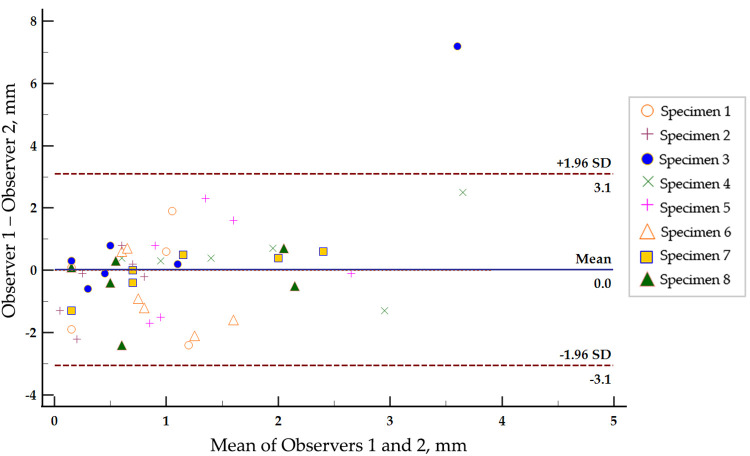
Figure 6.
Bland-Altman plot showing the interobserver differences in measurements of the change in radiocapitellar joint space during consecutive stages of progressive lateral collateral ligament disruption. The mean difference (bias) of the measurements between the observers (solid line) was 0 mm. The 95% limits of agreement (dashed lines) were –3.1 to 3.1 mm, and 65% of the differences between the observers were within 1 mm.
RCJ Space at 30° of Elbow Flexion
The RCJ space at 30° of elbow flexion increased progressively with sequential cutting of the LCL-cc (P < .001) (Table 2). Post hoc pairwise comparisons of the RCJ space between the intact model (stage 0) and each stage of sequential cutting of the LCL-cc (stages 1-3) demonstrated a nonsignificant increase of 1 mm in stage 1 (95% CI, –1 to 2 mm; P = .61) and significant increases of 2 mm (95% CI, 1-3 mm; P < .01) and 4 mm (95% CI, 2-5 mm; P < .01) in stages 2 and 3, respectively (Figure 7).
Table 2.
Difference in Radiocapitellar Joint Space Between Stages a
| 30° of Flexion | 90° of Flexion | |||
|---|---|---|---|---|
| MD (95% CI) | P | MD (95% CI) | P | |
| Stage 0 vs | ||||
| 1 | 1 (–1 to 2) | .61 | 0 (–1 to 1) | .14 |
| 2 | 2 (1 to 3) | <.01 | 1 (1 to 2) | <.01 |
| 3 | 4 (2 to 5) | <.01 | 2 (2 to 3) | <.01 |
| Stage 1 vs | ||||
| 2 | 1 (0 to 2) | .08 | 1 (0 to 2) | .02 |
| 3 | 3 (2 to 5) | <.01 | 2 (1 to 3) | <.01 |
| Stage 2 vs 3 | 2 (1 to 3) | .01 | 1 (1 to 2) | <.01 |
a Bold P values indicate statistical significance between stages (P < .05). MD, mean difference.
Figure 7.
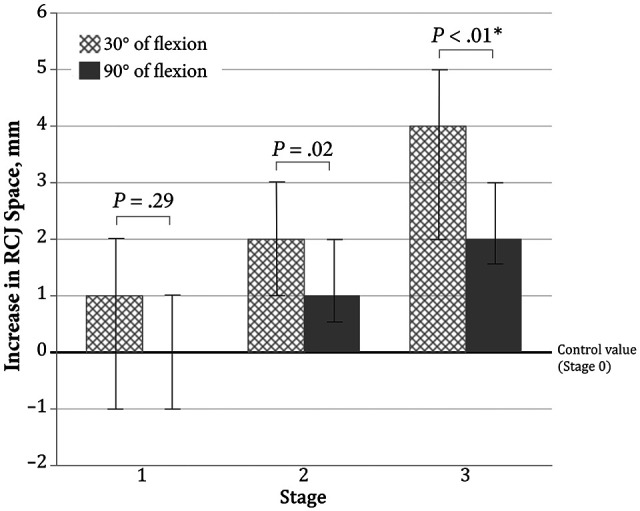
Increase in the radiocapitellar joint (RCJ) space (in millimeters) between stage 0 (baseline) and each stage of sequential cutting of the lateral collateral ligament–capsular complex (stages 1-3). Error bars indicate 95% CIs. *Statistically significant difference (P < .016 was considered significant according to Bonferroni correction for multiple comparisons).
RCJ Space at 90° of Elbow Flexion
As with the findings at 30° of elbow flexion, the RCJ space at 90° increased progressively with sequential cutting of the LCL-cc (P < .001) (Table 2). Similarly, the post hoc pairwise comparisons of the RCJ space between the intact model (stage 0) and each stage of sequential cutting of the LCL-cc (stages 1-3) demonstrated no increase in stage 1 (95% CI, –1 to 1 mm; P = .14) and significant increases of 1 mm (95% CI, 1-2 mm; P < .01) and 2 mm (95% CI, 2-3 mm; P < .01) in stages 2 and 3, respectively (Figure 7).
RCJ Space at 30° versus 90° of Elbow Flexion
The increase in the RCJ space was not significantly different between 30° and 90° of elbow flexion in stage 1 (1 mm at 30° vs 0 mm at 90°, P = .29) or in stage 2 (2 mm at 30° vs 1 mm at 90°, P = .02). However, after complete cutting of the LCL-cc (stage 3), the increase in the RCJ space was significantly greater at 30° than at 90° of elbow flexion (4 vs 2 mm, respectively, P < .01) (Figure 7).
Post Hoc Power Analysis
The post hoc power analysis revealed that with our sample size of 8, our chance of detecting a statistically significant difference between the experimental groups at P < .05 was >90% in all the comparisons shown in Table 2 with exception of stage 0 versus stage 1. For stage 0 versus stage 1, we had a 70% and 74% chance of detecting a statistically significant difference at 30° and 90° of flexion, respectively, at P < .05.
Discussion
The results of the present study show that elbow varus laxity can be reliably assessed using ultrasound to measure the RCJ space under gravity varus stress alone. As gravity is the minimum force that can reliably be applied to the elbow, the data with gravity force could be the baseline data used to assess varus instability attributed to LCL injury. According to our results, ultrasonographic measurement of the RCJ space can distinguish increasing varus laxity with increasing degrees of disruption of the LCL-cc.
The LCL complex is the soft tissue component that confers stability during varus stress of the elbow joint. The LCL complex origin is at the lateral epicondyle of the distal humerus and consists of 4 major structures: lateral ulnar collateral ligament, annular ligament, lateral radial collateral ligament, and accessory lateral collateral ligament. Although the increase in RCJ space seen using ultrasound was related to the severity of the LCL-cc disruption, statistically significant increases in elbow varus laxity were documented only with severe injury to the LCL-cc (two-thirds or more of the LCL-cc). The increase in varus laxity seen with disruption of the anterior one-third of the LCL-cc was small and not statistically significant, indicating that release of the anterior one-third of the LCL-cc during arthroscopic ECRB release should not result in a significant increase of elbow varus laxity. We did not specifically measure the effect of releasing one-half of the LCL-cc, so that remains unknown.
We evaluated the RCJ space in 2 positions of elbow flexion to determine whether the results varied as a function of the elbow flexion angle. These 2 angles of flexion reflect “the stable angle” (90°) versus “the less stable angle” (30°). In our cadaveric model, an increase in the RCJ space significantly differed as a function of the elbow flexion angle only when the entire LCL-cc was cut (stage 3). The increase in RCJ space in stage 3 was significantly higher when the elbow was positioned at 30° of flexion than at 90°. According to this finding, we suggest that measurements at 30° of elbow flexion would be more sensitive to evaluate elbow varus laxity; therefore, 30° of elbow flexion would be the preferred elbow position in further cadaveric or clinical studies on this topic.
This experimental cadaveric study has several limitations that warrant additional discussion, and clinicians should be cautious when extrapolating these results to clinical practice. First, given that soft tissue laxity in cadavers may be different from that in patients, it is possible that absolute values of the RCJ space in patients may be different from those presented here. While our model validated the hypothesis of a relative increase in varus elbow laxity as a function of an increase of the severity of the LCL-cc injury, clinical studies will be required to establish absolute values of RCJ space widening.
A second limitation is that, while the injury model affecting only the anterior one-third of the LCL-cc (stage 1) did not significantly increase the RCJ space, all measurements were made at time zero. In the clinical setting, the lateral elbow is subjected to repetitive varus stresses during activities of daily living, so it is possible that injuries affecting just the anterior one-third of the LCL-cc at time zero might theoretically progress to involve more of the LCL-cc over time. This would be consistent with what has been documented concerning repetitive valgus stresses on the medial side of the elbow leading to valgus instability. 1,6 Similarly, an intra-articular laxity sign attributed to degenerative changes of LCL-cc, probably induced by repetitive varus stresses, has been described. 2,3 However, it remains to be determined whether repetitive gravity varus stress would cause an increase in the severity of partial injuries of the LCL-cc and pathologic elbow varus laxity over time.
A third limitation is that varus laxity was measured only at the RCJ in this study. Therefore, the effect of the injury of the LCL-cc in the ulnohumeral joint space and its effect on posterolateral rotatory instability of the elbow remain unclear.
A fourth limitation is that, throughout the experiment, the forearm and wrist position remained unchanged in pronation and volar flexion. For standardizing the force, the elbow was mounted with 90° of internal rotation and 90° of forward flexion of the humerus. With the humerus in this position, the forearm naturally stayed pronated without any force except gravity. However, the position for the lateral pivot-shift test places the forearm in supination, thus, the pronated position of the forearm in this study could have diminished the amount of gapping that would have otherwise occurred. This position might have influenced the results presented here given that pronation and volar flexion with the elbow in extension result in stretching of the wrist extensors at their origin on the lateral humeral condyle. We observed in all specimens in this study stretching of the wrist extensors at the elbow in this position, and it is possible that the stretched wrist extensors affected the LCL-cc tensioning given their close anatomic relationship. 5,8,22 However, this observation has not been proven yet, and it remains unclear how the stretch in the wrist extensors origin affects the LCL-cc or the varus laxity of the elbow.
In addition to the limitations described above, the older mean age of the specimens, which could have affected the tissue quality of the ligaments; however, all the specimens were evaluated for exclusion according to clinical signs of ligament insufficiency or macroscopic findings of ligament degeneration. For our comparison of stage 0 versus 1, this study was not sufficiently powered to provide a >80% chance of detecting a significant difference at P < .05. However, with the mean RCJ gap differences between stages 0 and 1 being <1 mm, we propose that such a small mean gap progression was not a clinically meaningful difference.
Another limitation is the potential effect of measurement error on the presented results. In this study, the 2 observers had clinical training in the measurement method and made the measurements independently in an attempt to control for measurement error. However, measuring the joint gap electronically requires selection of 2 points (or pixels) on the screen for reference. This may have resulted in differences in the measured joint gap between observers given that the margin of the pixel that would present the margin of the cartilage or bony structure was left at the discretion of each observer. Despite this limitation, we found good to excellent agreement between the joint gap measurements performed by the 2 observers with an estimated measurement error of 0.9 mm, which is less than the reported differences between the experimental stages of LCL disruption presented in our results.
In addition, it is important to understand that each observer utilized the same reference landmarks for joint gap measurement during all stages in each specimen testing. To this end, since the purpose of this measurement is to detect an increase in joint gap formation rather than to accurately measure the actual joint space itself, it should be useful in clinical practice as long as the same reference points are used during the baseline measurement versus the gravity stress measurement in the affected limb. Note also that the baseline measurement can be performed with either the contralateral limb or the affected limb while supporting the forearm and closing the RCJ.
Finally, although the anterior capsule was excised to expose the joint and ensure an accurate sequential cutting of the LCL-cc, this should not have affected our results given the minimal stabilizing contribution of the anterior capsule in the varus elbow. 14,20
Although previous cadaveric studies 11,16,18 have evaluated elbow laxity after sequential cutting of the lateral collateral ligaments, this is the first study to assess the validity and reliability of ultrasonographic measurements of the RCJ space to evaluate elbow varus laxity. Although there are many factors to be considered before applying the results of this study in the clinic, we believe that it can be a useful reference if the physician could secure the baseline data as the normal joint gap. The physician could use the measurement of the opposite elbow as the baseline data if the elbow has no symptoms, or the physician could take the measurement while holding the affected forearm to close the joint gap. Then, the elbow can be gently released to follow gravity. One of the strengths of our model is that the technique used for measurement of the RCJ space may be easily reproduced in future studies and in clinical practice. The position of the elbow during the evaluation could be easily re-created in the clinical setting with 90° of shoulder forward flexion and 90° of humeral internal rotation. Similarly, since the evaluation is performed under gravity stress alone, the reproducibility of the evaluation may be better than if the practitioner had to perform any type of additional varus stress maneuver during the evaluation.
Conclusion
Elbow varus laxity can be reliably assessed via ultrasound by evaluation of the RCJ space under gravity stress. Ultrasonographic measurement of the RCJ space can distinguish increasing varus laxity seen with release of two-thirds or more of the LCL-cc.
Acknowledgment
The authors gratefully acknowledge the resource support provided by the Mayo Clinic Biomechanics Core Facility under the direction of Chunfeng Zhao, MD, as well as the editorial assistance provided by Grace K. Chaney and Colin M. O’Driscoll.
Footnotes
Final revision submitted May 24, 2021; accepted June 29, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Mayo Foundation for Medical Education and Research (S.W.O.: Principal Investigator). S.W.O. has received nonconsulting fees from SIGN Fracture Care International and royalties from Acumed, Wright Medical, and Aircast. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was granted by the Mayo Clinic Rochester Biospecimen Protocol Review Subcommittee.
References
- 1. Ahmad CS, ElAttrache NS. Valgus extension overload syndrome and stress injury of the olecranon. Clin Sports Med. 2004;23(4):665–676. [DOI] [PubMed] [Google Scholar]
- 2. Arrigoni P, Cucchi D, D’Ambrosi R, et al. Arthroscopic R-LCL plication for symptomatic minor instability of the lateral elbow (SMILE). Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2264–2270. [DOI] [PubMed] [Google Scholar]
- 3. Arrigoni P, Cucchi D, D’Ambrosi R, et al. Intra-articular findings in symptomatic minor instability of the lateral elbow (SMILE). Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2255–2263. [DOI] [PubMed] [Google Scholar]
- 4. Baker CL, Jr, Murphy KP, Gottlob CA, Curd DT. Arthroscopic classification and treatment of lateral epicondylitis: two-year clinical results. J Shoulder Elbow Surg. 2000;9(6):475–482. [DOI] [PubMed] [Google Scholar]
- 5. Bunata RE, Brown DS, Capelo R. Anatomic factors related to the cause of tennis elbow. J Bone Joint Surg Am. 2007;89(9):1955–1963. [DOI] [PubMed] [Google Scholar]
- 6. Cain EL, Jr, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31(4):621–635. [DOI] [PubMed] [Google Scholar]
- 7. Camp CL, O’Driscoll SW, Wempe MK, Smith J. The sonographic posterolateral rotatory stress test for elbow instability: a cadaveric validation study. PM R. 2017;9(3):275–282. [DOI] [PubMed] [Google Scholar]
- 8. Cohen MS, Romeo AA, Hennigan SP, Gordon M. Lateral epicondylitis: anatomic relationships of the extensor tendon origins and implications for arthroscopic treatment. J Shoulder Elbow Surg. 2008;17(6):954–960. [DOI] [PubMed] [Google Scholar]
- 9. Finlay K, Ferri M, Friedman L. Ultrasound of the elbow. Skeletal Radiol. 2004;33(2):63–79. [DOI] [PubMed] [Google Scholar]
- 10. Jacobson JA, Chiavaras MM, Lawton JM, et al. Radial collateral ligament of the elbow: sonographic characterization with cadaveric dissection correlation and magnetic resonance arthrography. J Ultrasound Med. 2014;33(6):1041–1048. [DOI] [PubMed] [Google Scholar]
- 11. King GJ, Morrey BF, An KN. Stabilizers of the elbow. J Shoulder Elbow Surg. 1993;2(3):165–174. [DOI] [PubMed] [Google Scholar]
- 12. Lattermann C, Romeo AA, Anbari A, et al. Arthroscopic debridement of the extensor carpi radialis brevis for recalcitrant lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(5):651–656. [DOI] [PubMed] [Google Scholar]
- 13. Morrey BF. Reoperation for failed surgical treatment of refractory lateral epicondylitis. J Shoulder Elbow Surg. 1992;1(1):47–55. [DOI] [PubMed] [Google Scholar]
- 14. Nielsen KK, Olsen BS. No stabilizing effect of the elbow joint capsule: a kinematic study. Acta Orthop Scand. 1999;70(1):6–8. [DOI] [PubMed] [Google Scholar]
- 15. O’Driscoll SW. Classification and evaluation of recurrent instability of the elbow. Clin Orthop Relat Res. 2000;370:34–43. [DOI] [PubMed] [Google Scholar]
- 16. O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73(3):440–446. [PubMed] [Google Scholar]
- 17. O’Driscoll SW, Jupiter JB, King GJ, Hotchkiss RN, Morrey BF. The unstable elbow. Instr Course Lect. 2001;50:89–102. [PubMed] [Google Scholar]
- 18. Olsen BS, Sojbjerg JO, Dalstra M, Sneppen O. Kinematics of the lateral ligamentous constraints of the elbow joint. J Shoulder Elbow Surg. 1996;5(5):333–341. [DOI] [PubMed] [Google Scholar]
- 19. Owens BD, Murphy KP, Kuklo TR. Arthroscopic release for lateral epicondylitis. Arthroscopy. 2001;17(6):582–587. [DOI] [PubMed] [Google Scholar]
- 20. Pollock JW, Brownhill J, Ferreira L, et al. The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J Bone Joint Surg Am. 2009;91(6):1448–1458. [DOI] [PubMed] [Google Scholar]
- 21. Sanchez-Sotelo J, Morrey BF, O’Driscoll SW. Ligamentous repair and reconstruction for posterolateral rotatory instability of the elbow. J Bone Joint Surg Br. 2005;87(1):54–61. [PubMed] [Google Scholar]
- 22. Shirato R, Wada T, Aoki M, et al. Effect of simultaneous stretching of the wrist and finger extensors for lateral epicondylitis: a gross anatomical study of the tendinous origins of the extensor carpi radialis brevis and extensor digitorum communis. J Orthop Sci. 2015;20(6):1005–1011. [DOI] [PubMed] [Google Scholar]
- 23. Smith AM, Castle JA, Ruch DS. Arthroscopic resection of the common extensor origin: anatomic considerations. J Shoulder Elbow Surg. 2003;12(4):375–379. [DOI] [PubMed] [Google Scholar]
- 24. Stewart B, Harish S, Oomen G, et al. Sonography of the lateral ulnar collateral ligament of the elbow: study of cadavers and healthy volunteers. AJR Am J Roentgenol. 2009;193(6):1615–1619. [DOI] [PubMed] [Google Scholar]
- 25. Teixeira PA, Omoumi P, Trudell DJ, et al. Ultrasound assessment of the lateral collateral ligamentous complex of the elbow: imaging aspects in cadavers and normal volunteers. Eur Radiol. 2011;21(7):1492–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]