Abstract
Purpose
Direct anterior approach (DAA) has recently become popular in total hip arthroplasty (THA). However, irrespective of the surgical approach used, component malposition is an important factor affecting function and complications after THA. This study aims to compare component positioning on the femoral and acetabular side between DAA and posterior approach (PA) to the hip joint. We hypothesized that the two approaches are similar in terms of component positioning.
Methods
We prospectively studied 50 patients, matched according to age, sex, and body mass index, undergoing THA, divided non-randomly into 2 groups. Group 1 comprised 25 patients (35 hips) undergoing THA using DAA and group 2 comprised 25 patients (25 hips) undergoing THA using PA. Ten patients from group 1 had simultaneous bilateral THA. Radiological parameters studied were acetabular inclination (AI), coronal femoral stem alignment (CFA), leg length difference (LLD), acetabular cup version (AV), and femoral stem version (FV).
Results
There was no significant difference in AI, CFA, LLD, AV, and FV between the two groups. Excellent to good inter and intra-observer reliability expressed in terms of intraclass correlation coefficient (ICC) was noted for all the radiographic measurements.
Conclusion
Both DAA and PA for THA achieve comparable radiological component positioning. DAA may not provide any advantage over PA in terms of positioning of the prosthesis.
Level of Evidence
Level II, non-randomized comparative study.
Keywords: Direct anterior approach, Posterior approach, Hip arthroplasty, Acetabular anteversion, Acetabular inclination, Leg length difference
Introduction
The direct anterior approach (DAA) has recently become popular in total hip arthroplasty (THA) [1–3]. It has the advantage of being a less invasive approach with true inter-nervous and inter-muscular planes [4–9]. This approach is reported to have a lower dislocation rate when compared to the posterior approach (PA) [10, 11]. The orientation of acetabulum and proximal femur are completely different in DAA and PA. The hip is dislocated anteriorly in DAA as compared to the PA and the intraoperative view of the acetabulum obtained during PA is different from that obtained during the DAA, interpreting intraoperative landmarks different. Similarly, limited exposure of the proximal femur in DAA may increase the risk of component malposition [12]. However, DAA also has the advantage of operating in a supine position [13] and to be able to use fluoroscopy intraoperatively [14–17]. However, these advantages of DAA come at the cost of a high learning curve [18]. These differences may result in variations in component positioning in these two surgical approaches [19].
Irrespective of the surgical approach used, component malposition is an important factor affecting function and complications after THA [20–24]. Improper component position can lead to impingement, dislocation, and accelerated wear of the components. Multiple previous studies have compared radiographic parameters component positionings like acetabular cup abduction angle and anteversion [7, 25–28]. Computed tomography (CT) scan is the investigation of choice to study component position on the femoral and the acetabular side [29].
This study aims to compare component positioning on the femoral and the acetabular side between DAA and PA. The null hypothesis for this study was that the two surgical approaches for THA provide similar results in terms of various parameters of component positioning like acetabular inclination, coronal femoral alignment, limb length difference, coronal plane femoral alignment, acetabular cup anteversion, and femoral stem anteversion. No similar comparative study has been conducted in the past taking into account all these radiological parameters.
Material and Methods
We prospectively studied 50 patients undergoing THA between March 2018 to March 2019. Written and informed consent was taken from each patient participating in this study. The study was approved by the institutional ethics committee. Patients with primary or secondary unilateral as well as bilateral hip hip pathology due to inflammatory arthritis, avascular necrosis of the femoral head, dysplasia of the hip, and fractured neck of the femur were included in the study. Details of various hip pathologies included in the study are depicted in Table 1. Patients were allocated to either group consecutively, non-randomly. Group 1 consisted of 25 patients (35 hips) undergoing THA using DAA and group 2 consisted of 25 patients (25 hips) undergoing THA using PA. Ten patients from the DAA group had undergone simultaneous single-stage bilateral THA. The study excluded all revision THA cases, patients with any systemic rheumatic illness, neuromuscular illnesses, significant spinal stiffness (positive Schober’s Test), and with BMI more than 30. All surgeries were performed by a single orthopaedic surgeon. To account for the surgical learning curve patients operated on in the first 6 months after DAA was being routinely used by the surgeon were not included in the study. Preoperative templating for cup size, offset length and stem sizing was done using a computerized digital templating tool (mediCAD Hectec GmbH).
Table 1.
Various etiologies of hips in Group 1 and Group 2
| Etiologies | Group 1 (n = 35) | Group 2 (n = 25) |
|---|---|---|
| 1. Avascular necrosis of femoral head | 17 | 13 |
| a. Idiopathic | 8 | 5 |
| a. Steroid induced | 6 | 3 |
| a. Alcohol induced | 1 | 2 |
| a. Post traumatic | 2 | 3 |
| 2. Inflammatory arthritis | 14 | 9 |
| a. Rheumatoid arthritis | 8 | 4 |
| b. Ankylosing spondylitis | 6 | 3 |
| c. Seronegative arthropathy | 0 | 2 |
| 3. Neck of femur fracture | 3 | 2 |
| 4. Neglected dysplastic hip | 1 | 1 |
n numbers of hips included
Surgical Procedures
Direct Anterior Approach (DAA)
A longitudinal skin incision of an approximate length of 10 cm was made starting 2 cm lateral and distal to the anterior superior iliac spine. The inter-muscular interval between tensor fascia lata and sartorius muscles was used. The lateral femoral cutaneous nerve of the thigh was identified and carefully retracted. In the deeper plane, a muscle plane was developed between the rectus femoris and vastus lateralis/gluteus medius. Ascending branches of the lateral circumflex artery were identified and cauterized. An inverse L-shaped capsulotomy was performed starting from the anteromedial femoral neck extending upwards to the rim of the acetabulum and then curving laterally along the acetabular margin. A provisional in-situ neck cut was made using an oscillating saw. Head was delivered out and acetabulum was reamed serially. Capsular release on the proximal femur is a very crucial step for further exposure of the proximal femur. The release was carried out along the capsular insertion on the femur, starting anteriorly and reaching the posterosuperior aspect. The posterior capsule, Gluteus minimus, piriformis, and obturator externus muscles were protected. The conjoint tendon of the Obturator internus and Gemelli were generally released during this procedure. The operating table was hyperextended at the hip joint at this stage to help in delivering the proximal femur out of the wound. The limb was adducted and externally rotated by moving it under the opposite leg in a figure of four fashion. The proximal femur was levered out using a bone hook and levers. A definitive neck-cut made at the desired level of the neck and femoral preparation was completed.
Intraoperatively during DAA, we used the transverse acetabular ligament, anterior acetabular wall, and patient’s supine position as a guide for anteversion and inclination of the acetabular component while the lesser trochanter and the native version of the femoral neck were used for assessing femoral component anteversion. The aim was to achieve 40–45 degrees of inclination and 15–20-degree of anteversion.
Intraoperative fluoroscopy is easier in DAA since the patient is positioned supine. Only anteroposterior radiographs were obtained intraoperatively, to aid as a guide for acetabular and femoral component positioning. They were compared with pre-operative radiographs for judging correction of limb length and component positioning.
Posterior Approach (PA)
It was performed with the patient in a lateral position. A curvilinear skin incision of around 15 cm was made, centered over the posterior third of the greater trochanter. Fascia lata was incised and fibers of the gluteus maximus were split. Short external rotators and hip capsule were detached in a single layer from the proximal femur and reflected posteriorly, protecting the sciatic nerve. The femoral head was dislocated with flexion, adduction, and internal rotation. Neck cut was made referencing from lesser trochanter. The acetabulum was exposed and reamed serially. The femoral canal was opened and prepared using serial broaches.
Uncemented FMT femoral stem and uncemented Trilogy acetabular shell with a polyethylene liner (Zimmer Biomet, Warsaw, Indiana, USA) were used in all the patients. All cases were performed under neuraxial blockage along with epidural analgesia.
Outcomes Measurement
Anteroposterior (AP) plain radiograph and CT scan of the pelvis were obtained 2 weeks after the surgery. Standard AP radiographs of the pelvis were taken with the x-ray beam centered on the symphysis pubis and legs in 10–15 degrees of internal rotation. CT scans were performed with a 128 slice machine including sections from bilateral hip joints to bilateral knee joints. All measurements were noted by two independent, blinded, observers on two separate occasions 2 weeks apart, using RadiAnt DICOM viewer software (Medixant, Poznan, Poland).
Calculation of Acetabular Inclination (AI) (Fig. 1)
Fig. 1.
Angle i depicting Acetabular inclination (AI), AB denotes inter-teardrop line, and CD tangent along the open ends of the acetabular shell
AI was measured on the AP view of X rays, using the inter-teardrop line as the reference as described by Sutherland et al. [30]. Tangent was drawn to the open face of the acetabular shell and its angle with the horizontal inter-teardrop line was measured.
Calculation of Coronal Plane Femoral Alignment (CFA) (Fig. 2)
Fig. 2.
Angle * denotes Coronal femoral stem alignment (CFA) calculated as the angle between the anatomic femoral axis and prosthesis axis, blue line (CD) depicts anatomic femoral axis, yellow line (AB) indicates prosthesis axis
This radiographic parameter was assessed on standard AP radiographs as described by Reina et al. [31]. The anatomic femoral axis was calculated as the line bisecting two horizontal lines taking two points on either side of the femoral cortex, 1 and 10 cm below the lesser trochanter. The prosthesis axis was defined as the line joining the proximal threaded hole on the shoulder of the prosthesis and the femoral stem tip at the distal end. The CFA was estimated as the angular deviation of the prosthesis axis from the anatomic femoral axis.
Calculation of Leg Length Difference (LLD) (Fig. 3)
Fig. 3.
Depicts leg length difference (LLD), yellow line denotes horizontal inter-teardrop line, for right hip Line A depicting distance from the tip of lesser trochanter to the inter-teardrop line (mm), for left hip (post-THA) Line B depicting distance from the tip of lesser trochanter to the inter-teardrop line (mm). LLD = A − B (mm)
LLD was calculated on plain AP radiograph as described in studies by Meermans et al. [32] and Kjellberg et al. [33]. The horizontal inter-teardrop line was used as the reference. The vertical distance of this line from the tip of the lesser trochanter to this inter-teardrop line was measured and compared on both sides. We aimed at achieving comparable leg lengths in cases of single staged bilateral THA. Any difference in leg lengths between the two legs was noted.
Calculation of Acetabular Cup Anteversion (AV) (Fig. 4)
Fig. 4.
Angle x denoting the acetabular cup anteversion (AV), Line AB drawn joining the posterior pelvic margin, line DE denotes the tangent along the anterior and posterior edge of the acetabular shell, Line CD denotes a perpendicular to the line AB. Angle x depicts AV, between lines CD and DE
AV was measured on the axial CT scan section as described by Wines et al. [34]. A tangent was drawn to the anterior and posterior edge of the acetabular cup. Another line was drawn joining the posterior pelvic margins. Angle was calculated between a perpendicular drawn to this line and the tangent drawn to the acetabulum shell.
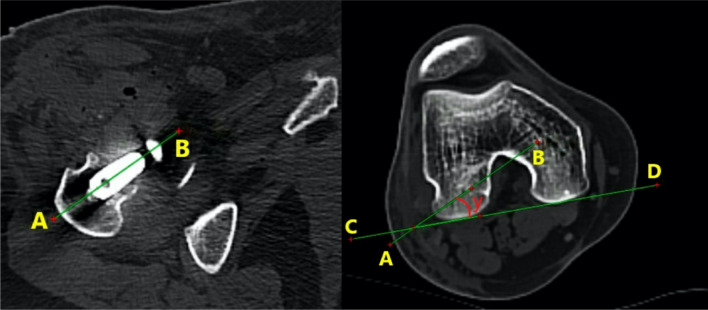
Calculation of Femoral Stem Anteversion (FV) (Fig. 5).
Fig. 5.
Angle y denoting femoral stem anteversion (FV). Line AB was drawn through the center of the femoral prosthesis head and neck, and Line CD joining the posterior points of medial and lateral condyles of the femur. Angle y subtended between the two lines AB and CD is known as FV
FV was also measured on axial CT scan sections as described by Fujishiro et al. [35]. One line was drawn through the head and neck of the femoral prosthesis and another line was drawn connecting the posterior-most aspect of the medial and lateral femoral condyles. The angle between these lines was considered the FV.
Statistical Analysis
All continuous variables were expressed as means and standard deviations and categorical variables in terms of absolute numbers. Categorical variables were compared using the Chi-square test between the two groups. Parameters were analyzed by the Shapiro–Wilk Test to check for normal distribution. Values of LLD and CFA were found to be not normally distributed. Continuous parametric variables like AI, AV, and FV for both the groups were compared using the Independent T-test. Non-parametric continuous variables like LLD, CFA between the two groups were compared using the Mann–Whitney U test. All statistical tests were two-sided with a level of significance of five percent. Results were considered statistically significant when the P value was less than 0.05.
Intra-observer and inter-observer reliability were tested by repeat measurements of all the parameters. They were expressed as intraclass correlation coefficients (ICC) with its 95% confidence interval (CI). All test results were analyzed using SPSS software version 23.0 (SPSS Inc., Chicago, IL, USA).
Results
Table 2 summarises details of patients including mean age, sex, and BMI. Both the groups were comparable in these parameters (P values were insignificant). Radiographic parameters of component positioning are tabulated in Table 3. The various parameters in Group 1 vs. Group 2 were mean AI 43.03° ± 7.11° vs. 44.52° ± 5.42°, mean CFA 3.05° ± 0.463° vs. 3.11° ± 0.572°, mean LLD 0.838 mm ± 0.52 mm vs. 0.956 mm ± 0.45 mm, mean AV 27.05° ± 6.0° vs. 26.43° ± 4.66° and mean FV 14.43° ± 3.47° vs. 15.52° ± 4.25° respectively. There was no significant difference concerning AI, CFA, LLD, AV, and FV among the two groups. Excellent to good inter and intra-observer reliability (values > 0.83) was observed for all the radiographic measurements of component positioning in both the groups (vide Table 4).
Table 2.
Comparison of patient characteristics between Group 1 and Group 2
| Variables | Group 1 (mean ± SD) | Group 2 (mean ± SD) | P value |
|---|---|---|---|
| Mean age (years) | 36.2 ± 15.4 | 43.03 ± 12.36 | 0.061 |
| Sex (male/females) | 18/7 | 15/10 | 0.069 |
| Mean BMI [kgs/m2] | 21.5 ± 2.14 | 22.26 ± 1.46 | 0.101 |
Table 3.
Comparison of radiological parameters between Group 1 and Group 2
| Variables | Group 1 (mean ± SD) | Group 2 (mean ± SD) | P value |
|---|---|---|---|
| Acetabular cup inclination (AI) [in degrees] | 43.03 ± 7.11 | 44.52 ± 5.42 | 0.383a |
| Coronal femoral stem alignment (CFA) [in degrees of varus/valgus] | 3.05 ± 0.463 | 3.11 ± 0.572 | 0.652b |
| Leg length difference (LLD) [in mm] | 0.838 ± 0.52 | 0.956 ± 0.45 | 0.287b |
| Acetabular shell anteversion (AV) [in degrees] | 27.05 ± 6.0 | 26.43 ± 4.66 | 0.664a |
| Femoral stem anteversion (FV) [in degrees] | 14.43 ± 3.47 | 15.52 ± 4.25 | 0.278a |
aP-value—calculated using Independent T test
bP-value—calculated using Mann–Whitney U Test
Table 4.
Comparison of intra and interobserver reliability between Group 1 and Group 2
| Variables | Group 1 | Group 2 | ||
|---|---|---|---|---|
| Intra-observer reliability (ICC, 95% CI) | Inter-observer reliability (ICC, 95% CI) | Intra-observer reliability (ICC, 95% CI) | Inter-observer reliability (ICC, 95% CI) | |
| Acetabular cup inclination (AI) [in degrees] | 0.979a (0.952–0.991) | 0.948 (0.885–0.977) | 0.953a (0.903–0.980) | 0.925 (0.837–0.966) |
| 0.945b (0.880–0.975) | 0.958b (0.908–0.981) | |||
| Coronal femoral stem alignment (CFA) [in degrees of varus/valgus] | 0.929a (0.845–0.968) | 0.962 (0.916–0.983) | 0.950a (0.890–0.978) | 0.938 (0.864–0.972) |
| 0.964b (0.920–0.984) | 0.963b (0.918–0.983) | |||
| Leg length difference (LLD) [in mm] | 0.904a (0.794–0.956) | 0.957 (0.905–0.981) | 0.951a (0.891–0.978) | 0.929 (0.846–0.968) |
| 0.827b (0.646–0.920) | 0.915b (0.817–0.962) | |||
| Acetabular shell anteversion (AV) [in degrees] | 0.929a (0.846–0.968) | 0.920 (0.827–0.964) | 0.896a (0.779–0.953) | 0.932 (0.852–0.969) |
| 0.955b (0.900–0.980) | 0.945b (0.879–0.975) | |||
| Femoral stem anteversion (FV) [in degrees] | 0.879a (0.745–0.945) | 0.894 (0.774–0.952) | 0.911a (0.808–0.960) | 0.949 (0.888–0.977) |
| 0.911b (0.808–0.960) | 0.949b (0.889–0.977) | |||
aIntra-observer reliability ICC—Between observer 1 at two separate occasions, 2 weeks apart
bIntra-observer reliability ICC—Between observer 2 at two separate occasions, 2 weeks apart
Discussion
DAA is a comparatively newer approach for hip arthroplasty. It has been said that with the use of intra-operative image guidance, component positioning may be more accurate with DAA [17]. Instability after THA is multifactorial, and component position is an important surgeon-controlled factor that must be taken care of during the surgery. Hence the current study compared radiological parameters of component positioning between THA performed using DAA and PA. The study findings suggest that THA by both the surgical approaches have comparable results in terms of component positioning.
Lewinnek et al. [36] had described a radiological “safe zone” to classify acetabular cup inclination and anteversion after THA. Acetabular inclination values in the range of 400 ± 100 and cup anteversion of 150 ± 100 were considered to be in the safe zone. The present study found that 5/35 hips (14.3%) in DAA versus 4/25 hips (16%) in PA groups were outside the safe acetabular inclination range (P = 0.855) and 10/35 hips (28.6%) in DAA versus 9/25 hips (36%) in PA were outside the safe acetabular anteversion zone (P = 0.583). Similarly, the study by Hamilton et al. highlights the percentage of hips outside the safe zone of cup inclination angle to be 10/100 hips (10%) in DAA versus 21/100 hips (21%) in PA and 8/100 hips (8%) in the DAA group versus 36/100 hips (36%) in PA group were out of safe anteversion zone [37]. However, at a mean follow-up of 12 months, none of the patients had any complication of impingement or dislocation. This target safe zone has been questioned by Abdel et al. [38] as they found that the majority (58%) of dislocations in their cases of dislocated THAs were within this safe zone of both acetabular inclination and anteversion. Recently, a combined sagittal index (CSI) [39] specifying a functional safe zone has been identified as a potential indicator to predict dislocation.
According to the study by Alexandrov et al. [40], DAA is a useful alternative to any other approach for THA owing to its comparable complication rates and similar radiological outcomes. However, unlike this present study, they did not compare DAA to any traditional surgical approach group to successfully conclude their results. The study by Beamer et al. [41] suggests that fluoroscopic guidance improves the component positioning in cases of both primary as well as complex THA as compared to the free-hand technique. It has also been suggested that image guidance improves component positioning and also improves the learning curve of THA with DAA [17].
In the retrospective study by Rathod et al. [14] of 825 THAs, 372 PA-THA were compared to fluoroscopically guided 453 DAA-THA for cup inclination and anteversion. They concluded that there are lesser chances of cup inclination and anteversion variability in the DAA group as compared to the PA group. Similarly, Weifeng et al. [16] compared two groups of patients undergoing DAA-THA with PA-THA, both under fluoroscopic guidance, using the intra-operative and post-operative record of acetabular cup inclination and anteversion. They concluded that DAA-THA had better component position and less variability than those undergoing PA-THA. Therefore they indicated that the surgical approach may have a role in better component positioning. Likewise, in the study by Barrett et al. [25], the DAA-THA group had better chances to be in the Lewinnek safe zone of component positioning than the PA-THA group. Matta et al. [42] reviewed 458 arthroplasties by DAA and found most of their cases had better target anteversion and inclination values. Bingham et al. [43] compared DAA under image guidance and DAA without image guidance, measuring AI, AV, and LLD. They found no difference in outcomes between the two groups.
Lin et al. [15] compared radiographs of 194 patients 86 patients who underwent PA and 108 patients who underwent DAA. They used plain AP radiographs for measurement of acetabular version, although CT scan identifies version more accurately. They included LLD and femoral offset apart from AI and AV. The femoral component version was not evaluated. The mean values of versions were not used for analysis. They concluded that the DAA group had better AI than the PA group, however, no significant difference was identified considering LLD, AV, and femoral offset. The present study evaluated AI, CFA, LLD, AV, and FV and found comparable radiological outcomes between THA by DAA and PA approach. A recent systematic review by Peng et al. [44] included 5 randomized controlled trials [7, 25–28] with a total of 503 cases for radiographic outcome analysis. They concluded no difference in AI and AV between DAA and PA groups. But, they did not consider FV, LLD, and CFA in their study. Also, none of the five studies included for radiographic outcome analysis considered CT scan imaging for the AI and AV calculation.
All surgeries were performed by a single arthroplasty surgeon which may be considered as the strength of the study but it decreases the overall generalization of the study results. The study was more comprehensive in terms of radiological parameters of component positioning studied, as it included AI, CFA, LLD, AV, and FV. CT scans were used for measurement of version. To the best of our knowledge, no similar study has been conducted in the past. The present study has some limitations like the non-randomized inclusion of patients in both the groups, a relatively smaller sample size. No sample size calculation or power-analysis was performed. Also, ten patients underwent bilateral THA in group 1, and none of the patients had a simultaneous bilateral procedure in group 2.
Conclusion
Both DAA and PA for THA achieve comparable radiological component positioning. DAA may not provide any advantage over PA in terms of positioning of the prosthesis.
Funding
Nil.
Compliance with Ethical Standards
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
The institutional ethics committee approved the study. Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. The study was conducted in All India Institute of Medical Sciences, Rishikesh, India.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tarun Goyal, Email: goyal.tarun@gmail.com.
Arghya Kundu Choudhury, Email: arghyakunduchoudhury@gmail.com.
Souvik Paul, Email: 1990.souvik@gmail.com.
Tushar Gupta, Email: iamtushargupta@gmail.com.
Lakshmana Das, Email: sekarldas@gmail.com.
References
- 1.Petis S, Howard JL, Lanting BL, Vasarhelyi EM. Surgical approach in primary total hip arthroplasty: anatomy, technique and clinical outcomes. Canadian Journal of Surgery. 2015;58:128–139. doi: 10.1503/cjs.007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohan K. The direct anterior approach to the hip joint. Ortho & Rheum Open Access. 2017;9(3):555761. doi: 10.19080/OROAJ.2017.09.555761. [DOI] [Google Scholar]
- 3.Paillard P. Hip replacement by a minimal anterior approach. International Orthopaedics. 2007;31(Suppl 1):S13–15. doi: 10.1007/s00264-007-0433-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Z, Hou J-Z, Wu C-H, Zhou Y-J, Gu X-M, Wang H-H, et al. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. Journal of Orthopaedic Surgery and Research. 2018;13:229. doi: 10.1186/s13018-018-0929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christensen CP, Jacobs CA. Comparison of patient function during the first six weeks after direct anterior or posterior total hip arthroplasty (THA): a randomized study. Journal of Arthroplasty. 2015;30:94–97. doi: 10.1016/j.arth.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 6.Zawadsky MW, Paulus MC, Murray PJ, Johansen MA. Early outcome comparison between the direct anterior approach and the mini-incision posterior approach for primary total hip arthroplasty: 150 consecutive cases. Journal of Arthroplasty. 2014;29:1256–1260. doi: 10.1016/j.arth.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 7.Zhao H-Y, Kang P-D, Xia Y-Y, Shi X-J, Nie Y, Pei F-X. Comparison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. Journal of Arthroplasty. 2017;32:3421–3428. doi: 10.1016/j.arth.2017.05.056. [DOI] [PubMed] [Google Scholar]
- 8.Restrepo C, Parvizi J, Pour AE, Hozack WJ. Prospective randomized study of two surgical approaches for total hip arthroplasty. Journal of Arthroplasty. 2010;25(671–679):e1. doi: 10.1016/j.arth.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Post ZD, Orozco F, Diaz-Ledezma C, Hozack WJ, Ong A. Direct anterior approach for total hip arthroplasty: indications, technique, and results. Journal of American Academy of Orthopaedic Surgeons. 2014;22:595–603. doi: 10.5435/JAAOS-22-09-595. [DOI] [PubMed] [Google Scholar]
- 10.Tsukada S, Wakui M. Lower dislocation rate following total hip arthroplasty via direct anterior approach than via posterior approach: five-year-average follow-up results. The Open Orthopaedics Journal. 2015;9:157–162. doi: 10.2174/1874325001509010157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheth D, Cafri G, Inacio MCS, Paxton EW, Namba RS. Anterior and anterolateral approaches for tha are associated with lower dislocation risk without higher revision risk. Clinical Orthopaedics. 2015;473:3401–3408. doi: 10.1007/s11999-015-4230-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schloemann DT, Edelstein AI, Barrack RL. Changes in acetabular orientation during total hip arthroplasty. The Bone & Joint Journal. 2019;101:45–50. doi: 10.1302/0301-620X.101B6.BJJ-2018-1335.R1. [DOI] [PubMed] [Google Scholar]
- 13.Grammatopoulos G, Gofton W, Cochran M, Dobransky J, Carli A, Abdelbary H, et al. Pelvic positioning in the supine position leads to more consistent orientation of the acetabular component after total hip arthroplasty. The Bone & Joint Journal. 2018;100-B:1280–1288. doi: 10.1302/0301-620X.100B10.BJJ-2018-0134.R1. [DOI] [PubMed] [Google Scholar]
- 14.Rathod PA, Bhalla S, Deshmukh AJ, Rodriguez JA. Does fluoroscopy with anterior hip arthroplasty decrease acetabular cup variability compared with a nonguided posterior approach? Clin Orthop. 2014;472:1877–1885. doi: 10.1007/s11999-014-3512-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin TJ, Bendich I, Ha AS, Keeney BJ, Moschetti WE, Tomek IM. A comparison of radiographic outcomes after total hip arthroplasty between the posterior approach and direct anterior approach with intraoperative fluoroscopy. Journal of Arthroplasty. 2017;32:616–623. doi: 10.1016/j.arth.2016.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ji W, Stewart N. Fluoroscopy assessment during anterior minimally invasive hip replacement is more accurate than with the posterior approach. International Orthopaedics. 2016;40:21–27. doi: 10.1007/s00264-015-2803-x. [DOI] [PubMed] [Google Scholar]
- 17.Slotkin EM, Patel PD, Suarez JC. Accuracy of fluoroscopic guided acetabular component positioning during direct anterior total hip arthroplasty. Journal of Arthroplasty. 2015;30:102–106. doi: 10.1016/j.arth.2015.03.046. [DOI] [PubMed] [Google Scholar]
- 18.Hartford JM, Bellino MJ. The learning curve for the direct anterior approach for total hip arthroplasty: A single surgeon’s first 500 cases. Hip Int. 2017;27:483–488. doi: 10.5301/hipint.5000488. [DOI] [PubMed] [Google Scholar]
- 19.Moretti VM, Post ZD. Surgical approaches for total hip arthroplasty. Indian Journal Orthopaedics. 2017;51:368–376. doi: 10.4103/ortho.IJOrtho_317_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Werner BC, Brown TE. Instability after total hip arthroplasty. World Journal of Orthopaedics. 2012;3:122–130. doi: 10.5312/wjo.v3.i8.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krenzel BA, Berend ME, Malinzak RA, Faris PM, Keating EM, Meding JB, et al. High preoperative range of motion is a significant risk factor for dislocation in primary total hip arthroplasty. Journal of Arthroplasty. 2010;25:31–35. doi: 10.1016/j.arth.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 22.Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clincal Orthopaedics. 2002;405:46–53. doi: 10.1097/00003086-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Rogers M, Blom AW, Barnett A, Karantana A, Bannister GC. Revision for recurrent dislocation of total hip replacement. Hip Int J Clin Exp Res Hip Pathol Ther. 2009;19:109–113. doi: 10.1177/112070000901900205. [DOI] [PubMed] [Google Scholar]
- 24.Mahoney CR, Pellicci PM. Complications in primary total hip arthroplasty: avoidance and management of dislocations. Instructional Course Lectures. 2003;52:247–255. [PubMed] [Google Scholar]
- 25.Barrett WP, Turner SE, Leopold JP. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. Journal of Arthroplasty. 2013;28:1634–1638. doi: 10.1016/j.arth.2013.01.034. [DOI] [PubMed] [Google Scholar]
- 26.Cheng TE, Wallis JA, Taylor NF, Holden CT, Marks P, Smith CL, et al. A prospective randomized clinical trial in total hip arthroplasty-comparing early results between the direct anterior approach and the posterior approach. Journal of Arthroplasty. 2017;32(3):883–890. doi: 10.1016/j.arth.2016.08.027. [DOI] [PubMed] [Google Scholar]
- 27.Zhang XL, Wang Q, Jiang Y. Zeng BF Minimally invasive total hip arthroplasty with anterior incision. Zhonghua wai ke za zhi. 2006;44(8):512–515. [PubMed] [Google Scholar]
- 28.Luo ZL, Chen M, Shang XF, et al. Direct anterior approach versus posterolateral approach for total hip arthroplasty in the lateral decubitus position. Zhonghua Yi Xue Za Zhi. 2016;96:2807–2812. doi: 10.3760/cma.j.issn.0376-2491.2016.35.009. [DOI] [PubMed] [Google Scholar]
- 29.Mushtaq N, To K, Gooding C, Khan W. Radiological imaging evaluation of the failing total hip replacement. Frontiers in Surgery. 2019 doi: 10.3389/fsurg.2019.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sutherland CJ, Wilde AH, Borden LS, Marks KE. A ten-year follow-up of one hundred consecutive Müller curved-stem total hip-replacement arthroplasties. Journal of Bone and Joint Surgery American Volume. 1982;64:970–982. doi: 10.2106/00004623-198264070-00002. [DOI] [PubMed] [Google Scholar]
- 31.Reina N, Salib CG, Perry KI, Hanssen AD, Berry DJ, Abdel MP. Mild coronal stem malalignment does not negatively impact survivorship or clinical results in uncemented primary total hip arthroplasties with dual-tapered implants. Journal of Arthroplasty. 2019;34:1127–1131. doi: 10.1016/j.arth.2019.01.055. [DOI] [PubMed] [Google Scholar]
- 32.Meermans G, Malik A, Witt J, Haddad F. Preoperative radiographic assessment of limb-length discrepancy in total hip arthroplasty. Clinical Orthopaedics. 2011;469:1677–1682. doi: 10.1007/s11999-010-1588-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kjellberg M, Al-Amiry B, Englund E, Sjödén GO, Sayed-Noor AS. Measurement of leg length discrepancy after total hip arthroplasty. The reliability of a plain radiographic method compared to CT-scanogram. Skeletal Radiology. 2012;41:187–191. doi: 10.1007/s00256-011-1166-7. [DOI] [PubMed] [Google Scholar]
- 34.Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. Journal of Arthroplasty. 2006;21:696–701. doi: 10.1016/j.arth.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Fujishiro T, Hayashi S, Kanzaki N, Hashimoto S, Kurosaka M, Kanno T, et al. Computed tomographic measurement of acetabular and femoral component version in total hip arthroplasty. International Orthopaedics. 2014;38:941–946. doi: 10.1007/s00264-013-2264-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. Journal of Bone and Joint Surgery. American Volume. 1978;60:217–220. doi: 10.2106/00004623-197860020-00014. [DOI] [PubMed] [Google Scholar]
- 37.Hamilton WG, Parks NL, Huynh C. Comparison of cup alignment, jump distance, and complications in consecutive series of anterior approach and posterior approach total hip arthroplasty. Journal of Arthroplasty. 2015;30(11):1959–1962. doi: 10.1016/j.arth.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 38.Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? the vast majority of dislocated THAs are within the lewinnek safe zone for acetabular component position. Clinical Orthopaedics. 2016;474:386–391. doi: 10.1007/s11999-015-4432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tezuka T, Heckmann ND, Bodner RJ, Dorr LD. Functional safe zone is superior to the lewinnek safe zone for total hip arthroplasty: why the lewinnek safe zone is not always predictive of stability. Journal of Arthroplasty. 2019;34:3–8. doi: 10.1016/j.arth.2018.10.034. [DOI] [PubMed] [Google Scholar]
- 40.Alexandrov, T., Ahlmann, E. R., Menendez, L. R. (2014) Early Clinical and Radiographic Results of Minimally Invasive Anterior Approach Hip Arthroplasty. Adv Orthop 2014:e954208. https://www.hindawi.com/journals/aorth/2014/954208/. Accessed 7 Jul 2020 [DOI] [PMC free article] [PubMed]
- 41.Beamer BS, Morgan JH, Barr C, Weaver MJ, Vrahas MS. Does fluoroscopy improve acetabular component placement in total hip arthroplasty? Clin Orthop. 2014;472:3953–3962. doi: 10.1007/s11999-014-3944-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop. 2005;441:115–124. doi: 10.1097/01.blo.0000194309.70518.cb. [DOI] [PubMed] [Google Scholar]
- 43.Bingham JS, Spangehl MJ, Hines JT, Taunton MJ, Schwartz AJ. Does intraoperative fluoroscopy improve limb-length discrepancy and acetabular component positioning during direct anterior total hip arthroplasty? Journal of Arthroplasty. 2018;33:2927–2931. doi: 10.1016/j.arth.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 44.Peng L, Zeng Y, Wu Y, Zeng J, Liu Y, Shen B. Clinical, functional and radiographic outcomes of primary total hip arthroplasty between direct anterior approach and posterior approach: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2020;21:338. doi: 10.1186/s12891-020-03318-x. [DOI] [PMC free article] [PubMed] [Google Scholar]