Abstract
Children with autism spectrum disorder (ASD) often display repetitive and restrictive patterns of behavior, which can be seen in food selectivity and other feeding problems. Feeding problems in children with ASD not only lead to medical complications for the child but also can lead to increased caregiver stress. In order for behavior analysts to ensure adherence to the Professional and Ethical Compliance Code for Behavior Analysts, many factors need to be addressed prior to and during feeding assessments and interventions. The need for interdisciplinary collaboration and ethical situations that may arise are reviewed. The purpose of this article is to assist the behavior analyst in determining best practices for feeding assessments and interventions while maintaining ethical compliance.
Keywords: feeding intervention, feeding assessment, ethics
One of the diagnostic criteria of autism spectrum disorder (ASD) is that the individuals engage in restrictive and repetitive patterns of behavior (American Psychiatric Association, 2013). For many children with ASD, this can be seen with their food selections, which result in various feeding problems (Williams & Seiverling, 2018). A survey, conducted in 2004 with caregivers of children with ASD, found that 72% of the respondents reported their children with ASD to have feeding problems (Schreck et al., 2004). Research also suggests that patterns of restricted feeding may equate to stereotyped behaviors and sensory responsiveness, which may be early signs of ASD (Cherif et al., 2018; Keen, 2008).
Feeding problems in children with ASD can be divided into three categories: food selectivity, food or liquid refusal, and refusal to self-feed (Williams & Foxx, 2007). Food selectivity has been defined in the literature as a strong aversion or liking to specific sorts of foods (Williams & Foxx, 2007). Food selectivity can be further classified as extreme food selectivity, in which the individual consumes only 10–15 different foods, and moderate food selectivity, in which the individual consumes more than 15 different foods but the total is still less than what is viewed as an “average” variety of consumption for their age (Ledford et al., 2018). Food or liquid refusal occurs when the individual refuses consumption of all foods or all liquids (Williams & Seiverling, 2018). These individuals may consume their intake of nutrients via tube feeds or liquids dependent on the type of refusal. Refusal to self-feed occurs when the individual allows others to provide food to them orally but refuses to complete the action independently while having the motor skills to do so (Williams & Foxx, 2007). Though not much is known about which behavioral feeding intervention to select based on the presenting feeding problem, the field of behavior analysis supports matching the intensity of the intervention to the severity of the behavior (Williams & Foxx, 2007).
Individuals with ASD are also often faced with other comorbid diagnoses, such as attention-deficit disorder (Avni et al., 2018; Thomas et al., 2018), anxiety disorder (Avni et al., 2018), sleep disorders (Thomas et al., 2018), and obsessive-compulsive disorder (Griffiths et al., 2017), which may further increase the complexity of symptoms of feeding problems. Many strategies are often attempted to reduce the complexity of symptoms prior to reaching out to behavior analysts, which sometimes results in a variety of professionals intervening at the same time (LaFrance et al., 2019; Newhouse-Oisten et al., 2017). This can further increase the complexity of feeding cases presented to a behavior analyst, due to various and complex learning histories and the possible aversions that may have become learned. The complexity of behavior, and the presence of comorbidity in individuals with ASD, makes interdisciplinary collaboration tremendously important, especially in the area of feeding issues (LaFrance et al., 2019).
Feeding problems can present a variety of long-term effects for the individual and caregivers alike. Bandini et al. (2017) assessed food selectivity in 18 children with ASD twice with each participant, the second assessment approximately 6 years after the first, to determine how food selectivity changes in children with ASD over time. The researchers found an increase in the prevalence of obesity in children and adolescents with food selectivity. They also noted an improvement in food refusal even though no increase in the variety of foods consumed was noted (Bandini et al., 2017). Levin et al. (2014) noted that nutritional deficiencies such as reduced protein, calcium, vitamin B12, and vitamin D are common in children with ASD with feeding selectivity. Additionally, food selectivity typically leads individuals with ASD to eat foods that are higher in fat and sodium, due to the limited variety consumed, which increases the individual’s risk for comorbid diagnoses of obesity, type 2 diabetes, chronic constipation, and hypertension (Peterson et al., 2016).
Inadequate nutrition can lead to increased difficulties for the individual in other domains as well. This requires the behavior analyst to collaborate with an interdisciplinary team, including the parents and caregivers, to best support the individual and family in all relevant areas. One side effect of feeding challenges is an increased risk for learning and behavioral problems (Levin et al., 2014). Another side effect of food selectivity is that it can lead to total food refusal, which can increase the risk of a diagnosis of failure to thrive or an insertion of a gastric feeding tube (Weber & Gutierrez, 2015). Ethical considerations of treatments, when comorbid diagnoses surrounding medical complications are present, are essential for all team members.
Feeding problems in children with ASD also have been demonstrated to increase caregiver stress (Bui et al., 2013; Curtin et al., 2015; A. J. Greer et al., 2008). A. J. Greer et al. (2008) noted that food selectivity and other feeding problems not only increase the individual’s risk for health problems but also negatively impact the parent–child relationship. Caregivers of children with chronic illnesses experience increased stress associated with the illness. Also, caregivers of children with food selectivity have reported feeling personally responsible for the feeding problems their child exhibits, as providing the nourishment the child needs is one of the fundamental responsibilities of a parent (A. J. Greer et al., 2008). When parents and caregivers are not able to complete this responsibility successfully, it has been shown to reduce their self-esteem, self-efficacy, and confidence in parenting (A. J. Greer et al., 2008), as well as reduce feelings of family cohesion or feelings of belonging (Curtin et al., 2015). This stress has been demonstrated to decrease upon the completion of intensive feeding treatment (A. J. Greer et al., 2008). However, even with the reduction of caregivers’ stress levels upon completion of the feeding intervention, about 30% of the caregivers still demonstrated clinical levels of stress, which may be accounted for by the feeling of a lack of support upon discharge (A. J. Greer et al., 2008). Continued collaboration with the family is clinically and ethically important to ensure generalization and maintenance of the skills acquired. Feeding treatment needs to be evaluated in terms of effectiveness, not only in regard to success in clinical conditions, but also in regard to success in other settings such as the home and to caregivers. This will not only increase feeding behavior in the individual but also assist with family and caregiver stress reduction.
With the majority of children diagnosed with ASD displaying various feeding problems (Schreck et al., 2004), the behavior analyst is faced with many ethical challenges surrounding the treatment of the feeding problem. Review articles to date have assisted behavior analysts to understand best practices from the standpoint of treatment outcomes of increased food acceptance and decreased problem mealtime behavior (Kerwin, 1999; Kerwin et al., 1995; Ledford et al., 2018; Sharp et al., 2010), but no literature has been published to assist the behavior analyst in selecting the most ethical course of responding when selecting feeding interventions. The following review is intended to provide behavior analysts with resources to assist with making collaborative and ethical decisions related to feeding when conducting assessments and when selecting treatments. The task is to select effective paths while minimizing negative side effects for the individual and family. Ethical decision making related to feeding will be reviewed with regard to the need for interdisciplinary collaboration for assessment and treatment, the navigation of the non-evidence-based and evidence-based treatment options, and the selection of the best ethical treatment option for clients.
The Need for Interdisciplinary Collaboration
The Behavior Analyst Certification Board’s (BACB’s) Professional and Ethical Compliance Code for Behavior Analysts (BACB, 2014) requires behavior analysts to practice only within their boundary of competence. Section 1.02 states that professional work is restricted to areas in which the individual has adequate training and supervised experience. If such experience is lacking, behavior analysts are obligated to obtain training or consultation to ensure appropriate intervention (BACB, 2014). There is a recognition that new areas of competence can be declared only when training and supervised experience have been completed. As feeding is a complex and multisystemic challenge, providing services for this presenting problem requires substantial additional study, training, and supervision and necessitates the expertise and input of several other disciplines.
Collaboration across the interdisciplinary team is essential for the individual’s success in feeding therapy, even if there is a lack of consensus about the path of treatment, or even about best practices. Most often, individuals with ASD and feeding challenges are working with many professionals from the medical, psychological, developmental, and educational fields, making the need for interdisciplinary collaboration especially important (Newhouse-Oisten et al., 2017). Section 4.02 of the Professional and Ethical Compliance Code for Behavior Analysts requires the behavior analyst to individualize the behavior-change program for the individual based on client-specific behaviors, current performance, and goals (BACB, 2014). Also, in Section 2.03, it requires behavior analysts to work cooperatively with other professions to further enhance treatments when appropriate, while also adhering to the principles of behavior analysis (BACB, 2014). It is also essential that all members of the interdisciplinary team acknowledge all treatments being implemented and how those treatments may interact with one another (Newhouse-Oisten et al., 2017). The collaborative process for feeding intervention is an ongoing process that continues past assessment, by circling continually back to other professionals throughout treatment, to ensure that treatment is not inadvertently causing harm and to ensure positive outcomes.
Medical
Collaboration with medical professionals greatly benefits the individual seeking feeding intervention by allowing for medical and structural evaluations and interventions implemented prior to the start of behavioral feeding intervention. Another section of the Professional and Ethical Compliance Code for Behavior Analysts also instructs the behavior analyst in regard to seeking medical consultation. Section 3.02 requires “behavior analysts recommend seeking a medical consultation if there is any reasonable possibility that a referred behavior is influenced by medical or biological variables” (BACB, 2014, p. 11). When working with individuals with feeding problems that require feeding therapy, the behavior analyst is required by the Professional and Ethical Compliance Code for Behavior Analysts to conduct the appropriate assessments and consultations. Behavior analysts are trained to focus attention on observable environmental events that occur before and after the behavior of interest. This does not provide behavior analysts with the medical knowledge required to successfully assess and implement all feeding interventions.
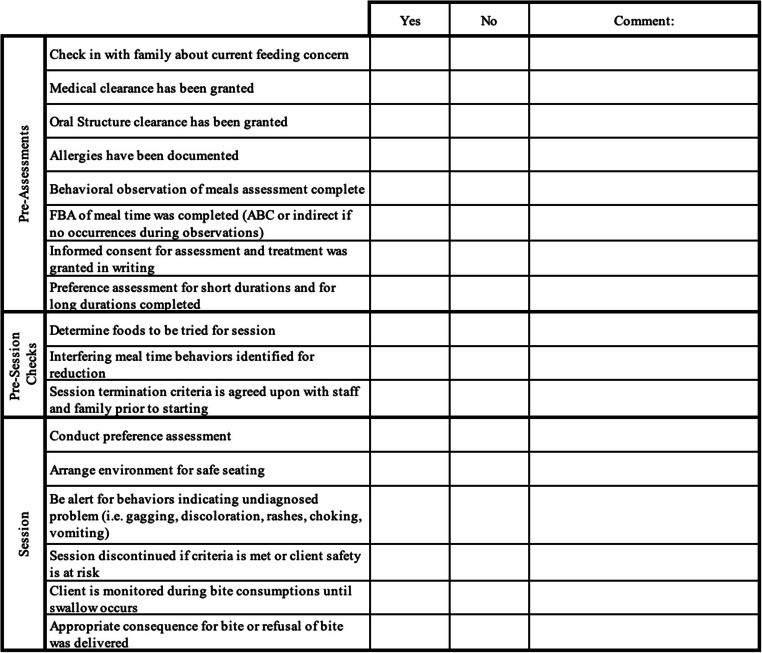
Feeding problems involve many aspects of the individual and the environment that all must be assessed to determine the most appropriate and ethical assessments and intervention, but they also require a comprehensive analysis of biological variables. Collaborating with medical professionals and other allied disciplines during assessments can help identify any medical symptoms that may lead to the feeding problems and possible food allergies or sensitivities that may exist (Miller et al., 2001). The gastroenterologist and pediatrician can diagnose and prescribe other diagnostic procedures within the child’s medical care while reviewing the child’s medical history to ensure medical causes of feeding sensitivities are controlled prior to behavioral intervention (Miller et al., 2001). Figure 1 provides a rubric for behavior analysts, and the first section includes a preassessment checklist to complete prior to any feeding intervention. This section of the tool will help ensure behavior analysts complete needed assessments prior to the implementation of a feeding program.
Fig. 1.
Rubric for Assisting Clinicians Prior to Implementing a Feeding Intervention With a Client
The use of a collaborative interdisciplinary team approach has been shown to accurately diagnose underlying medical causations such as cleft lip and palate, dysphagia, and chronic voice disorders (Miller et al., 2001). Assessment of swallowing is essential, as feeding selectivity may not be the primary concern if medical complications or physiological abnormalities exist within the individual. Some disciplines that may advise on medically complex feeding cases include gastroenterology, nursing, nutrition, occupational therapy, speech-language pathology, pulmonology, psychology, and dentistry (Miller et al., 2001). It is important to continue collaboration with these medical professionals throughout the feeding intervention, as novel medical complications may arise during intervention due to the individual trying novel foods and increasing the volume of food consumed.
It is also the case that many of these children have atypical gastrointestinal characteristics. A literature review was conducted of gastrointestinal symptoms and dysfunctions in children with ASD by McElhanon et al. (2014). It found that there is a higher prevalence of gastrointestinal symptoms in children with ASD than in those without. Limited information was provided regarding the etiology of the gastrointestinal symptoms, and more research was suggested to determine the impact of these symptoms and interventions for children with ASD (McElhanon et al., 2014). However, their research suggests there may be a link between these symptoms and the emergence, maintenance, and topographies of feeding problems in children with ASD (McElhanon et al., 2014). In any case, the prevalence of abnormal gastrointestinal findings warrants an assessment by a specialist during the assessment phase. The identification of a medical causation, such as abnormal gastrointestinal findings, may result in the need for various antecedent manipulations that are outside the behavior analyst’s scope of practice (Newhouse-Oisten et al., 2017). For example, it may be necessary to first introduce medication and monitor its impact throughout treatment.
Allied Health
Behavior analysts must ensure that the interdisciplinary assessment and treatment approach is individualized and ethical. Collaboration with allied health professionals assists in the creation of individualized treatments. Allied health professionals are health professionals who are not physicians or nurses, but rather clinicians who complement their work by referencing scientific, evidence-based practices for evaluating and treating various diagnoses (Dillenburger et al., 2014; Klaic et al., 2018). Allied health professionals include speech-language pathologists, nutritionists, dietitians, physical therapists, and occupational therapists.
Coordinating intervention with allied health professionals assists behavior analysts in individualizing assessment and treatment for children with ASD. Speech-language pathologists trained in feeding practices benefit the intervention by evaluating oral motor feeding skills, identifying signs of swallowing dysfunction, and assessing the oral structure of the individual’s mouth. Occupational therapists may help by assessing and treating issues in oral motor skills, seating and positioning, and self-feeding skills (Cermak et al., 2010). Nutritionists or registered dieticians conduct nutritional assessments to identify foods to target and foods to avoid, due to allergies or sensitivities. The manipulation of types of foods is another antecedent manipulation that can increase success in feeding programs when collaboration with medical personnel occurs. Each of these professionals presents with a different scope of practice and training; collectively, the addition of the various inputs enables an individualized feeding intervention (LaFrance et al., 2019).
The behavior analyst should work collaboratively with these professionals to ensure individualization, best practice interventions, and a continuous data-based evaluation of client progress. Collaboration is sometimes challenging across allied health disciplines due to differing worldviews. However, all professionals should seek information on all fields involved in assessment and treatment to understand the value each professional brings to helping the individual (LaFrance et al., 2019). Once the mealtime behavior is determined to be maintained by environmental events that can be manipulated, a behavior analyst is valuable in the treatment of these behaviors. The behavior analyst should always determine if the treatment can be translated into behavioral principles and goals for the client while maintaining client safety (see the Appendix).
Parents and Caregivers
Prior to beginning any assessments or interventions, the behavior analyst must obtain informed consent from the individual and/or the individual’s caregiver; such consent should specify assessment procedures, treatment parameters, and the interprofessional collaboration model. Section 3.03 of the Professional and Ethical Compliance Code for Behavior Analysts requires behavior analysts to provide a thorough description of assessments and procedures to the client and obtain written permission from the client before their implementation (BACB, 2014). Following the assessment, the behavior analyst is also obligated, by Section 3.04 of the Professional and Ethical Compliance Code for Behavior Analysts, to review the results of the assessment with the client with language comprehensible to the client (BACB, 2014).
This informed consent for the assessment and about the assessment results can be completed in many ways. It is essential that the behavior analyst explain assessments, procedures, and results in language that is understandable to the individual, and that this is presented without coercion to engage in any assessment or treatment. Section 1.05b of the Professional and Ethical Compliance Code for Behavior Analysts emphasizes that behavior analysts are to use language that is understandable to the client and to provide information at the outset and throughout intervention regarding the nature of the intervention and the progress made (BACB, 2014).
Ahearn et al. (1996) used a flowchart that outlined each consequence that would be applied to the feeding behaviors to describe the assessment process to the participant’s caregivers. Upon explanation of procedures, in terms the caregiver or individual understands, the behavior analyst must collect written informed consent before continuing with feeding assessment and intervention.
Upon consent being collected from parents and caregivers, it is also essential to include them in the implementation of treatment. Parent and caregiver interviews can further assist the behavior analyst in determining the individual’s preferences, which can later be formally assessed in a preference and reinforcer assessment. For example, reinforcers that can be engaged with for short durations can be used for intertrial reinforcement, whereas reinforcers that are engaged in for longer durations can be used for terminal reinforcers. Prior to all feeding sessions, collaborations with parents and nutritionists should involve determining the foods that will be presented during sessions and the interfering mealtime behaviors that the family would like targeted for decrease (see Fig. 1). Feeding session termination criteria should also be discussed and agreed on prior to the session. Parent and caregiver involvement in treatment implementation is also a critical component for the generalization of treatment outcomes across foods, people, and settings (Brown et al., 2002; Gentry & Luiselli, 2008; Luiselli & Luiselli, 1995).
The Role of the Behavior Analyst
Upon completion of the interdisciplinary assessments (see Figure 1), a behavior analyst can then assess the feeding problems and mealtime problem behavior with a functional assessment. Any treatment would need to be preceded by an assessment. According to Section 3.01 of the Professional and Ethical Compliance Code for Behavior Analysts, the behavior analyst is to conduct an updated assessment before recommending or implementing a behavior-change program, and the nature of assessment is dependent on client-specific needs and variables. If the behavior analyst is targeting a behavior for reduction, Section 3.01 also requires that they first complete a functional assessment (BACB, 2014).
Piazza et al. (2003) demonstrated that the use of a functional analysis of feeding behavior was successful in identifying the function of the individual’s feeding behavior. Upon implementation of function-based treatment of the individuals’ aberrant feeding behaviors, all met their treatment goal for oral intake of foods. Borrero et al. (2016) compared results of a descriptive assessment to an experimental analysis to determine the function of feeding behavior. The results suggested that the descriptive assessment yielded similar results to the experimental analysis, suggesting that descriptive assessments may be sufficient for identifying the function of feeding behaviors in individuals with ASD (Borrero et al., 2016).
Following the functional behavior assessment, the behavior analyst should continue to collaborate with the interdisciplinary team to determine the best intervention plan for the individual. The behavior analyst is a valuable team member for modifying environmental contingencies to increase the individual’s feeding behavior. The Professional and Ethical Compliance Code for Behavior Analysts states that the least restrictive procedure be used with clients, which may include a combination of strategies across disciplines. Specifically, Section 4.09 of the Professional and Ethical Compliance Code for Behavior Analysts emphasizes that the behavior analyst is to assess the restrictive nature of a procedure to then recommend the procedure that is least restrictive while maintaining effectiveness (BACB, 2014). In regard to behavioral assessments conducted and interventions implemented for feeding problems, the behavior analyst is required to implement the procedures that are least restrictive yet likely to be effective and efficient.
Navigating Non-Evidence-Based Practices
With interdisciplinary collaboration, it is important to acknowledge differing philosophies to develop a treatment with the individual’s best interests in mind (LaFrance et al., 2019). One area that can lead to some disagreements across disciplines is what constitutes empirically based practices, as fields do not define it similarly. This may then lead to discrepancies in the treatments recommended.
Section 2.09 of the Professional and Ethical Compliance Code for Behavior Analysts includes clients’ right to effective treatment. It emphasizes the rights of clients to effective intervention and behavior analysts’ responsibility to advocate for its implementation with their clients (BACB, 2014). The behavior analyst must share the extant literature with the client and disclose the results of comparison studies to assist the client in making an informed decision about intervention. In addition, behavior analysts warn consumers about interventions without merit.
One common area that is often recommended by occupational therapy or speech-language therapy is the use of sensory integration. Many occupational therapy resources identify the approach as having a limited data base and, as a result, recommend limiting its use to ensure effective outcomes (LaFrance et al., 2019). Peterson et al. (2016) conducted a search and found that 64% of self-identified pediatric feeding disorder programs listed the sequential oral sensory (SOS) approach as a primary form of treatment provided within their feeding programs, despite the limited empirical support for this method.
A study that investigated the prevalence of atypical sensory processing found that those with ASD had a higher prevalence than their typically developing peers, which may account for the frequent implementation of sensory-based interventions (Chistol et al., 2018). Chistol et al. (2018) suggested that addressing oral sensory processing with children with ASD may assist with increasing food acceptance (Chistol et al., 2018). The strategies listed include changing the texture and consistency of foods to allow the foods to have “more manageable sensory characteristics” and using a sensory-integration approach to decrease the individual’s sensitivity to sensory input (Chistol et al., 2018).
The SOS approach is an alternative treatment to behavioral feeding therapy. This approach involves a 12-week program that uses a desensitization hierarchy consisting of visual tolerance, interaction, smell, touch, taste, and eating to increase the child’s tolerance of new foods (Benson et al., 2013). If the child’s stress response becomes too high during intervention, the therapist then removes the presentation of the food and reduces the demand to previously mastered steps of the desensitization hierarchy to allow the child to relax and reorganize (Peterson et al., 2016). Benson et al. (2013) conducted a review of children who received SOS therapy for 1–3 years and found that 68% of children showed no improvements. It is a popular approach without scientific support.
Peterson et al. (2016) conducted a study to compare the effects of the SOS approach with the effects of a behavioral feeding intervention using escape extinction with nonremoval of the spoon during bite presentations. The researchers needed to modify the SOS protocol to allow for systematic comparisons between approaches. The behavioral intervention resulted in an increase in age-appropriate eating behaviors with the participants. It was also noted that all participants consumed foods with the behavioral intervention approach, whereas no participants consistently consumed foods with the SOS therapy approach (Peterson et al., 2016). These results represent a direct comparison of the methods and clearly support the effectiveness of the behavioral approach and the lack of effectiveness of the SOS approach.
Another study that compared sensory-integration and behavior treatments demonstrated that behavioral intervention components were necessary to treat the feeding disorders effectively (Addison et al., 2012). The sensory-integration perspective of feeding views inappropriate mealtime behavior and food selectivity as symptoms of the individual’s inability to process the sensory information and make an adaptive response (Addison et al., 2012). There is an a priori assumption that such processing difficulties are responsible for aberrant feeding behaviors. However, there is no empirical support for this explanation or for interventions based on this premise.
Many practitioners recommend sensory-integration therapy for children with feeding problems to reduce their sensory defensiveness and allow them to effectively process sensory information, even despite behavioral methods having strong research support (Seiverling et al., 2018). Seiverling et al. (2018) completed a study comparing a behavioral feeding intervention with and without premeal sensory-integration therapy. The use of sensory-integration therapy suggests there might be an enhanced treatment effect; however, Seiverling et al. did not observe any enhancement effect for a behavioral feeding intervention when sensory-integration therapy was used prior to mealtimes.
It is important for behavior analysts and the interdisciplinary team to recognize that there have been no noted empirical studies that support the various components of a sensory-integration approach for feeding intervention, but it continues to be a treatment recommendation by professionals from several disciplines (Addison et al., 2012). Cermak et al. (2010) suggested that 70% of children with ASD chose their foods based on texture, compared to only 11% of typically developing children, indicating some sensitivity/preference in this area. Cermak et al. suggested that this may be a manifestation of tactile defensiveness, so that certain textures of food and other activities involving the mouth are avoided, and as a result, sensory-based treatment is often recommended. However, behavioral alternatives to this intervention exist and are likely to be associated with vastly superior outcomes.
The use of sensory-integration techniques brings forward ethical considerations for the behavior analyst. The behavior analyst is required by the Professional and Ethical Compliance Code for Behavior Analysts to remain rooted in science in all interventions. Section 1.01 of the Professional and Ethical Compliance Code for Behavior Analysts requires behavior analysts to use their knowledge of science and behavior analysis when participating in academic, professional, or human services (BACB, 2014). Brodhead (2015) discussed how it is “important for [behavior analysts] to have a systematic strategy when faced with a non-behavioral treatment recommendation in order to maintain high standards of professional behavior” (p. 71).
Some aspects of sensory desensitization can be implemented within the behavioral feeding intervention and have been effective at increasing food acceptance in individuals who previously refused various textures. Patel et al. (2002) increased the consumption of foods by shaping and fading food consistencies presented to the individual, and demonstrated an increase in overall consumption. Patel et al. (2001) and Hagopian et al. (1996) used a fading procedure successfully to increase fluid consumption in a child with feeding problems. All of these studies systematically used fading and shaping to increase the participants’ acceptance of various textures. If these children were experiencing sensory defensiveness, it could be said these procedures addressed those sensory needs systematically through behavioral programming. Tolerance was shaped and systematically increased. This demonstrates that with collaboration with the interdisciplinary team, the behavior analyst can adapt a treatment recommended to include empirically supported behavioral principles.
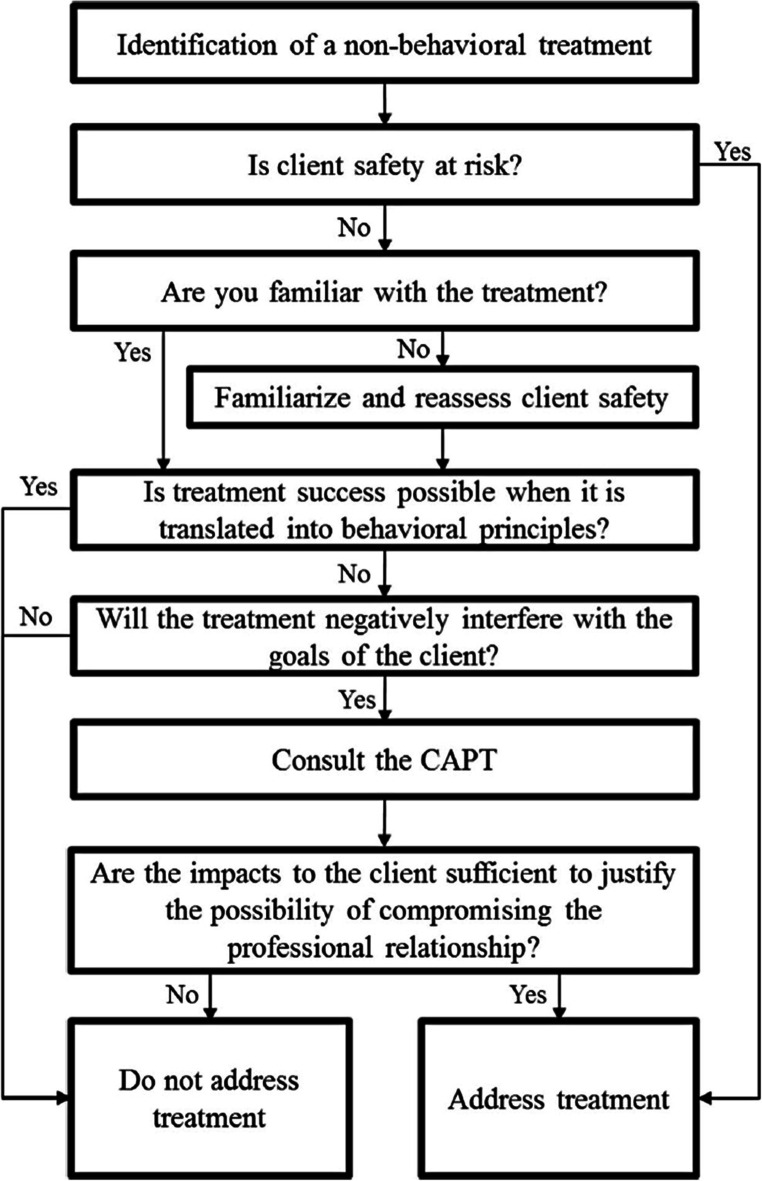
Behavior analysts must educate themselves about the recommended interventions and base their decisions on treatment implementation on the literature review and on the assessments of the individual. Using the decision tree provided by Brodhead (2015) could be helpful for determining if the treatment is best practice and if its implementation would be ethical (see the Appendix). Brodhead presented a decision-making model to be used in assessing nonbehavioral interventions. Some of the steps it assists with are assessing client safety risks, assessing clinician expertise, translating treatments into behavioral principles, assessing if the treatment would interfere with client goals, and assessing the professional relationship with other practitioners working with the client (Brodhead, 2015).
Navigating Evidence-Based Practices
In reviews of the literature, evidence-based practices have demonstrated success in the reduction of feeding problems (Kerwin et al., 1995; Ledford et al., 2018). The most commonly used evidence-based procedures are differential reinforcement, physical guidance, and escape extinction. Although each of these procedures is an evidence-based practice, a behavior analyst needs to refer to the Professional and Ethical Compliance Code for Behavior Analysts to further assist with determining which one of the practices is appropriate for implementation.
Positive Reinforcement Strategies
The use of differential reinforcement has consistently been demonstrated to be an effective intervention to increase appropriate mealtime behavior and feeding (Kerwin et al., 1995; Ledford et al., 2018). The literature review conducted by Kerwin et al. (1995) found that differential reinforcement was used across a variety of feeding problems, diverse populations of children, settings, training designs, and behaviors.
Ledford et al. (2018) conducted a literature review and found that the use of contingent rewards was present in 82% of the studies; however, it was implemented as a non-function-based intervention for 67% of the studies. Upon review, a behavior analyst would have to decide if the use of a non-function-based intervention aligns with Section 4.01 of the Professional and Ethical Compliance Code for Behavior Analysts, which requires interventions align with concepts of behavior analysis (BACB, 2014).
Some studies have compared the use of noncontingent reinforcement with the use of escape extinction. The results from one study suggest that the noncontingent positive reinforcement procedure was not effective in increasing food consumption but did appear to reduce the effects of extinction bursts in some of the participants, as evident in lower levels of inappropriate behavior (Piazza et al., 2003). Reed et al. (2004) conducted a similar study by also comparing the use of noncontingent reinforcement with extinction. Their results were similar, with overall findings suggesting that noncontingent reinforcement did not increase consumption but did reduce inappropriate behaviors associated with mealtime.
When implementing feeding procedures, the behavior analyst should be aware of the least restrictive procedure to use. Various positive reinforcement procedures have demonstrated success with feeding interventions, but results suggest that a more intrusive procedure may also be necessary.
The use of positive reinforcement procedures during feeding intervention has demonstrated an effect on the target behavior, but the behavior analyst needs to individualize the treatment for their client to ensure the best effective treatment. Noncontingent reinforcement and differential reinforcement are two of the positive reinforcement procedures that have demonstrated success. Other positive reinforcement procedures that have demonstrated success include modeling (R. D. Greer et al., 1991), shaping (Cosbey & Muldoon, 2017), fading (Brown et al., 2002), visual supports (Gentry & Luiselli, 2008), and high-probability or simultaneous presentations (Silbaugh & Swinnea, 2018). Section 4.03 of the Professional and Ethical Compliance Code for Behavior Analysts requires behavior analysts adapt interventions to ensure individualization of treatment based on client variables and needs (BACB, 2014). If the client’s goal is to decrease inappropriate mealtime behavior, research suggests positive reinforcement procedures could be effectively implemented. Positive reinforcement procedures are often implemented as a component of a treatment package, and more research is needed on the use of positive reinforcement as a sole treatment for feeding issues. Research on positive reinforcement as a sole treatment for feeding might assist behavior analysts in determining more efficient and effective interventions while reducing the use of and reliance on aversive stimuli.
Physical Prompting
Another component of feeding intervention packages that has demonstrated success is the use of physical prompting (Borrero et al., 2013). Physical prompts can be completed in various ways. The most common physical prompts used during feeding intervention are hand-over-hand physical prompting to promote self-feeding and a jaw prompt or finger prompt to promote the individual opening their mouth (Borrero et al., 2013). The use of physical prompting is an intrusive procedure, and the behavior analyst should attempt less intrusive procedures before using physical prompting in feeding interventions. Additionally, the interdisciplinary team should agree on the conditions for the termination of physical prompting prior to starting its use.
If no progress is observed with positive reinforcement procedures alone, the use of physical prompting may be necessary and has been shown to be effective. This may be because the individual is negatively reinforced on acceptance of a bite by the removal of the jaw prompt. The negative reinforcement from the removal of the jaw prompt may have a greater value to the individual than the negative reinforcement they received from food refusal (Borrero et al., 2013).
Upon review of the Professional and Ethical Compliance Code for Behavior Analysts, a behavior analyst would be faced with determining if procedures with a physical prompt can be ethically implemented with their client. The procedure of using physical prompts to decrease food refusal could also be viewed as a punishment procedure or an aversive method. Section 4.08 of the Professional and Ethical Compliance Code for Behavior Analysts highlights the need to use reinforcement-based procedures first and/or in combination with punishment-based procedures unless severity warrants more intrusive, immediate procedures (BACB, 2014). Consultation with medical and allied health professionals assists the behavior analyst in the ethical decision of whether physical prompting is necessary due to the severity of the individual’s feeding problem.
Many years ago, Ives et al. (1978) conducted a study that used forced feeding to increase food acceptance in a child with ASD. The authors reviewed how the physical prompt procedure is “not pleasant” to the individual and should not be used as a first-choice intervention for food refusal. The authors also discussed that the removal of the contingency resulted in an immediate increase in food refusal (Ives et al., 1978). This suggests that the physical prompts used were aversive to the individual, and the behavior pattern suggests punishment may have been the principle in effect.
Upon completion of a study comparing physical prompting and nonremoval of the spoon, Ahearn et al. (1996) conducted a social validity study with the participants’ caregivers. Upon watching videos of the two procedures, the caregivers were asked which procedure they would like to be trained on to implement with their child. This social validity check supports Section 4.02 of the Professional and Ethical Compliance Code for Behavior Analysts, which emphasizes the responsibility of the behavior analyst to include the client in the development and consent of treatment (BACB, 2014). All caregivers selected physical prompting over nonremoval of the spoon (Ahearn et al., 1996). Upon further questioning, it was revealed that physical prompting was perceived as resulting in more rapid results and producing fewer interfering behaviors (Ahearn et al., 1996). Such information, from the collaboration with the parents and caregivers, is important, as it may influence adherence.
Escape Extinction
Research has demonstrated that feeding problems are often maintained by negative reinforcement of the feeding behavior (LaRue et al., 2011). The implementation of escape extinction is a common procedure to reduce feeding problems maintained by escape from demands or an aversive presentation of a nonpreferred food (Ahearn et al., 2001; Borrero et al., 2013; Piazza et al., 2003). Escape extinction for feeding behavior is implemented by the continuation of food presentation and ends upon the acceptance of presented foods, even if the individual exhibits inappropriate mealtime behavior or refusal (Cooper et al., 2020). When the inappropriate mealtime behavior or refusal is no longer followed by the reinforcing consequence of escaping the meal or food presentation, the behavior should gradually decrease or stop entirely (Cooper et al., 2020).
The use of extinction should be implemented with caution. First, it is imperative that the behavior analyst determine the function of the behavior prior to implementing extinction to address the appropriate function of the behavior in order for extinction to be effective (Carr et al., 2000). Also, there are common negative side effects associated with escape extinction procedures. Some of these negative side effects include an initial increase in the frequency of the unwanted behavior, an initial increase in the magnitude of the unwanted behavior, spontaneous recovery of the unwanted behavior, increased aggression, and emotional behavior (Carr et al., 2000;Cooper et al., 2020 ; Vollmer & Athens, 2011). Another consideration is the need for consistent implementation with escape extinction; otherwise, one risks the behavior experiencing intermittent reinforcement (Carr et al., 2000). The more contact the individual has with negative reinforcement of escape during mealtime, the greater the resistance to extinction the behavior may exhibit, which would increase the caregiver’s effort to extinguish the unwanted behavior (Cooper et al., 2020; Vollmer & Athens, 2011). The increased effort required by caregivers to implement escape extinction suggests further collaboration is needed with caregivers when determining which intervention to implement and when to terminate the intervention if caregivers express increased concerns or if limited progress is observed.
The implementation of escape extinction with feeding interventions can be labeled as escape extinction, nonremoval of the spoon, re-presentation of expelled bites, escape prevention, and physical prompting for acceptance (Ledford et al., 2018). In a review article by Ledford et al. (2018), it was noted that nonremoval of the spoon was implemented in 40% of the reviewed articles, and re-presentation of expelled bites was implemented in 31% of the reviewed articles. It was also noted that the procedure matched the function of the participants’ food refusal 85% of the time for nonremoval of the spoon and 81% of the time for re-presentation of expelled bites (Ledford et al., 2018).
Before implementing escape extinction with a client, the behavior analyst must ensure that a medical consultation has occurred and that medical clearance is granted, as required by Section 3.02 of the Professional and Ethical Compliance Code for Behavior Analysts (BACB, 2014). Underlying medical conditions can interfere with the success of escape extinction, as the individual may be engaging in escape behaviors to prevent the pain associated with eating foods due to an underlying medical condition (LaRue et al., 2011). Upon treatment of the medical condition, escape extinction has been successful, as the individual then contacts the food without the pain that was previously paired with feeding (LaRue et al., 2011). Ongoing collaboration with medical professionals is essential to ensure the ethical treatment of the individual and the individual’s safety during the use of escape extinction, as other problem behaviors may arise.
Escape extinction has been implemented across many studies with demonstrated increases in participants’ food acceptance (Ahearn et al., 1996; Borrero et al., 2013;Piazza et al., 2003 ; Reed et al., 2004). Some researchers have suggested that the combination of positive reinforcement procedures and escape extinction may also reduce other inappropriate mealtime behaviors (Piazza et al., 2003; Reed et al., 2004). Borrero et al. (2013) did not implement other positive reinforcement procedures, and an extinction burst in inappropriate mealtime behavior was observed during the first treatment phase for one of their participants. Combining positive reinforcement with escape extinction may prevent an increase in inappropriate mealtime behaviors upon the introduction of escape extinction.
The studies noted previously were conducted in a clinic where the environment could be consistently controlled. To generalize the results to the client’s home environment, the behavior analyst must consider the variables that may interfere with the implementation of escape extinction. Section 4.07b of the Professional and Ethical Compliance Code for Behavior Analysts requires the identification of environmental variables that may impact the effectiveness of the intervention and the elimination of identified variables when it is possible to do so (BACB, 2014). Prior to implementation, the behavior analyst also must include the client in the development of the intervention (BACB, 2014, Section 4.02), which may also assist with minimizing various environmental constraints in the home environment.
Prior to the implementation of an escape extinction procedure, informed consent must be gathered in writing and termination criteria must be written and agreed on. Section 4.11 of the Professional and Ethical Compliance Code for Behavior Analysts emphasizes the identification of measurable termination criteria for the intervention that are then explained to and understood by the client (BACB, 2014). The termination criteria for escape extinction may include termination of the intervention if the inappropriate mealtime behavior escalates to a predetermined level. Preventing an increase in inappropriate mealtime behaviors upon implementation of escape extinction is important to consider to avoid harm to the individual and to decrease the risk of termination of services before target levels are achieved.
Nonremoval of the spoon has been reported anecdotally by parents to be hard for them to watch being implemented with their children (Tarbox et al., 2010). Escape extinction can be viewed as an intrusive procedure to parents who are untrained in behavior-change programs. For this reason, parents can find escape extinction not only hard to watch but also even harder to accurately implement, which then reduces treatment fidelity (Tarbox et al., 2010).
When behavior analysts provide information to the client and caregivers about the intervention, to receive informed consent at the start of services, the behavior analyst must also review other interventions that are available to the client. The Professional and Ethical Compliance Code for Behavior Analysts lists considerations in selecting among evidence-based procedures, including efficacy, practitioner familiarity, and the risk-benefit analysis of the treatment (BACB, 2014). The client and caregiver have the right to choose among interventions, and the behavior analyst must disclose the negative effects that escape extinction may have to the client (extinction bursts) and caregivers (increase stress during observation and implementation).
Conclusion and Recommendations
There are many elements to treating selective feeding and food refusal that require nuanced ethical analysis. This is a complex problem requiring a specialized skill set. Behavior analysts need to examine whether they have the skills to meet the complex needs associated with this intervention, or whether more supervision, training, or consultation is needed. In addition, this intervention should be provided only when consent is fully informed and parents are aware of the difficulties it can pose. Great attention must be paid to how the procedures are described.
In approaching these issues, assessment is crucial. Behavior analysts must work in concert with professionals with complementary expertise. Swallowing and coordination issues can be assessed by occupational therapists and speech-language pathologists with specialized training. Physicians can evaluate the presence of gastrointestinal abnormalities. Nutritionists can examine concerns about caloric adequacy and whether the individual is nutritionally compromised. A coordinated effort is required to ensure a complete and multidisciplinary approach. A functional assessment must be done by the behavior analyst to determine the possible function(s) of the feeding behaviors and to inform treatment. There is some evidence that a functional assessment may be adequate and that a more formal functional analysis may not be required. A rubric (Fig. 1) and treatment decision tree (see the Appendix) to assist clinicians in ensuring ethical practices during assessment may be helpful tools. Such tools provide clinicians with information about the steps necessary during assessments and prior to a feeding intervention plan.
From a treatment perspective, there are many options, but the clinician must evaluate which approach is best suited to the individual client. This requires evaluating many contextual factors, including the parents’ ability to tolerate and implement more intrusive procedures. Ethical concerns permeate every aspect of the process—from identifying the issue and assessing the problem in a comprehensive manner, to treating the behavior with effective and socially valid interventions.
Appendix
Fig. 2.
Decision Tree Provided by Brodhead (2015) for Assessing Nonbehavioral Interventions. Note. From “Maintaining Professional Relationships in an Interdisciplinary Setting: Strategies for Navigating Nonbehavioral Treatment Recommendations for Individuals With Autism,” by M. T. Brodhead, 2015, Behavior Analysis in Practice, 8, p. 73 (https://doi.org/10.1007/s40617-015-0042-7). Copyright 2015 by Springer Nature Customer Service Centre GmbH. Reprinted with permission.
Declarations
Conflict of interest
We have no known conflicts of interest to disclose.
Ethical approval
This review did not involve human participants and/or animals.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Addison LR, Piazza CC, Patel MR, Bachmeyer MH, Rivas KM, Milnes SM, Oddo J. A comparison of sensory integrative and behavioral therapies as treatment for pediatric feeding disorders. Journal of Applied Behavior Analysis. 2012;45(3):455–471. doi: 10.1901/jaba.2012.45-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahearn WH, Kerwin ME, Eicher PS, Lukens CT. An ABAC comparison of two intensive interventions for food refusal. Behavior Modification. 2001;25(3):385–405. doi: 10.1177/0145445501253002. [DOI] [PubMed] [Google Scholar]
- Ahearn, W. H., Kerwin, M. E., Eicher, P. S., Shantz, J., & Swearingin, W. (1996). An alternating treatments comparison of two intensive interventions for food refusal. Journal of Applied Behavior Analysis, 29(3), 321–332. 10.1901/jaba.1996.29-321. [DOI] [PMC free article] [PubMed]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
- Avni, E., Ben-Itzchak, E., & Zachor, D. A. (2018). The presences of comorbid ADHD and anxiety symptoms in autism spectrum disorder: Clinical presentation and predictors. Frontiers in Psychiatry, 9, 717. 10.3389/fpsyt.2018.00717. [DOI] [PMC free article] [PubMed]
- Bandini, L., Curtin, C., Phillips, S., Anderson, S. E., Maslin, M., & Must, A. (2017). Changes in food selectivity in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(2), 439–446. 10.1007/s10803-016-2963-6. [DOI] [PMC free article] [PubMed]
- Behavior Analyst Certification Board. (2014). Professional and ethical compliance code for behavior analysts. https://www.bacb.com/wp-content/uploads/BACB-Compliance-Code-english_190318.pdf
- Benson, J. D., Parke, C. S., Gannon, C., & Munoz, D. (2013). A retrospective analysis of the sequential oral sensory feeding approach in children with feeding difficulties. Journal of Occupational Therapy, Schools, & Early Intervention, 6, 289–300. 10.1080/19411243.2013.860758.
- Borrero CSW, England JD, Sarcia B, Woods JN. A comparison of descriptive and functional analyses of inappropriate mealtime behavior. Behavior Analysis in Practice. 2016;9:364–379. doi: 10.1007/s40617-016-0149-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrero CSW, Schlereth GJ, Rubio EK, Taylor T. A comparison of two physical guidance procedures in the treatment of pediatric food refusal. Behavioral Interventions. 2013;28:261–280. doi: 10.1002/bin.1373. [DOI] [Google Scholar]
- Brodhead MT. Maintaining professional relationships in an interdisciplinary setting: Strategies for navigating nonbehavioral treatment recommendations for individuals with autism. Behavior Analysis in Practice. 2015;8:70–78. doi: 10.1007/s40617-015-0042-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JF, Spencer K, Swift S. A parent training programme for chronic food refusal: A case study. British Journal of Learning Disabilities. 2002;30:118–121. doi: 10.1046/j.1468-3156.2002.00128.x. [DOI] [Google Scholar]
- Bui LTD, Moore DW, Anderson A. Using escape extinction and reinforcement to increase eating in a young child with autism. Behaviour Change. 2013;30(01):48–55. doi: 10.1017/bec.2013.5. [DOI] [Google Scholar]
- Carr, J. E., Coriaty, S., & Dozier, C. L. (2000). Current issues in the function-based treatment of aberrant behavior in individuals with developmental disabilities. In J. Austin & J. E. Carr (Eds.), Handbook of applied behavior analysis (pp. 91–112). Context Press.
- Cermak SA, Curtin C, Bandini LG. Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of the American Dietetic Association. 2010;110(2):238–246. doi: 10.1016/j.jada.2009.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherif L, Bouadbous J, Khemekhem K, Mkawer S, Ayadi H, Moalla Y. Feeding problems in children with autism spectrum disorders. Journal of Family Medicine. 2018;1(1):30–39. doi: 10.1177/10883576060210030401. [DOI] [Google Scholar]
- Chistol LT, Bandini LG, Must A, Phillips S, Cermak SA, Curtin C. Sensory sensitivity and food selectivity in children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2018;48(2):583–591. doi: 10.1007/s10803-017-3340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, J. O., Heron, T. E., & Heward, W. L. (2020). Applied behavior analysis (3rd ed.). Pearson Education.
- Cosbey J, Muldoon D. EAT-UP™ family-centered feeding intervention to promote food acceptance and decrease challenging behaviors: A single-case experimental design replicated across three families of children with autism spectrum. Journal of Autism and Developmental Disorders. 2017;47(3):564–578. doi: 10.1007/s10803-016-2977-0. [DOI] [PubMed] [Google Scholar]
- Curtin C, Hubbard K, Anderson SE, Mick E, Must A, Bandini LG. Food selectivity, mealtime behavior problems, spousal stress, and family food choices in children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders. 2015;45(10):3308–3315. doi: 10.1007/s10803-015-2490-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillenburger K, Röttgers HR, Dounavi K, Sparkman C, Keenan M, Thyer B, Nikopoulos C. Multidisciplinary teamwork in autism: Can one size fit all? Australian Educational and Developmental Psychologist. 2014;31(2):97–112. doi: 10.1017/edp.2014.13. [DOI] [Google Scholar]
- Gentry JA, Luiselli JK. Treating a child’s selective eating through parent implemented feeding intervention in the home setting. Journal of Developmental and Physical Disabilities. 2008;20(1):63–70. doi: 10.1007/s10882-007-9080-6. [DOI] [Google Scholar]
- Greer AJ, Gulotta CS, Masler EA, Laud RB. Caregiver stress and outcomes of children with pediatric feeding disorders treated in an intensive interdisciplinary program. Journal of Pediatric Psychology. 2008;33(6):612–620. doi: 10.1093/jpepsy/jsm116. [DOI] [PubMed] [Google Scholar]
- Greer RD, Dorow L, Williams G, McCorkle N. Peer-mediated procedures to induce swallowing and food acceptance in young children. Journal of Applied Behavior Analysis. 1991;24(4):783–790. doi: 10.1901/jaba.1991.24-783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths DL, Farrell LJ, Waters AM, White SW. Clinical correlates of obsessive compulsive disorder and comorbid autism spectrum disorder in youth. Journal of Obsessive-Compulsive and Related Disorders. 2017;14:90–98. doi: 10.1016/j.jocrd.2017.06.006. [DOI] [Google Scholar]
- Hagopian LP, Farrell DA, Amari A. Treating total liquid refusal with backward chaining and fading. Journal of Applied Behavior Analysis. 1996;29(4):573–575. doi: 10.1901/jaba.1996.29-573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ives CC, Harris SL, Wolchik SA. Food refusal in an autistic type child treated by a multi-component forced feeding procedure. Journal of Behavioral Therapy and Experimental Psychiatry. 1978;9:61–64. doi: 10.1016/0005-7916(78)90090-3. [DOI] [Google Scholar]
- Keen DV. Childhood autism, feeding problems and failure to thrive in early infancy: Seven case studies. European Child and Adolescent Psychiatry. 2008;17(4):209–216. doi: 10.1007/s00787-007-0655-7. [DOI] [PubMed] [Google Scholar]
- Kerwin ME. Empirically supported treatments in pediatric psychology: Severe feeding problems. Journal of Pediatric Psychology. 1999;24(2):193–214. doi: 10.1093/jpepsy/24.3.193. [DOI] [PubMed] [Google Scholar]
- Kerwin ME, Ahearn WH, Eicher PS, Burd DM. The costs of eating: A behavioral economic analysis of food refusal. Journal of Applied Behavior Analysis. 1995;28(3):245–260. doi: 10.1901/jaba.1995.28-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaic M, McDermott F, Haines T. How soon do allied health professionals lose confidence to perform EBP activities? A cross-sectional study. Journal of Evaluation in Clinical Practice. 2018;25(4):603–612. doi: 10.1111/jep.13001. [DOI] [PubMed] [Google Scholar]
- LaFrance DL, Weiss MJ, Kazemi E, Gerenser J, Dobres J. Multidisciplinary teaming: Enhancing collaboration through increased understanding. Behavior Analysis in Practice. 2019;12(3):709–726. doi: 10.1007/s40617-019-00331-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaRue RH, Stewart V, Piazza CC, Volkert VM, Patel MR, Zeleny J. Escape as reinforcement and escape extinction in the treatment of feeding problems. Journal of Applied Behavior Analysis. 2011;44(4):719–735. doi: 10.1901/jaba.2011.44-719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledford JR, Whiteside E, Severini KE. A systematic review of interventions for feeding-related behaviors for individuals with autism spectrum disorders. Research in Autism Spectrum Disorders. 2018;52:69–80. doi: 10.1016/j.rasd.2018.04.008. [DOI] [Google Scholar]
- Levin DS, Volkert VM, Piazza CC. A multi-component treatment to reduce packing in children with feeding and autism spectrum disorders. Behavior Modification. 2014;38(6):940–963. doi: 10.1177/0145445514550683. [DOI] [PubMed] [Google Scholar]
- Luiselli, J. K. & Luiselli, T. E. (1995). A behavior analysis approach toward chronic food refusal in children with gastrostomy-tube dependency. Topics in Early Childhood Special Education, 15(1), 1–18.
- McElhanon BO, McCracken C, Karpen S, Sharp WG. Gastrointestinal symptoms in autism spectrum disorder: A meta-analysis. Pediatrics. 2014;133(5):872–883. doi: 10.1542/peds.2013-3995. [DOI] [PubMed] [Google Scholar]
- Miller CK, Burklow KA, Santoro K, Kirby E, Mason D, Rudolph CD. An interdisciplinary team approach to the management of pediatric feeding and swallowing disorders. Children’s Health Care. 2001;30(3):201–218. doi: 10.1207/S15326888CHC3003_3. [DOI] [Google Scholar]
- Newhouse-Oisten MK, Peck KM, Conway AA, Frieder JE. Ethical considerations for interdisciplinary collaboration with prescribing professionals. Behavior Analysis in Practice. 2017;10(2):145–153. doi: 10.1007/s40617-017-0184-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel MR, Piazza CC, Kelly ML, Ochsner CA, Santana CM. Using a fading procedure to increase fluid consumption in a child with feeding problems. Journal of Applied Behavior Analysis. 2001;34(3):357–360. doi: 10.1901/jaba.2001.34-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel MR, Piazza CC, Santana CM, Volkert VM. An evaluation of food type and texture in the treatment of a feeding problem. Journal of Applied Behavior Analysis. 2002;35(2):183–186. doi: 10.1901/jaba.2002.35-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson KM, Piazza CC, Volkert VM. A comparison of a modified sequential oral sensory approach to an applied behavior-analytic approach in the treatment of food selectivity in children with autism spectrum disorder. Journal of Applied Behavior Analysis. 2016;49(3):485–511. doi: 10.1002/jaba.332. [DOI] [PubMed] [Google Scholar]
- Piazza CC, Fisher WW, Brown KA, Shore BA, Patel MR, Katz RM, Sevin BM, Gulotta CS, Blakely-Smith A. Functional analysis of inappropriate mealtime behaviors. Journal of Applied Behavior Analysis. 2003;36(2):187–204. doi: 10.1901/jaba.2003.36-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed GK, Piazza CC, Patel MR, Layer SA, Bachmeyer MH, Bethke SA, Gutshall KA. On the relative contributions of noncontingent reinforcement and escape extinction in the treatment of food refusal. Journal of Applied Behavior Analysis. 2004;37(1):27–42. doi: 10.1901/jaba.2004.37-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreck KA, Williams K, Smith AF. A comparison of eating behaviors between children with and without autism. Journal of Autism and Developmental Disorders. 2004;34(4):433–438. doi: 10.1023/b:jadd.0000037419.78531.86. [DOI] [PubMed] [Google Scholar]
- Seiverling L, Anderson K, Rogan C, Alaimo C, Argott P, Panora J. A comparison of behavioral feeding intervention with and without pre-meal sensory integration therapy. Journal of Autism and Developmental Disorders. 2018;48:3344–3353. doi: 10.1007/s10803-018-3604-z. [DOI] [PubMed] [Google Scholar]
- Sharp WG, Jaquess DL, Morton JF, Herzinger CV. Pediatric feeding disorders: A quantitative synthesis of treatment outcomes. Clinical Child and Family Psychology Review. 2010;13(4):348–365. doi: 10.1007/s10567-010-0079-7. [DOI] [PubMed] [Google Scholar]
- Silbaugh, B. C., & Swinnea, S. (2018). Failure to replicate the effects of the high-probability instructional sequence on feeding in children with autism and food selectivity. Behavior Modification. Advance online publication.10.1177/0145445518785111. [DOI] [PubMed]
- Tarbox J, Schiff A, Najdowski AC. Parent-implemented procedural modification of escape extinction in the treatment of food selectivity in a young child with autism. Education and Treatment of Children. 2010;33(3):223–234. doi: 10.1353/etc.0.0089. [DOI] [Google Scholar]
- Thomas S, Lycette K, Papadopoulos N, Sciberras E, Rinehart N. Exploring behavioral sleep problems in children with ADHD and comorbid autism spectrum disorder. Journal of Attention Disorders. 2018;22(10):947–958. doi: 10.1177/1087054715613439. [DOI] [PubMed] [Google Scholar]
- Vollmer, T. R., & Athens, E. (2011). Developing function-based extinction procedures for problem behavior. In W. W. Fisher, C. C. Piazza, & H. S. Roane (Eds.), Handbook of applied behavior analysis (pp. 151–164). The Gilford Press.
- Weber, J., & Gutierrez, A. (2015). A treatment package without escape extinction to address food selectivity. Journal of Visualized Experiments, (102), e52898. 10.3791/52898. [DOI] [PMC free article] [PubMed]
- Williams, K. E., & Foxx, R. (2007). Treating eating problems of children with autism spectrum disorders and developmental disabilities. Pro-Ed.
- Williams, K. E., & Seiverling, L. (2018). Broccoli boot camp. Woodbine House.