Abstract
Background
The main purpose of this study is to assess the compatibility of medial tibial condyle (MTC) morphometry of Indian population with that of six contemporary UKA prostheses tibial components. We hypothesized that from the currently available UKA designs at least one would fit the MTC morphometry optimally as per the manufacturer’s recommendation.
Methods
We used CT morphometric data of 100 (66 males and 34 females) consecutive nonarthritic adult knees with reference to the MTC to assess the compatibility of currently available (in India) UKA prostheses. Each MTC was measured in the anteroposterior dimension, mediolateral at pre-defined points and the MTC aspect ratio calculated. Proportion of knees which could be optimally fitted with the existing UKA tibial components was calculated.
Results
The mean age was 39.6 (SD 15.9) years. Anteroposterior and mediolateral dimensions in males were higher as compared to females (p < 0.001). As the anteroposterior dimension increased, the MTC aspect ratio decreased. There was asymmetry of anteroposterior halves with maximum mediolateral width being posterior to the central mediolateral width by 5.5 (SD 2.8) mm. Optimal anteroposterior fit ranged from 66 to 93%. However, optimal mediolateral fit as well, ranged from 5 to 37% with underhang present in 17–61% and > 2 mm medial overhang present in 0–35% cases. In 23% of cases, not a single implant could be fitted optimally.
Conclusion
Currently available UKA implants do not provide optimal tibial fit in nearly 25% of Indian patients. A surgeon needs to be aware of these limitations of existing implants when considering UKA.
Keywords: Unicompartmental knee arthroplasty, Medial tibial condyle, CT morphometry, Indian knees, Implant size and shape mismatch
Introduction
For optimal UKA results, selection of an appropriately sized tibial component is essential. Majority of the complications post-UKA are related to the tibia due to (a) faulty surgical technique leading to valgus subsidence with increased posterior slope [1], overhang causing soft tissue irritation and pain whereas underhang leading to loosening with subsidence [2], tibial plateau fracture secondary to anything that weakens or overloads the proximal tibia [3] or (b) suboptimal component fit leading to similar issues of pain, fracture, loosening and subsidence [4, 5]. Indeed, the reported variability in the clinical outcomes and implant survival with UKA [6, 7] is higher than that with TKA. This has contributed to UKA usage being restricted to around 10% [6, 7] although UKA can be used in up to 50% of cases presenting with end-stage symptomatic osteoarthritis [8]. Optimal coverage of cortical bone in particular the tibia is relevant especially in UKA cases. This provides adequate support and reduces the risk of implant subsidence.
Various studies across the globe have uncovered the differences in morphologic features of the knee among patients of different races [9–11], between male:female gender [12], between medial:lateral condyles [13] and between anatomic:non-anatomic tibial component designs [14] in context of different designs of total knee arthroplasty prostheses. Studies have also been conducted in Indian subjects [15, 16] to draw attention to the differences between their morphometry and the resultant mismatch with contemporary TKA prostheses designs. However, studies with respect to UKA prostheses designs are lacking with reference to the tibial components [17].
The primary objective of this study is to assess the compatibility of medial tibial condylar morphometry of Indian population with that of six contemporary UKA prostheses tibial components. We aimed to answer these following questions: (1) What percentage of knees had at least one implant which could fit optimally? (2) Was there a difference in the percentage of optimal fit cases in men vs. women?
Methods
Institutional ethics committee (IRB) approval for study protocol and waiver of informed consent was taken (Project no. EC/173/2018). We studied computed tomography (CT) data of 100 skeletally mature Indian knees. These patients had undergone CT scan of their knee for various clinical indications excluding pathologies which could alter the morphometry of Medial tibial condyle, i.e., fractures, neoplasia, congenital anomalies, old physeal injuries, arthritis. The medial tibial condyle dimensions were measured by a single surgeon using RadiAnt™ DICOM (Digital Imaging and Communications in Medicine) viewer software for Windows (Version—5.5.0, Poznan, Poland).
Steps for Morphometric Measurements of the Medial Tibial Condyle
In coronal plane, an axis was drawn on the tibial plateau which was equidistant from medial and lateral epicondyles of femur (with reference to femoral epicondylar axis) (Fig. 1). In sagittal plane, an axis was drawn which was 6 mm below the medial tibial plateau and 90° to the long axis of tibia. Another axis was drawn which was 7° posterior to the above-mentioned axis, mimicking the conservative resection of tibia for doing UKA (Fig. 2). These simulated cuts were chosen as per the manufacturers’ recommendations to accommodate minimum thickness of polyethylene bearing. The axial section obtained through above-mentioned planes was used for further measurements of different dimensions (Fig. 3). A line drawn in the plane which was equidistant from medial and lateral epicondyles of femur over the tibia, and this was designated as ML. A bisector line was drawn to the line ML, this was considered as Y. In an attempt to align the tibial component with the femoral mechanical axis, a line X was drawn medially and subtending an angle of 6 degrees anteriorly to the line Y [18]. In a bid to prevent damaging the ACL footprint on tibia, a line AP was drawn side by side to line X medially with 3 mm apart from each other. The AP line was divided into four equal parts and perpendicular lines were drawn from the points dividing AP line anteroposteriorly into ¼th and ¾th, ½ and ½, ¾th and ¼th, these lines were designated as D (25%), B (50%) and C (75%), respectively. The line A measures the widest dimension of the medial tibial condyle and ab is the distance between the lines A and B. It was also recorded if line A is anterior or posterior to line B (Fig. 4). The medial tibial condyle aspect ratio was computed from the formula A/AP × 100 [19].
Fig. 1.

Coronal CT showing axis parallel and collinear to the clinical epicondylar axis of femur mediolaterally
Fig. 2.

Sagittal CT showing axis passing through upper tibial cut of 6 mm thickness, perpendicular to the mechanical axis of the tibia with 7° posterior slope
Fig. 3.

Axial section obtained for measurements of different dimensions
Fig. 4.
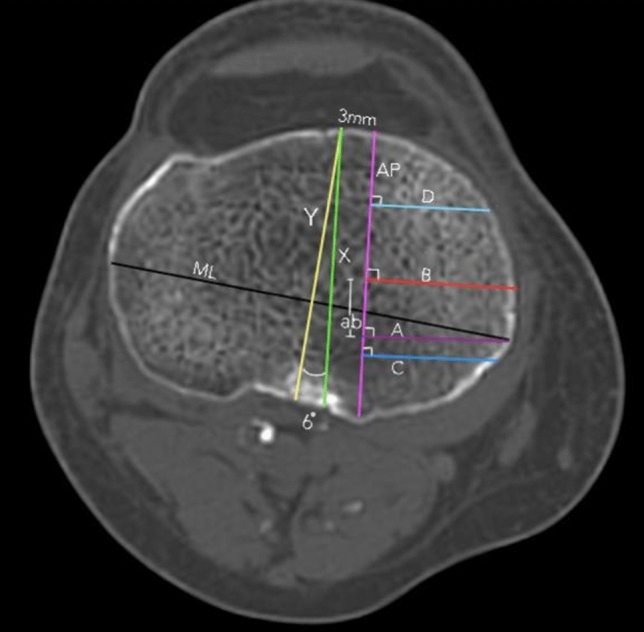
Anteroposterior and mediolateral dimensions at well-defined points
Different sizes of the currently available (in Indian market) UKA tibial component are as shown in Table 1 (in cm).
Table 1.
Measurements of anteroposterior (AP), mediolateral (ML) dimensions (in cm), medial tibial condylar aspect ratio (in percentage) of six UKA tibial components
| Size 1 | Size 2 | Size 3 | Size 4 | Size 5 | Size 6 | |
|---|---|---|---|---|---|---|
| AP–ML (ratio%) | AP–ML (ratio%) | AP–ML (ratio%) | AP–ML (ratio%) | AP–ML (ratio%) | AP–ML (ratio%) | |
| [1] Stryker Triathlon | 4.1–2.3 (56) | 4.4–2.5 (57) | 4.7–2.7 (57) | 5.0–2.9 (58) | 5.3–3.1 (58) | 5.6–3.3 (59) |
| [2] Depuy sigma high-performance partial knee system | 4.2–2.4 (57) | 4.5–2.6 (58) | 4.8–2.8 (58) | 5.1–3.0 (59) | 5.4–3.2 (59) | 5.7–3.4 (60) |
| [3] Smith and Nephew Journey | 3.8–2.4 (63) | 4.2–2.5 (60) | 4.6–2.7 (59) | 4.9–2.9 (59) | 5.2–3.0 (58) | 5.5–3.2 (58) |
| [4] Zimmer Biomet Oxford | 3.8–2.6 (68) | 4.1- 2.6 (63) | 4.4- 2.8 (64) | 4.7– 3.0 (64) | 5–3.2 (64) | 5.3–3.4 (64) |
| [5] Link Sled prosthesis—all poly | 4.5–2.2 (49) | 5.0–2.7 (54) | .5–2.9 (53) | 5.8–3.1 (53) | ||
| [6] Link Sled prosthesis—metal backed | 4.5–2.25 (50) | 5.0–2.5 (50) | 5.5–2.75 (50) |
Optimal fit is defined as anterior fit: flush or < 3 mm overhang, posterior fit: flush or < 2 mm overhang, medial fit: flush or ≤ 2 mm and lateral fit—flush, no gap [20].
Statistical analysis was performed using Student’s Independent t test and Pearson’s correlation using SPSS software for Windows (Version 20.0, SPSS, Chicago, IL, USA). A p value of < 0.05 was considered significant. Pearson’s correlation coefficient was represented as r.
Results
The mean age of the cohort was 39.6 (SD 15.9, range 20–70 years) and included 66 male and 34 female subjects. Average mediolateral (A) and anteroposterior (AP) dimensions were significantly higher among males when compared with females (p < 0.001) (Table 2).
Table 2.
Measurements of the various dimensions of the study subjects
| Measurements (in cm) | Female | Male | Total | p value | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| AP | 4.33 | 0.36 | 4.85 | 0.55 | 4.68 | 0.55 | < 0.001 |
| A | 2.54 | 0.28 | 2.97 | 0.38 | 2.82 | 0.40 | < 0.001 |
| B-50% | 2.48 | 0.27 | 2.98 | 0.30 | 2.81 | 0.37 | < 0.001 |
| C-75% | 2.41 | 0.22 | 2.84 | 0.34 | 2.69 | 0.36 | < 0.001 |
| D-25% | 1.98 | 0.34 | 2.32 | 0.32 | 2.20 | 0.37 | < 0.001 |
| AB | 0.55 | 0.30 | 0.55 | 0.26 | 0.55 | 0.28 | 0.9123 |
| Aspect ratio | 58.81 | 5.62 | 61.22 | 5.54 | 60.40 | 5.66 | 0.0441 |
Mediolateral Dimensions [A, B (50%), C (75%) and D (25%)]
The line A was posterior to the line B (50%) in all the study subjects irrespective of gender. The average distance between line A and B, i.e., ab was 5.5 ± 2.6 mm and 5.5 ± 3.0 in males and females, respectively [Table 2].
Comparison of the Optimal Anteroposterior and Mediolateral Fit of UKA Tibial Components
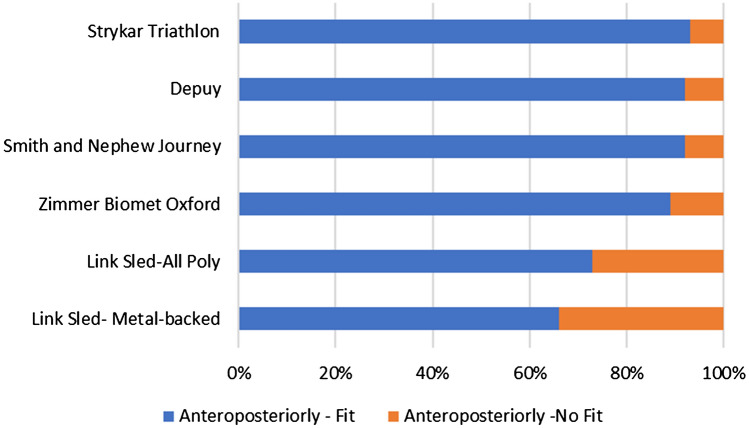
With the contemporary UKA tibial components, optimal anteroposterior fit (Anterior fit—flush or < 3 mm overhang, posterior fit—flush or < 2 mm overhang) ranged from 66% (Link Sled prosthesis—metal backed) to 93% (Stryker Triathlon). Among those with optimal anteroposterior fit, those with optimal mediolateral fit (Medial fit—flush to ≤ 2 mm overhang, lateral fit—flush, no gap) ranged from 5% (link sled prosthesis—metal backed) to 37% (Zimmer Biomet Oxford). Overall, out of 100 knees, only 77 knees could have at least one implant which could provide an optimal anteroposterior and mediolateral fit. The underhang was estimated to be from 17% (Biomet Oxford) to 61% (Link Sled prosthesis—all poly) and > 2 mm medial overhang ranged from 0 (Link Sled prosthesis—all poly) to 35% (Zimmer Biomet Oxford) (Figs. 5, 6).
Fig. 5.
Chart comparing optimal anteroposterior fit or no fit (in percentage) of UKA tibial components with respect to morphometric data
Fig. 6.
Chart comparing optimal anteroposterior fit and optimal mediolateral fit, underhang or > 2 mm overhang (in percentage) of UKA tibial components with respect to morphometric data
The optimal fit (both AP and ML), in males ranged from 7.6% (Link Sled—metal back) to 34.8% (Zimmer Biomet Oxford) whereas in females ranged from 0% (Link Sled—metal back) to 55.9% (Smith and Nephew Journey) (Fig. 7).
Fig. 7.
Chart comparing the Optimal fit (both anteroposteriorly and mediolaterally) of UKA tibial components in male and female subjects
Comparison of the Medial Tibial Condyle Aspect Ratio (A/AP × 100 in %) of Morphometric Data with that of UKA Tibial Components
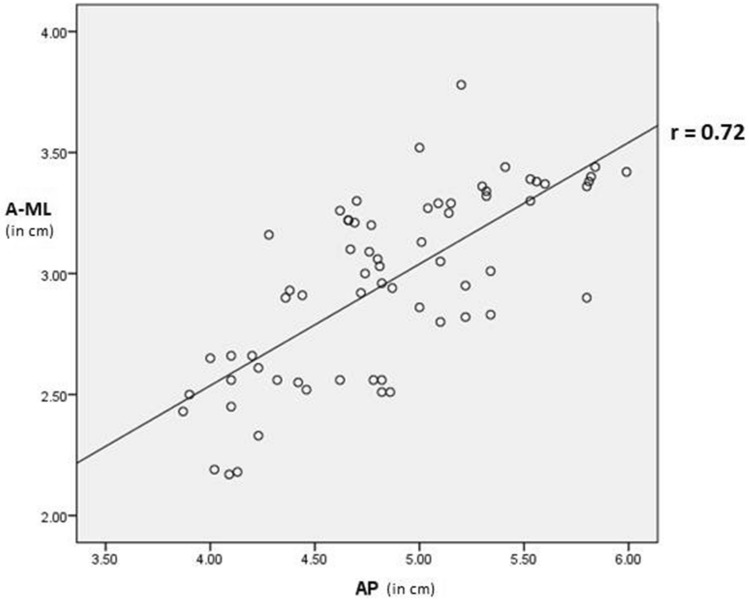
Although there was positive correlation between anteroposterior and mediolateral dimensions (Figs. 8, 9), we found that the morphometric data showed a progressive decline in the medial tibial condyle aspect ratio (A/AP × 100) as the AP dimension increased in all the study subjects.
Fig. 8.
Scatter plot of anteroposterior against mediolateral dimensions (in cm) of male subjects. Coefficient of correlation is 0.72 (r > 0.7), suggestive of high positive correlation between the two dimensions
Fig. 9.
Scatter plot of anteroposterior against mediolateral dimensions (in cm) of female subjects. Coefficient of correlation is 0.57 (r > 0.5), suggestive of moderate positive correlation between the two dimensions
Discussion
This study highlights the limitations in optimal tibial component sizes for UKA when used in Indian patients. Not a single implant could have been used with optimal fit in around one in four cases. In addition, out of the six implants studied, on an average no more than two implants could fit optimally for a patient when the optimal fit was possible.
The long-term survival results of UKA are encouraging [21] with designer surgeons reporting 98% survival at 10 years [22, 23]. This procedure also provides quicker functional recovery, an improved range of motion, and is more cost-effective than TKA [24]. The success of UKA relies on the surgical technique, the post-operative physiotherapy and the design of prosthesis [25, 26]. The match between resected surface of tibia and the tibial component is crucial. In TKA, if there is a smaller size component on tibial side, there will be inadequate support by the cortical rim and the implant can subside and loosen [27]. If it is too large, the overhang will cause soft tissue irritation and pain. The amount of cortical rim support in UKA is less than half of that available for TKA. Matching the shape and size of the implant to the resected surface is crucial especially in UKA to ensure optimal load transfer and this is particularly the case for tibial implant as majority of mechanical complications with UKA are tibia related. Although one can ascertain the best size that can fit a resected tibial plateau using tibial baseplate templates intra-operatively, by that time the surgeon has committed to using a particular company’s implant for that particular case. It is difficult to intra-operatively change to use of another company’s implant. Preoperative CT scans are not routinely performed in patients undergoing UKA. It is, therefore, difficult if not impossible to predict actual tibial size and shape at the site of desired resection without the aid of a cross-sectional imaging and this can lead to intra- and/or post-operative complications.
Most of the UKA implants are designed based on anthropometric measurements of Caucasian population. As compared with the western population, Indians have smaller built and shorter stature [15]. There is lack of literature on the fit of different designs of the tibial component for UKA, based on the morphometry of medial tibial condyle in the Indian population. The shape of the components is as critical as the anteroposterior and mediolateral dimensions to match the resected surface. The tibial component rotation was matched to that of femur component using epicondylar axis of femur as reference while measuring the length of mediolateral dimension [28]. The assessment of shape of medial tibial condyle was done by measuring mediolateral dimensions at four different points as described by Surendran et al. [18].
The widest part in mediolateral plane was present in the posterior half of the medial tibial condyle and the mediolateral width measured in posterior half was more than the one measured in anterior half of the medial tibial condyle in all the study subjects. This supports the hypothesis by Surendran et al. [18] that long hours of flexion attitude of knees during various activities of daily routine might create more stress on posterior half of the condyles. This higher stress, as per Wolff’s law stimulates hypertrophy in mediolateral dimension in the posterior half of tibial condyles in Indian population. This suggests asymmetry in the anterior and posterior halves of the medial tibial condyles. Hence, the design having an anteroposterior asymmetry with the widest mediolateral width present in the posterior half of the tibial component is suitable for our population.
Our results are similar to studies carried out in other non-Caucasian populations. Cheng et al. assessed the tibial fit in Chinese population for five different UKA implant designs [29]. The authors analyzed 3D-CT of 172 normal knees obtained from 94 males and 78 females. They concluded that the majority of the prostheses currently employed in China showed a tendency toward over sizing in the widest dimension of the tibia. Surendran et al. conducted a similar study in the Korean population [18]. They assessed 50 male and 50 female Korean 200 cadaveric knees using 3D-CT and examined tibial fit for 5 different UKA designs. The authors noticed the tendency toward mediolateral overhang. Another author Koh et al., assessed the misfit of existing UKA designs in Korean population [30]. The author concluded that frequency of having smaller medial tibial condylar dimensions were more in women than in men and there was mediolateral overhang in three out of five prostheses in the medial tibial condyles, leading to a mediolateral overhang when trying to optimize the AP coverage. A decrease in the medial tibial condyle aspect ratio with an increasing AP dimension was found for both the male and female population. Lastly Küçükdurmaz et al. assessed knee MRIs of 260 Turkish patients (150 women and 110 men) to establish the fit for four different UKA designs [31]. The authors concluded that there are significant differences between the anthropometric measurements of Turkish tibiae when compared with Western population. All these above-mentioned studies used tibial resection level same as used in the current study (6 mm below the upper MTC) and reached similar conclusions to the current study in Indian population.
The strengths of this study include use of CT scan data for precision, making sure that soft tissues did not interfere in measurements. None of the patients suffered from knee arthritis or any other pathology which could potentially have affected the size and shape of proximal tibia. The limitations of our study included smaller sample size, height of the patient was not recorded so the correlation of height and morphometry of MTC could not be opined, measurement of MTC morphometry only at one level (6 mm below articular surface) and using guidance from one manufacturer (Zimmer Biomet) only to define radiological criteria for optimal fit [20]. No other manufacturer guidance to define radiological criteria for optimal fit of that particular prostheses design was available in the public domain. We measured the dimensions of the medial tibial condyle at 6 mm below the articular surface with 7° posterior slope. This is a conservative tibial resection, and therefore, is likely to be the best-case scenario. If indeed, the tibial cut is more distal, the bone shape and dimensions will vary further and make it more difficult to fit even the smallest tibial component without a risk of posterior cortical blow out or significant anterior and/or medial overhang. Further studies are recommended to analyze morphometric data at different levels of cutting thickness and angles of slope.
Conclusions
Currently available UKA implants do not provide optimal tibial fit in nearly 25% of Indian patients. A surgeon needs to be aware of these limitations of existing implants when considering UKA.
Acknowledgements
This paper presents independent research supported by the National Institute for Health Research (NIHR) Leeds Biomedical Research Centre (BRC). Professor Pandit is a NIHR Senior Investigator. The views expressed in this article are those of the author(s) and not necessarily those of the NIHR, or the Department of Health and Social Care.
Funding
No funds, grants, or other support was received.
Availability of Data and Material
The data generated during and analyzed during the current study are available from the corresponding author on request.
Declarations
Conflict of Interest
The author C reports grants and personal fees from Zimmer Biomet, personal fees from Smith and Nephew, grants and personal fees from Depuy Synthes, personal fees from Medacta International, personal fees from Meril Life, grants from Invibio, grants and personal fees from GSK, personal fees from JRI, outside the submitted work.
Ethical Standard Statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liddle AD, Pandit HG, Jenkins C, et al. Valgus subsidence of the tibial component in cementless Oxford unicompartmental knee replacement. Bone Joint Journal. 2014;96-B(3):345–349. doi: 10.1302/0301-620X.96B3.33182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chau R, Gulati A, Pandit H, et al. Component overhang and unicompartmental knee replacement—does it matter? The Knee. 2009;16–5:310–313. doi: 10.1016/j.knee.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 3.Pandit H, Murray DW, Dodd CA, et al. Medial tibial plateau fracture and the Oxford unicompartmental knee. Orthopaedics. 2007;30(5 Suppl):28–31. [PubMed] [Google Scholar]
- 4.Ali AM, Newman SDS, Hooper PA, Davies CM, Cobb JB. The effect of implant position on bone strain following lateral unicompartmental knee arthroplasty. A Biomechanical Model Using Digital Image Correlation. Bone & Joint Research. 2017;6(8):522–529. doi: 10.1302/2046-3758.68.BJR-2017-0067.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pegg EC, Walter J, Mellon SJ, Pandit HG, et al. Evaluation of factors affecting tibial bone strain after unicompartmental knee replacement. Journal of Orthopaedic Research. 2013;31(5):821–828. doi: 10.1002/jor.22283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liddle AD, Judge A, Pandit H, Murray DW. Determinants of revision and functional outcome following unicompartmental knee replacement. Osteoarthritis Cartilage. 2014;22(9):1241–1250. doi: 10.1016/j.joca.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murray DW, Liddle AD, Dodd CA, Pandit H. Unicompartmental knee arthroplasty: is the glass half full or half empty? The Bone & Joint Journal. 2015;97-B(12):1732. doi: 10.1302/0301-620X.97B7.37439e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamilton TW, Rizkalla JM, Kontochristos L, et al. The interaction of caseload and usage in determining outcomes of unicompartmental knee arthroplasty: a meta-analysis. Journal of Arthroplasty. 2017;32(10):3228–3237.e2. doi: 10.1016/j.arth.2017.04.063. [DOI] [PubMed] [Google Scholar]
- 9.Kim TK, Phillips M, Bhandari M, Watson J, Malhotra R. What differences in morphologic features of the knee exist among patients of various races? A systematic review. Clinical Orthopaedics and Related Research. 2017;475(1):170–182. doi: 10.1007/s11999-016-5097-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma Q-L, Lipman JD, Cheng CK, Wang XN, Zhang YY, You B. A comparison between Chinese and Caucasian 3-dimensional bony morphometry in presimulated and postsimulated osteotomy for total knee arthroplasty. Journal of Arthroplasty. 2017;32(9):2878–2886. doi: 10.1016/j.arth.2017.03.069. [DOI] [PubMed] [Google Scholar]
- 11.Gurava Reddy AV, Sankineani SR, Agrawal R, Thayi C. Comparative study of existing knee prosthesis with anthropometry of Indian patients and other races, a computer tomography 3D reconstruction-based study. Journal of Clinical Orthopaedics and Trauma. 2020;11(Suppl 2):S228–S233. doi: 10.1016/j.jcot.2019.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kwak DS, Surendran S, Pengatteeri YH, et al. Morphometry of the proximal tibia to design the tibial component of total knee arthroplasty for the Korean population. The Knee. 2007;14(4):295–300. doi: 10.1016/j.knee.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Meier M, Zingde S, Best R, Schroeder L, Beckmann J, Steinert AF. High variability of proximal tibial asymmetry and slope: A CT data analysis of 15,807 osteoarthritic knees before TKA. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28(4):1105–1112. doi: 10.1007/s00167-019-05728-4. [DOI] [PubMed] [Google Scholar]
- 14.Dai Y, Scuderi GR, Bischoff JE, Bertin K, Tarabichi S, Rajgopal A. Anatomic tibial component design can increase tibial coverage and rotational alignment accuracy: A comparison of six contemporary designs. Knee Surgery, Sports Traumatology, Arthroscopy. 2014;22(12):2911–2923. doi: 10.1007/s00167-014-3282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaidya SV, Ranawat CS, Aroojis A, Laud NS. Anthropometric measurements to design total knee prostheses for the Indian population. Journal of Arthroplasty. 2000;15:79–85. doi: 10.1016/S0883-5403(00)91285-3. [DOI] [PubMed] [Google Scholar]
- 16.Gandhi S, Singla RK, Kullar JS, Suri RK, Mehta V. Morphometric analysis of upper end of tibia. Journal of Clinical and Diagnostic Research. 2014;8(8):AC10–AC13. doi: 10.7860/JCDR/2014/8973.4736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malhotra R, Gaba S, Wahal N, Kumar V, Srivastava DN, Pandit H. Femoral component sizing in oxford unicompartmental knee replacement: existing guidelines do not work for Indian patients. The Journal of Knee Surgery. 2019;32(3):205–210. doi: 10.1055/s-0038-1635113. [DOI] [PubMed] [Google Scholar]
- 18.Surendran S, Kwak DS, Lee UY, Park SE, Gopinathan P, Han SH, Han CW. Anthropometry of the medial tibial condyle to design the tibial component for unicondylar knee arthroplasty for the Korean population. Knee Surgery, Sports Traumatology, Arthroscopy. 2007;15:436–442. doi: 10.1007/s00167-006-0188-5. [DOI] [PubMed] [Google Scholar]
- 19.Hitt K, Shurman JR, II, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. The Journal of Bone and Joint Surgery. 2003;85:115122. doi: 10.2106/00004623-200300004-00015. [DOI] [PubMed] [Google Scholar]
- 20.Murray, D.W., et al. (1999). Oxford Unicompartmental knee: manual of the surgical technique (Biomet UK Ltd. Bridgend, pp. 1–40).
- 21.Deshmukh RV, Scott RD. Unicompartmental knee arthroplasty: long-term results. Clinical Orthopaedics and Related Research. 2001;392:272–278. doi: 10.1097/00003086-200111000-00035. [DOI] [PubMed] [Google Scholar]
- 22.Berger RA, Nedeff DD, Barden RM, Sheinkop MM, Jacobs JJ, Rosenberg AG, Galante JO. Unicompartmental knee arthroplasty: Clinical experience at 6- to 10-year followup. Clinical Orthopaedics. 1999;367:50–60. doi: 10.1097/00003086-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Murray DW, Goodfellow JW, O’Connor JJ. The oxford medial unicompartmental arthroplasty: a ten-year survival study. Journal of Bone and Joint Surgery. British Volume. 1998;80:983–989. doi: 10.1302/0301-620X.80B6.0800983. [DOI] [PubMed] [Google Scholar]
- 24.Carr A, Keyes G, Miller R, O’Connor J, Goodfellow J. Medial unicompartmental arthroplasty: a survival study of the Oxford meniscal knee. Clinical Orthopaedics. 1993;295:205–213. [PubMed] [Google Scholar]
- 25.NIH Consensus Statement on total knee replacement. (2003). NIH Consensus State Science Statements, vol. 20 (pp. 1–34). [PubMed]
- 26.Choong PF, Dowsey MM. Update in surgery for osteoarthritis of the knee. International Journal of Rheumatic Diseases. 2011;14:167–174. doi: 10.1111/j.1756-185X.2011.01617.x. [DOI] [PubMed] [Google Scholar]
- 27.Nielsen PT, Hansen EB, Rechnagel K. Cementless total knee arthroplasty in unselected cases of osteoarthritis and rheumatoid arthritis: a 3-year follow-up study of 103 cases. The Journal of Arthroplasty. 1992;7:137–143. doi: 10.1016/0883-5403(92)90006-C. [DOI] [PubMed] [Google Scholar]
- 28.Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y. Anthropometry of the proximal tibia to design a total knee prosthesis for the Japanese population. The Journal of Arthroplasty. 2002;17:1028–1032. doi: 10.1054/arth.2002.35790. [DOI] [PubMed] [Google Scholar]
- 29.Cheng FB, Ji XF, Zheng WX, Lai Y, Cheng KL, Feng JC, Li YQ. Use of anthropometric data from the medial tibial and femoral condyles to design unicondylar knee prostheses in the Chinese population. Knee Surgery, Sports Traumatology, Arthroscopy. 2010;18(3):352–358. doi: 10.1007/s00167-009-0876-z. [DOI] [PubMed] [Google Scholar]
- 30.Koh YG, Nam JH, Chung HS, Lee HY, Kang KT. Morphologic difference and size mismatch in the medial and lateral tibial condyles exist with respect to gender for unicompartmental knee arthroplasty in the Korean population. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28(6):1789–1796. doi: 10.1007/s00167-019-05600-5. [DOI] [PubMed] [Google Scholar]
- 31.Küçükdurmaz F, Tuncay I, Elmadağ M, Tunçer N. Morphometry of the medial tibial plateau in Turkish knees: correlation to the current tibial components of unicompartmental knee arthroplasty. Acta Orthopaedica et Traumatologica Turcica. 2014;48(2):147–151. doi: 10.3944/AOTT.2014.3006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated during and analyzed during the current study are available from the corresponding author on request.