Abstract
Purpose
Total knee arthroplasty (TKA) has improved leaps and bounds in terms of design to improve clinical outcomes and achieve better rehabilitation of the patients. Ultra-congruent inserts (UC) were designed to replace the need for posterior stabilized (PS) implants. The purpose of this review was to evaluate clinical outcomes, femoral rollback, functional scores, range of motion, sagittal laxity, complication rates, and isokinetic performance between UC and PS TKA among RCTs
Methods
Electronic databases such as PubMed, Scopus, opengrey, and Cochrane were searched from date of inception up to mid-April 2021, and meta-analysis was performed following PRISMA guidelines. This study analyzed outcomes, femoral rollback, tibial sagittal laxity and isokinetic performance.
Results
Ten RCTs identified 852 knees, of which 420 underwent UC TKAs and 432 underwent PS TKA. Compared to UC TKA, a significantly better sagittal stability (p = 0.17) and femoral rollback (p < 0.00001) in PS TKAs was noted, although no statistically significant difference was found in the assessment of the range of motion (p = 0.19) and functional scores. Both the groups had similar isokinetic performance with extensor torque (p = 0.97) and flexor torque (p = 0.37).
Conclusions
We conclude with the current meta-analysis that there are no added benefits for UC over PS inserts and these inserts have a higher sagittal laxity and less femoral roll back in cruciate sacrificing UC knee. But since there are no long-term wear data, UC inserts with CS technique should be used cautiously and may be used only when the PCL cannot be balanced adequately. There is no evidence or only a few to support the superiority of the AS TKA in terms of clinical outcomes or isokinetic performance or femoral external rotation over PS TKA.
Level of Evidence
Level I, Systematic review and meta-analysis of RCTs.
Keywords: Total knee arthroplasty, Ultra-congruent, Posterior stabilized, Functional joint scores, Isokinetic performance, Sagittal stability, Femoral rollback
Introduction
Total knee arthroplasty (TKA) over the decades has seen significant improvements and additions which helped to increase patient-reported outcomes. The newer models of TKA are introduced by multiple manufacturers in the market claiming to provide superior results to the other. Most of these varieties differ among themselves in the amount of bone resection or constraint offered or biomechanical superiority in vitro [1, 2].
The significance of posterior cruciate ligament (PCL) in TKA is well studied, but the debate on whether to retain PCL or to sacrifice it still exists. PCL helps in the posterior rollback of the femur in native knees, aids in proprioception and promotes normal knee kinematics [3, 4]. The proponents of the posterior stabilized (PS) knee implants stem from the idea of improved knee function with femoral rollback and anteroposterior stability if it is substituted with a cam and post. But the design has its unique complications such as post-cam wear, dislocation, and patellar clunk syndrome [5, 6]. The proponents of the CR or cruciate retaining prosthesis stems from the idea of retaining the PCL to preserve the bone stock, decrease the complications of post-cam articulation, and recreate femoral rollback [7]. The specific complications of the post-cam had made the manufacturers look for a more suitable prosthesis that would require less bone resection and have a lesser complication rate [6, 8]. The novel polyethylene inserts design such as anterior-stabilized bearings (AS) or ultra-congruent (UC) bearings was proposed as an alternative to the PS design allowing the surgeons to sacrifice PCL and use a CR femoral component using a congruent insert in a sagittal plane with an elevated anterior and posterior lip [9–12]. Ritter et al. noted that if the PCL is detached at the time of operation, conversion to a posterior-stabilized prosthesis may not be necessarily required as long as stability in the anteroposterior and coronal planes is achieved [3].
In the literature, there exists few noteworthy quality evidence on these implant models with regards to their intraoperative or in vivo kinematics or clinical outcomes in comparison to the PS knees. The potential concerns with UC inserts include abnormal anterior translation, increased patellofemoral peak pressure, and increased wear [13, 14]. The literature at present regarding the AS/UC implants has only one recent meta-analysis which has compared the PS and AS TKA [14]. This study included six retrospective studies along with seven prospective. Several RCTs have been published only recently and are not included in the previous review [15–19]. This meta-analysis aimed to compare the clinical outcomes, femoral rollback, anteroposterior stability, range of motion, complication rates, and isokinetic performance between UC and PS TKA among RCTs.
Materials and Methods
The current systematic review and meta-analysis was performed following PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [20].
Literature Search and Study Selection
The search was conducted in the online databases PubMed, Scopus, CENTRAL (Cochrane Central Register of Controlled Trials), opengrey, Lilacs and clinicaltrials.gov by the authors B.S.R and A.K.S.G. All three databases were searched from the date of inception until 15th April 2021. Unpublished or ongoing studies were searched in the System for Information on Grey Literature in Europe (www.opengrey.eu) and clinicaltrials.gov, respectively. The search was done with multiple search terms: “ultra-congruent”, “UC”, “anterior stabilized”, “cruciate substituting”, “cruciate stabilized”, “deep dished”, “total knee replacement”, “kinematics”, “stability”, “laxity”, “clinical outcome”, “function score” with Boolean operators “AND” and “OR”. The search flow diagram is depicted in Fig. 1. The first step was to identify the abstracts by the above-mentioned search methods following which they were screened and assessed for eligibility based on the criteria mentioned below. The full texts of the shortlisted abstracts were downloaded and reassessed for eligibility based on the predefined inclusion criteria. In addition, the reference lists of the shortlisted full texts were searched for relevant studies. The above process was repeated two times and any disagreement between the authors was sorted out by senior author R.B.K.
Fig. 1.
PRISMA flowchart
Eligibility Criteria
The review included all original studies which (1) compared functional outcomes of AS or UC TKA versus PS TKA using at least one outcome measures (complication rates, range of motion, patient-reported outcome measures: Knee Society Score (KSS), International Knee Society (IKS) Score, American Knee Society (AKS) Score, Oxford Knee Score (OKS), and Hospital for Special Surgery (HSS) Knee Score and Forgotten joint score (FJS), sagittal stability, femoral rollback, isokinetic performance; (2) were randomized controlled trials; and (3) were available in the English language.
The exclusion criteria included (1) articles with incomplete data; (2) case reports, reviews, biomechanical studies, expert opinions, letters to editor or editorials; (3) non-English language.
Data Extraction and Statistical Analysis
The data were extracted from the selected articles by two separate reviewers (AKC and SA) using a standardized form. The following data were extracted: author name, year of publication, journal, study location, design of study, level of evidence, sample size, follow-up period, and various functional outcome measures (mean and standard deviation) including complication rates as dichotomous variables were extracted. The authors of the studies were contacted if any missing data were found to request the specific information needed and if we were unable to contact the authors, or did not receive a response from them, the study data were excluded from the analysis. Any disagreements between the authors were sorted by the senior author (RBK).
The meta-analysis was conducted using the statistical software RevMan version 5.3. Q statistic distributed as Chi-square variate under the assumption of homogeneity of effect sizes was used for tests of heterogeneity. The heterogeneity of the sample was assessed with the I2 statistic with values of 25, 50, and 75% considered as low, moderate, and high heterogeneity, respectively [21]. The pooled estimates were assessed using the Random-effects model, as this model assumes that the included studies represent a random sample from the larger population of such studies wherein each study has its underlying effect size. Subgroup analysis was done wherever possible when the heterogeneity was high. Continuous data extracted were expressed as mean ± standard deviation and the treatment effect as mean differences reported with 95% confidence interval. The complications rates were included as dichotomous variables. If the standard deviation was not mentioned in the study, it was calculated using the range of values as per Hozo et al. [22].
Quality Assessment
The reviewers (S.A and A.K.S.G) assessed the quality of the included studies using the quality evaluation tool used by the Cochrane Bone, Joint and Muscle Trauma Group [23]. Cochrane Quality Assessment Tool includes 12 points where each point is scored 2, 1, or 0 (maximum score 24) depending on whether the question was fully, partly, or not answered at all for each study. Any disagreements were sorted out by the senior-most author (RBK) and a consensus was reached. High-quality studies have a score of 24 and low quality of 12. This criterion was not used as an exclusion criterion for the selected articles (Table 1).
Table 1.
Study characteristics of included studies
| Authors, year of publication | Location of study | Study design | Sample size, M/F, age | Follow-up (years) | Prosthesis type UC/PS | Prosthesis design | Cochrane quality assessment [23] | ||
|---|---|---|---|---|---|---|---|---|---|
| UC | PS | UC | PS | ||||||
| Kim et al. (2021) [18] | S. Korea | RCT | 50, 1/49, 68.2 | 50, 1/49, 68.2 | 2 | 2 | Persona/Persona | Fixed | 23 |
| Han and Kang (2020) [19] | S. Korea | RCT | 34, 1/33, 67.4 | 34, 1/33, 67.4 | 5.5 | 5.5 | Triathlon/Triathlon | Fixed | 23 |
| Akti et al. (2020) [15] | Turkey | RCT | 33, 4/29, 69.2 | 33, 7/26, 67.7 | 1 | 1 | Vanguard AS/Vanguard PS | Fixed | 21 |
| Jang et al. (2019) [17] | S. Korea | RCT | 45, 1/44, 70 | 45, 1/44, 70 | 2 | 2 | Vanguard AS/Vanguard PS | Fixed | 22 |
| Scott (2018) [16] | USA | RCT | 55, 27/28, 60.9 | 56, 27/29, 63.9 | 5 | 5 | Triathlon/Triathlon | Fixed | 24 |
| Lutzner et al. ( 2017) [11] | Germany | RCT | 60, 19/41, 71.5 | 62, 23/39, 69.9 | 1 | 1 | Columbus/Columbus | Fixed | 18 |
| Kim et al. (2016) [12] | S. Korea | RCT | 42, 2/40, 69 | 40, 2/38, 69.4 | 3 | 3 | E-motion/E-motion | Mobile | 20 |
| Sur et al. (2015) [24] | S. Korea | RCT | 28, 2/26, 68.4 | 28, 2/26, 68.4 | 5.2 | 5.2 | Triathlon/Triathlon | Fixed | 20 |
| Uvehammer et al. (2001) [25] | Sweden | RCT | 25, 10/15, 71 | 22, 12/10, 70 | 2 | 2 | AMK/AMK | Fixed | 18 |
| Laskin et al. (2000) [26] | USA | RCT | 48, NS, NS | 62, NS, NS | 1 | 1 | Genesis II/Genesis II | Fixed | 12 |
S Korea South Korea, CORR Clinical Orthopedic Related Research, JOA Journal of Arthroplasty, KSSTA Knee Surgery, Sports Traumatology, Arthroscopy, JBJS Journal of Bone and Joint Society, PS posterior-stabilized bearing, UC ultra-congruent, AS anterior-stabilized bearing, M/F male/female, RCT randomized control trial, USA United States of America
Results
Study Characteristics
The review included a total of 10 studies with 852 knees; of which 420 underwent TKA with UC TKA and 432 underwent PS TKA with a mean follow-up of 2.77 years. The study demographics are listed in Table 1. Eight studies compared groups according to function score, eight according to complication rates, eight compared ROM, four compared tibial sagittal stability, four compared posterior femoral rollback, and two compared the isokinetic performance [11, 12, 15–19, 24–26].
Quality Assessment
The quality assessment revealed that eight studies were of high quality and two were of moderate quality and no low-quality studies were included. Of the outcome measures assessed, range of motion was the most commonly reported in the studies. The publication bias was assessed with a funnel plot and based on the funnel plots, there appears to be even distribution hence a low possibility of publication bias (Fig. 2).
Fig. 2.
Range of motion funnel plot
Assessment of the Outcomes
Multiple outcomes were assessed for the study. Various PROMs were found to be used in the study (Table 1). The KSS score was used in eight studies and the WOMAC score was used in four studies [11, 12, 15, 17–19, 24, 26]. The pooled data revealed similar scores for the KSS functional score (95% CI: [− 4.50, 0.80]; I2 = 0%; mean difference = − 1.85; p = 0.17; Fig. 3A), knee scores (95% CI: [− 2.45, 2.38]; I2 = 70%; mean difference = − 0.03; p = 0.98; Fig. 3B) for the pain scores (95% CI: [− 1.52, 0.24]; I2 = 0%; mean difference = − 0.64; p = 0.15; Fig. 3C) between the two groups. For WOMAC scores (95% CI: [− 0.54, 1.62]; I2 = 0%; mean difference = 0.54; p = 0.33; Fig. 3D), both the groups were similar.
Fig. 3.
Assessment of patient-related outcomes. SD standard deviation, UC ultra-congruent, PS posterior stabilized, CI confidence interval
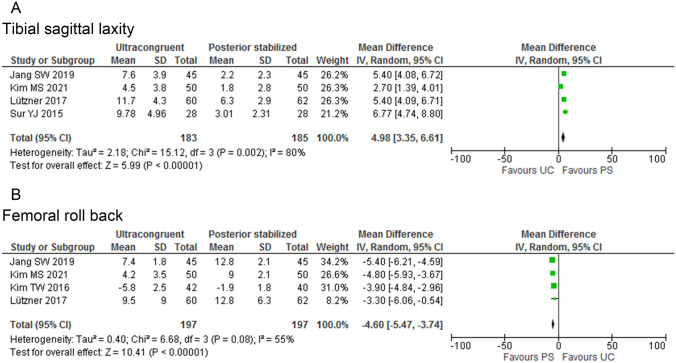
Sagittal Stability
Four studies reported on the sagittal laxity at 90° between the two groups (UC inserts: 198 knees and PS inserts: 202 knees) [11, 17, 18, 24]. The pooled data analysis revealed a better sagittal stability for the PS TKA in comparison to the AS TKA (95% CI: [− 4.50, 0.80]; I2 = 0%; mean difference = − 1.85; p = 0.17; Fig. 4A). The sagittal stability was significantly greater in patients with PS knees than with AS knees.
Fig. 4.
Knee kinematics. SD standard deviation, UC ultra-congruent, PS posterior stabilized, CI confidence interval
Knee Kinematics
Four studies reported on the femoral rollback between the two groups (197 knees in AS TKA and 199 knees in PS TKA) and pooled data analysis revealed a better femoral rollback for the PS TKA in comparison with AS TKA (95% CI: [− 5.47, − 3.74]; I2 = 0%; mean difference = − 4.60; p < 0.00001; Fig. 4B) [11, 12, 17, 18]. Apart from the femoral rollback, two studies compared the femoral translation on varying degrees of knee flexion [11, 12]. Kim et al. noticed although neither the UC nor the PS TKA group reproduced physiologic rotational kinematics, the mobile UC TKA group showed more external rotation of femur [12].
Complication Rates
Nine studies reported on the implant-related complication rates between the two groups (372 AS TKA and 370 PS TKA). The AS group had two complications compared to zero of the PS group [12, 15–19, 24, 25, 27]. No significant difference was seen between the groups (95% CI: [0.30, 29.06]; I2 = 0%; mean difference = 2.95; p = 0.35).
Isokinetic Performance
Two studies reported on the isokinetic performance between the groups [15, 19]. The pooled data analysis of peak extensor torque revealed similar torque levels between both the groups (95% CI: [− 2.80, 2.90]; I2 = 32%; mean difference = 0.05; p = 0.97; Fig. 5A). The pooled data analysis of peak flexor torque revealed similar levels between both the groups (95% CI: [− 5.42, 2.04]; I2 = 0%; mean difference = − 1.69; p = 0.37; Fig. 5B). These were measured at 60°/s.
Fig. 5.
Isokinetic performance. SD standard deviation, UC ultra-congruent, PS posterior stabilized, CI confidence interval
Range of Motion
Eight studies compared postoperative ROM between the two groups (UC inserts: 332 knees and PS inserts: 343 knees) [11, 12, 17–19, 24–26]. Pooled data analysis revealed no significant difference between AS and PS TKA (95% CI: [− 3.13, 0.64]; I2 = 37%; mean difference = − 1.25; p = 0.19; Fig. 6).
Fig. 6.
Range of motion (ROM); SD standard deviation, UC ultra-congruent, PS posterior stabilized, CI confidence interval
Discussion
The most significant finding of the systematic review was that the use of AS TKA is associated with similar functional outcomes, complication rates, peak flexor and extensor torque forces, postoperative ROM in comparison to the PS TKA but, is associated with lesser femoral rollback and increased sagittal laxity. We included only level 1 studies for the meta-analysis.
Literatures on the effectiveness of the AS TKA are a few [10, 11, 18]. The resection of PCL and use of the AS or the deep dished insert theoretically is a valid substitute for the PS TKA. The biomechanical studies often relate an increased paradoxical anterior femoral translation associated with resection of PCL [13]. The only systematic review that tries to assess the functioning of the AS TKA is by Bae et al. [14]. The study has limitations such as it being conducted with a mixture of study designs including prospective and retrospective studies. The data presented had a mixture such as including HSS score in Uvehammer et al. along with KSS function score meta-analysis, certain standard deviations are way too big to be true and authors have not mentioned how did they arrive at the missing SD in the studies and intraoperative ROM recorded by Fritzsche et al. was included in the meta-analysis of postoperative ROM [25, 26, 28]. The current review is a meta-analysis of RCTs which provides the best available quality.
AS TKA was introduced with a philosophy of decreasing the contact stresses and preventing post-cam wear and complications of the PS TKA. The function of PCL is to help in the physiologic femoral rollback. In AS TKA, the UC insert under its profile and lipping in the anterior and posterior ends helps in sagittal stability, and supposedly promotes a better physiological roll back with increased ROM [10, 11, 16]. A limited number of literatures support the superiority of AS TKA in comparison with CR TKA or PS TKA [29–31].
Danilidis et al. noted that the deep-dish inlays reduce the AP translation and centralization of contact pressure results in non-physiological rollback while comparing intraoperative kinematics of AS TKA [32]. Our study revealed a significantly decreased posterior femoral rollback for the AS TKA in comparison to the PS TKA. Fritzsche et al. and Kim et al. noted increasing posterior femoral translation on increasing knee flexion more for the PS TKA beyond 90 degrees [12, 28]. It might be explained by the post-cam mechanism being active at this flexion degree. Kim et al. revealed paradoxical anterior translation for both AS and PS TKA with PS TKA having lesser over the flexion angle [12]. The sagittal stability at 90° of knee flexion which refers to the anteroposterior translation was significantly better for the PS TKA in comparison to the AS TKA. The decreased femoral rollback along with increased sagittal laxity may produce increased shearing forces at the interfaces and decreased ROM. One major flaw exists wherein none of the included studies assessed the sagittal stability in the range 0–90°. The daily routine activities such as walking, running, and climbing stairs require less than 90° of knee flexion hence, it would have been ideal to study the stability in the range of 0–90° [33]. Theoretically, under its increased posterior femoral rollback, and cam and post-mechanism, the PS TKA is supposed to have more ROM than AS TKA [1, 13]. The current study noted no significant difference in ROM between the two prosthesis designs for TKA. Jang et al. and Sur et al. noted UC TKA to have more ROM than PS TKA [17, 24]. Han et al., Kim M S et al., Kim T W et al., and Lutzner et al. recorded PS TKA to have more ROM [11, 12, 18, 19].
The rotation of the femur with respect to the tibia during knee flexion and extension affects the quadriceps muscle function [12]. The AS or UC inserts avoid bone cuts but still need resection of the PCL. Hence, the ability of these inserts to adequately provide femoral rotation is often questionable and has led to the usage of the medial pivot TKA [34]. It is desirable to obtain external rotation of the femur with progressive knee flexion in TKA. Fritsche et al. noted that the use of UC inserts intraoperatively resulted in less anteroposterior stability and slightly less knee flexion compared to a PS insert [28]. Kim et al. noted a 4° less paradoxical internal rotation in AS TKA compared to PS TKA [12].
In the current study, both the UC and PS TKA had similar clinical outcomes concerning KSS scores and WOMAC scores. Soft tissue management in TKA is often seen as a predictor for the improvement in patient function. This factor along with the inability of the present scoring systems to aptly identify the small differences between the functional outcomes may be the cause for the above [35]. With regards to the complication rates, both the groups were similar, and surprisingly only one implant-related complication was seen in total with the UC group and zero with PS TKA. One might need a larger sample size to effectively see the complications as their incidence may be small. Kim MS et al. reported that both the groups showed similar dynamic stability under weight-bearing and knee functions at 2-year follow-up [18]. Yacovelli et al. in their retrospective review of 5970 patients with 3314 undergoing PS or 2656 undergoing CS TKA noted comparable function rates and revision rates at short-term follow-up of 43 months [36]. Lutzner et al. showed similar comparable functional outcomes between the group at 5-year follow-up [27].
Adequate strength of the quadriceps muscle or the extensor mechanism is an indicator of the functioning of TKA. An increased quadriceps force may be needed with implants that have less AP stability which may predispose to higher incidences of anterior knee pain and fatigue. Objective assessment of muscle strength can be done with Isokinetic performance [15]. In the current study, no significant differences were observed between the AS and PS TKA at 60°/s. Han S et al. mentioned the changes at 180°/s and noted similar torque levels both in flexion and extension between the groups. The extensor torque levels in the AS TKA were numerically more at 1st- and 2nd-year follow-ups, but it was not statistically significant [19]. Comparison of the patellofemoral pressures between the AS TKA and PS TKA in cadaveric studies indicate higher pressure in knees with AS TKA than in those treated with PS TKA and normal knees. The more reproducible femoral rollback in the PS TKA may lead to a resultant decrease of the moment arm of the extensor mechanism [37–39].
Total knee replacement aims to provide improved functional outcomes to arthritic patients. Newer implants may not necessarily mean better functional or in vivo kinematic results. This review helps the orthopedic surgeon to select the better implant between the AS and PS TKA while performing a PCL sacrifice. This meta-analysis has its strengths. First, only RCTs were included. Second, the review included implant-related complication rates and isokinetic performance assessment. Third, this review assesses functional outcomes with help of two different PROMs and assesses the ROM both intraoperatively and postoperatively. Fourth, to the best of our knowledge, it is the only article to comment on the intraoperative ROM, implant-related complication rates, flexor and extensor torques, femoral rollback, and WOMAC scores between the two groups.
The current review has its limitations. The functional outcomes used in the articles varied. Few studies reported upon the FJS, OKS, and HSS by which these outcomes could not be analyzed. Second, only one study commented on the intraoperative kinematic assessment of femoral rotation. Ideally, more studies are required. Third, significant heterogeneity was seen among the outcome measures used in the various studies. The random-effects model for meta-analysis which accounts for statistical heterogeneity between the studies in the analysis was used in those situations. Fourth, we could not compare survival rates and revisions between the groups as very few published studies exist to permit a valid meta-analysis. Fifth, many of the included studies and sample sizes were less than 50 in each arm. One would ideally have a larger sample size for effective comparison. In addition, there are no long-term follow-up studies for UC or CS Knee systems. However, we believe that the current review is the most suitable among the existing literature to comment upon AS vs PS in PCL sacrificed TKA. Sixth and lastly the various studies included had different implant designs, this might be a confounding factor.
Conclusion
We conclude with the current meta-analysis that there are some limited benefits in terms of higher sagittal laxity, but less femoral roll back in cruciate sacrificing UC knees. But since there are no long-term wear data, UC inserts with CS technique should be used cautiously and may be used only when the PCL cannot be balanced adequately. There is no evidence or only a few to support the superiority of the AS TKA in terms of clinical outcomes or isokinetic performance or femoral external rotation over PS TKA.
Author Contributions
BSR: planning of study, literature search, writing the manuscript, and quality assessment of the included studies. AKSG: literature search, writing the manuscript, and quality assessment of the included studies. SA: data management, outcome assessment, and quality assessment of the included studies. AKC: data management, outcome assessment, and manuscript preparation. RBK: planning of study, quality assessment of the included studies, and writing and revising the manuscript.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Data Availability
All included studies used in this systematic review and meta-analysis are available online. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. Data regarding this study are not available in any electronic databases.
Declarations
Conflict of Interest
All the authors declare that they do not have any competing interest, concerning this research, authorship, and/or publication of this article. On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Ethical Approval
Approval from the institutional ethics committee was not required for this review article.
Consent to Participate
No participants were enrolled for this review article. Hence, informed consent was not required.
Consent to Publish
All the authors have read the final prepared draft of the manuscript and approve this version, in its current format if considered further for publication.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Balgovind S.Raja, Email: balgovindsraja@gmail.com.
Aditya K. S. Gowda, Email: adityajr.orth@aiimsrishikesh.edu.in
Sajid Ansari, Email: sajidans89@gmail.com.
Arghya Kundu Choudhury, Email: arghyakunduchoudhury@gmail.com.
Roop Bhushan Kalia, Email: roopkalia2003@yahoo.com.
References
- 1.White PB, Turcan S, Satalich JR, et al. Clinical outcomes of a modern total knee arthroplasty prosthesis compared to its predecessor at 5-year follow-up: Matched pair analysis. Journal of Arthroplasty. 2020;35:3150–3155. doi: 10.1016/j.arth.2020.06.024. [DOI] [PubMed] [Google Scholar]
- 2.Ranawat CS, White PB, West S, Ranawat AS. Clinical and radiographic results of attune and PFC sigma knee designs at 2-year follow-up: A prospective matched-pair analysis. Journal of Arthroplasty. 2017;32:431–436. doi: 10.1016/j.arth.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 3.Ritter MA, Davis KE, Meding JB, Farris A. The role of the posterior cruciate ligament in total knee replacement. Bone & Joint Research. 2012;1:64–70. doi: 10.1302/2046-3758.14.2000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schultz RA, Miller DC, Kerr CS, Micheli L. Mechanoreceptors in human cruciate ligaments. A histological study. Journal of Bone and Joint Surgery. American Volume. 1984;66:1072–1076. doi: 10.2106/00004623-198466070-00014. [DOI] [PubMed] [Google Scholar]
- 5.Longo UG, Ciuffreda M, Mannering N, et al. Outcomes of posterior-stabilized compared with cruciate-retaining total knee arthroplasty. The Journal of Knee Surgery. 2018;31:321–340. doi: 10.1055/s-0037-1603902. [DOI] [PubMed] [Google Scholar]
- 6.Sequeira SB, Scott J, Novicoff W, Cui Q. Systematic review of the etiology behind patellar clunk syndrome. World Journal of Orthopedics. 2020;11:184–196. doi: 10.5312/wjo.v11.i3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott RD, Volatile TB. Twelve years’ experience with posterior cruciate-retaining total knee arthroplasty. Clinical Orthopaedics. 1986;205:100–107. [PubMed] [Google Scholar]
- 8.Puloski SK, McCalden RW, MacDonald SJ, et al. Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris. Journal of Bone and Joint Surgery. American Volume. 2001;83:390–397. doi: 10.2106/00004623-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Hofmann AA, Tkach TK, Evanich CJ, Camargo MP. Posterior stabilization in total knee arthroplasty with use of an ultracongruent polyethylene insert. Journal of Arthroplasty. 2000;15:576–583. doi: 10.1054/arth.2000.6633. [DOI] [PubMed] [Google Scholar]
- 10.Song E-K, Lim H-A, Joo S-D, et al. Total knee arthroplasty using ultra-congruent inserts can provide similar stability and function compared with cruciate-retaining total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25:3530–3535. doi: 10.1007/s00167-017-4553-3. [DOI] [PubMed] [Google Scholar]
- 11.Lützner J, Beyer F, Dexel J, et al. No difference in range of motion between ultracongruent and posterior stabilized design in total knee arthroplasty: A randomized controlled trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25:3515–3521. doi: 10.1007/s00167-016-4331-7. [DOI] [PubMed] [Google Scholar]
- 12.Kim TW, Lee SM, Seong SC, et al. Different intraoperative kinematics with comparable clinical outcomes of ultracongruent and posterior stabilized mobile-bearing total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24:3036–3043. doi: 10.1007/s00167-014-3489-0. [DOI] [PubMed] [Google Scholar]
- 13.Louisia S, Siebold R, Canty J, Bartlett RJ. Assessment of posterior stability in total knee replacement by stress radiographs: Prospective comparison of two different types of mobile bearing implants. Knee Surgery, Sports Traumatology, Arthroscopy. 2005;13:476–482. doi: 10.1007/s00167-004-0567-8. [DOI] [PubMed] [Google Scholar]
- 14.Bae J-H, Yoon J-R, Sung J-H, Shin Y-S. Posterior-stabilized inserts are preferable to cruciate-substituting ultracongruent inserts due to more favourable kinematics and stability. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;26:3300–3310. doi: 10.1007/s00167-018-4872-z. [DOI] [PubMed] [Google Scholar]
- 15.Akti S, Karakus D, Sezgin EA, Cankaya D. No differences in clinical outcomes or isokinetic performance between cruciate-substituting ultra-congruent and posterior stabilized total knee arthroplasties: A randomized controlled trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2020 doi: 10.1007/s00167-020-06275-z. [DOI] [PubMed] [Google Scholar]
- 16.Scott DF. Prospective randomized comparison of posterior-stabilized versus condylar-stabilized total knee arthroplasty: final report of a five-year study. Journal of Arthroplasty. 2018;33:1384–1388. doi: 10.1016/j.arth.2017.11.037. [DOI] [PubMed] [Google Scholar]
- 17.Jang SW, Kim MS, Koh IJ, et al. Comparison of anterior-stabilized and posterior-stabilized total knee arthroplasty in the same patients: A prospective randomized study. Journal of Arthroplasty. 2019;34:1682–1689. doi: 10.1016/j.arth.2019.03.062. [DOI] [PubMed] [Google Scholar]
- 18.Kim MS, Koh IJ, Kim CK, et al. Comparison of joint perception between posterior-stabilized and ultracongruent total knee arthroplasty in the same patient. Journal of Bone and Joint Surgery. American Volume. 2021;103:44–52. doi: 10.2106/JBJS.20.00279. [DOI] [PubMed] [Google Scholar]
- 19.Han H-S, Kang S-B. Anterior-stabilized TKA is inferior to posterior-stabilized TKA in terms of postoperative posterior stability and knee flexion in osteoarthritic knees: A prospective randomized controlled trial with bilateral TKA. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28:3217–3225. doi: 10.1007/s00167-019-05827-2. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 22.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Panjwani TR, Mullaji A, Doshi K, Thakur H. Comparison of functional outcomes of computer-assisted vs conventional total knee arthroplasty: a systematic review and meta-analysis of high-quality prospective studies. Journal of Arthroplasty. 2019;34(3):586–593. doi: 10.1016/j.arth.2018.11.028. [DOI] [PubMed] [Google Scholar]
- 24.Sur Y-J, Koh I-J, Park S-W, et al. Condylar-stabilizing tibial inserts do not restore anteroposterior stability after total knee arthroplasty. Journal of Arthroplasty. 2015;30:587–591. doi: 10.1016/j.arth.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 25.Uvehammer J, Kärrholm J, Regnér L, et al. Concave versus posterior-stabilized tibial joint surface in total knee arthroplasty: Randomized evaluation of 47 knees. Journal of Arthroplasty. 2001;16:25–32. doi: 10.1054/arth.2001.17939. [DOI] [PubMed] [Google Scholar]
- 26.Laskin RS, Maruyama Y, Villaneuva M, Bourne R. Deep-dish congruent tibial component use in total knee arthroplasty: A randomized prospective study. Clinical Orthopaedics. 2000 doi: 10.1097/00003086-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Lützner J, Beyer F, Lützner C, et al. Ultracongruent insert design is a safe alternative to posterior cruciate-substituting total knee arthroplasty: 5-year results of a randomized controlled trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2021 doi: 10.1007/s00167-021-06545-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fritzsche H, Beyer F, Postler A, Lützner J. Different intraoperative kinematics, stability, and range of motion between cruciate-substituting ultracongruent and posterior-stabilized total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;26:1465–1470. doi: 10.1007/s00167-017-4427-8. [DOI] [PubMed] [Google Scholar]
- 29.Rajgopal A, Aggarwal K, Khurana A, et al. Gait parameters and functional outcomes after total knee arthroplasty using persona knee system with cruciate retaining and ultracongruent knee inserts. Journal of Arthroplasty. 2017;32:87–91. doi: 10.1016/j.arth.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 30.Stirling P, Clement ND, MacDonald D, et al. Early functional outcomes after condylar-stabilizing (deep-dish) versus standard bearing surface for cruciate-retaining total knee arthroplasty. Knee Surgery & Related Research. 2019;31:3. doi: 10.1186/s43019-019-0001-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berend KR, Lombardi AV, Adams JB. Which total knee replacement implant should I pick? Correcting the pathology: The role of knee bearing designs. The Bone & Joint Journal. 2013;95-B:129–132. doi: 10.1302/0301-620X.95B11.32835. [DOI] [PubMed] [Google Scholar]
- 32.Daniilidis K, Skwara A, Vieth V, et al. Highly conforming polyethylene inlays reduce the in vivo variability of knee joint kinematics after total knee arthroplasty. The Knee. 2012;19:260–265. doi: 10.1016/j.knee.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Rowe PJ, Myles CM, Walker C, Nutton R. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: How much knee motion is sufficient for normal daily life? Gait & Posture. 2000;12:143–155. doi: 10.1016/s0966-6362(00)00060-6. [DOI] [PubMed] [Google Scholar]
- 34.Cacciola G, Mancino F, De Meo F, et al. Mid-term survivorship and clinical outcomes of the medial stabilized systems in primary total knee arthroplasty: A systematic review. Journal of Orthopaedics. 2021;24:157–164. doi: 10.1016/j.jor.2021.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wautier D, Thienpont E. Changes in anteroposterior stability and proprioception after different types of knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25:1792–1800. doi: 10.1007/s00167-016-4038-9. [DOI] [PubMed] [Google Scholar]
- 36.Yacovelli S, Grau LC, Hozack WJ, Courtney PM. Functional outcomes are comparable between posterior stabilized and cruciate-substituting total knee arthroplasty designs at short-term follow-up. Journal of Arthroplasty. 2021;36:986–990. doi: 10.1016/j.arth.2020.09.008. [DOI] [PubMed] [Google Scholar]
- 37.Borque KA, Gold JE, Incavo SJ, et al. Anteroposterior knee stability during stair descent. Journal of Arthroplasty. 2015;30:1068–1072. doi: 10.1016/j.arth.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 38.Heyse TJ, Becher C, Kron N, et al. Patellofemoral pressure after TKA in vitro: Highly conforming vs. posterior stabilized inlays. Archives of Orthopaedic and Trauma Surgery. 2010;130:191–196. doi: 10.1007/s00402-009-0920-y. [DOI] [PubMed] [Google Scholar]
- 39.Tanikawa H, Tada M, Harato K, et al. Influence of total knee arthroplasty on patellar kinematics and patellofemoral pressure. Journal of Arthroplasty. 2017;32:280–285. doi: 10.1016/j.arth.2016.06.044. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All included studies used in this systematic review and meta-analysis are available online. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. Data regarding this study are not available in any electronic databases.