Abstract
Recently, polyetheretherketone (PEEK) has been introduced to the dental market as a high-performance and chemically inert biomaterial. This study aimed to compare the wear resistance, abrasiveness, color stability, and displacement resistance of zirconia and PEEK milled crowns. An ideal tooth preparation of a first maxillary molar was done and scanned by an intraoral scanner to make a digital model. Then, the prosthetic crown was digitally designed on the CAD software, and the STL file was milled in zirconia (CaroZiir S, Carol Zircolite Pvt. Ltd., Gujarat, India) and PEEK (BioHpp, Bredent GmbH, Senden, Germany) crowns using five-axis CNC milling machines. The wear resistance, color stability, and displacement resistance of the milled monolithic zirconia with unfilled PEEK crowns using a chewing simulator with thermocyclic aging (120,000 cycles) were compared. The antagonist wear, material wear, color stability, and displacement were evaluated and compared among the groups using the Wilcoxon–Mann–Whitney U-test. Zirconia was shown to be three times more abrasive than PEEK (p value < 0.05). Zirconia had twice the wear resistance of PEEK (p value < 0.05). Zirconia was more color stable than PEEK (p value < 0.05). PEEK had more displacement resistance than zirconia (p value < 0.05). PEEK offers minimal abrasion, better stress modulation through plastic deformation, and good color stability, which make it a promising alternative to zirconia crown.
Keywords: PEEK, zirconia, crowns, biomaterials, biodegradation, CAD/CAM, chewing simulation, wear resistance, color stability, aging process, displacement resistance, dentistry, dental materials
1. Introduction
Wear and tribological properties are important in dentistry [1,2]. Progressive wear of the dental materials from the tooth and restorations occurs due to excessive mechanical and chemical processes such as mastication, erosion, and abrasion [3,4]. Hence, abrasion resistance, as well as abrasiveness, are important properties of restorative materials [5]. Recently, restorative materials with high wear resistance are being developed in the clinical scenario [6]. Although there are various in vitro studies on the wear and abrasiveness of the restorative materials, there are fewer studies representing the simulated oral conditions. Furthermore, the compressive strength and displacement resistance play an important role in the selection of restorative material, which can be studied from a universal testing machine [7].
The discoloration is another significant parameter that needs to be studied extensively. This value of the color stability of the restorative material is evaluated over a prolonged period using a spectrophotometer [8]. The surface roughness and surface free energy significantly influence the color stability of the material. The color stability is also affected by the thermocyclic aging of the restorative material. This leads to a color change from chroma change and hue difference [9].
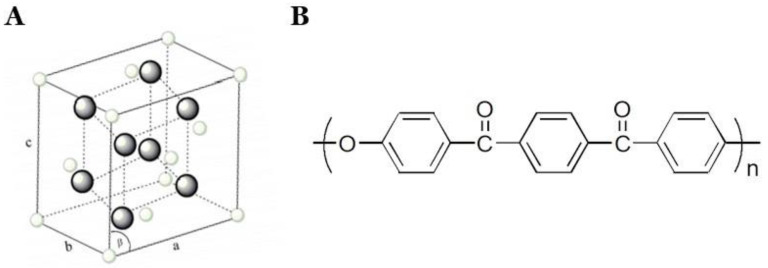
Zirconia (Zirconium oxide, ZrO2) is currently the most used tooth-colored restorative material in dentistry (Figure 1A). It has excellent esthetics, good biocompatibility, and superior mechanical properties to metals. The wear resistance of zirconia is higher than metal, and thus, it is even being used to fabricate implants and implant abutments due to its high strength [10]. Fully contoured monolithic zirconia is made through CAD/CAM technology completely. This eliminates the dental laboratory work in the manual fabrication of the crowns, thus increasing the precision [11,12].
Figure 1.
Structure of zirconia (A) and polyetheretherketone (PEEK) (B). Modified from [13].
Polyaryletherketone (PAEK) consists of polyetheretherketone (PEEK) and polyetherketoneketone (PEKK), and it was recently introduced in dentistry [14]. Recently, PEEK and PEKK were introduced to the dental market as high-performance and chemically inert biomaterials [14,15]. With its extremely low potential to trigger an allergy, PEEK has very few reported systemic immune responses after intraoral insertion [16]. PEEK can become an alternative to conventional and well-investigated veneering ceramics and denture base resin materials with low discoloration and improved mechanical properties (Figure 1B) [17]. PEEK-based materials are being used along with or instead of polymethyl methacrylate (PMMA) and resin composite materials in both removable and fixed dental prostheses. PEEK also has a low modulus of elasticity compared to the bone, which allows for a better absorption of functional stress by deformation. This acts as a great advantage over the ceramic materials used. PEEK also shows low abrasive wear of the enamel in comparison to ceramic materials. Carbon and glass fiber variants of PEEK have higher flexural strength and color stability. PEEK is highly color stable in comparison to PMMA and composite resin materials. To improve its esthetic properties, various manufacturers have added composite resins and titanium dioxide into the PEEK material. PEEK exhibits excellent chemical resistance due to its chemical structure; thus, it can withstand high temperatures without significant degradation [18,19].
There has been a vast development in digital technologies in dentistry including 3D scanning, designing, and 3D/4D/5D printing [20,21,22,23,24]. The zirconia, metal, PEEK, and PMMA prosthetic crowns can be digitally designed and milled using milling machines. Milling machines are available as three-axis, four-axis, and five-axis milling. The accuracy of the milling machine determines the final milled output. IMES icore 350i is a five-axis milling machine that is one of the standard machines for milling various prosthetic materials [25,26]. High-quality milling machines with standardized protocols that are used globally produced highly accurate crowns.
PEEK can be a promising alternative to titanium and zirconium to use in various clinical situations in dental practice due to its high-quality mechanical properties such as favorable elastic modulus, strength, rigidity, and light weight [15,27,28,29]. The PEEK prostheses have shown better properties than the unmodified form of PEEK. It can be modified with various biomaterials to produce a composite with improved properties for various biomedical applications [27,30,31,32,33,34,35,36,37], such as carbon fiber-reinforced PEEK (CFR-PEEK) [32,34,35], resin-PEEK [36], nilinated-poly (ether ether ketone) (AN-PEEK), and AN-PEEK/f-CNOs composite thin films [30].
Although PEEK is widely used at present, there are very limited studies that compared the mechanical properties of PEEK as fixed prostheses with other materials such as zirconia. In addition, no study compared the mechanical properties of zirconia and PEEK using five-axis milling. Thus, this study aimed to compare the wear resistance, abrasiveness, color stability, and displacement resistance of PEEK and zirconia milled crowns using a chewing simulator with thermocyclic aging.
2. Materials and Methods
The study was approved by the Scientific Review Board of Saveetha University (SRB/SDMDS09/18/PROSTHO/001). A total of 24 crowns were made, which were divided into two different groups based on two different materials taking reference to sample size from previous studies [38,39]. Group 1 (n = 12) consisted of milled zirconia crowns (CaroZiir S, Carol Zircolite Pvt. Ltd., Gujarat, India) and Group 2 (n = 12) consisted of milled PEEK crowns (BioHpp, Bredent GmbH, Senden, Germany). Each group was divided into 3 subgroups, as shown in Table 1. Group 1 consists of (1a) zirconia control, (1b) zirconia thermocycled, and (1c) zirconia worn and thermocycled, and Group 2 consists of (2a) PEEK control, (2b) PEEK thermocycled, and (2c) PEEK worn and thermocycled.
Table 1.
Details of zirconia and PEEK restorations used in this study.
| Groups | Prosthetic Crowns (n = 24) | |
|---|---|---|
| Zirconia (n = 12) | PEEK (n = 12) | |
| Control (C) | zirconia control (1a) (n = 4) |
PEEK control (2a) (n = 4) |
| Thermocycled (T) | zirconia thermocycled (1b) (n = 4) |
PEEK thermocycled = (2b) (n = 4) |
| Thermocycled + Worn (T + W) | zirconia worn and thermocycled (1c) (n = 4) |
PEEK worn and thermocycled (2c) (n = 4) |
2.1. Die Preparation
Tooth preparations were done on a first maxillary molars of the Typodont model (PER5001-UL-SCP-AK-28, Nissin Dental, Kyoto, Japan) using a taper flat end bur for the buccal and palatal surfaces and were replicated into multiple epoxy resin dies (Acculite Die Epoxy 8000 Fast, Henry Schein Inc., New York, NY, USA). The tooth preparations had 1.5 mm shoulder margins ideal for an all-ceramic restoration with a clearance of 2 mm occlusally according to the previous study [40].
2.2. Designing and Milling of Zirconia and PEEK Crowns
The teeth were scanned in with an intraoral scanner (Trios 3, 3Shape, Copenhagen, Denmark), and the first maxillary molar crown was digitally designed on the CAD software. From STL files, zirconia and PEEK crowns were created and milled using a 5-axis computerized numeric control (CNC) milling machine (IMES iCore 350i, imes-icore GmbH, Eiterfeld, Germany) [41,42]. The zirconia crowns were sintered at 1450 °C for 60 min [43].
Then, the digitally fabricated zirconia and PEEK crowns were polished with polishing paste and a rubber wheel according to the manufacturer’s protocol [44,45]. The crown sizes were 11.8 mm in length, 7 mm in width, 2 mm in thickness occlusal, and 1.5 mm thickness at the margin, the middle, and cervical portion of the crown [40]. These precise measurements were made while designing the crowns in the CAD software (3 Shape, Düsseldorf, Germany).
2.3. Cementation of the Crowns onto the Die
After the fabrication, the crowns were stored at room temperature (25 °C) for at least 1 day, and any possible crack formations were examined. Then, the crowns were sandblasted with 100 µm at 1 bar pressure for 10 s. They were conditioned with 2 layers of bonding agents (ScotchBond Universal, 3M ESPE, Seefeld, Germany) and then cured for 20 s using curing light (Elipar Deepcure, 3M ESPE, Seefeld, Germany) as recommended by the manufacturer [46,47]. Then, the crowns were permanently cemented onto the epoxy resin dies using luting resin cement (RelyX U200, 3M ESPE, Seefeld, Germany) in the isolated field.
2.4. Chewing Simulation
The crown samples were prepared in the resin die and mounted with fast-setting high-strength low-expansion plaster (WhipMix Mounting Plaster, Ivoclar Vivadent AG, Schaan Fürstentum, Liechtenstein). The steatite antagonists (Steatite, SD Mechatronik, Munich, Germany) were used to mimic enamel and mounted using acrylic resin onto the aluminum mounts. The steatite balls were of 4 mm width and length. They were kept in cusp to fossa occlusion with the zirconia and PEEK crowns.
The chewing simulator (CS-4, SD Mechatronik, Munich, Germany) had 4 testing chambers within a thermocycling chamber. They have 2 moving parts: the vertical bar (Z-axis) and the horizontal table (X-axis). The samples were mounted onto the table, which could move back and forth. The antagonists were connected to the vertical bar and moved vertically. The load of 5 kg weights was created and applied to the samples by the antagonists. The antagonist samples of 4 mm diameter (Steatite, SD Mechatronik, Munich, Germany) were held by the vertical bar and the horizontal bar held the force sensors in order to evaluate the force applied at each cycle. The load was added to each rod to increase the masticatory load on each sample to simulate the oral environment. Thermocycling was done from 4 to 60 °C and each cycle consisted of one cold and one hot cycle, and the filling time of the chamber was kept for 12 s [48,49]. Chewing stimulation was done for 120,000 cycles [50,51].
2.5. Surface Wear of Samples Using a Laserscanner
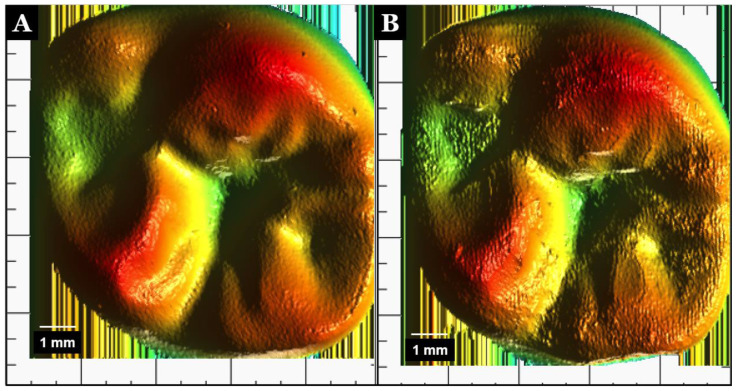
The zirconia and PEEK samples were pretested by a 3D laserscanner (LAS-20, SD Mechatronik, Munich, Germany), and the color graph was obtained. The surface wear of the samples was analyzed and recorded following the chewing simulator cycles with the thermocycling process. The vertical sensor resolution is 0.8 µm; thus, fine movements and cracks were detected. The samples were inserted onto the self-centering mount. The measurement fields were defined by a built-in camera, and the images were exported as jpeg files to be evaluated (Figure 2).
Figure 2.
Color images of crowns after wear. Zirconia (A) and PEEK (B).
2.6. Color Stability Using a Digital Spectrophotometer
A digital spectrophotometer (Vita Easyshade Compact, Vita Zahnfabrik, Bad Säckingen, Germany) has been used to determine the precise and reliable shade matching for natural teeth and ceramic restorations. It was also used to evaluate the color stability of the crowns before and after thermocycling and the chewing simulator. The digital spectrophotometer measured the wavelength range from 400 to 700 nm and used LED technology, which was unaffected by the environment.
2.7. Displacement of the Crown Using a Universal Testing Machine
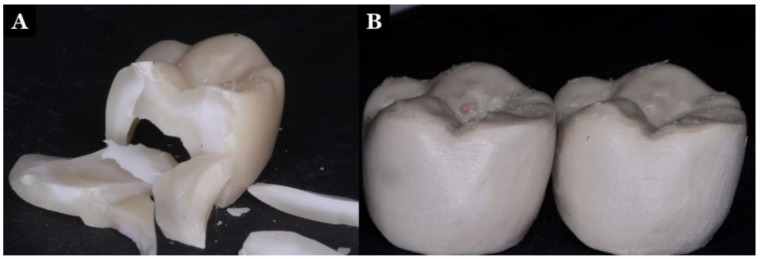
A universal testing machine (Instron 5566, Instron Ltd., Buckinghamshire, UK) capable of dynamic and static testing was used to evaluate the displacement of the crowns. The samples were mounted on the epoxy resin dies (Acculite Die Epoxy 8000 Fast, Henry Schein Inc., New York, NY, USA) and placed onto the platform of the universal testing machine. The zirconia and PEEK crowns were tested before and after the wear test and thermocycling process. They were subjected to a load of 2500 Ncm−1. The displacement of the material was observed in mm2 (Figure 3).
Figure 3.
Displaced and fractured zirconia crown (A) and displaced and flattened cusp of the PEEK crown (B).
2.8. Statistics
All the data obtained were analyzed using the SPSS (SPSS 20, SPSS Inc., Chicago, IL, USA). Normality tests for the antagonist wear (mm2), material wear (mm2), color stability (ΔE), and displacement (mm2) were done using the Kolmogorov–Smirnov test, Levene test, and Shapiro–Wilk test, and the data were not normally distributed. As the variables were not normally distributed, non-parametric tests using Wilcoxon–Mann–Whitney U-tests were used to compare the values among the groups. The significant level was set at p value = 0.05.
3. Results
Wear of the steatite antagonist caused by zirconia compared to PEEK showed a significant difference (p < 0.001), as the zirconia caused three times more antagonist wear than PEEK, as shown in Table 2.
Table 2.
Results of antagonistic wear produced by zirconia and PEEK crowns.
| Antagonist Wear (mm2) (Post-Wear) | Material | Wilcoxon–Mann–Whitney U Test | ||
|---|---|---|---|---|
| Zirconia | PEEK | W | p Value | |
| Mean (SD) | 6.17 (0.92) | 2.50 (0.60) | 144.00 | <0.001 * |
| Median (IQR) | 6.33 (0.94) | 2.62 (1) | ||
| Range | 4.25–7.5 | 1.5–3.5 | ||
SD = standard deviation, IQR = interquartile range. * Significant differences at p value < 0.05.
Similarly, the zirconia crowns were more wear-resistant than PEEK crowns over 120,000 cycles in the chewing simulator (p < 0.001), as shown in Table 3. PEEK crowns showed two times more wear than zirconia crowns (p < 0.001).
Table 3.
Results of wear of the zirconia and PEEK crowns.
| Material Wear (mm2) (Post-Wear) | Material | Wilcoxon–Mann–Whitney U-Test | ||
|---|---|---|---|---|
| Zirconia | PEEK | W | p Value | |
| Mean (SD) | 1.68 (0.49) | 3.75 (0.89) | 0.500 | <0.001 * |
| Median (IQR) | 1.68 (0.56) | 3.5 (1.12) | ||
| Range | 1–2.5 | 2.5–5.5 | ||
SD = standard deviation, IQR = interquartile range. * Significant differences at p value < 0.05.
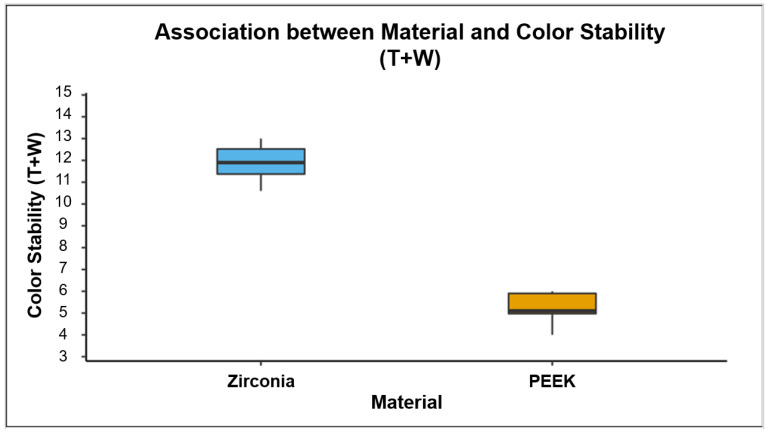
The ΔE values of color stability significantly decreased (p < 0.001) when the zirconia and PEEK crowns underwent wear and aging in the chewing simulator, as shown in Table 4. In addition, the ΔE value showed a significant difference among the control, thermocycled, and thermocycled and worn groups of both zirconia and PEEK crowns (p < 0.001). The color stability of thermocycled and worn zirconia was better than that of PEEK crowns (p < 0.001) (Figure 4).
Table 4.
Results of the color stability of the zirconia and PEEK crowns.
| Color Stability | Crown Materials | p Value | |||
|---|---|---|---|---|---|
| Zirconia | PEEK | ||||
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | ||
| Control (C) | 17.71 (0.68) | 17.85 (0.62) | 9.58 (0.51) | 9.50 (0.65) | <0.001 * |
| Thermocycled (T) | 14.72 (0.85) | 14.65 (1.12) | 6.23 (0.40) | 6.20 (0.58) | <0.001 * |
| Thermocycled + Worn (T + W) | 11.88 (0.81) | 11.90 (1.15) | 5.28 (0.60) | 5.10 (0.93) | <0.001 * |
| Friedman Test (p value) | <0.001 * | <0.001 * | |||
SD = standard deviation, IQR = interquartile range. * Significant differences at p value < 0.05.
Figure 4.
The Box-and-Whisker plot shows the distribution of color stability of thermocycled and worn zirconia and PEEK crowns. The color stability of thermocycled and worn zirconia was significantly better than that of the PEEK crowns (p < 0.001).
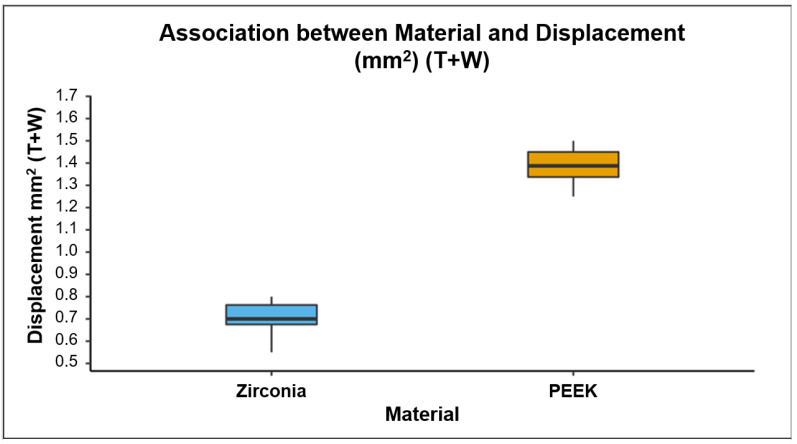
The resistance to displacement of the zirconia and PEEK materials decreased significantly (p < 0.001) following thermocycling and wear in the chewing simulator (Table 5). It also showed a significant difference between the control, thermocycled, and thermocycled and worn groups in both zirconia and PEEK crowns (p < 0.001). Furthermore, PEEK crowns showed significantly (p < 0.001) more resistance to displacement than zirconia crowns following thermocycling and wear in the chewing simulator (Figure 5).
Table 5.
Results of the change in displacement of the zirconia and PEEK crowns.
| Displacement (mm2) | Material | p Value | |||
|---|---|---|---|---|---|
| Zirconia | PEEK | ||||
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | ||
| Control | 0.73 (0.05) | 0.72 (0.06) | 1.90 (0.18) | 1.90 (0.20) | <0.001 * |
| Thermocycled (T) | 0.45 (0.11) | 0.44 (0.14) | 1.49 (0.09) | 1.48 (0.11) | <0.001 * |
| Thermocycled + Worn (T + W) | 0.70 (0.09) | 0.70 (0.09) | 1.39 (0.08) | 1.39 (0.11) | <0.001 * |
| Friedman Test (p value) | <0.001 * | <0.001 * | |||
SD = standard deviation, IQR = interquartile range. * Significant differences at p value < 0.05.
Figure 5.
The Box-and-Whisker plot shows the distribution of displacement (mm2) of thermocycled and worn zirconia and PEEK crowns. The displacement resistance of thermocycled and worn PEEK was higher than that of the zirconia crowns (p < 0.001).
4. Discussion
Although various new biomaterials are introduced for biomedical applications, PEEK has been widely used for dental applications [52,53,54,55,56,57]. The abrasion resistance, color stability, and displacement resistance of the restorative material are the important properties of restorative materials [5,6,7,9]. In this study, these properties are studied and compared between milled zirconia and PEEK crowns. It was found that the crowns made of zirconia produced three times more antagonist wear (p value < 0.05), maintained higher color stability (p value < 0.05), and offered the least displacement (p value < 0.05) compared with crowns made of PEEK. These findings are similar to the previous studies [58,59,60,61].
This study used standardized steatite balls, since it is a standard antagonist used for wear simulation studies [62]. The modulus of elasticity of this material is close to that of enamel. Steatite had good thermal conductivity and good thermal shock resistance; thus, it could withstand the constant force and thermocycling process in the chewing simulator. Thus, the steatite balls did not affect the results in this present study, as they had a modulus of elasticity close to the enamel and were used as antagonists in both study groups. In addition, zirconia and PEEK both showed satisfactory results [63,64,65]. Hence, it can be assumed that the properties of these two materials in this study are similar to the materials evaluated from the previous study by Daou [66].
In this study, the thermocycling temperature in the chewing simulator was simulated to match the oral environment. It was variable between −10 and 60 °C [40]. This was a standardized protocol used in the previously mentioned studies. Since this standardized protocol was used, it did not have confounding effects in the present study. A standardized axis origin was established for all the samples, and a 2 mm radius was allowed for movement in the x, y, and z-axis. Every sample went through the same amount of cycles (120,000 cycles) with a constant force of 200 Ncm−1 [67]. The movement of antagonists established was buccal to lingual with a thermal cyclic loading time of 12 s [40]. The occlusion was established as a cusp to the fossa in relation to the steatite balls occluding with the central fossa of the crowns, as mentioned in the previous studies [40,68]. The chewing simulator was standardized according to the manufacturer for the present study. Thus, it can be eliminated as one of the confounding factors.
The process of sintering was carried out at 1450 °C for 60 min, as recommended by the previous studies [69,70]. This was a standardized protocol followed for the sintering of zirconia [70]. However, this protocol is known to have a certain amount of shrinkage. This factor could affect the results of the study; however, the final measurements of the crowns were made, and this did not seem to affect the result of the study.
Zirconia can be polished or glazed, and it has been shown that polishing produces minimal wear compared to glazed zirconia [44,71,72,73]. So, we did polishing for the zirconia crowns instead of glazing [74,75,76]. PEEK was polished using a rubber wheel and polishing paste as recommended in previous studies [33]. Even polishing was carried out for both the materials; thus, this factor could have a limited effect on the results. This study only evaluated the wear resistance and did not consider the hardness or scratch resistance. Hence, these factors may be confounding factors.
In this study, strict environment and lighting protocol were maintained as reported in the previous study [71]. A calibrated Vita Easyshade guide digital spectrophotometer has been widely used for color assessment of various composite and porcelain materials [77,78]. The measurement made was independent of the surrounding light and heat present; thus, this parameter had limited or almost no effect on the final color stability of the zirconia and PEKK crowns.
The displacement in millimeters at a force of 2500 kN was evaluated for the PEEK and zirconia samples [79]. This was carried out using an Instron Electropuls E3000 all-electric dynamic testing machine. Since the machine was calibrated every time before testing, it could have little or no effect on the results of the present study.
The evaluation of the wear can be observed using various contact and non-contact profilometers such as True Definition (TD) from the 3M ESPE and 3D laserscanner (LAS-20) from SD MEchatronik [50]. Although many studies have mentioned that True Definition is more accurate than 3D laserscanner for the evaluation of wear, no statistical significance between both the machines was found [50,80], and the 3D laserscanner presents optimal accuracy [81]. In this present study, we used the 3D laserscanner to evaluate the wear pattern in two materials.
There are certain limitations to this study. Enamel was not used as an antagonist due to errors in standardization, the wear pattern was simulated only in the buccolingual direction, the circular movement of mastication was not replicated, and distilled water was used in the simulator instead of artificial saliva. Various confounding factors in this study can be the type of antagonist used, thermocycling process, characteristics of the chewing simulator, accuracy of the milling machine, and effect of the environment on the color stability. Although the surface wear can be studied from various techniques such as scanning electronic microscope (SEM) and energy-dispersive X-ray spectroscopy (EDS) [2], we used only the 3D laserscanner due to its availability and limited time.
The present report tested only wear, color stability, and displacement. It could be interesting in the future to test and compare PEEK materials also for flexural strength [82], synergic potential [83], and biocompatibility using cell culture [52,84]. In addition, the future scope of this research is a long-term split-mouth double-blinded randomized controlled clinical trial to evaluate the wear pattern and color stability of the zirconia and PEEK crowns.
5. Conclusions
Zirconia is currently the most used tooth-colored restorative material, and PEEK is used as an alternative to zirconium in dentistry. Within the limitation of this study, the crowns made of zirconia produced three times more antagonist wear, maintained higher color stability, and offered the least displacement compared with crowns made of PEEK. The PEEK crowns showed minimal abrasion, better stress modulation through plastic deformation, and good color stability, which makes it a promising alternative to zirconia for fabrication of the crown. The clinician can choose the material for the fabrication of dental prostheses according to the application considering its properties, advantages, and limitations.
Author Contributions
Conceptualization, S.S.A., D.G. and D.N.V.; methodology, S.S.A., D.G. and D.N.V.; software, S.S.A.; validation, A.H., D.R. and P.A. (Padma Ariga); formal analysis, D.N.V. and D.G.; investigation, S.S.A.; resources, A.H., D.R. and P.A. (Padma Ariga); data curation, D.N.V., D.G.; writing—original draft preparation, S.S.A. and P.A. (Padma Ariga); writing—review and editing, A.H., V.S. and D.R.; visualization, S.S.A., A.H., P.A. (Pokpong Amornvit), D.R. and V.S.; supervision, D.G.; project administration, D.G.; funding acquisition, D.N.V. and V.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding authors.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rokaya D., Srimaneepong V., Qin J., Siraleartmukul K., Siriwongrungson V. Graphene oxide/silver nanoparticle coating produced by electrophoretic deposition improved the mechanical and tribological properties of niti alloy for biomedical applications. J. Nanosci. Nanotechnol. 2019;19:3804–3810. doi: 10.1166/jnn.2019.16327. [DOI] [PubMed] [Google Scholar]
- 2.Diabb J., Rodríguez C.A., Mamidi N., Sandoval J.A., Taha-Tijerina J., Martínez-Romero O., Elías-Zúñiga A. Study of lubrication and wear in single point incremental sheet forming (spif) process using vegetable oil nanolubricants. Wear. 2017;376–377:777–785. doi: 10.1016/j.wear.2017.01.045. [DOI] [Google Scholar]
- 3.Lee A., He L.H., Lyons K., Swain M.V. Tooth wear and wear investigations in dentistry. J. Oral Rehabil. 2012;39:217–225. doi: 10.1111/j.1365-2842.2011.02257.x. [DOI] [PubMed] [Google Scholar]
- 4.Gkantidis N., Dritsas K., Ren Y., Halazonetis D., Katsaros C. An accurate and efficient method for occlusal tooth wear assessment using 3D digital dental models. Sci. Rep. 2020;10:10103. doi: 10.1038/s41598-020-66534-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gundugollu Y., Yalavarthy R.S., Krishna M.H., Kalluri S., Pydi S.K., Tedlapu S.K. Comparison of the effect of monolithic and layered zirconia on natural teeth wear: An in vitro study. J. Indian Prosthodont. Soc. 2018;18:336–342. doi: 10.4103/jips.jips_105_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ludovichetti F.S., Trindade F.Z., Werner A., Kleverlaan C.J., Fonseca R.G. Wear resistance and abrasiveness of cad-cam monolithic materials. J. Prosthet. Dent. 2018;120:318.e1–318.e8. doi: 10.1016/j.prosdent.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 7.Ríos S.E., Garcilazo G.A., Guerrero I.J., Meade R.I., Miguelena M.K. Comparative study of displacement resistance of four zirconia cements. Rev. Odont. Mex. 2017;21:235–240. [Google Scholar]
- 8.Kim J.C., Yu B., Lee Y.K. Influence of surface layer removal of shade guide tabs on the measured color by spectrophotometer and spectroradiometer. J. Dent. 2008;36:1061–1067. doi: 10.1016/j.jdent.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Lee S.H., Lee Y.K. Effect of thermocycling on optical parameters of resin composites by the brand and shade. Am. J. Dent. 2008;21:361–367. [PubMed] [Google Scholar]
- 10.Kongkiatkamon S., Booranasophone K., Tongtaksin A., Kiatthanakorn V., Rokaya D. Comparison of fracture load of the four translucent zirconia crowns. Molecules. 2021;26:5308. doi: 10.3390/molecules26175308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mandour M.H. Wear performance of three cad/cam monolithic restorations: Two-body wear and surface roughness. Egypt. Dent. J. 2017;63:1939–1953. doi: 10.21608/edj.2017.75172. [DOI] [Google Scholar]
- 12.Grech J., Antunes E. Zirconia in dental prosthetics: A literature review. J. Mater. Res. Technol. 2019;8:4956–4964. doi: 10.1016/j.jmrt.2019.06.043. [DOI] [Google Scholar]
- 13.Sorrentino R., Navarra C.O., Di Lenarda R., Breschi L., Zarone F., Cadenaro M., Spagnuolo G. Effects of finish line design and fatigue cyclic loading on phase transformation of zirconia dental ceramics: A qualitative micro-raman spectroscopic analysis. Materials. 2019;12:863. doi: 10.3390/ma12060863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alqurashi H., Khurshid Z., Syed A.U.Y., Rashid Habib S., Rokaya D., Zafar M.S. Polyetherketoneketone (pekk): An emerging biomaterial for oral implants and dental prostheses. J. Adv. Res. 2021;28:87–95. doi: 10.1016/j.jare.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Najeeb S., Zafar M.S., Khurshid Z., Siddiqui F. Applications of polyetheretherketone (peek) in oral implantology and prosthodontics. J. Prosthodont. Res. 2016;60:12–19. doi: 10.1016/j.jpor.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 16.Alexakou E., Damanaki M., Zoidis P., Bakiri E., Mouzis N., Smidt G., Kourtis S. Peek high performance polymers: A review of properties and clinical applications in prosthodontics and restorative dentistry. Eur. J. Prosthodont. Restor. Dent. 2019;27:113–121. doi: 10.1922/EJPRD_01892Zoidis09. [DOI] [PubMed] [Google Scholar]
- 17.Muhsin S.A., Hatton P.V., Johnson A., Sereno N., Wood D.J. Determination of polyetheretherketone (peek) mechanical properties as a denture material. Saudi Dent. J. 2019;31:382–391. doi: 10.1016/j.sdentj.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hallmann L., Mehl A., Sereno N., Hämmerle C.H.F. The improvement of adhesive properties of peek through different pre-treatments. Appl. Surf. Sci. 2012;258:7213–7218. doi: 10.1016/j.apsusc.2012.04.040. [DOI] [Google Scholar]
- 19.Stawarczyk B., Özcan M., Trottmann A., Schmutz F., Roos M., Hämmerle C. Two-body wear rate of cad/cam resin blocks and their enamel antagonists. J. Prosthet. Dent. 2013;109:325–332. doi: 10.1016/S0022-3913(13)60309-1. [DOI] [PubMed] [Google Scholar]
- 20.Tian Y., Chen C., Xu X., Wang J., Hou X., Li K., Lu X., Shi H., Lee E.-S., Jiang H.B. A review of 3D printing in dentistry: Technologies, affecting factors, and applications. Scanning. 2021;2021:9950131. doi: 10.1155/2021/9950131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Humagain M., Rokaya D. Integrating digital technologies in dentistry to enhance the clinical success. Kathmandu Univ. Med. J. (KUMJ) 2019;17:256–257. [PubMed] [Google Scholar]
- 22.Amornvit P., Rokaya D., Sanohkan S. Comparison of accuracy of current ten intraoral scanners. BioMed Res. Int. 2021;2021:2673040. doi: 10.1155/2021/2673040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khorsandi D., Fahimipour A., Abasian P., Saber S.S., Seyedi M., Ghanavati S., Ahmad A., De Stephanis A.A., Taghavinezhaddilami F., Leonova A., et al. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2021;122:26–49. doi: 10.1016/j.actbio.2020.12.044. [DOI] [PubMed] [Google Scholar]
- 24.Nesic D., Schaefer B.M., Sun Y., Saulacic N., Sailer I. 3D printing approach in dentistry: The future for personalized oral soft tissue regeneration. J. Clin. Med. 2020;9:2238. doi: 10.3390/jcm9072238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cardoso K.V., Adabo G.L., Mariscal-Muñoz E., Antonio S.G., Arioli Filho J.N. Effect of sintering temperature on microstructure, flexural strength, and optical properties of a fully stabilized monolithic zirconia. J. Prosthet. Dent. 2020;124:594–598. doi: 10.1016/j.prosdent.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Thoma D.S., Brandenberg F., Fehmer V., Knechtle N., Hämmerle C.H., Sailer I. The esthetic effect of veneered zirconia abutments for single-tooth implant reconstructions: A randomized controlled clinical trial. Clin. Implant Dent. Relat. Res. 2016;18:1210–1217. doi: 10.1111/cid.12388. [DOI] [PubMed] [Google Scholar]
- 27.Bathala L., Majeti V., Rachuri N., Singh N., Gedela S. The role of polyether ether ketone (peek) in dentistry—A review. J. Med. Life. 2019;12:5–9. doi: 10.25122/jml-2019-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Papathanasiou I., Kamposiora P., Papavasiliou G., Ferrari M. The use of peek in digital prosthodontics: A narrative review. BMC Oral Health. 2020;20:217. doi: 10.1186/s12903-020-01202-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Skirbutis G., Dzingutė A., Masiliūnaitė V., Šulcaitė G., Žilinskas J. A review of peek polymer’s properties and its use in prosthodontics. Stomatologija. 2017;19:19–23. [PubMed] [Google Scholar]
- 30.Mamidi N., Velasco Delgadillo R.M., Gonzáles Ortiz A., Barrera E.V. Carbon nano-onions reinforced multilayered thin film system for stimuli-responsive drug release. Pharmaceutics. 2020;12:1208. doi: 10.3390/pharmaceutics12121208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thiruchitrambalam M., Bubesh Kumar D., Shanmugam D., Jawaid M. A review on peek composites—Manufacturing methods, properties and applications. Mater. Today Proc. 2020;33:1085–1092. doi: 10.1016/j.matpr.2020.07.124. [DOI] [Google Scholar]
- 32.Han X., Yang D., Yang C., Spintzyk S., Scheideler L., Li P., Li D., Geis-Gerstorfer J., Rupp F. Carbon fiber reinforced peek composites based on 3D-printing technology for orthopedic and dental applications. J. Clin. Med. 2019;8:240. doi: 10.3390/jcm8020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu W., Geng P., Li G., Zhao D., Zhang H., Zhao J. Influence of layer thickness and raster angle on the mechanical properties of 3D-printed peek and a comparative mechanical study between peek and abs. Materials. 2015;8:5834–5846. doi: 10.3390/ma8095271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Q., Zhao W., Li Y., Yang W., Wang G. Flexural properties and fracture behavior of cf/peek in orthogonal building orientation by fdm: Microstructure and mechanism. Polymers. 2019;11:656. doi: 10.3390/polym11040656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Souza J.C.M., Pinho S.S., Braz M.P., Silva F.S., Henriques B. Carbon fiber-reinforced peek in implant dentistry: A scoping review on the finite element method. Comput. Methods Biomech. Biomed. Eng. 2021;24:1355–1367. doi: 10.1080/10255842.2021.1888939. [DOI] [PubMed] [Google Scholar]
- 36.Stawarczyk B., Taufall S., Roos M., Schmidlin P.R., Lümkemann N. Bonding of composite resins to peek: The influence of adhesive systems and air-abrasion parameters. Clin. Oral Investig. 2018;22:763–771. doi: 10.1007/s00784-017-2151-x. [DOI] [PubMed] [Google Scholar]
- 37.Chen S.G., Yang J., Jia Y.G., Lu B., Ren L. TiO2 and peek reinforced 3D printing pmma composite resin for dental denture base applications. Nanomaterials. 2019;9:1049. doi: 10.3390/nano9071049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aladağ A., Oğuz D., Çömlekoğlu M.E., Akan E. In vivo wear determination of novel cad/cam ceramic crowns by using 3D alignment. J. Adv. Prosthodont. 2019;11:120–127. doi: 10.4047/jap.2019.11.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim J.H., Lee S.J., Park J.S., Ryu J.J. Fracture load of monolithic cad/cam lithium disilicate ceramic crowns and veneered zirconia crowns as a posterior implant restoration. Implant Dent. 2013;22:66–70. doi: 10.1097/ID.0b013e318278a576. [DOI] [PubMed] [Google Scholar]
- 40.Heintze S.D., Eser A., Monreal D., Rousson V. Using a chewing simulator for fatigue testing of metal ceramic crowns. J. Mech. Behav. Biomed. Mater. 2017;65:770–780. doi: 10.1016/j.jmbbm.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 41.Park J.-Y., Bae S.-Y., Lee J.-J., Kim J.-H., Kim H.-Y., Kim W.-C. Evaluation of the marginal and internal gaps of three different dental prostheses: Comparison of the silicone replica technique and three-dimensional superimposition analysis. J. Adv. Prosthodont. 2017;9:159–169. doi: 10.4047/jap.2017.9.3.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zarone F., Russo S., Sorrentino R. From porcelain-fused-to-metal to zirconia: Clinical and experimental considerations. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2011;27:83–96. doi: 10.1016/j.dental.2010.10.024. [DOI] [PubMed] [Google Scholar]
- 43.Öztürk C., Can G. Effect of sintering parameters on the mechanical properties of monolithic zirconia. J. Dent. Res. Dent. Clin. Dent. Prospect. 2019;13:247–252. doi: 10.15171/joddd.2019.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Janyavula S., Lawson N., Cakir D., Beck P., Ramp L.C., Burgess J.O. The wear of polished and glazed zirconia against enamel. J. Prosthet. Dent. 2013;109:22–29. doi: 10.1016/S0022-3913(13)60005-0. [DOI] [PubMed] [Google Scholar]
- 45.Emera R., Altonbary G. Comparison between all zirconia, all peek, and zirconia-peek telescopic attachments for two implants retained mandibular complete overdentures: In vitro stress analysis study. J. Dent. Implant. 2019;9:24–29. doi: 10.4103/jdi.jdi_6_19. [DOI] [Google Scholar]
- 46.Kiliç V., Hürmüzlü F. Effect of light sources on bond strength of different composite resins repaired with bulk-fill composite. Odovtos-Int. J. Dent. Sc. 2021;23:103–115. [Google Scholar]
- 47.Zorba Y.O., Ilday N.O., Bayındır Y.Z., Demirbuga S. Comparing the shear bond strength of direct and indirect composite inlays in relation to different surface conditioning and curing techniques. Eur. J. Dent. 2013;7:436–441. doi: 10.4103/1305-7456.120679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yeo I.S., Lee J.H., Kang T.J., Kim S.K., Heo S.J., Koak J.Y., Park J.M., Lee S.Y. The effect of abutment screw length on screw loosening in dental implants with external abutment connections after thermocycling. Int. J. Oral Maxillofac. Implant. 2014;29:59–62. doi: 10.11607/jomi.3125. [DOI] [PubMed] [Google Scholar]
- 49.Evans J.G., Ley R.L.C., Barkmeier W.W. Resin bond strength to siliconated metal. J. Esthet. Dent. 1992;4:30–33. doi: 10.1111/j.1708-8240.1992.tb00651.x. [DOI] [Google Scholar]
- 50.Heintze S.D., Cavalleri A., Forjanic M., Zellweger G., Rousson V. A comparison of three different methods for the quantification of the in vitro wear of dental materials. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2006;22:1051–1062. doi: 10.1016/j.dental.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 51.Yılmaz E.C., Sadeler R. Investigation of three-body wear of dental materials under different chewing cycles. Sci. Eng. Compos. Mater. 2018;25:781–787. doi: 10.1515/secm-2016-0385. [DOI] [Google Scholar]
- 52.Diabb Zavala J.M., Leija Gutiérrez H.M., Segura-Cárdenas E., Mamidi N., Morales-Avalos R., Villela-Castrejón J., Elías-Zúñiga A. Manufacture and mechanical properties of knee implants using swcnts/uhmwpe composites. J. Mech. Behav. Biomed. Mater. 2021;120:104554. doi: 10.1016/j.jmbbm.2021.104554. [DOI] [PubMed] [Google Scholar]
- 53.Mamidi N., Delgadillo R.M.V., Castrejón J.V. Unconventional and facile production of a stimuli-responsive multifunctional system for simultaneous drug delivery and environmental remediation. Environ. Sci. Nano. 2021;8:2081–2097. doi: 10.1039/D1EN00354B. [DOI] [Google Scholar]
- 54.Rokaya D., Srimaneepong V., Sapkota J., Qin J., Siraleartmukul K., Siriwongrungson V. Polymeric materials and films in dentistry: An overview. J. Adv. Res. 2018;14:25–34. doi: 10.1016/j.jare.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mamidi N., Leija H.M., Diabb J.M., Lopez Romo I., Hernandez D., Castrejón J.V., Martinez Romero O., Barrera E.V., Elias Zúñiga A. Cytotoxicity evaluation of unfunctionalized multiwall carbon nanotubes-ultrahigh molecular weight polyethylene nanocomposites. J. Biomed. Mater. Res. A. 2017;105:3042–3049. doi: 10.1002/jbm.a.36168. [DOI] [PubMed] [Google Scholar]
- 56.Salernitano E., Migliaresi C. Composite materials for biomedical applications: A review. J. Appl. Biomater. Biomech. JABB. 2003;1:3–18. [PubMed] [Google Scholar]
- 57.Tibbitt M.W., Rodell C.B., Burdick J.A., Anseth K.S. Progress in material design for biomedical applications. Proc. Natl. Acad. Sci. USA. 2015;112:14444–14451. doi: 10.1073/pnas.1516247112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gou M., Chen H., Kang J., Wang H. Antagonist enamel wear of tooth-supported monolithic zirconia posterior crowns in vivo: A systematic review. J. Prosthet. Dent. 2019;121:598–603. doi: 10.1016/j.prosdent.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 59.Heimer S., Schmidlin P.R., Stawarczyk B. Discoloration of pmma, composite, and peek. Clin. Oral Investig. 2017;21:1191–1200. doi: 10.1007/s00784-016-1892-2. [DOI] [PubMed] [Google Scholar]
- 60.Wimmer T., Huffmann A.M., Eichberger M., Schmidlin P.R., Stawarczyk B. Two-body wear rate of peek, cad/cam resin composite and pmma: Effect of specimen geometries, antagonist materials and test set-up configuration. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2016;32:e127–e136. doi: 10.1016/j.dental.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 61.Aljanobi G., Al-Sowygh Z.H. The effect of thermocycling on the translucency and color stability of modified glass ceramic and multilayer zirconia materials. Cureus. 2020;12:e6968. doi: 10.7759/cureus.6968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sarıkaya I., Hayran Y. Effects of dynamic aging on the wear and fracture strength of monolithic zirconia restorations. BMC Oral Health. 2018;18:146. doi: 10.1186/s12903-018-0618-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bajraktarova-Valjakova E., Korunoska-Stevkovska V., Kapusevska B., Gigovski N., Bajraktarova-Misevska C., Grozdanov A. Contemporary dental ceramic materials, a review: Chemical composition, physical and mechanical properties, indications for use. Open Access Maced. J. Med. Sci. 2018;6:1742–1755. doi: 10.3889/oamjms.2018.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Qorri E., Gashi-Cenkoglu B., Propris F., Karabudak I. The use of biohpp (high performance polymer) as superstructure material in oral implantology. Clin. Oral Implant. Res. 2018;29:351. doi: 10.1111/clr.236_13358. [DOI] [Google Scholar]
- 65.Mirchandani B., Zhou T., Heboyan A., Yodmongkol S., Buranawat B. Biomechanical aspects of various attachments for implant overdentures: A review. Polymers. 2021;13:3248. doi: 10.3390/polym13193248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Daou E.E. The zirconia ceramic: Strengths and weaknesses. Open Dent. J. 2014;8:33–42. doi: 10.2174/1874210601408010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Caracostea Objelean A., Labunet A., Silaghi-Dumitrescu L., Moldovan M., Sava S., Badea M.E. In vitro chewing simulation model influence on the adhesive-tooth structure interface. Key Eng. Mater. 2016;695:77–82. doi: 10.4028/www.scientific.net/KEM.695.77. [DOI] [Google Scholar]
- 68.Heintze S.D., Zellweger G., Grunert I., Muñoz-Viveros C.A., Hagenbuch K. Laboratory methods for evaluating the wear of denture teeth and their correlation with clinical results. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2012;28:261–272. doi: 10.1016/j.dental.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 69.Juntavee N., Attashu S. Effect of different sintering process on flexural strength of translucency monolithic zirconia. J. Clin. Exp. Dent. 2018;10:e821–e830. doi: 10.4317/jced.54749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Heboyan A., Manrikyan M., Zafar M.S., Rokaya D., Nushikyan R., Vardanyan I., Vardanyan A., Khurshid Z. Bacteriological evaluation of gingival crevicular fluid in teeth restored using fixed dental prostheses: An in vivo study. Int. J. Mol. Sci. 2021;22:5463. doi: 10.3390/ijms22115463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shen Y.X., Tang W.Z. Analysis of vita shade guide with spectrophotometer under different color measurement conditions. Acad. J. Second. Mil. Med. Univ. 2015;36:100–102. doi: 10.3724/SP.J.1008.2015.00100. [DOI] [Google Scholar]
- 72.Avetisyan A., Markaryan M., Rokaya D., Tovani-Palone M.R., Zafar M.S., Khurshid Z., Vardanyan A., Heboyan A. Characteristics of periodontal tissues in prosthetic treatment with fixed dental prostheses. Molecules. 2021;26:1331. doi: 10.3390/molecules26051331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Heboyan A., Syed A.U.Y., Rokaya D., Cooper P.R., Manrikyan M., Markaryan M. Cytomorphometric analysis of inflammation dynamics in the periodontium following the use of fixed dental prostheses. Molecules. 2020;25:4650. doi: 10.3390/molecules25204650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kozmacs C., Hollmann B., Arnold W.H., Naumova E., Piwowarczyk A. Polishing of monolithic zirconia crowns-results of different dental practitioner groups. Dent. J. 2017;5:30. doi: 10.3390/dj5040030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chavali R., Lin C.P., Lawson N.C. Evaluation of different polishing systems and speeds for dental zirconia. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2017;26:410–418. doi: 10.1111/jopr.12396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Heboyan A., Manrikyan M., Markaryan M., Vardanyan I. Changes in the parameters of gingival crevicular fluid in masticatory function restoration by various prosthodontic constructions. Int. J. Pharm. Res. 2020;12:2088–2093. [Google Scholar]
- 77.AlGhazali N., Burnside G., Smith R.W., Preston A.J., Jarad F.D. Performance assessment of vita easy shade spectrophotometer on colour measurement of aesthetic dental materials. Eur. J. Prosthodont. Restor. Dent. 2011;19:168–174. [PubMed] [Google Scholar]
- 78.Kalantari M.H., Ghoraishian S.A., Mohaghegh M. Evaluation of accuracy of shade selection using two spectrophotometer systems: Vita easyshade and degudent shadepilot. Eur. J. Dent. 2017;11:196–200. doi: 10.4103/ejd.ejd_195_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Linjawi A.I., Abbassy M.A. Comparison of shear bond strength to clinically simulated debonding of orthodontic brackets: An in vitro study. J. Orthod. Sci. 2016;5:25–29. doi: 10.4103/2278-0203.176655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Salem S.K. Wear and microhardness of three different types of cad/cam ceramic materials. Egypt Dent. J. 2019;65:2857–2866. doi: 10.21608/edj.2019.72682. [DOI] [Google Scholar]
- 81.Bolaca A., Erdogan Y. In vitro evaluation of the wear of primary tooth enamel against different ceramic and composite resin materials. Niger. J. Clin. Pract. 2019;22:313–319. doi: 10.4103/njcp.njcp_358_18. [DOI] [PubMed] [Google Scholar]
- 82.Scribante A., Bollardi M., Chiesa M., Poggio C., Colombo M. Flexural properties and elastic modulus of different esthetic restorative materials: Evaluation after exposure to acidic drink. BioMed Res. Int. 2019;2019:5109481. doi: 10.1155/2019/5109481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Alrahlah A., Khan R., Al-Odayni A.-B., Saeed W.S., Bautista L.S., Vohra F. Evaluation of synergic potential of rgo/sio2 as hybrid filler for bisgma/tegdma dental composites. Polymers. 2020;12:3025. doi: 10.3390/polym12123025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rizo-Gorrita M., Herráez-Galindo C., Torres-Lagares D., Serrera-Figallo M., Gutiérre-Pérez J.L. Biocompatibility of polymer and ceramic cad/cam materials with human gingival fibroblasts (hgfs) Polymers. 2019;11:1446. doi: 10.3390/polym11091446. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding authors.