Abstract
Background
Eleven states have instituted laws allowing recreational cannabis use leading to growing public health concerns surrounding the effects of cannabis intoxication on driving safety. We hypothesized that after the 2016 legalization of cannabis in California, the use among vehicular injury patients would increase and be associated with increased injury severity.
Methods
San Diego County’s five adult trauma center registries in were queried from January 2010 to June 2018 for motor vehicle or motorcycle crash patients with completed toxicology screens. Patients were stratified as toxicology negative (TOX−), positive for only THC (THC+), only blood alcohol >0.08% (ETOH+), THC+ETOH, or THC+ with any combination with methamphetamine or cocaine (M/C). County medical examiner data were reviewed to characterize THC use in those with deaths at the scene of injury.
Results
Of the 11,491 patients identified, there were 61.6% TOX−, 11.7% THC+, 13.7% ETOH+, 5.0% THC+ETOH, and 7.9% M/C. THC+ increased from 7.3% to 14.8% over the study period and peaked at 14.9% post-legalization in 2017. Compared with TOX− patients, THC+ patients were more likely to be male and younger. THC+ patients were also less likely to wear seatbelts (8.5% vs 14.3%, p<0.001) and had increased mean Injury Severity Score (8.4±9.4 vs 9.0±9.9, p<0.001) when compared with TOX− patients. There was no difference in in-hospital mortality between groups. From the medical examiner data of the 777 deaths on scene, 27% were THC+.
Discussion
THC+ toxicology screens in vehicular injury patients peaked after the 2016 legalization of cannabis. Public education on the risks of driving under the influence of cannabis should be a component of injury prevention initiatives.
Level of evidence
III, Prognostic
Keywords: toxicology, injury prevention
Background
Of the 33 states in the USA that have legalized marijuana, 11 have instituted laws allowing for use of recreational cannabis. In these states, cannabis use has increased significantly compared with states that have not legalized cannabis.1 There is evidence showing that cannabis has therapeutic properties in the treatment of chronic pain, as an antiemetic in the treatment of chemotherapy-induced nausea and vomiting, and for improving patient-reported multiple sclerosis spasticity symptoms.2–4 Further, as recreational and medicinal cannabis becomes more popular, it is increasingly viewed as harmless.5 6 However, cannabis use can lead to impairment of learning, memory, and attention.2 7–12
Recent evidence suggests that there may be an association between cannabis use and an increased risk of motor vehicle crashes.2 13 14 Several studies have demonstrated an association between cannabis intoxication and impaired driving ability, as well as increased risk of motor vehicle crashes, fatal collisions, and driver culpability.15–18 A study conducted in Hawaii demonstrated that THC-positive patients were less likely to use protective devices.19 Cannabis positivity in trauma patients has also been shown to be associated with increased hospital length of stay, intensive care unit days, ventilator days, and a greater number of operative interventions.20 21 Conversely, studies by Movig and Longo reported that marijuana intoxication may not even be associated with an increased risk of motor vehicle crashes.22 23
In 2016, the recreational use of cannabis was legalized in California. With a lack of consensus on the risks related to operating a vehicle while under the influence of cannabis, and increasing legalization, it is imperative to define the relationship between cannabis use and vehicular crashes. The goal of this study is to describe, among those patients undergoing toxicology screening, the prevalence of cannabis positivity after vehicular crashes in San Diego County and to assess associations between cannabis use and outcomes in injured patients. We hypothesized that after the 2016 legalization, cannabis use would increase in vehicular injury patients and be associated with increased injury severity.
Methods
Five San Diego County trauma center registries were queried from January 2010 to June 2018 for motor vehicle (MVC) or motorcycle crash (MCC) patients with completed toxicology screens. All patients 16 years and older meeting these criteria were included in the study. For the purposes of this study, toxicology screening constituted having both blood and urine results completed. A blood alcohol level of >0.08% was considered positive and any urine toxicology positive for THC was consider positive. Patients were stratified into five groups: negative blood alcohol and urine screening (TOX−), THC positive only (THC+), alcohol positive only (ETOH+), THC and alcohol positive (THC+ETOH), or anyone who tested positive for any combination of toxicology with methamphetamine or cocaine (M/C). Annual toxicology screening rates were obtained from each of the five participating trauma centers. Of note, routine urine toxicology screening included THC, methamphetamines and cocaine at all institutions over the entire study period.
Patient variables included admission age, sex, and race/ethnicity. The data point “race/ethnicity” includes race and ethnicity combined into one categorical data point. Within the dataset, the category Asian/other includes the races Asians, Pacific Islanders, American Indians, and Alaskan Natives; Black includes non-Hispanic Blacks; Hispanic includes race defined as other with Hispanic ethnicity; White includes Non-Hispanic Whites; and Unknown is no race or ethnicity listed. Age and sex were reported as ascribed in the electronic health record. Injury-related data collected included date of injury, mechanism of injury (MVC or MCC), protective equipment (seatbelt and helmet use), and Injury Severity Score (ISS). Additional variables collected included operations and in-hospital mortality.
In addition, San Diego County medical examiner data from 2011 to 2018 were acquired to analyze THC positivity in people who died at the scene of vehicular crashes (MVC or MCC). Patient demographics (age, sex, race) and year of injury were also acquired. This dataset was analyzed separately from the hospital datasets.
The year 2010 was not available from the medical examiner, which is why the dates do not align with the trauma center dataset. However, we chose to include the additional year in the hospital dataset to increase the ability to show trends over time in relation to cannabis legislation and outcomes. The ability to demonstrate differences in the positive outcomes for this study increased with more patients included in our sample.
Ethics
Institutional Review Board (IRB) approval and data use agreements were obtained for all sites. The University of California, San Diego Human Research Protections Program, ID#1 81 506X, served as the central IRB for all centers including UC San Diego School of Medicine and Palomar Medical Center. Additional approvals were obtained for Scripps Hospitals by the Scripps IRB, IRB-15-6721, and Sharp Memorial through the Sharp Center for Research IRB #1912801. This study was approved as exempt from requiring individual patient consent due to the minimal risk and retrospective nature of the study.
Statistical analysis
The cohort as a whole was described with basic summations and percentages. To examine for potential predictors of THC+ toxicology, univariate analyses were performed. Age and ISS are skewed hence represented by median values with IQRs;, Kruskal-Wallis non-parametric test was used to assess differences in the ISS and age between the study groups. For Kruskal-Wallis analyses, post hoc pairwise comparisons were performed with Bonferroni correction for multiple tests. Pearson χ2 was used to assess for differences between groups for categorical variables sex, race, mechanism, use of safety devices, operative interventions, and mortality. Using TOX− as the reference group, binomial logistic regressions were used to characterize the association of THC positivity differences between study groups adjusting for other variables in the model; including for sex, mechanism, seatbelt use, helmet use, operative interventions and mortality.
Multivariate logistic regression was used to assess for toxicology results as predictors of our primary outcome measure injury severity. ISS of 1–8 was used as the reference range to compare the subgroup ISS ranges of 9–14, 15–25, and >25. TOX− was the reference group for the toxicology+subgroups.
Pearson correlations were used to assess differences in any THC positivity rate over time in increments of months as well as before and after legislation in 2016. Time-series regression analysis was performed to further assess the significance. To assess the impact of the January 2016 legalization on THC use over time, a linear regression was performed to assess percent positivity by including an interaction term for pre/post legislation by month.
Statistical analysis was conducted using SPSS Statistics V.26.0.0.0.
Results
Trauma center data
There were 11,491 patients from five trauma centers included in the study who had toxicology screening performed at admission. Overall, the average rate of toxicology screening during the study period was 59.4% SD 3.3%. This rate changed during the course of the study, starting at 58.7% in 2010 with a steep increase to 67.0% in 2018. However, the intervening years had minimal change compared with the 2010 rate of 58.7%, ranging from screening rates of 56.8% to 60.7%. Vehicular injury patients included in the study were predominantly male (65.5%) with 73.5% involved in an MVC and 26.5% MCC (table 1).
Table 1.
Cohort demographics
| Characteristic | Number of patients | |
| Total no | 11,491 | |
| Age (median/LQ–UQ) | 34 | 24–51 |
| Sex (male) | 7427 | 65.5% |
| Race/ethnicity | ||
| Asian/other | 1518 | 13.2% |
| Black | 968 | 8.4% |
| Hispanic | 3814 | 33.2% |
| Unknown | 245 | 2.1% |
| White | 4945 | 43.0% |
| Mechanism | ||
| MV occupant | 8443 | 73.5% |
| Seatbelt | 6512 | 77.1% |
| No seatbelt | 1023 | 12.1% |
| Other/unknown | 908 | 10.8% |
| Motorcycle | 3048 | 26.5% |
| Helmet | 2697 | 88.5% |
| No helmet | 281 | 9.2% |
| Unknown | 70 | 2.3% |
| ISS (median/LQ–UQ) | 5 | 2–11 |
| ICU admissions | 2412 | 21% |
| Operations | 2950 | 25.7% |
| Outcome (mortality) | 170 | 1.5% |
ICU, intensive care unit; ISS, Injury Severity Score; LOS, length of stay; MV, motor vehicle.
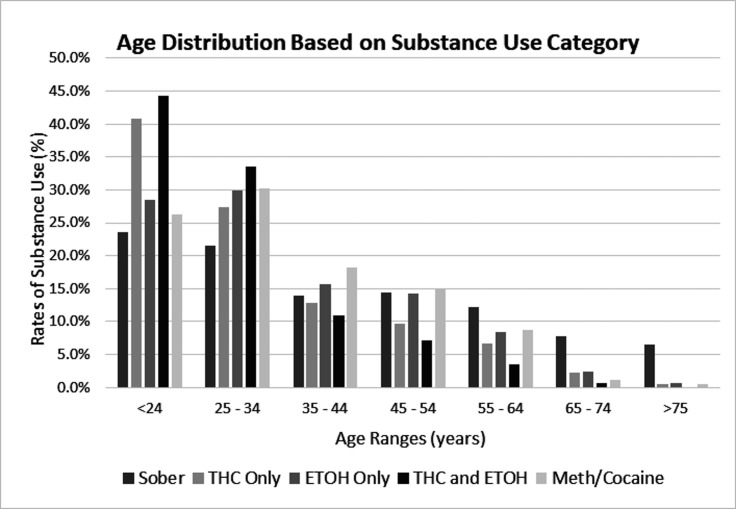
Toxicology screening found that 61.6% were identified as TOX−, 11.7% THC+, 13.7% ETOH+, 5.0% THC +ETOH, and 7.9% M/C. Compared with TOX− patients with a median age of 38 years (LQ–UQ 25–56), THC+ patients were younger with a median age of 27 years (LQ–UQ 21–39), p<0.001. The highest proportion of patients under the age of 35 were in the THC+ and THC+ETOH groups (68.2% and 77.9%, respectively), which are both significantly higher than TOX– patients under the age of 35 at 45.1%, p<0.001. Figure 1 depicts the age distribution for all subgroups, with youngest patients in the THC+ and THC +ETOH groups. THC + patients were also more likely to be male than TOX– patients (74.0% vs 59.7%; p<0.001). Across all groups, White patients were the most prevalent, followed by Hispanic then Black; the distributions within the different toxicology study groups can be found in table 2.
Figure 1.
Age distribution for all toxicology subgroups.
Table 2.
Patient demographic by toxicology screen classification
| Characteristic | TOX–† | THC only | ETOH only | THC and ETOH | Cocaine/meth | |||||
| Total no | 7078 | 61.6% | 1345 | 11.7% | 1580 | 13.7% | 578 | 5.0% | 910 | 7.9% |
| Age (median/LQ–UQ) | 28 | 25–56 | 27 | 21–39* | 31 | 24–45* | 26 | 22–33* | 32 | 24–45* |
| Sex (male) | 4224 | 59.7% | 995 | 74.0%* | 1076 | 68.1%* | 445 | 77.0%* | 687 | 75.5%* |
| Race/ethnicity | ||||||||||
| Asian/other | 1074 | 15.2% | 150 | 11.2% | 166 | 10.5% | 61 | 10.6% | 67 | 7.4% |
| Black | 520 | 7.3% | 160 | 11.9% | 126 | 8.0% | 54 | 9.3% | 108 | 11.9% |
| Hispanic | 2376 | 33.6% | 382 | 28.4% | 539 | 34.1% | 182 | 31.5% | 335 | 36.8% |
| White | 2967 | 41.9% | 615 | 45.7% | 716 | 45.3% | 261 | 45.2% | 386 | 42.4% |
| Unknown | 141 | 2.0% | 38 | 2.8% | 32 | 2.0% | 20 | 3.5% | 14 | 1.5% |
| Mechanism | ||||||||||
| MV occupant | 5052 | 71.4% | 891 | 66.2%* | 1323 | 83.7%* | 483 | 83.6%* | 694 | 76.3%* |
| Seatbelt | 4185 | 82.8% | 677 | 76.0%* | 878 | 66.4%* | 310 | 64.2%* | 462 | 66.6%* |
| No seatbelt | 429 | 8.5% | 127 | 14.3%* | 236 | 17.8%* | 98 | 20.3%* | 133 | 19.2%* |
| Unknown | 438 | 8.7% | 87 | 9.8%* | 209 | 15.8%* | 75 | 15.5%* | 99 | 14.3%* |
| Motorcycle | 2026 | 28.6% | 454 | 33.8% | 257 | 16.3% | 95 | 16.4% | 216 | 23.7% |
| Helmet | 1821 | 89.9% | 402 | 88.5% | 219 | 85.2%* | 81 | 85.3%* | 174 | 80.6%* |
| No helmet | 157 | 7.7% | 39 | 8.6% | 35 | 13.6%* | 14 | 14.7%* | 36 | 16.7%* |
| Unknown | 48 | 2.4% | 13 | 2.9% | 3 | 1.2%* | 0 | 0.0%* | 6 | 2.8%* |
| ISS (median/LQ–UQ) | 5 | 2–10 | 5 | 2–11* | 5 | 2–12* | 5 | 3–14* | 6 | 4–13* |
| Operations | 1685 | 24% | 376 | 28%* | 399 | 25.3% | 164 | 28.4%* | 326 | 35.8%* |
| Mortality | 111 | 1.6% | 18 | 1.3% | 18 | 1.1% | 11 | 1.9% | 12 | 1.3% |
*p<0.05.
†TOX– is the reference category.
ISS, Injury Severity Score.
THC+ patients were more likely than TOX– to be in a MCC (33.8% vs 28.6%, p<0.001) and less likely to wear a helmet (7.7% vs 8.6%, p=0.053). In addition, in comparison with TOX– patients, THC+ patients were less likely to wear seatbelts (8.5% vs 14.3%, p<0.001). There was no difference in in-hospital mortality. The comparisons of mechanism of injury, seatbelt use, helmet use, ISS, and operations for TOX– patient with all other toxicology subgroups are listed in table 2.
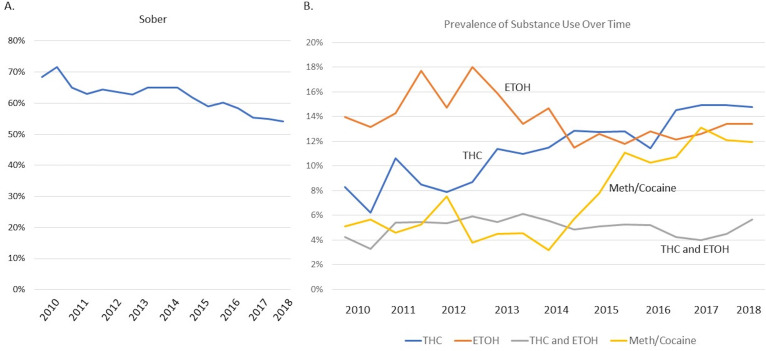
The semiannual percentage of TOX– patients decreased during the study period from 68.4% to 54.2% (figure 2A). THC+ and M/C increased during the study period with the percentage of THC+ patients increasing from 7.3% in 2010 to 14.8% in 2018. The percentage of THC+ETOH patients remained consistent over (figure 2B). THC positivity in the entire study population was assessed in a time-series analysis and demonstrated an increased Pearson correlation coefficient after legislation in 2016 (0.591, p<0.001), suggesting an increase in use over time. The Pearson correlation coefficient for increased THC positivity on a monthly basis is even stronger at 0.723, p<0.001 (R2 for the time series=0.523). Time-series linear regression demonstrates an increase per month of 0.125% (B=0.125) or 1.5% increase each year, p>0.001, demonstrating THC+ toxicology significantly increased during the study period. To assess the impact of THC legalization in January 2016 on THC positivity, a linear regression using an interaction term for pre/post legislation by month was performed. However, there was not a significant differential change in the rate of THC+ toxicology after the 2016 legislation, B=0.683, p=0.923 (R2=0.524). In summary, these data demonstrate a persistent and significant increase in THC+ rates over time; however, this rate was not accelerated by legalization.
Figure 2.
Distribution of toxicology results per year, depicting the change in positivity by subgroups: TOX–, THC+, ETOH+, THC +ETOH, and M/C.
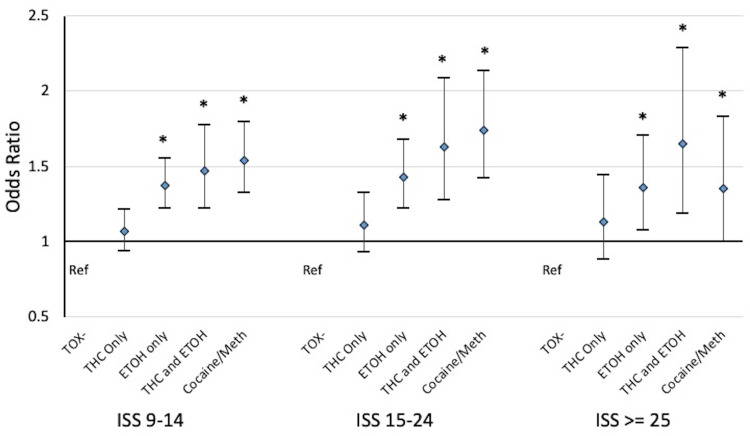
Multivariate analysis of ISS, using ISS 1–8 as the reference range to ISS 9–14, ISS 15–24, and ISS ≥25, did not demonstrate THC + compared with TOX– to be an independent predictor after adjusting for sex, age, race, year, payor, mechanism, and institution. However, ETOH+, THC +ETOH, and M/C subgroups all had increased odds of ISS 9–14, 15–24, and ≥25 when compared with TOX– patients (figure 3). The AUOC for each regression analysis is as follows: ISS 9–14=0.666, ISS 15–24=0.694, and ISS ≥25=0.712.
Figure 3.
Odds of increased injury severity for intoxicated patients compared with toxicology-negative patients. Each ISS category is compared with ISS 1–8 and the regressions are adjusted for age, gender, race, year of admission, payor, mechanism, and institution. *p>0.05. Ref, reference category.
Medical examiner data
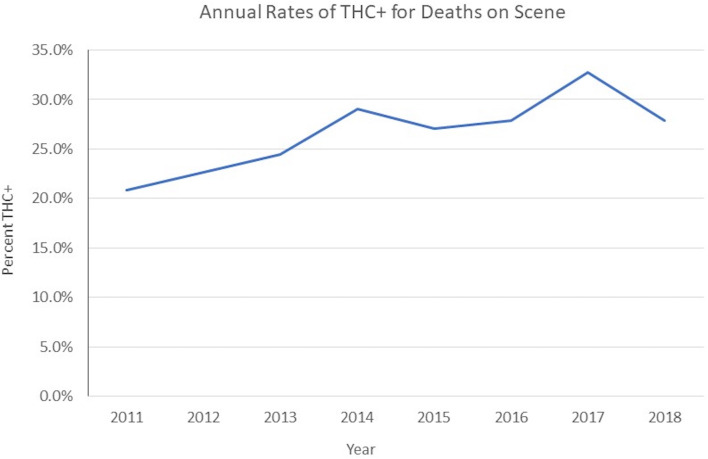
Data from the San Diego County Medical Examiner demonstrated 777 deaths at the scene during the study period; of those patients, 26.6% were THC+. The THC + people were significantly younger, more likely to be male, and in an MVC (table 3). The annual incidence of THC associated with deaths at the scene for MVC/MCC trended up from 20.8% in 2011 to 27.9% in 2018 with a peak in 2017 at 32.7% (figure 4).
Table 3.
Deaths on scene by THC positivity
| THC– | THC+ | P value | |||
| Total no | 570 | 73.4% | 207 | 26.6% | |
| Age (median/LQ–UQ) | 35 | 24–54 | 27 | 22–37 | <0.001 |
| Sex (male) | 425 | 74.6% | 178 | 86.0% | <0.001 |
| Race/ethnicity | <0.001 | ||||
| Asian/other | 52 | 9.1% | 9 | 4.3% | |
| Black | 36 | 6.3% | 21 | 10.1% | |
| Hispanic | 182 | 31.9% | 45 | 21.7% | |
| White | 277 | 48.6% | 118 | 57.0% | |
| Other | 23 | 4.0% | 14 | 6.8% | |
| Mechanism | <0.001 | ||||
| MV occupant | 383 | 67.2% | 158 | 76.3% | |
| Motorcycle | 187 | 32.8% | 49 | 23.7% | |
Figure 4.
Rate of cannabis positivity per year for deaths on scene after vehicular crashes.
Discussion
Cannabis positive toxicology screens are increasing in vehicular injury patients admitted to the five trauma centers that participated in this study. Patients testing positive for cannabis were younger, less likely to wear seatbelts, and had elevated ISS compared with TOX– vehicular injury patients. Our seven-and-a-half-year study period allows for close analysis of trends in trauma patients through changes in legislation. Although the changes are likely multifactorial, the peak in THC+ trauma patients the year after recreational cannabis legalization in 2016 demonstrates that changes in legislation related to the legality and availability of cannabis likely has an impact on drug usage trends. The impact of legalization on drug use trends has been previously seen in California with the legalization of medical marijuana in 2006 being associated with an increase in cannabinoid prevalence in drivers in fatal accidents after accounting for national trends in driver cannabinoid prevalence.24
Recent evidence suggests that states that legally permit medical cannabis dispensaries experience an increase in use prevalence among adults aged 21 years and older as well as an increase in average THC levels.25 A study conducted in Washington state found the proportion of THC + daytime drivers increased from 8% before retail sales to 23% 6 months after retail sales.26 Similarly, an analysis of trauma admissions in Colorado found that marijuana detection on urine drug screen increased significantly in the years after legalization.27
In this report, we analyzed how the toxicology reports of trauma patients correlated with mechanism of injury and how the results of these drug screenings impacted injury severity. We surveyed data from the five adult trauma centers that compose the San Diego County Trauma System. These trauma centers serve individuals from a wide range of socioeconomic and demographic backgrounds. THC + patients were more likely to be young males and were less likely to wear seatbelts, which is in agreement with the characteristics of THC + patients described in similar reports.20 Overall, THC or any other positive toxicology was associated with an increased ISS compared with TOX–, although the odds of having an increased ISS was higher in the THC +ETOH patients than ETOH + patients for all ISS categories. This suggests that the combined use of alcohol and THC may have a synergistic effect on driver impairment, translating to worse injuries.14 28
The use of medical cannabis in our study population is unknown. However, a study on a cohort of young individuals in LA found fewer individuals were medical cannabis patients after legalization.29 As our study population was similarly young, it is reasonable to think that an increase in medical cannabis use did not account for the rise in THC+ patients. In addition, the significance of medical versus non-medical use does not impact our findings as the possession of a medical marijuana card does not correlate with driving under the influence of cannabis.30
There is an unclear link between the concordant rise of M/C+ patients and the rise of THC + patients found in our study. Previous studies have suggested cannabis use predicts the use of illicit drug use; however, recreational marijuana legalization in Colorado and Washington was not associated with an increase in substance use disorder treatment admission.31 32 There may be local-regional reasons why this occurred in our study including our regional increasing homeless population, drug trafficking, and a known epidemic of methamphetamine use just across the border from us.33 34 Further studies are needed to understand this correlation.
Although there was a persistent and significant increase in THC+ rates over time, this rate was not accelerated after legalization and in fact in our series appears to plateau. The impacts of legalization are influenced by information diffusion which begins during the arduous process of legalization. By the time the law was enacted, individual behaviors may have already changed, explaining the plateau.35
The long-term impact of legalization on THC+ trauma patients is difficult to predict as studies on the association between cannabis laws and cannabis use have reported inconsistent results.36 Regardless, the nearly doubling in THC+ patients during our study period is concerning as THC+ drivers put themselves and everyone else on the road in danger. THC can impair critical abilities necessary for safe driving, including slowed reaction time, problems with road tracking, lane position variability, and decreased cognitive performance and executive functions as well as divided attention.37
Data from the San Diego County Medical Examiner were analyzed to evaluate the extent of THC+ toxicology in patients who died at the scene of injury. We found that during the entire study period, 26.6% of deaths at the scene of injury had THC+ toxicology. This cohort of fatalities is important to analyze as they are not represented in mortality data from individual trauma centers. A previous study analyzed the effect of marijuana legalization on MVC fatalities in Washington and Colorado, finding that crash fatality rates did not differ from states that had not legalized marijuana.38 Medical Examiner data also demonstrated that there was an association between THC+ vehicular deaths and a younger, predominantly male population. The young male population is known to engage in more per-capita violations and experience more per-capita injuries and fatalities than older cohorts and females.39
Limitations of this study include the lack of a legal threshold for driver impairment while under the influence of cannabis. In addition, cannabinoids can exist in the blood stream for several days after drug discontinuation in heavy cannabis users, and it is unknown what impact these residual levels have on the user’s physiological profile and level of impairment.40 41 For those patients who did have positive toxicology, we do not have data regarding timing of use and the crashes. Not all patients had a toxicology screen performed, and there was variability in the screening rates between institutions. These institutional differences, combined with the variation in toxicology screening over time, introduce the risk of selection bias which could have influenced these outcomes making generalization of these results difficult. Finally, motor vehicle and motorcycle crash injuries have the potential for different injury patterns and severity, and combining these mechanisms to assess roadway vehicular crashes could have influenced these outcomes. A larger prospective study would overcome many of these limitations and be the ideal way to study the association of cannabis use with vehicular crashes and injury severity.
These data should be used to fuel injury prevention initiatives starting with targeted public education, focusing on the under 35 age group, who are at the highest risk for being under the influence of cannabis at the time of injury. Educational campaigns should focus on the risks of driving under the influence of any substance, including cannabis, which may be negatively synergistic with other intoxicants. It is key that drug testing is developed for law enforcement to be able to screen for cannabis use in the field, facilitating their ability to enforce policy regarding driving intoxicated. Further studies are needed to address the question of how positive toxicology screens relate to timing of cannabis use, cannabis levels in the blood, and the relation of those blood levels to acute intoxication and impairment. Studies like these are important for increasing awareness of the dangers associated with cannabis use.
Footnotes
Presented at: This manuscript was presented at the 50th Annual Meeting of the Western Trauma Association, February 23-28, 2020 in Sun Valley, Idaho.
Contributors: JMB: data acquisition and analysis, interpretation of data, drafting of article. TWC: study design, data analysis and interpretation, drafting of article and critical revision. AMS: data acquisition, analysis and interpretation, critical revision of article. LR: data acquisition, interpretation of data, drafting of article. RS: data acquisition, critical revision of article. JS: data acquisition, critical revision of article. DW: data acquisition, critical revision of article. VB: data acquisition, critical revision of article. WLB: data acquisition, drafting of article and critical revision. LNG:
overall content and guarantor, study design, data analysis and interpretation, drafting of article and critical revision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Hasin DS, Sarvet AL, Cerdá M, Keyes KM, Stohl M, Galea S, Wall MM, et al. US adult illicit cannabis use, cannabis use disorder, and medical marijuana laws: 1991–1992 to 2012–2013. JAMA Psychiatry 2017;74:579–88. 10.1001/jamapsychiatry.2017.0724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.InCommittee on the Health Effects of Marijuana: An Evidence Review and Research Agenda. Board on Population Health and Public Health Practice. Health and Medicine Division. National Academies of Sciences, Engineering, and Medicine . The health effects of cannabis and cannabinoids. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington, D.C: The National Academies Press, 2017. 10.17226/24625 [DOI] [PubMed] [Google Scholar]
- 3.Koppel BS, Brust JCM, Fife T, Bronstein J, Youssof S, Gronseth G, Gloss D, et al. Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 2014;82:1556–63. 10.1212/WNL.0000000000000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, Keurentjes JC, Lang S, Misso K, Ryder S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA 2015;313:2456–73. 10.1001/jama.2015.6358. [DOI] [PubMed] [Google Scholar]
- 5.Carliner H, Brown QL, Sarvet AL, Hasin DS. Cannabis use, attitudes, and legal status in the U.S.: a review. Prev Med 2017;104:13–23. 10.1016/j.ypmed.2017.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berg CJ, Stratton E, Schauer GL, Lewis M, Wang Y, Windle M, Kegler M, et al. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Subst Use Misuse 2015;50:79–89. 10.3109/10826084.2014.958857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tashkin DP. Marijuana and lung disease. Chest 2018;154:653–63. 10.1016/j.chest.2018.05.005 [DOI] [PubMed] [Google Scholar]
- 8.Batalla A, Bhattacharyya S, Yücel M, Fusar-Poli P, Crippa JA, Nogué S, Torrens M, Pujol J, Farré M, Martin-Santos R. Structural and functional imaging studies in chronic cannabis users: a systematic review of adolescent and adult findings. PLoS One 2013;8:e55821. 10.1371/journal.pone.0055821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Broyd SJ, van Hell HH, Beale C, Yücel M, Solowij N. Acute and chronic effects of cannabinoids on human cognition—a systematic review. Biol Psychiatry 2016;79:557–67. 10.1016/j.biopsych.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 10.Schreiner AM, Dunn ME. Residual effects of cannabis use on neurocognitive performance after prolonged abstinence: a meta-analysis. Exp Clin Psychopharmacol 2012;20:420–9. 10.1037/a0029117. [DOI] [PubMed] [Google Scholar]
- 11.Martín-Santos R, Fagundo AB, Crippa JA, Atakan Z, Bhattacharyya S, Allen P, Fusar-Poli P, Borgwardt S, Seal M, Busatto GF, et al. Neuroimaging in cannabis use: a systematic review of the literature. Psychol Med 2010;40:383–98. 10.1017/S0033291709990729. [DOI] [PubMed] [Google Scholar]
- 12.Grant I, Gonzalez R, Carey CL, Natarajan L, Wolfson T, et al. Non-acute (residual) neurocognitive effects of cannabis use: a meta-analytic study. J Int Neuropsychol Soc 2003;9:679–89. 10.1017/S1355617703950016. [DOI] [PubMed] [Google Scholar]
- 13.Rogeberg O, Elvik R. The effects of cannabis intoxication on motor vehicle collision revisited and revised. Addiction 2016;111:1348–59. 10.1111/add.13347. [DOI] [PubMed] [Google Scholar]
- 14.Sewell RA, Poling J, Sofuoglu M. The effect of cannabis compared with alcohol on driving. Am J Addict 2009;18:185–93. 10.1080/10550490902786934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lenné MG, Dietze PM, Triggs TJ, Walmsley S, Murphy B, Redman JR. The effects of cannabis and alcohol on simulated arterial driving: influences of driving experience and task demand. Accid Anal Prev 2010;42:859–66. 10.1016/j.aap.2009.04.021 [DOI] [PubMed] [Google Scholar]
- 16.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ 2012;344:e536. 10.1136/bmj.e536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rogeberg O, Elvik R, White M. Correction to: “The effects of cannabis intoxication on motor vehicle collision revisited and revised” (2016). Addiction 2018;113:967–9. 10.1111/add.14140. [DOI] [PubMed] [Google Scholar]
- 18.Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem 2013;59:478–92. 10.1373/clinchem.2012.194381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steinemann S, Galanis D, Nguyen T, Biffl W, et al. Motor vehicle crash fatalaties and undercompensated care associated with legalization of marijuana. J Trauma Acute Care Surg 2018;85:566–71. 10.1097/TA.0000000000001983. [DOI] [PubMed] [Google Scholar]
- 20.Banks K, Biswas S, Wong M, Byerly S, Clark D, Lam L, Inaba K, Demetriades D. Cannabis use is associated with increased mechanical ventilation and polysubstance use in trauma patients. Am Surg 2019;85:226–9. 10.1177/000313481908500234 [DOI] [PubMed] [Google Scholar]
- 21.Singer M, Azim A, O'Keeffe T, Khan M, Jain A, Kulvatunyou N, Gries L, Jehan F, Tang A, Joseph B. How does marijuana affect outcomes after trauma in ICU patients? A propensity-matched analysis. J Trauma Acute Care Surg 2017;83:846–9. 10.1097/TA.0000000000001672 [DOI] [PubMed] [Google Scholar]
- 22.Movig KLL, Mathijssen MPM, Nagel PHA, van Egmond T, de Gier JJ, Leufkens HGM, Egberts ACG, et al. Psychoactive substance use and the risk of motor vehicle accidents. Accid Anal Prev 2004;36:631–6. 10.1016/S0001-4575(03)00084-8. [DOI] [PubMed] [Google Scholar]
- 23.Longo MC, Hunter CE, Lokan RJ, White JM, White MA, et al. The prevalence of alcohol, cannabinoids, benzodiazepines and stimulants amongst injured drivers and their role in driver culpability: part i: the prevalence of drug use in drive the drug-positive group. Accid Anal Prev 2000;32:613–22. 10.1016/s0001-4575(99)00111-6. [DOI] [PubMed] [Google Scholar]
- 24.Masten SV, Guenzburger GV. Changes in driver cannabinoid prevalence in 12 U.S. states after implementing medical marijuana laws. J Safety Res 2014;50:35–52. 10.1016/j.jsr.2014.03.009 [DOI] [PubMed] [Google Scholar]
- 25.Smart R, Pacula RL. Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: findings from state policy evaluations. Am J Drug Alcohol Abuse 2019;45:644–63. 10.1080/00952990.2019.1669626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eichelberger AH. Marijuana use and driving in Washington State: risk perceptions and behaviors before and after implementation of retail sales. Traffic Inj Prev 2019;20:23–9. 10.1080/15389588.2018.1530769. [DOI] [PubMed] [Google Scholar]
- 27.Chung C, Salottolo K, Tanner A, Carrick MM, Madayag R, Berg G, Lieser M, Bar-Or D. The impact of recreational marijuana commercialization on traumatic injury. Inj Epidemiol 2019;6:3. 10.1186/s40621-019-0180-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Downey LA, King R, Papafotiou K, Swann P, Ogden E, Boorman M, Stough C. The effects of cannabis and alcohol on simulated driving: influences of dose and experience. Accid Anal Prev 2013;50:879–86. 10.1016/j.aap.2012.07.016 [DOI] [PubMed] [Google Scholar]
- 29.Fedorova EV, Ataiants J, Wong CF, Iverson E, Lankenau SE. Changes in medical cannabis patient status before and after cannabis legalization in California: associations with cannabis and other drug use. J Psychoactive Drugs 2021;2021:1–11. 10.1080/02791072.2021.1926604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berg CJ, Daniel CN, Vu M, Li J, Martin K, Le L. Marijuana use and driving under the influence among young adults: a socioecological perspective on risk factors. Subst Use Misuse 2018;53:370–80. 10.1080/10826084.2017.1327979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Secades-Villa R, Garcia-Rodríguez O, Jin CJ, Wang S, Blanco C. Probability and predictors of the cannabis gateway effect: a national study. Int J Drug Policy 2015;26:135–42. 10.1016/j.drugpo.2014.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mennis J, Stahler GJ, Mason MJ. Treatment admissions for opioids, cocaine, and methamphetamines among adolescents and emerging adults after legalization of recreational marijuana. J Subst Abuse Treat 2021;122:108228. 10.1016/j.jsat.2020.108228 [DOI] [PubMed] [Google Scholar]
- 33.Case P, Patricia C, Ramos R, Brouwer KC, Firestone-Cruz M, Pollini RA, Fraga MA, Patterson TL, Strathdee SA, et al. At the borders, on the edge: use of injected methamphetamine in Tijuana and Ciudad Juarez, Mexico. J Immigr Minor Health 2008;10:23–33. 10.1007/s10903-007-9051-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thornton K. Report finds meth epidemic in full force in San Diego County, 2015. https://www.justice.gov/usao-sdca/pr/report-finds-meth-epidemic-full-force-san-diego-county. [Google Scholar]
- 35.Chen Xinguang “Jim”. Information diffusion in the evaluation of medical marijuana laws’ impact on risk perception and use. Am J Public Health 2016;106:e8. 10.2105/AJPH.2016.303443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yu B, Chen X, Chen X, Yan H. Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: results from the 1979–2016 National Survey on drug use and health. BMC Public Health 2020;20:156. 10.1186/s12889-020-8253-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Compton RP. Marijuana-impaired driving – a report to congress. Washington, DC: National Highway Traffic Safety Administration, 2017. [Google Scholar]
- 38.Aydelotte JD, Brown LH, Luftman KM, Mardock AL, Teixeira PGR, Coopwood B, Brown CVR. Crash fatality rates after recreational marijuana Legalization in Washington and Colorado. Am J Public Health 2017;107:1329–31. 10.2105/AJPH.2017.303848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vingilis E, Yildirim-Yenier Z, Vingilis-Jaremko L, Seeley J, Wickens CM, Grushka DH, Fleiter J. Young male drivers' perceptions of and experiences with YouTube videos of risky driving behaviours. Accid Anal Prev 2018;120:46–54. 10.1016/j.aap.2018.07.035 [DOI] [PubMed] [Google Scholar]
- 40.Khiabani HZ, Bramness JG, Bjørneboe A, Mørland J. Relationship between THC concentration in blood and impairment in apprehended drivers. Traffic Inj Prev 2006;7:111–6. 10.1080/15389580600550172 [DOI] [PubMed] [Google Scholar]
- 41.Odell MS, Frei MY, Gerostamoulos D, Chu M, Lubman DI. Residual cannabis levels in blood, urine and oral fluid following heavy cannabis use. Forensic Sci Int 2015;249:173–80. 10.1016/j.forsciint.2015.01.026 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request.