Abstract
Objective:
The Great Recession in 2008 was a period of severe economic upheaval and myriad financial stressors. Financial stress is associated with poorer health, but for whom is this stress the most health-relevant? The current study examined the association between financial stressors and mortality, as well as whether this association varied based on people’s financial status.
Method:
Participants from the Midlife in the United States study (N = 2,760) were assessed before (2004-2005) and after (2013-2014) the Great Recession (2008). Mortality status was then tracked from 2013 until 2017.
Results:
People who experienced more financial stressors during the Great Recession were at greater risk of early mortality over the 4-year follow up, HR = 1.14 [1.00, 1.29], p = .046. This association was moderated by the importance of financial security, B = 0.34 [0.08, 0.59], p = .009. Financial stressors were more strongly associated with mortality among people who reported that financial security was important to their wellbeing, HR = 1.29 [1.08, 1.54], p = .006, compared to people who reported it was not, HR = 1.02 [0.82, 1.26], p = .89. Household income and subjective financial status did not moderate the association between financial stressors and mortality.
Conclusions:
Experiencing financial stressors during the Great Recession was associated with increased mortality over 4-year follow up period, particularly for people who reported financial security was important to their wellbeing. Interventions designed to reduce financial stress to improve health may benefit from targeting people for whom such stressors are particularly important.
Keywords: Great Recession, financial stressors, psychological stress, job loss, mortality, health
INTRODUCTION
Psychological stress is linked to an increased risk of disease (1–4) and early death (5–6). One method to productively study the link between psychological stress and health is by examining health outcomes following the experience of difficult events. People are at increased risk of early death after experiencing stressful life events, including events experienced by individuals—such as job loss (7) and the death of a spouse (8)—as well as those experienced by entire populations, such as economic recessions (9) and natural disasters (10).
The Great Recession (11) was a recent global event that led to financial upheaval at the individual and societal level. Defined in terms of gross domestic product (GDP) as the two-year period of economic decline following the financial crisis of 2007, this event has been described as the most damaging economic crisis since the Great Depression (12). In total, 8.5 million jobs were lost in the United States alone (13), and these jobs were not recovered until mid-2014 (14). Although evidence for the health-relevance of economic recessions at a national level is mixed (15), downstream health consequences would be expected among the people who experienced financial stressors during the Great Recession, given that exposure to financial stressors (e.g., job loss) is associated with poorer mental (16) and physical health at the individual level (3,9,17).
Who might be particularly at risk for poorer health following a severe economic recession? The number of financial stressors people individually experienced during the Great Recession would likely be one contributing factor. People varied in the extent to which the financial crisis caused them to experience financially challenging or stressful events, such as declaring bankruptcy or losing a home. Those who experienced few (or no) negative financial events during this period might have been insulated from negative health consequences compared to those who experienced a number of such stressors. This potential heterogeneity in experiences and outcomes is effectively illustrated by a recent investigation of mental health during the Great Recession, which found that that the prevalence of depression and anxiety decreased among Americans as a whole from 2003 to 2013 (16). However, the subset of Americans who experienced financial stressors during the Great Recession evidenced increased rates of anxiety and depression over this same period (16). National patterns in the United States thus obscured a subset of people at particularly risk of poorer mental health outcomes. In a similar way, we might expect that people who experienced the financial stressors during the Great Recession to be most likely to face negative health consequences.
The importance and salience of financial stressors are also likely to play a role in the health-relevance of financial stressors. Stress appraisal theory (18) highlights the importance of people’s cognitive appraisals in their responses to stressful life events. When stressors are appraised as more threatening or people feel unable to cope with a stressor, they are particularly damaging to people’s mental and physical wellbeing. Individual differences in the extent to which financial stressors are important or threatening could play a role in determining who is most vulnerable to poorer health when experiencing financials stressors. For example, people with lower household incomes or fewer financial resources might appraise financial stressors more threatening. Alternatively, people who value financial security might be particularly affected when that security is threatened by events such as job loss or increased debt. When identifying the people for whom financial stressors during the Great Recession were most detrimental, the degree to which financial stressors might be particularly threatening or salient (19) could act as an important moderator of the absolute number of financial stressors.
Present Study
The present study examined the association between financial stressors during the Great Recession and subsequent mortality in a longitudinal cohort study of U.S. adults (N = 2,760). It was hypothesized that people who experienced more financial stressors during the Great Recession would have increased risk of early mortality over a 4-year follow up, from 2013 to 2017. In addition, it was predicted that the association between financial stressors and mortality would be moderated by financial variables measured prior to the Great Recession. The association between financial stressors and mortality was expected to be stronger among people who might appraise such stressors as particularly threatening or salient, specifically those with lower levels of household income, lower subjective financial status, or who reported that financial security was important to their wellbeing.
Method
Participants and Study Design
The current study used participants from the Midlife in the United States (MIDUS) study, a longitudinal cohort with three study waves collected every 10 years. The MIDUS 1 sample (20) used a random-digit dialing procedure to recruit non-institutionalized, English-speaking people between the ages of 25 and 74 in the United States in 1995 and 1996. The MIDUS 1 sample was assessed 10 years later for the MIDUS 2 assessments (21), which repeated much of the original MIDUS assessment. Participants were then assessed in another 10 years for the MIDUS 3 assessment (22), and their mortality was tracked for the subsequent 4.5 years, until November, 2017 (23). The study sample included participants assessed during MIDUS 2 and 3 who reported on Great Recession financial stressors, financial status, and study covariates at each occasion (N = 2,760). Participants from MIDUS 3 who were excluded (n = 534, 16.2% of MIDUS 3) were primarily excluded due to missing financial status data at MIDUS 2 (n = 529, 99.1% of missing). Five additional participants did not report either their education level (n = 3) or life satisfaction (n = 2) at MIDUS 2. Excluded participants included a higher percentage of men (t = 2.42, p = .016) and minorities (t = 4.76, p < .001), and were significantly younger (t = 2.88, p = .004), less educated (t = 4.28, p < .001), reported more financial stressors (t = 3.73, p < .001), and had lower self-rated health (t = 2.55, p = .011). All effects were small in size, ds ≤ 0.21. Participants who were excluded from the study did not significantly vary from those who were included in terms of mortality status, marital status, life satisfaction, or any measures of financial status. Figure 1 provides a timeline of the MIDUS study assessments and the Great Recession.
Figure 1.
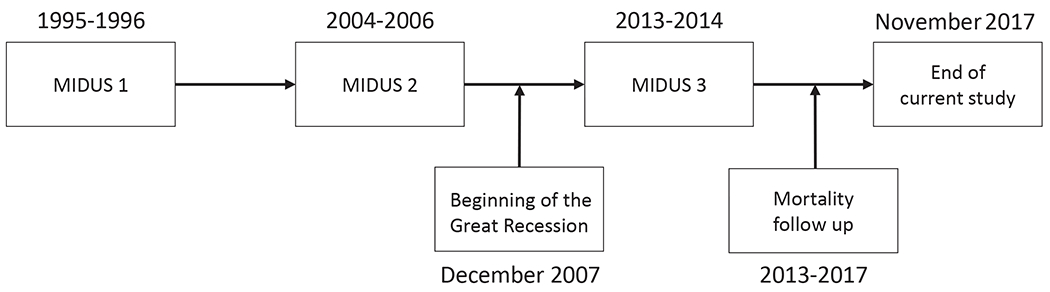
Timeline of MIDUS study data collection and the Great Recession. MIDUS = Midlife in the United States.
Measures
Financial stressors.
Financial stressors during the Great Recession were measured using a sum of 18 items. These items were added to the MIDUS 3 data collection by the MIDUS team specifically to assess the number of difficult financial experiences related to the Great Recession. These items matched those used in a prior study by Forbes & Krueger (16). Participants were asked, “Since the recession began in 2008 have you…”: declared bankruptcy, missed a credit card payment, missed other debt payments, increased their credit card debt, sold possessions to make ends meet, cut back on spending, exhausted unemployment benefits, lost a job, started a new job they didn’t like, took a job below their education or experience, took on another job, missed a mortgage or rent payment, were threatened with foreclosure or eviction, sold a home for less than it cost, lost a home to foreclosure, lost a home to something other than foreclosure, family or friends moved in to save money, or moved in with family or friends to save money. Scores were truncated to ten for participants who reported 11+ stressors (n = 21, 0.8%). Primary study results replicated when using the original count.
Mortality.
The MIDUS Mortality Study data (23) included information on all known MIDUS decedents as of November, 2017. Mortality tracing was conducted by the University of Wisconsin Survey Center. Methods included NDI searches and ongoing longitudinal sample maintenance (23). In this study sample, 70 deaths were recorded up to the censor date (2.5%), 4.2 years after the MIDUS 3 assessment on average. Causes of death were missing for 7 participants (10.0%). Of the 63 deaths with an ICD-10 cause of death, 24 were due to cancer (39.3%), 22 were due to a cardiovascular or related metabolic disease (36.1%), six were due to a chronic lung disease (9.8%), and four were due to a degenerative neurological disease (6.6%). The remaining five causes of death (8.2%) were due to pneumonia, bleeding from an ulcer, necrotizing fasciitis, a vehicle accident, and a fall.
Financial moderators.
Financial moderators included two measures of financial status—household income and subjective financial status—and two appraisals of the importance of finances—the importance of financial security to wellbeing and the importance of extra money to wellbeing. These four measures were assessed at MIDUS 2 (21).
Household income.
Participants reported on the yearly income for their household, including wages, pension, social security, and other sources. MIDUS truncated income to a max of $300,000.
Subjective financial status.
Participants reported on their financial situation at MIDUS 2 on a 11-point scale, ranging from “Worst” to “Best” (0 to 10).
Importance of financial security and importance of extra money.
Participants were asked to choose five areas out of 17 they felt were most important to a good life out (e.g., family relations, faith, autonomy; see 20). Selecting “having enough money to meet basic needs” as one of these five areas assessed whether participants felt financial security was important to their wellbeing. In addition to this moderator variable, selecting “having extra money” as one of the five areas was used to create a variable for participants’ reporting that having extra money was important to their wellbeing.
Study covariates.
Participants reported on a number of variables that were used as covariates. Demographic characteristics included age, sex, marital status, and minority status. Self-reported health was assessed by asking participants, “In general, would you say your health is?” Responses were on a 5-point scale from “Poor” to “Excellent.” Life satisfaction was assessed by asking participants “At present, how satisfied are you with your life?” Responses were on a 4-point scale from “Not at all” to “Very.” Education was assessed on a 12-point scale that assessed participants’ highest level of education, which ranged from no schooling/some grade school to a Ph.D. or equivalent degree. All variables were assessed at MIDUS 2 with the exception of age, which were assessed at MIDUS 3 to better account for variation in the date of MIDUS 3 assessment. The MIDUS 3 assessment date was included as a covariate. Most participants (88.3%) completed MIDUS 3 between June and August, 2013.
Data Analysis
Cox proportional hazard models were used to test the association between financial stressors during the Great Recession and time to death over the follow up period, from 2013-2017. The first model tested the association between financial stressors and mortality. The next models moderated this association by the three financial status variables—household income, subjective financial status, the importance of financial security—in independent models. The next model then compared whether an additional variable assessing the importance of extra money moderated the association between financial stressors and mortality. Exploratory sensitivity analyses were also conducted to test whether the association between financial stressors and mortality varied by financial status among people who reported financial security was important to their wellbeing. All models controlled for age, sex, physical health, life satisfaction, marital status, minority status, education, and date of MIDUS 3 assessment. Results for the primary predictors were reported in terms of hazard ratios (HRs), and unstandardized effects (B) are also reported for interaction terms. Analyses were conducted in SPSS version 27 and MPLUS version 8.3 (24) using maximum likelihood estimation.
Results
Study participants were 55.9% female and 63.9 years old on average (SD = 11.4). Importantly, the majority of participants (73.6%) felt the Great Recession was still ongoing at MIDUS 3, 2.5 years after the recession “ended” as defined by GDP. In total, 70 deaths were observed over the follow up (2.5%), predominantly a result of chronic diseases (91.8% of deaths). Table 1 provides sample demographics.
Table 1.
Demographic Characteristics of Study Participants
| N = 2,760 | |
|---|---|
| Number of financial stressors | 1.9 ± 2.2 (range = 0 to 10) |
| Age | 63.9 ± 11.4 (range = 39 to 93) |
| Percent women | 55.9% |
| Percent married | 72.8% |
| Percent white non-Hispanic | 92.9% |
| Percent with some college education | 72.7% |
| Median household income | $62,500 ± $60,941 |
| Subjective financial status | 6.6 ± 2.1 (range = 0 to 10) |
| Financial status reported as important to wellbeing | 33.6% |
Note: Data are percentages and means ± standard deviations unless otherwise noted. Age indexes participants’ ages at MIDUS 3.
Financial Stressors and Mortality Status
The more financial stressors people experienced during the Great Recession, the greater their risk of early death over the follow up period, HR = 1.14 [1.00, 1.29], p = .046, such that each additional financial stressor was associated with a 14% increased risk of death. Full results are presented in Table 2.
Table 2.
Association of financial stressors during the Great Recession of 2008 with increased risk of mortality: Main Effect and Interaction Effects of Survival Analysis Models
| Main effect model results | Interaction models results | |||
|---|---|---|---|---|
|
| ||||
| N = 2,760 | HR | 95% CI | HR | 95% CI |
| Financial stressors | 1.14* | [1.00, 1.29] | 0.96 | [0.78, 1.19] |
| Age | 1.12** | [1.09, 1.15] | 1.12** | [1.09, 1.15] |
| Sex | 0.79 | [0.49, 1.29] | 0.80 | [0.49, 1.31] |
| Marital status | 1.45 | [0.81, 2.61] | 1.41 | [0.78, 2.56] |
| Minority status | 1.19 | [0.66, 2.13] | 1.22 | [0.68, 2.19] |
| Education | 1.06 | [0.97, 1.17] | 1.06 | [0.96, 1.17] |
| Self-rated physical health | 1.70** | [1.33, 2.18] | 1.67** | [1.30, 2.15] |
| Life satisfaction | 0.92 | [0.60, 1.40] | 0.89 | [0.57, 1.39] |
| Date of MIDUS 3 | 0.22 | [0.03, 1.92] | 0.25 | [0.03, 1.99] |
| Household income | 1.00 | [0.99, 1.01] | ||
| Subjective financial status | 0.98 | [0.85, 1.12] | ||
| Importance of financial security | 0.52* | [0.26, 0.99] | ||
| Financial stressors × Subjective financial status | 0.96 | [0.92, 1.00] | ||
| Financial stressors × Household income | 1.00 | [0.99, 1.01] | ||
| Financial stressors × Importance of financial security | 1.40** | [1.09, 1.80] | ||
Note: All Interaction model results reflect results from the model that included the Financial stressors × Importance of financial security interaction term, with the exception of the estimates for the other two interaction terms, which reflect estimates from the independent models assessing those interaction terms. Household income was measured in hundreds of dollars. HR = hazard ratio. Marital status was coded as 0 = unmarried, 1 = married. Ethnicity was coded as 1 = non-Hispanic whites, −1 = all others. Sex was coded as 1 = men, 2 = women.
p ≤ .05.
p ≤ .01.
Moderation by Financial Status
The next models examined whether three variables related to financial status—household income, subjective financial status, the importance of financial security—moderated the association of financial stressors and mortality. None of the financial status variables were directly associated with mortality status (all ps ≥ .67). When adding the interaction effects independently, the association between financial stressors and mortality was not significantly moderated by either household income or subjective financial status (Table 2). However, the importance of financial security significantly moderated the association between financial stressors and mortality, B = 0.34 [0.08, 0.59], p = .009. People who reported financial security was important to their wellbeing were more likely to die if they experienced financial stressors, HR = 1.29 [1.08, 1.54], p = .006, whereas there was no association for those who did not, HR = 1.02 [0.82, 1.26], p = .89. Deaths were relatively evenly divided between these two groups: 40% of deceased participants (n = 28) reported financial security was important to their wellbeing, whereas 60% of deceased participants (n = 42) did not.
One additional question was whether the importance of having enough money to meet basic needs was particularly relevant to the association between financial stressors and mortality, or if the importance of having extra money to wellbeing might also moderate this association. When testing this interaction term by adding it to the final model from the previous analyses, the importance of extra money did not significantly moderate the association between financial stressors and mortality, B = −0.49 [−1.33, 0.35], p = .26, and the effect was in the opposite direction as that for financial security. These results suggest it is the importance of having enough money to meet basic needs, not having extra money, that was relevant to the primary results.
Sensitivity Analysis: Stratifying Moderation Results by Financial Status
The association between financial stressors and mortality did not vary based on household income or subjective financial status; however, it was possible that this association varied based on financial status among the people who valued financial security (n = 954). Exploratory sensitivity analyses were conducted to investigate this possibility. In this group, the interaction of household income and financial stressors was not associated with mortality over the follow up, B = −0.01 [−0.01, 0.00], p = .938. Descriptively, people with lower incomes evidenced similar mortality risk associated with financial stressors as people with higher incomes when stratifying the sample using a median split, HR = 1.31 [1.04, 1.66], p = .024 and HR = 1.30 [0.97, 1.73], p = .076. In contrast, subjective financial status and financial stressors interacted to predict mortality risk over the follow up, B = −0.07 [−0.13, 0.01], p = .014. People with lower subjective financial status evidenced a stronger association between financial stressors and mortality when compared to people with higher incomes, HR = 1.36 [1.08, 1.73], p = .010 and HR = 1.13 [0.79, 1.60], p = .506. The results suggest that financial stressors might be particularly consequential to the health of people with lower subjective financial status who also value financial security, though these results should be interpreted with caution given their exploratory nature.
Discussion
Using a sample of 2,760 U.S. adults, this study found that people who experienced financial stressors during the Great Recession were at greater risk of early death over a 4-year follow up. Each financial stressor was associated with 14% increased risk of death. The size of this effect was similar to the increased risk of death associated with one year of chronological aging (12%). The risk associated with financial stressors also varied based on whether people valued financial security. For people who reported financial security was important to their wellbeing, each financial stressor was associated with a 29% increased risk of mortality, whereas there was no increase in risk for those who did not.
Notably, it was the importance of having enough money to meet basic needs that increased the risk of early death associated with financial stressors, rather than household income or subjective financial status prior to the Great Recession. It was plausible that people in a worse financial position, in terms of either objective income or subjective rating of their financial status, could face more health consequences when facing the same number of financial stressors as those with more financial resources. However, these results do not provide evidence of this. Among those that reported financial stressors, these experiences were associated with mortality to a similar degree across income ranges and subjective financial statuses. These results align with previous research that has found financial strain is predictive of poorer physical health regardless of income level (25,26). Also of interest was that participants’ reports of the importance of having extra money to wellbeing was not relevant to the association between financial stressors and mortality. This suggests it is not having extra money that is relevant to this association, but the importance of having enough money to meet basic needs.
These findings are particularly relevant to the groups of people who are more likely to experience financial stressors. Financial stress is not equally distributed across populations—people who are economically disadvantaged are more likely to experience financial hardship and distress (27). For example, participants from this study were significantly more likely to experience financial stressors during the Great Recession if they had a lower subjective financial status (r = −0.37, p < .001) or household income prior to the Great Recession (r = −0.11, p < .001). Although financial stressors were associated with mortality across income ranges and subjective financial statuses, people who were more economically disadvantaged were at greater risk of experiencing such financial stressors. As a result, this group faces greater risk for the negative health consequences associated with financial stressors. Interventions that reduce the psychological impact of financial stressors could be one method to reduce these health consequences, particularly during periods of financial instability.
A central implication of this study is that financial stressors were most relevant to the health of people who identified financial security as important to their wellbeing. People who value financial security may appraise financial stressors as particularly threatening, aligning well with stress appraisal theory (18). Notably, the importance of financial security was not independently associated with mortality. People who identified financial security as important to their wellbeing were at risk for early death following the Great Recession—but only if they experienced financial stressors. Whether financial stress or another type of stressful event—such as trauma, divorce, or widowhood—there is considerable heterogeneity in people’s response to stressful life events. Most people are resilient in the face of adversity (28,29), making it essential to determine who is at the greatest risk after financial stressors to effectively allocate resources during periods of individual or societal economic adversity.
The timelines of the MIDUS data collection and the Great Recession are relevant to interpreting the results of the current study. The majority of MIDUS 3 assessments occurred in mid-2013, approximately 4 years after the end of the Great Recession as assessed by change in U.S. GDP. This lag time might create concerns regarding whether the current results can be attributed to the financial stressors during the Great Recession. It is important to note, however, a large majority of the sample (73.6%) indicated they felt the Great Recession was still ongoing when they completed the MIDUS 3 assessment. This matches with measures of job loss, which did not recover to pre-recession levels until mid-2014 (14). In addition, the assessment of the financial stressors was specific to financial events that occurred “since the recession began in 2008,” rather than any financial stressor since the prior MIDUS 2 assessment (2004-2005). These results reflect financial stressors during the Great Recession, but also support the broader health-relevance of psychological stress and stressful life events (1–10). The financial stressors assessed in this study can occur outside the context of the Great Recession, and it is possible that future financial crises could result in early mortality due to psychological stress.
The results of the current study should be understood in the context of its limitations. First, although the total sample was large, 70 deaths were observed over the follow up period. This limited the statistical power of the models used in the study, and the effects observed in this study should be interpreted within the context of a small absolute number of deaths in comparison to the total sample. Once additional data collection occurs in the MIDUS study in the future (e.g., a potential MIDUS 4), it would be useful to examine other outcomes, such as chronic diseases prevalence, that could be used to support and extend the current findings. Second, the count of financial stressors used in the study assessed whether events occurred, but not how often they might have occurred or the extent to which participants experienced the specific events as stressful. Future studies would benefit from assessing the frequency and intensity of financial stressors. Third, the study assessed participants approximately 4 years after the end of the Great Recession and cannot account for people who experienced financial stressors but died prior to MIDUS 3 assessment in 2013. Fourth, the study inferred the importance of the financial stressors from financial status variables, and future studies would benefit from directly assessing people’s primary and secondary appraisals of financial stressors.
Conclusions
This study examined the association of financial stressors during the Great Recession and mortality over a 4-year follow up, from 2013 to 2017. People who experienced more financial stressors were at greater risk of death over the follow up period, and this association was particularly strong among people who reported that financial security was important to their wellbeing. The results highlight the need to account for the context of stressful events when determining who is at risk for poorer health due to stressful life events. Public health interventions aiming to reduce the health consequences of economic upheaval at the individual and societal level would benefit from targeting people who experience financial stressors and report financial security is important to their wellbeing.
Conflict of Interest and Source of Funding:
The author has no conflicts of interest to declare. The author received support from a National Institute on Aging Training Grant (T32-AG000029). The author would like the acknowledge the review of this manuscript by Drs. Avshalom Caspi and Terrie E. Moffitt (Duke University). Publicly available data from the MIDUS study was used for this research. Since 1995 the MIDUS study has been funded by the following: John D. and Catherine T. MacArthur Foundation Research Network, National Institute on Aging (P01-AG020166), National Institute on Aging (U19-AG051426).
Abbreviations:
- MIDUS
Midlife in the United States
- GDP
gross domestic product
References
- 1.Cohen S, Williamson GM. Stress and infectious disease in humans. Psychol Bull 1991;109(1):5–24. [DOI] [PubMed] [Google Scholar]
- 2.Glaser R, Rabin B, Chesney M, Cohen S, Natelson B. Stress-induced immunomodulation: Implications for infectious diseases?. JAMA 1999;281(24):2268–70. [DOI] [PubMed] [Google Scholar]
- 3.Noelke C, Avendano M. Who suffers during recessions? Economic downturns, job loss, and cardiovascular disease in older Americans. Am J Epidemiol 2015;182(10):873–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phillips DP, Liu GC, Kwok K, Jarvinen JR, Zhang W, Abramson IS. The Hound of the Baskervilles effect: Natural experiment on the influence of psychological stress on timing of death. BMJ 2001;323(7327):1443–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA 2007;298(14):1685–87. [DOI] [PubMed] [Google Scholar]
- 6.Russ TC, Stamatakis E, Hamer M, Starr JM, Kivimäki M, Batty GD. Association between psychological distress and mortality: Individual participant pooled analysis of 10 prospective cohort studies. BMJ 2012;345:e4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Browning M, Heinesen E. Effect of job loss due to plant closure on mortality and hospitalization. J Health Econ 2012;31(4):599–616. [DOI] [PubMed] [Google Scholar]
- 8.Moon JR, Kondo N, Glymour MM, Subramanian SV. Widowhood and mortality: A meta-analysis. PloS One 2011;6(8):e23465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noelke C, Beckfield J. Recessions, job loss, and mortality among older US adults. Am J Pub Health 2014;104(11):e126–e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Niiyama M, Tanaka F, Nakajima S, Itoh T, Matsumoto T, Kawakami M, Naganuma Y, Omama S, Komatsu T, Onoda T, Sakata K, Ichikawa T, Nakamura M. Population-Based Incidence of Sudden Cardiac and Unexpected Death Before and After the 2011 Earthquake and Tsunami in Iwate, Northeast Japan. J Am Heart Assoc 2014;3(3):e000798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mucci N, Giorgi G, Roncaioli M, Perez JF, Arcangeli G. The correlation between stress and economic crisis: A systematic review. Neuropsychiatr Dis Treat 2016;12:983–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grusky DB, Western B, Wimer C. The Great Recession. New York: Russell Sage Foundation; 2011. [Google Scholar]
- 13.Seyfried B Employment during the Great Recession: Was this time different. Res Business Econ J 2011;3:1–14. [Google Scholar]
- 14.Center on Budget and Policy Priorities. Chart book: The legacy of the Great Recession. 2019. https://www.cbpp.org/research/economy/chart-book-the-legacy-of-the-great-recession
- 15.Burgard SA, Kalousova L. Effects of the Great Recession: Health and well-being. Ann Rev Sociol 2015;41:181–201. [Google Scholar]
- 16.Forbes MK, Krueger RF. The Great Recession and mental health in the United States. Clin Psychol Sci 2019;7(5):900–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York, NY: Springer; 1984. [Google Scholar]
- 18.Steptoe A, Emch S, Hamer M. Associations Between Financial Strain and Emotional Well-Being With Physiological Responses to Acute Mental Stress. Psychosom Med. 2020;82(9):830–837. [DOI] [PubMed] [Google Scholar]
- 19.Monroe SM. Modern approaches to conceptualizing and measuring human life stress. Ann Rev Clin Psychol 2008;4:33–52. [DOI] [PubMed] [Google Scholar]
- 20.Brim OG, Baltes PB, Bumpass LL, Cleary PD, Featherman DL, Hazzard WR, Kessler RC, Lachman ME, Markus HR, Marmot MG, Rossi AS, Ryff CD, Shweder RA. Midlife in the United States (MIDUS 1), 1995-1996. Ann Arbor, MI: ICPSR. doi: 10.3886/ICPSR02760.v18 [DOI] [Google Scholar]
- 21.Ryff C, Almeida DM, Ayanian J, Carr DS, Cleary PD, Coe C, Davidson R, Krueger RF, Lachman ME, Marks NF, Mroczek DK, Seeman T, Seltzer MM, Singer BH, Sloan RP, Tun PA, Weinstein M, Williams D. Midlife in the United States (MIDUS 2), 2004-2006. Ann Arbor, MI: ICPSR. doi: 10.3886/ICPSR04652.v7 [DOI] [Google Scholar]
- 22.Ryff C, Almeida DM, Ayanian J, Binkley N, Carr DS, Coe C, Davidson R, Karlamangla A, Krueger RF, Lachman ME, Love G, Mailick M, Mroczek DK, Radler B, Seeman T, Sloan RP, Thomas D, Weinstein M, Williams D. Midlife in the United States (MIDUS 3), 2013-2014. Ann Arbor, MI: ICPSR. doi: 10.3886/ICPSR36346.v7 [DOI] [Google Scholar]
- 23.Ryff C, Almeida D, Ayanian J, Binkley N, Carr DS, Coe C, Davidson R, Grzywacz J, Karlamangla A, Krueger R, Lachman M, Love G, Mailick M, Mroczek D, Radler B, Seeman T, Sloan R, Thomas D, Weinstein M, Williams D. Midlife in the United States: Mortality Data, 2016. Ann Arbor, MI: ICPSR. doi: 10.3886/ICPSR37237.v3 [DOI] [Google Scholar]
- 24.Muthén LK, & Muthén BO Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén; 1998-2012. [Google Scholar]
- 25.Puterman E, Adler N, Matthews KA, Epel E. Financial strain and impaired fasting glucose: the moderating role of physical activity in the Coronary Artery Risk Development in Young Adults study. Psychosom Med. 2012;74(2):187–192. [DOI] [PubMed] [Google Scholar]
- 26.Thurston RC, El Khoudary SR, Derby CA, et al. Low socioeconomic status over 12 years and subclinical cardiovascular disease: the study of women’s health across the nation. Stroke. 2014;45(4):954–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Birkenmaier J, Huang J, Kim Y. Food insecurity and financial access during an economic recession: Evidence from the 2008 SIPP. J Poverty 2016;20(2):194–213. [Google Scholar]
- 28.Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Ann Rev Clin Psychol 2011;7:511–35. [DOI] [PubMed] [Google Scholar]
- 29.Sbarra DA, Hasselmo K, Bourassa KJ. Divorce and health: Beyond individual differences. Curr Dir Psychol Sci 2015;24(2):109–13. [DOI] [PMC free article] [PubMed] [Google Scholar]


