Abstract
Early in the pandemic, concern that cardiovascular effects would accompany COVID-19 was fueled by lessons from the first SARS epidemic, knowledge that the SARS-COV2 entry receptor (Angiotensin-converting enzyme 2, ACE2) is highly expressed in the heart, early reports of myocarditis, and first-hand accounts by physicians caring for those with severe COVID-19. Over 18 months, our understanding of the cardiovascular manifestations has expanded greatly, leaving more new questions than those conclusively answered. Cardiac involvement is common (∼20%) but not uniformly observed in those who require treatment in a hospitalized setting. Cardiac MRI studies raise the possibility of manifestations in those with minimal symptoms. Some appear to experience protracted cardiovascular symptoms as part of a larger syndrome of post-acute sequelae of COVID-19. Instances of vaccine induced thrombosis and myocarditis are exceedingly rare but illustrate the need to monitor the cardiovascular safety of interventions that induce inflammation. Here, we will summarize the current understanding of potential cardiovascular manifestations of SARS-COV2. To provide proper context, paradigms of cardiovascular injury due to other inflammatory processes will also be discussed. Ongoing research and a deeper understanding COVID-19 may ultimately reveal new insight into the mechanistic underpinnings of cardiovascular disease. Thus, in this time of unprecedented suffering and risk to global health, there exists the opportunity that well conducted translational research of SARS-COV2 may provide health dividends that outlast the current pandemic.
Abbreviations: ACE2, Angiotensin-converting enzyme 2; PASC, post-acute sequelae of COVID-19; CVD, cardiovascular disease; TNF, Tumor necrosis factor; PAMP, Pathogen associated molecular patterns; DAMPs, Damage associated molecular patterns; CAR-T, Chimeric Antigen Receptor Therapy; DVT, deep venous thrombosis; TF, tissue factor; PSGL, P-selectin glycoprotein ligand; NETs, neutrophil extracellular traps; LV, Left Ventricular; CRP, C-reactive protein; LGE, late gadolinium enhancement; CBV, Coxsackie virus B; B19V, Parvovirus B12; CAR, coxsackievirus and adenovirus receptor; NS1, nonstructural protein 1; EC, endothelial cells; scRNAseq, single cell RNA sequencing; EMBx, endomyocardial biopsy; TTE, transthoracic echocardiograms; RV, right ventricular; GLS, global longitudinal strain; hsCRP, high sensitivity C-reative protein; VITT, vaccine-induced immune thrombotic thrombocytopenia; DTaP, Diphtheria, Tetanus, and Polio; VAERS, Vaccine Adverse Event Reporting System
MECHANISMS OF CARDIAC INVOLVEMENT IN COVID-19
An estimated 20% of those with hospitalized COVID-19 have biochemical evidence (based upon retrospective studies of cardiac-specific troponin measurements) of cardiac injury.1 Those with myocardial injury as a complication of COVID-19 have a marked increase in mortality,2 an association which may also link to pre-existing cardiovascular disease. For example, one retrospective study observed a mortality rate of 69% among those with prior CVD and an elevated troponin, compared to 13% in those with prior CVD but without COVID-19 related cardiac injury, 37.5% in those without CVD but with elevated troponin, and 7.6% in those with no prior CVD with COVID-19 uncomplicated by cardiac injury.3
These epidemiologic observations have spurred intense interest in understanding the relationships between prevalent cardiovascular risk, COVID-19 severity, and SARS-COV2 related myocardial injury. Given the heterogeneity of the clinical illness associated with SARS-COV2 infection and the inherent mechanistic complexity of acute/critical illness in general, it would not be surprising if multiple mechanisms of cardiac injury are operative during the course of COVID-19, at the individual level and/or the population level. Over a short span of time, a remarkable amount of information has been generated at the clinical, basic, and translational levels which suggest multiple pathways conspire to induce myocardial damage. The collateral/indirect effects of SARS-COV2 including hyper-inflammation and thrombophilia may be sufficient to explain cardiac injury. However, most (but not all) hearts examined histologically have viral protein or transcripts present, but classic lymphocytic myocarditis or myocardial necrosis is rare. Thus, at the time of this review, the extent to which cardiac damage is predominantly an effect of systemic processes indirectly related to the virus versus a direct consequence of translocated or transported SARS-COV2 virus remains a major focus.
Systemic hyper-inflammation and cardiac function
In several clinical settings, pro-inflammatory pathways triggered during systemic illness appear to be sufficient to induce acute and chronic changes in cardiomyocyte and/or cardiac fibroblast gene transcription and function. Indeed, the heart is well equipped to sense an inflammatory milieu. For instance, cardiomyocytes express both tumor necrosis factor (TNF)-α receptors 1 and 2.4 Cardiac myocytes and fibroblasts also express gp120, which allows for IL6-associated homeostatic effects including hypertrophy, fibrosis, and cell survival.5 Pathogen or damage associated molecular patterns can activate NOD-like receptors (ie, NLRP3) leading to inflammasome activation in cardiomyocytes and cardiac fibroblasts.6 Together, systemic inflammation can result in a range of cellular effects including contractile dysfunction7, hypertrophy8, cardiomyocyte cell death9, and/or fibrosis.8 , 10 Terminal effects are mediated by activation of canonical cell death pathways.11 , 12 These cells are also capable of paracrine activity. For instance, pressure overload of the heart leads to expression of TNF-α cytokine secretion.13 The expression of chemokines by resident immune cells and stromal cells result in secondary recruitment of monocytes and T lymphocytes which can participate in feed forward inflammation at the tissue level.14
Animal models have generally been supportive that cytokine signaling can trigger cardiomyocyte dysfunction. For instance, cardiac-specific TNF-α expression has been shown to be sufficient to cause cardiomyocyte death and heart failure.15 Genetic deletion of murine TNF-α ameliorates the pathophysiologic effects of angiotensin II, including cardiac hypertrophy.16 Cardiac TNF-α over-expression leads to a lymphocytic myocarditis and a progressive dilated heart failure phenotype in mice.9
Observations in human disease systems also support a potential relationship between systemic inflammation and ventricular performance. For example, left ventricular dysfunction is commonly observed (and may correlate with blood biomarkers of cardiac necrosis) in those with cytokine release syndrome following CAR-T therapy.17, 18, 19 Prompt administration of tocilizumab in this setting may reduce the risk of adverse cardiovascular events.19
Prevalent heart failure has been association with elevations in plasma levels of pro-inflammatory (TNF-α, IL6) cytokines20, especially when out of proportion to counter-regulatory anti-inflammatory mediators.21 This may stem from both local production (cardiomyocytes expression, cardiac macrophage expression22) and systemic production (given over-expression in monocyte supernatants21) in heart failure. Yet, the failure of phase 3 anti-TNF-α clinical trials (despite favorable biomarker changes in early phase trials) provides a cautious reminder that the distinctions between physiologic and pathophysiologic inflammation in heart failure remains incompletely understood.23 , 24 , 25 , 26 Thus, despite recently successful trials of anti-inflammatory strategies to prevent atherothrombosis,27 , 28 the extent to which immune activation is cause, effect, or epiphenomenon to ventricular dysregulation generally remains unknown.
Auto-reactive antibodies, including anti-heart antibodies, which correlate with clinical severity have also been described.29, 30, 31, 32 Whether breakdown in peripheral tolerance is simply a marker of immune activation/dysregulation or whether it contributes to disease severity or persistence will require additional study.
Inflammation and thrombophilia are linked via bi-directional mechanisms
Venous thrombosis and/or atherothrombotic cardiovascular events are relatively common complications in the setting of acute illness and stem in part from infection and/or inflammation. Rates of deep venous thrombosis (DVT) in those who do not receive thromboprophylaxis approach 20% of general medicine admissions and 50% of those undergoing surgery.33 , 34 Influenza and other common respiratory infections are accompanied by a 3–6 fold higher rate of acute myocardial infarction within 1 week of infection.35 Indeed, the magnitude of protection afforded by influenza vaccination against recurrent myocardial infarction or cardiovascular death36 is arguably on par with that afforded by medical therapies in aggregate.37
Decades of research have established several complex inter-related pathways which connect innate immune activation to clot formation. These pathways likely evolved to contain the dissemination of invading pathogens, but now account for substantial cardiopulmonary morbidity, mortality, and need for anti-thrombotic therapy. Upon activation by pathogen-associated molecular patterns or damage- associated molecular patterns, monocytes, neutrophils, and their microparticles express tissue factor, thus promoting the extrinsic clotting cascade.38 , 39 Tissue factor-dependent thrombin is a potent activator of platelets, which themselves bind monocytes and neutrophils. Platelet-leukocyte interactions, mediated by P-selectin and P-selectin glycoprotein ligand 1 among others, act to accelerate co-activation and also can direct these circulating elements to the endothelium.40, 41, 42 Neutrophils further activate the coagulation system via the formation of neutrophil extracellular traps which contains various pro-thrombotic constituents (fibrin, histones, DNA, neutrophil elastase, myeloperoxidase) which entrap platelets, inactivate natural thrombolytic pathways, and entrap pathogens.43 Inflammatory cytokines can induce additional tissue factor expression44 and also down regulate thrombomodulin and activated protein C to impair endogenous anti-coagulate activity.45 The endothelium is also a central active participant in translating inflammatory processes into thrombotic events. Pro-inflammatory stimuli upregulate a variety of adhesion molecules on endothelial cells which promotes capture of circulating leukocytes and platelets.46 , 47 The complement system, when engaged by pathogens or antibodies, can activate platelets48 and platelet-bound complement in turn further stimulates antigen presenting cells and neutrophils.49
Linkages between hyper-inflammation, thrombophilia, and cardiac injury in COVID-19
The pro-inflammatory state caused by SARS-COV2 infection has been well described and elevations in cytokine levels generally correspond with risk of mortality.50 The extent to which inflammation is a pathologic or adaptive response in this setting has not been fully determined. However, hyper-inflammation appears to contribute in part to overall morbidity and mortality from COVID-19 given the protective effects of dexamethasone.51 Therefore, it is plausible that systemically derived pro-inflammatory cytokines may cause or contribute to cardiac injury in those who develop cardiac injury and/or LV dysfunction in COVID-19. However, evidence for this is circumstantial. For instance, peak troponin levels in those with COVID-19 have been shown to correlate with markers of systemic inflammation (eg, IL6, CRP, neutrophilia).52 , 53 The absence of classic lymphocytic myocarditis54 , 55 or evident myocardial infection55 in many with cardiac injury with COVID-19 could be interpreted to support systemic hyper-inflammation as a frequent default cause of cardiac injury.56 Studies in rhesus macaques may support this hyper-inflammation hypothesis since these animals develop post-infection cardiac fibrosis after SARS-COV2 infection, but without evident leukocyte infiltration or infection of the myocardium.57
Convincing evidence from prospective clinical trials that hyper-inflammation is the major mechanism of cardiac injury is currently lacking. Of note, the RECOVERY trial of dexamethasone did not routinely evaluate for cardiac injury using troponin levels or echocardiograms, but the rates of cardiac death (usual care: 0.2% dexamethasone: 0.1%) and new major cardiac arrhythmias (usual care: 6.3% dexamethasone: 5.3%) were not significantly different.51 The GRECCO-19 trial showed a protective effect of colchicine against clinical deterioration in hospitalized COVID-19, but there was no difference in the primary biochemical endpoint of peak high sensitivity troponin levels.58 Randomized trials of IL-6 inhibition have reported clinical outcomes, but have not yet reported differences in biomarkers of cardiac injury.59, 60, 61, 62, 63 Of note, a propensity matched retrospective analysis of COVID-19 patients treated (or not) with Tocilizumab did not show a reduction in troponin levels,64 questioning a causal role for IL-6 in cardiac necrosis in the COVID-19 setting. Thus, the extent to which systemic inflammation alone is responsible for cardiac injury is uncertain, but given the ongoing trials investigating immunomodulation, future analyses may elucidate the causal position of various inflammatory pathways, relative to cardiac injury.
COVID-19 associated inflammation may also induce cardiac injury via the induction of a complex and profound pro-thrombotic state.65 Both venous and arterial thrombotic events have been frequently observed, often despite thromboprophylaxis, and independently associates with the risk of death.66, 67, 68, 69 NETosis in this setting has been described by several groups.70, 71, 72 An activated platelet phenotype has also been frequently described.73, 74, 75 Complement activation is associated with a severe course characterized by respiratory failure but whether this contributes to or protects against disease progression is unclear.76 , 77 The notion that thrombophilia is driven by hyper-inflammation is also suggested by the fact that D-dimers were reduced (albeit modestly) by dexamethasone.51
The extent to which thrombosis mediates cardiac injury is also unclear. Cardiac microvascular thrombosis has been described as a prominent feature in some,78 but not all histologic studies. Given the frequency of thrombosis despite typical pre-pandemic empiric thromboprophylaxis,68 , 69 anti-thrombotic strategies have evolved. Therefore, the contribution of thrombosis to cardiac injury may be a moving target, but our understanding is likely to evolve as ongoing studies refine the optimal approach to mitigating the risk of thrombophilia.79
Therefore, the extent to which systemic inflammation and its accompanied thrombophilia contribute to cardiac injury, the specific manifestations and physiologic importance, and the best means to provide cardio-protection (if needed) from cytokine elevations in COVID-19 remain critical knowledge gaps.
Viral tropism and myocarditis
Myocarditis (inflammation of the heart) can be provoked by viral, bacterial (eg, Borrelia species), or protozoa (eg, Trypanosoma cruzi) infections, auto-immunity, or cardiotoxins and has traditionally been defined pathologically using the Dallas criteria, but the incorporation of clinical features and cardiac MRI in contemporary practice can often refine the mechanism of disease and improves estimates of prognosis. By Dallas criteria,80 an endomyocardial biopsy is graded as myocarditis, borderline myocarditis, or no myocarditis based upon whether an inflammatory cells infiltrate is present with surrounding cardiomyocyte degeneration (in a non-ischemic appearance). The distribution, extent, and type of infiltrate can provide further subcategorization, and the appearance of associated fibrosis (and its distribution, extent, and type) is also analyzed. Immunohistochemistry, polymerase chain reaction, and transcriptomics are able to provide detailed immunologic and mechanistic information. Clinical features can categorize patients according to fulminant, acute, chronic active, and chronic persistent presentations. Paradoxically, patients with a fulminant clinical presentation often have a better prognosis than those with an acute/subacute course.81 However, the diagnostic implications of the histologic findings are limited by sampling error and intra-observer variation.82 Cardiac MRI is increasingly used to provide myocardial tissue characterization in those with suspected myocarditis. The consensus recommendations for the assessment for myocarditis (Lake Louise Criteria, updated in 2018) is based on at least one T1 abnormality (increased myocardial T1 relaxation times, increased extracellular volume fraction, or late gadolinium enhancement) with at least one T2-based criterion (increased myocardial T2 relaxation times, visible myocardial edema, or increased T2 signal intensity ratio).83 , 84
Coxsackie virus B (CBV) and Parvovirus B12 (B19V) are among the best studied causes of viral myocarditis and provide examples of a cardiomyocyte-tropism and endothelial cell tropism, respectively. CBV directly infects cardiomyocytes via a transmembrane receptor termed the coxsackievirus and adenovirus receptor (CAR). After entry CBV undergoes viral replication and follows a lytic life cycle leading to cardiomyocyte injury, cell death and consequent local immune response. In contrast to the cardiomyocyte tropism of CBV, B19V infects cardiac endothelial cells (EC).85 EC expression of the viral nonstructural protein 1 appears to be sufficient to induce a robust pro-inflammatory phenotype characterized by STAT3 phosphorylation in vitro.86 B19V infection also leads to EC apoptosis and subsequent indirect cardiomyocyte toxicity.87 In addition to proposed direct viral effects, auto-immune responses and molecular mimicry may also induce subsequent antibody mediated cardiac injury. Auto-reactive T cells and auto-antibodies to structural proteins including myosin as well as signaling proteins including the beta-adrenergic receptors have been characterized in a variety of human settings and animal models.88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99 Thus, viral exposure can lead to cardiac injury from direct cytotoxicity but may also occur in response to host responses. Early phase trials raise the possibility that anti-viral therapy87 and/or immunomodulation strategies100 may provide clinical benefit, but the extent to which the persistence of viral pathogens confer pathogenic effects remains ill defined.
SARS-COV2 tropism: the expression and function of ACE2 in the heart
Human tissue expression studies have shown that ACE2 is broadly expressed in the microvasculature of hearts and kidneys.101 , 102 More recent studies, including single cell RNA sequencing (scRNAseq) confirm ACE2 is highly expressed in the human heart.103, 104, 105, 106 For example, Tucker et al performed bulk and single nucleus RNA sequencing on the left ventricles of 11 individuals with dilated cardiomyopathy, 15 with hypertropic cardiomyopathy, and 16 controls with nonfailing hearts. In general, ACE2 expression was expressed on cardiomyocytes and cardiac fibroblasts but highest in pericytes, cells which are embedded in the basement membrane to surround and support the microvasculatature.106 Interestingly, heart failure was associated with downregulation of ACE2 in fibroblasts, pericytes, and vascular smooth muscle cells but a concomitant increase in ACE2 among cardiomyocytes. Increased ACE2 in those with heart failure reduced ejection fraction and aortic stenosis was also observed by Nicin et al.104 Thus, variance in ACE2 expression in those with heart failure may be best resolved using single cell sequencing techniques since such regulation appears to be cell specific and discordant among cell types within the heart. The use of angiotensin converting enzyme inhibitors may also increase ACE2 expression, especially on cardiomyocytes.104 , 106
SARS-CoV-2 entry into cells requires protease activity for priming of the spike protein. The serine protease TMPRSS2 is largely undetectable in the heart106, but heart tissue does express high levels of ITGA5107 , 108 and cathespins106 which may be capable of supporting SARS-CoV-2 entry.109
Overall, these data support a hypothesis that the increased risk of COVID-19 among those with co-morbid cardiovascular disease may stem from upregulated cardiomyocyte expression of ACE2 which precedes infection and may pre-dispose to cardiac injury.
Human studies of myocardial infection and injury by SARS-COV2 virus
Given the cardiac expression of ACE2, several groups have sought to establish whether SARS-COV2 infects human hearts as part of the clinical course of COVID-19 using endomyocardial biopsy (EMBx) specimens from living donors or autopsy specimens post mortem.
In an early report during the first wave in Italy, Tavazzi et al. were among the first to document cardiac infection in a patient with clinically fulminant “myocarditis” and cardiogenic shock using electron microscopy of EMBx tissue.110 Viral particles were localized to large vacuolated interstitial cells or macrophages. In contrast, cardiomyocytes and endothelial cells did not appear to be infected, and minimal fibrosis was observed without a pronounced lymphocytic infiltrate.
Escher and colleagues retrospectively evaluated 104 patients who underwent EMBx between February to March 2020 in Germany due to suspected myocarditis from unselected causes, and found SARS-COV2 present in 5 cases, using RT-PCR of the E gene.78 These 5 cases also had small artery damage, and 1 had evidence of myocarditis (and 1 borderline) by Dallas criteria.
Autopsies in those who succumb to COVID generally show high viral loads in the lung in association with lung damage accompanied by a lymphocytic infiltrate.111, 112, 113, 114 Venous thrombosis and pulmonary embolism are common findings as well.111 , 115 Despite the nearly uniformly robust lung pathology, extreme immune activation, and hypercoagulability in severe COVID-19, less consistent extra-pulmonary findings are generally observed.112, 113, 114 For instance, in a prospective cohort study including 12 post-COVID-19 autopsies by Wichmann et al, all 12 patients had high SARS-COV2 virus concentrations in the lung, 6/10 had viremia, and 5/12 had virus identified in other organs.115 In this series, 1 patient had a lymphocyte predominant myocardial infiltrate.
Using post-mortem tissue from consecutive autopsies from COVID-19 patients, Fox et al also report SARS-COV2 viral particles are common, using electron microscopy.116 They observed virus associated with the endothelium, but not cardiomyocytes. In this series, scattered myocyte death was occasionally seen, but no lymphocytic infiltrates or myocarditis by Dallas criteria was reported.
Linder and colleagues detected SARS-COV2 in the heart of 24 of 39 consecutive autopsies using viral RNA hybridization (probe V –nCoV2019-S).117 Those without myocardial SARS-COV2 infection tended to have lower cytokine gene expression although there was no difference in the leukocyte density, compared with heart with high SARS-COV2 viral loads. SARS-COV2 tended to localize to interstitial cells and macrophages, but not cardiomyocytes. There was evidence of active viral replication (ie, the negative strand of the RNA genome was datable) in 5 patients. Myocyte cell death was generally not observed in these COVID-19 non-survivors, irrespective of the presence or absence of virus in heart tissue.
Post-mortem cardiac specimens from four patients with clinically severe cardiac injury analyzed by Bailey et al showed SARS-COV2 spike and nucleocapsid RNA was identified via immunohistochemistry in each case.118 Viral antigens were generally observed in cardiomyocytes, and also occasionally identified in epicardial or perivascular adipocytes and pericytes.
A study of 6 consecutive autopsies from COVID-19 patients without suspected cardiac involvement by Bulfamant et al each had virus detectable (including both sense and anti-sense transcripts suggesting active transcription) by multiple modalities.119 Virus was identified in interstitial macrophages as well as cardiomyocytes. No vascular injury or endothelialitis was observed. Cardiomyocytes containing SARS-COV2 did not show signs of cell death, but did have evidence of disrupted cell-cell adhesions.
Pellegrini et al120 examined 40 hearts from patients who died of COVID19 infection to evaluate the prevalence and correlates of myocardial injury. A third of these hearts (35%) had myocyte necrosis especially in the LV, with majority showing evidence of cardiac thrombi (2/14 epicardial coronary thrombi and 9/14 microthrombi). These thrombi had greater fibrin and terminal complement G5b-9 compared with aspirate coronary thrombi from patients with MI without COVID19 infection. These findings suggest that microthrombosis may be partly responsible for the observed myocardial injury in COVID19.
A literature review of 22 separate studies including 277 autopsies suggests that at least one potential histopathologic abnormality may be present in 47.8% of cases.121 The rate of myocarditis was reported to be 7.2%, non-myocarditis inflammation was observed in 12.6%, single cell ischemia was seen in 13.7%, small vessel thrombi in 10.8%, and macrothrombi in 19.1%.121 As such, there may be within and between-patient heterogeneity of the mechanisms responsible for myocardial injury.
RAS dysregulation as a potential consequence of COVID-19
ACE2 has important and non-redundant peptidase functions in the heart and lung to maintain vascular integrity and regulate cardiotoxic products of the renin-angiotensin system. ACE2 converts angiotensin II into angiotensin 1–7, thus providing tissue level protection against angiotensin II-related hypertension, fibrosis, heat failure, inflammation, vasoconstriction, and lung injury.122 , 123 Angiotensin 1-7 also has cardioprotective activity via the Mas receptor. ACE2 also degrades des-Arg9-bradykinin which can have pro-inflammatory and vasocontrictive properties via activation of bradykinin 1 receptor.124 ACE2 deletion in mice leads to pathological ventricular hypertrophy in addition to pulmonary vascular permeability.125 The fact that ACE2 becomes co-opted by SARS-COV2 raises the possibility that disruptions in angiotensin II or des-Arg9-bradykinin levels may factor into the cardiovascular pathophysiology of COVID-19.
SARS spike proteins binds to ACE2 with very high affinity leading to viral entry.126 , 127 The possibility that this interaction could lead to physiologically relevant local ACE2 depletion is supported by a study from the first SARS pandemic by Oudit et al.128 In this report, myocardial ACE2 protein expression was greatly reduced in hearts with evident SARS-CoV infection, compared to those with SARS-CoV who had undetectable virus or controls who died of sepsis (non-SARS). Wu et al have shown that angiotensin II levels are elevated in severe COVID-19, a finding which could be explained by reduced ACE2 expression or function.129 Lui and colleagues have also reported elevated angiotensin II plasma levels in those with COVID-19, which correlated with viral load.130 In support of ACE2 being relevant to angiotensin II levels is that the infusion of human recombinant soluble ACE2 decreased angiotensin II levels in patient with COVID-19.131 Thus, ACE2 may be more than a critical gateway for SARS-COV2 entry- its functional disruption may participate in the loss of cardiopulmonary homeostasis during COVID-19.
COVID-19 RELATED CARDIOVASCULAR DISEASE AT THE POPULATION LEVEL
The exact prevalence of cardiac involvement in SARS-CoV-2 infection is difficult to estimate, owing in part to the heterogeneity of clinical severity of this disease. Cardiac injury rates have tended to be reported from study cohorts reflecting mostly sicker populations. There has not been a common definition of “cardiac involvement” by SARS-CoV-2. Patients who succumb to severe COVID19 infection often have high prevalence of cardiovascular co-morbidities and risk factors, and observed cardiac abnormalities may arise in part from pre-existing risk due to prior diagnosed or undiagnosed cardiovascular disease. Blood biomarkers such as cardiac troponin levels are widely available and highly sensitive. Imaging studies such as echocardiography or cardiac magnetic resonance imaging have been done less routinely, especially early in the pandemic when personal protective equipment was scare. Thus, information about cardiovascular complications is certainly clouded by ascertainment and other forms of selection bias, and currently estimated by integrating information from multiple cardiovascular tests reported retrospectively.
Rates of general myocardial injury by plasma biomarkers
Cardiovascular complications were reported early in the pandemic with blood biomarkers, followed by imaging studies showing a broad spectrum of cardiac findings. Troponin is a marker of myocardial injury and is routinely evaluated as part of the work up for acute coronary syndromes. Studies have shown that myocardial injury is not uncommon in patients with COVID19 infection but varies widely based on the cohort studies. Reported incidence of elevated troponins ranged between 8% and 62% depending on cohort characteristic (outpatient, inpatient or those hospitalized in the intensive care unit), mostly derived from retrospective studies which may be subject to referral/testing bias.132, 133, 134, 135, 136 A meta-analysis of 43 mostly retrospective studies (9475 patients) showed that the prevalence of cardiac injury was 19% (95% CI: 15%–22%) in all-comer COVID-19 patients, 36% (25%–47%) in patients with severe COVID-19, and 48% (30%–66%) in patients who died from COVID19 infection. Studies investigating high-sensitivity troponin generally showed higher percentage of patients with myocardial injury compared with earlier-generation troponin assays.1 Similar data on cardiac injury in asymptomatic or mild COVID19 is lacking. Thus, in general, myocardial injury in the setting of COVID19 infection, when defined by cardiac-specific troponins, may accompany 1 in 5 symptomatic infections, and is more common with greater COVID19 severity.
Troponin elevations may stem from a broad spectrum of processes including those generally expected in the setting of respiratory failure (eg, right ventricular dysfunction,137 demand ischemia/type II myocardial infarction, stress cardiomyopathy138 , 139), processes provoked by hyper-inflammation (atherosclerotic plaque rupture, ventricular dysfunction, high output/demand-supply mismatch), and direct cardiovascular pathology specific to SARS-COV2 (myocarditis,140 microvascular thrombosis/endotheliailitis,120 , 141 renin-angiotensin system dysregulation).
Ventricular dysfunction in the setting of COVID-19
Several studies have investigated ventricular function in COVID19 infection. Overall, the prevalence of ventricular dysfunction varies widely by cohort, comorbidities, disease severity and geographic location. Overall, clinical heart failure develops in 1% of hospitalized patients with COVID19 and 18% of patients in the ICU.142 , 143 In patients with COVID19 without prior cardiac history, severe cardiac disease (severe LV dysfunction or tamponade) was detected in 13% by echocardiography.144 In a large prospective study of 1,216 144 from 69 countries undergoing transthoracic echocardiograms (TTE), 55% had abnormal findings. 39% had left ventricular (LV) abnormalities and 33% had right ventricular (RV) abnormalities. Severe ventricular dysfunction (RV, LV, or biventricular) was found in 14% and tamponade was present in 1%. In this cohort, the indication for TTE was left sided heart failure (HF) in 40%, 26% had elevated cardiac biomarkers, and 20% had suspected right HF.
In another retrospective study of 870 patients with acute COVID-19 infection admitted to 13 hospitals in 4 continents, 17% had LV dysfunction (LV ejection fraction < 50%) and 29% had RV dysfunction (RV free wall strain >-20%). Patients admitted to the intensive care unit (ICU) generally had worse LV and RV function.145
Small studies have also shown that subclinical biventricular dysfunction as measured by strain echocardiography is common and is associated with poor outcomes in COVID19. In a prospective study of 218 patients with COVID19 (52 critically ill), LV dysfunction measured by reduced LV global longitudinal strain (GLS, <-21%) was observed in 83% of patients, and was more common in critically ill patients (98% vs 78%). GLS correlated with oxygen saturation, high sensitivity C-reative protein (hsCRP), and interleukin (IL)-6.146
Cardiac MRI abnormalities in patients with COVID-19
Cardiac magnetic resonance imaging (MRI) provides unprecedented insight into cardiac involvement owing to its ability to decipher fibrosis, inflammation/edema, in addition to structure and function. A prospective study by Puntmann et al of 100 patients recovered from COVID-19 (33% severe illness, >2 weeks post recovery) identified cardiac MRI abnormalities in 78%.147 MRI evidence of fibrosis, myocardial edema/inflammation, and pericardial involvement were each more frequently found in those recently recovered from COVID-19, compared to healthy controls and those matched for cardiovascular risk factors. Changes among those with a non-severe/non-hospitalized clinical course were only modestly less severe than those who required hospitalization.147
Another study in patients with severe COVID19 infection and evidence of myocardial injury by serum troponin, cardiac MRI revealed a higher percentage of abnormalities, including scar or ischemia (54%), with 26% having myocarditis-like scar, 22% with infarction or ischemia, and 6% with dual pathology.148
In those with less severe illness, rates of cardiac MRI abnormalities have been more varied. Rajpal et al reported 8 of 26 athletes with mild to asymptomatic COVID-19 had late gadolinium enhancement and 4 had myocarditis by cardiac MRI.149 In a prospective study of 1597 US competitive athletes who underwent screening with cardiac MRI,150 only 2.3% had findings suggestive of myocarditis. It is important that to note that many of these patients had no clinical evidence of myocarditis, making these MRI findings of unknown significance. Another study investigating patients with only mild symptoms showed no difference in the prevalence of cardiac MRI abnormalities compared with matched controls.151
A systematic review of 22 studies (2,954 patients) recovered from COVID19 illustrate this wide variation of CMR abnormalities.152 Fibrosis (late gadolinium enhancement) was observed in COVID-19 survivors with rates ranging from 4 to 100%. Myocardial edema (T2 elevation) was not detected in 4 of 15 studies, and in 2%–60% of those enrolled in the other 11 studies.153
These studies using cardiac MRI to understand potential cardiac manifestations have been provocative, but have not included corroboration with endomyocardial histology, have had limited clinical follow-up, and lack of baseline/pre-COVID19 cardiac MRI comparisons. The variability of these observations reflects heterogeneity of study populations and highlights the need to harmonize MRI techniques and protocols in future multi-center trials.154
Arrhythmias are frequent in those with COVID-19
Both atrial and ventricular arrhythmia have been seen observed in patients with COVID19 infections. In a meta-analysis of 31 studies (mostly retrospective cohort studies) that investigated prevalence of atrial and ventricular arrhythmia in 187,716 patients with COVID, the prevalence of atrial fibrillation (AF) varied widely (1%–34%), with a pooled prevalence of 8%. The heterogeneity of AF prevalence was partly explained by age, geographic location, prevalence of hypertension and diabetes.155 Among studies that reported outcomes, AF was associated with 4-fold increase in mortality (pooled OR: 3.97, 95% CI: 2.76–5.71).155 It is important to note that these studies included new onset and prior AF. Limited evidence investigating new onset AF showed that the incidence ranged between 4 and 7%.156 , 157 Compared with patients with historical AF, patients with new-onset AF had higher levels of inflammation (leukocyte count, higher C-reactive protein levels), and poorer oxygenation (lower PaO2/FiO2) reflective of more severe disease.157
In another meta-analysis of 56 mostly retrospective studies (17,435 COVID19 patients) showed that 16.8% had arrhythmia (8.2% for atrial fibrillation/atrial flutter/atrial tachycardia, 10.8% for conduction disorders, 8.6% for premature contraction and 3.3% for ventricular fibrillation/ventricular tachycardia.158 Possible mechanisms linking COVID19 with arrhythmia include systemic inflammation, myocardial injury, neurohormonal activation, hypoxia, or more rarely myocarditis. Similar to other cardiovascular manifestations, the extent to which arrhythmias are provoked by systemic illness or as direct consequence of SARS-COV2 remains unknown.
Predictors of cardiovascular involvement in COVID19
In general, studies have shown that myocardial involvement in COVID19 is associated with COVID19 severity and traditional cardiovascular risk factors and conditions. For instance, troponin elevations during COVID19 hospitalizations were associated with preexisting cardiovascular morbidity, including hypertension, diabetes, chronic kidney disease, atrial fibrillation, coronary artery disease, and heart failure.135 , 159, 160, 161 SARS-CoV-2 viremia has also associated with higher troponin levels.162
Similar associations between COVID-19 severity, pre-existing cardiovascular disease, and cardiac involvement have been established using cardiac imaging. For example, myocardial edema/inflammation seen on cardiac MRI was more common in patients with severe COVID19, compared with non-severe COVID19 and healthy controls. Higher T2 signal reflective of myocardial edema was associated with markers of COVID19 severity such as D-dimer, C-reactive protein, and lymphopenia.163 Prior history of ischemic heart disease or heart failure were associated with abnormalities on transthoracic echocardiogram in patients with COVID19.144 Similarly, a history of dyslipidemia and coronary disease were associated with cardiac MRI abnormalities.148 Together, these findings suggest that cardiac abnormalities seen during COVID19 may partly reflect prior cardiovascular disease as well as the severity of acute COVID-19 illness.
Clinical consequences of cardiac involvement
Regardless of manifestation, myocardial involvement (ie, troponin elevation, arrhythmia, ventricular dysfunction) is associated with poor outcomes. For instance, a meta-analysis of myocardial injury by blood biomarkers was associated with a staggering 14-fold increase in mortality in COVID19 patients.2 Prior cardiovascular disease and acute myocardial injury seem to have synergistic effects to increase risk in COVID19. One study showed that COVID19 patients with prior CVD and elevated troponin had 69% mortality, compared with CVD without troponin (13.3%), without CVD but with elevated troponin (37.5%), and no CVD and no elevated troponin (7.6%).3
A significant percentage of patients with COVID19 who require ICU care develop heart failure. Overall, clinical heart failure develops in 1% of hospitalized patients with COVID19 and 18% of patients in the ICU.142 , 143 In a prospective study of 214 patients with COVID19, measures of RV function and LV function were significantly associated with mortality.164 Small studies suggest that even subclinical ventricular dysfunction (LV and RV strain by echocardiography) is associated with mortality in patients with COVID19.164, 165, 166
Arrhythmia in COVID19 also portend higher risk of mortality. In a meta-analysis of 23 mostly retrospective studies including 108,745 patients with COVID19, AF was associated with a 13% relative increase in mortality and 14% relative increase in unfavorable outcomes.167 Another meta-analysis showed that cardiac arrhythmia were noted in 19% of COVID19 and 48% of COVID19 with poor outcomes (mortality, severe illness, or ICU admission).168
The duration of cardiac involvement remains unknown. Studies have reported persistent cardiac symptoms (termed Post-Acute Sequelae of SARS-CoV-2 infection) can extend 6 months and beyond after infection. In a prospective study of 1733 patients who recovered from COVID19 (75% requiring supplemental oxygen during acute illness), 5% reported chest pain and 9% reported palpitations at 6 months post recovery.169 No robust data exist for long-term follow-up of patients with cardiac injury or abnormal cardiac MRI and thus the clinical significance of these abnormalities remains to be elucidated.
Cardiovascular events after SARS-COV2 vaccination
In comparison to the cardiac injury which result from natural infection by SARS-COV2, cardiovascular manifestations after SARS-COV2 vaccination (myocarditis, pericarditis, and unusual thrombotic events) are exceedingly rare events, but are important to identify.
A syndrome of unusual thrombosis (ie, central venous sinus, portal vein) in combination with severe thrombocytopenia, termed vaccine-induced immune thrombotic thrombocytopenia has been reported as a rare complication of SARS-COV2 vaccination.170, 171, 172 The mortality rate associated with this complication may approach 40%. Patients tend to present 5 to 24 days after immunization, are predominantly young females, with platelet counts as low as 10,000 per cubic millimeter. An association with anti-platelet factor 4-polyanion auto-antibodies has been consistently reported, despite the absence of previous heparin administration.173 Treatment with intravenous immune globulin and corticosteroids improves platelet counts and may improve the safety of anti-coagulation. The incidence may approach 1 case per 100,000 patients immunized with an adenoviral based ChAdOx1 nCoV-19 (AstraZeneca) vaccine, and is less frequently reported after mRNA-based vaccines.
In contrast to the high mortality associated with cardiac injury in the setting of natural infection, myocarditis and pericarditis after immunization leads to hospitalizations which are frequently brief and symptoms which often resolve, treated with standard anti-inflammatory therapies. Myocarditis has been reported after mRNA vaccination at a rate ranging between 5 and 160 per million recipients.174, 175, 176, 177 In Diaz et al, myocarditis occurred early (median 3.5 days) after vaccination, was more likely in young male adults (75% males, median age 36) and more often after the second dose.178 In two recent large studies of individuals who received mRNA vaccine in Israel,179 , 180 there was a significant preponderance of post-vaccine myocarditis towards young males with most myocarditis occurring after second dose, and most were mild. Pericarditis was more delayed (20 days after vaccination) and tended to affect older adults (median age 59). Patients tend to have elevated blood biomarkers of myocardial injury and cardiac MRI findings including regional LV dysfunction, late gadolinium enhancement and elevated native T1 and T2 signals.175 Yet, the clinical course for these patients was typically benign in the short term without reported late sequelae.
It is important to note that myocarditis has also been described after other vaccinations such as small pox (eosinophilic-lymphocytic),181 DTaP (Diphtheria, Tetanus, and Polio) which are thought to be due to hypersensitivity reactions,182 and even seasonal influenza vaccines.183 Data on the incidence of myocarditis with non-COVID19 vaccinations are limited and are mostly reported in case reports and small series. In a recent review of myocarditis in the Vaccine Adverse Event Reporting System from 1990 to 2018,184 most reports were in males and most occurred within 2 weeks of vaccination. Implicated vaccines varied by age group, but overall were due to vaccinations for smallpox (59%) and anthrax (23%), but other vaccinations were also implicated including influenza, zoster, hepatitis B and Haemophilus influenzae type b.
Impact of COVID19 pandemic on patients with cardiovascular disease
The COVID19 pandemic has affected all aspects of healthcare delivery and even impacted those without COVID-19, especially those chronic diseases. For example, during various times in the pandemic, the strain on healthcare resources by COVID19 infected patients has led to deferral of elective procedures, including cardiac catheterizations and cardiac surgeries.185, 186, 187 Several trends were observed from large registries and single center studies which illustrate how the systems of care required for the routine management of cardiovascular disease has been disrupted for the worse. For example, patients with myocardial infarction more often had delayed presentations and poorer outcomes compared with pre-pandemic era.188, 189, 190 Other changes in healthcare delivery such as greater capacity for telehealth may ultimately lead to neutral or even beneficial effects. In patient with suspected coronary artery disease, there has been a shift from exercise stress testing to anatomic testing with coronary CT angiography due to the concern for exercise aerosolization and infection risk for the staff of the stress laboratories.191 Thus, studies which examine the long-term impact of these changes in care delivery may allow for data-driven optimization of chronic disease management which persist long after the pressures of the pandemic has passed.
SUMMARY AND CONCLUDING REMARKS
Despite the unimaginable toll the COVID-19 pandemic has extracted on the world, the investments in science and medicine over the past 100 years have made it possible to make and translate discoveries in real time. The capacity to identify and sequence the virus, develop vaccines and therapeutics, and adapt systems of care were impossible in previous epidemics. However, the remarkable variability in severity and clinical manifestations of SARS-COV2 infection remains among the most puzzling aspects to the COVID-19 pandemic. An example of this is cardiac injury, which occurs commonly but is not uniformly observed, even in those with fatal outcomes. Imaging abnormalities have even been described among those with minimal respiratory manifestations.
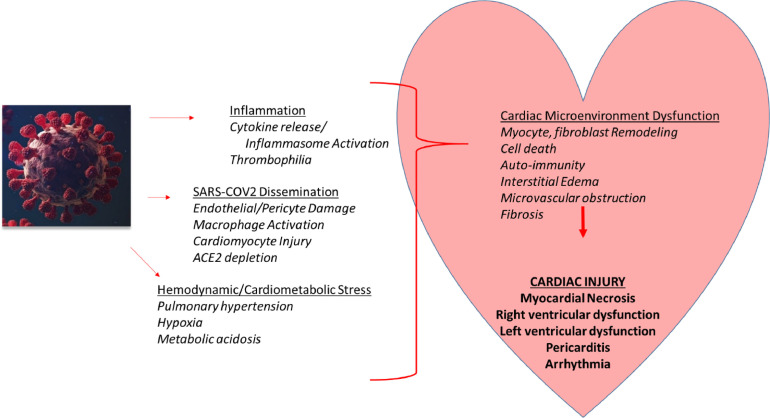
Studies to date suggest that the underlying pathophysiology of COVID-19 associated cardiac injury may be multi-factorial (Figure 1 ), derived from both systemic pertubations (hyper-inflammation and thrombophilia) and possible direct effects of the virus. Unlike influenza B, atherothrombosis occurs after SARS-COV2 infection but is not the major mechanism accounting for cardiovascular risk in this setting. Studies to date suggest that viral deposition or expression is not uncommon, but classic features of lymphocytic myocarditis are rarely observed. Instead, direct potential cardiotoxic effects of SARS-COV2 could stem from disruption of the RAS system, a microangiopathy via endothelial cell/pericyte involvement (akin to parvovirus), or cardiomyocyte damage (akin to coxsackie B). Thus, a major current challenge is to determine (at the individual and population levels) whether SARS-COV2, when localized to the heart, contributes to cardiac injury. Prospective interventional trials will likely become critical to elucidating the specific contribution of these possible mechanisms.
Fig 1.
Cardiac Injury as a Result of Multiple Mechanisms, Triggered by SARS-COV2. SARS-COV2 incites a host response which stimulates pro-inflammatory and pro-thrombotic pathways with potential adverse effects on the cardiac microenvironment. SARS-CoV2 viral particles have also been identified in the heart of some with severe COVID-19, raising the possibility that dissemination of the virus to the heart may mediate cardiac injury. Given the cardio-protective role of ACE2 for homeostatic maintenance of the cardiac microenvironment, additional damage may occur through depletion of ACE2. In those with severe acute illness, hemodynamic and cardiometabolic stressors also likely contribute to the adverse cardiovascular effects. Thus, cardiac injury may represent a common final pathway, reflecting multiple pathways triggered by the SARS-COV2 and the host response, leading to compromised cardiovascular performance.
As the world passes 200 million cases of (documented) SARS-COV2, even the possibility of low frequency persistent cardiovascular effects or risk constitute a substantial threat to global public health for years to come. Continued work is therefore needed to refine cardiovascular risk stratification and the clinical management of SARS-COV2 infection to minimize not only survival, but long-term organ function, including extra-pulmonary tissues such as the heart, kidneys, and brain. The relationship between immune activation and cardiovascular disease is not unique to SARS-COV2, and common cardiovascular problems (atherosclerosis, arrhythmias, cardiomyopathies) are often rooted in inflammation and/or repair, sometimes from viral exposures. Thus, in this time of unprecedented suffering and risk to global health, there exists the opportunity that well conducted translational research of SARS-COV2 may also shed light on our understanding of cardiovascular resilience in general and thus pay health dividends that outlast the current pandemic.
ACKNOWLEDGMENTS
This study was funded in part by the National Institutes of Health and the National Cancer Institute (U01CA260513; Zidar) as well as the United States Veteran Administration (COVID19-8900-05; Zidar). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Veteran Affairs or the National Institutes of Health. Both authors have read the journal's policy on disclosure of potential conflicts of interest and no conflict of interest exists between any of the authors and the contents of this paper. Both authors of the manuscript made substantive contributions to 1) the conception and design or analysis and interpretation of the data, 2) drafting or revising the manuscript, and 3) final approval of the manuscript.
Conflicts of Interest: All authors have read the journal's policy on disclosure of potential conflicts of interest and have none to declare.
REFERENCES
- 1.Zhao B-C, Liu W-F, Lei S-H, et al. Prevalence and prognostic value of elevated troponins in patients hospitalised for coronavirus disease 2019: a systematic review and meta-analysis. J Intensive Care. 2020;8:88. doi: 10.1186/s40560-020-00508-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toloui A, Moshrefiaraghi D, Madani Neishaboori A, Yousefifard M, Haji Aghajani M. Cardiac complications and pertaining mortality rate in COVID-19 patients; a systematic review and meta-analysis. Arch Acad Emerg Med. 2021;9:e18. doi: 10.22037/aaem.v9i1.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Higuchi Y, McTiernan CF, Frye CB, McGowan BS, Chan TO, Feldman AM. Tumor necrosis factor receptors 1 and 2 differentially regulate survival, cardiac dysfunction, and remodeling in transgenic mice with tumor necrosis factor-alpha-induced cardiomyopathy. Circulation. 2004;109:1892–1897. doi: 10.1161/01.CIR.0000124227.00670.AB. [DOI] [PubMed] [Google Scholar]
- 5.Fischer P, Hilfiker-Kleiner D. Role of gp130-mediated signalling pathways in the heart and its impact on potential therapeutic aspects. Br J Pharmacol. 2008;153(Suppl 1):S414–S427. doi: 10.1038/bjp.2008.1. Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen G, Chelu MG, Dobrev D, Li N. Cardiomyocyte inflammasome signaling in cardiomyopathies and atrial fibrillation: mechanisms and potential therapeutic implications. Front Physiol. 2018;9:1115. doi: 10.3389/fphys.2018.01115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bozkurt B, Kribbs SB, Clubb FJ, Jr., et al. Pathophysiologically relevant concentrations of tumor necrosis factor-alpha promote progressive left ventricular dysfunction and remodeling in rats. Circulation. 1998;97:1382–1391. doi: 10.1161/01.cir.97.14.1382. [DOI] [PubMed] [Google Scholar]
- 8.Meléndez GC, McLarty JL, Levick SP, Du Y, Janicki JS, Brower GL. Interleukin 6 mediates myocardial fibrosis, concentric hypertrophy, and diastolic dysfunction in rats. Hypertension. 2010;56:225–231. doi: 10.1161/HYPERTENSIONAHA.109.148635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kubota T, McTiernan CF, Frye CS, et al. Dilated cardiomyopathy in transgenic mice with cardiac-specific overexpression of tumor necrosis factor-alpha. Circ Res. 1997;81:627–635. doi: 10.1161/01.res.81.4.627. [DOI] [PubMed] [Google Scholar]
- 10.Yu Q, Vazquez R, Khojeini EV, Patel C, Venkataramani R, Larson DF. IL-18 induction of osteopontin mediates cardiac fibrosis and diastolic dysfunction in mice. Am J Physiol Heart Circ Physiol. 2009;297:H76–H85. doi: 10.1152/ajpheart.01285.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amgalan D, Chen Y, Kitsis RN. Death receptor signaling in the heart. Circulation. 2017;136:743–746. doi: 10.1161/CIRCULATIONAHA.117.029566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeng C, Duan F, Hu J, et al. NLRP3 inflammasome-mediated pyroptosis contributes to the pathogenesis of non-ischemic dilated cardiomyopathy. Redox Biol. 2020;34 doi: 10.1016/j.redox.2020.101523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kapadia SR, Yakoob K, Nader S, Thomas JD, Mann DL, Griffin BP. Elevated circulating levels of serum tumor necrosis factor-alpha in patients with hemodynamically significant pressure and volume overload. J Am Coll Cardiol. 2000;36:208–212. doi: 10.1016/s0735-1097(00)00721-x. [DOI] [PubMed] [Google Scholar]
- 14.Damås JK, Eiken HG, Oie E, et al. Myocardial expression of CC- and CXC-chemokines and their receptors in human end-stage heart failure. Cardiovasc Res. 2000;47:778–787. doi: 10.1016/s0008-6363(00)00142-5. [DOI] [PubMed] [Google Scholar]
- 15.Haudek SB, Taffet GE, Schneider MD, Mann DL. TNF provokes cardiomyocyte apoptosis and cardiac remodeling through activation of multiple cell death pathways. J Clin Invest. 2007;117:2692–2701. doi: 10.1172/JCI29134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sriramula S, Haque M, Majid DSA, Francis J. Involvement of tumor necrosis factor-α in angiotensin II–mediated effects on salt appetite, hypertension, and cardiac hypertrophy. Hypertension. 2008;51:1345–1351. doi: 10.1161/HYPERTENSIONAHA.107.102152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fitzgerald JC, Weiss SL, Maude SL, et al. Cytokine release syndrome after chimeric antigen receptor T cell therapy for acute lymphoblastic leukemia. Critic Care Med. 2017;45:e124–e131. doi: 10.1097/CCM.0000000000002053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shalabi H, Sachdev V, Kulshreshtha A, et al. Impact of cytokine release syndrome on cardiac function following CD19 CAR-T cell therapy in children and young adults with hematological malignancies. J ImmunoTher Cancer. 2020;8 doi: 10.1136/jitc-2020-001159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alvi RM, Frigault MJ, Fradley MG, et al. Cardiovascular events among adults treated with chimeric antigen receptor T-cells (CAR-T) J Am Coll Cardiol. 2019;74:3099–3108. doi: 10.1016/j.jacc.2019.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Torre-Amione G, Kapadia S, Benedict C, Oral H, Young JB, Mann DL. Proinflammatory cytokine levels in patients with depressed left ventricular ejection fraction: a report from the Studies of Left Ventricular Dysfunction (SOLVD) J Am Coll Cardiol. 1996;27:1201–1206. doi: 10.1016/0735-1097(95)00589-7. [DOI] [PubMed] [Google Scholar]
- 21.Aukrust P, Ueland T, Lien E, et al. Cytokine network in congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1999;83:376–382. doi: 10.1016/s0002-9149(98)00872-8. [DOI] [PubMed] [Google Scholar]
- 22.Devaux B, Scholz D, Hirche A, Klövekorn WP, Schaper J. Upregulation of cell adhesion molecules and the presence of low grade inflammation in human chronic heart failure. Eur Heart J. 1997;18:470–479. doi: 10.1093/oxfordjournals.eurheartj.a015268. [DOI] [PubMed] [Google Scholar]
- 23.Mann DL, McMurray JJ, Packer M, et al. Targeted anticytokine therapy in patients with chronic heart failure: results of the Randomized Etanercept Worldwide Evaluation (RENEWAL) Circulation. 2004;109:1594–1602. doi: 10.1161/01.CIR.0000124490.27666.B2. [DOI] [PubMed] [Google Scholar]
- 24.Chung ES, Packer M, Lo KH, Fasanmade AA, Willerson JT. Investigators ftA. randomized, double-blind, placebo-controlled, pilot trial of infliximab, a chimeric monoclonal antibody to tumor necrosis factor-α, in patients with moderate-to-severe heart failure: results of the anti-tnf therapy against congestive heart failure (ATTACH) trial. Circulation. 2003;107:3133–3140. doi: 10.1161/01.CIR.0000077913.60364.D2. [DOI] [PubMed] [Google Scholar]
- 25.Balakumar P, Singh M. Anti-tumour necrosis factor-α therapy in heart failure: future directions. Basic Clin Pharmacol Toxicol. 2006;99:391–397. doi: 10.1111/j.1742-7843.2006.pto_508.x. [DOI] [PubMed] [Google Scholar]
- 26.Deswal A, Bozkurt B, Seta Y, et al. Safety and efficacy of a soluble p75 tumor necrosis factor receptor (Enbrel, Etanercept) in patients with advanced heart failure. Circulation. 1999;99:3224–3226. doi: 10.1161/01.cir.99.25.3224. [DOI] [PubMed] [Google Scholar]
- 27.Tardif J-C, Kouz S, Waters DD, et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med. 2019;381:2497–2505. doi: 10.1056/NEJMoa1912388. [DOI] [PubMed] [Google Scholar]
- 28.Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 29.Blagova O, Varionchik N, Zaidenov V, Savina P, Sarkisova N. Anti-heart antibodies levels and their correlation with clinical symptoms and outcomes in patients with confirmed or suspected diagnosis COVID-19. Eur J Immunol. 2021;51:893–902. doi: 10.1002/eji.202048930. [DOI] [PubMed] [Google Scholar]
- 30.Sacchi MC, Tamiazzo S, Stobbione P, et al. SARS-CoV-2 infection as a trigger of autoimmune response. Clin Transl Sci. 2021;14:898–907. doi: 10.1111/cts.12953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sacchi MC, Tamiazzo S, Lauritano EC, Bonometti R. Case report of COVID-19 in an elderly patient: could SARS-CoV2 trigger myositis? Eur Rev Med Pharmacol Sci. 2020;24:11960–11963. doi: 10.26355/eurrev_202011_23857. [DOI] [PubMed] [Google Scholar]
- 32.Wallukat G, Hohberger B, Wenzel K, et al. Functional autoantibodies against G-protein coupled receptors in patients with persistent Long-COVID-19 symptoms. J Transl Autoimmun. 2021;4 doi: 10.1016/j.jtauto.2021.100100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kelly J, Rudd A, Lewis RR, Hunt BJ. Screening for subclinical deep-vein thrombosis. QJM: Int J Med. 2001;94:511–519. doi: 10.1093/qjmed/94.10.511. [DOI] [PubMed] [Google Scholar]
- 34.Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost. 2000;83:14–19. [PubMed] [Google Scholar]
- 35.Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378:345–353. doi: 10.1056/NEJMoa1702090. [DOI] [PubMed] [Google Scholar]
- 36.Clar C, Oseni Z, Flowers N, Keshtkar-Jahromi M, Rees K. Influenza vaccines for preventing cardiovascular disease. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD005050.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ma T-T, Wong ICK, Man KKC, et al. Effect of evidence-based therapy for secondary prevention of cardiovascular disease: Systematic review and meta-analysis. Plos One. 2019;14 doi: 10.1371/journal.pone.0210988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zidar DA, Juchnowski S, Ferrari B, et al. Oxidized LDL levels are increased in HIV infection and may drive monocyte activation. JAIDS J Acquir Immune Defic Syndr. 2015;69:154–160. doi: 10.1097/QAI.0000000000000566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Funderburg NT, Mayne E, Sieg SF, et al. Increased tissue factor expression on circulating monocytes in chronic HIV infection: relationship to in vivo coagulation and immune activation. Blood. 2010;115:161–167. doi: 10.1182/blood-2009-03-210179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.von Bruhl ML, Stark K, Steinhart A, et al. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J Exp Med. 2012;209:819–835. doi: 10.1084/jem.20112322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dann R, Hadi T, Montenont E, et al. Platelet-derived MRP-14 induces monocyte activation in patients with symptomatic peripheral artery disease. J Am Coll Cardiol. 2018;71:53–65. doi: 10.1016/j.jacc.2017.10.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.da Costa Martins PA, van Gils JM, Mol A, Hordijk PL, Zwaginga JJ. Platelet binding to monocytes increases the adhesive properties of monocytes by up-regulating the expression and functionality of beta1 and beta2 integrins. J Leukoc Biol. 2006;79:499–507. doi: 10.1189/jlb.0605318. [DOI] [PubMed] [Google Scholar]
- 43.Bonaventura A, Liberale L, Carbone F, et al. The pathophysiological role of neutrophil extracellular traps in inflammatory diseases. Thromb Haemost. 2018;118:6–27. doi: 10.1160/TH17-09-0630. [DOI] [PubMed] [Google Scholar]
- 44.Freeman ML, Panigrahi S, Chen B, Juchnowski S, Sieg SF, Lederman MM, Funderburg NT, Zidar DA. CD8+ T-Cell-Derived Tumor Necrosis Factor Can Induce Tissue Factor Expression on Monocytes. J Infect Dis. 2019;220:73–77. doi: 10.1093/infdis/jiz051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nawroth PP, Stern DM. Modulation of endothelial cell hemostatic properties by tumor necrosis factor. J Exp Med. 1986;163:740–745. doi: 10.1084/jem.163.3.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Furio E, García-Fuster MJ, Redon J, et al. CX3CR1/CX3CL1 Axis Mediates Platelet-Leukocyte Adhesion to Arterial Endothelium in Younger Patients with a History of Idiopathic Deep Vein Thrombosis. Thromb Haemost. 2018;118:562–571. doi: 10.1055/s-0038-1629897. [DOI] [PubMed] [Google Scholar]
- 47.Schulz C, Schäfer A, Stolla M, et al. Chemokine fractalkine mediates leukocyte recruitment to inflammatory endothelial cells in flowing whole blood: a critical role for P-selectin expressed on activated platelets. Circulation. 2007;116:764–773. doi: 10.1161/CIRCULATIONAHA.107.695189. [DOI] [PubMed] [Google Scholar]
- 48.Verschoor A, Langer HF. Crosstalk between platelets and the complement system in immune protection and disease. Thromb Haemost. 2013;110:910–919. doi: 10.1160/TH13-02-0102. [DOI] [PubMed] [Google Scholar]
- 49.Peerschke EI, Yin W, Ghebrehiwet B. Complement activation on platelets: implications for vascular inflammation and thrombosis. Mol Immunol. 2010;47:2170–2175. doi: 10.1016/j.molimm.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Del Valle DM, Kim-Schulze S, Huang H-H, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med. 2020;26:1636–1643. doi: 10.1038/s41591-020-1051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2020;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Klinkhammer B, Go R, Hollenberg S, et al. Troponin correlates with inflammatory markers in COVID-19. J Am Coll Cardiol. 2021;77(18_Supplement_1):3029. [Google Scholar]
- 53.Khan M, Shah N, Mushtaq H, Jehanzeb V. Profiling laboratory biomarkers associated with COVID-19 disease progression: a single-center experience. Int J Microbiol. 2021;2021 doi: 10.1155/2021/6643333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Basso C, Leone O, Rizzo S, et al. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J. 2020;41:3827–3835. doi: 10.1093/eurheartj/ehaa664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dal Ferro M, Bussani R, Paldino A, et al. SARS-CoV-2, myocardial injury and inflammation: insights from a large clinical and autopsy study. Clin Res Cardiol. 2021;110(11):1–10. doi: 10.1007/s00392-021-01910-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abbasi J. Researchers investigate what COVID-19 does to the heart. JAMA. 2021;325:808–811. doi: 10.1001/jama.2021.0107. [DOI] [PubMed] [Google Scholar]
- 57.Kac Michael Sayegh, Lanfang Wang, Hoang Timothy, et al. Systemic inflammation in acute SARS-CoV-2 infection may lead to elevated cardiac cytokines and adverse remodeling. Circ Res. 2020;127:E273. [Google Scholar]
- 58.Deftereos SG, Giannopoulos G, Vrachatis DA, et al. Effect of colchicine vs standard care on cardiac and inflammatory biomarkers and clinical outcomes in patients hospitalized with coronavirus disease 2019: The GRECCO-19 randomized clinical trial. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.13136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hermine O, Mariette X, Tharaux PL, Resche-Rigon M, Porcher R, Ravaud P. Effect of tocilizumab vs usual care in adults hospitalized with COVID-19 and moderate or severe pneumonia: a randomized clinical trial. JAMA Intern Med. 2021;181:32–40. doi: 10.1001/jamainternmed.2020.6820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Salvarani C, Dolci G, Massari M, et al. Effect of tocilizumab vs standard care on clinical worsening in patients hospitalized with COVID-19 pneumonia: a randomized clinical trial. JAMA Intern Med. 2021;181:24–31. doi: 10.1001/jamainternmed.2020.6615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stone JH, Frigault MJ, Serling-Boyd NJ, et al. Efficacy of tocilizumab in patients hospitalized with Covid-19. N Engl J Med. 2020;383:2333–2344. doi: 10.1056/NEJMoa2028836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rosas IO, Bräu N, Waters M, et al. Tocilizumab in hospitalized patients with severe Covid-19 pneumonia. N Engl J Med. 2021;384:1503–1516. doi: 10.1056/NEJMoa2028700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Salama C, Han J, Yau L, et al. Tocilizumab in patients hospitalized with Covid-19 pneumonia. N Engl J Med. 2020;384:20–30. doi: 10.1056/NEJMoa2030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Weber BN, Zhou G, Kim A, et al. Impact of interleukin-6 receptor blockade with tocilizumab on cardiac injury in patients with COVID-19: a retrospective cohort study. Open Forum Infect Dis. 2021;8(2) doi: 10.1093/ofid/ofab012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bonaventura A, Vecchié A, Dagna L, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol. 2021;21:319–329. doi: 10.1038/s41577-021-00536-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Elbadawi A, Elgendy IY, Sahai A, et al. Incidence and outcomes of thrombotic events in symptomatic patients with COVID-19. Arterioscler Thromb Vasc Biol. 2020;41(1) doi: 10.1161/ATVBAHA.120.315304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA. 2020;324:799–801. doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Klok FA, Kruip M, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zuo Y, Yalavarthi S, Shi H, et al. Neutrophil extracellular traps in COVID-19. JCI Insight. 2020;5(11) doi: 10.1172/jci.insight.138999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang J, Li Q, Yin Y, et al. Excessive neutrophils and neutrophil extracellular traps in COVID-19. Front Immunol. 2020;11:2063. doi: 10.3389/fimmu.2020.02063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Veras FP, Pontelli MC, Silva CM, et al. SARS-CoV-2–triggered neutrophil extracellular traps mediate COVID-19 pathologySARS-CoV-2 directly triggers ACE-dependent NETs. Journal of Experimental Medicine. 2020;217(12) doi: 10.1084/jem.20201129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Manne BK, Denorme F, Middleton EA, et al. Platelet gene expression and function in patients with COVID-19. Blood. 2020;136:1317–1329. doi: 10.1182/blood.2020007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zaid Y, Puhm F, Allaeys I, Naya A, Oudghiri M, Khalki L, Limami Y, Zaid N, Sadki K, Ben El Haj R, Mahir W, Belayachi L, Belefquih B, Benouda A, Cheikh A, Langlois MA, Cherrah Y, Flamand L, Guessous F, Boilard E. Platelets Can Associate with SARS-Cov-2 RNA and Are Hyperactivated in COVID-19. Circ Res. 2020;127:1404–1418. doi: 10.1161/CIRCRESAHA.120.317703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang S, Liu Y, Wang X, et al. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J Hematol Oncol. 2020;13:120. doi: 10.1186/s13045-020-00954-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Holter JC, Pischke SE, de Boer E, et al. Systemic complement activation is associated with respiratory failure in COVID-19 hospitalized patients. Proc Nat Acad Sci. 2020;117:25018–25025. doi: 10.1073/pnas.2010540117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Java A, Apicelli AJ, Liszewski MK, et al. The complement system in COVID-19: friend and foe? JCI Insight. 2020;5 doi: 10.1172/jci.insight.140711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Escher F, Pietsch H, Aleshcheva G, et al. Detection of viral SARS-CoV-2 genomes and histopathological changes in endomyocardial biopsies. ESC Heart Fail. 2020;7:2440–2447. doi: 10.1002/ehf2.12805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Talasaz AH, Sadeghipour P, Kakavand H, et al. Recent randomized trials of antithrombotic therapy for patients with COVID-19. J Am Coll Cardiol. 2021;77:1903–1921. doi: 10.1016/j.jacc.2021.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Aretz Thomas, Myocarditis H. The dallas criteria. Hum Pathol. 1987;18:619–624. doi: 10.1016/s0046-8177(87)80363-5. [DOI] [PubMed] [Google Scholar]
- 81.McCarthy RE, 3rd, Boehmer JP, Hruban RH, et al. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med. 2000;342:690–695. doi: 10.1056/NEJM200003093421003. [DOI] [PubMed] [Google Scholar]
- 82.Baughman KL. Diagnosis of myocarditis: death of Dallas criteria. Circulation. 2006;113:593–595. doi: 10.1161/CIRCULATIONAHA.105.589663. [DOI] [PubMed] [Google Scholar]
- 83.Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72:3158–3176. doi: 10.1016/j.jacc.2018.09.072. [DOI] [PubMed] [Google Scholar]
- 84.Friedrich MG, Sechtem U, Schulz-Menger J, et al. Cardiovascular magnetic resonance in myocarditis: a JACC white paper. J Am Coll Cardiol. 2009;53:1475–1487. doi: 10.1016/j.jacc.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Klingel K, Sauter M, Bock CT, Szalay G, Schnorr JJ, Kandolf R. Molecular pathology of inflammatory cardiomyopathy. Med Microbiol Immunol. 2004;193:101–107. doi: 10.1007/s00430-003-0190-1. [DOI] [PubMed] [Google Scholar]
- 86.Duechting A, Tschöpe C, Kaiser H, et al. Human parvovirus B19 NS1 protein modulates inflammatory signaling by activation of STAT3/PIAS3 in human endothelial cells. J Virol. 2008;82:7942–7952. doi: 10.1128/JVI.00891-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Van Linthout S, Elsanhoury A, Klein O, et al. Telbivudine in chronic lymphocytic myocarditis and human parvovirus B19 transcriptional activity. ESC Heart Fail. 2018;5:818–829. doi: 10.1002/ehf2.12341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Henke A, Huber S, Stelzner A, Whitton JL. The role of CD8+ T lymphocytes in coxsackievirus B3-induced myocarditis. J Virol. 1995;69:6720–6728. doi: 10.1128/jvi.69.11.6720-6728.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lasrado N, Gangaplara A, Arumugam R, et al. Identification of Immunogenic Epitopes That Permit the Detection of Antigen-Specific T Cell Responses in Multiple Serotypes of Group B Coxsackievirus Infections. Viruses. 2020;12(3):347. doi: 10.3390/v12030347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Massilamany C, Upadhyaya B, Gangaplara A, Kuszynski C, Reddy J. Detection of autoreactive CD4 T cells using major histocompatibility complex class II dextramers. BMC Immunol. 2011;12:40. doi: 10.1186/1471-2172-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Huber SA, Job LP. Differences in cytolytic T cell response of BALB/c mice infected with myocarditic and non-myocarditic strains of coxsackievirus group B, type 3. Infect Immun. 1983;39:1419–1427. doi: 10.1128/iai.39.3.1419-1427.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schulze K, Witzenbichler B, Christmann C, Schultheiss HP. Disturbance of myocardial energy metabolism in experimental virus myocarditis by antibodies against the adenine nucleotide translocator. Cardiovasc Res. 1999;44:91–100. doi: 10.1016/s0008-6363(99)00204-7. [DOI] [PubMed] [Google Scholar]
- 93.Schulze K, Becker BF, Schauer R, Schultheiss HP. Antibodies to ADP-ATP carrier–an autoantigen in myocarditis and dilated cardiomyopathy–impair cardiac function. Circulation. 1990;81:959–969. doi: 10.1161/01.cir.81.3.959. [DOI] [PubMed] [Google Scholar]
- 94.Neumann DA, Rose NR, Ansari AA, Herskowitz A. Induction of multiple heart autoantibodies in mice with coxsackievirus B3- and cardiac myosin-induced autoimmune myocarditis. J Immunol. 1994;152:343–350. [PubMed] [Google Scholar]
- 95.Neumann DA, Lane JR, LaFond-Walker A, et al. Heart-specific autoantibodies can be eluted from the hearts of Coxsackievirus B3-infected mice. Clin Exp Immunol. 1991;86:405–412. doi: 10.1111/j.1365-2249.1991.tb02945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Neumann DA, Burek CL, Baughman KL, Rose NR, Herskowitz A. Circulating heart-reactive antibodies in patients with myocarditis or cardiomyopathy. J Am Coll Cardiol. 1990;16:839–846. doi: 10.1016/s0735-1097(10)80331-6. [DOI] [PubMed] [Google Scholar]
- 97.Neu N, Beisel KW, Traystman MD, Rose NR, Craig SW. Autoantibodies specific for the cardiac myosin isoform are found in mice susceptible to Coxsackievirus B3-induced myocarditis. J Immunol. 1987;138:2488–2492. [PubMed] [Google Scholar]
- 98.Li Y, Heuser JS, Cunningham LC, Kosanke SD, Cunningham MW. Mimicry and antibody-mediated cell signaling in autoimmune myocarditis. J Immunol. 2006;177:8234–8240. doi: 10.4049/jimmunol.177.11.8234. [DOI] [PubMed] [Google Scholar]
- 99.Massilamany C, Gangaplara A, Reddy J. Intricacies of cardiac damage in coxsackievirus B3 infection: implications for therapy. Int J Cardiol. 2014;177:330–339. doi: 10.1016/j.ijcard.2014.09.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Schultheiss HP, Piper C, Sowade O, et al. Betaferon in chronic viral cardiomyopathy (BICC) trial: Effects of interferon-β treatment in patients with chronic viral cardiomyopathy. Clin Res Cardiol. 2016;105:763–773. doi: 10.1007/s00392-016-0986-9. [DOI] [PubMed] [Google Scholar]
- 101.Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem. 2000;275:33238–33243. doi: 10.1074/jbc.M002615200. [DOI] [PubMed] [Google Scholar]
- 102.Donoghue M, Hsieh F, Baronas E, et al. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9. Circ Res. 2000;87:E1–E9. doi: 10.1161/01.res.87.5.e1. [DOI] [PubMed] [Google Scholar]
- 103.Hikmet F, Méar L, Edvinsson Å, Micke P, Uhlén M, Lindskog C. The protein expression profile of ACE2 in human tissues. Mol Syst Biol. 2020;16:e9610. doi: 10.15252/msb.20209610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nicin L, Abplanalp WT, Mellentin H, et al. Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts. Eur Heart J. 2020;41:1804–1806. doi: 10.1093/eurheartj/ehaa311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res. 2020;116:1097–1100. doi: 10.1093/cvr/cvaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tucker NR, Chaffin M, Bedi KC, et al. Myocyte-Specific Upregulation of ACE2in Cardiovascular Disease. Circulation. 2020;142:708–710. doi: 10.1161/CIRCULATIONAHA.120.047911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lin HB, Liu PP. COVID-19 and the Heart: ACE2 Level and the Company it Keeps Hold the Key. JACC Basic Transl Sci. 2020;5:884–887. doi: 10.1016/j.jacbts.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bristow MR, Zisman LS, Altman NL, et al. Dynamic regulation of SARS-Cov-2 binding and cell entry mechanisms in remodeled human ventricular myocardium. JACC Basic Transl Sci. 2020;5:871–883. doi: 10.1016/j.jacbts.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bristow MR, Zisman LS, Altman NL, et al. Dynamic regulation of SARS-Cov-2 binding and cell entry mechanisms in remodeled human ventricular myocardium. JACC Basic Transl Sci. 2020;5:871–883. doi: 10.1016/j.jacbts.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tavazzi G, Pellegrini C, Maurelli M, et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911–915. doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Edler C, Schröder AS, Aepfelbacher M, et al. Dying with SARS-CoV-2 infection-an autopsy study of the first consecutive 80 cases in Hamburg, Germany. Int J Legal Med. 2020;134:1275–1284. doi: 10.1007/s00414-020-02317-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Resp Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sekulic M, Harper H, Nezami BG, et al. Molecular detection of SARS-CoV-2 infection in FFPE samples and histopathologic findings in fatal SARS-CoV-2 cases. Am J Clin Pathol. 2020;154:190–200. doi: 10.1093/ajcp/aqaa091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Schaller T, Hirschbühl K, Burkhardt K, et al. Postmortem examination of patients with COVID-19. Jama. 2020;323:2518–2520. doi: 10.1001/jama.2020.8907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wichmann D, Sperhake J-P, Lütgehetmann M, et al. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann Intern Med. 2020;173:268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Fox SE, Li G, Akmatbekov A, et al. Unexpected features of cardiac pathology in COVID-19 infection. Circulation. 2020;142:1123–1125. doi: 10.1161/CIRCULATIONAHA.120.049465. [DOI] [PubMed] [Google Scholar]
- 117.Lindner D, Fitzek A, Bräuninger H, et al. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. 2020;5:1281–1285. doi: 10.1001/jamacardio.2020.3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bailey AL, Dmytrenko O, Greenberg L, et al. SARS-CoV-2 infects human engineered heart tissues and models COVID-19 myocarditis. JACC Basic Transl Sci. 2021;6:331–345. doi: 10.1016/j.jacbts.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bulfamante GP, Perrucci GL, Falleni M, et al. Evidence of SARS-CoV-2 Transcriptional Activity in Cardiomyocytes of COVID-19 Patients without Clinical Signs of Cardiac Involvement. Biomedicines. 2020;8(12):626. doi: 10.3390/biomedicines8120626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pellegrini D, Kawakami R, Guagliumi G, et al. Microthrombi as a major cause of cardiac injury in COVID-19. Circulation. 2021;143:1031–1042. doi: 10.1161/CIRCULATIONAHA.120.051828. [DOI] [PubMed] [Google Scholar]
- 121.Halushka MK, Vander Heide RS. Myocarditis is rare in COVID-19 autopsies: cardiovascular findings across 277 postmortem examinations. Cardiovasc Pathol. 2021;50 doi: 10.1016/j.carpath.2020.107300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Imai Y, Kuba K, Penninger JM. The discovery of angiotensin-converting enzyme 2 and its role in acute lung injury in mice. Exp Physiol. 2008;93:543–548. doi: 10.1113/expphysiol.2007.040048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Crackower MA, Sarao R, Oudit GY, et al. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature. 2002;417:822–828. doi: 10.1038/nature00786. [DOI] [PubMed] [Google Scholar]
- 124.Abassi Z, Skorecki K, Hamo-Giladi DB, Kruzel-Davila E, Heyman SN. Kinins and chymase: the forgotten components of the renin-angiotensin system and their implications in COVID-19 disease. Am J Physiol Lung Cell Mol Physiol. 2021;320:L422–L429. doi: 10.1152/ajplung.00548.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yamamoto K, Ohishi M, Katsuya T, et al. Deletion of angiotensin-converting enzyme 2 accelerates pressure overload-induced cardiac dysfunction by increasing local angiotensin II. Hypertension. 2006;47:718–726. doi: 10.1161/01.HYP.0000205833.89478.5b. [DOI] [PubMed] [Google Scholar]
- 126.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281–292e286. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lan J, Ge J, Yu J, et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 128.Oudit GY, Kassiri Z, Jiang C, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39:618–625. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wu Z, Hu R, Zhang C, Ren W, Yu A, Zhou X. Elevation of plasma angiotensin II level is a potential pathogenesis for the critically ill COVID-19 patients. Critic Care. 2020;24:290. doi: 10.1186/s13054-020-03015-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Liu Y, Yang Y, Zhang C, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zoufaly A, Poglitsch M, Aberle JH, et al. Human recombinant soluble ACE2 in severe COVID-19. Lancet Respir Med. 2020;8:1154–1158. doi: 10.1016/S2213-2600(20)30418-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sandoval Y, Januzzi JL, Jr., Jaffe AS. Cardiac troponin for assessment of myocardial injury in COVID-19: JACC review topic of the week. J Am Coll Cardiol. 2020;76:1244–1258. doi: 10.1016/j.jacc.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Giustino G, Croft LB, Stefanini GG, et al. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol. 2020;76:2043–2055. doi: 10.1016/j.jacc.2020.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kho J, Ioannou A, Van den Abbeele K, Mandal AKJ, Missouris CG. Pulmonary embolism in COVID-19: Clinical characteristics and cardiac implications. Am J Emerg Med. 2020;38:2142–2146. doi: 10.1016/j.ajem.2020.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Giustino G, Croft LB, Oates CP, et al. Takotsubo cardiomyopathy in COVID-19. J Am Coll Cardiol. 2020;76:628–629. doi: 10.1016/j.jacc.2020.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Roca E, Lombardi C, Campana M, et al. Takotsubo Syndrome Associated with COVID-19. European journal of case reports in internal medicine. 2020;7(5) doi: 10.12890/2020_001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ho JS, Sia C-H, Chan MY, Lin W, Wong RC. Coronavirus-induced myocarditis: a meta-summary of cases. Heart Lung. 2020;49:681–685. doi: 10.1016/j.hrtlng.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Frustaci A, Francone M, Verardo R, Capobianchi MR, Chimenti C. Virus-negative necrotizing coronary vasculitis with aneurysm formation in human SARS-CoV-2 infection. Infect Dis Rep. 2021;13:597–601. doi: 10.3390/idr13030055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Argenziano MG, Bruce SL, Slater CL, et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. 2020;369:m1996. doi: 10.1136/bmj.m1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zeng JH, Wu WB, Qu JX, et al. Cardiac manifestations of COVID-19 in Shenzhen, China. Infection. 2020;48:861–870. doi: 10.1007/s15010-020-01473-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Dweck MR, Bularga A, Hahn RT, et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21:949–958. doi: 10.1093/ehjci/jeaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Karagodin I, Carvalho Singulane C, Woodward GM, et al. Echocardiographic correlates of in-hospital death in patients with acute COVID-19 infection: the world alliance societies of echocardiography (WASE-COVID) study. J Am Soc Echocardiogr. 2021;34:819–830. doi: 10.1016/j.echo.2021.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Li R, Wang H, Ma F, Cui GL, Peng LY, Li CZ, Zeng HS, Marian AJ, Wang DW. Widespread myocardial dysfunction in COVID-19 patients detected by myocardial strain imaging using 2-D speckle-tracking echocardiography. Acta Pharmacol Sin. 2021;42:1567–1574. doi: 10.1038/s41401-020-00595-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Kotecha T, Knight DS, Razvi Y, et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42:1866–1878. doi: 10.1093/eurheartj/ehab075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rajpal S, Tong MS, Borchers J, et al. Cardiovascular Magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol. 2021;6:116–118. doi: 10.1001/jamacardio.2020.4916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Daniels CJ, Rajpal S, Greenshields JT, Rosenthal GL, Chung EH, Terrin M, Jeudy J, Mattson SE, Law IH, Borchers J, Kovacs R, Kovan J, Rifat SF, Albrecht J, Bento AI, Albers L, Bernhardt D, Day C, Hecht S, Hipskind A, Mjaanes J, Olson D, Rooks YL, Somers EC, Tong MS, Wisinski J, Womack J, Esopenko C, Kratochvil CJ, Rink LD. Prevalence of Clinical and Subclinical Myocarditis in Competitive Athletes With Recent SARS-CoV-2 Infection: Results From the Big Ten COVID-19 Cardiac Registry. JAMA Cardiol. 2021;6:1078–1087. doi: 10.1001/jamacardio.2021.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Joy G, Artico J, Kurdi H, et al. Prospective case-control study of cardiovascular abnormalities 6 months following mild COVID-19 in healthcare workers. JACC Cardiovasc Imaging. 2021;14:2155–2166. doi: 10.1016/j.jcmg.2021.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Shafiabadi Hassani N, Talakoob H, Karim H, Mozafari Bazargany MH, Rastad H. Cardiac Magnetic Resonance Imaging Findings in 2954 COVID-19 Adult Survivors: A Comprehensive Systematic Review. Journal of magnetic resonance imaging: JMRI. 2021 doi: 10.1002/jmri.27852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Shafiabadi Hassani N, Talakoob H, Karim H, Mozafari Bazargany MH, Rastad H. Cardiac Magnetic Resonance Imaging Findings in 2954 COVID-19 Adult Survivors: A Comprehensive Systematic Review. J Magn Reson Imaging. 2021 doi: 10.1002/jmri.27852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Phelan D, Kim JH, Elliott MD, et al. Screening of Potential cardiac involvement in competitive athletes recovering from COVID-19: an expert consensus statement. JACC Cardiovasc Imaging. 2020;13:2635–2652. doi: 10.1016/j.jcmg.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Romiti GF, Corica B, Lip GYH, Proietti M. Prevalence and impact of atrial fibrillation in hospitalized patients with COVID-19: a systematic review and meta-analysis. J Clin Med. 2021;10:2490. doi: 10.3390/jcm10112490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.A Pardo Sanz, L Salido Tahoces, R Ortega Pérez, E González Ferrer, Á Sánchez Recalde, Zamorano Gómez JL. New-onset atrial fibrillation during COVID-19 infection predicts poor prognosis. Cardiol J. 2021;28:34–40. doi: 10.5603/CJ.a2020.0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Iacopino S, Placentino F, Colella J, et al. New-onset cardiac arrhythmias during COVID-19 hospitalization. Circulation Arrhythmia Electrophysiol. 2020;13 doi: 10.1161/CIRCEP.120.009040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Liao S-C, Shao S-C, Cheng C-W, Chen Y-C, Hung M-J. Incidence rate and clinical impacts of arrhythmia following COVID-19: a systematic review and meta-analysis of 17,435 patients. Critic Care. 2020;24:690. doi: 10.1186/s13054-020-03368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Demir OM, Ryan M, Cirillo C, et al. Impact and determinants of high-sensitivity cardiac Troponin-T concentration in patients with COVID-19 admitted to critical care. Am J Cardiol. 2021;147:129–136. doi: 10.1016/j.amjcard.2021.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Case BC, Yerasi C, Forrestal BJ, Shea C, Rappaport H, Medranda GA, Zhang C, Abramowitz J, Satler LF, Ben-Dor I, Hashim H, Rogers T, Waksman R. Clinical Impact and Predictors of Troponin Elevation in Patients With COVID-19. Cardiovascular revascularization medicine: including molecular interventions. 2021;33:41–44. doi: 10.1016/j.carrev.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, Zhao S, Somani S, Van Vleck T, Vaid A, Chaudhry F, De Freitas JK, Fayad ZA, Pinney SP, Levin M, Charney A, Bagiella E, Narula J, Glicksberg BS, Nadkarni G, Mancini DM, Fuster V. Prevalence and Impact of Myocardial Injury in Patients Hospitalized With COVID-19 Infection. J Am Coll Cardiol. 2020;76:533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Siddiqi HK, Weber B, Zhou G, et al. Increased prevalence of myocardial injury in patients with SARS-CoV-2 viremia. Am J Med. 2021;134:542–546. doi: 10.1016/j.amjmed.2020.09.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Pan C, Zhang Z, Luo L, et al. Cardiac T1 and T2 mapping showed myocardial involvement in recovered COVID-19 patients initially considered devoid of cardiac damage. J Magn reson Imaging JMRI. 2021;54:421–428. doi: 10.1002/jmri.27534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Lassen MCH, Skaarup KG, Lind JN, et al. Echocardiographic abnormalities and predictors of mortality in hospitalized COVID-19 patients: the ECHOVID-19 study. ESC Heart Fail. 2020;7:4189–4197. doi: 10.1002/ehf2.13044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Stockenhuber A, Vrettos A, Androschuck V, et al. A pilot study on right ventricular longitudinal strain as a predictor of outcome in COVID-19 patients with evidence of cardiac involvement. Echocardiography. 2021;38:222–229. doi: 10.1111/echo.14966. [DOI] [PubMed] [Google Scholar]
- 166.Janus SE, Hajjari J, Karnib M, Tashtish N, Al-Kindi SG, Hoit BD. Prognostic value of left ventricular global longitudinal strain in COVID-19. Am J Cardiol. 2020;131:134–136. doi: 10.1016/j.amjcard.2020.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Yang H, Liang X, Xu J, Hou H, Wang Y. Meta-analysis of atrial fibrillation in patients with COVID-19. Am J Cardiol. 2021;144:152–156. doi: 10.1016/j.amjcard.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Pranata R, Huang I, Raharjo SB. Incidence and impact of cardiac arrhythmias in coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. Indian Pacing Electrophysiol J. 2020;20:193–198. doi: 10.1016/j.ipej.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Schultz NH, Sørvoll IH, Michelsen AE, et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N Engl J Med. 2021;384:2124–2130. doi: 10.1056/NEJMoa2104882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med. 2021;384:2092–2101. doi: 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Scully M, Singh D, Lown R, et al. Pathologic antibodies to platelet factor 4 after ChAdOx1 nCoV-19 vaccination. N Engl J Med. 2021;384:2202–2211. doi: 10.1056/NEJMoa2105385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Cines DB, Bussel JB. SARS-CoV-2 vaccine–induced immune thrombotic thrombocytopenia. N Engl J Med. 2021;384:2254–2256. doi: 10.1056/NEJMe2106315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Montgomery J, Ryan M, Engler R, Hoffman D, McClenathan B, Collins L, Loran D, Hrncir D, Herring K, Platzer M, Adams N, Sanou A, Cooper LT., Jr Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol. 2021;6:1202–1206. doi: 10.1001/jamacardio.2021.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kim HW, Jenista ER, Wendell DC, Azevedo CF, Campbell MJ, Darty SN, Parker MA, Kim RJ. Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination. JAMA Cardiol. 2021;6:1196–1201. doi: 10.1001/jamacardio.2021.2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bautista García J, Peña Ortega P, Bonilla Fernández JA, Cárdenes León A, Ramírez Burgos L, Caballero Dorta E. Acute myocarditis after administration of the BNT162b2 vaccine against COVID-19. Rev Esp Cardiol. 2021;74:812–814. doi: 10.1016/j.rec.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Rosner CM, Genovese L, Tehrani BN, Atkins M, Bakhshi H, Chaudhri S, Damluji AA, de Lemos JA, Desai SS, Emaminia A, Flanagan MC, Khera A, Maghsoudi A, Mekonnen G, Muthukumar A, Saeed IM, Sherwood MW, Sinha SS, O'Connor CM, deFilippi CR. Myocarditis Temporally Associated With COVID-19 Vaccination. Circulation. 2021;144:502–505. doi: 10.1161/CIRCULATIONAHA.121.055891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A. Myocarditis and Pericarditis After Vaccination for COVID-19. Jama. 2021;326:1210–1212. doi: 10.1001/jama.2021.13443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Witberg G, Barda N, Hoss S, et al. Myocarditis after Covid-19 vaccination in a large health care organization. N Engl J Med. 2021;385:2132–2139. doi: 10.1056/NEJMoa2110737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Mevorach D, Anis E, Cedar N, Bromberg M, Haas EJ, Nadir E, Olsha-Castell S, Arad D, Hasin T, Levi N, Asleh R, Amir O, Meir K, Cohen D, Dichtiar R, Novick D, Hershkovitz Y, Dagan R, Leitersdorf I, Ben-Ami R, Miskin I, Saliba W, Muhsen K, Levi Y, Green MS. Keinan-Boker L and Alroy-Preis S. Myocarditis after BNT162b2 mRNA Vaccine against Covid-19 in Israel. N Engl J Med. 2021;385:2140–2149. doi: 10.1056/NEJMoa2109730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Murphy JG, Wright RS, Bruce GK, et al. Eosinophilic-lymphocytic myocarditis after smallpox vaccination. Lancet. 2003;362:1378–1380. doi: 10.1016/S0140-6736(03)14635-1. [DOI] [PubMed] [Google Scholar]
- 182.Boccara F, Benhaiem-Sigaux N, Cohen A. Acute myopericarditis after diphtheria, tetanus, and polio vaccination. Chest. 2001;120:671–672. doi: 10.1378/chest.120.2.671. [DOI] [PubMed] [Google Scholar]
- 183.Nagano N, Yano T, Fujita Y, et al. Hemodynamic collapse after influenza vaccination: a vaccine-induced fulminant myocarditis? Can J Cardiol. 2020;36:1554.e5--7. doi: 10.1016/j.cjca.2020.05.005. [DOI] [PubMed] [Google Scholar]
- 184.Su JR, McNeil MM, Welsh KJ, et al. Myopericarditis after vaccination, vaccine adverse event reporting system (VAERS), 1990–2018. Vaccine. 2021;39:839–845. doi: 10.1016/j.vaccine.2020.12.046. [DOI] [PubMed] [Google Scholar]
- 185.Ad N, Luc JGY, Nguyen TC, et al. Cardiac surgery in North America and coronavirus disease 2019 (COVID-19): regional variability in burden and impact. J Thorac Cardiovasc Surg. 2021;162:893–903.e894. doi: 10.1016/j.jtcvs.2020.06.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Ullah A, Fraser DGW, Fath-Ordoubadi F, Holt CM, Malik N. Decrease in cardiac catheterization and MI during COVID pandemic. Am Heart J Plus. 2021;1 doi: 10.1016/j.ahjo.2020.100001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Yong CM, Ang L, Welt FG, et al. Cardiac procedural deferral during the coronavirus (COVID-19) pandemic. Catheter Cardiovasc Interv. 2020;96:1080–1086. doi: 10.1002/ccd.29262. [DOI] [PubMed] [Google Scholar]
- 188.Aldujeli A, Hamadeh A, Briedis K, et al. Delays in presentation in patients with acute myocardial infarction during the COVID-19 pandemic. Cardiol Res. 2020;11:386–391. doi: 10.14740/cr1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation. Circulation. 2014;129:837–847. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Hammad TA, Parikh M, Tashtish N, et al. Impact of COVID-19 pandemic on ST-elevation myocardial infarction in a non-COVID-19 epicenter. Catheter Cardiovasc Interv. 2021;97:208–214. doi: 10.1002/ccd.28997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Pontone G, Scafuri S, Mancini ME, et al. Role of computed tomography in COVID-19. J Cardiovasc Comput Tomogr. 2021;15:27–36. doi: 10.1016/j.jcct.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]