1. Introduction
There is a strong link between limiting life-sustaining treatments(LST) and short-term outcomes, as is illustrated in a recent publication in this journal from Germany [1].
Once a patient has been admitted to the intensive care unit (ICU), limitation of LST is frequently discussed and applied. In the current pandemic, such information is of particular importance given the ongoing discussions in many countries about triage of (elderly) COVID-19 patients [2].
In this short communication we present data on the impact of limitation of LST on the outcome of elderly COVID-19 patients in Europe.
2. Methods
During the present COVID-19 pandemic we conducted a prospective multicentre observational study in elderly patients (≥70 years) with COVID-19 who were admitted to ICUs in Europe (ClinicalTrials.gov ID: NCT04321265) [3]. The main aim was to analyse the ICU, 30-day and 90-day mortality rates. We also recorded limitation of LST during the ICU stay, either as withholding or withdrawal of active treatment. No common definition of limitation of LST was applied as each ICU followed national guidelines. Patients were included in the study if they had a PCR-verified SARS-CoV-2 infection and if their age was ≥70 years. A pre-defined list of variables was collected at admission: co-morbidities, frailty using the Clinical Frailty Scale (CFS) organ dysfunction (SOFA score) and medication [4]. We also collected information on usual ICU procedures such as mode of ventilation, cardiovascular and renal support. Patients with complete data on treatment limitations, frailty and 30-day survival were included in this study.
3. Results
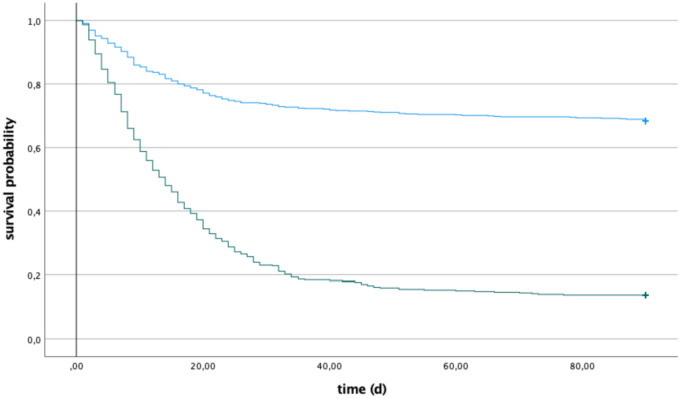
The study included 1266 patients with a mean age of 75 years, from 138 ICUs in 28 countries, admitted between 19th March and 26th May 2020. Table 1 shows data subdivided into two subgroups according to the presence or absence of limitation of LST during the ICU admission. Patients with limitation of LST were older, with a higher SOFA score and were more often frail (CFS of 4 or more). The overall 30-day mortality for the entire patient cohort was 43%. The number of patients, where limitation of LST was applied, was 466 (37%), most frequently due to withholding LST. The 30-day mortality of elderly patients with limitation of LST was 79%, where as the mortality of patients without such limitations was 23%. The cumulative number of deaths until day 90 in each group is shown in Fig. 1 as unadjusted Kaplan Meier survival curves.
Table 1.
Data on patients with (LST+) and without (LST-). Data given as median and IQR or %.
| Group | LST+ | LST- |
|---|---|---|
| N | 466 (37%) | 800 (64%) |
| Age (year) | 76 (73–80) | 74 (72–77) |
| ICU LOS (days) | 11 (4.8–21.2) | 11.3 (5–22.9) |
| SOFA score | 6 (3–8) | 5 (3–8) |
| Frailty (CFS ≥4)1 | 61% | 39% |
| Diabetes | 160 (25%) | 294 (37%) |
| Pulmonary Disease | 114 (24%) | 186 (23%) |
| Chronic heart failure | 78 (17%) | 117 (15%) |
| Hypertension | 304 (85%) | 464 (58%) |
| Mortality 30d2 | 79% | 23% |
| Mortality 90d3 | 86% | 32% |
p < 0.0001.
Fig. 1.
Kaplan Meyer survival curves: Patients with limitation of LST (LST+, bottom curve) and no limitation (LST-, upper curve).
4. Discussion
In this large international study, we found that the crude mortality in elderly patients with covid-19 is hugely influenced by the application of limitation of LST. This is not unexpected, and while several confounding factors are undoubtedly at play, the bottom line is that applying limitations on LST is strongly associated with outcome. Hence, the absence of such information in current published COVID-19 studies on outcome is surprising, especially in critically ill old patients. In fact, we have not found any recent major studies on outcome during the present pandemic where a detailed description of the use of limitation of LST is given [4,5]. This issue was neither revealed nor discussed in a recent meta-analysis. This is probably as the majority of studies included (91%) were retrospective in nature and medical records rarely document limitation of LST [6]. Limitation of LST is considered a controversial issue with a number of cultural challenges. It is therefore difficult to study and might be left out in order not to complicate the analysis. This is illustrated by the fact that there is a large variation between (European) countries in how often limitation of LST is instigated [7]. Additionally, the implementation of LST have been shown to change over time and was reported recently to have increased in some countries [8].
5. Conclusion
Limitation of LST was frequently found in this large European population of critically ill elderly COVID-19 patients and was strongly linked with mortality. We therefore would encourage the research community to reveal the use of limitation of LST in all cohort studies of critically ill patients where the main objective is outcome. Without such data it is difficult to assess the association of any other ICU variable or treatment modality in relation to short term outcomes. Both our data and the study by Bruno et al. [1] in this journal are a reminder of this.
Ethics approval and consent to participate
The study was carried out in 28 countries, mainly European, and each country received permission from national or regional research ethical committees and informed consent, when necessary.
Availability of data and materials
The dataset used and analysed during the study can be made available from the corresponding author on reasonable request.
Funding
This study was supported in France by a grant from Fondation Assistance Publique-Hôpitaux de Paris pour la recherche. In Norway, the study was supported by a grant from the Health Region West. In addition, the study was funded by a grant from the European Open Science Cloud (EOSC), EOSCsecretariat.eu has received funding from the European Union's Horizon Programme call H2020-INFRAEOSC-05-2018-2019, grant Agreement number 831644.
Declaration of Competing Interest
All authors declare no conflict of interest.
Acknowlegdement
The COVIP study group including all national and local investigators from 138 ICUs are thanked for their continuing support during the present pandemic.
References
- 1.Bruno R.R., Wernly B., Beil M., et al. Therapy limitation in octogenarians in German intensive care units is associated with a longer length of stay and increased 30 days mortality: A prospective multicenter study. J Crit Care. 2020;60:58–63. doi: 10.1016/j.jcrc.2020.07.024. [DOI] [PubMed] [Google Scholar]
- 2.DeJong C., Chen A.H., Lo B. An ethical framework for allocating scarce inpatient medications for COVID-19 in the US. JAMA. 2020;323(23):2367–2368. doi: 10.1001/jama.2020.8914. [DOI] [PubMed] [Google Scholar]
- 3.Jung C., Flaatten H., Fjølner J., et al. The impact of frailty on survival in elderly intensive care patients with COVID-19–the COVIP Study. Crit Care. 2021;25(149) doi: 10.21203/rs.3.rs-245592/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richardson S., JS Hirsch JS, M Narasimhan, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hewitt J., Carter B., Vilches-Moraga A. et al; COPE study collaborators. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;8:e444–e451. doi: 10.1016/S2468-2667(20)30146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dorjee K., Kim H., Bonomo E., Dolma R. Prevalence and predictors of death and severe disease in patients hospitalized due to COVID-19: A comprehensive systematic review and meta-analysis of 77 studies and 38,000 patients. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0243191. e0243191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guidet B., Flaatten H., Boumendil A., et al. Withholding or withdrawing of life-sustaining therapy in older adults (≥ 80 years) admitted to the intensive care unit. Intensive Care Med. 2018 May 17;43(1−11):1–12. doi: 10.1007/s00134-018-5196-7. [DOI] [PubMed] [Google Scholar]
- 8.Sprung C.L., Ricou B., Hartog C.S., et al. Changes in end-of-life practices in European intensive care units from 1999 to 2016. JAMA. 2019;322(17):1–12. doi: 10.1001/jama.2019.14608. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used and analysed during the study can be made available from the corresponding author on reasonable request.