On 1st January 2015, the first article was published in Digital Health: an editorial by its founders, Profs Theodoros N. Arvanitis and John Powell. 1 Six years on, as the journal receives its first Impact Factor, we reflect as an editorial team on how the journal has progressed in the context of the ever-changing field of digital health, and our vision for the future.
How the journal has developed since 2015
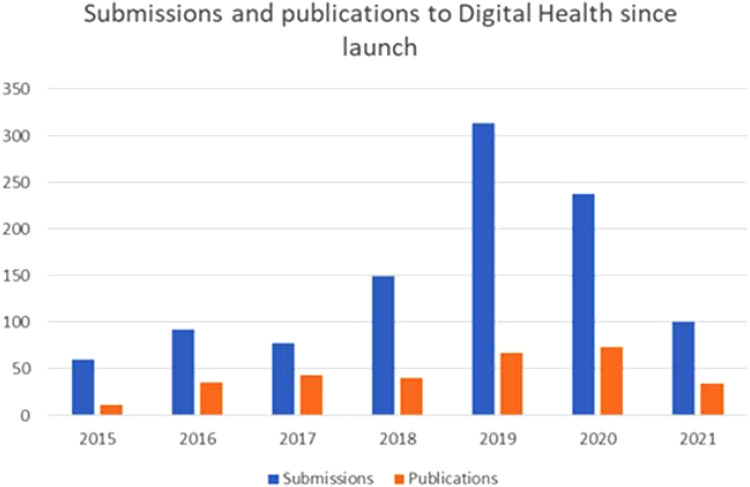
The first of the aims cited in that first editorial were for the journal to ‘provide an open access forum for high-quality, peer-reviewed academic papers in Digital Healthcare’ and to ‘become a high-impact international journal’. Under the guidance of our founding editors, we have published nearly 300 peer-reviewed papers since 2015 (Figure 1), and as of June 2021 have just been awarded our first Impact Factor of 3.495. As for the international reach of the journal (submissions from 46 different countries and publications from 30 different countries – see Figure 2), the editors have built up a worldwide network of collaborators, which now has at its core a transatlantic editorial team and extends to reviewers from across the globe.
Figure 1.
Yearly distribution for the journal’s submissions and published peer-review papers.
Figure 2.
Global distribution of countries for the journal's submissions and accepted published contributions.
Digital Health's founders also intended the journal to publish ‘articles of relevance to multiple stakeholders in the digital health revolution, including researchers, practitioners, patients, policy-makers, engineers and technology developers.’ Our themes include, but are not limited to, the areas of e-health, healthcare IT, health informatics, biomedical engineering, connected health, internet health care, social media and online social networks, telemedicine, telehealth, telecare, medical imaging, mobile health, mobile technologies, wearable devices, genomics and personal genetic information, personalized medicine, Big Data and data management, wellness and prevention, gerontology and social care services, simulation and gamification, patient accessibility, acceptability and behaviour, policy and regulation, and the social, political, cultural and ethical implications of advances in the field of digital healthcare. The breadth of our published articles is indeed representative of the interdisciplinary revolution of digital technologies in healthcare and the associated social care sector, bridging the evolution of advances in informatics and technology in medicine, health and all aspects of healthcare with the application of these developments in clinical practice, the patient experience, and their social, political and economic implications.
How the world of digital health has developed since 2015
The trends predicted by the editors in 2015 have by and large come to pass. We have indeed observed the ‘development of new technologies, particularly networked communications such as internet and mobile technologies, [and] trends towards smart, wearable and pervasive technologies’, as well as ‘the role of the empowered patient and the shift in models of health service delivery towards patient-centered care, and patient-led care, as seen in emphasis on self-management solutions.’ We have also witnessed the development of the Internet of Medical Things, connected devices, virtual reality, Big Data, algorithms and artificial intelligence.
The need ‘to find new approaches to addressing the demands of an ageing population with ever-increasing levels of long-term conditions, while reducing costs’ has provoked a great deal of research, and continues to be a key motivator in the digital health sector.
Something we did not foresee back in 2015 was the COVID-19 pandemic and its astounding impact on digital health solution development and uptake. The progress made will have a lasting effect, most notably in terms of telemedicine. Teleconsultations, in particular, have been normalized, with many patients hoping to retain the possibility of remote consultations after the pandemic, believing that they can facilitate access to doctors, reduce the number of people in emergency rooms, and solve the problem of medical deserts. Other developments have been the use of tele-expertise, the development of apps for telemonitoring, the uptake of telemedicine on a much wider scale (e.g., in institutions such as national health systems), remote consultations for people in quarantine or isolation, the development of ‘test and trace’ apps, and the use of ‘ePPE’ – patients in hospital receiving consultations through technology to reduce the risk of contamination. We have also observed advances in applications of AI, particularly in teleradiology, data analysis, trend prediction, workflow organization, and diagnosis, which can be especially useful in combination with tele-expertise. The pandemic also necessarily affected medical teaching, much of which was forced to become virtual. The journal received nearly 100 papers (of which 9 papers are being currently published) on COVID-19 in relation to digital health, covering topics such as surveillance of the disease via apps and public health monitoring, using telehealth and telemedicine to enable medical access remotely, the role of social media and big data in tracking and controlling the spread, digital management of disease, as well as the use of social media for public health education.
The future of digital health
Our hopes and expectations for the future are to see digital health solutions being developed as a response to medical deserts, healthcare inequality, ageing populations, and climate change, as well as other infectious disease outbreaks and chronic diseases, which threaten to become the next pandemic across countries with ageing populations. The COVID-19 outbreak clearly demonstrated the benefits of international digital communication, which allowed the rapid diffusion of information on a massive scale, synchronization of the international response, and collaboration between researchers. These communication channels will continue to be vital in the fight against pandemics, including that of chronic disease. We also expect to see a continued increase in the use of smartphones for disease tracking, communications, patient self-management and empowerment, and training of health professionals. We expect to see these trends across the globe, including in developing countries, where smartphones were widely used for tracking and diffusion of information during the pandemic.
The future of digital health is exciting and important, as digital health technology can be the catalyst for changing the way we deliver health and care provision to all citizens. In particular, in the ever-growing digital capability of our society, digital health technologies can effectively support disease management through the power of data and information. Through electronic healthcare records and complementary quantified self/self-management health and wellbeing digital signatures, an individual's health and wellbeing data is becoming more readily available and offers multiple opportunities in understanding the complexity of disease. As such, health and wellbeing data, originating from digital health technologies, can also provide better insights for the whole patient journey in the context of long-term conditions. Quality digital healthcare data, combined with currently available evidence-based medical knowledge, supports professionals in achieving informed, more precise, and personalized decisions on an individual patient's care delivery and management. Furthermore, digital solutions can offer the opportunity to transparently use this information and, hence, empower the individual patient/citizen in their awareness of health and wellbeing. Digitally enhanced patient empowerment directly involves the individual in their own health and wellbeing management. In this manner, digital health technologies can promote patients’ independence, supporting them in enhanced and socially integrated life activities. Finally, technology can promote the notion of a digital community, where patients, carers and citizens can exchange views and knowledge on the best available choices for an individual's health care and wellbeing options. Because of all the aforementioned benefits of digital health, we can observe that this digital revolution is transformative for healthcare, with a multitude of benefits to individuals and society as a whole. However, we must also consider the practical implications and potential pitfalls of digital healthcare technology. These include the economic models for telemedicine systems, the reimbursement of telemedical acts by insurance companies, and the security of patient data, particularly in light of recent hacking scandals involving hospitals. Particular attention should be given to the security of health and social care data in smartphone applications. In general, users (including healthcare professionals) should be made aware of the security risks associated with using such tools, and applications should be developed with data security and respect for patient privacy as priorities. Creators and users of the applications should also ensure that they operate within appropriate legal frameworks for data protection. This should help to prevent data leakages and reassure patients who are concerned about a ‘Big Brother’ state.
Additionally, although digital health solutions may be helpful in combatting climate change, it is important to remember that the production, maintenance, running and disposal of technological tools can be detrimental in this regard. We must also bear in mind accessibility to healthcare and the potential exclusion of people who are not technology-literate, who do not have internet access, or whose disability prevents them from using digital health solutions. Developing and integrating digital health solutions requires (and ideally facilitates) organizational changes, and their successful integration requires training for all potential users. For these reasons, we hope to see advancements in the education of health professionals in digital technologies and their applications. This is doubly important, as these same professionals will also be required to educate their patients and the wider public about the use of these technologies, convincing them to embrace a digitized health system that begins at home.
Above all, we must not lose sight of the patient. Improving the care, safety and experience of each individual patient should be the end goal of all our efforts.
The future of the digital health journal
With that vision of the future in mind, we aim to move forward as a journal by continuing to publish high-quality articles by a diverse range of authors from around the world, and we particularly welcome submissions from authors in developing countries. We hope to be at the forefront of discoveries in digital health, encouraging researchers to innovate and ensure the openness and scientific integrity of their research. We also wish to collaborate with academic societies in our field to increase the open access and visibility of the journal's reported scientific outputs and, hence, improve communication within the broader field of digital health.
We would like to thank our team of peer reviewers and associate editors for their investment in the success of the journal: Their work has been, and will continue to be, integral to our growth.
Footnotes
Conflict of interest: The authors have no conflicts of interest to declare.
Ethical approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Funding: No funding has been received for this editorial.
Informed consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial registration: Not applicable, because this article does not contain any clinical trials.
ORCID iDs: Thierry Moulin https://orcid.org/0000-0002-6639-8117
Jennifer Dobson https://orcid.org/0000-0001-5788-8563
John D Hixson https://orcid.org/0000-0003-3053-6474
Theodoros N Arvanitis https://orcid.org/0000-0001-5473-135X
Reference
- 1.Powell J, Arvanitis TN. Welcome to the digital health revolution. Digit Health 2015. 1:1. DOI: 10.1177/2055207614561571 [DOI] [PMC free article] [PubMed] [Google Scholar]