Abstract
Primary acinic cell carcinoma arising in the nose is exceptionally rare. In this report, we present a unique case of an acinic cell carcinoma of the nasal lateral wall, and it is only the second such case to be reported. We also engage in a systematic review of all 18 cases of acinic cell carcinoma of the nose reported in the literature in English so far.
Keywords: epistaxis, nasal cavity, nasal tumor, nasal mass, acinic cell carcinoma
Introduction
Acinic cell carcinoma is an uncommon salivary tumor, which arises most frequently in the parotid gland and rarely in the minor salivary glands [1]. Most of the acinic cell carcinomas originating in minor salivary glands have been found in the oral cavity [1]. Primary acinic cell carcinoma arising in the nose is exceptionally rare, and it is thought to account for only 1-4% of all malignant nasal neoplasms [2]. Only 18 cases of acinic cell carcinoma arising in the nasal cavity have been previously reported in the literature in English [3].
Case presentation
A 62-year-old male patient presented to our emergency room with a history of right nasal mass for 10 years. The patient reported occasionally experiencing epistaxis and in the last six months, there had been a slow, gradual growth. However, it had not been noticed during that period.
He had a round, soft, well-defined mass on the lateral nasal wall (Figure 1). An ultrasound revealed a solid oval lesion with some internal vascularization in the right wing of the nose, measuring 15 x 11 x 19 mm, which apparently caused an interruption of the cortical bone. For additional characterization of the lesion, a CT scan was performed. The CT scan showed a homogeneous nodular structure of soft tissue, centered on the region of the frontal maxillary apophysis on the right, with its erosion, and extending into the nasal vestibule. The structure measured approximately 17-18 mm in diameter; it had smooth, regular contours, and the adjacent bone limit was molded, constituting characteristics suggestive of benignity (Figures 2, 3).
Figure 1. Image showing a round mass on the right-side wall of the nose.
Figure 2. CT scan - coronal view.
CT scan showing a homogeneous nodular mass of soft tissue with the erosion of the frontal maxillary apophysis extending into the nasal vestibule
CT: computed tomography
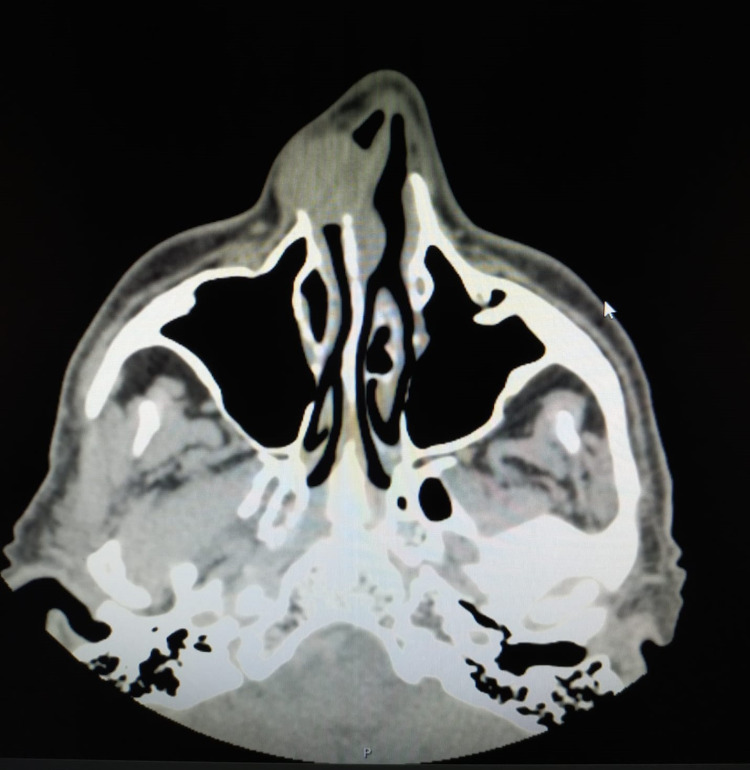
Figure 3. CT scan - axial view.
CT scan showing a homogeneous nodular mass of soft tissue with the erosion of the frontal maxillary apophysis extending into the nasal vestibule
CT: computed tomography
The surgical removal of the mass was performed. The macroscopic findings during the procedure suggested that the primary site of the mass was the right lateral wall, with expansion to the vestibule and without invasion of the nasal septum. The mass was totally excised along with the area of the surrounding skin. The postoperative period was uneventful and the patient was discharged on the same day.
Microscopically, the tumor had the appearance of classic acinic cell carcinoma. Necrosis and mitosis were absent. The neoplasm was intersected by the margins (fulguration). Given the unexpected histological diagnosis, a staging CT was performed, which showed a total excision of the lesion and no signs of local recurrence or metastasis. It was decided that the patient should undergo radiotherapy by the oncology department. At the follow-up six months later, the patient had no signs of recurrence (Figure 4).
Figure 4. CT scans showing no signs of local recurrence.
A: axial view; B: coronal view
CT: computed tomography
Discussion
Acinic cell carcinoma is a rare, slow-growing, low-grade malignancy tumor of the salivary gland [4]. Acinic cell carcinoma comprises only 0.3-0.5% of all minor salivary neoplasms and usually occurs in the oral cavity, and lesions arising in the nasal cavity are extremely rare [1]. There are a few reported cases in the literature in English; the previously reported cases are summarized in Table 1 [3-17].
Table 1. Previously reported cases of acinic cell carcinoma of the nose.
M: male; F: female; S: surgery; RT: radiotherapy; N/S: not specified
| Author/references | Age in years/gender | Location | Symptoms | Treatment | Follow-up |
| Current case | 62/M | Nasal lateral wall | Epistaxis | S + RT | 6 months |
| Hou et al., 2017 [3] | 63/F | Nasal septum | Obstruction, hyposmia, and epistaxis | S | 2 years |
| Gangadhara Somayaji et al., 2014 [5] | 65/F | Nasal lateral wall | Obstruction, epistaxis | S | 1 year |
| Hammami et al., 2010 [4] | 47/F | Nasal septum | Obstruction, hyposmia | S + RT | 4 years |
| Manganaris et al., 2010 [6] | 51/F | Vestibule | Pain | S | 3 years |
| Neto et al., 2005 [7] | 60/F | Superior meatus | Obstruction | S | 17 years |
| Neto et al., 2005 [7] | 42/F | Inferior turbinate | Obstruction | S | 7 years |
| Neto et al., 2005 [7] | 65/M | Inferior turbinate | Obstruction | S | 4 years |
| Neto et al., 2005 [7] | 50/M | Nasal cavity | Obstruction | S + RT | 12 years and recurrence |
| Sapçi et al., 2000 [8] | 47/M | Nasal septum | Obstruction, epistaxis | S | 1.5 years |
| Jasin et al., 1999 [9] | 44/F | Nasal septum | N/S | S | 2.5 years |
| Von Biberstein et al., 1999 [10] | 76/F | Middle turbinate | Nasal polyp | S | 3 years |
| Schmitt et al., 1994 [11] | 60/M | Inferior turbinate | Obstruction | N/S | N/S |
| Valerdiz-Casasola et al., 1993 [12] | 47/M | Nasal cavity | Obstruction, epistaxis | S + RT | 10 months |
| Takimoto et al., 1989 [13] | 60/F | Middle and inferior turb | Nasal polyp, epistaxis | S | 2 years |
| Hanada et al., 1988 [14] | 68/M | Inferior turbinate | Obstruction | S + RT | 3 years |
| Finkelhor et al., 1987 [15] | 45/F | Nasal septum | Obstruction | S | N/S |
| Ordonez et al., 1986 [16] | 60/F | Superior meatus | Nasal polyp, epistaxis | S | 7 years |
| Perzin et al., 1981 [17] | 75/F | Inferior turbinate | Obstruction, epistaxis | S | N/S |
The mean age of the patients was 57.2 years (range: 42-76 years). Women constituted the majority of the patients (63%). Nine cases developed on turbinate, five were located on the nasal septum, two on the nasal cavity and nasal lateral wall, and only one case was reported on the vestibule. The most common presenting complaint was nasal obstruction (84%), followed by epistaxis (42%) and hyposmia (10.5%). There were no tumor markers or imaging characteristics that allowed for a preoperative diagnosis, and all cases were diagnosed after surgical excision. The diagnoses were based entirely on histopathological evaluations [3].
Acinic cell carcinomas should be treated by complete surgical excision and the prognosis is related to tumor extension and the quality of resection [3,5,17]. Postoperative radiation is not routinely advocated for these low-grade salivary malignancies but may be used for tumors with positive surgical excision margins, tumors with extensive perineural and/or lymphovascular invasion, advanced or high-grade tumors, or recurrent tumors [18]. Chemotherapy for acinic cell carcinoma is considered ineffective [3]. Elective neck dissection is not warranted, because the incidence of cervical nodal metastasis is relatively low, with the reported nodal metastasis rates for parotid acinic cell carcinomas being 5-10% [2,17,18].
The treatment in all cases was surgery, and in five cases, patients underwent radiotherapy as well. To date, recurrence has been reported in only one case.
Conclusions
Acinic carcinoma is rarely located in the nasal cavity. Its nasal lateral wall origin is highly unusual. Curative treatment is surgery alone or surgery associated with radiotherapy. Patients with acinic cell carcinoma should be followed up for long periods, because recurrence may occur many years after the treatment. However, further studies with longer follow-up periods are needed to gain deeper insight into the clinical behavior of nasal acinic cell carcinoma.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Spiro RH. Head Neck Surg. 1986;8:177–184. doi: 10.1002/hed.2890080309. [DOI] [PubMed] [Google Scholar]
- 2.Acinic cell carcinoma of salivary origin. A clinicopathologic study of 67 cases. Spiro RH, Huvos AG, Strong EW. Cancer. 1978;41:924–935. doi: 10.1002/1097-0142(197803)41:3<924::aid-cncr2820410321>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 3.Primary acinic cell carcinoma of the nasal septum: a case report and review of the literature. Hou S, Wei J, Tian Y. http://www.ijcem.com/files/ijcem0047271.pdf Int J Clin Exp Med. 2017;10:9622–9627. [Google Scholar]
- 4.Acinic cell carcinoma of the nasal septum (Article in French) Hammami B, Dhouib H, Sallemi M, Ben Hmida A, Ben Mahfoudh K, Daoud J, Ghorbel A. Rev Stomatol Chir Maxillofac. 2010;111:88–90. doi: 10.1016/j.stomax.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Acinic cell carcinoma of the nasal cavity. Gangadhara Somayaji KS, Sunu Ali Z, Nalapad Abdulla M, Nambiar VR, Johns TK. Arch Med Health Sci. 2014;2:220–222. [Google Scholar]
- 6.Acinic cell carcinoma of the nasal vestibule. Report of a unique case. Manganaris A, Bates TJ, Roberts D, Simo R. Rhinology. 2010;48:113–116. doi: 10.4193/Rhin08.143. [DOI] [PubMed] [Google Scholar]
- 7.Sinonasal acinic cell carcinoma: a clinicopathologic study of four cases. Neto AG, Pineda-Daboin K, Spencer ML, Luna MA. Head Neck. 2005;27:603–607. doi: 10.1002/hed.20186. [DOI] [PubMed] [Google Scholar]
- 8.Acinic cell carcinoma originating in the nasal septum. Sapçi T, Yìldìrìm G, Peker K, Karavus A, Akbulut UG. https://www.rhinologyjournal.com/Rhinology_issues/74.pdf. Rhinology. 2000;38:140–143. [PubMed] [Google Scholar]
- 9.Acinic cell carcinoma of the nasal septum. Jasin M, Hutchunson R. Otolaryngol Head Neck Surg. 1999;121:222–223. [Google Scholar]
- 10.Acinic cell carcinoma of the nasal cavity. von Biberstein SE, Spiro JD, Mancoll W. Otolaryngol Head Neck Surg. 1999;120:759–762. doi: 10.1053/hn.1999.v120.a84689. [DOI] [PubMed] [Google Scholar]
- 11.Acinic cell carcinoma arising in nasal cavity: diagnosis by fine-needle aspiration. Schmitt FC, Wal R, Santos Gda C. Diagn Cytopathol. 1994;10:96–97. doi: 10.1002/dc.2840100124. [DOI] [PubMed] [Google Scholar]
- 12.Acinic cell carcinoma of the sinonasal cavity with intracytoplasmic crystalloids. Valerdiz-Casasola S, Sola J, Pardo-Mindan FJ. Histopathology. 1993;23:382–384. doi: 10.1111/j.1365-2559.1993.tb01225.x. [DOI] [PubMed] [Google Scholar]
- 13.Acinic cell carcinoma of the nasal cavity: a case report. Takimoto T, Kano M, Umeda R. https://pubmed.ncbi.nlm.nih.gov/2637476/ Rhinology. 1989;27:191–196. [PubMed] [Google Scholar]
- 14.Acinic cell carcinoma originating in the nasal cavity. Hanada T, Moriyama I, Fukami K. Arch Otorhinolaryngol. 1988;245:344–347. doi: 10.1007/BF00457991. [DOI] [PubMed] [Google Scholar]
- 15.Pathologic quiz case 1. Acinous cell carcinoma. Finkelhor BK, Maves MD. https://pubmed.ncbi.nlm.nih.gov/3620139/ Arch Otolaryngol Head Neck Surg. 1987;113:1120–1122. [PubMed] [Google Scholar]
- 16.Acinic cell carcinoma of the nasal cavity: electron-optic and immunohistochemical observations. Ordonez NG, Batsakis JG. J Laryngol Otol. 1986;100:345–349. doi: 10.1017/s0022215100099266. [DOI] [PubMed] [Google Scholar]
- 17.Acinic cell carcinoma arising in nasal cavity: report of a case with ultrastructural observations. Perzin KH, Cantor JO, Johannessen JV. Cancer. 1981;47:1818–1822. doi: 10.1002/1097-0142(19810401)47:7<1818::aid-cncr2820470716>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 18.Ellis GL, Auclair PL. Atlas of Tumor Pathology. Vol. 3. Washington, DC: Armed Forces Institute of Pathology; 1995. Tumors of salivary glands; pp. 183–203. [Google Scholar]