Abstract
To guide intervention efforts, we identified the proportion of individuals previously engaged in opioid agonist therapy among people who died of an accidental opioid-involved overdose. Most individuals (60.9%) had never received any prior buprenorphine or methadone treatment. Individuals who died of an overdose in 2020 had a similar demographic profile and treatment history compared with prior years. To prevent additional accidental opioid-involved overdose deaths, efforts should be directed toward linking individuals to care.
In 2018, the rate of accidental drug overdose deaths in Rhode Island was 50% higher than the national average.1 Despite its numbers gradually declining for the previous three years, Rhode Island in 2020 was on track to have its highest number of accidental overdose deaths ever recorded.2 Prior engagement with opioid agonist therapy among this population is currently unknown. Additionally, it is unclear whether individuals previously in recovery were disproportionally affected by the opioid and COVID-19 syndemic in 2020.3
INTERVENTION
To guide intervention efforts and determine whether individuals in recovery were disproportionally affected by the syndemic, we identified the proportion of individuals previously engaged in opioid agonist therapy (methadone: January 2010–June 2020; buprenorphine: April 2016–June 2020) among people who died of an accidental opioid-involved overdose.
PLACE AND TIME
This analysis was performed by the Rhode Island Department of Health (RIDOH) in July 2020. To inform prevention activities, results were presented internally and to external partners in August 2020 and to the public in September 2020.
PERSON
All accidental opioid-involved overdose deaths (defined as those with opioids listed as a cause of death) occurring in Rhode Island between January 1, 2018, and June 30, 2020, were identified using data from the Office of the State Medical Examiner (OSME). To ensure that complete treatment history could be obtained, out-of-state residents were excluded from the analysis. Of the 815 accidental overdose deaths occurring during the study period, 697 involved opioids, of which 626 occurred among Rhode Island residents.
PURPOSE
The objective of the analysis was to identify the proportion of individuals previously engaged in methadone or buprenorphine treatment for opioid use disorder by year of death. The results from this analysis helped RIDOH identify whether prevention efforts should be directed toward providing additional support to individuals in long-term recovery, currently engaged with treatment, or never engaged in treatment.
IMPLEMENTATION
To obtain treatment information for all accidental opioid-related overdose deaths, OSME data were linked with the Rhode Island Prescription Drug Monitoring Program (PDMP) and the Rhode Island Behavioral Health On-Line Database (RI-BHOLD) to obtain prior buprenorphine and methadone treatment history, respectively. To do this, a unique identifier was created using the last five letters of an individual’s last name, the first three letters of their first name, and their date of birth. Using this identifier, OSME data were linked to Rhode Island Vital Records to ensure accuracy of matching characteristics and to obtain their social security number. Individuals who did not link were manually matched; four individuals could not be linked, so only their OSME identifier was used for the analysis. This identifier was also used to obtain decedents’ prescription history for buprenorphine products approved by the Food and Drug Administration for opioid agonist therapy, as recorded in the PDMP from April 1, 2016, to June 30, 2020. For individuals who did not match to the PDMP, a second unique identifier using Vital Records information was created and the linkage was reperformed. Methadone treatment history between January 1, 2010, and June 30, 2020, was obtained from RI-BHOLD. Individuals were first matched by social security number (96% of matches) and then by full name and date of birth. For this analysis, buprenorphine treatment was assumed based on dispensed medication and the days’ supply and includes buprenorphine dispensed by out-of-state pharmacies. With methadone, by contrast, treatment is primarily given through direct observed therapy, receipt of treatment is known, and data on methadone treatment received out of state are not available.
For the analysis, demographic characteristics from OSME, buprenorphine prescription history from the PDMP, and methadone treatment history from RI-BHOLD were compared by year of death. Any treatment history was defined as receipt of any prior buprenorphine prescription or methadone treatment. To determine whether an individual stopped treatment within 30 days of death or whether they were engaged in treatment at the time of death, we utilized the last day an individual received methadone treatment or the fill date of the buprenorphine prescription and the days’ supply. Categorical measures were compared with χ2 tests. Analyses were performed in SAS version 9.4 (SAS Institute, Cary, NC).
EVALUATION
Overall, most accidental opioid-related overdose deaths occurred in males (76.8%), non-Hispanic Whites (78.3%), and those aged 25 to 44 years (53.2%; Table 1). When demographic characteristics by year of death were compared, no significant differences were observed.
TABLE 1—
Demographic Characteristics of Rhode Island Residents Who Died of an Accidental Opioid-Related Overdose, Stratified by Prior Treatment History: Rhode Island, January 1, 2018–June 30, 2020
| Overall, No. (%) |
Any Prior Methadone or Buprenorphine Treatmenta | P b | ||
| Yes, No. (%) |
No, No. (%) |
|||
| Age, y | .002 | |||
| 18–24 | 33 (5.3) | < 5 (. . .) | 31 (8.1) | |
| 25–34 | 159 (25.4) | 61 (24.9) | 98 (25.7) | |
| 35–44 | 174 (27.8) | 80 (32.7) | 94 (24.7) | |
| 45–54 | 124 (19.8) | 51 (20.8) | 73 (19.2) | |
| 55–64 | 114 (18.2) | 44 (18.0) | 70 (18.4) | |
| ≥ 65 | 22 (3.5) | 7 (2.9) | 15 (3.9) | |
| Gender | .029 | |||
| Female | 145 (23.2) | 68 (27.8) | 77 (20.2) | |
| Male | 481 (76.8) | 177 (72.2) | 304 (79.8) | |
| Race/ethnicity | < .001 | |||
| Non-Hispanic White | 490 (78.3) | 220 (89.8) | 270 (70.9) | |
| Non-Hispanic Black | 50 (8.0) | 8 (3.3) | 42 (11.0) | |
| Hispanic (any race) | 78 (12.5) | 17 (6.9) | 61 (16.0) | |
| Other | 8 (1.3) | 0 (0.0) | 8 (2.1) | |
| Matched to PDMP for any controlled substance prescriptionc | < .001 | |||
| Yes | 462 (73.8) | 223 (91.0) | 239 (62.7) | |
| No | 164 (26.2) | 22 (9.0) | 142 (37.3) | |
Note. PDMP = Rhode Island Prescription Drug Monitoring Program. The sample size was n = 626.
Includes buprenorphine products Food and Drug Administration–approved for opioid agonist therapy dispensed between April 1, 2016 and June 30, 2020, and methadone treatment received between January 1, 2010 and June 30, 2020.
χ2 test.
Matching indicates an individual was dispensed any schedule II-V medications or opioid antagonists between April 1, 2016 and June 30, 2020.
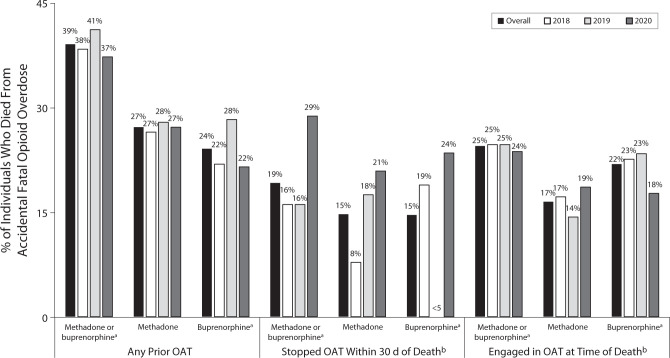
Overall, 245 individuals (39.1%) who died of an accidental opioid-involved overdose between January 2018 and June 2020 received any prior methadone or buprenorphine treatment for opioid use disorder based on the available data; of those, 170 (27.2%) received any prior methadone treatment and 151 (24.1%) received any prior buprenorphine (Figure 1; Table A, available as a supplement to the online version of this article at http://www.ajph.org). Although more data are available for people who died in later time periods, the proportion of individuals who received any prior treatment was similar from 2018 to 2020 (P = .7). Among individuals who received methadone or buprenorphine treatment, 60 (24.5%) were enrolled in treatment at the time of death and 47 (19.2%) died within 30 days of treatment cessation. The proportion of individuals who died in the 30 days following treatment cessation increased somewhat, from 16% in 2018 and 2019 to 29% in 2020.
FIGURE 1—
Methadone and Buprenorphine Treatment Characteristics Among Rhode Island Residents Who Died of an Accidental Opioid-Related Overdose: Rhode Island, January 1, 2018–June 30, 2020
Note. OAT = opioid agonist therapy. The sample size was n = 626.
aIncludes buprenorphine products Food and Drug Administration–approved for opioid agonist therapy dispensed between April 1, 2016, and June 30, 2020, and methadone treatment received between January 1, 2010, and June 30, 2020. bLimited to individuals who received buprenorphine or methadone treatment. Calculated from the last day an individual received methadone treatment or the fill date of the buprenorphine prescription and the days’ supply.
When demographic characteristics by any treatment history were compared, individuals who were non-Hispanic White had a higher proportion engaged in treatment (44.9%) compared with non-Hispanic Black (16.0%) and Hispanic (21.8%) individuals. Additionally, 48.2% of individuals who matched to the PDMP for any controlled substance prescription were engaged in treatment, compared 13.4% for individuals who did not match (Table 1). When stratified by treatment type (methadone and buprenorphine), similar results were obtained.
Of note, data from the PDMP are limited to after April 1, 2016, and data from RI-BHOLD are limited to after January 1, 2010, so some individuals likely received treatment that predates the available data, particularly for buprenorphine. Unfortunately, we cannot determine from this analysis if the low proportion of individuals in treatment reflects individuals who want treatment but have barriers to access or are not currently interested in treatment.
ADVERSE EFFECTS
We are not aware of any adverse events that occurred because of this analysis.
SUSTAINABILITY
We plan to reperform this analysis regularly until this information is no longer needed to direct prevention activities of RIDOH and its partners in response to the syndemic.
PUBLIC HEALTH SIGNIFICANCE
In Rhode Island, most individuals (60.9%) who died of an accidental opioid-involved overdose had not received any prior methadone or buprenorphine treatment for opioid use disorder. Despite a 33% increase in accidental opioid-involved overdose deaths in January through July 2020 compared with the same time period in 2019,2 this study did not identify any differences in demographic characteristics or treatment history by year of death. The high proportion of individuals engaged in treatment who had received a prior controlled substance prescription suggests that, for this population, individuals who are more connected to the health care system may be more likely to initiate treatment. Additionally, the lower proportion of individuals engaged in treatment among younger age groups (< 25 years of age) and among non-Hispanic Black, Hispanic, and other minority racial/ethnic groups suggests that additional outreach efforts should be directed at linking these populations to care. To help address the opioid epidemic in Rhode Island, efforts to promote harm reduction practices, link individuals to treatment, identify facilitators that help link individuals to care, and remove barriers that limit utilization and retention should continue to be a priority.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
HUMAN PARTICIPANT PROTECTION
This study was deemed exempt by the Rhode Island Department of Health (RIDOH) institutional review board; data were stored on encrypted servers at RIDOH.
References
- 1.Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/drugoverdose/data/statedeaths.html
- 2.Hallowell BD, Weidele HR, Scagos RP. Accidental drug overdose deaths in Rhode Island: January 1, 2016–July 31, 2020. R I Med J (2013) 2020;103(10):62–65. [PubMed] [Google Scholar]
- 3.Katz J, Goodnough A, Sanger-Katz M. In shadow of pandemic, US drug overdose deaths resurge to record. New York Times. July 15, 2020https://www.nytimes.com/interactive/2020/07/15/upshot/drug-overdose-deaths.html