Abstract
Purpose of Review
Management of Epstein-Barr virus post-transplant lymphoproliferative disorder (EBV PTLD) is complex, involving risk stratification, prevention and/or pre-emptive measures involving monitoring EBV DNAemia and balancing treatment options, using a combination of reduction of immune suppression, anti-B cell therapy, and cytotoxic T lymphocytes (CTLs).
Recent Findings
The highest risk factor for the development of EBV PTLD in hematopoietic cell transplant (HCT) remains T cell depletion, with increasing use of anti-thymocyte globulin (ATG) or alemtuzumab in conditioning. In solid organ transplantation (SOT), the incidence of PTLD is highest among EBV seronegative recipients who are at risk for primary EBV infection following transplant in the first 12 months. Prevention is a critical component of the management of EBV PTLD. Although pre-emptive therapy remains standard of care, there continues to be heterogenicity and debate over the optimal choice of EBV DNA quantification and the threshold to use. Novel therapies such as donor-derived multi-pathogen and EBV specific CTLs for the prevention and third party CTLs for the treatment of EBV-PTLD are promising, with rapidly expanding evidence, including large scale Phase III trials currently underway.
Summary
With an increasing number of risk groups for developing EBV PTLD in HCT and SOT, management strategies using prophylaxis or pre-emptive therapy remain standard of care, however the use of prophylactic or pre-emptive EBV specific or multi-pathogen CTLs show promising results and safety profiles.
Keywords: Epstein-Barr virus (EBV), Epstein-Barr virus post-transplant lymphoproliferative disorder (EBV-PTLD)
INTRODUCTION
Epstein-Barr virus (EBV) is a γ-herpes virus which largely causes an asymptomatic primary infection in immunocompetent hosts, establishing a life-long latent infection in B cells which is controlled by T lymphocytes and NK cells [1, 2]. Over 90% of adults and 50% of children globally are infected with EBV [2]. However, in patients undergoing allogeneic hematopoietic cell transplantation (HCT) and solid organ transplantation (SOT), EBV infects naïve B cells to transform into proliferating blasts, potentially resulting in post-transplant lymphoproliferative disorder (EBV PTLD) [3]. EBV infected B cells in SOT recipients are usually of recipient origin, while in HCT, typically of donor origin [4]. Unlike HCT, only approximately half of PTLD in SOT is EBV positive, and the majority of late presenting PTLD is EBV negative [5]. EBV PLTD is recognized as a significant cause of morbidity and mortality in this population with an associated mortality of over 50% [6, 7].
Management of EBV PTLD is complex, involving risk stratification, prevention and/or pre-emptive measures involving monitoring EBV DNAemia and balancing treatment options, using a combination of reduction of immune suppression, if possible, anti-B cell therapy, and more recently, cytotoxic T lymphocytes (CTLs). While guidelines have been updated for the SOT population in 2019 [5], the most recent management guidelines in HCT remain the 2016 European Conference on Infections in Leukemia (ECIL-6) guidelines [3]. This review aims to summarize the most recent developments on the new risk groups for developing EBV PTLD, monitoring and diagnostic approaches, prevention strategies and treatment options.
NEW RISK GROUPS AND RATE OF EBV VIREMIA AND PTLD IN SPECIFIED POPULATIONS
HCT risk groups
The most significant risk factor for the development of EBV PTLD in HCT is in vivo T cell depletion, most commonly using anti-thymocyte globulin (ATG) or alemtuzumab in conditioning [8-12] (See Table 1). In a recent Center for International Blood and Marrow Transplant Research (CIBMTR) report of identified PTLD cases post-HCT, 78% were conditioned with ATG or alemtuzumab. The study demonstrated an overall survival one year post diagnosis of PTLD of 53%. Although this risk factor is not a recent development, the use of ATG in HCT practice is changing, with its use becoming more widespread, including in mismatched and matched unrelated donor (MMRD and MURD) recipients as well as increasingly in matched related donor (MRD) recipients with high GVHD risk [13-15]. One recent report of using ATG for all MMRD and MURD recipients by Ali et al. demonstrated a 71% reactivation of EBV (≥1000 IU/mL), however a relatively low rate of PTLD (2.4%) using a pre-emptive management approach [15].
Table 1.
Risk factors for EBV PTLD in HCT and SOT
| Factors which INCREASE the risk of developing EBV PTLD | |
|---|---|
| HCT [3, 10-12, 84-87] | SOT |
| Anti-thymocyte Globulin (ATG) or alemtuzumab | <12 months after transplant |
| In vivo T-cell Depletion | Intestine > lung > heart > liver > pancreas > kidney |
| EBV serology donor/recipient mismatch (recipient-negative/donor-positive) | Donor EBV+/ Recipient EBV− |
| Cord blood transplantation | Children |
| Reduced intensity conditioning | Belatacept immunosuppression |
| HLA mismatch | |
| Splenectomy | |
| Second HSCT | |
| Severe acute or chronic GvHD requiring intensive immunosuppressive therapy | |
| Infusion of mesenchymal stromal cells | |
| Factors which REDUCE the risk of developing EBV PTLD | |
| HCT | SOT |
| Rituximab exposure within 6 months pre-HSCT | >12 months after transplant |
| Post-transplant cyclophosphamide (without ATG) | Kidney > pancreas > liver > heart > lung > intestine |
| Sirolimus use for GVHD Prophylaxis | Recipient EBV+ |
| CD4+ T-lymphocyte count >50 at day +30 | Adults |
The incidence of PTLD is low when using post-transplant cyclophosphamide (PTCy) in the setting of haploidentical donor recipients [16], with a large retrospective analysis of adult alloHSCT recipients demonstrating no PTLD at 1 year post HSCT [17]. However, a recent report of ATG in combination with PTCy for GVHD prophylaxis demonstrated a 63.7% EBV reactivation and 12% incidence of PTLD [18]. In addition, a recent large single center retrospective analysis of consecutive HCT patients by Ru et al. demonstrated that the two independent risk factors for EBV reactivation were haploidentical donor (HR 1.8, p= 0.001) and ATG use (HR 4.4, p<0.001), with the caveat that ATG was administered to all haploidentical donor HCTs [12].
SOT risk groups
In SOT recipients, the incidence of PTLD varies depending on donor/recipient EBV serostatus, organ(s) transplant, and immunosuppressive regimen [5]. Donor and recipient EBV serology is measured prior to solid organ transplantation as markers of latent EBV infection within the donor and pre-existing EBV-specific immunity in the recipient. When primary EBV infection occurs after solid organ transplantation, EBV-directed CD8+ T-cell responses are diminished, and latent EBV infection is established in a larger B-cell reservoir than when primary EBV infection occurs in immunocompetent hosts [19]. Thus, the incidence of PTLD is highest among EBV seronegative recipients who are at risk for primary EBV infection following transplant. The relative risk of PTLD in EBV seronegative recipients (R−) versus EBV seropositive recipients (R+) ranges from 2.6-9.9 [20, 21]. Recipient EBV seronegativity is more common in pediatric (~55%) compared to adult (~10%) SOT recipients and children therefore have a higher incidence of PTLD [20, 22]. Latently infected donor B-cells often travel with solid organ allografts from EBV seropositive donors (D+) and serve as an important source of primary EBV infection in seronegative recipients. In adults, PTLD incidence among EBV donor positive, recipient negative (D+/R−) transplants is 2-3 times higher than the incidence among EBV D−/R− transplants [23].
The incidence of PTLD varies by organ transplanted and is highest among recipients of intestine (up to 20%) allografts, followed by lung (3-10%), heart (2-8%), liver (1-5%) and kidney (0.8-2.5%) [24]. The relatively high risk of PTLD in intestinal and lung recipients may be due to the abundance of lymphatic tissue within these organs (and thus a large reservoir of B-cells), coupled with the high intensity of maintenance immunosuppression required to prevent allograft rejection [19]. Induction with potent T-cell depletion using muromonab-CD3 (OKT3) or alemtuzumab is associated with a higher risk of PTLD compared to induction with ATG or anti-IL-2 receptor antibodies such as basiliximab [25]. In a Phase III randomized trial of maintenance cyclosporine versus belatacept, the T-cell co-stimulation blocking agent in kidney transplant recipients, belatacept was associated with a higher incidence of PTLD than cyclosporine in EBV seronegative patients [26]. Over half of PTLDs in patients receiving belatacept involved the central nervous system and the majority were fatal.
Of note, EBV RNA (EBER) expression does not occur in all PTLDs following SOT, and the proportion of PTLDs that are EBV-negative in SOT recipients has increased over the past 30 years from 10% between 1990-1995 to 48% between 2008-2013 [27]. Whether EBV has a role in the pathogenesis of EBV-negative PTLD is not clear. An EBV “hit and run” hypothesis, whereby EBV infects B-cells, induces chromosomal aberrations, then exists the cell, has been proposed but has not undergone rigorous evaluation [28]. In a single center investigation of 4171 SOT recipients, the cumulative incidence of EBV-negative PTLD was higher in EBV R− compared to EBV R+ (HR 3.56, P=0.008), but the hazard ratio for development of EBV-positive PTLD was roughly 4-fold higher (HR 14.2, P<0.009) [20].
NEW MONITORING/DIAGNOSTICS
Pre-emptive approaches, standardization and kinetics of EBV DNA assay and samples
Surveillance of EBV DNAemia using nucleic acid testing remains the current standard management approach in preventing PTLD in high-risk populations. Following the detection of EBV DNAemia to a specific threshold, interventions with either pre-emptive therapy and/or a reduction of immunosuppression, if possible, are implemented [3, 5, 29] (See Table 2). However, there remains variability in the sample used to measure EBV DNAemia, including plasma, whole blood or peripheral blood mononuclear cells (PBMCs). Whilst the optimal sample is currently debated, plasma seems the most reliable marker for EBV PTLD [30]. There is also a large variation in practice for when to intervene; due to this historic heterogeneity, the ECIL guidelines for HCT have not recommended a specific threshold of when to intervene, with EBV DNAemia ranging from 1000 copies/mL to 40,000 copies/mL recommended. However, with the implementation of WHO international standardization (IS) of EBV measurement to international units/mL (IU/mL) in 2011, there has been a growing body of evidence for the standardization of EBV DNAemia monitoring for pre-emptive therapy [31]. Solano et al. demonstrated in a small cohort of T cell replete HCT recipients (ATG in 17% of patients) that plasma EBV DNA-load kinetics analyses were unlikely to be useful in predicting the occurrence of high-level EBV DNAemia, PTLD, or recurrent EBV DNAemia [32]. However, studies focusing on the viral kinetics of EBV DNAemia in T-cell deplete populations such as ATG conditioned recipients, indicated that there is a clear need to instigate pre-emptive therapy, although the ideal EBV DNAemia level to intervene remains unclear [3, 33-36], (See Table 3). Recent large single center analyses have suggested that an EBV DNA level of 1000IU/mL to 10,000IU/mL on plasma or whole blood may be an optimal pre-emptive threshold [37-39].
Table 2.
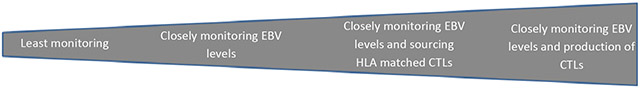
Characteristics of the available strategies to manage PTLD in high-risk HCT and SOT patients
| Prophylaxis with rituximab |
Pre-emptive/treatment strategy with rituximab |
Pre-emptive/treatment with third party CTLs |
Prophylaxis with donor- derived CTLs |
|
|---|---|---|---|---|
| General principle | Circulating anti-CD20 prevents B-cell proliferation and EBV reactivation | Anti-CD20 prevents/treats B-cell/EBV proliferation when EBV DNAemia is rising | Third party EBV specific CTLs treat EBV proliferation when EBV DNAemia is rising | Donor-derived EBV specific CTLs prevent EBV proliferation |
| Typical application | Administration of rituximab (200mg-375mg/m2) immediately prior to cell infusion/organ donation | Following regular (usually weekly) monitoring of EBV DNAemia, pre-emptively treating with 375mg/m2 weekly at a specific threshold to prevent the incidence of PTLD or treat early PTLD | Following regular (usually weekly) monitoring of EBV DNAemia, pre-emptively treating with HLA matched third party EBV specific CTLs at a specific threshold to prevent the incidence of PTLD or treat early PTLD | Administration of donor-derived EBV specific CTLs following cell infusion/organ donation |
| Safety concerns | Minimal: Increased infection risk from B-cell depletion | Minimal: Increased infection risk from B-cell depletion | Potential concerns with GVHD/organ rejection, however this has not been proven | Potential concerns with GVHD/organ rejection, however this has not been proven |
| Use of rituximab |

|
|||
| Overall estimated cost of therapy |

|
|||
| Logistical challenges for application |
|
|||
| Level of Evidence in HCT | + | +++ | + | + |
| Level of Evidence in SOT | + | + | + | + |
| Considerations | Currently no consensus for EBV assay/sample used and EBV DNAemia threshold to use for pre-emptive treatment | Large phase III and expanded access trials in commercial product (Tabelecleucel) pending, not currently FDA approved HLA matching is not always possible |
Facilities to produce donor-derived EBV CTLs are uncommon The cost and turnaround time to produce donor-derived CTLs is prohibitive |
|
All strategies can be used in conjunction with reduction of immunosuppression following EBV DNAemia monitoring
Table 3.
Summary of recent reported EBV preventative strategies using rituximab in HCT
| Study | Patients and HCT Protocol | Monitoring | Sample | Pre-emptive EBV threshold |
Treatment details | EBV reactivation and PTLD rates |
|---|---|---|---|---|---|---|
| Jain et al. 2019 [37, 38] | N = 488 myeloablative and non-myeloablative HCT GVHD Px included a selection of TAC, MMF, MTX ATG 2.5-7.5mg/kg in 306/488 patients |
Weekly until day 100, or beyond this if GVHD, immunosuppressants or previous EBV PTLD. Repeat testing every 3-5 days after reactivation |
Whole blood | >2,000copies/mL and continues to rise on a weekly basis; OR 2,000-5,000copies/mL and considered high risk of EBV reactivation; OR >5,000copies/mL |
Pre-emptive rituximab 375mg/m2 weekly | 14% (67/488) EBV reactivations as per criteria 1.4% (7/488) EBV PTLD |
| Van Besien et al. 2019 [49] | N = 198 haplo-cord donors, supplemented by CD34 selected third-party cells to accelerate recovery most commonly FluMel+/−TBI GVHD Px included TAC, MMF, ATG 4.5-6mg/kg, rituximab 375mg/m2, 2 weeks prior to HSCT (n=38), prior treatment with rituximab (n=13), no rituximab (n=147) |
Twice weekly during hospitalization, then weekly for the first 100 days, then second weekly until day180 or as clinically indicated | Not reported | Not reported, PTLD reported based on “rapid increasing EBV levels”, positive PET scan and biopsy proven PTLD | Prophylactic rituximab 375mg/m2 was administered 2 weeks prior to HSCT (n=38) unless prior treatment with rituximab was given for primary B-cell malignancy (n=13). | Prior rituximab: 2% (1/51) EBV viremia (>200 copies/mL). No EBV PTLD No prior rituximab: 18% (27/146) EBV viremia. 12% (16/146) EBV PTLD |
| Ru et al. 2020 [12] | N = 890 Bu/Cy, TBI/Cy, Flu/Bu/Cy or Flu/Bu/Ara-C GVHD Px included CSP, MTX; MMF and ATG for URD and Haplo (27.9%) |
Weekly until day +90, then fortnightly until day +180 | Whole blood | 105 Copies/mL or 104 Copies/mL for 2 weeks | Initially reduction in immunosuppression and treatment with ganciclovir/foscarnet, then pre-emptive treatment with rituximab (no dose given) | 19.6% (175/890) EBV reactivation. 0.7% (7/890) EBV PTLD Incidence of ATG patients not reported separately. The cumulative incidence of EBV reactivation was 2.9%, 11.7%, 27.3%, and 41.9% for patients with 0, 1, 2, and 3 risk factors including ATG, haplo, and GVHD |
| Marzolini et al. 2021 [36] | N = 515 Cy/TBI or Flu/Cy/TBI GVHD Px included Alemtuzumab 20-100mg |
Weekly up to day 100 | Plasma | Only treated if clinical signs of “EBV disease” | Immunosuppression reduced and rituximab 375mg/m2 was administered weekly for 4 weeks | 35% (192/515) EBV reactivation. 3.9% (20/515) EBV disease, 19 PTLD, 1 EBV encephalitis. |
Abbreviations: AraC, cytarabine; ATG, antithymocyte globulin; Bu, busulfan; CSP, cyclosporin; Cy, cyclophosphamide; Flu, fludarabine; GVHD, graft versus host disease; Mel, melphalan; MMF, mycophenolate; MTX, methotrexate; Px, prophylaxis; TAC, tacrolimus; TBI, total body irradiation.
SOT recipients who are EBV-seronegative prior to transplant are frequently monitored for EBV DNAemia at regular intervals following transplant. Reduction of immunosuppression (RIS) in response to EBV DNAemia has been shown to reduce the incidence of early PTLD in studies of pediatric SOT recipients that use historical control groups [40, 41]. While pre-emptive RIS in response to EBV DNAemia has not been evaluated using randomized, contemporaneous cohorts, RIS during primary EBV infection theoretically promotes the development of EBV-specific T-cell responses and is frequently used as a pre-emptive strategy in both adult and pediatric EBV-seronegative SOT recipients [5].
Antiviral prophylaxis or pre-emptive therapy with acyclovir and ganciclovir, which are commonly used to prevent non-EBV herpesvirus infections post-transplant, have not been effective in preventing PTLD in SOT or HCT recipients [3, 5]. While retrospective observational studies examining the association between antivirals and PTLD in SOT have shown mixed results, neither prophylactic nor pre-emptive antivirals were associated with a decreased incidence of PTLD in a large meta-analysis [42]. In a prospective study of pediatric liver transplant recipients in which SOT recipients received ganciclovir for 2 weeks immediately followed by 50 weeks of either oral acyclovir or placebo, there was no difference in the incidence of PTLD between groups [43]. Likewise, antivirals have not been effective in the treatment of PTLD in SOT recipients, perhaps because antivirals are most effective at targeting lytic EBV infection rather than the latently infected state characteristic of PTLD. Pharmacologic agents that induce transformation of EBV from the latent to the lytic phase, such as the histone deacetylase inhibitor arginine butyrate and the proteasome inhibitor bortezomib, sensitize latently infected B-cells to the effects of antivirals; these agents have been used in small observational trials [5].
Diagnostic strategies
The diagnostic strategy for suspected EBV PTLD includes routine blood tests, review of recent EBV DNA results, imaging and ideally a tissue biopsy [3, 5]. Imaging has traditionally been with CT scan, however PET-CT is increasingly used due to improved sensitivity and specificity, allowing for accurate staging and identification of sites for biopsy [5]. A recent analysis of the diagnostic performance of PET-CT demonstrated a sensitivity of 85%, specificity of 90% and good inter-observer reliability [44]. Biopsy of an involved site is the gold standard diagnostic test and should be performed wherever possible. Occasionally this is not feasible due to anatomical or clinical limitations, in which case treatment may be initiated for probable disease, on the basis of EBV DNA and PET-CT results [3, 5].
NEW PREVENTION STRATEGIES
Prophylaxis with Rituximab
Previous studies have demonstrated that pre-transplant rituximab safely and effectively lowers the incidence of EBV reactivation following allogeneic HCT for B-cell malignancies [45]. Thus, the role of rituximab prophylaxis for high risk HCT patients is becoming more established, as evidenced by its recommendation by a recent proposed approach by Hamed et al. [46-50]. For example, Van Besien et al. administered a single dose of rituximab 375mg/m2 two weeks prior to haplo-cord alloHSCT unless the patient had a recent prior exposure to rituximab due to treatment for a primary B-cell malignancy. Compared to a control group, EBV reactivation occurred in 1/51 (2%) with rituximab exposure vs 27/146 (18%) without (P=0.004). PTLD developed in 16/146 (12%) without prior rituximab exposure vs none with rituximab exposure. In SOT recipients, the role of peri-transplant rituximab in preventing PTLD is less clear. The Swiss Transplant Cohort Study found no significant difference in the incidence of PTLD between SOT recipients receiving induction regimens with or without rituximab, although no patients who received rituximab developed PTLD [51].
Prevention strategies using CTLs
The most recent emerging strategy for the prevention and treatment of EBV PTLD is the use of donor derived or third party EBV-specific CTLs. The utility of CTLs has been demonstrated for over a decade, with historical studies demonstrating approximately 95% successful elimination of EBV viremia, and 65%-88% success for the treatment of PTLD, even after the failure of rituximab-based therapy [7, 52-55]. However, access and HLA compatibility has posed a challenge for the wide applicability of their use [3]. Evidence for CTLs as a prevention strategy in SOT recipients is limited. In an observational study of 21 SOT recipients at high risk for PTLD who received autologous EBV-specific CTLs, only one patient developed PTLD [5]. Recently, multi-pathogen specific donor-derived CTLs have been described as a broad infection prevention strategy for high risk HCT recipients [56-59].
mTOR inhibitors
The use of mammalian target of rapamycin inhibitors (mTORi), particularly sirolimus, has also recently been described as a potentially beneficial agent against EBV viremia and PTLD [48]. A recent study by Hellewell et al. demonstrated GVHD prophylaxis with an mTORi was significantly less likely to develop an EBV DNAemia post HCT [60]. The mechanism of action for this effect is likely to be due to inhibition of the proliferation of transformed cell lines [61]. Further investigation into this effect in clinical practice is required. This effect in SOT however remains unproven despite the wide application of changing therapy to an mTORi for PTLD prevention [62].
Vaccines
A vaccine that induces adaptive EBV immunity and prevents uncontrolled primary EBV infection could offer protection against PTLD among EBV seronegative recipients. However, no such vaccine has been developed to date. A phase II trial in healthy EBV seronegative young adult SOT recipients, comparing placebo to a vaccine containing recombinant EBV subunit glycoprotein 350 (gp350) showed that the subunit vaccine induced anti-gp350 antibodies in 99% of participants and had 78% efficacy in reducing symptomatic infectious mononucleosis, but did not prevent EBV infection as assessed by anti-VCA (anti-viral capsid antigen) seroconversion [63]. EBV vaccines that induces T-cell responses may have greater efficacy in reducing primary EBV infection and are currently in development [64].
NEW TREATMENT OPTIONS
Although a reduction in immune suppression has historically been the backbone of PTLD treatment, the response rate from this strategy alone is low, and timely addition of rituximab and/or CTLs is recommended [3, 5, 65]. In SOT recipients, 44-79% of patients with CD20 positive PTLD respond to RIS and rituximab alone, and 25% will experience complete remission without any additional chemotherapy [24]. Cytotoxic chemotherapy is used for CD20 negative PTLDs or when rituximab monotherapy is unsuccessful [5]. Conversely in HCT, RIS is rarely successful as a sole intervention for the treatment of proven or probable PTLD [3], and should be combined with rituximab therapy, with response rates of 84% in patients who received both rituximab and RI, compared to 61% in rituximab alone [65].
CTLs in HCT
T cell therapies have demonstrated efficacy in the treatment of PTLD, including after rituximab failure [7, 52-55]. Unselected donor lymphocyte infusions (DLI) are a potential option, with responses in up to 70% of patients [52]. However, DLI carries a significant risk of inducing GVHD so is not commonly used in this setting. EBV specific CTLs produce at least equivalent response rates [7, 52-55], but have not been associated with GVHD, even when not HLA-matched [52, 66]. Access to these products has historically been an issue due to the timing of producing donor-derived CTLs, particularly as PTLD can be a rapidly progressive disease. A recently reported Phase II trial was able to overcome this barrier by establishing a cryopreserved bank of “third party” or “off-the-shelf” EBV-CTLs, allowing patients to be treated within 1-2 days of referral [66]. From a bank of 330 EBV-CTLs, 46 patients were treated with a response rate in HCT patients of 68% and one-year survival in responding patients of 88.9%. The promise and flexibility of CTL therapy was further demonstrated by a recent case report of a patient who successfully received five T cell infusions from three separate donors for three viral infections, including EBV-PTLD [67]. EBV CTL use is rapidly expanding with a number clinical trials emerging in recent years, including a large phase III study evaluating the use of commercially available EBV CTL in HCT and SOT (MATCH, NCT03392142 and ALLELE, NCT03394365) with promising preliminary abstracts published [68, 69], as well as a number of phase I studies in progress [52, 70].
CTLs in SOT
Data regarding EBV-specific CTLs for EBV-positive PTLD in SOT recipients is limited. Most PTLDs in SOT are recipient in origin, and HLA mismatch between donor-derived cells lines and the recipient tumor limits the efficacy of donor-derived CTLs [71]. Furthermore, lymphocytes from deceased SOT donors may not be readily available. Third-party EBV-specific CTLs with best available HLA match circumvents the issues of donor lymphocyte accessibility and donor/recipient HLA mismatch, and has been used successfully for treatment of PTLD in SOT recipients. In 33 patients receiving third-party EBV-specific CTLs for refractory EBV-positive PTLD (31 SOT, 2 HCT), 52% achieved partial or complete response at 6 months, and closer HLA matching was associated with better responses [55]. In a cohort of 10 pediatric SOT recipients with EBV-positive PTLD receiving EBV-specific CTLs, 8 (80%) achieved remission [72].
New Chemotherapy/BITE/CAR-T therapy
CD-19-directed chimeric antigen receptor-T-(CAR-T) cell immunotherapy is an effective treatment for relapsed or refractory diffuse large B-cell lymphoma (DLBCL) [73, 74]. DLBCL accounts for 90% of monomorphic PTLDs in SOT recipients and may be either EBV-positive or EBV-negative [24]. Data for efficacy of CD-19-directed CAR-T therapies for PTLD in SOT recipients is limited. In a case series of three SOT recipients who received CD-19-directed CAR-T for DLBCL due to EBV-negative PTLD, all three patients developed significant immune effector cell associated neurotoxicity (ICANS), did not achieve clinical response, and died within four months after CAR-T infusion [75]. Programmed cell death protein 1 (PD-1) and programmed cell death ligand-1 (PD-L1) are frequently expressed in PTLD tumor cells in both SOT and HCT recipients, suggesting a future role for the treatment of PTLD, but also carries a risk of inducing graft versus host disease or solid organ allograft rejection [76]. Other potential agents in which individual case reports have described varying responses include daratumumab in rituximab-resistant, CD38 expressing EBV− PTLD following HCT [77]; zanibrutinib for CNS PTLD following HCT [78], and ibrutinib (together with CTLs) following SOT [79]. Bortezomib has also been reported in combination with rituximab [50], as well as brentuximab in CD30 expressing PTLD [80].
OUTCOMES
Despite recent advances in the prevention and treatment of EBV-PTLD, the outcomes remain poor. In a recent HCT international registry study, of 432 cases of PTLD identified, the 1-year overall survival was 53%, however only 38% of these deaths were directly attributed to PTLD [81]. In a Spanish multicenter study, 102 PTLD were identified among 12,641 HCT, leading to an estimated frequency of 0.8%. Survival was similar to the CIBMTR study, with a 2-year overall survival of 33% and the PTLD-related mortality 45% [82].
The outcomes of PTLD following SOT appear marginally better, with a report of 80 PTLD cases demonstrating a 3-year overall survival of 62%. Interestingly, patients who received rituximab-based therapy as part of initial treatment had 3-year overall survival of 73% compared with 33% without rituximab [83]. A similar report of 176 adult SOT recipients demonstrated a 2-year survival of 60% and 5-year survival of 47-49% [27].
CONCLUSION
With outcomes remaining poor after diagnosis, prevention is a critical component of the management of EBV PTLD, particularly in high-risk populations such as T-cell depleted HCT recipients and D+/R− SOT recipients. The most commonly used management strategy remains the utilization of pre-emptive therapy, however there continues to be heterogenicity and debate over the optimal choice of EBV DNA quantification and the threshold of how and when to intervene. In particular, the risk-benefit balance of over-treating with rituximab versus delaying pre-emptive treatment too long and missing the development of PTLD, which can be rapid, particularly in a T cell depleted HCT recipient. Future management strategies with prophylactic or pre-emptive EBV specific or multi-pathogen CTLs have shown promising results and safety profiles, which may be the pre-emptive treatment of choice over rituximab following the publication of current phase III trials.
KEY POINTS:
Prevention is a critical component of the management of EBV PTLD, particularly in high-risk populations such as T-cell depleted HCT and EBV D+/R− SOT.
Although pre-emptive management remains standard of care, there continues to be debate and variability of practice in the optimal choice of EBV DNA quantification and the threshold to use.
Future management strategies with prophylactic or pre-emptive EBV specific or multi-pathogen CTLs show promising efficacy and safety profiles
FUNDING
This work was supported by the National Institute of Allergy and Infectious Diseases (T32AI118690 to M.R.H.) at the National Institutes of Health. JL is supported by a Leukaemia Foundation (LF) and Haematology Society of Australia and New Zealand (HSANZ) New Investigator PhD Scholarship. MS is supported by NHMRC CRE and Investigator Grants (1116876 and 1173791). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
DECLARATION OF INTEREST
J.L. reports receiving honoraria from MSD and Gilead. M.R.H reports receiving speaking honoraria from Cigna LifeSource and Thermo Fisher Scientific.
REFERENCES
Papers of special note have been highlighted as either of interest (*) or of considerable interest (**) to readers.
- 1.Kimura H, Ito Y, Suzuki R, Nishiyama Y. Measuring Epstein-Barr virus (EBV) load: the significance and application for each EBV-associated disease. Rev Med Virol 2008; 18:305–319. [DOI] [PubMed] [Google Scholar]
- 2.Balfour HH Jr., Dunmire SK, Hogquist KA. Infectious mononucleosis. Clin Transl Immunology 2015; 4:e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Styczynski J, van der Velden W, Fox CP et al. Management of Epstein-Barr Virus infections and post-transplant lymphoproliferative disorders in patients after allogeneic hematopoietic stem cell transplantation: Sixth European Conference on Infections in Leukemia (ECIL-6) guidelines. Haematologica 2016; 101:803–811. ** The most current, well recognized guidelines for PTLD in HCT, including prevention, diagnostic and management guidance
- 4.Haidar G, Singh N. Viral infections in solid organ transplant recipients: novel updates and a review of the classics. Curr Opin Infect Dis 2017; 30:579–588. [DOI] [PubMed] [Google Scholar]
- 5. Allen UD, Preiksaitis JK, Practice ASTIDCo. Post-transplant lymphoproliferative disorders, Epstein-Barr virus infection, and disease in solid organ transplantation: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant 2019; 33:e13652. ** The most current, well recognized guidelines for PTLD in SOT, including prevention, diagnostic and management guidance
- 6.van Esser JW, Niesters HG, van der Holt B et al. Prevention of Epstein-Barr virus-lymphoproliferative disease by molecular monitoring and preemptive rituximab in high-risk patients after allogeneic stem cell transplantation. Blood 2002; 99:4364–4369. [DOI] [PubMed] [Google Scholar]
- 7.Styczynski J, Einsele H, Gil L, Ljungman P. Outcome of treatment of Epstein-Barr virus-related post-transplant lymphoproliferative disorder in hematopoietic stem cell recipients: a comprehensive review of reported cases. Transpl Infect Dis 2009; 11:383–392. [DOI] [PubMed] [Google Scholar]
- 8.Baron F, Mohty M, Blaise D et al. Anti-thymocyte globulin as graft-versus-host disease prevention in the setting of allogeneic peripheral blood stem cell transplantation: a review from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica 2017; 102:224–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kekre N, Antin JH. ATG in allogeneic stem cell transplantation: standard of care in 2017? Counterpoint. Blood Adv 2017; 1:573–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fujimoto A, Hiramoto N, Yamasaki S et al. Risk Factors and Predictive Scoring System For Post-Transplant Lymphoproliferative Disorder after Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant 2019; 25:1441–1449. [DOI] [PubMed] [Google Scholar]
- 11.Kalra A, Roessner C, Jupp J et al. Risk factors for post-transplant lymphoproliferative disorder after Thymoglobulin-conditioned hematopoietic cell transplantation. Clin Transplant 2018; 32. [DOI] [PubMed] [Google Scholar]
- 12. Ru Y, Zhang X, Song T et al. Epstein-Barr virus reactivation after allogeneic hematopoietic stem cell transplantation: multifactorial impact on transplant outcomes. Bone Marrow Transplant 2020; 55:1754–1762. * One of four large scale HCT analyses to describe the rate for EBV DNAemia and PTLD on the past 2 years. A particular focus on risk factors.
- 13.Bonifazi F, Rubio MT, Bacigalupo A et al. Rabbit ATG/ATLG in preventing graft-versus-host disease after allogeneic stem cell transplantation: consensus-based recommendations by an international expert panel. Bone Marrow Transplant 2020; 55:1093–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Othman J, Greenwood M, Moore J et al. Unrelated Donor Transplant Recipients Given Thymoglobuline Have Superior GRFS When Compared to Matched Related Donor Recipients Undergoing Transplantation without ATG. Biol Blood Marrow Transplant 2020. [DOI] [PubMed] [Google Scholar]
- 15.Ali MM, Grønvold B, Remberger M et al. Addition of anti-thymocyte globulin in allogeneic stem cell transplantation with peripheral stem cells from matched unrelated donors improves graft-versus-host disease and relapse free survival. Clinical Lymphoma Myeloma and Leukemia 2021; S2152-2650:00179–00178. [DOI] [PubMed] [Google Scholar]
- 16.Esquirol A, Pascual MJ, Kwon M et al. Severe infections and infection-related mortality in a large series of haploidentical hematopoietic stem cell transplantation with post-transplant cyclophosphamide. Bone Marrow Transplant 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanakry JA, Kasamon YL, Bolanos-Meade J et al. Absence of post-transplantation lymphoproliferative disorder after allogeneic blood or marrow transplantation using post-transplantation cyclophosphamide as graft-versus-host disease prophylaxis. Biol Blood Marrow Transplant 2013; 19:1514–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salas MQ, Prem S, Remberger M et al. High incidence but low mortality of EBV-reactivation and PTLD after alloHCT using ATG and PTCy for GVHD prophylaxis. Leuk Lymphoma 2020; 61:3198–3208. [DOI] [PubMed] [Google Scholar]
- 19.Green M, Michaels MG. Epstein-Barr virus infection and posttransplant lymphoproliferative disorder. Am J Transplant 2013; 13 Suppl 3:41–54; quiz 54. [DOI] [PubMed] [Google Scholar]
- 20.Peters AC, Akinwumi MS, Cervera C et al. The Changing Epidemiology of Posttransplant Lymphoproliferative Disorder in Adult Solid Organ Transplant Recipients Over 30 Years: A Single-center Experience. Transplantation 2018; 102:1553–1562. [DOI] [PubMed] [Google Scholar]
- 21.Dharnidharka VR, Lamb KE, Gregg JA, Meier-Kriesche HU. Associations between EBV serostatus and organ transplant type in PTLD risk: an analysis of the SRTR National Registry Data in the United States. Am J Transplant 2012; 12:976–983. [DOI] [PubMed] [Google Scholar]
- 22.Yamada M, Nguyen C, Fadakar P et al. Epidemiology and outcome of chronic high Epstein-Barr viral load carriage in pediatric kidney transplant recipients. Pediatr Transplant 2018; 22:e13147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sampaio MS, Cho YW, Shah T et al. Impact of Epstein-Barr virus donor and recipient serostatus on the incidence of post-transplant lymphoproliferative disorder in kidney transplant recipients. Nephrol Dial Transplant 2012; 27:2971–2979. [DOI] [PubMed] [Google Scholar]
- 24.Dierickx D, Habermann TM. Post-Transplantation Lymphoproliferative Disorders in Adults. N Engl J Med 2018; 378:549–562. [DOI] [PubMed] [Google Scholar]
- 25.Hall EC, Engels EA, Pfeiffer RM, Segev DL. Association of antibody induction immunosuppression with cancer after kidney transplantation. Transplantation 2015; 99:1051–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Durrbach A, Pestana JM, Florman S et al. Long-Term Outcomes in Belatacept- Versus Cyclosporine-Treated Recipients of Extended Criteria Donor Kidneys: Final Results From BENEFIT-EXT, a Phase III Randomized Study. Am J Transplant 2016; 16:3192–3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luskin MR, Heil DS, Tan KS et al. The Impact of EBV Status on Characteristics and Outcomes of Posttransplantation Lymphoproliferative Disorder. Am J Transplant 2015; 15:2665–2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferla V, Rossi FG, Goldaniga MC, Baldini L. Biological Difference Between Epstein-Barr Virus Positive and Negative Post-transplant Lymphoproliferative Disorders and Their Clinical Impact. Front Oncol 2020; 10:506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lindsay J, Yong MK, Greenwood M et al. Epstein-Barr virus related post-transplant lymphoproliferative disorder prevention strategies in allogeneic hematopoietic stem cell transplantation. Rev Med Virol 2020; 30:e2108. [DOI] [PubMed] [Google Scholar]
- 30.Kanakry JA, Hegde AM, Durand CM et al. The clinical significance of EBV DNA in the plasma and peripheral blood mononuclear cells of patients with or without EBV diseases. Blood 2016; 127:2007–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Semenova T, Lupo J, Alain S et al. Multicenter Evaluation of Whole-Blood Epstein-Barr Viral Load Standardization Using the WHO International Standard. J Clin Microbiol 2016; 54:1746–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Solano C, Mateo EM, Perez A et al. Epstein-Barr virus DNA load kinetics analysis in allogeneic hematopoietic stem cell transplant recipients: Is it of any clinical usefulness? J Clin Virol 2017; 97:26–32. [DOI] [PubMed] [Google Scholar]
- 33.Wareham NE, Mocroft A, Sengelov H et al. The value of EBV DNA in early detection of post-transplant lymphoproliferative disorders among solid organ and hematopoietic stem cell transplant recipients. J Cancer Res Clin Oncol 2018; 144:1569–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kalra A, Roessner C, Jupp J et al. Epstein-barr virus DNAemia monitoring for the management of post-transplant lymphoproliferative disorder. Cytotherapy 2018; 20:706–714. [DOI] [PubMed] [Google Scholar]
- 35.Raberahona M, Wackenheim C, Germi R et al. Dynamics of Epstein-Barr viral load after hematopoietic stem cell transplantation and effect of preemptive rituximab therapy. Transpl Infect Dis 2016; 18:889–895. [DOI] [PubMed] [Google Scholar]
- 36. Marzolini M, Wilson A, Sanchez E et al. Natural history of EBV replication and viral load dynamics after alemtuzumab based allogeneic stem cell transplantation. Transplantation and Cellular Therapy 2021. * One of four large scale HCT analyses to describe the rate for EBV DNAemia and PTLD on the past 2 years. A particular focus on alemtuzumab GVHD prophyalxis
- 37. Jain T, Kosiorek HE, Grys TE et al. Single dose versus multiple doses of rituximab for preemptive therapy of Epstein-Barr virus reactivation after hematopoietic cell transplantation. Leuk Lymphoma 2019; 60:110–117. * One of four large scale HCT analyses to describe the rate for EBV DNAemia and PTLD on the past 2 years. A particular focus on pre-emptive threshold for rituximab therapy
- 38.Jain T, Kung ST, Kosiorek H et al. Outcomes with Pre-Emptive Rituximab (pre-R) Treatment for Epstein-Barr Viremia (EBV) after Allogeneic Hematopoietic Stem Cell Transplantation (HCT). Biology of Blood and Marrow Transplantation 2017; 23:S279–S280. [Google Scholar]
- 39.Michallet M, Sobh M, Ranchon F et al. Epstein-Barr Virus (EBV) Reactivation, Its Treatment with Rituximab and Their Impact on Relapse after Allogeneic Hematopoietic Stem Cell Transplantation for Hematological Malignancies. Blood 2016; 128:3695–3695. [Google Scholar]
- 40.Lee TC, Savoldo B, Rooney CM et al. Quantitative EBV viral loads and immunosuppression alterations can decrease PTLD incidence in pediatric liver transplant recipients. Am J Transplant 2005; 5:2222–2228. [DOI] [PubMed] [Google Scholar]
- 41.McDiarmid SV, Jordan S, Kim GS et al. Prevention and preemptive therapy of postransplant lymphoproliferative disease in pediatric liver recipients. Transplantation 1998; 66:1604–1611. [DOI] [PubMed] [Google Scholar]
- 42.AlDabbagh MA, Gitman MR, Kumar D et al. The Role of Antiviral Prophylaxis for the Prevention of Epstein-Barr Virus-Associated Posttransplant Lymphoproliferative Disease in Solid Organ Transplant Recipients: A Systematic Review. Am J Transplant 2017; 17:770–781. [DOI] [PubMed] [Google Scholar]
- 43.Green M, Kaufmann M, Wilson J, Reyes J. Comparison of intravenous ganciclovir followed by oral acyclovir with intravenous ganciclovir alone for prevention of cytomegalovirus and Epstein-Barr virus disease after liver transplantation in children. Clin Infect Dis 1997; 25:1344–1349. [DOI] [PubMed] [Google Scholar]
- 44.Montes de Jesus FM, Kwee TC, Kahle XU et al. Diagnostic performance of FDG-PET/CT of post-transplant lymphoproliferative disorder and factors affecting diagnostic yield. Eur J Nucl Med Mol Imaging 2020; 47:529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burns DM, Rana S, Martin E et al. Greatly reduced risk of EBV reactivation in rituximab-experienced recipients of alemtuzumab-conditioned allogeneic HSCT. Bone Marrow Transplant 2016; 51:825–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bacigalupo A, Dominietto A, Soracco M et al. Rituximab Prophylaxis of EBV Reactivation after Alternative Donor Transplants Following Anti-Thymocyte Globulin-Based Conditioning Regimens. Blood 2008; 112. [Google Scholar]
- 47.Dominietto A, Tedone E, Soracco M et al. In vivo B-cell depletion with rituximab for alternative donor hemopoietic SCT. Bone Marrow Transplant 2012; 47:101–106. [DOI] [PubMed] [Google Scholar]
- 48.Peccatori J, Forcina A, Clerici D et al. Sirolimus-based graft-versus-host disease prophylaxis promotes the in vivo expansion of regulatory T cells and permits peripheral blood stem cell transplantation from haploidentical donors. Leukemia 2015; 29:396–405. [DOI] [PubMed] [Google Scholar]
- 49. Van Besien K, Bachier-Rodriguez L, Satlin M et al. Prophylactic rituximab prevents EBV PTLD in haplo-cord transplant recipients at high risk. Leuk Lymphoma 2019; 60:1693–1696. * One of four large scale HCT analyses to describe the rate for EBV DNAemia and PTLD on the past 2 years. A particular focus on high risk (hplo-cord HCT with rituximab prophylaxis
- 50. Al Hamed R, Bazarbachi AH, Mohty M. Epstein-Barr virus-related post-transplant lymphoproliferative disease (EBV-PTLD) in the setting of allogeneic stem cell transplantation: a comprehensive review from pathogenesis to forthcoming treatment modalities. Bone Marrow Transplant 2020; 55:25–39. * An excellent summary of EBV PTLD in HCT with a more detailed, practical approach to management compared to the 2016 ECIL guidelines.
- 51.Walti LN, Mugglin C, Sidler D et al. Association of antiviral prophylaxis and rituximab use with posttransplant lymphoproliferative disorders (PTLDs): A nationwide cohort study. Am J Transplant 2021; 21:2532–2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Doubrovina E, Oflaz-Sozmen B, Prockop SE et al. Adoptive immunotherapy with unselected or EBV-specific T cells for biopsy-proven EBV+ lymphomas after allogeneic hematopoietic cell transplantation. Blood 2012; 119:2644–2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Leen AM, Bollard CM, Mendizabal AM et al. Multicenter study of banked third-party virus-specific T cells to treat severe viral infections after hematopoietic stem cell transplantation. Blood 2013; 121:5113–5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Heslop HE, Slobod KS, Pule MA et al. Long-term outcome of EBV-specific T-cell infusions to prevent or treat EBV-related lymphoproliferative disease in transplant recipients. Blood 2010; 115:925–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Haque T, Wilkie GM, Jones MM et al. Allogeneic cytotoxic T-cell therapy for EBV-positive posttransplantation lymphoproliferative disease: results of a phase 2 multicenter clinical trial. Blood 2007; 110:1123–1131. [DOI] [PubMed] [Google Scholar]
- 56.Gottlieb DJ, Clancy LE, Withers B et al. Prophylactic antigen-specific T-cells targeting seven viral and fungal pathogens after allogeneic haemopoietic stem cell transplant. Clin Transl Immunology 2021; 10:e1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Blyth E, Jiang W, Clancy L et al. Allogeneic stem cell transplant (HSCT) for acute lymphoblastic leukaemia (ALL) using CD34 selected stem cells followed by prophylactic infusions of pathogen-specific and CD19 CAR T cells. Cytotherapy 2020; 22:S17–S18. [Google Scholar]
- 58.Papadopoulou A, Koukoulias K, Alvanou M et al. Multipathogen-specific T cells against viral and fungal infections. Bone Marrow Transplant 2021; 56:1445–1448. [DOI] [PubMed] [Google Scholar]
- 59.Tzannou I, Papadopoulou A, Watanabe A et al. Adoptive immunotherapy with rapidly-generated multivirus-specific T cells against Adv, EBV, CMV, HHV6 and BK after allogeneic hematopoietic stem cell transplant. Biology of Blood and Marrow Transplantation 2018; 24:S75. [Google Scholar]
- 60.Hellewell EM, Skeffington LR, Kenyon MI et al. Incidence of Epstein-Barr Virus (EBV) Detection in the Blood, Pre-Emptive Therapy, and EBV-Posttransplantation Lymphoproliferative Disorder (EBV-PTLD) after Allogeneic Hematopoietic Cell Transplantation (HCT) across a Broad Range of HCT Approaches and All Graft Sources. Biology of Blood and Marrow Transplantation 2019; 25:S353–S354. [Google Scholar]
- 61.Reddy N, Rezvani K, Barrett AJ, Savani BN. Strategies to prevent EBV reactivation and posttransplant lymphoproliferative disorders (PTLD) after allogeneic stem cell transplantation in high-risk patients. Biol Blood Marrow Transplant 2011; 17:591–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pascual J, Royuela A, Fernandez AM et al. Role of mTOR inhibitors for the control of viral infection in solid organ transplant recipients. Transpl Infect Dis 2016; 18:819–831. [DOI] [PubMed] [Google Scholar]
- 63.Sokal EM, Hoppenbrouwers K, Vandermeulen C et al. Recombinant gp350 vaccine for infectious mononucleosis: a phase 2, randomized, double-blind, placebo-controlled trial to evaluate the safety, immunogenicity, and efficacy of an Epstein-Barr virus vaccine in healthy young adults. J Infect Dis 2007; 196:1749–1753. [DOI] [PubMed] [Google Scholar]
- 64.van Zyl DG, Mautner J, Delecluse HJ. Progress in EBV Vaccines. Front Oncol 2019; 9:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Styczynski J, Gil L, Tridello G et al. Response to rituximab-based therapy and risk factor analysis in Epstein Barr Virus-related lymphoproliferative disorder after hematopoietic stem cell transplant in children and adults: a study from the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Clin Infect Dis 2013; 57:794–802. [DOI] [PubMed] [Google Scholar]
- 66.Prockop S, Doubrovina E, Suser S et al. Off-the-shelf EBV-specific T cell immunotherapy for rituximab-refractory EBV-associated lymphoma following transplantation. J Clin Invest 2020; 130:733–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Di Ciaccio PR, Avdic S, Sutrave G et al. Successful treatment of CMV, EBV, and adenovirus tissue infection following HLA-mismatched allogeneic stem cell transplant using infusion of third-party T cells from multiple donors in addition to antivirals, rituximab, and surgery. Transpl Infect Dis 2021; 23:e13528. [DOI] [PubMed] [Google Scholar]
- 68.Prockop S, Hiremath M, Ye W et al. A Multicenter, Open Label, Phase 3 Study of Tabelecleucel for Solid Organ Transplant Subjects with Epstein-Barr Virus-Driven Post-Transplant Lymphoproliferative Disease (EBV+ PTLD) after Failure of Rituximab or Rituximab and Chemotherapy. In: American Society of Hematology; Washington, DC; 2019. [Google Scholar]
- 69.Worel N, Perez-Simon J, Barba P et al. 29P ALLELE study: A multicenter, open label, phase III study of tabelecleucel for solid organ or allogeneic hematopoietic cell transplant subjects with Epstein-Barr virus-driven post-transplant lymphoproliferative disease (EBV+ PTLD) after failure of rituximab or rituximab and chemotherapy. Annals of Oncology 2020; 31:S1426–S1427. [Google Scholar]
- 70.Withers B, Blyth E, Clancy LE et al. Long-term control of recurrent or refractory viral infections after allogeneic HSCT with third-party virus-specific T cells. Blood Adv 2017; 1:2193–2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.O'Reilly RJ, Prockop S, Hasan AN et al. Virus-specific T-cell banks for 'off the shelf' adoptive therapy of refractory infections. Bone Marrow Transplant 2016; 51:1163–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chiou FK, Beath SV, Wilkie GM et al. Cytotoxic T-lymphocyte therapy for post-transplant lymphoproliferative disorder after solid organ transplantation in children. Pediatr Transplant 2018; 22. [DOI] [PubMed] [Google Scholar]
- 73.Locke FL, Ghobadi A, Jacobson CA et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1-2 trial. Lancet Oncol 2019; 20:31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schuster SJ, Bishop MR, Tam CS et al. Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N Engl J Med 2019; 380:45–56. [DOI] [PubMed] [Google Scholar]
- 75.Krishnamoorthy S, Ghobadi A, Santos RD et al. CAR-T therapy in solid organ transplant recipients with treatment refractory posttransplant lymphoproliferative disorder. Am J Transplant 2021; 21:809–814. [DOI] [PubMed] [Google Scholar]
- 76.Schiefer AI, Salzer E, Füreder A et al. PD-L1 and PD1 expression in post-transplantation lymphoproliferative disease (PTLD) of childhood and adolescence: An inter- and intra-individual descriptive study covering the whole spectrum of PTLD categories. Cancer Med 2019; 8:4656–4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Strunz PP, Schmalzing M, Heidemeier A et al. Response to daratumumab in rituximab-resistant EBV-associated PTLD following allogenic stem cell transplantation from an EBV seronegative donor. Leuk Lymphoma 2019; 60:3573–3576. [DOI] [PubMed] [Google Scholar]
- 78. Yang TT, Chen WH, Zhao YM et al. Zanubrutinib Treatment of Central Nervous System Posttransplant Lymphoproliferative Disorder After Allogeneic Hematopoietic Stem Cell Transplantation: A Case Report. Front Oncol 2021; 11:672052. * A recent large regisitry report of 432 PTLD cases following HCT with mulitvariable survival anaysis.
- 79.Law SC, Hoang T, O'Rourke K et al. Successful treatment of Epstein-Barr virus-associated primary central nervous system lymphoma due to post-transplantation lymphoproliferative disorder, with ibrutinib and third-party Epstein-Barr virus-specific T cells. Am J Transplant 2021. [DOI] [PubMed] [Google Scholar]
- 80.Mika T, Strate K, Ladigan S et al. Refractory Epstein-Barr Virus (EBV)-Related Post-transplant Lymphoproliferative Disease: Cure by Combined Brentuximab Vedotin and Allogeneic EBV-Specific T-Lymphocytes. Front Med (Lausanne) 2019; 6:295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Naik S, Riches M, Hari P et al. Survival outcomes of allogeneic hematopoietic cell transplants with EBV-positive or EBV-negative post-transplant lymphoproliferative disorder, A CIBMTR study. Transpl Infect Dis 2019:e13145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Garcia-Cadenas I, Yanez L, Jarque I et al. Frequency, characteristics, and outcome of PTLD after allo-SCT: A multicenter study from the Spanish group of blood and marrow transplantation (GETH). Eur J Haematol 2019; 102:465–471. [DOI] [PubMed] [Google Scholar]
- 83.Evens AM, David KA, Helenowski I et al. Multicenter analysis of 80 solid organ transplantation recipients with post-transplantation lymphoproliferative disease: outcomes and prognostic factors in the modern era. J Clin Oncol 2010; 28:1038–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Landgren O, Gilbert ES, Rizzo JD et al. Risk factors for lymphoproliferative disorders after allogeneic hematopoietic cell transplantation. Blood 2009; 113:4992–5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Uhlin M, Wikell H, Sundin M et al. Risk factors for Epstein-Barr virus-related post-transplant lymphoproliferative disease after allogeneic hematopoietic stem cell transplantation. Haematologica 2014; 99:346–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fox CP, Burns D, Parker AN et al. EBV-associated post-transplant lymphoproliferative disorder following in vivo T-cell-depleted allogeneic transplantation: clinical features, viral load correlates and prognostic factors in the rituximab era. Bone Marrow Transplant 2014; 49:280–286. [DOI] [PubMed] [Google Scholar]
- 87.Chakrabarti S, Milligan DW, Pillay D et al. Reconstitution of the Epstein-Barr virus-specific cytotoxic T-lymphocyte response following T-cell-depleted myeloablative and nonmyeloablative allogeneic stem cell transplantation. Blood 2003; 102:839–842. [DOI] [PubMed] [Google Scholar]


