The 2017 American College of Cardiology/American Heart Association (ACC/AHA) blood pressure (BP) guideline provides a Class IA recommendation for the use of home BP monitoring, team-based care, and telehealth strategies to improve BP control among patients with hypertension.1 However, most studies have been conducted in integrated health systems among white populations with higher socioeconomic status. This study aimed to evaluate the feasibility, safety, and effectiveness of home BP telemonitoring with remote hypertension management among a predominately rural and low-income population.
This prospective cohort study at the University of Mississippi Medical Center (UMMC) was conducted from September 4, 2018 through June 15, 2020. Patients with uncontrolled clinic hypertension, BP ≥ 140/90 mm Hg, were recruited and provided informed consent using a digital method previously described.2 Exclusion criteria included Stage 4 or 5 chronic kidney disease, cardiovascular event in the preceding 3 months, congestive heart failure with a left ventricular ejection fraction <50%, pregnancy, and institutionalization or major comorbidity limiting ability to perform self-monitoring. Participants received a telemonitoring kit, including an electronic tablet and home BP monitor with Bluetooth connectivity – Welch Allyn RPM-BP100SBP upper arm cuff available with large or extra-large cuff sizes. Via the tablet, a nurse coordinator provided virtual onboarding, including visual cuff size assessment and BP measurement instruction. Prior to measuring BP, participants were instructed to sit quietly for 5 minutes with both feet flat on the floor with back and arm supported. Participants were instructed to transmit daily BP readings including 2 measurements obtained one minute apart. BP reviews were conducted every 3 weeks by the clinical pharmacist. If average BP was not at goal BP <130/80 mm Hg then antihypertensive medication therapy was up-titrated by the pharmacist according to pre-specified algorithm based on the 2017 ACC/AHA guideline.1 If patients experienced adverse effects, medication dosages would be lowered or the drug switched. Blood pressure summaries and medication changes were communicated with the patient’s primary care team through the electronic medical record.
In total, 120 individuals were enrolled in this study. At baseline, participants had a mean (SD) age of 59.3 (10.8) years, 65% were women, and 59.2% were African American. More than one in four (27.5%) did not complete high school and nearly half (46.7%) reported an annual household income <$30,000. Participants lived a mean (SD) of 32.6 (31) miles from UMMC main campus and 29.2% resided in a federally designated rural county. Of the 120 enrolled individuals, 103 (85.8%) participants successfully completed the entire 6-month study protocol. Reasons for study withdrawal included non-adherence (12), did not wish to continue the study (3), hospitalization (1), and other (1).
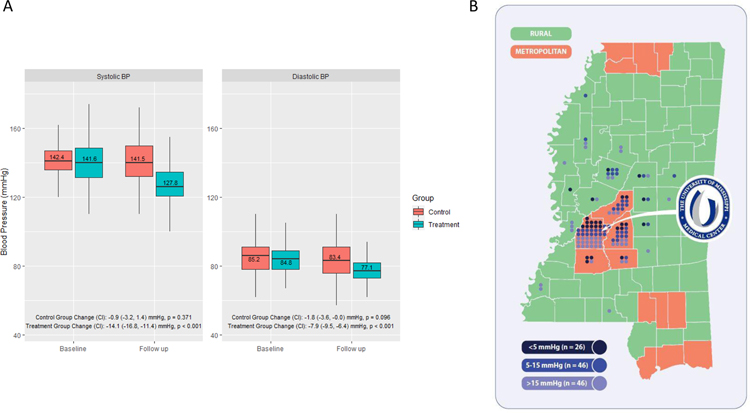
The mean duration of study participation was 178 days (5.9 months). A total of 118 participants completed at least 1 follow up BP review. Overall, there were a total of 982 BP reviews. The mean (SD) number of BP measurements per review was 22.4 (17.2). Medication therapy was intensified in 238 reviews. The mean (SD) number of prescribed antihypertensive medications at baseline compared to follow up increased from 2.0 (1.3) to 2.6 (1.3), p <0.001. At baseline, the mean (SD) systolic and diastolic BP was 141.6 (14.1) and 84.8 (10.1) mm Hg, respectively. At 6 month follow the mean (SD) systolic and diastolic BP was 127.8 (11.9) and 77.1 (8.3) mm Hg, respectively. The mean difference in systolic BP change was −14.1 mm Hg (95% CI to −16.8 to −11.4 mm Hg) at follow up (p <0.001). The mean difference in diastolic BP change was −7.9 mm Hg (95% CI −9.5 to −6.4 mm Hg) at follow up (p <0.001). Among participants with at least one follow up review a total of 59 (50%) achieved average BP <130/80 mm Hg, and 95 (80.5%) achieved average goal BP <140/90 mm Hg. A total of 46 (38.9%) participants achieved mean home BP reduction >15 mm Hg, of which 16 (13.5%) resided in a federally designated rural county (Figure). There were 4 serious adverse events (3.3%) that were possibly or definitely related to the intervention and included syncope (2), symptomatic hypotension (1), and angioedema (1).
Figure. Change in blood pressure and geographic residence of study participants.
A, Change in treatment and matched control systolic and diastolic BP measurement at baseline and follow up. B, Map showing county residence of study participants stratified by rural and metropolitan counties and degree of blood pressure reduction <5 mmHg, 5–15 mmHg, >15 mmHg.
The comparison group comprised an electronic health record query including adult patients seen at UMMC in 2018 with a primary diagnosis of hypertension, systolic BP ≥140 mm Hg or diastolic BP ≥90 mm Hg, a follow up visit within 6–12 months, and none of the exclusion criteria outlined above. A total of 871 patients were identified. Overall, among unmatched controls the baseline mean (SD) systolic and diastolic BP were 152.7 (15.4) and 84.4 (12.0) mm Hg and the mean difference in BP change was −7.3 mm Hg (95% CI to −8.7 to −6.0 mm Hg, p <0.001) and −2.4 mm Hg (95% CI −3.3 to −1.6 mm Hg, p <0.001), respectively. Propensity score was estimated with a multivariate logistic regression using age, sex, race, and baseline systolic and diastolic BP as predictors. Using optimal matching, treatment and control groups were matched in a 1:2 ratio with an absolute propensity score distance <0.25 and balanced baseline characteristics. Among matched controls, mean (SD) age was 60.2 (14.8) years, 67% were female, and 54.9% were African American. At baseline, the mean (SD) systolic and diastolic BP was 142.4 (11.8) and 85.2 (10.6) mm Hg, respectively. At follow the mean (SD) systolic and diastolic BP was 141.5 (15.6) and 83.4 (13.9) mm Hg, respectively. The mean difference in systolic BP change for matched controls was −0.9 mm Hg (95% CI to −3.2 to 1.4 mm Hg, p =0.37). The mean difference in diastolic BP change for matched controls was −1.8 mm Hg (95% CI −3.6 to 0.0 mm Hg, p = 0.096) (Figure). All data analyses were conducted using SAS statistical software (version 9.4, SAS Institute Inc, Cary, NC).
Our results show that home BP telemonitoring with remote hypertension management in a rural and low-income population is feasible and associated with significant BP reduction. In the current study >85% of enrolled participants completed the 6-month protocol with a 14.1 mm Hg mean reduction in systolic BP. Over 900 BP reviews and 200 medication adjustments were conducted remotely with a significant increase in number of prescribed antihypertensive medications. The intervention also appeared to have an acceptable level of safety. A major finding of this study was the association of home BP telemonitoring and BP reduction among rural, minority, and low-income individuals with hypertension. In the current study nearly one third of participants resided in a rural county, a majority were African American, almost half reported a household income <$30,000/year. Acknowledging limitations in the non-randomized design and BP measurement technique, comparing results from the intervention and matched control group suggests that remote telemonitoring with hypertension management is associated with greater reductions in BP and lower achieved target BP as compared to usual clinic based care. The present study adds to prior work showing that BP telemonitoring with pharmacist case management is superior to usual care in controlling BP among individuals with hypertension. Prior studies have been conducted among populations that were predominately white, higher socioeconomic status, and/or receiving care in integrated health systems3–5 – highlighting the need to evaluate telehealth treatment strategies in underserved populations. These findings are particularly relevant in the current health care environment. In 2019, the Centers for Medicare and Medicaid introduced expanded reimbursement for remote patient monitoring. This potentially enabling change in the reimbursement environment highlights the critical need for research to guide the optimal clinical adoption of home based telemonitoring management strategies. Insights from the current study have informed implementation of an active clinical program utilizing home BP telemonitoring for hypertension management at our institution. Further research is needed to evaluate measures of clinical and economic impact for remote telemonitoring services delivered as part of routine clinical care.
Funding/Support:
The University of Mississippi Medical Center received grants from Federal Office of Rural Health Policy, Health Resources and Services Administration, and the US Department of Health and Human Services under cooperative agreement award 6 U66RH31459-02-03 that supported this study. Dr Clark received support from the American Heart Association (award 19CDA34760232) during the conduct of the study. Additional support was received from the National Institute of General Medical Sciences/National Institutes of Health (grant 5U54GM115428).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported.
Disclaimer: The information, conclusions, and opinions expressed are those of the authors, and no endorsement by Federal Office of Rural Health Policy, Health Resources and Services Administration, and the US Department of Health and Human Services is intended or should be inferred.
References
- 1.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 06 2018;71(6):e13–e115. doi: 10.1161/HYP.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 2.Clark D, Woods J, Patki D, et al. Digital Informed Consent in a Rural and Low-Income Population. JAMA Cardiol. May 2020;doi: 10.1001/jamacardio.2020.0984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA July 2013;310(1):46–56. doi: 10.1001/jama.2013.6549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. June 2008;299(24):2857–67. doi: 10.1001/jama.299.24.2857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bosworth HB, Powers BJ, Olsen MK, et al. Home blood pressure management and improved blood pressure control: results from a randomized controlled trial. Arch Intern Med. July 2011;171(13):1173–80. doi: 10.1001/archinternmed.2011.276 [DOI] [PubMed] [Google Scholar]