Abstract
Objective
Optimal tooth reduction is a key requirement for aesthetics, function, and the longevity of fixed restorations. Research has demonstrated that controlled and conservative tooth preparation is crucial for the long-term success of adhesive restorations. Different techniques of fabricating reduction guides have been previously reported in literature. The present technical note describes the fabrication technique and clinical application of a customized metal preparation reduction guide.
Material and method
Patient presented with tilted maxillary left central incisor. The flared-out part of the tooth was modified prior to veneer restoration preparation. Resin pattern reduction guide was fabricated on the diagnostic cast with a window on the tilted mesial portion of the tooth. After intraoral evaluation, resin pattern guide was casted. Metal reduction guide was place intraorally and reduction was provided on the exposed surface of the tooth. After the removal of the tilted portion, a harmonious arch form allowed the clinician to provide adequate evaluation and preparation for veneer restorations.
Results
The device demonstrated good practical value, allowing for selective and controlled reduction of tooth structure, and definitive protection of adjacent tooth surfaces from iatrogenic damage. The clinical outcome successfully addressed the patient’s restorative and aesthetic needs, and the veneer was stable 2 years postoperatively.
Conclusion
Use of a metal guide assists clinicians to provide a more predictable reduction of a desired tooth surface, while decreasing the risk of compromising the other/adjacent tooth surfaces.
Keywords: Veneers, Prosthodontics, Esthetic dentistry, Tooth preparation
1. Introduction
Ideal tooth preparation ensures a uniform and sufficient reduction of tooth structure, without affecting the periodontal health, aesthetics, and structural durability of the restoration (Chen and Raigrodski, 2008). It is widely accepted that extensive tooth preparation can cause hypersensitivity and pulpal damage (Cheung et al., 2005, Foster, 1990, Saito et al., 2013, Schwartz et al., 1970, Wisithphrom et al., 2006). The ability to retreat restored teeth is an important consideration of the restorative dentist when selecting a conservative or aggressive treatment option; this factor is especially important for young adult patients (Holm et al., 2003). Ideally, the most conservative strategy should always be adopted (Libby et al., 1997). Furthermore, introduction of new ceramic materials and advanced adhesive techniques have increased the popularity of all ceramic restorations and facilitated the development of innovative and conservative preparation designs for single and multiple restorations (Doyle et al., 1990, Faunce and Myer, 1976, Fradeani and Aquilano, 1997, Lehner et al., 1993, Pospiech et al., 1996, Scherrer and de Rijk, 1993, Sorensen et al., 1998). The high reliability of the enamel bond, achievable with the adhesive systems, has significantly impacted the design of tooth preparation, which targets maximal preservation of tooth structure (Buonocore, 1963). In general, as bonding to enamel yields higher bond strengths than that obtained for dentin, conservation of enamel has become an important consideration in the design of tooth preparation (Crispin, 1993a).
Veneers have emerged as a common and conservative fixed restorative technique; veneers require less than half the amount of tooth reduction in comparison to complete coverage crowns (Edelhoff and Sorensen, 2002). Nevertheless, adequate facial reduction is necessary to guarantee optimal adhesion. Excessive facial reduction can lead to compromised bond strength because of the penetration into the dentinal structure (Ozturk et al., 2013). Dr. Charles Pincus was the first to describe porcelain veneers in the late 1920s. These veneers were retained by a denture adhesive during cinematic filming (Pincus, 1938). However, adhesion proved to be unreliable, and the veneers had to be removed after filming (Pincus, 1938). Aristidis and Dimitra (2002) reported a 98.4% success rate of 184 veneers placed over a period of 5 years, while Friedman (1998) reported a 91% success rate of 191 veneers after 10 years. Veneers were initially indicated for the restoration of fractured, malformed, and discolored teeth (Crispin, 1993b, Wei and Tang, 1989). However, veneers today are included in more complex treatment scenarios, such as full mouth rehabilitation and restoration of endodontically treated teeth and worn dentition (Christensen, 1985, Ferrari et al., 1992, Tjan et al., 1989).
Tooth reduction guides are endorsed by the dental community as valuable tools that ensure sufficient space for the restorative material after tooth preparation, which protect against undesirable outcomes (Livaditis, 2002, Magne and Douglas, 1999). Use of a diagnostic wax-up is fundamental in the preparation of a tooth reduction guide and attainment of the final, desired prosthetic contours (Fareed and Solaihim, 1989). Conventional reduction guides are fabricated with either polyvinylsiloxane (PVS) putty impression material, acrylic resin, or a vacuum-formed thermoplastic sheet (Bluche et al., 1997, Gardner et al., 1990, Moskowitz et al., 1984). The reduction guide is seated intraorally, and clearance for the future restoration is evaluated visually and quantified. Despite extensive knowledge around these conventional tooth guides, very little is known about customized cast metal preparation reduction guides.
In the present report, a patient presented with slightly tilted and rotated anterior teeth and requested veneers. Limited orthodontic treatment was offered to the patient; however, the patient declined this option. Diagnostic casts were evaluated to quantify the amount of tooth structure that needed to be removed to establish harmonic maxillary arch contours. The present technical note describes the fabrication technique and clinical application of a customized metal reduction guide for minimally invasive veneer preparation.
2. Materials and methods
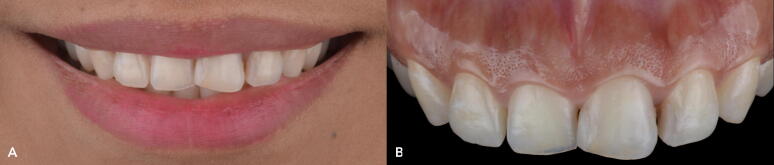
A 30-year-old female patient presented to the Autonomous University of Queretaro school of dentistry graduate prosthodontics clinic, with the chief complaint of disliking her front teeth. On clinical examination, the following findings were noted: the patient was diagnosed with incisal wear on the maxillary six anterior teeth, non-ideal gingival contours, anterior labial flaring of maxillary left central incisor, multiple diastemata between maxillary central and lateral incisors, and stained composite restorations (Fig. 1). A multidisciplinary approach that included orthodontic treatment and periodontal surgery was offered to the patient. However, she refused any surgical intervention or prolonged treatment plan. Porcelain veneers were the treatment option that the patient consented to. To address the aesthetic concerns of the patient, the flared-out (labial) aspect of maxillary left central incisor had to be reduced on the diagnostic dental cast prior to wax-up, mock-up, minimal intraoral guided teeth preparation, and cementation of the veneers. The following steps were followed:
-
1.
Diagnostic casts of type 4 dental stone (Fujirock, GC America) were fabricated.
-
2.
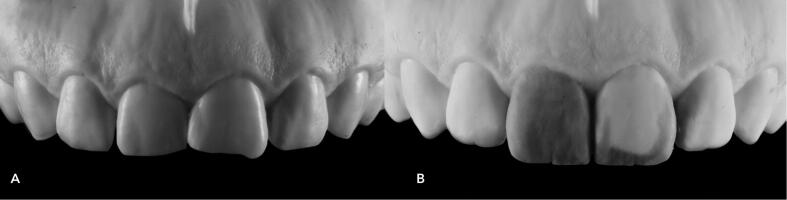
A Self-cure acrylic resin reduction guide (Pattern Resin LS, GC America) was manufactured on the diagnostic cast with a window over the flared-out aspect of maxillary left central incisor; this part of the stone cast was then removed with a cylindrical diamond bur (ZR6881, Komet USA), followed by diagnostic wax-up/build-up (Wax GEO Classic Renfert) (Fig. 2).
-
3.
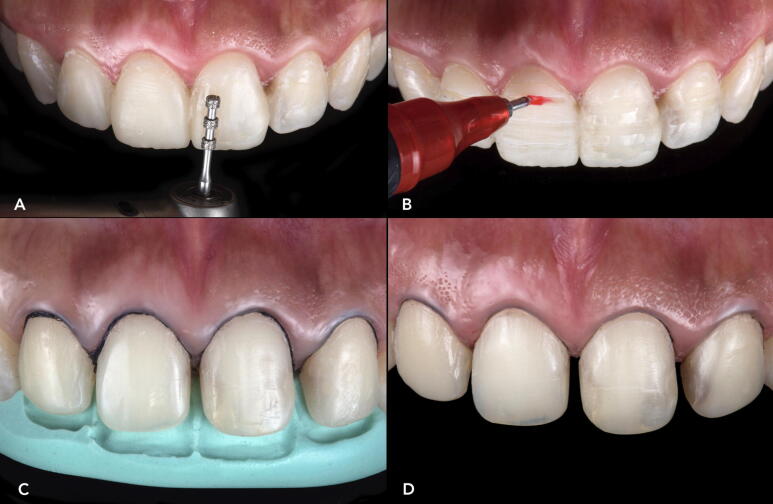
The resin pattern reduction guide was smoothed using an acrylic bur (K79ACR, Komet USA) and used intraorally to evaluate the fit (Fig. 3).
-
4.
This resin pattern reduction guide was used to cast a Chromium Cobalt metal alloy guide. At the tooth preparation appointment, the metal reduction guide was positioned intraorally, and the flared-out aspect was removed using a cylindrical diamond bur (ZR6881, Komet USA) (Fig. 4).
-
5.
An intraoral diagnostic mock-up of the final, intended result was created using temporary bis-acryl resin material (Structur Premium, VOCO) (Fig. 5A). To ensure an accurate and conservative reduction, the anterior teeth were prepared directly through the diagnostic mark-up using reductions grooves (Fig. 5B) and a putty reduction guide (Platinum 85, Zhermack) (Fig. 5C). The prepared surfaces were finalized using coarse, medium, and fine polishing discs (Sof-Lex XT Disc, 3 M).
-
6.
A double-cord impression technique was used. A size #00 retraction cord was packed deep in the sulcus followed by #0 retraction cord (Retraction Cord Plain Knitted, Ultrapak), and final impressions were taken (Fig. 5D).
-
7.
The final master cast was fabricated using a type IV dental stone (Fujirock, GC America). A refractory cast was then produced on which the feldspathic porcelain (Noritake Super porcelain EX-3, Kuraray Dental) veneers were handcrafted.
-
8.
The line angles were carefully defined during the finishing of the ceramic veneers (Fig. 6A).
-
9.
A rubber dam (Dental Dam, Nic Tone) was placed from the second premolar to the second premolar and held with clamps (Clamp #00, Hu-Friedy) to achieve complete isolation.
-
10.
The ceramic restorations were cemented using a composite bonding agent, Variolink Esthetic LC (Ivoclar Vivadent), and in accordance with the manufacturer’s instructions.
-
11.
The occlusion was checked and adjusted, and the restorations were polished using polishing points (Dialite Feather Lite, Brasseler) and a polishing paste (Dialite Intra-Oral Polishing Paste, Brasseler) (Fig. 6B and C). At the 2-year follow-up visit, the patient was still satisfied with the clinical outcome (Fig. 6D).
Fig. 1.
(A) Initial smile. (B) Initial clinical presentation.
Fig. 2.
(A) Diagnostic cast. (B) Modified cast and wax-up.
Fig. 3.

Intraoral evaluation of the resin reduction guide prior to metal casting.
Fig. 4.

(A) Metal reduction cast; lateral view depicting the window. (B) Metal reduction cast; frontal view.
Fig. 5.
(A) Diagnostic mock-up. (B) Reduction grooves. (C) Evaluating tooth reduction. (D) Final tooth preparations.
Fig. 6.
(A) Final ceramic veneers. (B) Bonded, final veneers. (C) Final smile. (D) Two-year follow-up.
3. Discussion
Improvements in adhesive dentistry have enabled more conservative approaches in aesthetic dentistry. Currently, patients seek aesthetic care to improve health, appearance, dentofacial harmony, and certain physical conditions (Brunton et al., 2000, Manos, 1993, Theobald et al., 2006). Small abnormalities or discrepancies in the anterior teeth may result in a compromised appearance and drive some individuals to seek corrective aesthetic procedures (Brunton et al., 2000). As dental clinicians cannot guarantee the longevity of any restoration, conservative tooth preparation that preserves most of the tooth structure will allow for placement of a second restoration, such as a full coverage crown if this becomes necessary (Chen and Raigrodski, 2008).
Optimal reduction of tooth structure for a ceramic veneer, without the help of a reduction guide, can be technically difficult. Over-preparation of the tooth is commonplace in the absence of a reduction guide, leading to dentinal exposure and eventually, an unreliable bond. Consequently, reduction guides are always recommended when preparing teeth for ceramic veneers (Jurado et al., 2020). Restorative dentists should familiarize themselves with the different types of tooth preparation reduction guides that are available to allow for proper clinical application (Jurado, 2019). The most common of these, the putty guide, is used to evaluate the incisal as well as the facial and/or palatal reduction that is required (Brunton et al., 2000). However, the putty guide does not allow for complete visualization of the involved tooth surfaces in comparison to the clear matrix guide, as the putty guide cannot be perforated for the examination of tooth reduction in specific locations on the teeth. Neither putty guides, nor transparent plastic matrices, enable reduction of a specific area of a tooth that is proclined or tilted. However, this challenge can be overcome through the use of a metal reduction guide that allows for the selective removal of proclined or titled tooth areas to achieve the desired contour.
Fabrication of metal reduction guides poses a challenge for many clinicians who lack knowledge of casting techniques and/or do not possess the necessary laboratory equipment. However, if the restorative dentist effectively communicates the requirements and goals of the customized metal cast guide to the dental technician, it can be readily fabricated by the dental laboratory. Clinicians will need to mark the areas to be modified when using the customized metal guide and request the technician to fabricate the guide following the lost wax technique, similar to the method employed in the manufacturing of metal-based restorations. The expenses of the customized metal cast fabrication are negligible, since fabrication does not rely on a detailed manufacturing process, such as that used in the production of inlay restorations. Furthermore, such a guide does not need to be produced from precious metal alloys. Material expense is thus less than that incurred for a conventional gold restoration.
Controlled tooth preparation ensures adequate reduction of tooth structure and creation of optimal space for the final restoration, whether this restoration is handcrafted in the dental laboratory or during dental surgery, using computer-aided design and computer-aided manufacturing (Savi et al., 2015, Stanley et al., 2018). Furthermore, guided and minimally invasive tooth preparation can retain sufficient tooth structure to allow for a situation where a full coverage crown may be needed in the future due to failure or secondary caries. This report emphasizes the need for conservative and controlled tooth reduction and urges clinicians to carefully consider this point from the patient’s perspective.
4. Conclusion
Conservative and ideal tooth preparation ensures optimal space for adequate contour and thickness of the final indirect restoration. The use of a customized metal guide for reduction in specific areas where teeth are tilted, flared-out, or rotated, can greatly assist in the controlled removal of tooth structure. The customized metal guide protects the adjacent tooth surfaces from iatrogenic damage and enables the clinician to precisely remove the selected surfaces. Once the specific areas have been reduced, the clinician can proceed with traditional mock-up and tooth preparation.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Carlos Jurado: Conceptualization, Methodology, Writing - original draft. Saad AlResayes: Methodology, Writing - review & editing. Mohammed Sayed: Methodology, Writing - review & editing. Jose Villalobos-Tinoco: Resources, Writing - review & editing, Supervision. Nayely Llanes-Urias: Conceptualization, Methodology, Supervision. Akimasa Tsujimoto: Writing - original draft, Resources.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to thank Heriberto Ureta Valenzuela, a certified dental technician (CDT) for ceramic restorations.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Carlos Alberto Jurado, Email: carlosjurado@atsu.edu.
Saad AlResayes, Email: salresayes@ksu.edu.sa.
Mohammed Edrees Sayed, Email: drsayed203@gmail.com.
Jose Villalobos-Tinoco, Email: josvt_7@hotmail.com.
Nayely Llanes-Urias, Email: njllu@hotmail.com.
Akimasa Tsujimoto, Email: akimasa-tsujimoto@uiowa.edu.
References
- Aristidis G., Dimitra B. Five-year clinical performance of porcelain laminate veneers. Quintessence Int. 2002;33:185–189. [PubMed] [Google Scholar]
- Bluche l., Bluche P., Morgano S. Vacuum-formed matrix as a guide for the fabrication of multiple direct patterns for cast post and cores. J. Prosthet. Dent. 1997;77:326–327. doi: 10.1016/s0022-3913(97)70192-6. [DOI] [PubMed] [Google Scholar]
- Brunton P.A., Aminian A., Wilson N.H. Tooth preparation techniques for porcelain laminate veneers. Br. Dent. J. 2000;189:260–262. doi: 10.1038/sj.bdj.4800739. [DOI] [PubMed] [Google Scholar]
- Buonocore M.G. Principles of adhesive retention and adhesive materials. J. Am. Dent. Assoc. 1963;67:382–391. doi: 10.14219/jada.archive.1963.0301. [DOI] [PubMed] [Google Scholar]
- Chen Y., Raigrodski A. A conservative approach for treating young adult patients with porcelain laminate veneers. J. Esthet. Restor. Dent. 2008;20:223–238. doi: 10.1111/j.1708-8240.2008.00184.x. [DOI] [PubMed] [Google Scholar]
- Cheung G.S., Lai S.C., Ng R.P. Fate of vital pulps beneath a metal-ceramic crown or a bridge retainer. Int. Endod. J. 2005;38:521–530. doi: 10.1111/j.1365-2591.2005.00982.x. [DOI] [PubMed] [Google Scholar]
- Christensen G. Veneering of teeth. State of the art. Dent. Clin. North Am. 1985;29:372–391. [PubMed] [Google Scholar]
- Crispin B.J. Enamel thickness. J. Esthet. Dent. 1993;5:37. [Google Scholar]
- Crispin B.J. Expanding the application of facial ceramic veneers. J. Calif. Dent. Assoc. 1993;21:43–46. [PubMed] [Google Scholar]
- Doyle M.G., Goodacre C.J., Munoz C.A., Andres C.J. The effect of tooth preparation design on the breaking strength of Dicor crowns 3. Int. J. Prosthodont. 1990;3:327–340. [PubMed] [Google Scholar]
- Edelhoff D., Sorensen J. Tooth structure removal associated with various preparation designs for anterior teeth. J. Prosthet. Dent. 2002;87:503–509. doi: 10.1067/mpr.2002.124094. [DOI] [PubMed] [Google Scholar]
- Fareed K., Solaihim A. Making a fixed restoration contour guide. J. of Prosthet. Dent. 1989;61:112–114. doi: 10.1016/0022-3913(89)90116-9. [DOI] [PubMed] [Google Scholar]
- Faunce F.R., Myer D.R. Laminate veneer restoration of permanent incisors. J. Am. Dent. Assoc. 1976;93:790–792. doi: 10.14219/jada.archive.1976.0055. [DOI] [PubMed] [Google Scholar]
- Ferrari M., Patroni S., Balleri P. Measurement of enamel thickness in relation to reduction for etched laminate veneers. Int. J. Periodontics Restor. Dent. 1992;12:407–413. [PubMed] [Google Scholar]
- Foster L.V. Failed conventional bridge work from general dental practice: clinical aspects and treatment needs of 142 cases. Br. Dent. J. 1990;168:199–201. doi: 10.1038/sj.bdj.4807133. [DOI] [PubMed] [Google Scholar]
- Fradeani M., Aquilano A. Clinical experience with Empress crowns. Int. J. Prosthodont. 1997;10:241–247. [PubMed] [Google Scholar]
- Friedman M.A. A 15-year review of porcelain failure: a clinician’s observations. Compend. Contin. Educ. Dent. 1998;19:625–628. [PubMed] [Google Scholar]
- Gardner L., Rahn A., Parr G. Using a tooth-reduction guide for modifying natural teeth. J. Prosthet. Dent. 1990;63:637–639. doi: 10.1016/0022-3913(90)90319-8. [DOI] [PubMed] [Google Scholar]
- Holm C., Tidehag P., Tillberg A., Molin M. Longevity and quality of FDPs: a retrospective study of restorations, 30, 20 and 10 years after insertion. Int. J. Prosthodont. 2003;16:283–289. [PubMed] [Google Scholar]
- Jurado C.A. Optimal tooth reduction for veneer restorations: a case report. Int. J. Prosthodont. Restor. 2019;9:99–103. [Google Scholar]
- Jurado C.A., Villalobos-Tinoco J., Tsujimoto A., Castro P., Torrealba Y. The art of minimal tooth reduction for veneer restorations. Eur. J. Gen. Dent. 2020;9:45–52. [Google Scholar]
- Lehner C., Studer S., Brodbeck U., Scharer P. Short-term results of IPS-Empress full porcelain crowns. J. Prosthodont. 1993;6:462–467. doi: 10.1111/j.1532-849x.1997.tb00061.x. [DOI] [PubMed] [Google Scholar]
- Libby G., Arcuri M.R., LaVelle W.E., Hebl L. Longevity of fixed partial dentures. J. Prosthet. Dent. 1997;78:127–131. doi: 10.1016/s0022-3913(97)70115-x. [DOI] [PubMed] [Google Scholar]
- Livaditis G. Indirectly formed matrix for multiple composite core restorations: two clinical treatments illustrating an expanded technique. J. Prosthet. Dent. 2002;88:245–251. doi: 10.1067/mpr.2002.128124. [DOI] [PubMed] [Google Scholar]
- Magne P., Douglas W. Additive contour of porcelain veneers: a key element in enamel preservation, adhesion and esthetics for aging dentition. J. Adhes. Dent. 1999;1:81–92. [PubMed] [Google Scholar]
- Manos D. Cosmetic dentistry: patients' perspectives. Gen. Dent. 1993;41:468–470. [PubMed] [Google Scholar]
- Moskowitz M., Loft G., Reynolds J. Using irreversible hydrocholloid to evaluate preparations and fabricate temporary immediate provisional restorations. J. Prosthet. Dent. 1984;51:330–333. doi: 10.1016/0022-3913(84)90215-4. [DOI] [PubMed] [Google Scholar]
- Ozturk E., Bolay S., Hickel R., IIie N. Shear bond strength of porcelain laminate veneers to enamel, dentine and enamel-dentine complex bonded with different adhesive luting systems. J. Dent. 2013;41:97–105. doi: 10.1016/j.jdent.2012.04.005. [DOI] [PubMed] [Google Scholar]
- Pincus C.R. Building mouth personality. J. South California Dent. Assoc. 1938;14:125–129. [Google Scholar]
- Pospiech P., Rammelsberg P., Unsold F. A new design for all-ceramic resin-bonded fixed partial dentures. Quintessence Int. 1996;27:753–758. [PubMed] [Google Scholar]
- Saito K., Nakatomi M., Ohshima H. Dynamics of bromodeoxyuridine label-retaining dental pulp cells during healing after cavity preparation in mice. J. Endod. 2013;39:1250–1255. doi: 10.1016/j.joen.2013.06.017. [DOI] [PubMed] [Google Scholar]
- Savi A., Crescini A., Tinti C., Manfredi M. Ultra-thin veneers without tooth preparation in extensive oligodontia. Int. J. Periodontics. Restor. Dent. 2015;35:e97–e103. doi: 10.11607/prd.2399. [DOI] [PubMed] [Google Scholar]
- Scherrer S.S., de Rijk W.G. The fracture resistance of all-ceramic crowns on supporting structures with different elastic moduli. Int. J. Prosthodont. 1993;6:462–467. [PubMed] [Google Scholar]
- Schwartz N.L., Whitsett L.D., Berry T.G., Stewart J.L. Unserviceable crowns and fixed partial dentures: life-span and causes for loss of serviceability. J. Am. Dent. Assoc. 1970;81:1395–1401. doi: 10.14219/jada.archive.1970.0398. [DOI] [PubMed] [Google Scholar]
- Sorensen J.A., Choi C., Fanuscu M.I., Mito W.T. IPS Empress crown system: three-year clinical trial results. J. Calif Dent. Assoc. 1998;26:130–136. [PubMed] [Google Scholar]
- Stanley M., Paz A.G., Miguel I., Coachman C. Fully digital workflow, integrating dental scan, smile design and CAD-CAM: case report. BMC Oral Health. 2018;18:134. doi: 10.1186/s12903-018-0597-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theobald A.H., Wong B.K., Quick A.N., Thomson W.M. The impact of the popular media on cosmetic dentistry. N. Z. Dent. J. 2006;102:58–63. [PubMed] [Google Scholar]
- Tjan A., Dunn J., Sanderson I. Microleakage patterns of porcelain and castable ceramic laminate veneers. J. Prosthet. Dent. 1989;61:276–282. doi: 10.1016/0022-3913(89)90127-3. [DOI] [PubMed] [Google Scholar]
- Wei S.H., Tang E. Laminate veneers for the aesthetic restoration of anterior teeth. Ann. R. Australas. Coll. Dent. Surg. 1989;10:148–159. [PubMed] [Google Scholar]
- Wisithphrom K., Murray P.E., About I., Windsor L.J. Interactions between cavity preparation and restoration events and their effects on pulp vitality. Int. J. Periodontics Restor. Dent. 2006;26:596–605. [PubMed] [Google Scholar]