Abstract
Purpose
The physical and mechanical performance of a newly commercialized dental restorative material (alkasite) was compared with glass ionomer cement (GIC) and nano-hybrid composite.
Methodology
Human extracted premolars were used to investigate the shear bond strength. Restorative materials were placed on the dentine surface and were aged in deionized water for 14 days. The 3-D surface roughness was evaluated before and after chewing simulation cycles (50,000). The samples were fatigued mechanically using a chewing simulator and investigated with a scanning electron microscope (SEM).
Results
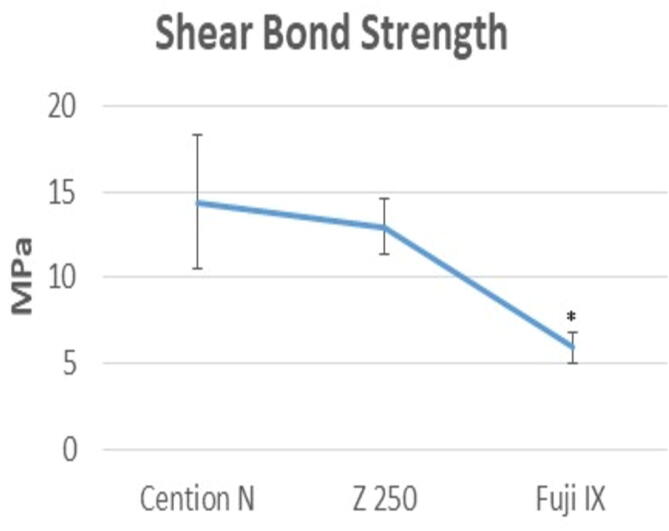
For shear bond strength, alkasite showed significantly high values than GIC, whereas non-significant difference was observed between alkasite and nano-hybrid composite. After the chewing simulation (50,000 cycles), non-significant difference was found between GIC and nano-hybrid composite, where surface roughness values were highest for GIC and lowest for alkasite.
Conclusion
The newly developed restorative material (alkasite) has shown better results than existing restorative materials.
Keywords: Cention N, Glass ionomer cement, Nano-hybrid composite, Shear bond strength, Surface roughness
1. Introduction
Due to ongoing research in the field of restorative dentistry, there is continuous advancement in the properties of aesthetic materials (Fugolin and Pfeifer, 2017). These researches led to the introduction of advanced materials, which are claimed to serve field of aesthetic dentistry in a better way (Badami and Ahuja, 2014). Dental resin-based composites are one of the most widely used restorative materials due to its relatively better mechanical and aesthetic properties (Nayyer et al., 2018). The resin-based composites are mainly composed of organic matrix and filler particles, however, various different formulations have been introduced in the market since their first introduction (Naz et al., 2015). Cention N (Ivoclar Vivadent, USA) is one of the newly introduced tooth-colored materials and is classified as an “alkasite” (Samanta et al., 2017), which has been designated as a subgroup of composite materials. However, it is capable of releasing fluoride, calcium, and hydroxyl ions, resulting in anti-cariogenic material (Ilie, 2018). As it is dual-cured, it can be used as a bulk-filling material (Chowdhury et al., 2018).
Manufacturer of Cention N has compared most of its properties with those of amalgam and glass ionomer cement (GIC). It was claimed that the compressive strength and durability were comparable to amalgam and ion-releasing was comparable to GIC. In terms of aesthetics, it is claimed to be superior to GIC because of being more translucent (Mazumdar et al., 2019). However, authors could not find any study where it was compared to other aesthetic restorative material, e.g. resin-based composite.
Dental restorative materials experience different forces in the oral cavity, especially during chewing, therefore, these materials need to withstand the effects of these forces and serve for longer periods (Tsujimoto et al., 2018). The chewing process is related to the shearing phenomenon, therefore, the interfacial strength of the materials is represented by the shear bond strength (Nujella et al., 2012). The shearing forces acting on the restorations may dislodge the material on the tooth-restorative interface. Shear bond strength measurement describes the ability of the material to withstand these shearing forces before being debonded from the tooth or undergoing adhesive or cohesive fracture (Hedge and Bhandary, 2008).
Forces within the oral cavity, like those of chewing, tooth brushing, clenching, and bruxism may also affect the surface characteristics of any restorative material (Dionysopoulos et al., 2017). The restorations must be able to maintain its surface texture and smoothness within the oral environment. There are limited in vitro studies and clinical trials on Cention N, however, no study has been done to evaluate its shear bond strength, and limited data is available regarding its surface smoothness before and after chewing simulation (Mazumdar et al., 2019, Deepak and Nivedhitha, 2017). Therefore, this study is designed to investigate and to compare the above-mentioned properties of Cention N with GIC and nano-hybrid resin-based composite. It was hypothesized that Cention N would show high strength and better resistance under fatigued environment than GIC and nano-hybrid composite.
2. Materials and methods
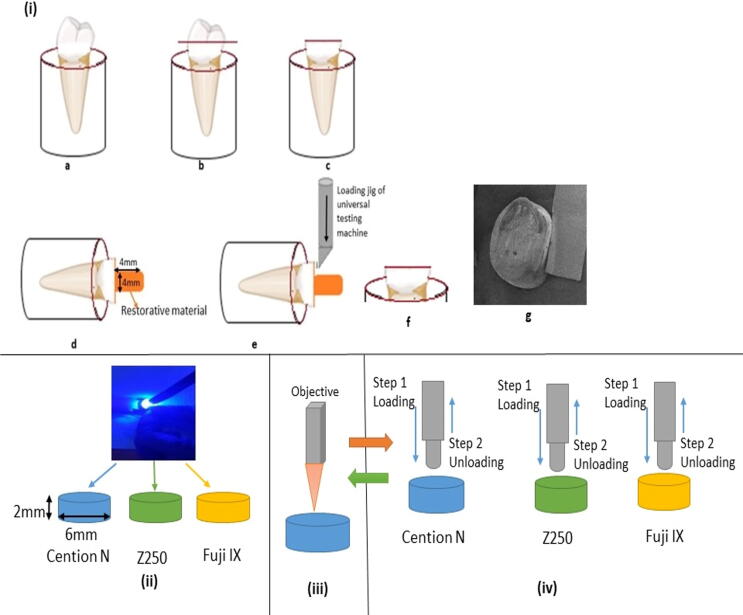
Prior to the start of the experimental procedure, ethical permission was received from the Institutional Ethical Committee. The materials used in this study are listed in Table 1 and were used as per the manufacturers’ instructions. Samples were prepared for tests of shear bond strength, surface roughness, and for chewing simulation. The schematic pattern of methodology is given in Fig. 1.
Table 1.
Description of the restorative materials used in the study.
| Materials | Type | Manufacturer |
Components (a description of abbreviations) |
|---|---|---|---|
| Cention N | Alkasite | Ivoclar Vivadent AG, Schaan, Liechtenstein | UDMA, DCP, Aromatic aliphatic-UDMA, PEG-400 DMA Barium aluminium silicate glass, Ytterbium trifluoride, Isofiller, Calcium barium aluminium fluorosilicate glass, calciumfluoro silicate glass. Particle size: 0.1–35 µm |
| Filtek Z-250 XT | Nano-hybrid composite | 3 M ESPE, Seefeld, Germany | bis-GMA, UDMA and bis-EMA, PEGDMA, TEGDMA. Additional contents: stabilizers, catalysts and pigments. Particle size 20 nm for silica and 0.1–10 µm for zirconia/silica particles and approximately 81.8 wt% filler load |
| GC Fuji IX GP Extra | Posterior Glass ionomer restorative cement | GC Corporation, Tokyo, Japan | Polyacrylic acid, aluminosilicate glass, distilled Water |
UDMA = urethane dimethacrylate, DCP = dicalcium phosphate, PEG-400 DMA = polyethylene glycol-400 dimethacrylate, bis-GMA = bisphenol glycol dimethacrylate, bis-EMA = bisphenol ethylmethacrylate, PEGDMA = polyethylene glycol dimethacrylate, TEGDMA = triethylene dimethacrylate
Fig. 1.
Schematic diagram of methodology showing (i) preparation of samples for bond strength and morphological analysis of dentine surface, (a) representative human extracted premolar, (b and c) 3 mm coronal part of tooth from occlusal surface was cut to expose the dentine structure, the dentine surface was prepared accordingly for each restorative material, (d) the restorative material (4 × 4 mm2) was placed on dentine surface through silicone mold and cured as per manufacturer’s instruction, (e) shear testing was performed with custom-made jig using Instron universal testing machine, (f and g) samples prepared for SEM analysis.
2.1. Shear bond strength analysis
2.1.1. Sample preparation
For shear bond strength analysis, a total of 30 caries-free human premolar extracted teeth were collected and were immersed in sterile saline till tested. Teeth were mounted on self-cure acrylic blocks to embed the root portion and exposed the crown portion only. Then 3 mm of the coronal tooth structure was removed using diamond burs to expose the occlusal dentine. The exposed portion of dentine was polished on grinding/polishing machine with size 600 and 2000 grit papers (MetaServ250 grinder polisher, Buehler, Esslingen, Germany) (Tani and Finger, 2002). The sample size was calculated as per World Health Organisation (WHO) specification (Lwanga et al., 1991) and the prepared teeth were distributed into three groups (n = 10);
Group 1: Cention N (Ivoclar Vivadent AG, Schaan, Liechtenstein) based samples, where surface of dentine was treated with 37% phosphoric acid for 15 s and then washed, after drying Adper™ Single Bond Plus, (3 M ESPE, Seefeld, Germany) was applied and light cured for 20 s.
Group 2: Filtek Z250 XT (nano-hybrid; 3 M ESPE, Seefeld, Germany) base samples, whereby dentine surface treatment was done as in Group 1.
Group: Fuji IX GP Extra GC Corp, Tokyo, Japan based samples and no dentine surface treatment was done.
Cylindrical silicon molds (4 × 4 mm2; diameter × height) were used to place each restoration as per manufacturer’s instruction on the occlusal surface. After placing the restorations teeth were aged in deionized water for 14 days at 37 °C. The samples were placed on a digital shaker surface using Compact Digital Mini Shaker, Thermo Scientific™ USA) to maintain the dynamic condition.
2.1.2. Experimental procedure
Instron Universal Testing Machine (Instron 8871, Norwood, MA, USA) was used to evaluate the shear bond strength, whereby the crosshead speed was 0.5 mm.min−1 and the load cell was 1KN. The mean and standard deviation values were obtained, and values were described in MPa. After the debonding procedure, the dentine surface was analysed under a Scanning Electron Microscope (SEM) (TESCAN VEGA-3 LMU, Czech Republic). Before SEM analysis, samples were gold coated under sputter for the 90 s. Images were taken at different magnifications and energy dispersive spectroscopy (EDS, Oxford Instruments, UK) were taken of each sample. Five scans were taken at different points for each sample to characterize the failure modes i.e., Type 1: adhesive failure, Type II: cohesive failure (within restoration), Type III: mixed Type 1 and II failure, and Type IV: cohesive dentine failure.
2.2. 3-D surface roughness analysis
2.2.1. Sample preparation
A total of ten specimens of each material were prepared using custom-made silicon molds (6 × 2 mm2; diameter × height). For each sample preparation, the mold was placed on clean glass slab and were filled with restorative materials from each group. The carver was used to remove the flushed-out excess material, and light-curing (SmartLite Pro, Dentsply Sirona, Bensheim, Germany) was done according to the manufacturer’s instructions for each material. The prepared samples were measured with digital Vernier Caliper (Agar Scientific Ltd, Essex, United Kingdom) to standardize the size.
2.2.2. Experimental procedure
The samples were polished using the Sof-Lex XT Finishing and Polishing Discs (coarse, medium 40 μm, fine 24 μm, and superfine 8 μm, 3 M ESPE, Germany) sequentially for 10 s with each finishing/polishing disc. Then polished samples were tested with the help of a 3D surface scanner (ContourGT-K Bruker, Tucson, AZ, USA) before and after chewing simulation. The samples were examined using a 3D optical microscope under a 50 g load for 15 s with the presence of vibration-resistant, air isolation and time-tested properties, which provided accurate results regarding repeatability and quantity.
2.3. Chewing simulation analysis
The chewing simulation test was conducted using CS-4.2 SD Mechatronik GmbH, Feldkirchen-Westerham, Germany. To simulate the chewing motion, the upper metallic antagonist (tip diameter ~2 mm) movement was set at of 2.0 mm. vertically, with a speed of 40 mm/s and load weight was corresponding to a loading force of approximately 72 N. All specimens were mounted in an acrylic mold to maintain the same place and height and samples were fatigued for a total of 50,000 cycles. After the chewing simulation, the surface images were analyzed with SEM. All samples were gold coated and images were taken at different magnifications.
2.4. Statistical analysis
Statistical analysis within three groups was done by one-way ANOVA using a post hoc Tukey’s test where a p-value of 0.05 was considered to be significant. The analysis was done using SPSS version 18 (IBM Software, NY, USA).
3. Results
3.1. Shear bond strength analysis
The results obtained for shear bond strength are given in Fig. 2. After 14 days, it was found that the mean value was highest for Cention N (14.38 ± 3.88 MPa), and lowest for Fuji IX (5.96 ± 0.91 MPa). Statistically non-significant difference (p ≥ 0.05) was observed between the Cention N and Filtek Z250 XT, whereas, Fuji IX showed significantly lower (p ≤ 0.05) values when compared individually with both Cention N and Filtek Z250 XT.
Fig. 2.
Comparative shear bond strength values (mean and standard deviation) of alkasite (Cention N) with hybrid composite (Filtek Z250 XT) and glass ionomer cement (Fuji IX), where (*) representing statistically low significant value of Fuji IX compared to other groups.
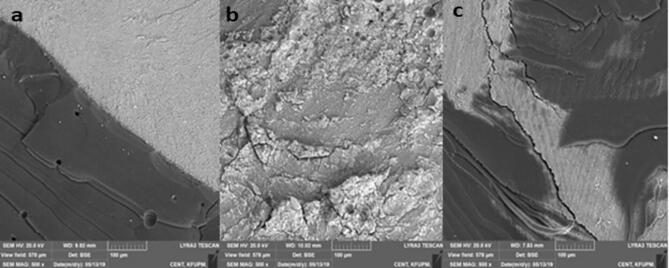
All three restorative materials showed Type III failure mode as shown in SEM images (Fig. 3a–c). Cention N showed the highest Type II failure (85%), whereas Filtek Z250 XT and Fuji IX showed 64% and 75%, respectively. The statistical difference was non-significant among the groups.
Fig. 3.
SEM images of dentine surface after debonding, the generalized behavior is a mixed failure (Type III), where the remaining surface of restorative materials observe on the dentine surface. Cention N showing more restorative material on dentine surface compared to Filtek Z350 XT and Fuji IX.
3.2. Surface roughness analysis
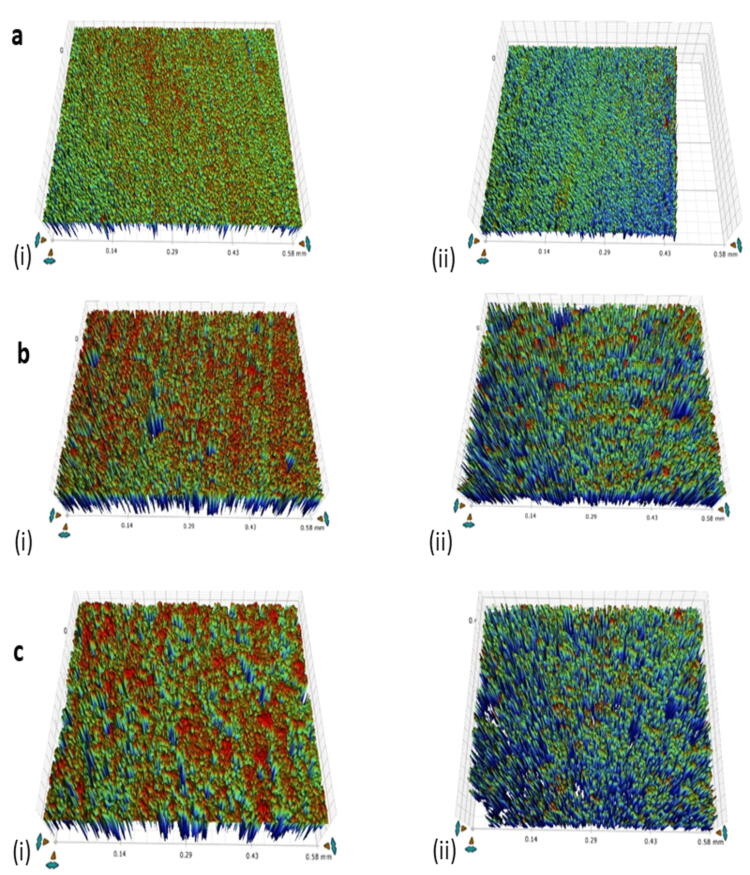
The mean surface roughness (Ra) value before chewing simulation was lowest for Filtek Z250 (260.58 ± 55.42 nm) and was highest for Fuji IX (390.35 ± 34.54 nm). Surface roughness for Filtek Z250 XT, presented in Fig. 4a (i) was significantly (p ≤ 0.05) lower compared to both Cention N (378.28 ± 85.21 nm) and Fuji IX, presented in Fig. 4b (i) and Fig. 4c (i), respectively.
Fig. 4.
The 3-D surface profile of (a) Filtek Z250 XT, (b) Cention N, and (c) Fuji IX, where the surface roughness difference observe (i) before and (ii) after chewing simulation and it shows that before simulation low Ra value for Filtek Z250 XT compare to other groups, however, after simulation, Cention N shows resistance and low Ra value.
After the chewing simulation (50,000 cycles), mean surface roughness (Ra) values were highest for Fuji IX (550.10 ± 132.39 nm) and lowest for Cention N (442.98 ± 62.45 nm), as shown in Fig. 4b (ii). The difference between the surface roughness values for Fuji IX (550.1 ± 132.39 nm) and Filtek Z250 XT (503.66 ± 134.0 nm) was not statistically significant (p ≤ 0.05).
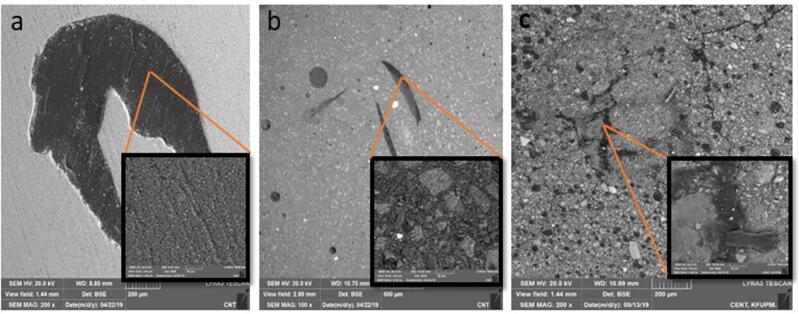
3.3. SEM images after chewing simulation
After chewing simulation, the images showed comparatively higher numbers of pits and valleys than before chewing simulation. More pits were observed in Filtek Z250 XT (Fig. 5a) and Fuji IX (Fig. 5b)) after 50,000 cycles than Cention N (Fig. 5c). Among tested restorative materials, Cention N showed a smoother surface and better resistance than other groups. More defects were found in Fuji IX and Filtek Z250 XT, indicating sites from where reinforcing agents had dislodged from the resin matrix.
Fig. 5.
SEM images show the surface texture of (a) Filtek Z250 XT, (b) Cention N, and (c) Fuji IX after chewing simulation and images in inner boxes show surface at higher magnifications. The images are showing more surface roughness with Fuji IX compared to other groups, where Cention N show the least pits and valleys. The higher magnification images in inner boxes are showing particle size variations and their uniform distribution.
4. Discussion
It is desirable for any commercial material to fulfil clinical requirements and its acceptability depends upon its performance under in vivo and in vitro conditions (Wang et al., 2003). This study showed that the newly introduced commercial restorative material, Cention N (alkasite) exhibited better performance in terms of bond strength and surface characteristics compared to other restorative materials and hypothesis was achieved. Cention N was placed with the adhesive according to manufacturer’s recommendations. According to manufacturers, material can be used with or without adhesive (George and Bhandary, 2018). The same etching and bonding protocols were used as of nano-hybrid composite material. Cention N placement was easier due to its use as a bulk filling material. It could be cured to full depth because of the highly cross-linked monomer network and shrinkage stress reliever in its formulation (Mazumdar et al., 2018).
The bond strength values of Cention N were comparable or even slightly higher than those of the composite group, which might be due to differences in composition too. The PEG-400 DMA in the liquid part of the Cention N is hydrophilic (Navarro et al., 2019) and might play a role in increased bond strength (Seker et al., 2019). Moreover, being a shrinkage stress reliever it might help to reduce shrinkage stresses on the tooth-restorative interface. Cention N is a dual-cured material in which the setting reaction starts after mixing powder and liquid, with a setting time of four minutes (Ilie N. 2018). However, as it also contains photoinitiator Ivocerin and an acyl phosphine oxide initiator, optional light curing can be done for fast curing and convenience (Kaur et al., 2019). In this study, each sample was light-cured for 15 s to hasten the setting process.
Overall, the mean bond strength value for the nano-hybrid composite was lower than those required to prevent bond disruption at the tooth-restorative interface over a long period. Though the literature includes several studies showing significantly higher bond strength values for resin-based composites (Hegde and Bhandary, 2008, Chopade et al., 2016). Various factors determine the final mean values of shear bond strength, and in this regard, no single study seems to replicate any other such study. A few of the reported factors affecting the bond strength of any restorative material are the condition of mineralized dentine, etching technique, type of adhesive and composite used, depth of dentine, moisture conditions of substrate, curing mode, and storage time after restoration (Korkmaz et al., 2010, Choi et al., 2017, Manuja et al., 2012).
In the present study, the samples were immersed for 14 days. This might be a major factor in the relatively low values of bond strength for composite restorations compared to other studies. It is reported that the bond strength of restorative materials reduces with water aging (Hoshika et al., 2015, Heikkinen et al., 2013). It is advisable to evaluate results after some time to investigate the effect of moisture on a material’s properties. The hydrolytic degradation initiates after the ingress of water molecules through the resin–filler interface and disintegrates the chemical bond, subsequently reduces the longevity and mechanical strength of the restorative material (Khalid et al., 2018). As of the date of this research, no other study evaluating the shear bond strength values for Cention N had been published. Therefore, the results of the present study could not be compared to others.
The surface properties of the materials were tested before and after fatiguing the restorations thorough mechanical load by the chewing simulator. An ideal restorative material should be resistant to all the challenges faced in the oral cavity that could lead to the wear of a material. These challenges may result in a loss of volume of material through abrasive effect, fatigue, adhesion or by chemical means (Mair et al., 1996).
Loading of the restorations was done by the chewing simulator, which is said to simulate oral loads closely (Heintze et al., 2017). Loading was done at 72 N, which is the average of loads experienced in the oral cavity (Heintze, 2006). After polishing procedures, surface roughness was minimal for Filtek Z250 XT. This smoothness seems to be the result of the type of filler particles in the composite. The average particle size of the fillers was 0.1–1.0 µm (Heintze et al., 2017). Cention N had a larger filler particle size of 0.1–35 µm (Ilie, 2018). This might be the reason for its lower surface smoothness compared to the nano-hybrid composite. Initial surface roughness values were highest for Fuji IX. These values were comparable to the other study reporting the surface roughness of different brands of GICs before and after polishing (Bala et al., 2012).
After the chewing simulation, the results were found to be different from the initial results. For all the materials, the values for surface roughness were increased from their initial values, showing the fatigue of these materials under force. These values were higher for GIC and composites than Cention N. This shows that though the filler particle size is an important factor, it is not the only factor responsible for the wear resistance of any resin-based material. Other factors, such as the type of filler particles, the formulation of the resin matrix, the degree of polymerization, the bonding character between matrix and filler phases, and the loading of the matrix by the filler, all contribute to the fatigue resistance of a restorative materials (Krithika et al., 2006). While Filtek Z250 XT showed good fatigue resistance properties because of small particle size and good matrix-filler bond and high loading of the matrix by filler. Cention N still showed better results compared to composite. These results might be due to its highly cross-linked matrix material, which has a high degree of polymerization imparting high strength and wear resistance to the material (Krithika et al., 2006). All fillers are surface modified to ensure good incorporation into the polymer matrix, resulting in good interfacial bonding between matrix and filler and resistance of fillers to be extruded out from the surface.
Aesthetically acceptable results are considered when the surface of restoration is as reflective as enamel; this happens when the surface roughness is below 1.0 µm (Northeast and Van Noort, 1988). All the three groups in the present study showed surface roughness values below the recommended value of 1.0 µm, and hence are clinically acceptable from an aesthetic viewpoint. The minimum value for surface roughness that promotes plaque accumulation has been described to be 0.2 µm. Values for all three test groups were slightly higher than this threshold value, to begin with, and after 50,000 cycles of chewing simulation, they were significantly higher. In comparison to both restorative materials, Cention N showed greater resistance to surface roughness. It is expected that this new material has the potential to be used for long periods of time in the clinical environment.
5. Conclusion
Shear bond strength values with dentine were found to be highest for alkasite (Cention N) among all three tested groups, however the difference with nano-hybrid composite was non-significant. The surface roughness of alkasite after chewing simulation was comparatively much lower than that of GIC and nano-hybrid composite and difference was non-significant. It is concluded that alkasite (Cention N) may be considered as a material of choice for posterior restorations in terms of these tested properties.
6. Ethical permission
Prior to start this experimental work, ethical permission was taken from the institutional research committee (College of Dentistry, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia).
CRediT authorship contribution statement
Fariha Naz: Conceptualization, Project administration, Supervision, Writing-original draft. Abdul Samad Khan: Conceptualization, Project administration, Supervision, Validation, Writing - review and editing. Mohammed Abdul Kader: Data Curation, Writing - review & editing. Lamis Omar Saad Al Gelban: Investigation, Methodology. Nada Mohammad Ali Mousa: Investigation, Methodology. Raghad Saeed Hader Asiri: Investigation, Methodology. Abbas Saeed Hakeem: Investigation, Resources, Validation.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Badami V., Ahuja B. Biosmart materials: breaking new ground in dentistry. Sci. World J. 2014;2014 doi: 10.1155/2014/986912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bala O., Arisu H.D., Yikilgan I., Arslan S., Gullu A. Evaluation of surface roughness and hardness of different glass ionomer cements. Eur. J. Dent. 2012;6:79. [PMC free article] [PubMed] [Google Scholar]
- Choi A.-N., Lee J.-H., Son S.-A., Jung K.-H., Kwon Y.H., Park J.-K. Effect of dentin wetness on the bond strength of universal adhesives. Materials. 2017;10:1224. doi: 10.3390/ma10111224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopade R.V., Karade P.M., Kulkarni A.P., Bade K.S., Lavate A.B., Chodankar K.V. An evaluation and comparison of shear bond strength of two adhesive systems to enamel and dentin: an in vitro study. J. Int. Oral Health. 2016;8:86. [Google Scholar]
- Chowdhury D., Guha C., Desai P. Comparative evaluation of fracture resistance of dental amalgam, Z350 composite resin and cention-N restoration in class II cavity. J. Dent. Med. Sci. 2018;17:52–56. [Google Scholar]
- Deepak S., Nivedhitha M.S. Proximal contact tightness between two different restorative materials–An in vitro study. J. Adv. Pharm. Educat. Res. 2017;7:153–156. [Google Scholar]
- Dionysopoulos D., Tolidis K., Sfeikos T., Karanasiou C., Parisi X. Evaluation of surface microhardness and abrasion resistance of two dental glass ionomer cement materials after radiant heat treatment. Adv. Mater. Sci. Eng. 2017;2017 [Google Scholar]
- Fugolin A., Pfeifer C. New resins for dental composites. J. Dent. Res. 2017;96:1085–1091. doi: 10.1177/0022034517720658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George P., Bhandary S. A comparative microleakage analysis of a newer restorative material–An ex vivo study. IOSR J. Dent. Med. Sci. 2018;17:56–60. [Google Scholar]
- Hegde M.N., Bhandary S. An evaluation and comparison of shear bond strength of composite resin to dentin, using newer dentin bonding agents. J. Conserv. Dent. 2008;11:71–75. doi: 10.4103/0972-0707.44054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heikkinen T.T., Matinlinna J.P., Vallittu P.K., Lassila L.V.J. Long term water storage deteriorates bonding of composite resin to alumina and zirconia short communication. Open Dent. J. 2013;7:123–125. doi: 10.2174/1874210601307010123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heintze S. How to qualify and validate wear simulation devices and methods. Dent. Mater. 2006;22:712–734. doi: 10.1016/j.dental.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Heintze S., Eser A., Monreal D., Rousson V. Using a chewing simulator for fatigue testing of metal ceramic crowns. J. Mech. Behav. Biomed. Mater. 2017;65:770–780. doi: 10.1016/j.jmbbm.2016.09.002. [DOI] [PubMed] [Google Scholar]
- Hoshika S., De Munck J., Sano H., Sidhu S.K., Van Meerbeek B. Effect of conditioning and aging on the bond strength and interfacial morphology of glass-ionomer cement bounded to dentin. J. Adhes. Dent. 2015;17:141–146. doi: 10.3290/j.jad.a33994. [DOI] [PubMed] [Google Scholar]
- Ilie N. Comparative effect of self- or dual-curing on polymerization kinetics and mechanical properties in a novel, dental-resin-based composite with alkaline filler. Running title: resin-composites with alkaline fillers. Materials. 2018;11:E108. doi: 10.3390/ma11010108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur M., Mann N.S., Jhamb A., Batra D. A comparative evaluation of compressive strength of Cention N with glass Ionomer cement: an in-vitro study. Int. J. Clin. Pediatr. Dent. 2019;12:47–49. [Google Scholar]
- Khalid H., Syed M.R., Rahbar M.I., Iqbal H., Ahmad S., Kaleem M., Matinlinna J.P., Khan A.S. Effect of nano-bioceramics on monomer leaching and degree of conversion of resin-based composites. Dent. Mater. J. 2018;37:940–949. doi: 10.4012/dmj.2017-338. [DOI] [PubMed] [Google Scholar]
- Korkmaz Y., Gurgan S., Firat E., Nathanson D. Shear bond strength of three different nano-restorative materials to dentin. Oper. Dent. 2010;35:50–57. doi: 10.2341/09-051-L. [DOI] [PubMed] [Google Scholar]
- Krithika A., Kandaswamy D., Sathish E.S. Wear analysis of nano ceramic composites against a ceramic antagonist. J. Conserv. Dent. 2006;9:152. [Google Scholar]
- Lwanga, S.K., Lemeshow, S., 1991. World Health O. Sample size determination in health studies: a practical manual / S. K. Lwanga and S. Lemeshow. Geneva: World Health Organization.
- Mair L., Stolarski T., Vowles R., Lloyd C. Wear: mechanisms, manifestations and measurement. Report of a workshop. J. Dent. 1996;24:141–148. doi: 10.1016/0300-5712(95)00043-7. [DOI] [PubMed] [Google Scholar]
- Manuja N., Nagpal R., Pandit I.K. Dental adhesion: mechanism, techniques and durability. J. Clin. Pediatr. Dent. 2012;36:223–234. [PubMed] [Google Scholar]
- Mazumdar P., Das A., Guha C. Comparative evaluation of hardness of different restorative materials (restorative gic, cention n, nanohybrid composite resin and silver amalgam)-an in vitro study. Int. J. Adv. Res. 2018;6:826–832. [Google Scholar]
- Mazumdar P., Das A., Das U.K. Comparative evaluation of microleakage of three different direct restorative materials (silver amalgam, glass ionomer cement, cention N), in Class II restorations using stereomicroscope: an in vitro study. Ind. J. Dent. Res. 2019;30:277. doi: 10.4103/ijdr.IJDR_481_17. [DOI] [PubMed] [Google Scholar]
- Navarro L., Minari R.J., Vaillard S.E. Photo-curable poly-(ethylene glycol)–fumarate elastomers with controlled structural composition and their evaluation as eluting systems. RSC Adv. 2019;9:482–490. doi: 10.1039/c8ra09336a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayyer M., Zahid S., Hassan S.H., Mian S.A., Mehmood S., Khan H.A., Kaleem M., Zafar M.S., Khan A.S. Comparative abrasive wear resistance and surface analysis of dental resin-based materials. Eur. J. Dent. 2018;12:57–66. doi: 10.4103/ejd.ejd_380_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naz F., Yousaf O., Chattha M.R. Preference regarding technique selection for posterior composite restorations among the dentists in Lahore. Pak. Oral Dent. J. 2015;35:500–503. [Google Scholar]
- Northeast S., Van Noort R. Surface characteristics of finished posterior composite resins. Dent. Mater. 1988;4:278–288. doi: 10.1016/s0109-5641(88)80023-x. [DOI] [PubMed] [Google Scholar]
- Nujella B.S., Choudary M.T., Reddy S.P., Kumar M.K., Gopal T. Comparison of shear bond strength of aesthetic restorative materials. Contemp. Clin. Dent. 2012;3:22. doi: 10.4103/0976-237X.94541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samanta S., Das U.K., Mitra A. Comparison of microleakage in class V cavity restored with flowable composite resin, glass ionomer cement and centionn. Imp. J. Interdiscip. Res. 2017;3:180–183. [Google Scholar]
- Seker A., Arslan B., Chen S. recovery of polyphenols from grape pomace using polyethylene glycol (peg)-grafted silica particles and peg-assisted cosolvent elution. Molecules. 2019;24:2199. doi: 10.3390/molecules24122199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tani C., Finger W.J. Effect of smear layer thickness on bond strength mediated by three all-in-one self-etching priming adhesives. J. Adhes. Dent. 2002;4:283–289. [PubMed] [Google Scholar]
- Tsujimoto A., Barkmeier W.W., Fischer N.G., Nojiri K., Nagura Y., Takamizawa T., Latta M.A., Miazaki M. Wear of resin composites: Current insights into underlying mechanisms, evaluation methods and influential factors. Jap. Dent. Sci. Rev. 2018;54:76–87. doi: 10.1016/j.jdsr.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]