Abstract
Objectives
Maxillary gingival recessions can be managed by both semilunar coronally repositioned flap (SLCRF) and coronally advanced flap (CAF). The objective of this study was to compare SLRCF and CAF in terms of wound healing and periodontal parameters in the presence of magnification.
Materials and methods
Thirty patients with Miller’s class I gingival recession in maxillary anteriors and premolars were assigned to 2 groups including SLCRF and CAF. All procedures were performed using 2.5× magnifying loupes. Wound healing and periodontal clinical parameters were assessed at baseline and at 2nd, 4th, 8th and 12th week.
Results
No significant difference was observed in wound healing and mean percentage root coverage in both the groups at 12th week (p > 0.05). However, SLCRF showed a statistically significant reduction in percentage of root coverage (PRC) at 12th week compared to 2nd week (p < 0.05). A significant gain in Clinical attachment level, width of keratinised tissue and a significant reduction in Recession Depth and Probing Depth were seen in both the groups at 12th week.
Conclusion
Within the limitation of this study, both techniques resulted in similar wound healing at 12th week with the use of magnification. CAF provided more root coverage compared to SLCRF technique in the maxillary class I gingival recession defects.
Keywords: Gingival recession, Microsurgery, Surgical flaps, Treatment outcome, Wound healing
1. Introduction
Gingival recession (GR) is defined as the apical displacement of the gingival margin to cemento-enamel junction due to periodontal disease or other anatomic factors (Loe et al., 1992). It has been reported to affect most of the adult population and also cause displeasing aesthetics, root sensitivity, root caries (Naik et al., 2016). In the management of GR, non-surgical and surgical methods including pedicle, free gingival and connective tissue grafts, and guided tissue regeneration (GTR) have been used (Tarnow, 1986) . The selection of the treatment protocol has been reported to be based on the amount of root coverage required and other factors such as donor site, recipient site and thickness of the flap and position of the teeth in the arch (Edel, 1974, Miller, 1982; Tarnow, 1986).
Pedicle flaps have been indicated in areas with the presence of adequate amount of keratinized attached gingiva close to the recession defect site (Zucchelli et al., 2004). The survival of the pedicle graft is dependent upon the vascular supply network from surrounding tissues, such as from free gingival anastomoses, periodontal ligament and underlying supra-periosteal vessels and alveolar bone (Baldi et al., 1999). Coronally advanced pedicle flap (CAF) is also one of the most widely used surgical technique indicated for the treatment of Miller’s class I and class II GR defects when there is adequate amount of attached gingiva left apical to the recession defect. CAF is a pedicle flap, simple to perform and may lead to acceptable aesthetic results (Baldi et al., 1999). Semilunar coronally repositioned flap (SLCRF) technique is also a widely preferred protocol used in the areas with minimal labial probing depth (PD) and adequate band of keratinized gingiva. It is described as simple, fast, tensionless and a suture-less flap that does not involve the adjacent papillae, does not shorten the vestibule and results in a seamless color blend with adjacent tissues (Tarnow, 1986).
The use of magnification in dental practice including in periodontology specialty has gained popularity in last few years (Kang et al., 2015). The periodontal surgical approach with magnification allows an atraumatic approach, improves dexterity of the operator, improves the visual acuity, ergonomic benefits, decreased patient morbidity, predictability, rapid healing and improved patient satisfaction (Yadav et al., 2018). Therefore, the aim of the current study was to compare SLCRF and CAF on wound healing, periodontal clinical parameters and postoperative outcomes in the presence of loupe magnification in the treatment of maxillary Miller’s class I recession defects.
2. Materials and methods
This study was designed as a prospective, single blinded, randomised controlled clinical study, carried out in Department of Periodontics, SRM Dental College, Ramapuram, Chennai, India. This study was approved by Institutional review board and Ethical committee, before we started recruiting patients and all patients were given adequate information about the procedure, benefits and risks associated with the procedure and encouraged patients to ask questions. (Ethical committee clearance number: SRMU/M&HS/SRMDC/2012/MDS-PGSTUDENT/503). Following to which if patients agreed to participate in the study, they signed an appropriate consent form in agreement with the Helsinki Declaration on human experimentation.
2.1. Inclusion criteria
Inclusion criteria for all groups were the presence of Miller’s class I gingival recessions (Miller, 1985) (≥2mm) in maxillary anteriors or premolars, probing depth < 3 mm without bleeding on probing, width of keratinized tissue ≥ 2 mm, thick gingival biotype, absence of caries or restorations in the areas to be treated, patient’s primary concern of root sensitivity or aesthetics, full mouth plaque score ≤ 20%.
2.2. Exclusion criteria
Patients with active untreated periodontal disease, smoking habits, immuno-suppressive diseases, bleeding disorders, lack of compliance and cervical defects were excluded.
2.3. Presurgical evaluation and group design
All clinical parameters were carried out by one calibrated examiner. The follow up appointments were blinded to the clinician and the clinician did not know the type of surgical design patient had underwent. Clinical parameters were measured using UNC (University of North Carolina)-15 probe and with the aid of magnification 2.5X (Stac Loupes, Canada) to achieve the precision. The score was rounded off to a nearest millimetre (Hu-Friedy, Frankfurt, Germany). Probing depth (PD) was measured from the gingival margin to the base of the sulcus, CAL was measured from cemento-enamel junction (CEJ) to the base of the pocket and recession depth (RD) was measured from the identifiable CEJ to the gingival margin on the mid-buccal aspect of the tooth. WKT was measured from gingival margin to muco-gingival junction (MGJ). Percentage of root coverage was calculated using the following formula given by Borghetti and Louise in 1994 (Borghetti and Louise, 1994). Following clinical parameters, were assessed at base line and at follow up appointments 4th, 8th and 12th week; clinical attachment level (CAL), Probing Depth (PD). Apico-coronal width of keratinized tissue (WKT), Percentage of root coverage (PRC), Wound healing index (WHI) was assessed at 2nd, 4th, 8th and 12th week. WHI was recorded using the following scale: score 1 = uneventful healing with no gingival edema, erythema, suppuration, patient discomfort, or flap dehiscence; score 2 = uneventful healing with slight gingival edema, redness, patient discomfort, or flap dehiscence, without suppuration; and score 3 = poor wound healing with significant gingival edema, redness, patient discomfort, flap dehiscence, or with suppuration (Huang et al, 2005a, Huang LH et al, 2005b). Recession depth was assessed at baseline, 2nd, 4th, 8th and 12th week. Percentage of root coverage was calculated as follows: Recession at baseline − Recession at follow up × 100/Recession at baseline.
All patients underwent phase 1 therapy, such as stabilising active caries and periodontal disease, including root surface debridement (as indicated) polishing, removal of plaque retentive factors, tailored oral hygiene instructions, modification of tooth brushing technique as necessary. Following phase 1 therapy, patients were reviewed at 3 months and bleeding and plaque scores were assessed. Patients who demonstrated a total plaque score of less than 20% and appropriate atraumatic brushing technique, were recruited for the study. Patients were randomly assigned to one of the treatment groups: Group 1- SLCRF and Group 2 – CAF. Randomisation was done by computer generated random number list was prepared by another co-ordinator who was not involved in the study.
2.4. Surgical procedures
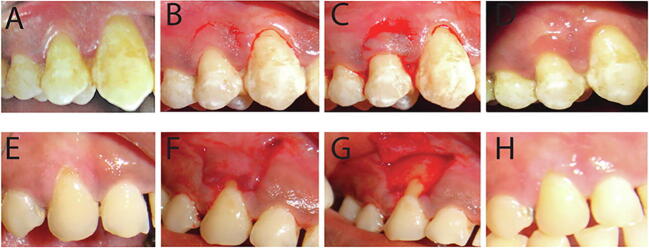
All surgical Procedure was performed by one calibrated clinician. The recession site was anesthetised using 2% lignocaine with adrenaline at a concentration of 1:80000, through infiltration technique. The SLCRF procedure was performed as described by Tarnow DP 1986. (3) Exposed root surfaces were prepared and conditioned and a semilunar incision was placed following the outline of the gingival margin and the incision ended into each adjacent interdental papilla without going all the way up to the tip of the papilla. To ensure adequate blood supply to the flap minimum 2 mm of gingiva was left intact. The height of the semilunar flap was greater than the distance between the CEJ and the bone, so that the apical border of the flap rested onto the bone not on the exposed root surface. Further an intrasulcular incision was initiated at mid buccal site and then a split thickness flap continued to release the flap to make it collapse coronally onto the exposed root surface (Fig. 1A,B,C,D). The flap was then held firmly onto the root surface using a moist gauze with mild pressure for about 5 min and evaluated for its stability. No sutures were placed following the coronal movement of the flap. A periodontal pack (Coe-pak) was placed and reviewed at a week and then again at 15 days.
Fig. 1.
A to D – SLCRF: Preoperative view (A), Semilunar incision (B), Semilunar flap in position (C), Post-operative view (D); E to H- CAF: preoperative view (E), Vertical and horizontal incision of CAF (F), Elevation of the flap (G), Post-operative view (H).
The CAF procedure was performed as described several authors (Baldi et al., 1999). Following a thorough debridement, two horizontal incisions placed into mesial and distal to the recession site. The site of this incision was at a distance from the tip of the papilla to the amount of recession plus one millimetre. Two divergent vertical incisions were placed from the end of the horizontal incision extending into the alveolar mucosa avoiding a butt joint between the flap and the adjacent tissues. The vertical incisions were joined by the intra-sulcular incisions. The resulting flap was elevated as split-full-split thickness flap, corono- apically. The flap was them mobilised coronally so that the marginal flap was able to sit passively coronal to the CEJ of the tooth with the recession site, without any tension (Fig. 1E,F,G,H). The root was then thoroughly debrided and conditioned. The interdental papillae, coronal to the horizontal incision, was then de-epithelialised to create connective tissue beds ready to receive the under surface of the surgical papillae of CAF, to which they were sutured. The suture material used was 5-0, 11 mm Ethicon Vicryl Rapide Suture, Braided, Undyed, 3/8 Circle Reverse Cutting, 45 cm. A surgical dressing (Coe Pak, GC AMERIC INC) was changed after 7 days and removed after 14 days and sutures were removed at this stage.
2.5. Post-operative evaluation
Patient’s were given systemic analgesics as appropriate and were advised to continue their home care except in the surgical area. They were prescribed 0.2% chlorhexidine gluconate mouthrinses twice daily at a different time from tooth brushing to achieve the maximum benefit of dentifrices. Patients recommenced mechanical cleaning, 3 weeks later with a soft tooth brush with roll technique at the surgical site. Patients were reviewed at 2nd, 4th, 8th and 12th week.
2.6. Sample size determination
The sample size was determined based on the results of the study by (Santana et al., 2010) where the data on comparison on clinical outcome of CAF and SLCRF was obtained. Power analysis was performed assuming α = 0.05. The estimated effect size was 1.36 and to achieve 90% power, the required sample size was a total of 26 patients with 13 patients in each group. To compensate for 10% dropouts, a total of 30 patients with 15 in each group were recruited.
2.7. Statistical analysis
Statistical analysis was performed using the IBM SPSS Statistics for windows, Version 22.0, (IBM Corp., Armonk, NY). Normality tests, Kolmogrov-Smirnov and Shapiro-Wilk tests were used to assess the distribution of variables and results indicated that, all variables do not follow the normal distribution. Hence non-parametric tests were employed to analyse the data. Descriptive statistics were presented as mean ± standard deviation. Mann-Whitney test was applied to compare between the groups. For intra-group comparisons, i.e., between two-time points, Wilcoxon Signed Rank test was employed. To compare proportions between groups Chi-Square test was applied. Statistical significance was set at the 95% probability level (P < 0.05).
3. Results
All patients completed the study and were followed up until 12th week. The recession sites were in 4 maxillary second premolars, 12 maxillary first premolars, 11 maxillary canines, 2 maxillary lateral incisors and 1 maxillary central incisor. Healing was uneventful for all 30 patients during the follow up. In group 1 (SLCRF) 15 patients were recruited (12 males and 3 females). Semilunar coronally repositioned flap (SLCRF) procedure was done on 4 maxillary second premolars, 6 maxillary first premolars, 2 maxillary canines, 2 maxillary lateral incisor and 1 maxillary central incisor. Coronally advanced pedicle flap was performed in 15 patients were recruited (9 males and 6 females). CAF was done on 6 maxillary first premolars and 9 maxillary canines. Descriptive statistics of both groups are presented in Table 1.
Table 1.
Descriptive statistics of clinical parameters (mean ± Standard deviation) of both groups (Group 1 – SLCRF; Group 2 – CAF).
| Variables | Baseline | 2 weeks | 4 weeks | 8 weeks | 12 weeks | |
|---|---|---|---|---|---|---|
| PRC% | Group 1 | – | 100 ± 0 | 100 ± 0 | 83.5 ± 30.6 | 76.9 ± 31.8 |
| Group 2 | – | 98.4 ± 6.2 | 98.4 ± 6.2 | 91.5 ± 16.2 | 91.5 ± 16.2 | |
| CAL (mm) | Group 1 | 3.19 ± 0.66 | – | 0.0 ± 0 | 0.37 ± 0.90 | 0.59 ± 1.12 |
| Group 2 | 3.68 ± 1.02 | – | 0.15 ± 0.59 | 0.37 ± 0.86 | 0.37 ± 0.86 | |
| WHI | Group 1 | – | 1.87 ± 0.52 | 1.13 ± 0.35 | 1.0 ± 0 | 1.0 ± 0 |
| Group 2 | – | 1.67 ± 0.49 | 1.0 ± 0 | 1.0 ± 0 | 1.0 ± 0 | |
| RD | Group 1 | 1.66 ± 0.46 | 0.0 ± 0 | 0.0 ± 0 | 0.24 ± 0.42 | 0.37 ± 0.48 |
| Group 2 | 1.92 ± 0.61 | 0.15 ± 0.35 | 0.15 ± 0.35 | 0.28 ± 0.41 | 0.28 ± 0.41 | |
| PD | Group 1 | 1.65 ± 0.45 | – | 1.12 ± 0.25 | 1.23 ± 0.35 | 1.37 ± 0.38 |
| Group 2 | 2.00 ± 0.54 | – | 1.17 ± 0.32 | 1.17 ± 0.32 | 1.29 ± 0.34 | |
| WKT | Group 1 | 4.12 ± 0.34 | – | 4.68 ± 0.58 | 4.65 ± 0.63 | 4.65 ± 0.63 |
| Group 2 | 3.89 ± 0.85 | – | 4.46 ± 0.69 | 4.46 ± 0.69 | 4.41 ± 0.75 |
PRC – Percentage of root coverage.
CAL – Clinical attachment loss.
WHI – Wound Healing index.
RD – Recession depth.
PD – Probing depth.
WKT – Width of Keratinised tissue.
Patients were instructed to keep up with the oral hygiene to an optimum level. When comparing the healing patterns of the study groups, SLCRF sites healed in a distinct pattern compared to CAF. SLCRF left very little elevated wound edges scar at the semilunar incision site at 12th week evaluation. CAF healing progressed initially well with distinguishable vertical incisions; however, the gingival colour, contour and texture of the healed tissues were similar to the adjacent tissues at 12th week evaluation.
Clinical periodontal parameters were compared in two study groups. Intragroup comparison between the pre and post-surgical measurements at different time intervals of SLCRF (group 1) showed a statistically significant difference from baseline to 12th week in all clinical parameters. While in group 2 there was a statistically significant difference between baseline to 12th week in all clinical parameters except in percentage of root coverage (PRC) (Table 2).
Table 2.
Intra group comparison of clinical parameters from baseline to 12th week of group I (SLCRF) and group II (CAF).
| Variables | P-value |
|||
|---|---|---|---|---|
| 2 weeks | 4 weeks | 8 weeks | 12 weeks | |
| PRC – GI | – | 0.999 | 0.066 | 0.024* |
| GII | – | 0.999 | 0.109 | 0.109 |
| CAL – GI | – | 0.001* | 0.001* | 0.001* |
| GII | – | 0.001* | 0.001* | 0.001* |
| WHI – GI | – | 0.001* | 0.001* | 0.001* |
| GII | – | 0.002* | 0.002* | 0.002* |
| RD - GI | <0.001* | <0.001* | 0.001* | 0.001* |
| GII | 0.001* | 0.001* | 0.001* | 0.001* |
| PD - GI | – | 0.004* | 0.007* | 0.049* |
| GII | – | 0.002* | 0.002* | 0.007* |
| WKT - GI | – | 0.007* | 0.008* | 0.008* |
| GII | – | 0.018* | 0.018* | 0.018* |
p < 0.05.
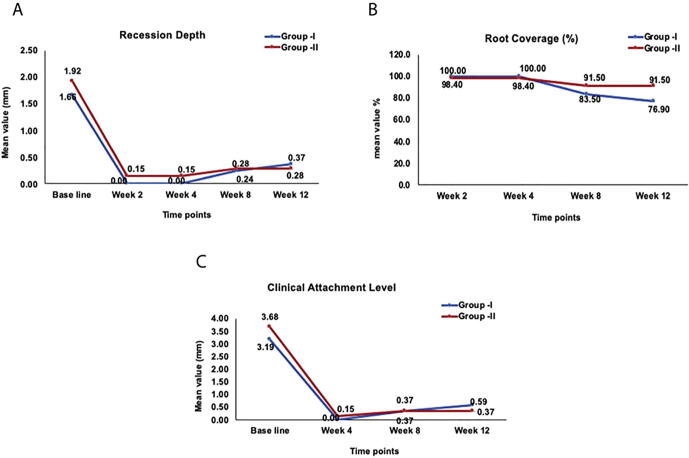
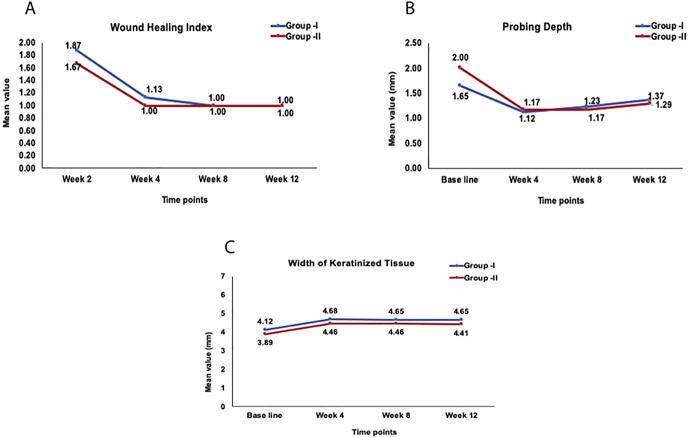
Frequency of root coverage of group I and group II are depicted in Table 3. On comparison of group I and group II there was no difference observed between in any clinical parameters and at any time intervals. (Linear graphs Fig. 2, Fig. 3).
Table 3.
Frequency of Recession Coverage with Group I (SLCRF) and Group II (CAF).
| Group | 100% | 99–75% | 74–50% | 49–0% |
|---|---|---|---|---|
| I | 9 | 0 | 5 | 1 |
| II | 11 | 2 | 2 | 0 |
Fig. 2.
Linear graph depicting Recession depth (RD), (A), Percentage root coverage (PRC) (B), and clinical attachment level (CAL) (C), at baseline, 4, 8 and 12 weeks for group 1 and 2.
Fig. 3.
Linear graph depicting wound healing index (WHI), (A), Probing Depth (PD) (B), and width of keratinised tissue (WKT) (C), at baseline, 4, 8 and 12 weeks for group 1 and 2.
4. Discussion
The present controlled clinical study compared two flap design in the management of Miller’s class 1 gingival recession defects in the maxillary aesthetic zones. The results indicated that both flap designs were successful in obtaining the root coverage. However, the coronally advanced pedicle flap showed a better clinical outcome in percentage of root coverage, recession depth, clinical attachment loss and probing depth (Fig. 3).
The current study evaluated various periodontal clinical parameters such as percentage of root coverage (PRC), clinical attachment loss (CAL), wound healing index (WHI), recession depth (RD), probing depth and WKT for 12 week post operation period. CAL, PD & WKT were recorded at baseline, 4th week, 8th week and 12th week post surgically to prevent any trauma and disturbance during healing. PRC and WHI were recorded at 2nd, 4th, 8th and 12th week post surgically. RD was measured at baseline and at all time intervals.
In this study, 100% percentage of root coverage was seen in 9 out of 15 in SLCRF group and 11 out of 15 in CAF group. In CAF group the mean PRC obtained at 2 weeks was 98.4% and at 8th week, it was reduced to 91.5%. This was maintained constant till the 12th week which was statistically not significant (p = 0.109). In contrast, SLCRF showed a progressive change in the obtained 100% at 2nd week to 83.5% at 8th week with a p value of 0.066 and further reduced to 76.9% at 12 weeks with p value of 0.024. This reduction in SLCRF was statistically significant when compared to baseline, which was not significant in CAF group. When the two groups were compared, there was a greater PRC observed in group II (CAF) than group I (SLCRF) at 12th week, though not statistically significant.
In SLCRF design, the wound contraction occurs at the base of the flap, which may pull the flap margin apically. Additionally, no sutures or adhesives were used to stabilize the pedicle, and thus there was no antagonistic force to counteract the apical retraction (Petroll et al., 1998). Few reports suggested modification of SLCRF by introducing the sutures for better flap stabilisation and control of mobilised flap in the desired position, to achieve reduction in the likelihood of apical tissue retraction (Haghighat, 2006). Thus, the usage of sutures (Marggraf, 1985, Romanos et al., 1993) or adhesives (Bittencourt et al., 2006, Bittencourt et al., 2007) may have resulted in superior root coverage as reported in previous studies, compared to the current study.
A part of defence mechanism is healing response to re-establish the integrity of the tissue. Several local and systemic factors can influence wound healing. Dehiscence at the wound margins is a key complication following surgery, which can disrupt the early phases of wound healing. In periodontal surgeries initial wound stability is critical for the success of the graft. Several previous studies have reported considerable superior clinical outcomes in root coverage procedures by using microsurgical approach (Burkhardt and Lang, 2005). All the procedures in this study were performed using magnification (Shanelec et al., 2003)
With respect to WHI, there was no statistically significant difference between the groups. This could be attributed to the use of microsurgical instruments and magnifying loupes for all the procedures, which reduces tissues trauma and improves vascularization (Burkhardt and Lang, 2005). In contrast, other reports suggested a significantly delayed reddish, healing phase, followed by a noticeable semilunar white scar located just a few millimetres apical to the CEJ in SLCRF macrosurgical procedures (Santana et al., 2010).
Additionally, there was a significant difference in WHI from 2 weeks to 4 weeks, 8 weeks and 12 weeks. The WHI was stable from 4th week in both the groups. This could be attributed to the completion of epithelial healing with layers by 21–28 days and connective tissue healing including its vasculature which continues to mature for 35–42 days (Gonzales et al., 2004).
The treatment outcome may be influenced by patient, technique and defect specific factors. Few patient factors such as age, genetic predisposition towards expression of growth factors, may influence the wound healing. One study suggested that patients older than 70 years have significantly lower rates of successful wound healing than younger patients (Coerper et al., 2004). However, current study, recruited subjects belonged to age range of 19–50 years. Nevertheless, it is difficult to ascertain each patient’s wound healing capacity. Furthermore, many studies in the past have used platelet rich plasma or enamel matrix derivative to enhance wound healing outcome and have reported conflicting results (Okuda et al., 2001, Huang et al, 2005a, Huang LH et al, 2005b).
In both the groups there was a statistically significant gain in CAL at 4 weeks with a p value of 0.001 which was maintained till 12 weeks. This is in accordance with the study conducted by Santana et al., 2010. In the present study, the inter group comparison did not show any significant difference in the gain in CAL.
In group II (CAF), there was a statistically significant reduction in RD from baseline to 2 weeks, further RD stability was noted from 8th weeks, which was constant till the 12th week. Whereas in SLCRF, a statistically significant progressive increase in RD was observed from 2nd to 12th week. This could be due to secondary intention of healing at the base of the flap causing the retraction and scarring of the tissue apically. Furthermore, current study did not measure recession width, perhaps that parameter would have provided us with good insight into the current results.
In both the groups, there was a statistically significant difference in terms of PD when compared to baseline. In SLCRF a statistically significant reduction in PD from baseline to 4 weeks was seen. Which increased in 8th week and 12th week. In CAF also, a significant reduction of PD from baseline to 4 weeks with was observed, which was constant till 8 weeks and additionally increased at 12th week. These findings are in contrary to the results of the study conducted by (Santana et al., 2010, Bittencourt et al., 2006) There are several local and systemic factors which influence wound healing including wound healing and host response. In the current study we did aim to maintain patient’s plaque score < 20% and we were satisfied with compliance of the patients. However, there is a possibility of some patient’s brushing habits were ineffective when they were brushing without supervision at home.
In both the groups, there was a statistically significant difference in terms of WKT when compared to baseline. In SLCRF there was a statistically significant gain in WKT from baseline to 4th week. Which reduced in 8th week and remained stable till 12th week. In CAF there was significant gain in WKT from baseline to 4th week, which was constant till 8th week. Additionally, it was significantly reduced in the 12th week. These findings are in accordance with few studies (Bittencourt et al., 2006, Pini-Prato et al., 1999). In the SLCRF the granulation tissue that fills the semilunar area will generally turn into the same type of tissue that was present before the repositioning. The increase in the width of keratinized tissue is due to the tendency of the coronally displaced mucogingival line, to regain its original, “genetically determined” position, after the soft tissue margin attains stability at the level of the cementoenamel junction (Gürgan et al., 2004).
In the present study, there was no creeping attachment noticed in any of the cases, which occurs as a consequence of tissue maturation during a period of about 1-year post treatment. This could be because, the time period of follow up for the current study was only 12 weeks and this we acknowledge this as a limitation along with not recording the recession width at baseline and patient’s perception post operatively about aesthetics and sensitivity. This study was a parallel group study rather than split mouth design, however recruiting patients for split mouth design would not have been completed in the time frame set for this study, However, this study provides additional data and insight into effectiveness of these procedures in a different population than what has been reported in the past. Finally, current study has strengths of using a blind assessor, use of magnification and microsurgical instruments and a trained single operator.
5. Conclusion
Within the limitation of this study, both techniques resulted in similar wound healing at 12th week with the use of magnification. Further studies including long term follow up should be needed to verify our results.
5.1. Clinical significance
In the literature several studies have reported the clinical outcome between the SLCRF and CAF techniques employed in the management of Miller’s class I maxillary gingival recessions, however this study reports the wound healing outcome as well as clinical attachment level (CAL), Probing Depth (PD). Apico-coronal width of keratinized tissue (WKT), Percentage of root coverage (PRC), Wound healing index (WHI) and Recession depth (RD). This study adds further evidence to the existing literature.
Ethical committee clearance number
This study was approved by Institutional Review board, SRM Dental College, Ramapuram campus, Bharathi Salai, Chennai, 600089, India. Ethical committee clearance number was obtained. Following is the Ethical committee clearance number: (Ethical committee clearance number: SRMU/M&HS/SRMDC/2012/MDS-PGSTUDENT/503).
Funding
N/A self-funded, supported by Department of Periodontics, SRM Dental College, Ramapuram, Chennai, 600089, India.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Baldi C., Pini-Prato G., Pagliaro U., Nieri M., Saletta D., Muzzi L. Coronally advanced flap procedure for root coverage. is flap thickness a relevant predictor to achieve root coverage? A 19-case series. J. Periodontol. 1999;70(9):1077–1084. doi: 10.1902/jop.1999.70.9.1077. [DOI] [PubMed] [Google Scholar]
- Bittencourt S., Del Peloso Ribeiro E., Sallum E.A., Sallum A.W., Nociti F.H., Jr., Casati M.Z. Comparative 6-month clinical study of a semilunar coronally positioned flap and subepithelial connective tissue graft for the treatment of gingival recession. J. Periodontol. 2006;77(2):174–181. doi: 10.1902/jop.2006.050114. [DOI] [PubMed] [Google Scholar]
- Bittencourt S., Ribeiro Edel P., Sallum E.A., Sallum A.W., Nociti F.H., Jr., Casati M.Z. Root surface biomodification with EDTA for the treatment of gingival recession with a semilunar coronally repositioned flap. J. Periodontol. 2007;78(9):1695–1701. doi: 10.1902/jop.2007.060507. [DOI] [PubMed] [Google Scholar]
- Borghetti A., Louise F. Controlled clinical evaluation of the subpedicle connective tissue graft for the coverage of gingival recession. J. Periodontol. 1994;65(12):1107–1112. doi: 10.1902/jop.1994.65.12.1107. [DOI] [PubMed] [Google Scholar]
- Burkhardt R., Lang N.P. Coverage of localized gingival recessions: Comparison of micro-and macrosurgical techniques. J. Clin. Periodontol. 2005;32(3):287–293. doi: 10.1111/j.1600-051X.2005.00660.x. [DOI] [PubMed] [Google Scholar]
- Coerper S., Wicke C., Pfeffer F., Köveker G., Becker H.D. Documentation of 7051 chronic wounds using a new computerized system within a network of wound care centers. Arch. Surg. 2004;139(3):251–258. doi: 10.1001/archsurg.139.3.251. [DOI] [PubMed] [Google Scholar]
- Edel A. Clinical evaluation of free connective tissue grafts used to increase the width of keratinized gingiva. J. Clin. Periodontol. 1974;1:185–196. doi: 10.1111/j.1600-051x.1974.tb01257.x. [DOI] [PubMed] [Google Scholar]
- Gonzales J.R., Klimek J., Meyle J. Aesthetic periodontal plastic surgery-a case report. Perio. 2004;3(1):263–276. [Google Scholar]
- Gürgan, C.A., Murat Oruç, A., Akkaya, Murat, 2004. Alterations in location of the mucogingival junction 5 years after coronally repositioned flap surgery. J. Periodontal. 75(6), 893-901. [DOI] [PubMed]
- Haghighat K. Modified semilunar coronally advanced flap. J. Periodontol. 2006;77(7):1274–1279. doi: 10.1902/jop.2006.050426. [DOI] [PubMed] [Google Scholar]
- Huang L.H., Neiva R.E., Wang H.L. Factors affecting the outcomes of coronally advanced flap root coverage procedure. J. Periodontol. 2005;76(10):1729–1734. doi: 10.1902/jop.2005.76.10.1729. [DOI] [PubMed] [Google Scholar]
- Huang L.H., Neiva R.E., Soehren S.E., Giannobile W.V., Wang H.L. The effect of platelet-rich plasma on the coronally advanced flap root coverage procedure: a pilot human trial. J. Periodontol. 2005;76(10):1768–1777. doi: 10.1902/jop.2005.76.10.1768. [DOI] [PubMed] [Google Scholar]
- Kang J., Meng S., Li C., Luo Z., Guo S., Wu Y. Microsurgery for root coverage: A systematic review. Pakistan J. Med. Sci. 2015;31(5):1263–1268. doi: 10.12669/pjms.315.7782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löe H., Anerud A., Boysen H. The natural history of periodontal disease in man: Prevalence, severity, and extent of gingival recession. J. Periodontol. 1992;63:489–495. doi: 10.1902/jop.1992.63.6.489. [DOI] [PubMed] [Google Scholar]
- Marggraf E. A direct technique with a double lateral bridging flap for coverage of denuded root surface and gingiva extension. J. Clin. Periodontol. 1985;12(1):69–76. doi: 10.1111/j.1600-051x.1985.tb01355.x. [DOI] [PubMed] [Google Scholar]
- Miller P.D., Jr. Root coverage using a free soft tissue autograft following citric acid application. I. Technique. Int. J. Periodontics Restorative Dent. 1982;2(1):65–67. [PubMed] [Google Scholar]
- Miller P.D., Jr. A classification of marginal tissue recession. Int. J. Periodontics Restorative Dent. 1985;5(2):8–13. [PubMed] [Google Scholar]
- Naik V.-K., Jacob C.-A., Nainar D.-A. Assessment of non-carious root surface defects in areas of gingival recession: A descriptive study. J. Clin. Exp. Dent. 2016;18(4):e397–e402. doi: 10.4317/jced.52831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuda K., Miyazaki A., Momose M., Murata M., Nomura T., Kubota T., Wolff L.F., Yoshie H. Levels of tissue inhibitor of metalloproteinases-1 and matrix metalloproteinases-1 and -8 in gingival crevicular fluid following treatment with enamel matrix derivative (EMDOGAIN) J. Periodontal Res. 2001;36(5):309–316. doi: 10.1034/j.1600-0765.2001.360506.x. [DOI] [PubMed] [Google Scholar]
- Petroll W.M., Cavanagh H.D., Jester J.V. Assessment of stress fiber orientation during healing of radial keratotomy wounds using confocal microscopy. Scanning. 1998;20(2):74–82. doi: 10.1002/sca.1998.4950200202. [DOI] [PubMed] [Google Scholar]
- Pini-Prato G., Baldi C., Pagliaro U., Nieri M., Saletta D., Rotundo R., Cortellini P. Coronally advanced flap procedure for root coverage. Treatment of root surface: Root planing versus polishing. J. Periodontol. 1999;70(9):1064–1076. doi: 10.1902/jop.1999.70.9.1064. [DOI] [PubMed] [Google Scholar]
- Romanos G.E., Bernimoulin J.-P., Marggraf E. The double lateral bridging flap for coverage of denuded root surface: longitudinal study and clinical evaluation after 5 to 8 years. J. Periodontal. 1993;64(8):683–688. doi: 10.1902/jop.1993.64.8.683. [DOI] [PubMed] [Google Scholar]
- Santana R.B., Mattos C.M.L., Dibart S. A clinical comparison of two flap designs for coronal advancement of the gingival margin: Semilunar versus coronally advanced flap. J. Clin. Periodontol. 2010;37(7):651–658. doi: 10.1111/j.1600-051X.2010.01582.x. [DOI] [PubMed] [Google Scholar]
- Shanelec Dennis A., Tibbetts Ô.S. Periodontal microsurgery. J. Esthet Restor. Dent. 2003;15(7):402–407. doi: 10.1111/j.1708-8240.2003.tb00965.x. [DOI] [PubMed] [Google Scholar]
- Tarnow D.P. Semilunar coronally repositioned flap. J. Clin. Periodontol. 1986;13:182–185. doi: 10.1111/j.1600-051x.1986.tb01456.x. [DOI] [PubMed] [Google Scholar]
- Yadav V.S., Salaria S.K., Bhatia A., Yadav R. Periodontal microsurgery: Reaching new heights of precision. J. Indian Soc. Periodontol. 2018;22(1):5–11. doi: 10.4103/jisp.jisp_364_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucchelli G., Cesari C., Amore C., Montebugnoli L., De Sanctis M. Laterally moved, coronally advanced flap: a modified surgical approach for isolated recession-type defects. J. Periodontol. 2004;75(12):1734–1741. doi: 10.1902/jop.2004.75.12.1734. [DOI] [PubMed] [Google Scholar]