Abstract
Background
Occlusal appliances can distribute aggressive loads which are generated by bruxism and can reduce their frequency. The facebow record, when used in the construction of occlusal appliances, helps in minimizing occlusal discrepancies. This study aimed to compare the effect of CAD/CAM stabilization occlusal splint made with and without facebow for management of bruxer patients.
Method
24 Patients who were diagnosed as bruxers were randomly assigned into two equal groups and obtained maxillary CAD/CAM occlusal stabilizing splint recorded with centric relation either with or without using a facebow. The patient satisfaction using the visual analog scale (VAS) was recorded at baseline, one month and three months’ follow-up periods. The adjustment time of both splints, from the start of splint delivery until becoming well-fitted and occlusally adjusted, was calculated using a stopwatch.
Results
The CAD/CAM occlusal splints with or without the use of facebow improved the patient's satisfaction with no statistically significant difference between both groups at baseline, one month and three months with p values of 0.73, 0.24 and 0.45 respectively. The comparison between the two modalities regarding the adjustment time showed no statistically significant difference between both groups (P = 0.06).
Conclusion
According to the results of this study; no difference was detected in patient satisfaction and the time required for adjustment of CAD/CAM occlus.
Keywords: Facebow, Bruxism, Occlusal splint, CAD/CAM
1. Introduction
An occlusal stabilization splint is defined as a removable appliance, covering the occluding surfaces of teeth in one jaw, usually made of acrylic material, generating accurate teeth occlusal contacts with the opposing jaw (Klasser and Greene, 2009, Deshpande and Mhatre, 2010). Based on The Academy of Prosthodontics (2005) a dental occlusal splint is described as “a removable artificial occlusal surface used for diagnosis or therapy affecting the relationship of the mandible to the maxillae. It may be used for occlusal stabilization, treatment of TMJ disorders, or to prevent wear of the dentition”.
Occlusal splints aim to prevent the maximal intercuspal position when the patient tries to close by forcing the mandible to move in a different position, consequently developing a new muscular and articular equilibrium. Therefore, the patient will not clench the teeth anymore and protect his TMJ and teeth and thus relieve temporomandibular pain as well as bruxism and restore the function (Srivastava et al., 2013, Manfredini et al., 2015).
“Bruxism is a repetitive jaw-muscle activity characterized by clenching or grinding of the teeth and/or by bracing or thrusting of the mandible. Bruxism has two distinct circadian manifestations: it can occur during sleep (indicated as sleep bruxism) or during wakefulness (indicated as awake bruxism)”(Lobbezoo et al., 2013).
Bruxism can generate forces as much as six times the normal masticating forces (Manfredini et al., 2015) Occlusal splints can disperse these loads along with the masticatory structure. Therefore, the splints can reduce the frequency of bruxing occurrences but not its intensity (Alqutaibi and Aboalrejal, 2015).
Facebow transfer ensures that the maxillary cast is oriented in a similar or at least comparable distance to the hinges of the articulator as are the natural maxillary teeth to the assumed “axis of rotation” of the TMJ (Nagy and Goldstein, 2019).
Previous studies reported that the facebow record has a significant effect on the construction of occlusal appliances such as stabilization appliances (Shodadai et al., 2001, Gámez and Espinosa, 2013). The use of this tool will minimize the risk of occlusal faults; thus, the accuracy of occlusion of the oral stabilization appliances will be enhanced upon their insertion. Besides, occlusal splints fabricated on casts by using facebow may have more occlusal contacts during insertion and require less occlusal adjustment than those mounted without a facebow (Shodadai et al., 2001).
With the introduction of CAD/CAM technology, the functional deficiencies associated with conventionally-fabricated splints were significantly improved (Algabri et al., 2017). From this point, the concept of the CAD/CAM stabilizing splint appeared as a substitute treatment option for TMDs patients. Up to date, published data about CAD/CAM occlusal splint are scarce, and most of them are case reports. However, this investigation is the first to compare a computer designed and manufactured occlusal splint made with and without facebow.
The null hypothesis tested was that no differences would be found between CAD/CAM stabilization occlusal splint made with and without facebow concerning patient satisfaction and time needed for adjustment.
2. Material and methods
2.1. Sampling and eligibility criteria
A total sample size of 24 patients (12 patients per group) with a confidence level of 95% and a power of 80% will be adequate to detect the effect size of 0.8. The eligibility criteria include; age range from 20 to 45 years, any sex, those willing to contribute in the trial, signing informed consent, with natural dentition with less than eight missing teeth with replacement except wisdom teeth and complaining of teeth wear as a result of bruxism were selected.
2.2. Patients examination
All patients were examined clinically at the department of prosthodontics, Cairo university. Clinical examination was derived from the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) (Dworkin, 1992). The comprehensive examination comprised of two portions; The first portion included a complete history questionnaire which specified data about signs of TMD including muscular pain or fatigue and TMJ noise, which restricts the daily activities in addition to the presence of headache and earache. The second portion included the clinical examination using sets of diagnostic approaches to evaluate the vertical range of opening with and without passive stretch, clicking during mandibular movements, joint pain, extraoral and intraoral muscle pain on palpation.
All patients were evaluated for bruxism independently by two qualified investigators. The clinical inspection was done to assess teeth wear by drying the teeth with air and cotton rolls, and then clinical examination is done by a dental mirror.
Data regarding symptoms were gathered, including noises related to bruxism reported by a relative, clenching through the day, repeated awakening at night though grinding or clenching, and sense of muscle pain throughout the day or awakening. In this trial, patients were assumed to be positive bruxers when the clinical, and at least one of the symptoms indicators were present. Each patient received a questionnaire on signs and symptoms of bruxism, comprising of ten questions. This evaluation assessed bruxism by using a standardized questionnaire (Gámez, 2013) besides the history interview of the dental examination (RDC/TMD). The participant was considered as a bruxer when responded for at least one of the first five questions or three of the last five questions; besides, they showed either tooth attrition or masseter muscle hypertrophy (Table 1).
Table 1.
A screening questionnaire for detecting bruxer.
| Without facebow |
With facebow |
P-value | |||
|---|---|---|---|---|---|
| Yes | No | Yes | No | ||
| 1. Do you feel or have been told that you clench your teeth during the day? | 9 (75.0%) |
3 (25.0%) |
8 66.7% |
4 33.3% |
0.65 |
| 2. Do you feel or have been told that you clench your teeth at night? | 11 (91.7%) |
1 (8.3%) |
12 100.0% |
0 0.0% |
0.30 |
| 3. Do you feel or have been told that you grind your teeth during the day? | 4 (33.3%) |
8 (66.7%) |
2 16.7% |
10 83.3% |
0.34 |
| 4. Do you feel or have been told that you grind your teeth at night? | 6 (50.0%) |
6 (50.0%) |
7 58.3% |
5 41.7% |
0.78 |
| 5. Do you have any type of pain or discomfort around your face or neck? | 7 (58.3%) |
5 (41.7%) |
6 50.0% |
6 50.0% |
0.82 |
| 6. Do you have some kind of sensitivity or pain by your ear? | 9 (75.0%) |
3 (25.0%) |
7 58.3% |
5 41.7% |
0.39 |
| 7. Do you feel any jaw discomfort when you wake up? | 4 (33.3%) |
8 (66.7%) |
5 41.7% |
7 58.3% |
0.54 |
| 8. Do you have frequent headaches? | 4 (33.3%) |
8 (66.7%) |
7 58.3% |
5 41.7% |
0.22 |
| 9. Do you have any type of fracture or abnormal teeth wear? | 4 (33.3%) |
8 (66.7%) |
4 33.3% |
8 66.7% |
1 |
| 10. Do you feel being stressed often? | 11 (91.7%) |
1 (8.3%) |
12 100.0% |
0 0.0% |
0.30 |
2.3. Study design
This trial was planned as a double-blinded parallel randomized trial. After clinical examinations for 24 selected patients, random sequence generation was performed. The subjects were randomly allocated into; Group1 (with facebow) 12 patients with a mean age of 34.8 years (two males and ten females): The patients received maxillary CAD/CAM occlusal stabilizing splint recorded with centric relation using facebow record. Group 2 (without facebow) 12 patients with a mean age of 36.2 years (three males and nine females): The patient received maxillary CAD/CAM occlusal stabilizing splint recorded with centric relation without using the facebow record.
The randomized numbers were walled in serially numbered, identical, and solid envelopes. Blinding of participants and investigators was achieved as the color of the two types of inserted splints were the same. The investigators were neither commenting on the possibilities of participants' treatment and nor present when patients completed the questionnaires regarding the visual analogue scale (VAS). Furthermore, regarding the adjustment time, blinding was necessary to be done. The protocol of this trial was permitted by the Committee of Ethics of Faculty of Dentistry, Cairo University, Egypt.
2.4. Fabrication of CAD-CAM splint
For both groups, irreversible hydrocolloid impressions (Cavex Holland B.V) were made for maxillary and mandibular arches. Master casts were poured with gypsum that was manipulated with a vacuum mixer (Vacuum mixer. BEGO Motova sl. Germany), with a powder/water ratio of 100 g/20 ml mixed for 30 s. The pouring was under constant vibration (Lab vibrator, BEGO Motova sl. Germany) into the impression. After setting, the impressions were separated from the casts. For group1, the maxillary cast was mounted using arbitrary earpiece facebow (Bio-art facebow, BRAZIL) with a semi-adjustable articulator (Fig. 1a). For group2, the maxillary cast was mounted in a conventional way without facebow
Fig. 1.
(a) Maxillary cast mounted using facebow, (b) Lower cast mounted on an articulator using interocclusal registration material.
Bite registration was taken for both groups using an anterior jig and bite registration paste (Vinyl Polysiloxane, Futar D Fast, USA) for mounting lower cast (Fig. 1b).
In both groups, adjustments of the articulator were 15° Bennett angle and 45°condylar inclination. The upper and lower casts with bite registration were then scanned using dental wings scanner (DWOS, Germany).
The CAD/CAM splints were designed by DWOS software (Dental Wings, Germany) (Fig. 2) and finally 3D printed (ZENiTH, DENTIS, South Korea) (Fig. 3).
Fig. 2.
computer-aided designing of the splint. (a) The contour of the splint was traced by placing the dots one by one or by drawing freely on the teeth using “Edited current margin design”. (b) The splint was refined by editing the splint surface for maximum comfort and esthetics; (c) fitting surface of the finished splint.
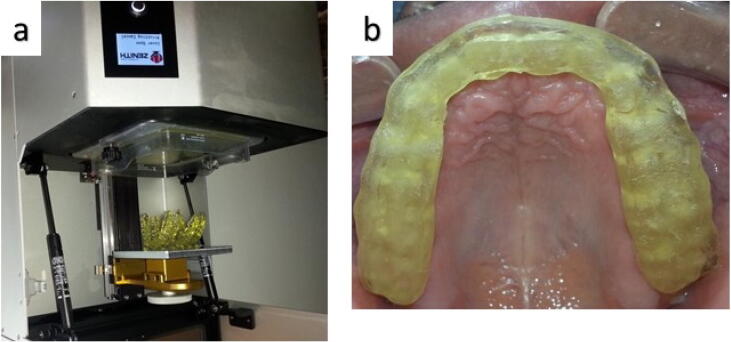
Fig. 3.
(a) Splints constructed using 3D printer; (b) intraoral occlusal view of CAD/CAM splint.
The material used for fabrication of the splints was a monomer based on acrylic esters (Next Dent Ortho Rigid, Netherlands). For both groups, the design of the splints had a flat occlusal surface that allows for a contact of posterior teeth functional cusps and anterior incisal edges in centric position, with canine guidance during lateral movements.
Patient satisfaction with the visual analogue scale was recorded at baseline, one month, and three months follow-up periods. The adjustment time of both splints was calculated using a stopwatch.
2.5. Statistical analysis
The data were summarized as means and standard deviations and analysed with SPSS statistical package. A comparison between the mean values of both groups was made by an independent t-test. The ANOVA test was used for the comparison of the effect of time in different follow-up periods.
3. Results
A sample of twenty-four patients with a mean age of 35.5 years (5 Male, 19 Female), were included in this study. There were no differences between groups regarding gender or age distribution. Fig. 4 showed the CONSORT flow chart of this study.
Fig. 4.
CONSORT flow chart.
The participants were subjected to a screening questionnaire for detecting bruxers, as shown in Table 1. No significant difference in response to the screening questions in both groups was found (P > 0.05).
3.1. Patient's satisfaction
The VAS results did not show a statistically significant difference between two splints. Both occlusal splints with or without the use of facebow improved the patient's satisfaction without differences at baseline, one month and three months with a p-value of 0.73, 0.24 and 0.45 respectively as indicated by student t-test (Table 2).
Table 2.
Comparison of VAS results of two groups.
| Without facebow |
With facebow |
P value | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Baseline | 6.9 | 1.55 | 7.1 | 1.35 | 0.73 |
| One month | 4.8 | 1.72 | 4.1 | 1.04 | 0.24 |
| 3 months | 3.1 | 1.21 | 2.9 | 0.93 | 0.45 |
| P value | < 0.01* | < 0.01* | |||
3.2. Time of adjustments
from the start of splint delivery until becoming well-fitted and occlusally adjusted, was calculated using a stopwatch. The time needed for adjustment for group 1 was 15 ± 5.25 while that required for group 2 was 19 ± 4.5. No statistically significant difference was found (P > 0.05).
4. Discussion
High-quality oral restorations must be designed throughout fabrication techniques by applying effective procedures. However, there are different ideas about the most effective method in transferring dental casts to the articulator. Some researchers have necessitated for the need of true hinge axis (HA) points (Salam, 2016, Singh et al., 2017). Other investigators have considered arbitrary mounting to be adequate (Morneburg and Proschel, 2002). Another study has deemed the need for a face bow is unnecessary but have relied on mean settings for mounting (Tangerud, 2000). The difference in opinions raises the question as to which one is the most satisfactory approach. For addressing this question, a randomized clinical trial regarding CAD-CAM occlusal stabilization splints fabricated with and without facebow.
Up to our knowledge, no previous studies are comparing patient satisfaction in CAD/CAM stabilization occlusal splint made with and without facebow. The results of the present study did not find significant differences in terms of patient satisfaction between both groups. This finding can be compared to previous studies (Kawai et al., 2005, Omar et al., 2013), which evaluated completely edentulous patients and showed no significant variations in patient satisfaction with classical (using facebow) or simplified fabrication methods (without using facebow).
On the contrary, previous studies (Heydecke et al., 2007, Heydecke et al., 2008) evaluating the effect of facebow on overall satisfaction using VAS measures, aesthetics, and stability were significantly better for the simple technique. They found that 25% of patients favored the classical method using facebow, 60% of patients liked the simple approach, and 15% of them did not show any preference.
Regarding the time for adjustment, no significant difference was found between both groups that are in accordance to a study conducted by Shodadai et al. (2001), where each patient received two conventional splints made with or without facebow registration. They found that there was no significant difference between both methods. The authors proposed a combination of reasons to clarify why the use of an arbitrary facebow may not be beneficial which include: alteration (usually increase) of vertical dimension after requiring the interocclusal record, no proof for pure rotation of the condyle and the presence of a condylar hinge axis during the opening of the mandible; condylar movements always change and cannot be predicted on mandibular opening; using rigid hinge axis articulators; and the occurrence of pain in the temporomandibular.
Another study conducted by Gámez (2013), was carried out to compare the number of occlusal contacts recorded and adjustment time in Michigan occlusal splints fabricated with or without facebow transfer in bruxism patients. The occlusal contact points over the two types of splints were similar. Besides, adjustment time was comparable for the two approaches.
A published review showed that the use of a facebow is superfluous (Yohn, 2016). However, several authors have raised concern over the scientific conduct of that report (Khanna, 2016, Wilkerson, 2016). Supporters of the facebow transfer consider that the facebow should be kept in the dental practice as a correct arc of closure is depends on a correct condylar axis position, and this is essential in maintaining the centric relation position (Yohn, 2016).
The limitations of the present study include the use of an earpiece facebow type without comparing it to other different types like fascia facebow, which can alter the current results. Another limitation is the small size of the sample, which can affect reduce the external validity and generalizability of the results. Therefore, other studies using different types of facebow and with larger sample size are needed to overcome these limitations.
5. Conclusion
According to the results of this study, the use of the earpiece facebow in construction of the CAD/CAM occlusal stabilizing splint did not has an effect on the patient satisfaction and the time required for adjustment.
Ethical statement
The study was approved by the Institutional Review Board (IRB), College of Dentistry, Cairo University.
CRediT authorship contribution statement
Ahmed Yaseen Alqutaibi: Conceptualization, Methodology, Validation, Investigation, Resources, Data curation, Writing - review & editing, Visualization. Radwan Algabri: Conceptualization, Methodology, Validation, Investigation, Writing - review & editing. Wafaa Ibrahim Ibrahim: Writing - review & editing, Visualization. Sary Borzangy: Formal analysis, Data curation, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Algabri R.S., Alqutaibi A.Y., Abo-Alrejal H., Al Adashi O., Abdulrahman F., Amr Elkhadem A. Effect of computer-aided design/computer-assisted manufacture versus conventional occlusal splints on the management of temporomandibular disorders: a systematic review and meta-analysis. Int. Dent. Med. J. Adv. Res. 2017;3:1–9. [Google Scholar]
- Alqutaibi A., Aboalrejal A. Types of occlusal splint in management of temporomandibular disorders (TMD) J. Arthritis. 2015;4(176):2. [Google Scholar]
- Deshpande R.G., Mhatre S. TMJ disorders and occlusal splint therapy–a review. Int. J. Dental Clin. 2010;2(2) [Google Scholar]
- Dworkin S.F. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J. Craniomandib. Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- Gámez J.D.A., Espinosa I.A. Facebows in the development of Michigan occlusal splints. Rev. Fac. Odontol. Univ. Antioq. 2013;25:117–131. [Google Scholar]
- Heydecke G., Akkad A.S., Wolkewitz M., Vogeler M., Turp J.C., Strub J.R. Patient ratings of chewing ability from a randomised crossover trial: lingualised vs. first premolar/canine-guided occlusion for complete dentures. Gerodontology. 2007;24(2):77–86. doi: 10.1111/j.1741-2358.2007.00153.x. [DOI] [PubMed] [Google Scholar]
- Heydecke G., Vogeler M., Wolkewitz M., Turp J.C., Strub J.R. Simplified versus comprehensive fabrication of complete dentures: patient ratings of denture satisfaction from a randomized crossover trial. Quintessence Int. 2008;39(2):107–116. [PubMed] [Google Scholar]
- Kawai Y., Murakami H., Shariati B., Klemetti E., Blomfield J.V., Billette L., Lund J.P., Feine J.S. Do traditional techniques produce better conventional complete dentures than simplified techniques? J. Dent. 2005;33(8):659–668. doi: 10.1016/j.jdent.2005.01.005. [DOI] [PubMed] [Google Scholar]
- Khanna N. More on face bows. J. Am. Dent. Assoc. 2016;147(9):697–698. doi: 10.1016/j.adaj.2016.07.006. [DOI] [PubMed] [Google Scholar]
- Klasser G.D., Greene C.S. Oral appliances in the management of temporomandibular disorders. Oral Surgery, Oral Med., Oral Pathol., Oral Radiol., Endodontol. 2009;107(2):212–223. doi: 10.1016/j.tripleo.2008.10.007. [DOI] [PubMed] [Google Scholar]
- Lobbezoo F., Ahlberg J., Glaros A., Kato T., Koyano K., Lavigne G., De Leeuw R., Manfredini D., Svensson P., Winocur E. Bruxism defined and graded: an international consensus. J. Oral Rehabil. 2013;40(1):2–4. doi: 10.1111/joor.12011. [DOI] [PubMed] [Google Scholar]
- Manfredini D., Ahlberg J., Winocur E., Lobbezoo F. Management of sleep bruxism in adults: a qualitative systematic literature review. J. Oral Rehabil. 2015;42(11):862–874. doi: 10.1111/joor.12322. [DOI] [PubMed] [Google Scholar]
- Morneburg T.R., Proschel P.A. Predicted incidence of occlusal errors in centric closing around arbitrary axes. Int. J. Prosthodont. 2002;15(4):358–364. [PubMed] [Google Scholar]
- Nagy W.W., Goldstein G.R. Facebow use in clinical prosthodontic practice. J. Prosthodont. 2019;28(7):772–774. doi: 10.1111/jopr.12944. [DOI] [PubMed] [Google Scholar]
- Omar R., Al-Tarakemah Y., Akbar J., Al-Awadhi S., Behbehani Y., Lamontagne P. Influence of procedural variations during the laboratory phase of complete denture fabrication on patient satisfaction and denture quality. J. Dent. 2013;41(10):852–860. doi: 10.1016/j.jdent.2013.07.013. [DOI] [PubMed] [Google Scholar]
- Salam E. The Effect of Hinge Axis Position on Mandibular Movements. Al-Azhar Dent. J. Girls. 2016;3(1):11–15. [Google Scholar]
- Shodadai S.P., Turp J.C., Gerds T., Strub J.R. Is there a benefit of using an arbitrary facebow for the fabrication of a stabilization appliance? Int. J. Prosthodont. 2001;14(6):517–522. [PubMed] [Google Scholar]
- Singh S., Rehan S., Palaskar J., Mittal S. Hinge axis-location, clinical use and controversies. J. Res. Dent. 2017;4(6):158–161. [Google Scholar]
- Srivastava R., Jyoti B., Devi P. Oral splint for temporomandibular joint disorders with revolutionary fluid system. Dental Res. J. 2013;10(3):307. [PMC free article] [PubMed] [Google Scholar]
- Tangerud, T.C.G., 2000. Jaw registration and occlusal morphology. In: Karlsson, S., Nilner, K., Dahl, B.L. (Eds.), A Textbook of Fixed Prosthodontics. Gothia, Stockholm, pp. 209–230.
- The Academy of Prosthodontics, 2005. The glossary of prosthodontic terms. J. Prosthet. Dent. 94(1), 10–92. [DOI] [PubMed]
- Wilkerson D.C. The need for face bows. J. Am. Dent. Assoc. 2016;147(9):696–697. doi: 10.1016/j.adaj.2016.07.005. [DOI] [PubMed] [Google Scholar]
- Yohn K. The face bow is irrelevant for making prostheses and planning orthognathic surgery. J. Am. Dent. Assoc. 2016;147(6):421–426. doi: 10.1016/j.adaj.2015.12.011. [DOI] [PubMed] [Google Scholar]