Abstract
Aims
This research aims to measure and compare the fracture resistance and modes of failure of the following three chemically varied computer-aided design/computer-aided manufacturing (CAD/CAM) ceramic veneering materials: IPS e.max CAD, Vita Enamic, and Shofu HC.
Materials and methods
Twenty-seven sound human upper premolars were collected and stored in saline at room temperature until the experiment started and were assigned to three groups at random (n = 9). Putty indices were prepared to ensure a standardized butt joint preparation. An InEos X5 scanner was used to scan all the samples, and the resulting data were transferred to a CAD/CAM milling machine for veneer fabrication based on the materials used. Twenty-seven machined ceramic veneers were milled from three different ceramic materials. The cementation process was conducted for each material according to the manufacturer's instructions. To quantify the fracture resistance, all the samples underwent 2000 water cycles in a thermocycler and were then mounted in a universal testing machine at a 90° angle at the occlusal part of the veneer. The modes of failure were determined under a stereomicroscope and grouped into type I, ceramic fracture; type II, combined ceramic and tooth fracture; and type III, root fracture.
Results
Shofu HC had the highest mean (±standard deviation) fracture resistance (480.8 ± 92.8 N), followed by IPS e.max CAD (415.9 ± 147.2 N) and Vita Enamic (372.3 ± 123.9 N). However, the results of a one-way analysis of variance did not reveal statistically significant differences among the experimental groups (p = 0.194). The different groups exhibited different modes of failure, with ceramic fracture being the most common type of failure.
Conclusion
All the materials tested in this study exhibited strong fracture resistance values, thereby indicating their use as veneering materials for the upper premolars.
Keywords: CAD/CAM, Fracture resistance, IPS e.max CAD, Hybrid ceramic, Veneers, In vitro
1. Introduction
Over the past years, esthetic dentistry has gradually developed into a significant aspect of restorative dentistry, particularly in veneer placement, owing to the resulting favorable esthetic and long-term outcomes (Gresnigt, 2011, Alothman and Bamasoud, 2018). Veneers are also used for posterior teeth due to increased patient expectations and demands for an excellent esthetic appearance (Summitt et al., 2006).
Several types of veneering materials have been used over the past years. The selection of materials plays a crucial role in the lifespan of restorations, as each material has its own composition and properties (Alothman and Bamasoud, 2018, Fons-Font et al., 2006). Ceramic is one of the most commonly used materials for indirect dental restoration.
The advances progress in the field of digital computer technology has led to the increased usage of CAD/CAM systems in dental practice (Nejatidanesh et al., 2018). This allows for performing the restoration procedure in a more delicate, precise, functional, and faultless manner, thereby increasing the accuracy and quality of dental restorations (Blatz and Conejo, 2019, Mörmann, 2006, Miyazaki et al., 2009). The continuous developments made to this approach have enabled the manufacture of numerous machinable materials with variable indications (Nejatidanesh et al., 2018).
The advances in CAD/CAM technology have led to the introduction of IPS e.max CAD, a lithium disilicate glass-ceramic material, for the first time in 2006 (Ivoclar Vivadent, Scientific Documentation IPS e.max CAD, 2011; Li et al., 2014). It has been used as a monolithic material to produce crowns, three-unit bridges, implant-supported hybrid restorations, veneers, inlays, and onlays ( Ivoclar Vivadent, 2011; Pieger et al., 2014). Owing to its excellent strength, esthetic properties, and user-friendliness, the use of IPS e.max CAD has been growing throughout the years (Willard and Gabriel Chu, 2018).
A polymer-infiltrated ceramic network material known as “hybrid ceramic” has been developed. This material combines the advantages of both composites and all-ceramic restorations. It has a microstructure resembling that of a natural tooth (Coldea et al., 2013, Della Bona et al., 2014). In 2013, the first hybrid ceramic material, “Vita Enamic,” (VITA Zahnfabrik, Bad Säckingen, Germany) comprised of interpenetrating networks of 14% composite with 86% ceramic was introduced (Coldea, 2014). In 2017, the Shofu Company launched a new type of hybrid ceramic called “Shofu HC.” It consists of 61% zirconium silicate embedded within a nanofiller composite that forms a skeleton that evenly absorbs the masticatory loads and enhances fracture resistance (Shofu, 2017).
Clinical evaluation of ceramic veneer restorations showed an overall survival rate of 97.5% over 5 to 7 years, with fracture and debonding as the predominant types of failure (Monaraks and Leevailoj, 2018). Fracture resistance needs to be considered while selecting a restorative material and is of particular significance, especially in posterior teeth, on which the masticatory load is considerable (Belli et al., 2017). Due to the insufficient research related to this topic in the literature, the objective of this study was to measure and compare the fracture resistance of three chemically different CAD/CAM ceramic materials for fabricating veneer, IPS e.max CAD, Vita Enamic, and Shofu HC. In addition to assessing their modes of failure in a standard veneer preparation for the maxillary premolars.
2. Materials and methods
2.1. Teeth selection
This study was conducted after obtaining Research Ethics Committee of Ajman University (UGD-H-18-11-22-14). Using an ultrasonic scaler, twenty-seven extracted, sound, non-cracked, non-discolored, and unworn human maxillary premolars were cleaned. The teeth were then stored at room temperature in saline. Teeth had been obtained due to orthodontic and periodontal reasons within the 6 months prior to the experiment.
2.2. Teeth mounting
With the help of a periodontal probe, the teeth were marked 2 mm apical to the cementoenamel junction (CEJ). To simulate the periodontal ligament, the teeth were dipped in heated modeling wax until up to 2 mm below the CEJ, which produces the effect of a spacer. To simulate the presence of the alveolar bone, the teeth were mounted in self-cure resin (SpofaDental, Duracryl Plus,) 2 mm apical to the CEJ using a mold that is 16 mm wide and 25.8 mm high; they were mounted parallel to the long axis of the mold to mimic the natural biologic width. The modeling wax was then replaced with light body polyvinyl siloxane (Hydrorise light body fast set, Zhermack SpA, Italy) impression material. All the aforementioned steps were performed for standardized teeth mounting (Soares et al., 2005).
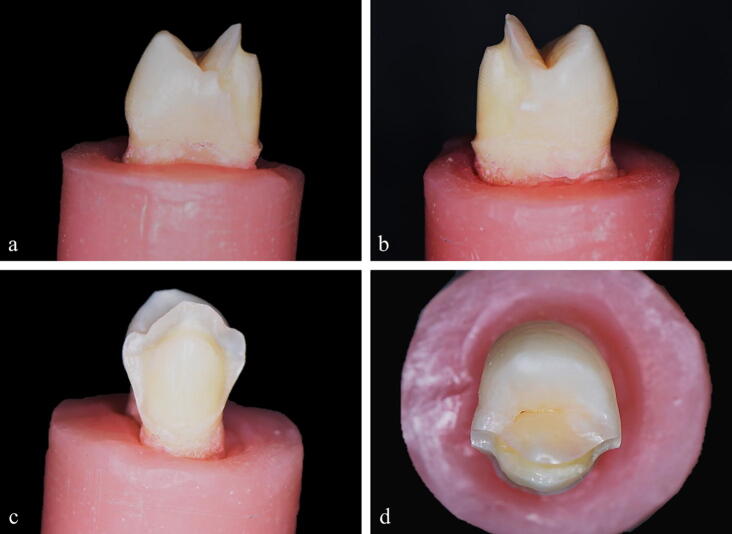
2.3. Tooth preparation
Heavy body silicone (Hydrorise putty- fast set, Zhermack SpA, Italy) was used to fabricate indices for all the teeth to ensure standardized preparation of mounted specimens. Before the process was commenced, the outlines of the preparation were marked. All the teeth were prepared under magnification loupes (3.1x) with a high-speed hand piece under constant cooling. The standardized preparation of the teeth was accomplished using veneer preparation burs (ecoline, Kalletal, Germany). The facial preparation was 0.5 mm in the middle and occlusal thirds and 0.4 mm cervically. The buccal cusp was reduced by 1 mm bucco-palatally and 1.5 mm occluso-cervically. The preparation was completed using the butt joint design. The preparation was finished 1 mm occlusal to the CEJ and just labial to the contact area (Fig. 1). The reduction was restricted to the enamel. Finally, the preparation was checked using a specially marked probe and the customized putty index from the lateral view to ensure that adequate facial and occlusal reduction was achieved (Abdul Khaliq and Al-Rawi, 2014).
Fig. 1.
Standardized tooth preparation. (a & b) Proximal view. (c) Facial view. (d) Occlusal view.
2.4. Teeth grouping
The prepared teeth were distributed into three groups at random (n = 9):
Group I: IPS e.max CAD (Ivoclar Vivadent, Schaan, Liechtenstein, Germany).
Group II: Vita Enamic (VITA Zahnfabrik, Bad Säckingen, Germany).
Group III: Shofu HC (Shofu, Tokyo, Japan).
2.5. Scanning and veneer fabrication
The InEos X5 scanner (Dentsply Sirona, Bensheim, Germany) scanned all samples, and the digital scan data was saved and transferred to a Sirona inLab MC X5 (Dentsply Sirona) CAD/CAM machine. Standardized designs of the veneers were established for the upper premolars and were adjusted using the machine software, and an order for milling samples was set for veneer fabrication (Fig. 2).
Fig. 2.

(a) Image generated by the inEos X5 scanner (Dentsply Sirona) depicting the design of the veneer. (b) Image depicting the fitting of the veneer over the corresponding scanned tooth preparation. (c) The veneer shell.
The IPS e.max CAD ceramic laminate veneers appear to be blue in color in their pre-sintered form. Once milled, the veneers were fired in a ceramic furnace (Ivoclar Vivadent). This process imparts the glass ceramic with its ultimate strength and esthetic properties.
The veneer shells had the same dimensions of the standardized tooth reduction. This was confirmed using a digital dial gauge, with accuracy of 0.01 mm.
2.6. Try-in
After obtaining the veneer shells, the veneer try-ins were performed on the corresponding teeth using an OptraStick adhesive-tipped handling instrument to ensure a primary fit.
2.7. Cementation
Group I (IPS. e.max CAD): The veneer surfaces were etched with 5% hydrofluoric acid (HF) (IPS Ceramic etching, Ivoclar vivadent) for 20 s, washed, and then dried. Single Bond, Universal Adhesive bonding agent (3 M ESPE, St. Paul, MN, USA) was applied to the internal surface of the veneers and excess was removed by using gentle air flow for 5 s to ensure the solvent evaporation. The prepared teeth were etched with 34% phosphoric acid etching gel (3 M ESPE, Scotchbond™, Universal Etchant) for 15 s. The gel was thoroughly rinsed off using a water spray for 10 s. The excess moisture was then removed by gentle air blow, leaving the prepared surface with a slightly glossy moist appearance. The Single Bond Universal Adhesive bonding agent (3 M ESPE) was applied by rubbing it onto the entire prepared surface for 20 s using a disposable applicator; this was followed by air spreading for 5 s without light curing. RelyX Veneer cement (3 M ESPE, St. Paul, MN, USA) was applied onto the internal surface of the veneers. They were seated and held in place while maintaining gentle pressure, and the excess cement was removed using a clean microbrush. The next step involved spot light curing via a dental lightcuring unit (2500mAh, mini LED, SATELEC ACTEON) applied onto the facial surface of the veneer for 20 s. Following which the excess cement was removed. Then light curing was then performed for approximately 30 s for each of the labial, lingual, interproximal, and occlusal surfaces (per the manufacturer instructions, for every 1 mm of ceramic material, the segment needs to be polymerized for at least 10 s).
Group II (Vita Enamic): The inner surfaces of the veneers were etched using 5% HF for 60 s, then rinsed and air dried. This was followed by acid etching with 34% phosphoric acid etching gel (3 M ESPE, Scotchbond™, Universal Etchant) for 5 s. The RelyX ceramic primer (3 M ESPE, St. Paul, MN, USA) was applied onto the internal surfaces of the veneers, and they were air dried gently. The prepared teeth surfaces were etched using 34% phosphoric acid etching gel (3 M ESPE, Scotchbond™, Universal Etchant) for 30 s, washed for 30 s, and air dried for 20 s. Equal amounts of ED primer II A & B of Panavia (Kuraray Noritake Dental Inc, Chiyoda-ku, Tokyo, Japan) were mixed together, and the mixture was applied onto the etched surfaces of the teeth, allowed to react for 30 s, and then air-dried. Equal amounts of Panavia F2.0 pastes A & B were dispensed, mixed for 20 s, and then applied directly onto the internal surface of the veneers. The excess cement was removed, and light curing was performed for 20 s per surface.
Group III (Shofu HC blocks): The internal surfaces of the veneers were etched using 5% HF for 20 s, washed thoroughly, and then dried. The surfaces were cleaned with ethanol (alcohol). HC primer (Shofu, Tokyo, Japan) was then applied and dried until it no longer moved, followed by light curing for 10 s. The prepared teeth surfaces were etched using 34% phosphoric acid etching gel for 15–30 s and then rinsed off with a water spray for at least 5 s. The excess moisture was then removed, leaving the prepared surface with a slightly glossy wet appearance. One drop each of ResiCem Primer A and B were dispensed onto a dish, mixed, then applied onto the teeth, kept in place for 20 s, and air dried. ResiCem Paste (Shofu, Tokyo, Japan) was applied onto the adhesive surfaces of the pretreated veneers. The veneers were seated on the prepared surfaces, then pressed. The excess paste was wiped off thoroughly with a microbrush, and the veneer was light cured for 10 s. The areas where the light was not able to reach were chemically cured. After cementation, all the samples were kept in an incubator for 24 h.
2.8. Thermocycling
In order to simulate a two-year period of the aging process, all the samples were subjected to 2000 cycles of water baths in a thermocycler (SD Mechatronik, Feldkirchen-Westerham, Germany) at temperatures changing from 5 °C to 55 °C with 5 s interval (Chun et al., 2010).
2.9. Measuring fracture resistance
All the samples were mounted onto the universal testing machine (M350-5CT, Testomatric, UK) perpendicular to the tooth’s long axis to simulate the effect of force application during function (Fig. 3). Load to fracture was applied at the speed of 0.5 mm/min (Akoğlu and Gemalmaz, 2011, Linhares et al., 2018) using a locally manufactured customized plunger (chisel shaped steel rod with its flat end having a diameter of 1 mm and a length of 3 mm) fixed onto the upper movable part of the machine (Khatib et al., 2009) set at the occlusal surface of the veneer (Gresnigt et al., 2011). The highest load reading at which each sample was fractured was recorded in Newtons (N) by a software system.
Fig. 3.

The specimen was aligned onto a universal testing machine using an angle adjustment table so that the load was applied along the long axis of all the samples perpendicular to their veneer’s occlusal surface.
2.10. Modes of failure
The samples were inspected under a stereomicroscope at 30x magnification (Upser-SGI limited, Edenbridge, UK) to determine the modes of failure. The modes of failure were classified into three types: type 1, ceramic fracture; type 2, combined ceramic and tooth fracture; and type 3, root fracture.
2.11. Data analysis
The SPSS software application (IBM SPSS analytics version 22, Chicago, IL, USA) was used to perform the statistical analysis. The data were analyzed using the Kolmogorov-Smirnov test to check the assumption of normality. A one-way analysis of variance (ANOVA) with significance level set at p < 0.05 was used to measure the failure load. The numbers and types of failures were assessed. The differences among the study groups were detected using a chi-square test.
3. Results
3.1. The force of fracture
The fracture strengths (mean ± standard deviation) were 480.8 ± 92.8 N, 415.9 ± 147.2 N, and 372.3 ± 123.9 N for group III, group I, and group II, respectively (Fig. 4). The results of the ANOVA revealed no significant differences among the experimental groups (p = 0.194).
Fig. 4.
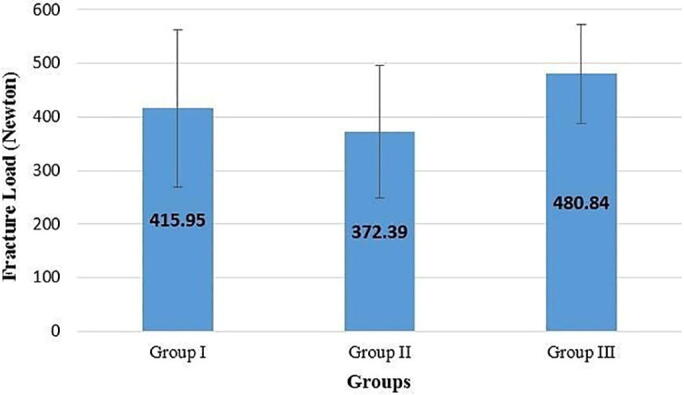
A bar chart representing the mean fracture strength (N) in the different groups.
3.2. Modes of failure
The results of the chi-square test did not reveal significant differences among the tested groups. The most common type of failure was ceramic fracture that was exhibited by 55.6% of the preparations. The least common type of failure was root fracture observed in 14.8% of the preparations. The combined ceramic and tooth fracture was observed in 29.6% of the specimens (Fig. 5).
Fig. 5.
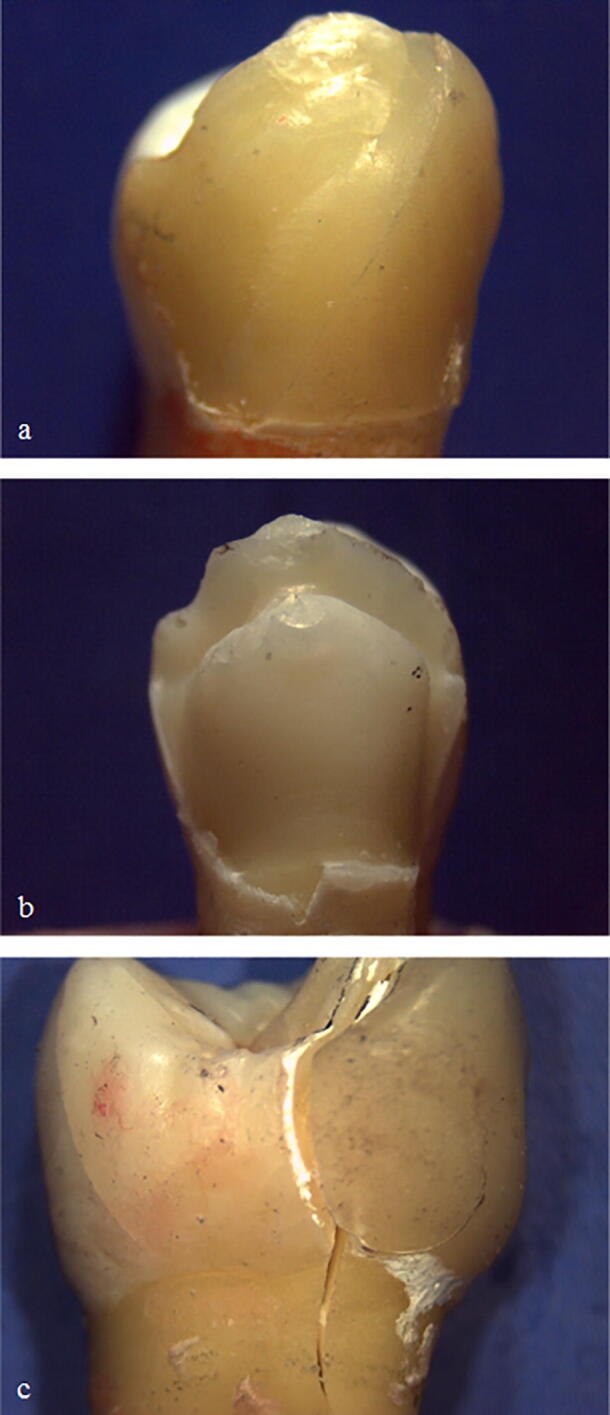
Representative photographs of failed specimens. (a) Type 1: Ceramic fracture. (b) Type 2: Combined ceramic and tooth fracture. (c) Type 3: Root fracture.
The percentage of each type of failure in each group is presented in Table 1.
Table 1.
The number of samples and mode of failure frequency of the veneer failure modalities in each experimental group.
| Fracture Types | Group I | Group II | Group III | Total |
|---|---|---|---|---|
| Type I: Ceramic fracture | 6 (66.7%) | 4 (44.4%) | 5 (55.6%) | 15 (55.5%) |
| Type II: Combined ceramic and tooth fracture | 3 (33.3%) | 2 (22.2%) | 3 (33.3%) | 8 (29.6%) |
| Type III: Root fracture | 0 (0.0%) | 3 (33.3%) | 1 (11.1%) | 4 (14.8%) |
| Total | 9 (100.0%) | 9 (100.0%) | 9 (100.0%) | 27 (100.0%) |
4. Discussion
There are limited studies that tested the fracture resistance property of various laminate veneer materials. Additionally, there are very few studies that have tested upper premolar veneers for fracture resistance. In this study, the upper premolars were selected due to their relatively comparable sizes to those of other teeth in the oral cavity. Clinically, Increased patients’ esthetic demands to the extent of including posterior teeth, such as upper premolars, was also an important factor in teeth selection. Among the tested materials, Shofu HC was discussed for the first time in this paper, as no other studies have investigated the fracture strength of this type of veneer material.
Among the types of failures associated with ceramic restorations, material fracture emerged as the biggest concern (Reiss and Walther, 2000, Donovan, 2008). Although feldspathic ceramics are strong, they are brittle with low fracture toughness and a vulnerability to failure in the presence of flaws (Ruse and Sadoun, 2014). Two diametrically opposed solutions have been proposed for overcoming this problem. One involves the advancement of tougher materials, such as lithium disilicate glass–ceramic (Guess et al., 2013), and the other involves the use of more flexible materials, such as a hybrid ceramic (He et al., 2011).
Assessing the clinical performance of ceramic veneers revealed lower survival rates in cases in which adhesive cementation was carried out without tooth preparation (Shaini et al., 1997). In vitro studies have demonstrated that ceramic fracture was frequently associated with the palatal chamfer preparation design. On the other hand, the butt joint preparation technique resulted in minimal reduction of tooth strength, and the evidence supports the use of butt joint preparations (Chai et al., 2018). In this study, the reduction depth and cementation followed were recommended by the manufacturers (Ivoclar Vivadent, VITA Zahnfabrik, and Shofu) that claim that only if their recommendations were followed, these materials would be in their strongest state.
The fracture resistance test results were the highest in group III with a mean value of 481 N. This can be attributed to the composition of the densely packed nanofiller of the Shofu block embedded in 61% zirconium silicate, as reported by Shofu in 2017 (Shofu, 2017). The lower modulus of elasticity (9.6 GPa) exhibited by Shofu HC correlates to its increased deformation under the applied load, thereby indicating a greater ability to absorb stress when compared to IPS e.max CAD and Vita Enamic. Another possible factor that could be responsible for the high fracture resistance in this group is the effective bonding of the ResiCem primers and cement. The mixture of the self-conditioning dental primers A and B gently penetrates the microstructures of the enamel and dentin. This can also justify the type I and type II failure modes that were observed with this material.
The material that exhibited the second highest value of fracture resistance was IPS e.max CAD with a mean of 416 N, and the most frequent mode of failure with this material was type I, followed by type II failure. These findings can be attributed to the considerable strength of the ceramic content as it is composed of 70% fine-grain lithium disilicate crystals embedded in a glassy matrix, as described by Ivoclar Vivadent ( Ivoclar Vivadent, 2011). Another factor that could potentially be responsible for these findings is the bond strength between the ceramic and prepared tooth surface.
Vita Enamic was the least fracture resistant material with a mean of 372 N. The modes of failure in this group were relatively comparable to those of the other groups, with the most common mode of failure being type I, followed by type III and type II failures. Vita Enamic consists of two 3-dimensional interpenetrating network structures: the predominant fine-structure feldspar ceramic network (75% by volume or 86% by weight) that is reinforced by a polymer network consisting of methacrylate polymer (14% by weight or 25% by volume) (Coldea, 2014). The increased content of the glassy phase weakens the framework by lowering the resistance to crack propagation (Alla, 2013, Sakaguchi and Powers, 2007).
The results of the one-way ANOVA demonstrated that there were no statistically significant differences among the experimental groups (p = 0.194). In this study, all the CAD/CAM ceramic veneers were adhesively bonded to the etched enamel. This type of cementation allowed for a conservative preparation and a stronger bond to the enamel surface.
IPS e.max CAD (group I) exhibited higher fracture resistance values than Vita Enamic (group II). This finding is in agreement with the results of the studies by Albero et al., 2015, Sagsoz and Yanıkoglu, 2018, Al-Akhali et al., 2017, and Sagsoz et al. (2018). Although these studies used blocks, monolithic crowns, occlusal veneers, and inlays, respectively, their findings are still in consistent with the findings of this study. Two recent studies (Al-Akhali et al., 2017, Andrade et al., 2018) used occlusal veneers made of similar materials (Vita Enamic and IPS e.max CAD) along with other different comparative materials and reported the same results. In 2017, Al-Akhali et al. evaluated the performance of occlusal veneers placed on the first upper premolars and found that the IPS e.max CAD samples exhibited higher fracture resistance than the Vita Enamic samples; however, no statistically significant differences were noted among these tested groups. Andrade et al. (2018) showed the same findings in a study that tested the fracture resistance of occlusal veneers on 60 natural wisdom teeth. They found that Vita Enamic had the lowest fracture resistance while IPS e.max CAD had the highest.
It is noteworthy that all the veneering materials tested in this study represented ceramic fractures as the most frequent type of failure observed in 55.5% of the samples. This type of failure is relatively favorable and allows for easy intraoral repair. The most likely reasons are the type of teeth preparation and the design of the experimental setup including the fracture load point and the load direction that resulted in chipping or veneer fracturing before the applied force was transmitted to the tooth structure (Lin et al., 2012).
In addition to adequate adhesion and high flexural strength, the relatively weak enamel margins or dehydrated tooth surfaces could potentially be other reasons behind the type II failures observed in a total of 29.6% of the specimens. Further, 14.8% of the specimens among all tested groups were found to exhibit type III failures (Root fractures). Since equal amounts of dental tissue have been prepared, the differences in the properties of the teeth structure resulted in variations of enamel thickness between teeth, especially at CEJ, which may have been contributed to this finding. As well as variations in the storage media, duration of time elapsed since the extraction, individuals’ ages, and quality of the extracted teeth. Generally, human teeth are quite diverse in their quality, and therefore, standardization among samples is challenging (Peumans et al., 1999). Good bonding strength between the tooth and the veneer resulted in no debonding.
5. Conclusion
Within this study's limitations, there were no statistically significant differences in fracture resistance among the three chemically different types of CAD/CAM materials used for fabricating labial veneers. Furthermore, no significant differences between the three groups were identified in terms of failure modes, with ceramic fracture being the most frequent type of failure.
Clinical significance: Selecting an appropriate material for veneering the posterior teeth is critical for clinicians, especially in regions where there is excessive occlusal load. All the CAD/CAM veneer materials showed high resistance to ceramic fracture.
6. Funding statement
This research was supported by Ajman University.
CRediT authorship contribution statement
Abdul Rahman Mohammed Saleh: Conceptualization, Supervision, Methodology, Data curation. Mena Al-Ani: Writing - original draft, Methodology, Visualization, Investigation, Data curation. Tuqa ALRawi: Writing - original draft, Methodology, Visualization, Investigation, Data curation. Ghufran Al-Edressi: Writing - original draft, Methodology, Visualization, Investigation, Data curation.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Special thanks goes to Ajman University for financial support and granting us the opportunity of utilizing its facilities.
Footnotes
Peer review under responsibility of King Saud University.
References
- Abdul Khaliq A., Al-Rawi I. Fracture strength of laminate veneers using different restorative materials and techniques (A comparative in vitro study) J. Bagh. College Dentistry. 2014;26(4):1–8. [Google Scholar]
- Akoğlu B., Gemalmaz D. Fracture resistance of ceramic veneers with different preparation designs. J. Prosthodont. 2011;20(5):380–384. doi: 10.1111/j.1532-849X.2011.00728.x. [DOI] [PubMed] [Google Scholar]
- Al-Akhali M., Chaar M.S., Elsayed A., Samran A., Kern M. Fracture resistance of ceramic and polymer-based occlusal veneer restorations. J. Mech. Behav. Biomed. Mater. 2017;74:245–250. doi: 10.1016/j.jmbbm.2017.06.013. [DOI] [PubMed] [Google Scholar]
- Albero A., Pascual A., Camps I., Grau-Benitez M. Comparative characterization of a novel cad-cam polymer-infiltrated-ceramic-network. J. Clin. Exp. Dent. 2015;7(4):495–500. doi: 10.4317/jced.52521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alla R.K. Jaypee Brothers Medical Publishers Pvt. Limited; New Delhi, India: 2013. Dental Materials Science; pp. 333–354. [Google Scholar]
- Alothman Y., Bamasoud M.S. The success of dental veneers according to preparation design and material type. Open Access Maced. J. Med. Sci. 2018;6(12):2402–2408. doi: 10.3889/oamjms.2018.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade J.P., Stona D., Bittencourt H.R., Borges G.A., Burnett Júnior L.H., Spohr A.M. Effect of different computer-aided design/computer-aided manufacturing (CAD/CAM) materials and thicknesses on the fracture resistance of occlusal veneers. Oper. Dent. 2018;43(5):539–548. doi: 10.2341/17-131-L. [DOI] [PubMed] [Google Scholar]
- Belli R., Wendler M., de Ligny D., Cicconi M.R., Petschelt A., Peterlik H., Lohbauer U. Chairside CAD/CAM materials. Part 1: Measurement of elastic constants and microstructural characterization. Dent. Mater. 2017;33(1):84–98. doi: 10.1016/j.dental.2016.10.009. [DOI] [PubMed] [Google Scholar]
- Blatz M.B., Conejo J. The current state of chairside digital dentistry and materials. Dent. Clin. North Am. 2019;63(2):175–197. doi: 10.1016/j.cden.2018.11.002. [DOI] [PubMed] [Google Scholar]
- Chai S.Y., Bennani V., Aarts J.M., Lyons K. Incisal preparation design for ceramic veneers: a critical review. J. Am. Dent. Assoc. 2018;149(1):25–37. doi: 10.1016/j.adaj.2017.08.031. [DOI] [PubMed] [Google Scholar]
- Chun Y.H., Raffelt C., Pfeiffer H., Bizhang M., Saul G., Blunck U., Roulet J.F. Restoring strength of incisors with veneers and full ceramic crowns. J. Adhes. Dent. 2010;12(1):45–54. doi: 10.3290/j.jad.a17533. [DOI] [PubMed] [Google Scholar]
- Coldea, A., 2014. Suitability of Polymer-Infiltrated-Ceramic-Networks for CAD/CAM based dental restorative materials (Thesis, Doctor of Philosophy). University of Otago. Available from: http://hdl.handle.net/10523/5017. [Accessed: 3rd March 2019].
- Coldea A., Swain M.V., Thiel N. Mechanical properties of polymer- infiltrated-ceramic-network materials. Dent. Mater. 2013;29(4):419–426. doi: 10.1016/j.dental.2013.01.002. [DOI] [PubMed] [Google Scholar]
- Della Bona A., Corazza P.H., Zhang Y. Characterization of a polymer- infiltrated ceramic-network material. Dent. Mater. 2014;30(5):564–569. doi: 10.1016/j.dental.2014.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan T.E. Factors essential for successful all-ceramic restorations. J. Am. Dent. Assoc. Suppl. 2008;139:14S–18S. doi: 10.14219/jada.archive.2008.0360. [DOI] [PubMed] [Google Scholar]
- Fons-Font A., Solá-Ruíz M.F., Granell-Ruíz M., Labaig-Rueda C., Martínez-González A. Choice of ceramic for use in treatments with porcelain laminate veneers. Med. Oral Patol. Oral Cir. Bucal. 2006;11(3):E297–E302. [PubMed] [Google Scholar]
- Gresnigt M. Department of Fixed and Removable Prosthodontics, University of Groningen, Netherlands; Thesis: 2011. Clinical and laboratory evaluation of laminate veneers, chapter one: Introduction. [Google Scholar]
- Gresnigt M.M., Ozcan M., Kalk W., Galhano G. Effect of static and cyclic loading on ceramic laminate veneers adhered to teeth with and without aged composite restorations. J. Adhes. Dent. 2011;13(6):569–577. doi: 10.3290/j.jad.a21742. [DOI] [PubMed] [Google Scholar]
- Guess P.C., Selz C.F., Steinhart Y.N., Stampf S., Strub J.R. Prospective clinical split-mouth study of pressed and CAD/CAM all-ceramic partial-coverage restorations: 7- year results. Int. J. Prosthodont. 2013;26(1):21–25. doi: 10.11607/ijp.3043. [DOI] [PubMed] [Google Scholar]
- He L.H., Purton D., Swain M.V. A novel polymer infiltrated ceramic for dental simulation. J. Mater. Sci. Mater. Med. 2011;22(7):1639–1643. doi: 10.1007/s10856-011-4350-3. [DOI] [PubMed] [Google Scholar]
- Ivoclar Vivadent, 2011. Scientific Documentation; IPS e.max CAD. Liechtenstein. [Online] Available from: http://www.ivoclarvivadent.com/en/p/laboratory- professional/products/all-ceramics/ips-emax- technicians/ [Accessed: 12th April 2019].
- Khatib D., Katamish H., Ibrahim A.S. Fracture load of two CAD/CAM ceramic veneers with different preparation designs. C.D.J. 2009;25(3):425–432. [Google Scholar]
- Li R.W., Chow T.W., Matinlinna J.P. Ceramic dental biomaterials and CAD/CAM technology: state of the art. J. Prosthodont. Res. 2014;58(4):208–216. doi: 10.1016/j.jpor.2014.07.003. [DOI] [PubMed] [Google Scholar]
- Lin T.M., Liu P.R., Ramp L.C., Essig M.E., Givan D.A., Pan Y.H. Fracture resistance and marginal discrepancy of porcelain laminate veneers influenced by preparation design and restorative material in vitro. J. Dent. 2012;40(3):202–209. doi: 10.1016/j.jdent.2011.12.008. [DOI] [PubMed] [Google Scholar]
- Linhares L.A., Pottmaier L.F., Lopes G.C. Fracture resistance of veneers in premolars. Eur. J. Dent. 2018;12(2):191–198. doi: 10.4103/ejd.ejd_349_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyazaki T., Hotta Y., Kunii J., Kuriyama S., Tamaki Y. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dent. Mater. J. 2009;28(1):44–56. doi: 10.4012/dmj.28.44. [DOI] [PubMed] [Google Scholar]
- Monaraks R., Leevailoj C. The Longevity of Ceramic Veneers: Clinical Evaluation of Mechanical, Biologic and Aesthetic Performances of Ceramic Veneers, a 7-year Retrospective Study. J. Dent. Assoc. Thai. 2018;68(3):288–301. [Google Scholar]
- Mörmann W.H. The evolution of the CEREC system. J. Am. Dent. Assoc. 2006;137:7S–13S. doi: 10.14219/jada.archive.2006.0398. [DOI] [PubMed] [Google Scholar]
- Nejatidanesh F., Savabi G., Amjadi M., Abbasi M., Savabi O. Five year clinical outcomes and survival of chairside CAD/CAM ceramic laminate veneers - a retrospective study. J. Prosthodont. Res. 2018;62(4):462–467. doi: 10.1016/j.jpor.2018.05.004. [DOI] [PubMed] [Google Scholar]
- Peumans M., Van Meerbeek B., Yoshida Y., Lambrechts P., Vanherle G. Porcelain veneers bonded to tooth structure: an ultra-morphological FE-SEM examination of the adhesive interface. Dent. Mater. 1999;15(2):105–119. doi: 10.1016/s0109-5641(99)00020-2. [DOI] [PubMed] [Google Scholar]
- Pieger S., Salman A., Bidra A.S. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2014;112(1):22–30. doi: 10.1016/j.prosdent.2014.01.005. [DOI] [PubMed] [Google Scholar]
- Reiss B., Walther W. Clinical long-term results and 10-year Kaplan-Meier analysis of CEREC restorations. Int. J. Comput. Dent. 2000;3(1):9–23. [PubMed] [Google Scholar]
- Ruse N.D., Sadoun M.J. Resin-composite blocks for dental CAD/CAM applications. J. Dent. Res. 2014;93(12):1232–1234. doi: 10.1177/0022034514553976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagsoz N.P., Yanıkoglu N. Evaluation of the fracture resistance of computer-aided design/computer-aided manufacturing monolithic crowns prepared in different cement thicknesses. Niger. J. Clin. Pract. 2018;21(4):417–422. doi: 10.4103/njcp.njcp_137_17. [DOI] [PubMed] [Google Scholar]
- Sagsoz O., Yildiz M., Hojjat Ghahramanzadeh A.S.L., Alsaran A. In vitro Fracture strength and hardness of different computer-aided design/computer-aided manufacturing inlays. Niger. J. Clin. Pract. 2018;21(3):380–387. doi: 10.4103/njcp.njcp_58_17. [DOI] [PubMed] [Google Scholar]
- Sakaguchi, R.L., Powers, J.M., 2007. Craig’s Restorative Dental Materials, 12th ed. Elsevier, A division of Reed Elsevier India Pvt. Ltd. New Delhi, India: Mosby. 443–464.
- Shaini F.J., Shortall A.C., Marquis P.M. Clinical performance of porcelain laminate veneers. A retrospective evaluation over a period of 6.5 years. J. Oral Rehabil. 1997;24(8):553–559. doi: 10.1046/j.1365-2842.1997.00545.x. [DOI] [PubMed] [Google Scholar]
- Shofu. (2017) Shofu Block & Disk HC. [Online] Available from: http://www.shofu.com/en/products/ceramics-dentures/new/shofu-block-disk-hc/ [Accessed: 20th April 2019].
- Soares C.J., Pizi E.C., Fonseca R.B., Martins L.R. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz. Oral Res. 2005;19(1):11–16. doi: 10.1590/s1806-83242005000100003. [DOI] [PubMed] [Google Scholar]
- Summitt, J.B., Robbins, J.W., Schwartz, R.S., 2006. Fundamentals of operative dentistry: a contemporary approach, third ed. Chicago, Quintessence Books.
- Willard A., Gabriel Chu T.M. The science and application of IPS e.Max dental ceramic. Kaohsiung. J Med. Sci. 2018;34(4):238–242. doi: 10.1016/j.kjms.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]