Abstract
Objectives
Assessment of the effect of aging and bonding on the reparability of different temporary crown and bridge materials using a flowable resin composite.
Methods
The materials used included two bis-acryl and two polymethylmethacrylate materials. The materials were aged either dry, in distilled water, or in a 75% ethanol/water solution. Each group was divided into three subgroups (n = 6) according to the bonding method: application of a universal adhesive, application of a universal primer followed by a universal adhesive, or no bonding. Materials were repaired with a light-cure flowable resin composite; then, they were subjected to thermocycling and tested by shear bond strength. The data were analysed using three-way ANOVA, one-way ANOVA, and Tukey post hoc tests (α = 0.05).
Results
The shear bond strength was significantly higher for bis-acryl compared to polymethylmethacrylate materials (p < 0.001). In terms of aging conditions, shear bond strength was in the order of 75% ethanol/water solution < dry < water. The application of bonding agents significantly increased the shear bond strength of polymethylmethacrylate-based materials (p < 0.001). The difference between water and dry storage was insignificant (p = 0.558); however, storage in a 75% ethanol/water solution showed significantly lower values compared to both dry and water storage in most of experimental groups (p < 0.001). Polymethylmethacrylate-based materials mainly demonstrated adhesive failure, while bis-acryl materials predominantly showed cohesive failure.
Conclusion
The bond strength of a light-cure flowable resin composite is significantly higher with bis-acryl compared to that with polymethylmethacrylate-based substrates. Aging in water does not have a significant effect; however, the 75% ethanol/water solution tends to negatively affect repairability. The application of different bonding agents positively affects the repair strength, especially for polymethylmethacrylate-based substrates.
Keywords: Repair, Temporary dental prostheses, Resin composite, Aging, Bonding agent, Provisional
1. Introduction
Temporary crown and bridge materials, which are used for the fabrication of provisional or temporary fixed prosthetic restorations, should possess certain properties such as mechanical strength and repairability. The chairside repair of surface or marginal defects of provisional restorations may require the dentist’s clinical decision to either repair or replace the restoration. For minor defects, repairing the restoration may be the best decision because it is faster and economic (Bohnenkamp and Garcia, 2004). This decision depends on several parameters such as the size of the repair area, time of damage, and repair material to be used (Balkenhol et al., 2008).
Several studies have assessed the reparability of different temporary crown and bridge materials using specific resin composites (Balkenhol et al., 2008, Wiegand et al., 2015, Wendler et al., 2016). Bonding between a repair material and a substrate can occur through either micro-mechanical retention, chemical retention, or a combination of both. To repair temporary crown and bridge materials, different surface treatment approaches have been proposed and assessed. These approaches include roughening of the surface through grinding with a diamond bur or sandblasting with Al2O3 particles (Ha et al., 2016, Jeong and Kim, 2019), tribochemical silica coating (Wiegand et al., 2015, Ha et al., 2016), application of bonding agents (Jeong and Kim, 2019), and more recently by laser surface treatment (Bektas et al., 2012).
There are few studies in the literature that assessed the effect of aging of temporary crown and bridge materials on their reparability. Ethanol/water solution is a relevant aging medium for dental materials because it is considered to be a food-simulating liquid, according to the Food and Drug Administration guidelines (Food and Drug Administration, 1976), and it is also a component that is present in many mouth rinses (Moran, 1997). The effect of aging in an ethanol–water solution on the repair strength of different temporary crown and bridge materials has not been previously assessed. In addition, there are no studies assessing the effect of different bonding conditions on the repairability of different temporary crown and bridge materials using a flowable resin composite. Therefore, the aim of this study is to assess the effect of aging in water and in a 75% ethanol/water solution, together with the application of certain bonding agents on the reparability of different temporary crown and bridge materials using a light-cure flowable resin composite material. In this study, reparability was assessed by measuring the shear bond strength at the repair interface.
2. Materials and methods
Temporary crown and bridge materials included a powder and liquid polymethylmethacrylate (PMMA) material (Duralay), CAD/CAM PMMA material, and two chemical-cure bis-acrylic materials (Protemp 4 and Luxatemp Star). In addition, the materials included a universal adhesive (3M Single Bond Universal Adhesive), universal primer (Tokuyama Universal Primer), and light-cure flowable resin composite (Filtek Z350 XT flowable). The information on materials is summarized in Table 1.
Table 1.
Test materials, composition, and manufacturer details.
| Material and manufacturer | Type and Preparation Mode | Composition | Shade/Batch number | |
|---|---|---|---|---|
| Temporary crown and bridge materials | Duralay (Reliance, Alsip IL, USA) | Self-curing temporary crown and bridge material (powder and liquid manual mix) | PMMA > 98% | 69/071817 |
| CAD/CAM PMMA Blocks (NHT High Technology, Latvia) | Monolayer dental milling block | PMMA | A1/171203010 | |
| Protemp 4 (3M, ESPE, Seefeld, Germany) | Bis-acrylic composite, chemical-cure temporary crown and bridge material, auto-mix | Bis-GMA and a second functionalized dimethacrylate resin, silanated zirconia–silica and fumed silica fillers. Filler loading: 78 wt% (0.6 μm) | A2/4108536 | |
| Luxatemp Star (DMG, Hamburg, Germany) | Bis-acrylic composite, chemical-cure temporary crown and bridge material, auto-mix | Glass filler in a matrix of multifunctional methacrylates, catalysts, stabilizers, and additives. Free of PMMA. Filler loading: 42 wt% = 24 vol% (0.02–2.5 μm) | A2/795205 | |
| Bonding agents | 3M Single Bond Universal Adhesive (3M ESPE, Seefeld, Germany) | Light-cure adhesive | MDP phosphate monomer, dimethacrylate resins, HEMA, Vitrebond copolymer, filler, ethanol, water, initiators, and silane | 661,539 |
| Tokuyama Universal Primer (Tokuyama Dental, Taitou-kuTokyo, Japan) | Primer | MTU-6 (thiouracil monomer), 3-methacryloxypropyltrimethoxysilane, phosphoric acid monomer, MAC-10, bis-GMA, TEGDMA, UDMA, ethanol, and acetone | 013 | |
| Repair material | Filtek Z350 XT flowable (3M ESPE, Seefeld, Germany) | Visible light-activated flowable nanocomposite | Matrix: bis-GMA, TEGDMA, procrylat resins. Fillers: ytterbium trifluoride (0.1–5.0 μm), non-agglomerated/non-aggregated surface-modified 20-nm silica, surface-modified aggregated zirconia/silica clusters (0.6–10 μm), 65 wt%, 46 vol% | A2/N959610 |
PMMA: polymethylmethacrylate, HEMA: hydroxyethylmethacrylate, MDP: methacryloyloxydecyl dihydrogen phosphate, MTU-6: 6-methacryloxyhexyl 2-thiouracil-5-carboxylate, MAC-10: 10-undecanedicarboxylic acid, bis-GMA: bisphenol A-glycidyl methacrylate, TEGDMA: triethylene glycol dimethacrylate, UDMA: urethane dimethacrylate.
2.1. Sample preparation
The sample preparation procedure is shown in Fig. 1. For each sample, a sample carrier was prepared using a cylindrical plastic block. A cylindrical hole was prepared on one side of the plastic block to accommodate the temporary crown and bridge test material. A temporary crown and bridge material were mixed according to the manufacturer instructions and dispensed into the cylindrical hole with a slight overfill. A celluloid strip was applied over the filled cavity and pressed with a glass slide against the plastic block so that excess material was forced out and a flat surface was created. Excess was removed when the material was set. For the CAD/CAM PMMA material, cylindrical specimens were prepared using a milling machine (Expert 5, OPERA SYSTEM, Monaco) and inserted into the sample carrier holes to ensure that adequate retention is achieved. The samples did not receive any surface finishing or polishing.
Fig. 1.
Diagram illustrating sample preparation and experimental procedures.
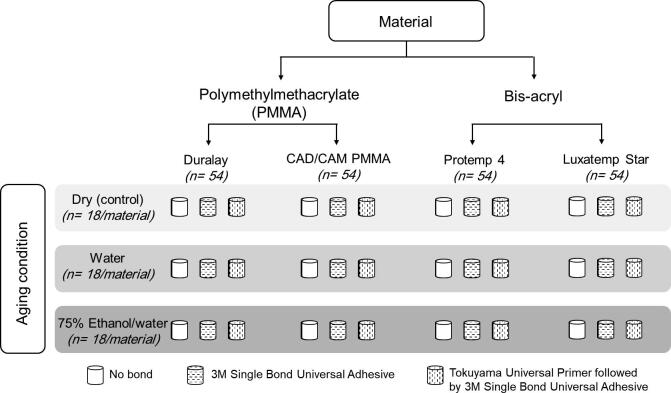
The investigation involved 36 groups (n = 6) with a total of 216 samples. One third of the samples was stored dry (control), another third was stored in distilled water, and the last third was stored in a 75% ethanol/water solution. The samples were stored in designated media in a 37 °C incubator for 7 days. Then, the samples of each group were subdivided into three subgroups. The first group was treated with a Tokuyama universal primer followed by the application of a 3M Single Bond Universal Adhesive (TUP + SUA). The second group was treated by the application of only SUA. The third group did not receive any bonding agent (NB) to act as a control. The experimental design protocol is illustrated in Fig. 2. The assignment of samples of each temporary crown and bridge material to be treated under different aging and bonding conditions was random. The bonding agents were applied according to the manufacturer instructions after the surface was thoroughly dried for 10 s using a grease-free three-way syringe for 10 s. Then, the flowable resin composite was applied to the middle surface of the temporary crown and bridge material using a putty mould (2-mm thickness, 4-mm diameter) adapted on the top surface of the plastic block. A celluloid strip was applied to the top surface of the mould; then, it was pressed with a 1-mm thick glass slide to eject excess material, which resulted in a flat surface. The resin composite was light-cured for 20 s through a glass slide and a celluloid strip using an LED curing unit (E-Morlit, APOZA Enterprise co., LTD., Taiwan) operating in the fast mode. Irradiance (1145 mW/cm2) was determined before each use using a digital radiometer (Smile Dental LED radiometer, USA). The samples were thermocycled (500 cycles; 15 s in 50 °C water, 15 s in 5 °C water, and a 10-s dwell time) and then stored in water at 37 °C for 24 h before testing.
Fig. 2.
Flow chart illustrating experimental groups and study design. Each cylinder represents an experimental group (n = 6).
2.2. Shear bond strength test and failure mode analysis
The samples were subjected to load until failure using a universal testing machine (INSTRON, USA). Each sample was checked for accurate dimensions using a digital caliper before testing. The load direction was parallel to the temporary crown and bridge material/resin composite interface; the cross-head speed used was 0.5 mm/min. Shear bond strength was obtained using the following formula (Rasmussen, 1996):
where σsf is the shear bond strength (MPa), Ff is the failure load (N), and A is the area (mm2).
The failure mode (adhesive, cohesive, and mixed) for each sample was determined by a blinded examiner under a stereomicroscope at 40× magnification. Adhesive failure was observed when failure occurred at the interface between the flowable composite and the temporary crown and bridge material. Cohesive failure was observed when failure occurred exclusively within either the flowable composite or the temporary crown and bridge material. Mixed failure was observed when there was adhesive failure with cohesive failure of any of the neighbouring substrates (flowable composite or temporary crown and bridge material).
2.3. Statistical analysis
The sample size for each experimental group was calculated using a 95% study power, a standard deviation of 5 MPa, and a clinically estimated significant difference of 10 MPa. Data analysis was performed using an IBM statistical package for the social sciences (SPSS) version 25 (IBM Corporation, New York, USA). The effect of each independent factor (material, aging condition, and bonding condition) and the effect of independent factors' interaction on shear bond strength were assessed using three-way ANOVA. To compare the mean values between different bonding and storage conditions for each material, one-way ANOVA and Tukey post hoc tests were applied. The Games–Howell post hoc test was used to compare the mean values when variances were not homogenous. The chi-square test was used to assess the relationship between the failure mode and three independent variables, i.e., material, aging condition, and bonding condition. The significance level was set at 5%.
3. Results
The three-way ANOVA test showed a significant effect of material, aging condition, and bonding condition, as well as a significant interaction between each pair of variables and all three variables on shear bond strength (p < 0.001). Regardless of the aging and bonding conditions, shear bond strength values for different materials were in the order of CAD/CAM PMMA < Duralay < Luxatemp Star < Protemp 4.
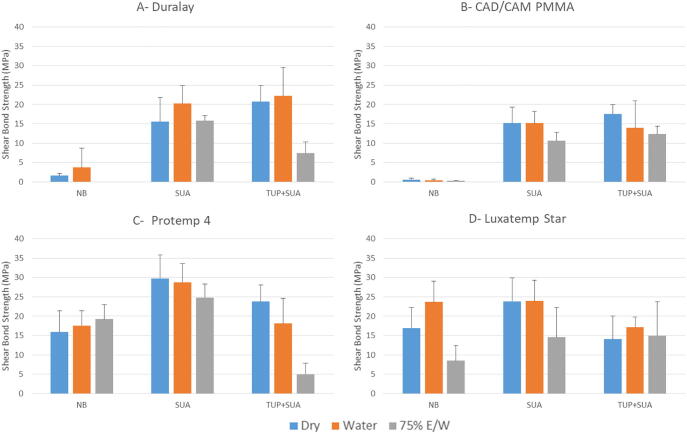
The shear bond strength data for different experimental groups and post hoc comparisons are summarized in Table 2 and shown in Fig. 3. Regarding aging conditions, the mean shear bond values were in the order of 75% ethanol/water solution < dry < water. The difference between water and dry storage was insignificant (p = 0.558); however, storage in a 75% ethanol/water solution showed significantly lower values compared to both dry and water storage (p < 0.001). There were slight deviations from these orders when the values were independently compared for each material. Different bonding conditions showed a significant effect on the shear bond strength (p < 0.001). For Duralay and CAD/CAM PMMA, the shear bond strength was in the order of NB < SUA < TUP + SUA, where SUA and TUP + SUA showed a significantly higher shear bond strength compared to NB (p < 0.001). This order slightly varied under different storage conditions. For Protemp 4 and Luxatemp Star, SUA showed a higher shear bond strength compared to other bonding conditions; however, the difference was not always significant.
Table 2.
Shear bond strength (MPa) of different materials under different aging and bonding conditions. The results are presented as the mean value (standard deviation). The values with the same lower case superscript letter per row indicate statistically homogenous groups. The values with the same upper case superscript letter per column for each test group indicate statistically homogenous groups (Tukey test, α = 0.05).
| Material | Bonding Condition | Aging Condition |
||
|---|---|---|---|---|
| Dry | Water | 75% Ethanol/Water | ||
| Duralay | NB | 1.57 (0.63)A,a | 3.68 (5.07)A,a | 0.00 (0.00)A,a |
| SUA | 15.53 (6.22)B,a | 20.21 (4.62)B,a | 15.79 (1.25)B,a | |
| TUP + SUA | 20.68(4.13) B,a | 22.23 (7.30)B,a | 7.37 (2.90)C,b | |
| CAD/CAM PMMA | NB | 0.55 (0.43)A,a | 0.35 (0.29)A,a | 0.28 (0.05)A,a |
| SUA | 15.14 (4.12)B,a | 15.16 (3.03)B,a | 10.66 (2.08)B,a | |
| TUP + SUA | 17.55 (2.40)B,a | 13.93 (6.96)B,a | 12.34 (2.08)B,a | |
| Protemp 4 | NB | 15.88 (5.51)A,a | 17.58 (3.79)A,a | 19.20 (3.77)A,a |
| SUA | 29.77 (6.09)B,a | 28.80 (4.80)B,a | 24.82 (3.49)B,a | |
| TUP + SUA | 23.81 (4.24)A,B,a | 18.13 (6.55)A,a | 4.96 (2.83)C,b | |
| Luxatemp Star | NB | 16.93 (5.36)A,B,a | 23.68 (5.33)A,a | 8.52 (3.88)A,b |
| SUA | 23.84 (6.06)B,a | 23.91 (5.37)A,a | 14.52 (7.78)A,a | |
| TUP + SUA | 14.02 (6.04)A ,a | 17.16 (2.63)A,a | 15.00 (8.72)A,a | |
NB: No bonding agent.
SUA: 3M Single Bond Universal Adhesive.
TUP + SUA: Tokuyama universal primer followed by a 3M Single Bond Universal Adhesive.
Fig. 3.
Bar charts illustrating the mean shear bond strength of different materials under different aging and bonding conditions. Error bars represent the standard deviation. NB stands for no bond application, SUA for the 3M Single Bond Universal Adhesive, and TUP + SUA for the Tokuyama Universal Primer followed by the 3M Single Bond Universal Adhesive application. 75% E/W stands for the 75% ethanol/water solution.
The failure analysis showed that the failure mode was mainly either adhesive or cohesive. Mixed failure was observed in a very small percentage of samples (Table 3). A total of 83.3% and 88.9% of the Duralay and CAD/CAM PMMA samples exhibited adhesive failure, respectively. The failure of Protemp 4 and Luxatemp Star was mainly cohesive. A total of 72.2% and 83.3% of the samples exhibited cohesive failure, respectively. The chi-square test showed the significant effect of the material type on the type of failure (p < 0.001). In addition, there was a significant correlation between the bonding condition and the type of failure (p = 0.001). SUA and TUP + SAU showed a more cohesive failure compared to NB (55.6%, 56.9%, and 25.8%, respectively). The relation between failure mode and aging condition was not significant (p = 0.247). Thus, the mode of failure was more reliant on the material type followed by the bonding condition, while storage condition tended to have no significant effect.
Table 3.
Failure mode of different experimental groups expressed in percentage.
| Material | Bonding Condition | Aging Condition |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Dry |
Water |
75% Ethanol/Water |
||||||||
| Adhesive failure | Cohesive failure | Mixed failure | Adhesive failure | Cohesive failure | Mixed failure | Adhesive failure | Cohesive failure | Mixed failure | ||
| Duralay | No Bond | 100 | 0 | 0 | 100 | 0 | 0 | – | – | – |
| SUA | 100 | 0 | 0 | 100 | 0 | 0 | 66.7 | 33.3 | 0 | |
| TUP + SUA | 66.7 | 33.3 | 0 | 33.3 | 66.7 | 0 | 100 | 0 | 0 | |
| CAD/CAM PMMA | NB | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 | 0 |
| SUA | 66.7 | 33.3 | 0 | 100 | 0 | 0 | 100 | 0 | 0 | |
| TUP + SUA | 100 | 0 | 0 | 100 | 0 | 0 | 33.3 | 66.7 | 0 | |
| Protemp 4 | NB | 16.7 | 50 | 33.3 | 66.7 | 33.3 | 0 | 66.7 | 33.3 | 0 |
| SUA | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 | |
| TUP + SUA | 0 | 100 | 0 | 0 | 100 | 0 | 66.7 | 33.3 | 0 | |
| Luxatemp Star | NB | 0 | 100 | 0 | 50 | 50 | 0 | 83.3 | 16.7 | 0 |
| SUA | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 | |
| TUP + SUA | 0 | 100 | 0 | 0 | 100 | 0 | 16.7 | 83.3 | 0 | |
NB: No bonding agent.
SUA: 3M Single Bond Universal Adhesive.
TUP + SUA: Tokuyama universal primer followed by a 3M Single Bond Universal Adhesive.
4. Discussion
In this study, the reparability of different temporary crown and bridge materials using a light-cure flowable resin composite was investigated by shear bond strength testing. The effect of aging and bonding agent application on shear bond strength was also assessed. The quantification of bond strength between a substrate and a repair material has been broadly used in dental material research to evaluate the success of the repair process. Although there is no consensus on the amount of clinically acceptable repair bond strength, the closer the bond strength is to the cohesive strength value of the repair material or the substrate, the more efficient is the repair. In this study, the surface of the substrate material was not mechanically treated or roughened prior to the repair because the aim was mainly to assess the effect of the material, aging, and bonding conditions. The samples were aged for 7 days prior to the repair to provide adequate time for the maximum monomer conversion of the substrate material and surface saturation with the storage medium (Asaoka and Hirano, 2003, Yan et al., 2010).
A light-cure flowable resin composite was chosen in the current study as the repair material for different substrates because it is a convenient and an easily controllable material during clinical application especially when the defect size is small (Bohnenkamp and Garcia, 2004). The selection of bonding agents was based on a popular universal adhesive that is usually directly applied to the substrate surface to enhance bonding. In addition, a universal primer bonding agent, which is applied to the surface prior to universal adhesive application, has been proposed by some manufactures; thus, its effect was also assessed.
In this study, a significantly higher shear bond strength and cohesive mode of failure was observed for bis-acrylic materials compared to PMMA-based materials when a flowable resin composite was used as the repair material. This is explained by the similarity in chemical composition between bis-acrylic materials and the flowable resin composite because both are composed of dimethacrylate monomers, which results in the formation of a strong chemical bond (Yanikoglu et al., 2002, Baur and Ilie, 2013, Jeong and Kim, 2019). A similar result was obtained in a previous study, which assessed the tensile bond strength of resin composite and PMMA CAD/CAM blocks with resin cements. The tensile bond strength with resin composite blocks was significantly higher than with PMMA blocks regardless of the surface conditioning method (Keul et al., 2013).
The use of a universal adhesive with or without a universal primer significantly increased the bond strength and the occurrence of cohesive failure especially for PMMA-based substrates. This can be explained by improved surface wettability and micro-entanglement with surface porosity by the low viscosity bonding agent (Puckett et al., 1991, Papazoglou and Vasilas, 1999). In addition, the use of a bonding agent may improve bonding with the subsequently added resin composite through the formation of a sticky oxygen-inhibited layer (Hisamatsu et al., 2002). Furthermore, it is possible that dimethacrylate monomers that are present in the adhesive may chemically bond with the PMMA substrate through reactive methacrylate groups and form strong covalent bonds (Cramer et al., 2010). This result is consistent with that in a previous study, which showed that bonding of air-abraded CAD/CAM PMMA materials and a resin composite cement was not achievable without additional surface treatment with adhesives (Baehr et al., 2013).
The CAD/CAM PMMA material is expected to show inferior shear bond strength compared to that achieved with conventional hand-mixed PMMA materials. The CAD/CAM blocks are prepared under optimum mixing and polymerization conditions, which results in higher material density, greater degree of conversion, and improved mechanical performance (Alt et al., 2011, Göncü Başaran et al., 2011, Stawarczyk et al., 2012). The high degree of conversion means that there are few remaining double bonds available for chemical interaction with the repair material, which may result in weaker repair bond strength (Balkenhol et al., 2007, Dall'Oca et al., 2007). This is confirmed by the results of the current study because the CAD/CAM PMMA material exhibited lower shear bond strength values compared to those of conventional PMMA material.
In this study, storage in water resulted in shear bond strength values that were generally not significantly different from those of the control (dry) group. However, storage in a 75% ethanol/water solution tended to decrease the bond strength probably owing to the swelling effect of the substrate, which may have resulted in a smoother surface (Ferracane, 2006). This has not been previously investigated; however, the effect of aging on resin composite repair was assessed in a previous study using three different aging procedures including thermocycling (5000 cycles at the temperature between 5 °C and 55 °C), storage in boiling water for 8 h, and immersion in citric acid for 1 week. It was determined that only thermocycling significantly reduced the bond strength (Özcan et al., 2007).
Considering the limitations of in vitro assessment, the results obtained in this study suggest that the repair of the bis-acrylic temporary crown and bridge materials with a flowable resin composite is a reliable approach even after a period of aging in the oral cavity especially when a suitable bonding agent is applied. However, considering other factors (e.g., the effect of thermocycling and natural saliva), mechanical surface treatment may be advantageous prior to the repair to improve the bond strength, as has been shown in previous studies. The repair of PMMA-based materials using a flowable resin composite is not recommended because it demonstrated a significantly lower bond strength (compared to bis-acrylic materials) and predominantly an adhesive mode of failure. However, this approach may be applicable for the repair of small size defects using a suitable bonding agent to improve the bond strength.
5. Conclusions
The shear bond strength using a light-cure flowable resin composite as a repair material is significantly higher with bis-acryl compared to PMMA-based substrates. The effect of aging in water on bond strength is not significant compared to dry aging, while aging in a 75% ethanol/water solution tends to have a negative effect. The application of bonding agents positively affects the repair strength especially for polymethylmethacrylate-based substrates.
CRediT authorship contribution statement
Ruwaida Z. Alshali: Conceptualization, Methodology, Formal analysis, Supervision, Writing - review & editing. Dalea M. Bukhary: Writing - review & editing. Mohammed A. AlQahtani: Conceptualization, Resources, Writing - review & editing. Naflaa O. Alenazi: Investigation, Resources, Writing - original draft. Abeer H. Alzahrani: Investigation, Resources, Writing - original draft. Hayam A. Alobaid: Investigation, Resources, Writing - original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
The authors are grateful to the Advanced Dental Research Laboratory Centre of King Abdulaziz University (Jeddah, Saudi Arabia) and to all involved personnel who contributed in this research.
*This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Peer review under responsibility of King Saud University.
References
- Alt V., Hannig M., Wöstmann B., Balkenhol M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent. Mater. 2011;27:339–347. doi: 10.1016/j.dental.2010.11.012. [DOI] [PubMed] [Google Scholar]
- Asaoka K., Hirano S. Diffusion coefficient of water through dental composite resin. Biomaterials. 2003;24:975–979. doi: 10.1016/s0142-9612(02)00435-0. [DOI] [PubMed] [Google Scholar]
- Baehr N., Keul C., Edelhoff D., Eichberger M., Roos M., Gernet W., Stawarczyk B. Effect of different adhesives combined with two resin composite cements on shear bond strength to polymeric CAD/CAM materials. Dent. Mater. J. 2013;32:492–501. doi: 10.4012/dmj.2012-329. [DOI] [PubMed] [Google Scholar]
- Balkenhol M., Ferger P., Mautner M.C., Wöstmann B. Provisional crown and fixed partial denture materials: mechanical properties and degree of conversion. Dent. Mater. 2007;23:1574–1583. doi: 10.1016/j.dental.2007.06.024. [DOI] [PubMed] [Google Scholar]
- Balkenhol M., Meyer M., Michel K., Ferger P., Wöstmann B. Effect of surface condition and storage time on the repairability of temporary crown and fixed partial denture materials. J. Dent. 2008;36:861–872. doi: 10.1016/j.jdent.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Baur V., Ilie N. Repair of dental resin-based composites. Clin. Oral Investig. 2013;17:601–608. doi: 10.1007/s00784-012-0722-4. [DOI] [PubMed] [Google Scholar]
- Bektas Ö.Ö., Eren D., Siso S.H., Akin G.E. Effect of thermocycling on the bond strength of composite resin to bur and laser treated composite resin. Laser Med. Sci. 2012;27:723–728. doi: 10.1007/s10103-011-0958-2. [DOI] [PubMed] [Google Scholar]
- Bohnenkamp D.M., Garcia L.T. Repair of bis-acryl provisional restorations using flowable composite resin. J. Prosthet. Dent. 2004;92:500–502. doi: 10.1016/j.prosdent.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Cramer N.B., Couch C.L., Schreck K.M., Boulden J.E., Wydra R., Stansbury J.W., Bowman C.N. Properties of methacrylate–thiol–ene formulations as dental restorative materials. Dent. Mater. 2010;26:799–806. doi: 10.1016/j.dental.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dall'Oca S., Papacchini F., Goracci C., Cury Á.H., Suh B.I., Tay F.R., Polimeni A., Ferrari M. Effect of oxygen inhibition on composite repair strength over time. J. Biomed. Mater. Res. B Appl. Biomater. 2007;81:493–498. doi: 10.1002/jbm.b.30689. [DOI] [PubMed] [Google Scholar]
- Ferracane J.L. Hygroscopic and hydrolytic effects in dental polymer networks. Dent. Mater. 2006;22:211–222. doi: 10.1016/j.dental.2005.05.005. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration, 1976. FDA Guidelines for Chemistry and Technology Requirements of Indirect Additive Petitions. Washington, DC: FDA
- Göncü Başaran E., Ayna E., Vallittu P.K., Lassila L.V. Load-bearing capacity of handmade and computer-aided design–computer-aided manufacturing-fabricated three-unit fixed dental prostheses of particulate filler composite. Acta. Odontol. Scand. 2011;69:144–150. doi: 10.3109/00016357.2010.545034. [DOI] [PubMed] [Google Scholar]
- Ha S.R., Kim S.H., Lee J.-B., Han J.-S., Yeo I.-S. Improving shear bond strength of temporary crown and fixed dental prosthesis resins by surface treatments. J. Mater. Sci. 2016;51:1463–1475. [Google Scholar]
- Hisamatsu N., Atsuta M., Matsumura H. Effect of silane primers and unfilled resin bonding agents on repair bond strength of a prosthodontic microfilled composite. J. Oral Rehabil. 2002;29:644–648. doi: 10.1046/j.1365-2842.2002.00899.x. [DOI] [PubMed] [Google Scholar]
- Jeong K.W., Kim S.H. Influence of surface treatments and repair materials on the shear bond strength of CAD/CAM provisional restorations. J. Adv. Prosthodont. 2019;11:95–104. doi: 10.4047/jap.2019.11.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keul C., Martin A., Wimmer T., Roos M., Gernet W., Stawarczyk B. Tensile bond strength of PMMA-and composite-based CAD/CAM materials to luting cements after different conditioning methods. Int. J. Adhes. Adhes. 2013;46:122–127. [Google Scholar]
- Moran J.M. Chemical plaque control–prevention for the masses. Periodontology. 1997;15:109–117. doi: 10.1111/j.1600-0757.1997.tb00110.x. [DOI] [PubMed] [Google Scholar]
- Özcan M., Barbosa S.H., Melo R.M., Galhano G.A.P., Bottino M.A. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent. Mater. 2007;23:1276–1282. doi: 10.1016/j.dental.2006.11.007. [DOI] [PubMed] [Google Scholar]
- Papazoglou E., Vasilas A.I. Shear bond strengths for composite and autopolymerized acrylic resins bonded to acrylic resin denture teeth. J. Prosthet. Dent. 1999;82:573–578. doi: 10.1016/s0022-3913(99)70056-9. [DOI] [PubMed] [Google Scholar]
- Puckett A., Holder R., O'Hara J. Strength of posterior composite repairs using different composite/bonding agent combinations. Oper. Dent. 1991;16:136–140. [PubMed] [Google Scholar]
- Rasmussen S.T. Analysis of dental shear bond strength tests, shear or tensile? Int. J. Adhes. Adhes. 1996;16:147–154. [Google Scholar]
- Stawarczyk B., Ender A., Trottmann A., Özcan M., Fischer J., Hämmerle C.H. Load-bearing capacity of CAD/CAM milled polymeric three-unit fixed dental prostheses: effect of aging regimens. Clin. Oral Investig. 2012;16:1669–1677. doi: 10.1007/s00784-011-0670-4. [DOI] [PubMed] [Google Scholar]
- Wendler M., Belli R., Panzer R., Skibbe D., Petschelt A., Lohbauer U. Repair bond strength of aged resin composite after different surface and bonding treatments. Materials. 2016;9:547. doi: 10.3390/ma9070547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiegand A., Stucki L., Hoffmann R., Attin T., Stawarczyk B. Repairability of CAD/CAM high-density PMMA-and composite-based polymers. Clin. Oral Investig. 2015;19:2007–2013. doi: 10.1007/s00784-015-1411-x. [DOI] [PubMed] [Google Scholar]
- Yan Y., Kim Y., Kim K., Kwon T. Changes in degree of conversion and microhardness of dental resin cements. Oper. Dent. 2010;35:203–210. doi: 10.2341/09-174-L. [DOI] [PubMed] [Google Scholar]
- Yanikoglu D.N., Duymus D.Z., Bayindir D.F. Comparative bond strengths of autopolymerising denture resin and light cured composite resin to denture teeth. Int. Dent. J. 2002;52:20–24. doi: 10.1111/j.1875-595x.2002.tb00592.x. [DOI] [PubMed] [Google Scholar]