Abstract
Objective
To compare the translucency and masking of zirconia-reinforced lithium silicate with lithium disilicate glass-ceramic and hybrid composite.
Materials and methods
One hundred and twenty disc-shaped specimens were fabricated using Enamic, Celtra Duo, IPS E.max CAD, and Suprinity. Twelve groups were prepared according to material type and thickness (0.5, 1.0, and 1.5 mm). The specimens were tested over five substrates: composite resin-A3.5 shade (A3.5 control group), zirconia-A1 shade (ZR), nickel–chromium alloy (NC), black (B), and white (W). A spectrophotometer operating at wavelengths from 360 to 750 nm and a view-area size of 9.53 mm was used for color measurement.
Results
Mean color difference values (ΔΕ) were found to be lowest in Suprinity and highest in IPS E.max. CAD. Color difference values were significantly related to substrate shade. The A3.5 substrate revealed the significantly lowest ΔΕ values of all the substrates (P = 0.05). Regarding the translucency parameters for ceramics of different thicknesses, a significant difference was observed among all groups except in Suprinity.
Conclusions
Different ceramic types with different thicknesses and substrate strongly affect translucency and masking.
Clinical significance
Fabricating durable aesthetic restorations that also meets patients’ expectations is among the most significant challenges in dentistry. With high demand for more natural restorations, ceramics based on computer-aided design (CAD) and computer-aided manufacture (CAM) became popular and exhibited excellent results. However, various factors such as abutment shade, luting cement color, and ceramic type, thickness, and translucency may affect the prosthesis shade. The objective of this study was to evaluate the effects of these factors on the final shades of CAD/CAM-based ceramic restorations.
Keywords: Ceramics, CAD/CAM ceramics, Translucency, Ceramic thickness, Color masking, Substrates
1. Introduction
As the global demand for cosmetic dental treatment has risen, the variety of available ceramic material to achieve the most aesthetically desirable outcomes has increased.
The term “ceramic” denotes a class of products prepared from non-metallic, inorganic materials by firing and sintering at high temperatures with highly pressurized gas. The term “porcelain” refers to a mixture of components such as kaolin, quartz, and feldspar fired at high temperatures to achieve coalescence.
Metal-free ceramic restorations were introduced in 1965 when McLean and Hughes used an aluminous porcelain inner core (40–50% alumina crystals) in porcelain jacket crowns (Juntavee and Attashu, 2018). However, the use of this material (in its monolithic form) was restricted only to the anterior teeth region, as it lacked sufficient mechanical properties and lower flexural strength. Other drawbacks included the lack of sufficient translucency, color mismatches, and patient concerns. However, recently introduced monolithic lithium dioxide and zirconia prostheses supported by high-strength cores be can be used in the posterior regions (metal or ceramic) (Helvey, 2014) as well. Thus, to overcome the mechanical and aesthetic drawbacks of conventional of dental ceramics, a wide range of metal-free ceramics have been introduced using various fabrication techniques, including computer-aided design (CAD) and computer-aided manufacture (CAM) technology (Oh et al., 2018).
The first commercially available CAD/CAM system, CEREC, was developed in the mid-1980s by Davidowitz and Kotick (2011). Their machinable ceramic technique allowed the production of full-contoured restorations as well as single- or multiple-unit frameworks using a computer scanner, designing unit, and a milling machine for the clinicians to fabricate dental ceramic restoration in a single appointment (the so-called “chairside” procedure) (Sannino et al., 2014).
With the evolution of CAD/CAM systems, contemporary ceramic materials now possess enhanced aesthetics, have wear rates similar to enamel, and are durable enough for fabricating full crowns and bridges, providing durable, high-quality restorations (Sannino et al., 2014).
All-ceramic restorations are attractive prosthodontic options for clinicians due to their excellent biocompatibility, life-like aesthetic properties and translucency, long-term color stability, and high wear resistance (Conrad et al., 2007, Ahmed, 2019) in addition to being excellent thermal and electrical insulators. The chemical inertness of all-ceramic systems is also an essential advantage, since they do not release toxic, harmful compounds to neighboring tissues, thereby reducing the risk of developing surface roughness and/or bacterial adhesion. On the other hand, dental ceramics are inherently brittle and may cause considerable wear of opposing dentition, leading to clinical failures of prostheses (Christensen, 1999, Anusavice et al., 2003, Sadowsky, 2006). Despite the high cost of all-ceramic restorations and the need for an experienced dental ceramic technician and expensive milling machines, the rising cost of precious metals used in metal-ceramic restorations have made metal-free ceramic restorations competitive with metal-ceramic restorations (Anusavice et al., 2003, Sadowsky, 2006).
Ceramic crowns have been used for the last four decades to overcome the aesthetic limitations of porcelain fused to metal crowns. Ceramics are made from various materials with various techniques, each combination of which exhibits unique physical and behavioral properties. Historically, the first metal-free crowns were resin-based, but these were soon abandoned because they lacked sufficient mechanical properties. In dental practice, newer metal-free crowns are increasingly available using a wide range of available ceramic materials. Monolithic alumina and zirconia are common, but sufficient data from clinical and in vitro studies regarding these materials is lacking (Minguez and Lyons, 2007, Zarone et al., 2011)
Many factors including but not limited to ceramic type, number of firing cycles (Tabatabaei et al., 2019), thickness, translucency, luting resin cement shade (Bacchi et al., 2019), and supporting substrate color (Seyidaliyeva et al., 2020) all play integral roles in determining the final shades of ceramic crowns. Translucency is one of the most significant factors, however (Zarone et al., 2011). The dominant color of natural teeth is the consequence of the light reflected by dentin and absorbed and scattered by enamel (Seghi et al., 1986, Juntavee and Attashu, 2018). The shade of the underlying dentin determines the shade of the natural tooth due to the high transparency of the enamel. The incisal and interproximal portions of natural teeth show higher translucency due to their lack of underlying dentin.
Many studies have used translucency parameters (TPs) and contrast ratios to measure the translucency of dental porcelain and the variation of thickness regarding white and black backgrounds (Johnston et al., 1995, Liu et al., 2010). Crystals in ceramic matrices tend to control the relative amount of light absorbed, reflected, and transmitted owing to their chemical nature, size, and number relative to the wavelength of the source light (Heffernan et al., 2002). The higher the number of crystals in a glassy matrix, the lower the translucency of the ceramic. Zirconia dioxide has the highest opacity owing to the absence of a glass matrix and a higher number of crystals.
Various properties of ceramics, such as translucency and opalescence, play critical roles in achieving life-like aesthetics when replacing natural dentition. Consequently, there has been an immense upsurge worldwide in the use of all-ceramic restorations for the aesthetic replacement of missing teeth (Heffernan et al., 2002). Among all-ceramic crowns, zirconia shows optimal physical and mechanical properties, making zirconia restoration clinically popular for full contour crowns, fixed partial dentures, and implant abutments. However, the translucency of zirconia remains a significant drawback, especially in replacing anterior teeth. Thus, the development of more translucent zirconia is a goal in prosthetic dentistry. Furthermore, supporting substrates that may shift colors, such as cast metal cores and endodontically treated teeth, also play roles in determining the final colors of ceramic restorations (Vichi et al., 2011).
To mask discolored teeth, clinicians use less translucent ceramic to mimic natural teeth’s appearance, a phenomenon known as “masking ability.” The masking ability of restorative materials is evaluated by measuring the color difference (ΔE) in the CIELab color system, which uses spectrophotometry that can detect even minute color change undetectable by the naked eyes using color attributes of lightness (L*), red/green value (a*), and yellow/blue value (b*).
This formula calculates ΔE to determine the differences between colors (Tabatabaian et al., 2019):
where ΔE is close to zero for ideal masking ability.
More recently, developments in the fabrication and changes in the microstructure of zirconia have generated zirconia restorations with higher translucency, such as Suprinity (VITA Zahnfabrik, Bad Sackingen, Germany), which is zirconia-reinforced lithium silicate (ZLS) ceramic (approx. 10 wt%). This material exhibits excellent durability and consistently high load capacity owing to its structural characteristics, special fine-grained fillers, and homogeneous matrix. It also exhibits outstanding aesthetic properties, such as excellent translucency, fluorescence, and opalescence (Sannino et al., 2014). Another recently introduced ZLS material is Celtra Duo (Dentsply, PA, US).
A significant color difference between the background and the control requires greater ceramic thickness of ceramic for ideal masking ability. The optimal thickness for A1 and A3.5 resin composite as well as zirconia (ZR) is 0.4 mm, while 0.8 mm is optimal for for nickel–chromium alloy (NC) and more than 0.8 mm for black (B), and white (W).
Church (2016) compared four high-translucency monolithic zirconia oxide materials to high-translucency lithium disilicate glass-ceramic. At similar thicknesses, they found that lithium disilicate was less translucent; on the other hand, highly translucent zirconia was as translucent as lithium disilicate.
In another study, Choi and Razzoog (2013) found that the concealing potential of zirconia had higher ΔE values on black backgrounds than lighter, tooth-colored backgrounds. Wang et al. (2013) concluded that zirconia was less sensitive to changes in thickness than glass ceramics.
Suputtamongkol et al. (2013) concluded that the color of the most commonly used background core structure affected the final shade of zirconia-based restorations after measuring ΔE and discovering minor variations in the color of zirconia crowns. Hence, it appears that substrates are not entirely masked by zirconia crowns.
Currently, few studies have evaluated the translucency and masking potential of new zirconia-based dental restorations. This study therefore aims to compare the translucency and masking ability of ZLS to lithium disilicate glass-ceramic and hybrid composites. The null hypotheses of this study are the following: (1) There is no difference in the translucency of the tested ceramic materials with different thicknesses and backgrounds and (2) there is no difference in the color-masking ability of the tested ceramic materials with different thicknesses and backgrounds. The alternative hypotheses are the following: (1) There is a difference in the degree of translucency of the tested ceramic materials with different thicknesses and backgrounds and (2) there is a difference in the color-masking ability of the tested ceramic materials with different thicknesses and backgrounds.
2. Materials and methods
Four ceramic materials were used to prepare 120 disc-shaped specimens: (1) polymer-infiltrated ceramic (ENAMIC) (Vita Zahnfabrik, Bad Saeckingen, Germany), (2) lithium disilicate crystals embedded in a glassy matrix (IPS E.Max CAD) (Ivoclar Vivadent, Schaan, Liechtenstein), (3) Celtra Duo (Dentsply, PA, US), and (4) Suprinity (VITA Zahnfabrik, Bad Sackingen, Germany). Each group consisted of 30 specimens, which were further distributed into three subgroups (n = 10) according to thickness (0.5, 1.0, and 1.5 mm), yielding a total of 12 groups.
The specimens were tested over five substrates: A3.5 shade composite resin (A3.5), A1 shade zirconia (ZR), nickel–chromium alloy (NC), black (B), and white (W). A spectrophotometer (Ultrascan XE, HunterLab, Reston, VA, USA) was used for color measurement at wavelengths from 360 to 750 nm and a view-area size of 9.53 mm.
2.1. Fabrication of ceramic specimens
An ISOMET 2000 precision saw was used to cut blocks into 10-mm diameter discs with the three thicknesses specified above. IPS E.max CAD specimens were sintered following the manufacturer’s instructions and then adjusted using an adjustment and polishing kit (an Automata grinding and polishing unit) to achieve the desired thicknesses (±0.05 mm). Specimens with excessively high or low thicknesses were not selected for testing. Subsequently, the specimens were cleaned with 98% ethyl alcohol and dried using compressed air.
2.2. Fabrication of backgrounds
Background discs were 10 mm in diameter and thickness. Control specimens for resin backgrounds were incrementally prepared with multiple layers of a microhybrid composite resin (Z250; 3 M ESPE) using a plastic mold. A Blue Phase G2 curing unit with an 800 mW/cm2 intensity was used to polymerize resin increments for 40 s. All fabricated resin specimens were then polished using 800-grit silicon carbide abrasive papers.
Using a designing software, a special cylindrical pattern was applied to prepare ZR specimens to be milled from blanks using a milling machine, liquated in an A2 shade liquid for 10 s, and sintered at 1520 °C for 12 h. The same techniques were used to mill white and black polytetrafluoroethylene (PTFE) materials (Teflon; Omnia Plastica SpA) for fabricating the W and B backgrounds. The acrylic resin mold (Duralay; Reliance Dental Mgf Co.) was then cast in an NC alloy (VeraBond V; Aalba Dent, Inc.) to prepare cast-metal backgrounds and was subsequently polished using a base-metal polishing kit (Coral Stones; Shofu Inc.). Specimens were washed and rinsed in an ethanol solution and subsequently air-dried.
2.3. Color measurements
A commercial polyvinyl siloxane (PVS) impression material (Chromaclone™ PVS, Ultradent, UT, US) was adapted around the spectrophotometer to reject surrounding light, ensure optimal background seating, and replicate uniform testing parameters for all groups. The specimens were then positioned on the backgrounds without an underlying medium, and the CIELab values (L∗, brightness; a∗, red-green value; and b∗, yellow-blue value) of the specimens were measured (Coloreye 7000A spectrophotometer). Three measurements were made for each sample using each background. Color change values were recorded and compared with the CIELab values of each specimen on the selected background.
The equation used to measure ΔE was the following:
To evaluate masking ability, threshold values for acceptability (ΔE = 5.5) and perceptibility (ΔE = 2.6) were assumed in order. After measuring CIELab values, the TPs of the samples at different thicknesses were calculated using the following equation:
where TP refers to the translucency parameter and W and B refer to the shade value of each specimen on white backing and black backgrounds, respectively.
2.4. Statistical analysis
The obtained data were subjected to statistical analyses using two-way analysis of variance (ANOVA) with Tukey’s post hoc multiple comparison between groups. A P-value equal to or less than 0.05 was deemed statistically significant. The software utilized for statistical analysis was Statistical Package for the Social Sciences (SPSS), version 20.0 (SPSS, International Business Machines (IBM) Inc., Chicago, IL, US).
3. Results
Table 1 shows the ΔΕ values of each CAD/CAM ceramic and substrate thickness.
Table 1.
Δ E for Different CAD/CAM Ceramics and Thicknesses on Translucency and Color Masking of Different Substrates.
| A3.5 |
Black |
P1 value | White |
P2 value | Nickel chromium |
P3 value | Zirconia |
P4 value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||
| ENA | ||||||||||||||
| 0.5 mm | 1.07 | 0.67 | 1.73 | 0.95 | <0.001* | 2.73 | 1.93 | <0.001* | 2.18 | 1.33 | <0.001* | 2.52 | 1.51 | <0.001* |
| 1 mm | 0.72 | 0.81 | 0.78 | 0.92 | 0.550 | 1.31 | 1.00 | <0.001* | 0.96 | 1.03 | 0.002* | 1.27 | 1.13 | <0.001* |
| 1.5 mm | 0.50 | 0.38 | 1.47 | 0.59 | <0.001* | 1.26 | 0.58 | <0.001* | 0.62 | 0.42 | 0.027* | 0.79 | 0.49 | <0.001* |
| MAX | ||||||||||||||
| 0.5 mm | 0.70 | 0.31 | 1.12 | 0.71 | <0.001* | 1.08 | 0.64 | 0.001* | 0.64 | 0.37 | 0.183 | 0.81 | 0.58 | 0.215 |
| 1 mm | 0.73 | 0.50 | 0.77 | 0.43 | 0.429 | 1.30 | 0.58 | <0.001* | 0.89 | 0.44 | 0.038* | 1.05 | 0.48 | <0.001* |
| 1.5 mm | 0.46 | 0.32 | 0.45 | 0.35 | 0.776 | 0.81 | 0.58 | 0.001* | 0.51 | 0.33 | 0.257 | 0.42 | 0.33 | 0.428 |
| SUP | ||||||||||||||
| 0.5 mm | 1.39 | 1.21 | 2.59 | 2.73 | 0.001* | 0.82 | 0.94 | 0.029* | 3.11 | 3.71 | 0.003* | 0.70 | 0.31 | 0.003* |
| 1 mm | 0.86 | 0.62 | 2.07 | 1.85 | <0.001* | 1.08 | 0.65 | 0.076 | 2.14 | 1.62 | <0.001* | 0.92 | 0.42 | 0.581 |
| 1.5 mm | 4.48 | 2.72 | 3.47 | 2.55 | <0.001* | 3.01 | 2.04 | <0.001* | 1.57 | 0.88 | <0.001* | 1.63 | 1.04 | <0.001* |
| CEL | ||||||||||||||
| 0.5 mm | 1.15 | 0.67 | 1.61 | 0.98 | <0.001* | 1.42 | 0.88 | 0.165 | 1.15 | 0.65 | 0.983 | 1.24 | 0.79 | 0.567 |
| 1 mm | 1.37 | 0.69 | 1.34 | 0.73 | 0.598 | 1.02 | 0.68 | 0.001* | 3.20 | 12.01 | 0.413 | 1.18 | 0.63 | 0.027* |
| 1.5 mm | 1.36 | 0.85 | 1.16 | 0.80 | 0.045* | 1.02 | 0.69 | <0.001* | 1.06 | 0.76 | 0.002* | 0.77 | 0.62 | <0.001* |
P value was calculated between A3.5 & Black.
P value was calculated between A3.5 & White.
P value was calculated between A3.5 & Nickel chromium.
P value was calculated between A3.5 & Zirconia.
Regarding masking ability, ΔΕ values were lowest in the Suprinity (SUP) group and Enamic (ENA) group followed by Celtra Duo (CEL) and were highest in the IPS E.Max CAD(MAX) group (Fig. 1, Fig. 2, Fig. 3, Fig. 4).
Fig. 1.

Mean ΔE of ENA for different backgrounds and thicknesses.
Fig. 2.

Mean ΔE of MAX for different backgrounds and thicknesses.
Fig. 3.
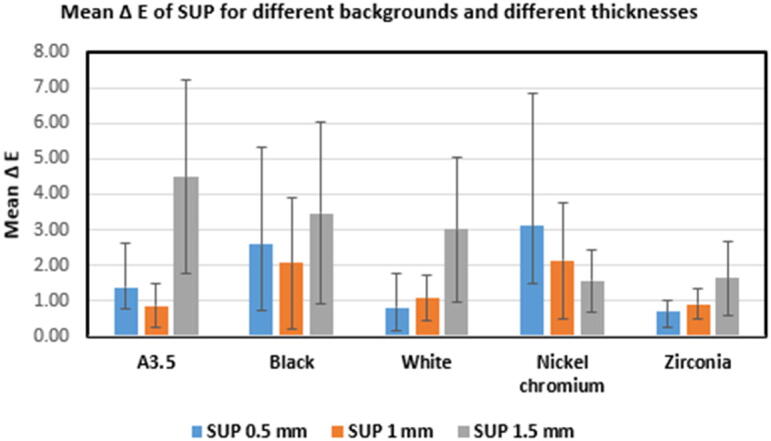
Mean ΔE of SUP for different backgrounds and thicknesses.
Fig. 4.
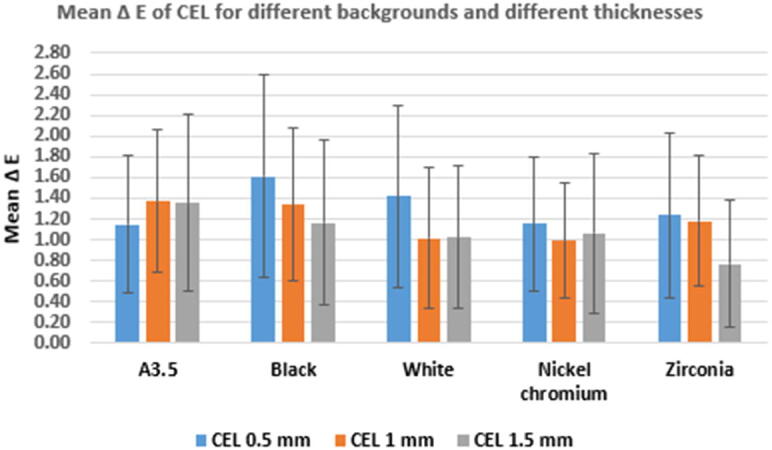
Mean ΔE of CEL for different backgrounds and thicknesses.
Substrate shade was significantly related to ΔΕ value. The A3.5 substrate revealed the lowest color difference values, while NC and zirconia were less likely to show color difference values. On white and black, the values were close. The reference A3.5 substrate group presented significantly lower values (P = 0.05).
The ΔΕ values among tested materials were the following (Table 2):
-
(a)
Between A3.5 and black: SUP < CEL < ENA < MAX
-
(b)
Between A3.5 and white: SUP < ENA < CEL < MAX
-
(c)
Between A3.5 and Nickel chromium: SUP < ENA < CEL < MAX
-
(d)
Between A3.5 and zirconia: ENA < SUP < CEL < MAX
-
(e)
TP: ENA < MAX < CEL < SUP
Table 2.
Δ E for Different CAD/CAM Ceramics on Translucency and Color Masking of Different Substrates.
| A3.5 |
Black |
P1 value | White |
P2 value | Nickel chromium |
P3 value |
Zirconia |
P4 value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||
| ENA | 0.77 | 0.68 | 1.33 | 0.92 | <0.001* | 1.77 | 1.46 | <0.001* | 1.26 | 1.20 | <0.001* | 1.53 | 1.33 | <0.001* |
| MAX | 0.63 | 0.40 | 0.78 | 0.59 | 0.002* | 1.06 | 0.63 | <0.001* | 0.68 | 0.41 | 0.142 | 0.76 | 0.54 | 0.003* |
| SUP | 2.24 | 2.36 | 2.71 | 2.45 | 0.013 | 1.63 | 1.66 | <0.001* | 2.28 | 2.45 | 0.915 | 1.08 | 0.78 | <0.001* |
| CEL | 1.29 | 0.74 | 1.37 | 0.85 | 0.213 | 1.15 | 0.77 | 0.078 | 1.07 | 0.66 | <0.001* | 1.06 | 0.71 | 0.002* |
P value was calculated between A3.5 & Black.
P value was calculated between A3.5 & White.
P value was calculated between A3.5 &Nickel chromium.
P value was calculated between A3.5 &Zirconia.
Regarding the TPs of ceramics with different thicknesses, ENA, MAX, and CEL exhibited significant differences, while no significant difference was observed for SUP (Table 3).
Table 3.
TP for Ceramic by different thickness.
| 0.5 mm |
1 mm |
P1 value | 1.5 mm |
P2 value | P3 value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||||
| ENA | 20.28 | 2.43 | 13.62 | 0.92 | <0.001* | 10.29 | 0.50 | <0.001* | <0.001* |
| MAX | 21.33 | 1.73 | 13.35 | 0.59 | <0.001* | 10.28 | 0.42 | <0.001* | <0.001* |
| SUP | 42.49 | 4.26 | 42.28 | 2.79 | 0.825 | 43.25 | 4.47 | 0.498 | 0.316 |
| CEL | 23.94 | 1.79 | 14.81 | 0.52 | <0.001* | 10.39 | 0.48 | <0.001* | <0.001* |
P value was calculated between 0.5 mm & 1 mm.
P value was calculated between 0.5 mm & 1.5 mm.
P value was calculated between1 mm & 1.5 mm.
Higher TP was related to thinner material; a thickness of 0.5 mm showed significantly higher translucency than 1 mm and 1.5 mm (Table 3).
Table 4 shows the TPs of different thicknesses by ceramic type. There was significant difference between ENA and SUP, followed by MAX and SUP, SUP and CEL, MAX and CEL, and ENA and CEL, with no significant difference between ENA and MAX.
Table 4.
TP for different thickness by Ceramic.
| ENA |
MAX |
P1 value | SUP |
P2 value | CEL |
P3 value | P4 value | P5 value | P6 value | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||||
| 0.5 mm | 20.28 | 2.43 | 21.33 | 1.73 | 0.059 | 42.49 | 4.26 | <0.001* | 23.94 | 1.79 | <0.001* | <0.001* | <0.001* | <0.001* |
| 1 mm | 13.62 | 0.92 | 13.35 | 0.59 | 0.182 | 42.28 | 2.79 | <0.001* | 14.81 | 0.52 | <0.001* | <0.001* | <0.001* | <0.001* |
| 1.5 mm | 10.29 | 0.50 | 10.28 | 0.42 | 0.936 | 43.25 | 4.47 | <0.001* | 10.39 | 0.48 | 0.442 | <0.001* | 0.358 | <0.001* |
P value was calculated between ENA & MAX.
P value was calculated between ENA & SUP.
P value was calculated between ENA & CEL.
P value was calculated between MAX & SUP.
P value was calculated between MAX & CEL.
P value was calculated between SUP & CEL
4. Discussion
Color tends to strongly influence the appearances of dental restorations. Surface roughness, glossiness, and translucency also contribute to the overall aesthetics of dental prostheses (O'Brien et al., 1984). The human eye easily detects slight changes in color but is less capable of matching objects (Douglas and Brewer, 1998). Consequently, shade matching poses difficulties for dental technicians fabricating dental prostheses. The synchronization of ceramic shade with human teeth is even more difficult due to light from underlying background color. Hence, alteration in the backgrounds and thicknesses of ceramics can alter final outcomes (Yeh et al., 1982).
The present study utilized white, black, NC, A3.5 shade composite, and zirconia for backgrounds with varying specimen thicknesses. Various studies have evaluated the influence exerted by ceramic thickness on translucency, and results generally show greater translucency with thinner ceramics. This influence is more evident in high-glass ceramics (Yeh et al., 1982).
Table 1 shows the ΔΕ value of each CAD/CAM ceramic with different thicknesses and substrates. MAX specimens with thicknesses of 0.5, 1, and 1.5 mm had the highest masking ability among CEL, ENA, and Suprinity, demonstrating that masking ability depends on ceramic thickness and composition.
A3.5 shade composite background was selected to mimic natural dentin color and was used as a control group. It turned out that A3.5 was the best background material, followed by zirconia, white, NC, and black. Not all ceramic types and thicknesses effectively masked the black background. These results agree with the findings of Shono and Nahedh (2012), who showed that no tested ceramics could entirely conceal a black background. However, color-masking ability was enhanced when thickness was increased from 1.0 to 1.5 mm(Shono and Alnahedh, 2012).
It is vital to consider the limitations of ceramics. First, different materials have different microstructures. Second, thicker ceramic tends to mask better than thinner ceramic. Third, the substrate color affects the final color outcome (Sethakamnerd, 2017).
Therefore, the colors of artificial teeth are essential factors in ceramic selection. In clinical settings, non-discolored teeth should be restored with more translucent ceramic, while tooth discoloration or metal posts demand the use of opaquer material. Minor changes in thickness should be advocated when highly translucent ceramics are used for fabricating thin restorations, since they enhance the aesthetic outcomes of final restorations (Helvey, 2014).
Translucency, which a state of partial opacity, is the extent to which an object prevents or allows any background color to alter the final shade or color of prosthesis (Johnston et al., 1995).
In our study, the TP value of SUP was significantly higher than the other ceramics, CEL, ENA, and MAX. When thickness increased from 0.5 to 1.5 mm, the translucency decreased. SUP contained zirconia, which affected the translucency of the material (Fig. 5). Also, no significant differences were observed between the TPs of SUP, while significant differences existed in ENA, MAX, and CEL.
Fig. 5.
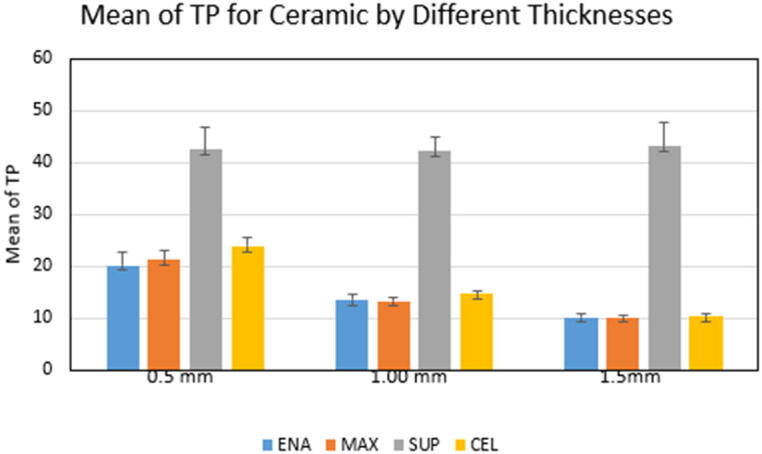
Mean TP of ceramics by thickness.
These findings agree with those of previous studies that have reported strong correlations between thickness and translucency. Wang et al. (2013) measured the TPs of zirconia and glass-based ceramics at different thicknesses, indicating that both materials and their thicknesses affect the translucency of the ceramic restorations. For instance, the thickness of monolithic zirconia tends to affect its final color, requiring a minimum thickness of 0.9 mm to achieve acceptable aesthetics (Tabatabaian et al., 2017).
5. Conclusions
Considering the limitations of this study, the following can be concluded:
-
1.
Translucency and masking abilities are affected by ceramic material types and thicknesses.
-
2.
Masking abilities are affected by background colors.
-
3.
IPS E.MAX CAD exhibited the highest masking ability and Suprinity the least.
-
4.
The underlying black substrate was not totally masked by any tested ceramic.
The masking ability of ceramics tends to improve with greater thickness, while translucency improves with less thickness.
Ethical Statement
The research was conducted in King Saud University using samples not requiring an ethical approval.
CRediT authorship contribution statement
Abdullah Saeed Alayad: Conceptualization, Methodology, Writing - review & editing. Abdulaziz Alqhatani: Writing - original draft. Mohammed S. Alkatheeri: Writing - original draft. Mohammed Alshehri: Visualization, Investigation. Mohammed A. AlQahtani: Writing - original draft. Aljoharah Ebrahim Bin Osseil: Data curation, Project administration, Resources. Rawan Abdullah Almusallam: Data curation, Project administration, Resources.
Acknowledgments
Acknowledgements
The authors extend their appreciation to the Deanship of Scientific Research and the College of Dentistry Research Center (CDRC), King Saud University, Riyadh, Saudi Arabia.
Permission Note
This letter confirms that this paper has been submitted solely to The Saudi Dental Journal and that it is not concurrently under consideration for publication in another journal. This letter also confirms that the submitted work, including images, are original.
Disclosure statement
The authors do not have any financial interest in the companies whose materials are included in this article.
Place of Research
Biomaterial Laboratory, college of dentistry, King Saud University, Riyadh, Kingdom of Saudi Arabia.
Footnotes
Peer review under responsibility of King Saud University.
References
- Ahmed H.J. Craig's restorative dental materials. Br. Dent. J. 2019;226(1):9. [Google Scholar]
- Anusavice K.J., Shen C., Rawls H. Saunders; St. Louis, Missouri: 2003. Phillips' Science of Dental Materials. [Google Scholar]
- Bacchi A., Boccardi S., Alessandretti R., Pereira G.K.R. Substrate masking ability of bilayer and monolithic ceramics used for complete crowns and the effect of association with an opaque resin-based luting agent. J. Prosthodontic Res. 2019;63(3):321–326. doi: 10.1016/j.jpor.2019.01.005. [DOI] [PubMed] [Google Scholar]
- Choi Y.J., Razzoog E. Masking ability of zirconia with and without veneering porcelain. J. Prosthodontics: Implant, Esthetic Reconstr. Dent. 2013;22(2):98–104. doi: 10.1111/j.1532-849X.2012.00915.x. [DOI] [PubMed] [Google Scholar]
- Christensen G.J. Intracoronal and extracoronal tooth restorations 1999. J. Am. Dental Assoc.. 1999;130(4):557–560. doi: 10.14219/jada.archive.1999.0251. [DOI] [PubMed] [Google Scholar]
- Church, T., 2016. Translucency and Strength of High Translucency Monolithic Zirconium Oxide Materials, 81 MEDICAL GROUP SAN ANTONIO United States. [PubMed]
- Conrad H.J., Seong W.-J., Pesun I.J. Current ceramic materials and systems with clinical recommendations: a systematic review. J. Prosthetic Dent. 2007;98(5):389–404. doi: 10.1016/S0022-3913(07)60124-3. [DOI] [PubMed] [Google Scholar]
- Davidowitz G., Kotick P.G. The use of CAD/CAM in dentistry. J. Dent. Clin. 2011;55(3):559–570. doi: 10.1016/j.cden.2011.02.011. [DOI] [PubMed] [Google Scholar]
- Douglas R.D., Brewer J.D. Acceptability of shade differences in metal ceramic crowns. J. Prosthetic Dent. 1998;79(3):254–260. doi: 10.1016/s0022-3913(98)70233-1. [DOI] [PubMed] [Google Scholar]
- Heffernan M.J., Aquilino S.A., Diaz-Arnold A.M., Haselton D.R., Stanford C.M., Vargas M.A. Relative translucency of six all-ceramic systems. Part I: core materials. J. Prosthetic Dent. 2002;88(1):4–9. [PubMed] [Google Scholar]
- Helvey G. Classifying dental ceramics: numerous materials and formulations available for indirect restorations. J. Compend. Cont. Educ. Dent. 2014;35(1):38–43. [PubMed] [Google Scholar]
- Johnston W.M., Ma T., Kienle B.H. Translucency parameter of colorants for maxillofacial prostheses. Int. J. Prosthod. 1995;8(1) [PubMed] [Google Scholar]
- Juntavee N., Attashu S. Effect of sintering process on color parameters of nano-sized yttria partially stabilized tetragonal monolithic zirconia. J. Clin. Exp. Dent. 2018;10(8) doi: 10.4317/jced.55034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M.C., Aquilino S.A., Lund P.S., Vargas M.A., Diaz-Arnold A.M., Gratton D.G., Qian F. Human perception of dental porcelain translucency correlated to spectrophotometric measurements. J. Prosthod.: Implant, Esthetic Reconst. Dent. 2010;19(3):187–193. doi: 10.1111/j.1532-849X.2009.00542.x. [DOI] [PubMed] [Google Scholar]
- Minguez C., Lyons K. Failure of crowns and bridges–a review of the literature. N. Z. Dent. J. 2007;103(1):7. [PubMed] [Google Scholar]
- O'Brien W.J., Johnston W.M., Fanian F., Lambert S. The surface roughness and gloss of composites. J. Dent. Res. 1984;63(5):685–688. doi: 10.1177/00220345840630051601. [DOI] [PubMed] [Google Scholar]
- Oh S., Shin S.-M., Kim H.-J., Paek J., Kim S.-J., Yoon T.H., Kim S.-Y. Influence of glass-based dental ceramic type and thickness with identical shade on the light transmittance and the degree of conversion of resin cement. Int. J. Oral Sci. 2018;10(1):5. doi: 10.1038/s41368-017-0005-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadowsky S.J. An overview of treatment considerations for esthetic restorations: a review of the literature. J. Prosthetic Dent. 2006;96(6):433–442. doi: 10.1016/j.prosdent.2006.09.018. [DOI] [PubMed] [Google Scholar]
- Sannino G., Germano F., Arcuri L., Bigelli E., Arcuri C., Barlattani A. Cerec CAD/CAM chairside system. J. Oral Implantol. 2014;7(3):57. [PMC free article] [PubMed] [Google Scholar]
- Seghi R.R., Johnston W.M., O'brien W. Spectrophotometric analysis of color differences between porcelain systems. J. Prosthet. Dent. 1986;56(1):35–40. doi: 10.1016/0022-3913(86)90279-9. [DOI] [PubMed] [Google Scholar]
- Sethakamnerd P.L.C. Masking ability of two ceramics with different thicknesses on various substrates. M. Dent. J. 2017;37(2):233–242. [Google Scholar]
- Seyidaliyeva Aida, Rues Stefan, Evagorou Zinonas, Hassel Alexander J., Rammelsberg Peter, Zenthöfer Andreas. Color stability of polymer‐infiltrated‐ceramics compared with lithium disilicate ceramics and composite. J. Esthet. Restor. Dent. 2020;32(1):43–50. doi: 10.1111/jerd.v32.110.1111/jerd.12525. [DOI] [PubMed] [Google Scholar]
- Shono Norah, Alnahedh Hend. Contrast ratio and masking ability of three ceramic veneering materials. J Operative dentistry. 2012;37(4):406–416. doi: 10.2341/10-237-L. [DOI] [PubMed] [Google Scholar]
- Shono N., Nahedh H.A. Contrast ratio and masking ability of three ceramic veneering materials. J Operative dentistry. 2012;37(4):406–416. doi: 10.2341/10-237-L. [DOI] [PubMed] [Google Scholar]
- Suputtamongkol K., Tulapornchai C., Mamani J., Kamchatphai W., Thongpun N. Effect of the shades of background substructures on the overall color of zirconia-based all-ceramic crowns. J. Adv. Prosthod. 2013;5(3):319–325. doi: 10.4047/jap.2013.5.3.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabatabaei, M.H., Matinfard, F., Omrani, L.R., Mahounak, F.S., Ahmadi, E.J.T.O.D.J., 2019. Evaluation of the final color of ceramic veneers with different self-adhesive resin cements. 13(1).
- Tabatabaian, F., Dalirani, S., Namdari, M., 2019. Effect of thickness of zirconia ceramic on its masking ability: an in vitro study. 28(6), 666–671. [DOI] [PubMed]
- Tabatabaian F., Sharif M.J., Massoumi F., Namdari M. The color masking ability of a zirconia ceramic on the substrates with different values. J. Dent. Res., Dent. Clin., Dent. Prosp. 2017;11(1):7. doi: 10.15171/joddd.2017.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vichi A., Louca C., Corciolani G., Ferrari M. Color related to ceramic and zirconia restorations: a review. Dent. Mater. 2011;27(1):97–108. doi: 10.1016/j.dental.2010.10.018. [DOI] [PubMed] [Google Scholar]
- Wang F., Takahashi H., Iwasaki N. Translucency of dental ceramics with different thicknesses. J. Prosthetic Dent. 2013;110(1):14–20. doi: 10.1016/S0022-3913(13)60333-9. [DOI] [PubMed] [Google Scholar]
- Yeh C., Powers J., Miyagawa Y. Materials science: color of selected shades of composites by reflection spectrophotometry. J. Dent. Res. 1982;61(10):1176–1179. doi: 10.1177/00220345820610101401. [DOI] [PubMed] [Google Scholar]
- Zarone F., Russo S., Sorrentino R.J.D.m. From porcelain-fused-to-metal to zirconia: clinical and experimental considerations. J Dental materials. 2011;27(1):83–96. doi: 10.1016/j.dental.2010.10.024. [DOI] [PubMed] [Google Scholar]


