Abstract
Background
Cannabis is one of the most widely used substances worldwide. Heavy use is associated with an increased risk of cannabis use disorders, psychotic disorders, acute cognitive impairment, traffic injuries, respiratory problems, worse pregnancy outcomes, and there are indications for genotoxic and epigenotoxic adverse effects. International regulation of medical and non-medical cannabis use is changing rapidly and substantially, highlighting the importance of robust public health monitoring. This study aimed to describe the trends of key public health indicators in European Union (27 member states + UK, Norway and Turkey) for the period 2010 to 2019, their public health implications, and to identify the steps required to improve current practice in monitoring of cannabis use and harm in Europe.
Methods
Data on four key cannabis indicators (prevalence of use, prevalence of cannabis use disorder [CUD], treatment rates, and potency of cannabis products) in Europe were extracted from the United Nations Office on Drugs and Crime, European Monitoring Centre for Drugs and Drug Addiction and the Global Burden of Disease study. For prevalence of use and CUD, the first and last available estimate in each country were compared. For treatment rates and cannabis potency, linear regression models were conducted.
Findings
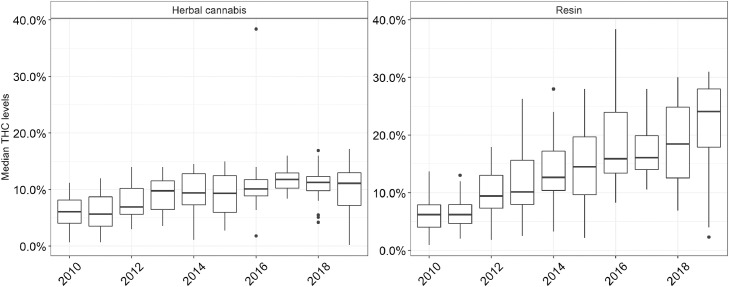
Between 2010 and 2019, past-month prevalence of cannabis use increased by 27% in European adults (from 3·1 to 3·9%), with most pronounced relative increases observed among 35-64 year-olds. In 13 out of 26 countries, over 20% of all past-month users reported high-risk use patterns. The rate of treatment entry for cannabis problems per 100,000 adults increased from 27·0 (95% CI: 17·2 to 36·8) to 35·1 (95% CI: 23·6 to 46·7) and has mostly plateaued since 2015. Modest increases in potency were found in herbal cannabis (from 6·9% to 10·6% THC) while median THC values tripled in cannabis resin (from 7·6% to 24·1% THC).
Interpretation
In the past decade, cannabis use, treatment rates and potency levels have increased in Europe highlighting major concerns about the public health impact of cannabis use. Continued monitoring and efforts to improve data quality and reporting, including indicators of high-risk use and cannabis-attributable harm, will be necessary to evaluate the health impact of international changes in cannabis regulation.
Funding
This study received no specific funding.
Keywords: public health, cannabis, cannabis use disorder, potency, treatment rates
Research in context.
Evidence before this study
We searched Pubmed (search terms: [“cannabis” OR “marihuana” OR “marijuana”] AND [“epidemiology” OR “public health” OR “harm”] AND “Europe”) for any review on public health monitoring of cannabis use in Europe. To date, a comprehensive review of cannabis use indicators in Europe is lacking. Some studies have reported increases in cannabis use, treatment demand and potency levels in some or most European studies. Two international bodies carry out regular monitoring of cannabis indicators and publish select findings in annual reports.
Added value of this study
The current study is the first to review and combine all publicly available data suitable for public health monitoring of cannabis use in Europe. We estimate that in 2019, 3.9% of European adults aged 15 to 64 have used cannabis use in the past month – an increase of 27% against 2010 levels, which was more pronounced in older age groups. In the same period, high-risk cannabis use patterns, treatment demand and potency levels have also increased in most countries.
Implications of all the available evidence
The available indicators suggest increasing cannabis use and public health concerns in Europe. Improved data reporting and quality is required in order to monitor changes of high-risk cannabis use and attributable harm, as well as to evaluate changes in cannabis policies.
Alt-text: Unlabelled box
1. Introduction
In 2018, the global 12-month-prevalence of cannabis use was estimated at 3·9% [1]. Based on surveys from 2015 to 2020, it is estimated that 15·4% of EU inhabitants aged 15 to 35 used cannabis in the previous year [2]. Occasional and more so heavy use of cannabis is associated with a number of adverse outcomes, including cannabis use disorder (CUD; [3]) and an increased risk of psychosis [4], [5], [6], [7], acute cognitive impairment [8,9] as well as other outcomes such as motor vehicle accidents [10], respiratory problems, testicular cancer [11] and lower birthweight of offspring (for current reviews, see [11], [12], [13], [14], [15]). In 2019, the Global Burden of Disease (GBD) study estimated that 0·6% of the European population met criteria for CUD, resulting in 158,000,000 disability adjusted life years [16]. In addition, there are indications that cannabinoids are genotoxic and epigenotoxic with yet to determined multigenerational implications on population health [17].
At least 23 European countries permit some form of cannabis use for medical purposes, albeit regulatory frameworks differ largely [18,19]. In some countries, such as Spain, only cannabinoid-based preparations are approved for select diseases (e.g. Nabiximols [20]), while other countries, such as Germany or UK, have established a more liberal approach, which allows (specialist) physicians to prescribe unprocessed herbal cannabis for certain illnesses [21,22]. Based on a growing body of evidence supporting the therapeutic potential of cannabis [23], the World Health Organization recommended that cannabis should be rescheduled in order to facilitate medicinal regulations in member states. With some delays, the rescheduling was carried out in December 2020 by the United Nations Commission on Narcotic Drugs [24]. It is now reasonable to expect more European countries to follow this decision and legalise unprocessed herbal cannabis for medical purposes.
Moreover, in light of the liberalisation of cannabis policy in North America [25,26], the option of recreational legalisation is broadly discussed in many European countries (see e.g. [27,28]). In fact, Luxembourg announced a decision to legalize the sale of cannabis for recreational use in 2019 [29]. In the same year, the Netherlands passed a controlled cannabis supply experiment bill which will evaluate the impact of legalising the supply of cannabis for recreational use in an experimental design [30]. Lastly, legislative changes towards decriminalization have been implemented in 2001 in Portugal [31] and more recently in Czechia [32].
In order to provide a strong empirical framework for assessing the health effects of changes in cannabis policy in Europe, rigorous public health monitoring of cannabis in Europe is crucial [33]. Currently, public health monitoring of adult cannabis use is carried out by two international bodies that routinely collect and publish data on several cannabis indicators, including prevalence of use, treatment rates, and potency levels. First, the United Nation Office on Drugs and Crime (UNODC) collects annual data on prevalence of illegal drug use as well as further drug-related indicators (cultivation, trafficking) from all UN member states [34]. In their annual “World Drug Reports”, these data are summarized at the regional as well as global level [1]. Second, the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) – the responsible body for monitoring illegal drug use and drug addiction in Europe – compiles a number of cannabis-related indicators, which also serve as base for the annual European Drug Reports [2]. In addition to these two agencies collecting empirical data on cannabis, the GBD study routinely estimates the prevalence of CUD for all countries [16].
In the current contribution, we extracted and analysed cannabis indicator data from publicly available sources, including prevalence of use, prevalence of cannabis use disorder (CUD), treatment rates, and potency of cannabis products in Europe. We aimed to describe the trends of these indicators for the period 2010 to 2019 and the possible public health implications. Further, we aimed to highlight limitations in the available data, in order to identify the steps required to improve current practice in monitoring of cannabis use and harm in Europe.
2. Methods
For this work, we aimed to describe trends between 2010 and 2019 in available cannabis indicators for all EU-27 member states, in addition to the UK, Norway and Turkey. The selection of countries was mainly driven by data availability as for these countries, cannabis indicators are compiled by the EMCDDA. As data for elderly people were not available, we limited the analyses to the age group 15 to 64. As data sources, we reviewed indicators relevant to public health monitoring from EMCDDA, UNODC, and the GBD study.
2.1. EMCDDA data
The EMCCDA is a EU agency which “exists to provide […] a factual overview of European drug problems and a solid evidence base to support the drugs debate” (https://www.emcdda.europa.eu/about_en). A total of 30 member states regularly provide data to the EMCDDA, which are presented in their ‘Statistical Bulletin’ [35], and are summarized in the annual European Drug Report [2]. We selected the following to be relevant for public health monitoring, none of which are provided with uncertainty intervals:
2.2. Prevalence of use (EMCDDA)
We obtained prevalence estimates from n=102 general population surveys with response rates ranging between 19.4% and 100% (mean: 56.1%; for more details see Supplementary Material 2 – sheet “GPS – METHODS”). The general population surveys are mostly national and conducted by EMCDDA member states.
Two types of cannabis indicators are obtained for: prevalence of use, defined as any use in the past year or past month; and high-risk use, defined as daily or near daily cannabis use (cannabis use on 20 days or more in the last month). For past-year and past-month prevalence of use, age-stratified estimates are provided (15 to 24, 25 to 34, 35 to 44, 45 to 54, 55 to 64 years) by the EMCDDA. For (almost) daily cannabis use, data by age are not available and estimates are only reported for the most recent year (2014 to 2020). In order to construct time trends, we obtained earlier data points from the EMCDDA archives. For Germany, the 2018 estimate was not yet included on the EMCDDA website and was taken from a publication [36].
2.3. Treatment demand indicator (EMCDDA)
The treatment demand indicator (TDI) reflects information about the number and the profile of people who enter treatment for drug problems each year. A uniform protocol guides EMCDDA member states to collect the required data in a comparable way across all countries [37]. For the formal TDI definition and further methodological details, see Supplemental Material 1.
For interpreting TDI data, variations in coverage of treatment entries between countries and over time need to be taken into consideration. We attempted to consider differences in coverage of TDI data, i.e., the share of all relevant treatment units covered by the indicator, between country and over time. However, a complete assessment of TDI coverage is not available but the most recent report for the year 2014 marks substantial cross-country differences in the TDI coverage rates – from 60% to 100% for out-patient treatment centers and from 30% to 100% for in-patient treatment centers (for country-specific and temporal data, see Supplemental Material 1 - Supplementary Figure 1 and Supplementary Material 2) [38]. To further elaborate on TDI coverage variations, we examined how the number of treatment units covered by the TDI differs between countries and developed over time (all data taken from EMCDDA website: [35]).
2.4. Cannabis Potency (EMCDDA)
EMCDDA member states monitor and report cannabis potency according to the total concentration of delta-9-tetrahydrocannabinol (THC) in sample weight, to the nearest 0·1%. For the current analyses, we obtained the median THC levels in herbal cannabis and resin [35]. In contrast to survey and TDI data, the EMCDDA does not disclose any details on the underlying sources of THC data per country and year. While the THC data aim to be representative of the retail level, the agency acknowledges several methodological limitations that might render some data not representative. It can be assumed that the presented data are predominantly obtained from a sample of police seizures of cannabis [39]. For Germany, THC data were corrected and completed by the respective EMCDDA focal point [40].
2.5. UNODC data
We reviewed UNODC data [41] but could not identify any cannabis-related indicators relevant for public health monitoring that are not already captured by the EMCDDA data collection. In fact, both agencies collect data on prevalence of use and on treatment rates. However, we chose to refer to EMCDDA data for the following reasons: the UNODC ‘general population’ prevalence database does not include information on the age range of the target population or exact references. Further, it contains several estimates derived from the school survey initiative ESPAD, which should not be reported as general population estimates. As for TDI, we compared data from UNODC and EMCDDA for 2017 for 16 countries with data available in both data bases. For any drug treatment, data were only consistent in half of the countries. Further, treatment demand for CUD was only reported as percentage of all treatment demand in the UNODC data base, requiring recalculations and additional assumptions to report CUD treatment rates. Based on this assessment, we restricted our analyses to data provided by the EMCDDA.
2.6. GBD data
Data on CUD prevalence including uncertainty intervals by 5-year age bands were retrieved from the GBD study for the years 2010 to 2019 [42]. In the GBD study, CUD is defined by ICD-10 (F12.2) or DSM-IV (304.30) criteria for cannabis dependence and prevalence estimates are based on school and adult survey data. In brief, cannabis use prevalence estimates were first converted into regular use estimates and then into CUD estimates. The first conversion ratio (from any use to regular use) was determined using a meta-analytical approach, resulting in a factor of 2·9 (i.e., there is one regular user for 3 any user). The second conversion ratio (from regular use to CUD) was determined using a Bayesian meta-regression, which accounted for risk differences between youth and adults. For more details on the estimation of CUD, see supplement of [43]).
2.7. Population data
We used population data from the UN World Population Prospects 2019 [44]. The estimates are based on national censuses and information from vital registration systems and consider trends in fertility, mortality and migration.
2.8. Processing of data
All available data were retrieved from the indicated data sources, however, for prevalence of use, potency and TDI, data were missing for some countries and years.
To obtain country- and year-specific CUD estimates for the 15 to 64 year old target population, age-specific data were aggregated using UN population data. Using TDI data, treatment rates, expressed as the number of treatment entries per 100,000 adults were estimated.
We calculated the share of (almost) daily users among past-month users as an indicator for high-risk consumption patterns for countries with available data. This indicator sheds light on differences in (high-risk) use patterns between countries.
To obtain European averages across all countries with available data, population-weighted means of the indicators were calculated using UN population data. For THC concentrations, weighted averages would have required to account for the respective share of both resin and herbal cannabis in total use per country, however, these data were not available. Thus, we aggregated the country-level estimates by reporting medians and interquartile ranges.
2.9. Statistical analyses
All data were analysed using R version 4·0·5 [45] and are available as Supplementary Material 2, including the corresponding R code.
Given the lack of uncertainty intervals for most indicators, meta-analytical trend analyses were not feasible.
For estimating changes in the indicators at the European level, the oldest and most recent data points were selected and reported. For prevalence of use, at least one of these two points was not available in four countries (Austria, Estonia, Greece, Malta), which were excluded from estimating changes. The difference in adult and age-specific prevalence of use as well as for THC levels did not account for the degree of uncertainty associated with each point estimate, as these data were not available from the EMCDDA data repository. Respective confidence intervals thus only consider between-country variation of point estimates and should thus be interpreted cautiously.
To describe country-level trends in prevalence of use and CUD, statistical models were not applied as too few data points were available for most countries (prevalence of use) or because the estimates were predicted from statistical models (prevalence of CUD). Thus, for these two indicators, we only compared the first and last available estimate in each country to estimate changes from the oldest to the most recent data point.
To describe country-level trends in treatment rates and THC concentrations, linear regression models were conducted, separately for each country with at least 5 observations. In each model, year was entered as a single covariate, describing the annual change score in the outcome. Results are reported for all models in which the coefficient was significantly different from 0 at alpha = 1%.
2.10. Role of the funding source
This study has received no specific funding.
3. Results
3.1. Prevalence of cannabis use
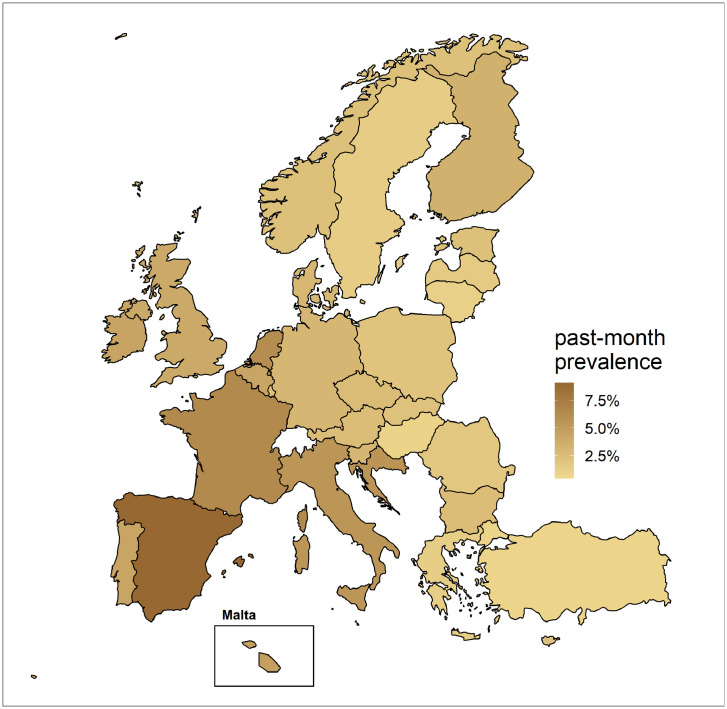
The most recent estimates of prevalence of use are summarized in the map in Figure 1. Overall, cannabis use appears to be more common in Western than in Eastern countries. Based on data collected between 2013 and 2019, past-month prevalence of use was below 1% in Malta, Hungary, and Turkey. In three countries (Croatia, Italy, the Netherlands), between 5 and 6% of adults reported past-month cannabis use. Highest use rates were recorded in Spain (9·1%) and France (6·4%). The country-level cannabis use prevalence rates are further reported in Supplemental Material 1 (Supplemental Table 1).
Figure 1.
Past-month prevalence of cannabis use in Europe, based on most recently available survey estimates.
Re-examining the available EMCDDA data for all countries since 2010 allowed for a more precise analyses of trends of cannabis use in Europe. At the European level, cannabis consumption appeared to have increased in the past decade. Comparing the last and first available estimates, an increasing past-month prevalence was identified for 24 out of 26 countries that had at least two data points available. The country-specific changes in prevalence of use for the adult population are further illustrated in Supplemental Material 1 (Supplemental Figure 2).
Age-specific comparisons of first versus last years suggest that an increase in both past-month and past-year use was observed across all age groups in Europe (see Table 1). Among younger adults, cannabis consumption is overall more prevalent and absolute increases were more pronounced in this age group. Among 35 to 64 year-olds, increases were smaller in absolute terms but greater in relative terms. In this age group, prevalence of use increased by 50% or more between 2010 and 2019.
Table 1.
Prevalence of past-month and past-year cannabis use in Europe, based on earliest and most recent survey estimates from 26 countries
| 2010 1 | 2019 2 | Absolute prevalence difference 3 | Relative prevalence difference3 | ||
|---|---|---|---|---|---|
| PAST MONTH | 15 to 64 | 3·1 (2·3 to 3·9) | 3·9 (2·9 to 4·8) | +0·8 (0·3 to 1·4) | +26·6% |
| By age group | |||||
| 15 to 24 | 7·0 (5·1 to 8·8) | 8·6 (6·5 to 10·6) | +1·7 (0·6 to 2·8) | +24·8% | |
| 25 to 34 | 5·1 (3·7 to 6·4) | 6·0 (4·5 to 7·6) | +1·2 (0·3 to 2·1) | +23·4% | |
| 35 to 44 | 2·0 (1·4 to 2·7) | 3·2 (2·1 to 4·3) | +1·2 (0·6 to 1·9) | +60·4% | |
| 45 to 54 | 1·1 (0·8 to 1·4) | 1·7 (1·0 to 2·4) | +0·6 (0·1 to 1·1) | +56·9% | |
| 55 to 64 | 0·4 (0·2 to 0·6) | 0·7 (0·4 to 1·0) | +0·3 (0·1 to 0·6) | +82·2% | |
| PAST YEAR | 15 to 64 | 5·6 (4·3 to 6·9) | 6·8 (5·4 to 8·2) | +1·3 (0·4 to 2·2) | +22·7% |
| By age group | |||||
| 15 to 24 | 13·2 (10·1 to 16·2) | 15·7 (12·1 to 19·3) | +2·7 (0·9 to 4·6) | +20·7% | |
| 25 to 34 | 9·0 (6·8 to 11·2) | 10·6 (8·3 to 13) | +1·9 (0·5 to 3·2) | +20·8% | |
| 35 to 44 | 3·6 (2·7 to 4·6) | 5·4 (3·9 to 6·8) | +1·8 (0·9 to 2·7) | +49·6% | |
| 45 to 54 | 2·0 (1·5 to 2·5) | 3·1 (2·2 to 3·9) | +1·1 (0·5 to 1·6) | +53·2% | |
| 55 to 64 | 0·8 (0·6 to 1·1) | 1·3 (1 to 1·6) | +0·5 (0·1 to 0·9) | +62·8% | |
Note. Figures in brackets indicate 95% asymptotic confidence intervals based on standard error of reported survey point estimates, not considering variation around each point estimate.
N=22 out of N=26 countries had survey estimates available in 2010, 2011, or 2012, with the remaining estimates obtained from the years 2013 (N=1), 2014 (N=2), or 2015 (N=1)
N=21 out of N=26 countries had survey estimates available in 2017, 2018, or 2019, with the remaining estimates obtained from 2016 (N=3), 2015 (N=2), or 2013 (N=1)
calculated as the population-weighted absolute/relative difference between earliest and most recent point estimate
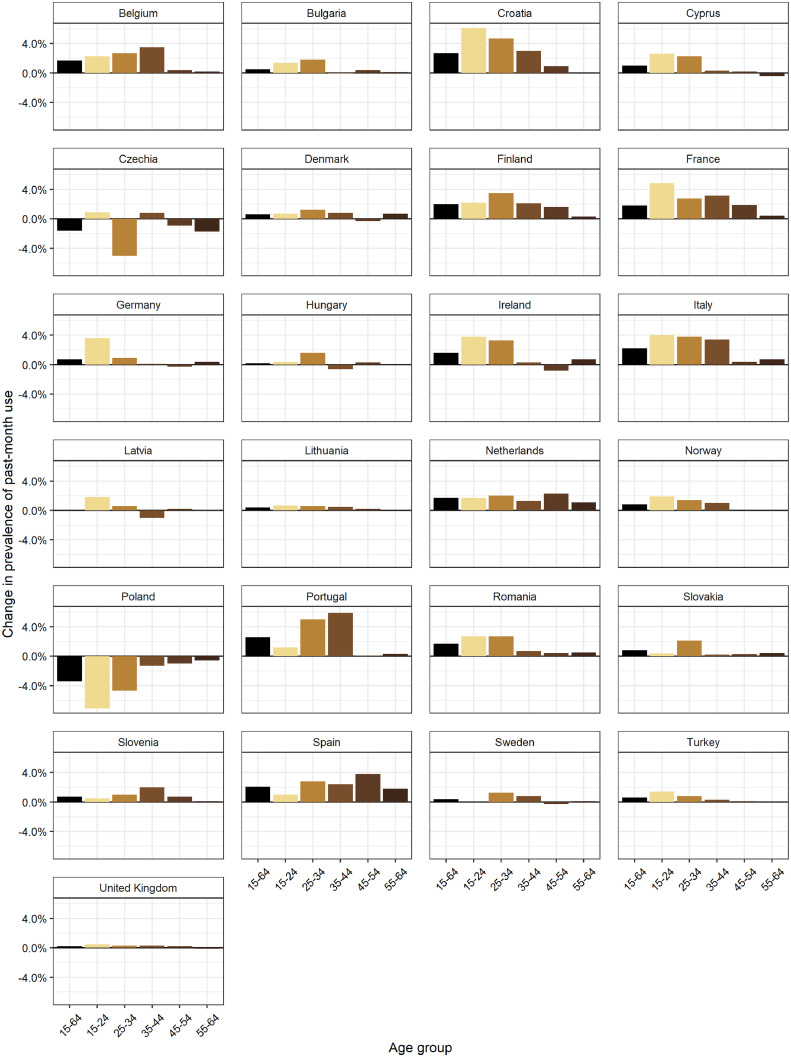
The age-specific trends in prevalence of past-month use at the country level, based on the first and last available estimate, are further displayed in Figure 2. Only in Czechia and Poland, marked decreases in prevalence of use in most if not all age groups were observed. In France, the Netherlands, and Spain, pronounced increases among middle-aged adults were identified. In contrast, Germany reports increases in total use which were driven mostly by younger adults. Very similar country patterns were present for age-specific changes in past-year prevalence (see Supplemental Figure 3).
Figure 2.
Percentage point change in past-month prevalence of cannabis use between earliest and most recent survey estimate (since 2010), by country. Countries with only one data point (Austria, Estonia, Greece, Malta) and without age-specific data (Luxembourg) are not displayed. The empty bar for 15 to 24 year-olds in Sweden indicates no change in prevalence of use.
Prevalence estimates for (almost) daily cannabis use among 15 to 64 year olds are displayed in Supplemental Figure 4. In 18 countries out of 26 countries with available data, indications for increasing trends in (almost) daily cannabis use could be observed. Most pronounced increases were reported in Portugal (from 0·5% in 2012 to 3·0% in 2016) and Spain (from 2·5% in 2011 to 3·7% in 2017; see Supplemental Table 2 for estimates for all countries).
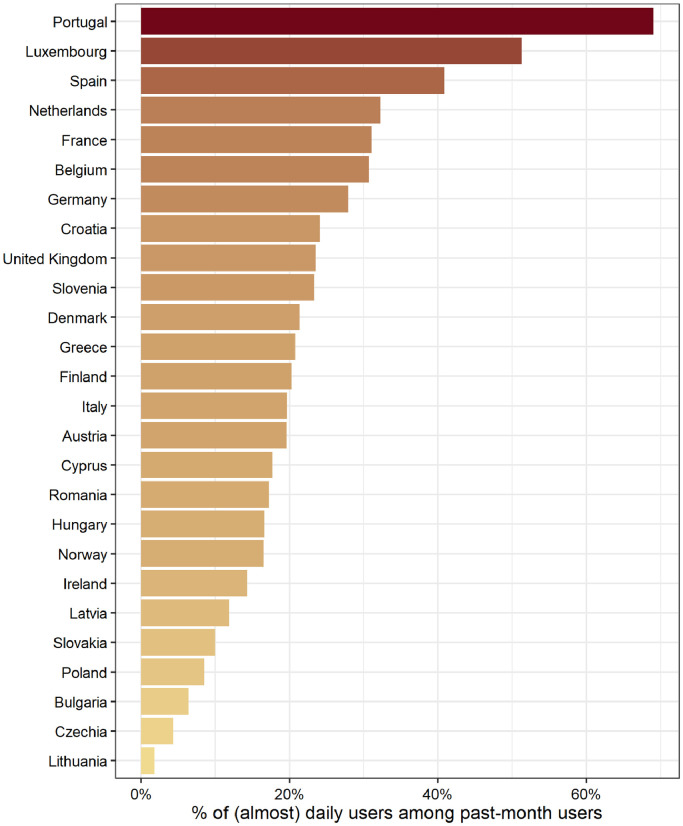
Based on the last available estimates, the share of (almost) daily users among past-month users differed largely across all European countries. In countries like Lithuania, Czechia, Bulgaria and Poland, less than one in ten users reported high-risk use patterns. In contrast, 50% and 70% of all past-month users reported (almost) daily use in Luxembourg and Portugal, respectively. In half of all countries examined, the share of past-month users engaging in (almost) daily use was 20% or higher (see Figure 3).
Figure 3.
Share of (almost) daily cannabis user among past-month cannabis users, for the most recent year with available data.
3.2. Prevalence of cannabis use disorder
According to GBD study estimates, 0·5% of the adult (15-64) population met CUD criteria in 2019 (95% CI: 0·2 to 0·9%), similar 2010 figures (0·6%, 95% CI: 0·2 to 0·9%). There was substantial heterogeneity in the prevalence of CUD, ranging from 0·1% in Turkey to 1·2% in the UK. As illustrated in Supplemental Material 1 (Supplemental Figure 5), CUD prevalence between 2010 and 2019 pointed downwards in most countries. However, given the large confidence intervals and the small differences in point estimates, the GBD data suggest no meaningful trends in CUD prevalence for any country.
3.3. Treatment rates for cannabis use disorder
In 2019, 115,477 treatment entries were registered by 25 countries and reported to the EMCDDA.
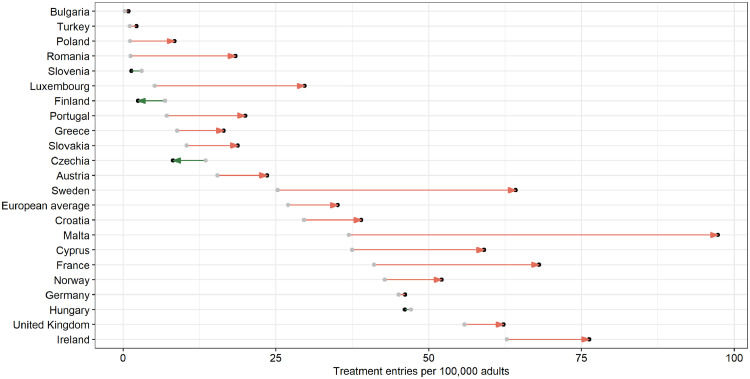
At the country level, vast differences in treatment rates are reported. In Bulgaria and Slovenia, less than 2 treatment entries for cannabis problems per 100,000 adults were recorded in 2019. In contrast, more than 100 treatment entries per 100,000 adults were registered in Malta. For an illustration of country-specific trends of treatment rates, see Supplemental Material 1 (Supplemental Figure 6).
Based on the 22 countries with available data in the years 2010 and 2019 (representing 76% of the population aged 15 to 64 among all 28 studied countries in the year 2019), the rate of treatment entries for cannabis as primary problem per 100,000 adults increased from 27·0 (95% CI: 17·2 to 36·8) to 35·1 (95% CI: 23·6 to 46·7). The changes in treatment rates are also displayed in Figure 4. Regression models suggest a significantly declining treatment rate only for the Netherlands (annualized decrease in treatment entries per 100,000 adults: -2·4, p=·005), Finland (-0·4, p=·002), and Slovenia (-·3, p=·01). In ten countries, treatment rates significantly increased. Modest increases were recorded in Greece, Poland, Austria, Slovakia, and Portugal (annualized increase in treatment entries per 100,000 adults between +0·8 and 1·9, all p<·001), while more pronounced increases were present in Romania, Belgium, France, Malta, and Sweden (annualized increase in treatment entries per 100,000 adults between +4·3 and 6·4, all p<·01).
Figure 4.
Change in treatment admissions per 100,000 adults between 2010 and 2019 for all countries with available data and their average. Green color indicates countries with declining trend, red color indicates countries with increasing trend. Arrows are only presented for countries with a change in treatment rates of at least 3 admissions per 100,000 adults.
Based on those 17 countries providing continuous data between 2010 and 2019, the upward slope in treatment rates had come to a halt in the year 2015 and has mostly plateaued since then (see Supplemental Material 1 - Supplementary Figure 7).
The available data on TDI coverage suggests a high degree of variation between countries and over time, including a declining number of treatment units from which data were collected since 2014 (see Supplemental Material 1 - Supplementary Figure 1).
3.4. Cannabis potency
Median THC concentrations in herbal cannabis were reported by 22 countries. Between 2010 and 2019, THC concentration modestly increased, from 6·9% (Interquartile range (IQR): 4·7 to 9·2%) to 10·6% (IQR: 7·2 to 12·7%; see also Figure 5). Regression analyses suggest that THC concentrations in herbal cannabis did not significantly decline in any country in Europe. However, significantly increasing THC concentrations in herbal cannabis rose were identified in six countries (Portugal, Estonia, Czechia, Poland, Sweden, Hungary) at an annual rate of 0·5 to 1·1 percentage points.
Figure 5.
Boxplots of median THC levels reported annually by 25 countries (Austria, Belgium, Bulgaria, Croatia, Cyprus, Czechia, Denmark, Estonia, Finland, France, Germany, Hungary, Ireland, Italy, Luxembourg, Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, Turkey), by cannabis type. Each box indicates the interquartile range and the horizontal bar represents the median of all reported values in that year.
In cannabis resin, the THC concentrations tripled from 7·6% (IQR: 4·2 to 11·7%) to 24·1% (IQR: 16·5 to 27·5%), as suggested by data provided by 20 countries between 2010 and 2019 (see also Figure 5). At the country level, regression models found no significantly declining THC concentrations in resin in any country but significantly increasing THC concentrations were present in eight countries. In Austria, Germany, Portugal, Italy, and Estonia, annualized change rates ranged between +0·8 and +1·5 percentage points. In France, Sweden, and Luxembourg, THC concentrations in resin rose at an annual rate of 2·3 to 2·5 percentage points.
Country-level trajectories of THC in resin and herbal cannabis are further displayed in Supplementary Figure 8.
4. Discussion
4.1. Summary
Public health monitoring indicates that cannabis use is prevalent in Europe. Although estimates should be interpreted with caution due to potential error, the best available data at present indicates that an estimated 3·9% of all adults aged 15 to 64 reporting past month use. There is a considerable variation in prevalence of use, ranging from 9·1% in Spain to less than 1% in Malta, Hungary, and Turkey. Approximately 1 in 7 past-month users were estimated to meet CUD criteria, with substantial heterogeneity between countries. In countries where cannabis use is more common, such as in the Netherlands and Spain, the share of users meeting CUD criteria appears to be lower than in countries where cannabis use is less common, such as Malta and Hungary. However, there are also exceptions to this, such as the UK, which has both relatively high rates of cannabis use and of CUD.
At the European level, the bulk of trend data converge on showing that cannabis use and related problems have increased in the past decade. The available data indicates that rises in prevalence rates were reported in all age groups. Among adults aged 35 to 64 years, prevalence of past month use increased by 50% or more. These findings are similar to reports from European student surveys [46] and recent trends in the USA, where the largest increases in prevalence of use have occurred in middle-aged adults [47]. Consistent with rising prevalence of any use and high-risk use patterns, treatment rates have also risen in many countries, reaching a plateau in 2014. The high level of treatment rates for cannabis creates problems for healthcare providers. Psychosocial interventions such as Motivational Interviewing and Cognitive Behavioural Therapy have been shown to be effective at reducing cannabis use [48,49]. However, there is a lack of approved pharmacotherapies for the treatment of cannabis use disorders, and limited effectiveness of psychosocial interventions for people with comorbid mental health problems such as psychosis [50].
Lastly, stark and modest increases in cannabis potency levels have been registered for resin and herbal cannabis, respectively, corroborating previous analyses in Europe and internationally [51], [52], [53]. In contrast to these trends, CUD prevalence is estimated to have declined in the past decade in most countries. These findings are consistent with survey data from the United States, showing that while the prevalence of cannabis use increased from 2001-2002 to 2012-2013, the prevalence of cannabis use disorders in cannabis users decreased [54]. However, potency level may be implicated with other health outcomes than CUD, such as psychotic outcomes [55] or genotoxic and epigenotoxic effects [17].
4.2. Limitations and implications
In the following, we describe the implications of the findings for each indicator, after outlining the limitations that need to be considered.
4.3. Prevalence of use
This indicator is based on general population surveys, which have the usual problems of substance use surveys in the last decade: non-representative sampling frame excluding key risk groups, high degree of non-response and use of self-report [56]. Moreover, the validity of prevalence estimates may vary between countries, which could increase risk of bias when comparing estimates across different countries. Undercoverage is not as easily quantified as for legal substances such as alcohol, as objective indicators such as sales data or wastewater analyses do not routinely exist or are hard to interpret in comparison to the standard indicators [57], [58], [59]. Further, the lack of uncertainty measures prohibited to apply robust statistical methods to study trends in cannabis consumption. Lastly, we do not have any information on the purpose of consumption but assume that only a minor fraction of users do take cannabis for medical purposes (for a summary of European data, see [19]). For future monitoring, survey data should distinguish between medical and recreational cannabis users.
Despite these limitations, survey-based cannabis use prevalence constitutes one of the best indicators available for public health monitoring purposes. In the 2021 European Drug Report, the EMCDDA focuses on cannabis use among young adults [2]. While we also found indications for increasing use in this age groups, our findings add that cannabis consumption has apparently become more common among 35 to 64 year-olds. Albeit absolute use levels remain lower in this age group, this is a trend worth noting. This trend could be driven by an aging population of users (i.e., growing out of cannabis use becomes less common) or by the increase in medical use of cannabis. Prescription data from Germany show that patients using cannabis flowers on prescription are on average 46 years old [60]. Another possibility, supported by data from the USA [61], is that the proportion of older adults who disapprove of cannabis use may have decreased over time.
While the underlying reasons for an aging population of cannabis users are yet to be singled out, the prolonged use of cannabis might be associated with an increase in the risk of lung cancer [62] or chronic obstructive pulmonary disease [13] – both of which are rather rare among younger adults. Moreover, acute cannabis use is a risk factor for traffic collisions [63,64] and this affects all ages regardless of the purpose of use (recreational or medical) [65]. Thus, if the aging and growing population of cannabis users are driving under the influence of cannabis, this could increase the number of motor vehicle accidents in Europe.
Our findings further suggest an increase in (almost) daily cannabis use prevalence. While similar trends have been reported for the USA [66], such patterns have not been reported for Europe so far. Further research should examine whether prevalence of risky use patterns increased over and above prevalence of any use – or in other words: have use patterns among current users become riskier?
4.4. Cannabis use disorder
In contrast to all other trends, the prevalence of CUD did not show indications of increases in Europe. As the CUD data constitute smoothed estimates obtained from statistical models, there are some problems inherent to these data, such as not appropriately representing the true fluctuation in the data. However, as CUD prevalence is estimated from cannabis use prevalence, the diverging trends question the validity of the CUD estimates. The consistency of select GBD estimates have been questioned in previous studies (e.g., [67,68]) and our results add that estimation procedures for CUD prevalence may be revisited and improved. An additional consideration is that the validity of CUD estimates may vary between countries, which limits comparability of estimates across countries.
Given the outlined limitations associated with available TDI and CUD data, there is a need to improve indicators for high-risk cannabis use or experience of cannabis-related problems in Europe. We propose to use high-frequency use patterns, such as (almost) daily use and the EMCDDA should provide these data by country, year, sex, and age on their website. In the long-run, however, an indicator for high-risk use considering more than just frequency of use should be established [69,70], ideally supplemented with data on quantity of use (see e.g. data from Canada [71]).
4.5. Treatment rates
Our analyses show that the number of treatment units contributing to the TDI varies greatly between countries and over time. The large gaps in treatment rates far exceed the variation that would be expected based on prevalence of use and of CUD, questioning the validity of the estimates across time and space. Moreover, up-to-date information on TDI coverage, i.e., the share of all relevant treatment units covered in each country, is not available. Thus, we recommend that between-country comparisons should not be undertaken without accounting for methodological differences. Further, an increase in treatment rates can reflect a number of different factors (in addition to treatment demand itself), such as TDI reporting completeness or quality, a higher willingness of users to seek treatment, or increased availability of treatment. We recommend that, where feasible, improvements to TDI data quality should be made to facilitate understanding of true treatment demand and enable robust estimates of change.
4.6. Cannabis potency
Cannabis potency data are predominantly collected through analysis of police seizures at the national level. As such, they should not be assumed to be representative of the type of cannabis used at the retail level. Law enforcement methods create a risk of bias in selection according to various factors such as degree of criminal involvement, ethnicity, age, gender, and location. By contrast, cannabis potency data reported by the Netherlands (Trimbos Institute) can be assumed to be representative of cannabis available at the retail level, as data are collected using a standardised protocol consisting of random sampling from national retail outlets each year [72]. We recommend that, where possible, additional European countries should sample cannabis from sources other than seizures in order to improve the reliability and validity of the data. As policies towards cannabis are becoming more permissive in Europe, this may facilitate improved monitoring of cannabis potency at the retail level. An additional consideration is that for all countries reporting data on cannabis potency, the reliability of data may be influenced by the sample size of cannabis products used to create summary estimates for each country and year, and the laboratory equipment and analytical protocol used to estimate potency. Information on these potentially confounding variables are not available at present. Finally, concentrations of cannabidiol are not monitored at present.
The public health relevance of cannabis potency indicators is evidenced by findings that THC concentration was associated with progression to the first symptom of CUD (1.4 times per each unit of THC [73]) and greater severity of CUD [74], especially among younger people. High-potency cannabis was also associated with increased risk of psychosis [75], and with frequency of use, cannabis-related problems and anxiety [76].
Our findings suggest greater THC concentrations in cannabis resin, which is produced by extracting material from the cannabis plant. The increase in potency of cannabis resin in Europe may be attributable to a shift towards THC-dominant cannabis plants in Morocco - the primary producer of cannabis resin for the European market [77]. The increased THC concentrations in resin may translate into greater risk of harm for users preferring this type of cannabis. Possibly, the increased risk could be offset by dose titration [78] or higher concentration of cannabidiol found in resin (for data on concentration, see [72]; for the effects of cannabidiol, see [79]). However, as findings on the protective effects of cannabidiol have been inconsistent [80], it remains to be studied empirically whether resin use is associated with an increased risk.
In light of the increased public health risks and the uncertainty in the underlying data, we see the need for improved monitoring of cannabis potency in Europe. The need for better data is further substantiated by changes in the cannabis market, such as the emergence of products containing high levels of cannabidiol in Europe [81] and the widespread use of highly concentrated cannabis extracts in North America.
5. Conclusions
Between 2010 and 2019, cannabis use, risky use patterns, treatment rates and potency levels have increased in Europe. The combination of rising prevalence, risky use and potency levels suggest that, overall, THC exposure has increased in the European population. To fully understand the public health implications of the observed trends, the quality and reporting of available data should be improved and supplemented with additional data on high-risk cannabis use patterns and cannabis-attributable harm.
Author contributions
Conceptualisation: Jakob Manthey; data curation: Jakob Manthey, Carolin Kilian; formal analysis: Jakob Manthey; funding acquisition: N/A; Investigation: Jakob Manthey, methodology: Jakob Manthey; project administration: Jakob Manthey, resources: Jakob Manthey, Jürgen Rehm; software: N/A; supervision, validation: all authors, visualisation: Jakob Manthey, Carolin Kilian; writing – original draft: Jakob Manthey; writing– review & editing: all authors
Data sharing statement
All data analysed for this publication were obtained from publicly available sources and can be accessed in Supplementary Material 2, which also contains the R code used for the analyses.
Editor note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interest
H.L.P. works under the CERCA Programme/Generalitat de Catalunya and receives funding from the Spanish Ministry of Science, Innovation and Universities, Instituto de Salud Carlos III through a “Juan Rodes” contract (JR19/00025). The remaining authors declare no conflict of interest.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2021.100227.
Appendix. Supplementary materials
References
- 1.United Nations Office on Drugs and Crime . United Nations publication; 2020. World Drug Report 2020. [Google Scholar]
- 2.European Monitoring Centre for Drugs and Drug Addiction . Publications Office of the European Union; Luxembourg: 2021. European drug report 2021: trends and developments. [Google Scholar]
- 3.Connor JP, Stjepanović D, Le Foll B, Hoch E, Budney AJ, Hall WD. Cannabis use and cannabis use disorder. Nature Reviews Disease Primers. 2021;7(1):16. doi: 10.1038/s41572-021-00247-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaucher J, Keating BJ, Lasserre AM, et al. Cannabis use and risk of schizophrenia: a Mendelian randomization study. Mol Psychiatry. 2018;23(5):1287–1292. doi: 10.1038/mp.2016.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gage SH, Jones HJ, Burgess S, et al. Assessing causality in associations between cannabis use and schizophrenia risk: a two-sample Mendelian randomization study. Psychol Med. 2017;47(5):971–980. doi: 10.1017/S0033291716003172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. 2016;42(5):1262–1269. doi: 10.1093/schbul/sbw003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung J, Chan GCK, Hides L, Hall WD. What is the prevalence and risk of cannabis use disorders among people who use cannabis? A systematic review and meta-analysis. Addict Behav. 2020 doi: 10.1016/j.addbeh.2020.106479. [DOI] [PubMed] [Google Scholar]
- 8.Scott J, Slomiak ST, Jones JD, Rosen AG, Moore TM, Gur RC. Association of cannabis with cognitive functioning in adolescents and young adults: a systematic review and meta-analysis. JAMA Psychiatry. 2018 doi: 10.1001/jamapsychiatry.2018.0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Figueiredo PR, Tolomeo S, Steele JD, Baldacchino A. Neurocognitive consequences of chronic cannabis use: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2020;108:358–369. doi: 10.1016/j.neubiorev.2019.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, Li G. Marijuana use and motor vehicle crashes. Epidemiol Rev. 2012;34:65–72. doi: 10.1093/epirev/mxr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghasemiesfe M, Barrow B, Leonard S, Keyhani S, Korenstein D. Association between marijuana use and risk of cancer: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(11) doi: 10.1001/jamanetworkopen.2019.16318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Memedovich KA, Dowsett LE, Spackman E, Noseworthy T, Clement F. The adverse health effects and harms related to marijuana use: an overview review. CMAJ Open. 2018;6(3):E339–EE46. doi: 10.9778/cmajo.20180023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campeny E, Lopez-Pelayo H, Nutt D, et al. The blind men and the elephant: systematic review of systematic reviews of cannabis use related health harms. Eur Neuropsychopharmacol. 2020;33:1–35. doi: 10.1016/j.euroneuro.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 14.National Academies of Sciences E, and Medicine. Health and Medicine Division. Board on Population Health and Public Health Practice. Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda . National Academies Press (US); Washington, DC: 2017. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. [PubMed] [Google Scholar]
- 15.Mohiuddin M, Blyth FM, Degenhardt L, et al. General risks of harm with cannabinoids, cannabis, and cannabis-based medicine possibly relevant to patients receiving these for pain management: an overview of systematic reviews. Pain. 2021;162 doi: 10.1097/j.pain.0000000000002000. [DOI] [PubMed] [Google Scholar]
- 16.Institute for Health Metrics and Evaluation . University of Washington; Seattle, USA: 2020. GBD Results Tool. [Google Scholar]
- 17.Reece AS, Hulse GK. Epidemiological overview of multidimensional chromosomal and genome toxicity of cannabis exposure in congenital anomalies and cancer development. Sci Rep. 2021;11(1):13892. doi: 10.1038/s41598-021-93411-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abuhasira R, Shbiro L, Landschaft Y. Medical use of cannabis and cannabinoids containing products - regulations in Europe and North America. Eur J Intern Med. 2018;49:2–6. doi: 10.1016/j.ejim.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 19.European Monitoring Centre for Drugs and Drug Addiction . Publications Office of the European Union; Luxembourg: 2018. Medical use of cannabis and cannabinoids. [Google Scholar]
- 20.Flachenecker P, Henze T, Zettl UK. Nabiximols (THC/CBD oromucosal spray, Sativex(R)) in clinical practice–results of a multicenter, non-interventional study (MOVE 2) in patients with multiple sclerosis spasticity. Eur Neurol. 2014;71(5-6):271–279. doi: 10.1159/000357427. [DOI] [PubMed] [Google Scholar]
- 21.Rehm J, Elton-Marshall T, Sornpaisarn B, Manthey J. Medical marijuana. What can we learn from the experiences in Canada, Germany and Thailand? The International Journal on Drug Policy. 2019;74:47–51. doi: 10.1016/j.drugpo.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Freeman TP, Hindocha C, Green SF, Bloomfield MAP. Medicinal use of cannabis based products and cannabinoids. BMJ. 2019;365:l1141. doi: 10.1136/bmj.l1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.dos Santos RG, Hallak JEC, Crippa JAS. In: Cannabinoids and neuropsychiatric disorders. Murillo-Rodriguez E, Pandi-Perumal SR, Monti JM, editors. Springer International Publishing; Cham: 2021. Neuropharmacological effects of the main phytocannabinoids: a narrative review; pp. 29–45. [Google Scholar]
- 24.United Nations Commission on Narcotic Drugs. WHO scheduling recommendations on cannabis and cannabis-related substances. 2020. https://www.unodc.org/unodc/en/commissions/CND/Mandate_Functions/current-scheduling-recommendations.html accessed 17 March 2021.
- 25.Hall W, Lynskey M. Assessing the public health impacts of legalizing recreational cannabis use: the US experience. World Psychiatry. 2020;19(2):179–186. doi: 10.1002/wps.20735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hill KP, George TP. Cannabis legalisation in Canada: a crucial trial balloon. The Lancet Psychiatry. 2019;6(1):5–6. doi: 10.1016/S2215-0366(18)30460-7. [DOI] [PubMed] [Google Scholar]
- 27.Charpak Y, Couteron JP. France and marijuana: an unbalanced debate where public health competence is missing. Eur J Public Health. 2019;29(3):389. doi: 10.1093/eurpub/ckz063. [DOI] [PubMed] [Google Scholar]
- 28.Leus X, Van Hal G. A new wave of marijuana legalization: country case study from Belgium. Eur J Public Health. 2019;29(3):388. doi: 10.1093/eurpub/ckz062. [DOI] [PubMed] [Google Scholar]
- 29.The Guardian. Luxembourg to be first European country to legalise cannabis. 2019. https://www.theguardian.com/world/2019/aug/07/luxembourg-to-be-first-european-country-to-legalise-cannabis accessed 17 March 2021.
- 30.Government of the Netherlands. Controlled cannabis supply chain experiment. 2019. https://www.government.nl/topics/drugs/controlled-cannabis-supply-chain-experiment accessed 17 March 2021.
- 31.Greenwald G. Drug decriminalization in Portugal: lessons for creating fair and successful drug policies. Cato Institute Whitepaper Series; 2009.
- 32.Belackova V, Brandnerova M, Vechet D. How close to the “Honeypot?”. Int Criminal Justice Rev. 2018;28(3):206–225. [Google Scholar]
- 33.International Drug Policy Consortium. Principles for the responsible legal regulation of cannabis. 2020. https://idpc.net/publications/2020/09/principles-for-the-responsible-legal-regulation-of-cannabis accessed 17 March 2021.
- 34.Research and Trend Analysis Branch . United Nations publication; Vienna: 2020. World Drug Report 2020 Methodology Report. [Google Scholar]
- 35.European Monitoring Centre for Drugs and Drug Addiction . European Monitoring Centre for Drugs and Drug Addiction; Lisbon, Portugal: 2021. Statistical bulletin 2021. [Google Scholar]
- 36.Seitz N-N, John L, Atzendorf J, Rauschert C, Kraus L. Kurzbericht Epidemiologischer Suchtsurvey 2018. Tabellenband: Konsum illegaler Drogen, multiple Drogenerfahrung und Hinweise auf Konsumabhängigkeit und -missbrauch nach Geschlecht und Alter im. Jahr. 2018:2019. [Google Scholar]
- 37.European Monitoring Centre for Drugs and Drug Addiction . Publications Office of the European Union; Luxembourg: 2012. Treatment demand indicator (TDI). Standard protocol 3.0. [Google Scholar]
- 38.European Monitoring Centre for Drugs and Drug Addiction . Publications Office of the European Union; Luxembourg: 2016. TDI Methodological information on 30 European countries. Methods and Definitions of TDI data reported to the EMCDDA in 2014. [Google Scholar]
- 39.European Monitoring Centre for Drugs and Drug Addiction . European Monitoring Centre for Drugs and Drug Addiction; Lisbon, Portugal: 2021. Statistical Bulletin 2021 — methods and definitions for price, purity and potency. [Google Scholar]
- 40.Schneider F. Potency levels of herbal cannabis and resin in Germany between 2010 and 2019. Deutsche Beobachtungsstelle für Drogen und Drogensucht. 2021 [Google Scholar]
- 41.United Nations Office on Drugs and Crime. dataUNODC. 2021.
- 42.Institute for Health Metrics and Evaluation . University of Washington; Seattle, USA: 2021. GBD Results Tool. [Google Scholar]
- 43.Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat . Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat; New York, USA: 2019. World Population Prospects: The 2019 Revision, Key Findings and Advance Tables. [Google Scholar]
- 45.R Core Team . 4.0.5 ed. R Foundation for Statistical Computing; Vienna, Austria: 2021. R: A language and environment for statistical computing. [Google Scholar]
- 46.The ESPAD Group . Publications Office of the European Union; Luxembourg: 2020. ESPAD Report 2019. Results from the European School Survey Project on Alcohol and Other Drugs. [Google Scholar]
- 47.Mauro PM, Carliner H, Brown QL, et al. Age differences in daily and nondaily cannabis use in the United States, 2002–2014. J Stud Alcohol Drugs. 2018;79(3):423–431. doi: 10.15288/jsad.2018.79.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Calomarde-Gómez C, Jiménez-Fernández B, Balcells-Oliveró M, Gual A, López-Pelayo H. Motivational interviewing for cannabis use disorders: a systematic review and meta-analysis. Eur Addict Res. 2021:1–15. doi: 10.1159/000515667. [DOI] [PubMed] [Google Scholar]
- 49.Gates PJ, Sabioni P, Copeland J, Le Foll B, Gowing L. Psychosocial interventions for cannabis use disorder. Cochrane Database Syst Rev. 2016;(5) doi: 10.1002/14651858.CD005336.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lees R, Hines LA, D'Souza DC, et al. Psychosocial and pharmacological treatments for cannabis use disorder and mental health comorbidities: a narrative review. Psychol Med. 2021;51(3):353–364. doi: 10.1017/S0033291720005449. [DOI] [PubMed] [Google Scholar]
- 51.Freeman TP, Craft S, Wilson J, et al. Changes in delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) concentrations in cannabis over time: systematic review and meta-analysis. Addiction. 2021;116(5) doi: 10.1111/add.15253. [DOI] [PubMed] [Google Scholar]
- 52.Chandra S, Radwan MM, Majumdar CG, Church JC, Freeman TP, ElSohly MA. New trends in cannabis potency in USA and Europe during the last decade (2008-2017) Eur Arch Psychiatry Clin Neurosci. 2019 doi: 10.1007/s00406-019-00983-5. [DOI] [PubMed] [Google Scholar]
- 53.Freeman TP, Groshkova T, Cunningham A, Sedefov R, Griffiths P, Lynskey MT. Increasing potency and price of cannabis in Europe, 2006–16. Addiction. 2019;114(6):1015–1023. doi: 10.1111/add.14525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the united states between 2001-2002 and 2012-2013. JAMA Psychiatry. 2015;72(12):1235–1242. doi: 10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Murray RM, Quigley H, Quattrone D, Englund A, Di Forti M. Traditional marijuana, high-potency cannabis and synthetic cannabinoids: increasing risk for psychosis. World Psychiatry. 2016;15(3):195–204. doi: 10.1002/wps.20341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rehm J, Kilian C, Rovira P, Shield KD, Manthey J. The elusiveness of representativeness in general population surveys for alcohol. Drug Alcohol Rev. 2021;40(2):161–165. doi: 10.1111/dar.13148. [DOI] [PubMed] [Google Scholar]
- 57.European Monitoring Centre for Drugs and Drug Addiction. PERSPECTIVES ON DRUGS: wastewater analysis and drugs: a European multi-city study, 2020. accessed 17 March 2021.
- 58.Gonzalez-Marino I, Baz-Lomba JA, Alygizakis NA, et al. Spatio-temporal assessment of illicit drug use at large scale: evidence from 7 years of international wastewater monitoring. Addiction. 2020;115(1):109–120. doi: 10.1111/add.14767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Werschler T, Brennan A. Wastewater-based estimates of cannabis and drug use in Canada: pilot test detailed results. 2019. https://www150.statcan.gc.ca/n1/pub/11-621-m/11-621-m2019004-eng.htm accessed 17 March 2021.
- 60.Schmidt-Wolf G, Cremer-Schaeffer P. Three years of cannabis as medicine-preliminary results of the survey accompanying the prescription of medical cannabis in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2021;64(3):368–377. doi: 10.1007/s00103-021-03285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Salas-Wright CP, Vaughn MG, Cummings-Vaughn LA, et al. Trends and correlates of marijuana use among late middle-aged and older adults in the United States, 2002–2014. Drug Alcohol Depend. 2017;171:97–106. doi: 10.1016/j.drugalcdep.2016.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baumeister SE, Baurecht H, Nolde M, et al. Cannabis use, pulmonary function, and lung cancer susceptibility: a Mendelian randomization study. J Thorac Oncol. 2021 doi: 10.1016/j.jtho.2021.03.025. [DOI] [PubMed] [Google Scholar]
- 63.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. doi: 10.1136/bmj.e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rogeberg O, Elvik R. The effects of cannabis intoxication on motor vehicle collision revisited and revised. Addiction. 2016;111(8):1348–1359. doi: 10.1111/add.13347. [DOI] [PubMed] [Google Scholar]
- 65.Lloyd SL, Lopez-Quintero C, Striley CW. Sex differences in driving under the influence of cannabis: the role of medical and recreational cannabis use. Addict Behav. 2020;110 doi: 10.1016/j.addbeh.2020.106525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Caulkins JP. Recognizing and regulating cannabis as a temptation good. The International Journal on Drug Policy. 2017;42:50–56. doi: 10.1016/j.drugpo.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 67.Manthey J, Rehm J. Mortality from alcoholic cardiomyopathy: exploring the gap between estimated and civil registry data. J Clin Med. 2019;8(8) doi: 10.3390/jcm8081137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wan X, Yang GH. Is the mortality trend of ischemic heart disease by the GBD2013 study in China Real? Biomed Environ Sci. 2017;30(3):204–209. doi: 10.3967/bes2017.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Freeman TP, Lorenzetti V. ‘Standard THC units’: a proposal to standardize dose across all cannabis products and methods of administration. Addiction. 2020;115(7):1207–1216. doi: 10.1111/add.14842. [DOI] [PubMed] [Google Scholar]
- 70.López-Pelayo H, Matrai S, Balcells-Olivero M, et al. Standard units for cannabis dose: Why is it important to standardize cannabis dose for drug policy and how can we enhance its place on the public health agenda? International Journal of Drug Policy. 2021;97:103350. doi: 10.1016/j.drugpo.2021.103350. [DOI] [PubMed] [Google Scholar]
- 71.Callaghan RC, Sanches M, Benny C, Stockwell T, Sherk A, Kish S. Who consumes most of the cannabis in Canada? Profiles of cannabis consumption by quantity. Drug Alcohol Depend. 2019 doi: 10.1016/j.drugalcdep.2019.107587. [DOI] [PubMed] [Google Scholar]
- 72.Niesink RJ, Rigter S, Koeter MW, Brunt TM. Potency trends of Delta9-tetrahydrocannabinol, cannabidiol and cannabinol in cannabis in the Netherlands: 2005-15. Addiction. 2015;110(12):1941–1950. doi: 10.1111/add.13082. [DOI] [PubMed] [Google Scholar]
- 73.Arterberry BJ, Treloar Padovano H, Foster KT, Zucker RA, Hicks BM. Higher average potency across the United States is associated with progression to first cannabis use disorder symptom. Drug Alcohol Depend. 2018 doi: 10.1016/j.drugalcdep.2018.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Freeman TP, Winstock AR. Examining the profile of high-potency cannabis and its association with severity of cannabis dependence. Psychol Med. 2015;45(15):3181–3189. doi: 10.1017/S0033291715001178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Di Forti M, Quattrone D, Freeman TP, et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. The Lancet Psychiatry. 2019 doi: 10.1016/S2215-0366(19)30048-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hines LA, Freeman TP, Gage SH, et al. Association of high-potency cannabis use with mental health and substance use in adolescence. JAMA Psychiatry. 2020;77(10):1044–1051. doi: 10.1001/jamapsychiatry.2020.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chouvy PA, Macfarlane J. Agricultural innovations in Morocco's cannabis industry. Int J Drug Policy. 2018;58:85–91. doi: 10.1016/j.drugpo.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 78.Leung J, Stjepanović D, Dawson D, Hall WD. Do cannabis users reduce their THC dosages when using more potent cannabis products? A review. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.630602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Freeman AM, Petrilli K, Lees R, et al. How does cannabidiol (CBD) influence the acute effects of delta-9-tetrahydrocannabinol (THC) in humans? A systematic review. Neurosci Biobehav Rev. 2019;107:696–712. doi: 10.1016/j.neubiorev.2019.09.036. [DOI] [PubMed] [Google Scholar]
- 80.Mongeau-Perusse V, Jutras-Aswad D. Challenging CBD protective effect against THC-related outcomes: a call for robust clinical trials. Addiction. 2020 doi: 10.1111/add.15254. [DOI] [PubMed] [Google Scholar]
- 81.Manthey J. Cannabis use in Europe: current trends and public health concerns. Int J Drug Policy. 2019;68:93–96. doi: 10.1016/j.drugpo.2019.03.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.