Abstract
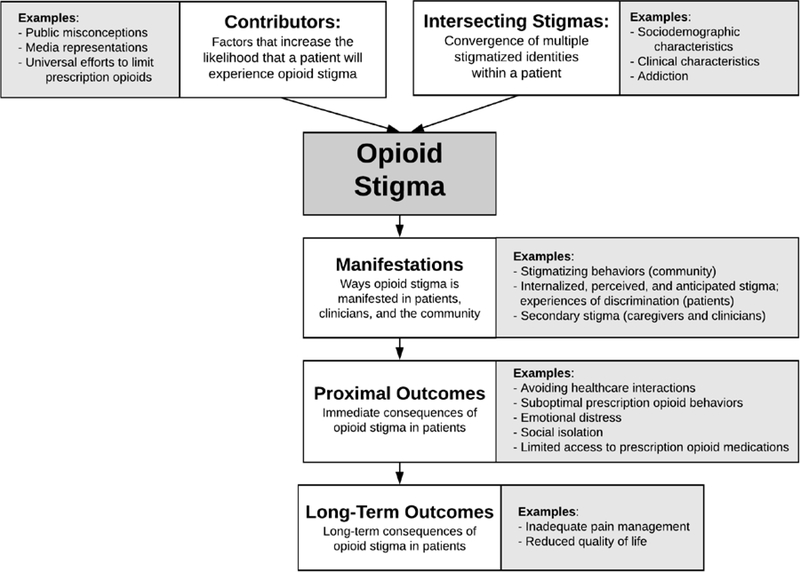
Millions of patients with cancer pain are treated with prescription opioids each year. However, efforts to mitigate the ongoing opioid crisis result in unintended consequences with opioid pain management, including opioid stigma. Emerging research indicates that opioid stigma is problematic in patients with cancer, but few studies have examined contributors to and impacts of opioid stigma in this population. To guide future research in this area, we propose a conceptual framework – the Opioid Stigma Framework, or OSF – with which to understand and improve opioid stigma in patients with cancer pain. Development of the OSF was guided by a literature review of stigma in health-related conditions, adaptation of the existing Health Stigma and Discrimination Framework, a topical review of challenges related to opioid cancer pain management, and author expertise in cancer, pain, and opioid prescribing. The proposed OSF highlights five domains: 1) contributors to opioid stigma, or factors that increase the likelihood that a patient will experience opioid stigma; 2) intersecting stigmas, or the convergence of multiple stigmatized identities within a patient; 3) stigma manifestations, or the ways opioid stigma is manifested in patients, clinicians, and the community; 4) proximal outcomes, or the immediate consequences of opioid stigma in patients; and 5) long-term impacts in patients. The OSF provides two main avenues to facilitate future research: 1) providing a framework to explore the mechanisms that underlie opioid stigma and its impact on cancer pain management, and 2) supporting the development of targeted, tailored interventions to eliminate opioid stigma.
INTRODUCTION
Roughly 16.9 million cancer survivors live in the United States, with almost 1.9 million new diagnoses anticipated this year.[2,62,71,82] Approximately half of all patients with cancer will experience pain related to their disease process and/or treatment, with rates rising to 75% in advanced disease.[8,9] Effective pain management is integral to comprehensive cancer care and to enhance patient quality of life.[12,59,66,88] Prescription opioids are routinely prescribed for moderate-to-severe cancer pain management, which is an evidence-based practice supported by many professional guidelines.[4,37,63,102]
The ongoing opioid crisis complicates the use of prescription opioids in the United States.[96] Opioid prescribing for pain contributed to sharp increases in opioid-related morbidity and mortality, resulting in negative public attitudes toward prescription opioids and heightened scrutiny toward opioid prescribing practices.[61,96] As a result, professional guidelines and state-level legislation now broadly encourage cautious, conservative use of opioids for pain management.[29] Although opioid limitations commonly exempt cancer pain, patients with cancer may still experience adverse consequences.[3,4,68,79,95] Opioid stigma is one such consequence.[16]
Health-related stigma (e.g., stigma related to health conditions), or the labelling of traits as socially undesirable, is broadly recognized as a barrier to achieving optimal proximal and long-term health outcomes in medical patients.[31,33,38,40,57,73,90,91] When applied to cancer pain, opioid stigma may manifest as internalized fears about one’s own prescription opioid use, anticipated judgments from others, and/or experiences of discrimination. Additionally, stigma presents many barriers to achieving optimal health outcomes, whether by limiting engagement in care, impeding proactive health behaviors, reducing resource availability and social support, and/or exacerbating emotional distress.[22,33,38,40,57,73,76,90,91,101] It is now established that opioid stigma is problematic in patients with cancer pain. Our prior work explored opioid stigma in patients undergoing active cancer treatment seen in a supportive care clinic. Of 97 respondents prescribed opioids, 61% of patients endorsed at least one aspect of opioid stigma. Additionally, 29% of these participants endorsed stigma-related behaviors, primarily centered on taking less opioid medication than needed (20%). This research suggests that opioid stigma has the potential to be highly impactful in patients with cancer.[16] However, few studies have examined potential contributors to and ameliorating factors of opioid stigma, nor are the lasting effects of stigmatizing experiences well understood in this population. Future research is critical to understand and intervene on opioid stigma in patients with cancer.
Development of a conceptual framework is a critical step to guide research in opioid stigma. This paper proposes a conceptual Opioid Stigma Framework (OSF) with which to understand and improve opioid stigma in patients with cancer pain. We then discuss several avenues for future research in opioid stigma using the OSF as a guide.
METHODS
The goal of framework development is to identify factors that relate to the central concept – here, opioid stigma in cancer pain – and describe proposed relationships between these factors, as well as potential targets for intervention.[42] There is no standardized methodology for the creation of a conceptual framework, though common approaches include adapting existing frameworks, integrating expert opinion, and evaluating existing literature conceptually related to the central concept.[34,70] Thus, our approach to the OSF began with a broad review of stigma in health-related conditions, including HIV,[31,33,81,91] obesity,[73] mental health,[23,40] and chronic pain.[76,101,103] From this literature, we selected an existing framework as a guide (described below).[83] We also conducted a topical review of existing literature in challenges related to opioid pain management and cancer pain, with emphasis on potential contributors to or consequences of opioid stigma.
Using this literature and our prior pilot work [16], we proposed factors related to the experience of opioid stigma and adapted the guiding framework to reflect these factors. We gathered a transdisciplinary group of co-authors with clinical and research expertise in cancer, pain, opioid prescribing, and health-related stigma and presented the proposed OSF to them for feedback on proposed concepts and to generate additional contributors and consequences of opioid stigma. The OSF was revised according to co-author feedback. Finally, we created a figure to represent the OSF (Figure 1).
Figure 1.
Proposed opioid stigma framework.
GUIDING CONCEPTUAL FRAMEWORK
The existing framework that we chose to serve as our guide was the Health Stigma and Discrimination Framework (HSDF), a multi-level theoretical framework that articulates the stigmatization process as a progressive series of domains.[83] The HSDF has several advantages over other conceptual models of stigma. For example, unlike prior stigma models that focus solely on one disease process, the HSDF integrates common contributors to and consequences of stigma across patient groups. Additionally, the HSDF uses a comprehensive socio-ecological framing that includes individual, interpersonal, community, organizational, and public policy factors. Thus far, applications of the HSDF focus on stigma related to health conditions rather than medical treatments, making our interpretation unique.
PROPOSED APPLICATION OF THE HSDF TO OPIOID STIGMA IN CANCER PAIN
In this section, we describe each of the HSDF domains as adapted for the OSF. In some cases, the original HSDF domains have been simplified for clarity. A visual depiction of the OSF is presented in Figure 1.
Contributors to Opioid Stigma
Contributors to opioid stigma increase the likelihood that a patient with cancer pain will experience opioid stigma. This includes public misconceptions regarding the relative risks and benefits of prescription opioids for pain management. Prescription opioids are often clinically indicated for cancer pain management. However, in light of the rising rates of opioid use disorder and opioid-related mortality, emphasis is increasingly placed on the risks of prescription opioid use. Weighing the risks and benefits of prescription opioids is a nuanced, personal choice in conjunction with clinician recommendations, and making informed decisions can be difficult for patients. For example, patients may have difficulty understanding the likelihood of side effects, risks of addiction and overdose when used as prescribed, and relative strength of the evidence for opioid management in cancer pain versus other painful conditions. Additionally, qualitative interviews in this area indicate that patients with chronic pain engaged in palliative care (including patients with cancer) associate prescription opioids with death and dying.[43]
Media representations of prescription opioid use may also contribute to opioid stigma. Media broadcasts use the term “opioid crisis” to describe a broad range of issues and opioid types (e.g., prescription opioids, heroin, fentanyl), which contributes to public confusion about the definition of an “opioid.” Conflating medical and non-medical opioid use likely contributes to public skepticism and suspicion of patients who use opioids to manage cancer pain. Media campaigns may further contribute to negative stereotypes by highlighting stories of fraudulent injuries. For example, a 2018 “The Truth about Opioids” ad campaign produced by the Truth Initiative and the White House Office of National Drug Control Policy (ONDCP) ran graphic ads depicting young adults injuring themselves with hammers and doors and intentionally wrecking vehicles in order to obtain prescription opioids.[64] Bias created by media campaigns may hinder patients from feeling comfortable disclosing their pain, asking questions about their opioids, and discussing management options with their healthcare providers.
Finally, universal efforts to limit prescription opioids may present additional challenges with stigma, including increasing patient burden required to access prescription opioids, internalized stigma for patients with cancer pain, and public skepticism. Multiple federal and state-level efforts broadly aim to curb opioid prescribing. For example, the United States government declared the opioid crisis to be a national public health emergency in 2018, and a Presidential initiative was announced with the explicit aim of decreasing nationwide opioid prescriptions by a third within a 3-year period.[87] Similarly, the Centers for Disease Control and Prevention (CDC)’s 2016 guidelines advocating for conservative prescription opioid practices were associated with an overall decline in prescribing, sparking concerns about misapplication to patients with cancer.[28,29,53] State laws now commonly restrict opioid prescribing for acute pain, reflecting CDC recommendations. Cancer pain is often explicitly exempted from prescription opioid limitations. However, research indicates that opioid prescriptions for patients with cancer have significantly declined in recent years, coinciding with changes in federal and state guidance.[36,48]
Intersecting Stigmas
Intersecting stigmas refers to the convergence of multiple stigmatized identities within a person or group.[11,92] When stigmas intersect, negative consequences can emerge above beyond the effects of any single source of stigma. Pain management for patients who are socially marginalized is already challenging, and sociodemographic characteristics such as race/ethnicity, sex/gender identity, and socioeconomic status (SES) of the patient may compound opioid stigma.[25] For example, women and patients of color are more likely to report under- or un-managed pain.[5,7,44,45,85] People of color are also less likely to be offered prescription opioids, more likely to encounter access issues at the pharmacy, and often undergo more oversight throughout the duration of their treatment (e.g., frequent urinary drug monitoring) as compared to non-Hispanic white patients.[5,44,45,85] Similarly, opioids are prescribed less frequently in emergency room visits for patients in the lowest quartile of SES as compared to those in the highest quartile, regardless of whether SES was measured as poverty, household income, or educational level.[50]
Clinical characteristics of the patient present additional sources of intersecting stigma. Stigma is associated with certain cancer diagnoses depending on perceived causes of the disease, including whether the patient is considered responsible for their cancer and whether the disease is physically obvious to observers. For example, lung cancer is highly stigmatized due to widespread negative attitudes toward smoking and physical abnormalities associated with these diagnoses (e.g., disfigurement of the mouth).[18,80] In stigmatized patients with cancer, negative attitudes may extend to cancer pain itself (e.g. “they brought it on themselves”) and prescription opioid management strategies (e.g., perceiving prescription opioid use as a sign of weakness). Notably, stigma can also associated with conditions that commonly co-occur with cancer, such as pre-existing chronic pain. Patients with chronic pain may be accustomed to being viewed as “difficult patients” to manage.[22] Prior stigmatizing experiences associated with chronic pain management may also impact how opioid stigma manifests in a patient with cancer pain.
Stigma associated with addiction is well-documented and presents another avenue for intersecting stigma.[1,10,89] Addiction is commonly viewed as a moral weakness associated with negative stereotypes, resulting in the patient being blamed for their own diagnosis and labeled a “substance abuser.” Treatment for addiction is similarly stigmatized, which results in difficulty accessing and engaging in potentially helpful interventions. In patients with co-occurring addiction and pain, navigating safe and effective opioid strategies can be particularly challenging.[14,19,20,74] Clinicians may be wary of prescribing opioids and lack comprehensive education on addiction management.[51] Meanwhile, patients with co-occurring pain and addiction may be wary of accurately reporting their pain and addiction behaviors, especially if they believe their clinician will discontinue their opioid prescription or engage in stigmatizing behaviors.[10,60,106]
Stigma Manifestations
Opioid stigma manifestations comprise: 1) stigmatizing behaviors reflecting negative public attitudes, stereotypes, and judgments about patients who use prescription opioids; 2) manifestations specific to the patient experience, including perceived stigma, reflecting the patient’s perceptions of public attitudes and stereotypes; internalized stigma, in which the patient absorbs and applies these negative attitudes toward themselves; anticipated stigma, in which patients expect poor treatment in the future; and direct experiences of discrimination; and 3) secondary stigma, in which people associated with the patient (e.g., support systems and/or clinicians) are negatively impacted by opioid stigma.[24,31,33]
Stigmatizing behaviors are enacted by other people and reveal negative attitudes, stereotypes, and judgments towards patients who use opioids.[83] In the public sphere, stigmatizing behaviors may include members of the community gossiping about patients who use prescription opioids, exclusion, and social isolation of the patient. In healthcare settings, clinicians and pharmacists may exhibit skepticism towards patients who request opioids for pain management and leverage additional clinical oversight measures.
Opioid stigma can also be manifested in a variety of the patient’s own experiences.[83] Perceived stigma refers to the patient’s perceptions of public attitudes and stereotypes.[15,52] Perceptions of stigma can reflect unflattering media representations of prescription opioids; perceived barriers to opioid access in the clinic or pharmacy; experiences with suspicious friends, or family; and encounters with skeptical clinicians. Internalized stigma occurs when patients absorb these negative attitudes and apply them personally.[38,57,90] For example, patients who internalize opioid stigma may come to believe that they are responsible for or deserve their pain, feel that they are being punished, express less confidence in their ability to manage their opioid prescriptions, and/or feel that they do not deserve to be included in their community and social activities. Anticipated stigma refers to expectations of poor treatment in the future.[32] Patients may avoid potentially unpleasant healthcare encounters, anticipate judgment or stereotyping from friends, family, or clinicians, and/or worry about how their community may perceive their prescription opioid use. Finally, patients with cancer pain may also report direct experiences of discrimination related to opioid stigma, limiting their access to prescription opioids when needed. Patients with cancer pain report difficulty with filling prescriptions, obtaining a prescription from a clinician, barriers in insurance approval, and feeling judged by clinicians.[16]
A final category of stigma manifestations is secondary or associative stigma, which impacts people associated with the patient (e.g., support systems or clinicians).[98,99] Support people such as family members or close friends may be integrally involved in a patient’s opioid pain management, with tasks ranging from attending medical appointments, organizing daily pills, and/or picking up medications from the pharmacy. Stigma may extend to support people if they are viewed as permissive or enabling of the patient’s prescription opioid use, or if others believe that these support people are likely to use or divert the prescription medications themselves. Clinicians who prescribe opioids for cancer pain may also be targets of secondary stigma. Cancer pain is treated by a variety of specialties, from oncologists to palliative care physicians to primary care physicians in the community.[56,65] Given the increased regulatory oversight, clinicians may worry about scrutiny of their prescribing practices and fear legal prosecution.[27,47] Clinicians may also be pejoratively labeled (e.g., “pill-pushers”) and blamed for their perceived role in the opioid crisis. Secondary stigma comes at a high cost: stigmatized clinicians report decreased job satisfaction and increased burnout.[105]
Proximal Outcomes
Potential proximal outcomes associated with opioid stigma include patients limiting or avoiding healthcare interactions, suboptimal prescription opioid behaviors, emotional distress, and social isolation. Additionally, we anticipate that opioid stigma reaches clinicians and health systems, which in turn limits patient access to opioid pain management.
Opioid stigma may lead patients to avoid healthcare interactions, characterized by canceling or no-showing to medical appointments, declining referrals to pain management specialists, and/or deflecting awkward conversations about pain and prescription opioids. Patients may be unsure how to phrase questions about their opioids and worry that their clinicians will respond with suspicion or skepticism.[16,39,86] They may also be fearful of abrupt opioid tapers. Unfortunately, patients who avoid healthcare interactions lose important opportunities to become integrally involved in their own healthcare, source reliable health information, and clarify misconceptions.
Patients who experience opioid stigma may also begin to engage in suboptimal prescription opioid behaviors. Hoarding, saving medication for a future need, and generally under-using opioid prescriptions can be suboptimal behaviors that directly impact patients’ pain control, while simultaneously increasing the amount of opioids available in the community for possible diversion. Alternatively, some patients may opt to decline prescription opioids or not fill prescriptions at the pharmacy due to stigma-related fears.[16]
Based on other models of pain and health-related stigma, we anticipate that stigmatized patients with cancer pain experience emotional distress such as fear, anxiety, irritability, and awkwardness, particularly when interacting with their clinicians. Patients may also feel distrustful of the medical system and lack confidence in their clinicians, spurring a sense of helplessness and perceived injustice.[31,57,72,91]
Social support is an important aspect of comprehensive cancer care and pain management interventions. However, experiences with opioid stigma can contribute to social isolation in stigmatized patients. Patients who use prescription opioids may avoid discussing pain with their family and friends, similar to avoidance of clinicians. Additionally, a subset of patients may avoid social events where other people may notice their opioid use (e.g., taking medications or using a patch).[16]
Clinicians may also be impacted by opioid stigma, which can result in limited access to opioids for patients with cancer pain. Clinicians may endorse negative perceptions of patients with pain, view opioid pain management as time-intensive and burdensome, and avoid conversations with patients about their prescription opioids due to awkwardness or lack of knowledge.[13,54,78,97] Additionally, clinicians can be the targets of secondary stigma themselves (described above, Stigma Manifestations). As a result, clinicians may be reluctant to treat cancer-related pain, decline to prescribe opioids, and/or opt to refer to pain management specialists.
On a systemic level, broad efforts to minimize prescribing as an opioid crisis management strategy also limit access to opioids for patients with cancer pain. Insurance restrictions, federal and state-level regulations, and recommendations from professional groups have been complex and inconsistently applied. For example, the CDC’s 2016 guidelines advocating for more conservative opioid prescribing were intended to address a narrow group of patients: adults with non-cancer pain treated in primary care settings.[29] However, the guidelines were adopted widely by health plans and clinical practices outside of the guideline’s scope. State laws that limit opioid prescribing have sparked similar concerns about legal repercussions, pill counts, and exempted patient groups, leading Medical Boards and the CDC to publish clarifications of their intent.[93,100] Insurance policies are also a powerful force in opioid prescribing. In many states, Medicare and Medicaid impose opioid quanitity limits and require exception submissions to approve higher quantities.[41,94] In general, misapplication can impact patient ability to access opioid medications and specialty care, limit time allotted with their clinicians, and increase financial burden and pharmacy shortages. Additionally, forced opioid tapers are dangerous and destabilizing, increase patient suffering, and preclude patient-centered care.[26]
Long-term Impacts
As yet, little is known about the long-term impacts of opioid stigma in patients with cancer pain. However, given anticipated proximal outcomes and drawing from other health-related stigma literature, we posit that there are two significant, long-term impacts of opioid stigma that occur as a direct result of negative proximal outcomes: inadequate pain management and reduced quality of life.
Prescription opioids are recommended for the management of moderate-to-severe cancer-related pain, as supported by decades of national and international guidelines.[4,37,63] Ideally, clinicians would couple these recommendations with a comprehensive pain assessment to guide personalized opioid prescribing for each patient’s unique needs. Such an assessment should account for the patient’s current pain intensity and management strategies, their pain history and prior treatments, previous or current addiction to opioids or other substances, and potential misuse risk factors that may complicate the success of prescription opioid pain management.[17,49,69,77,104] A comprehensive and personalized pain management plan requires frequent and open communication between the clinician and patient. If patients are avoiding healthcare appointments, feel awkward and uncomfortable discussing their pain in clinic, decline clinically indicated prescription opioid medications, and engage in suboptimal opioid behaviors, their pain is likely to go under- or untreated.[16] Similarly, if clinicians limit their prescribing due to secondary stigma and fear of oversight, inadequate pain management is an inevitable long-term outcome.[67]
Similarly, research indicates that patients who experience stigma have reduced quality of life. Quality of life is a multifaceted concept comprised of many components, including functional limitations, inability to work, disturbed sleep, reduced physical activity levels and energy, a reduced sense of self-efficacy and confidence, psychological distress, and social isolation.[30,55] For patients with cancer pain, this experience is likely compounded by inadequate pain management.[21,32,35] More research is needed to understand the extent to which opioid stigma reduces specific components of quality of life.
DISCUSSION AND FUTURE DIRECTIONS
The OSF offers an innovative conceptualization of an understudied challenge in cancer pain management: opioid stigma. It is broadly recognized that enhancing pain management – including reducing barriers to effective treatment strategies – is a key national priority in pain research. The OSF could be a key component in addressing this pressing clinical need.
The OSF provides three main avenues for future research in this novel, developing area. Foundational mixed-methods research is needed to fully understand the scope and trajectory of opioid stigma, its impact on proximal and long-term health outcomes, potential ameliorating factors, and how to systematically measure it. Research with key stakeholders that centers the experiences of patients with cancer pain will help to identify crucial intervention targets, including contributors and consequences of opioid stigma that are not yet known. From the very earliest stages onward, input from diverse stakeholders is needed to understand how opioid stigma may present differently in patients who experience intersecting sources of stigma, such as patients from ethnic and racial minority groups, low socioeconomic status backgrounds, and with a variety of disease types and addiction histories. A psychometrically validated measure of opioid stigma is also needed to ensure standardized assessment and comparison across future studies. Such a tool is crucial in order to reliably assess the scope and impact of opioid stigma in patients with cancer.
The second role of the OSF is to support the development of targeted, tailored interventions that reduce or eliminate opioid stigma entirely. Prior research suggests that interventions to improve stigma by increasing stigma-related knowledge, attitudes, and intended behaviors can be successful in patients with medical and/or mental health conditions. [46,58,84], and a recent systemic review indicated that the majority of multi-level stigma-reduction interventions resulted in statistically significant decreases in stigma[75]. The OSF outlines multiple levels at which stigma may be leveraged and/or experienced, including patients, clinicians, communities, and healthcare systems. Thus, multiple targets are needed in the development of novel opioid stigma interventions. We anticipate that patient-, support person-, and clinician-level interventions would include tailored education, communication skills training, and facilitation of safe, effective opioid prescribing and adherence behaviors appropriate for each level. Systemic interventions in healthcare systems, insurance policies, and state- and federal-level legislation should focus on designing clinically relevant and nuanced guidelines for opioid prescribing that account for diverse, individualized pain management needs across the cancer continuum. Future work can use the OSF to guide the design of stigma interventions, including treatment targets (e.g., stigmatizing behaviors) and outcome measures (e.g., successful pain management).
Finally, the OSF is primarily focused on patients who report pain associated with an active cancer diagnosis. Evidence supporting opioid pain management is strongest in this patient group, who have high rates of moderate-to-severe pain, are legally exempt from opioid prescribing laws in most states, and for whom opioid pain management is considered to be the standard of care. Emerging literature in this area also focuses on the scope and impact of opioid stigma in patients with active disease, including patients with advanced cancer.[6,16] However, additional research is needed to examine how applicable this framework is for a diverse group of patients, including sociodemographic groups (e.g., aging patients, patients with medical co-morbidities that complicate treatment) and clinical subgroups. For example, little is known about the extent of stigmatizing experiences in cancer survivors, who may experience unique challenges associated with chronic cancer pain as they transition out of active treatment and into survivorship (e.g., shifting risks and benefits for prescription opioids over time, intersecting chronic pain stigma, barriers to accessing specialty care, etc). Future research should examine unique stigmatizing experiences across patient subgroups, and we plan to update the OSF accordingly.
LIMITATIONS
The proposed OSF has several limitations to consider. First, because literature examining opioid stigma in cancer pain is limited, the OSF is not finalized. Rather, it is intended to be a modifiable guideline for future research, which can be updated as new information is collected. Second, although we conducted a topical literature review to understand existing research on this topic, the sparsity of literature in this area suggests that there are likely additional contributors and consequences of opioid stigma that have not been identified yet. Finally, while we did not include non-cancer related pain in our present model, a similar approach may also be taken for non-cancer pain conditions.
CONCLUSIONS
The OSF offers a conceptual framework with which to understand proposed contributors to and consequences of a novel and emerging research area: opioid stigma in cancer pain. The OSF is intended to be hypothesis-generating and support innovative future research to better understand mechanisms that underlie opioid stigma’s influence on cancer pain management. We anticipate that as this literature grows, we will update and adapt the OSF as well. Continued research is crucial to expand our understanding of these mechanisms, update the OSF, and design tailored, targeted interventions to eradicate opioid stigma.
Acknowledgements:
Dr. Bulls’ time was financially supported by an institutional K award at the University of Pittsburgh (NIH KL2 TR001856 (PI: Doris Rubio)).
REFERENCES
- [1].Adams JM, Volkow ND. Policy forum: Ethical imperatives to overcome stigma against people with substance use disorders. AMA J Ethics 2020;22:702–708. [DOI] [PubMed] [Google Scholar]
- [2].American Cancer Society . Cancer Facts and Figures 2021. 2021. p. Available: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf. Accessed 4 Mar 2021.
- [3].American Society of Clinical Oncology (ASCO). ASCO Policy Brief on Opioid Therapy and Access to Treatment. 2016. Available: https://www.asco.org/sites/new-www.asco.org/files/content-files/advocacy-and-policy/documents/2016-Opioid-policy-brief.pdf.
- [4].American Society of Clinical Oncology (ASCO). ASCO Policy Statement on Opioid Therapy: Protecting Access to Treatment for Cancer-Related Pain. 2016. Available: https://www.asco.org/sites/new-www.asco.org/files/content-files/advocacy-and-policy/documents/2016-ASCO-Policy-Statement-Opioid-Therapy.pdf.
- [5].Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain 2009;10:1187–1204. [DOI] [PubMed] [Google Scholar]
- [6].Azizoddin DR, Knoerl R, Adam R, Kessler D, Tulsky JA, Edwards RA. Cancer pain self-management in the context of a national opioid epidemic: Experiences of patients with advanced cancer using opioids. Cancer 2021. Available: https://abdn.pure.elsevier.com/en/publications/cancer-pain-self-management-in-the-context-of-a-national-opioid-e. Accessed 14 Apr 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth 2013;111:52–58. doi: 10.1093/bja/aet127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].van den Beuken-van Everdingen MHJ, Hochstenbach LMJ, Joosten EAJ, Tjan-Heijnen VCG, Janssen DJA. Update on Prevalence of Pain in Patients With Cancer: Systematic Review and Meta-Analysis. J Pain Symptom Manag 2016;51:1070–1090.e9. [DOI] [PubMed] [Google Scholar]
- [9].van den Beuken-van Everdingen MHJ, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J High prevalence of pain in patients with cancer in a large population-based study in The Netherlands. Pain 2007;132:312–320. doi: 10.1016/j.pain.2007.08.022. [DOI] [PubMed] [Google Scholar]
- [10].Van Boekel LC, Brouwers EPM, Van Weeghel J, Garretsen HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug Alcohol Depend 2013;131:23–35. [DOI] [PubMed] [Google Scholar]
- [11].Bowleg L The problem with the phrase women and minorities: Intersectionality-an important theoretical framework for public health. Am J Public Health 2012;102:1267–1273. doi: 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Breivik H, Cherny N, Collett B, de Conno F, Filbet M, Foubert AJ, Cohen R, Dow L. Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol 2009;20:1420–1433. [DOI] [PubMed] [Google Scholar]
- [13].Breuer B, Fleishman SB, Cruciani RA, Portenoy RK. Medical oncologists’ attitudes and practice in cancer pain management: A national survey. J Clin Oncol 2011;29:4769–4775. doi: 10.1200/JCO.2011.35.0561. [DOI] [PubMed] [Google Scholar]
- [14].Bruera E, Paice JA. Cancer Pain Management: Safe and Effective Use of Opioids. Am Soc Clin Oncol Educ B 2015:e593–e599. [DOI] [PubMed] [Google Scholar]
- [15].Budhwani H, De P. Perceived Stigma in Health Care Settings and the Physical and Mental Health of People of Color in the United States. Heal Equity 2019;3:73–80. doi: 10.1089/heq.2018.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bulls HW, Hoogland AI, Craig D, Paice J, Chang YD, Oberoi-Jassal R, Rajasekhara S, Haas M, Bobonis M, Gonzalez BD, Portman D, Jim HSL. Cancer and Opioids: Patient Experiences With Stigma (COPES)—A Pilot Study. J Pain Symptom Manage 2019;57:816–819. doi: 10.1016/j.jpainsymman.2019.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Caraceni A, Shkodra M. Cancer pain assessment and classification. Cancers (Basel) 2019;11. doi: 10.3390/cancers11040510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cataldo JK, Slaughter R, Jahan TM, Pongquan VL, Hwang WJ. Measuring stigma in people with lung cancer: psychometric testing of the cataldo lung cancer stigma scale. Oncol Nurs Forum 2011;38:E46–E54. doi: 10.1188/11.ONF.E46-E54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Chang YP, Compton P. Management of chronic pain with chronic opioid therapy in patients with substance use disorders. Addict Sci Clin Pract 2013;8:1–11. doi: 10.1186/1940-0640-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Cheatle M, Comer D, Wunsch M, Skoufalos A, Reddy Y. Treating pain in addicted patients: Recommendations from an expert panel. Popul Health Manag 2014;17:79–89. doi: 10.1089/pop.2013.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Cheng CM, Chang CC, Der Wang J, Chang KC, Ting SY, Lin CY. Negative impacts of self-stigma on the quality of life of patients in methadone maintenance treatment: The mediated roles of psychological distress and social functioning. Int J Environ Res Public Health 2019;16:1299. doi: 10.3390/ijerph16071299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Collier R “Complainers, malingerers and drug-seekers” - the stigma of living with chronic pain. CMAJ 2018;190:E204–E205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Corrigan P How stigma interferes with mental health care. Am Psychol 2004;59:614–625. [DOI] [PubMed] [Google Scholar]
- [24].Corrigan PW, Rafacz J, Rüsch N. Examining a progressive model of self-stigma and its impact on people with serious mental illness. Psychiatry Res 2011;189:339–343. doi: 10.1016/j.psychres.2011.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Craig KD, Holmes C, Hudspith M, Moor G, Moosa-Mitha M, Varcoe C, Wallace B. Pain in persons who are marginalized by social conditions. Pain 2020;161:261–265. doi: 10.1097/j.pain.0000000000001719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Darnall BD, Juurlink D, Kerns RD, Mackey S, Van Dorsten B, Humphreys K, Gonzalez-Sotomayor JA, Furlan A, Gordon AJ, Gordon DB, Hoffman DE, Katz J, Kertesz SG, Satel S, Lawhern RA, Nicholson KM, Polomano RC, Williamson OD, McAnally H, Kao MC, Schug S, Twillman R, Lewis TA, Stieg RL, Lorig K, Mallick-Searle T, West RW, Gray S, Ariens SR, Potter JS, Cowan P, Kollas CD, Laird D, Ingle B, Grove JJ, Wilson M, Lockman K, Hodson F, Palackdharry CS, Fillingim RB, Fudin J, Barnhouse J, Manhapra A, Henson SR, Singer B, Ljosenvoor M, Griffith M, Doctor JN, Hardin K, London C, Mankowski J, Anderson A, Ellsworth L, Budzinski LD, Brandt B, Hartley G, Heck DN, Zobrosky MJ, Cheek C, Wilson M, Laux CE, Datz G, Dunaway J, Schonfeld E, Cady M, Ledantec-Boswell T, Craigie M, Sturgeon J, Flood P, Giummarra M, Whelan J, Thorn BE, Martin RL, Schatman ME, Gregory MD, Kirz J, Robinson P, Marx JG, Stewart JR, Keck PS, Hadland SE, Murphy JL, Lumley MA, Brown KS, Leong MS, Fillman M, Broatch JW, Perez A, Watford K, Kruska K, You DS, Ogbeide S, Kukucka A, Lawson S, Ray JB, Martin TW, Lakehomer JB, Burke A, Cohen RI, Grinspoon P, Rubenstein MS, Sutherland S, Walters K, Lovejoy T. International stakeholder community of pain experts and leaders call for an urgent action on forced opioid tapering. Pain Med (United States) 2019;20:429–433. doi: 10.1093/pm/pny228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Dineen KK, DuBois JM. Between a Rock and a Hard Place: Can Physicians Prescribe Opioids to Treat Pain Adequately While Avoiding Legal Sanction? Am J Law Med 2016;42:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Dowell D, Haegerich T, Chou R. No Shortcuts to Safer Opioid Prescribing. N Engl J Med 2019;380:2285–2287. doi: 10.1056/nejmp1904190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States. MMWR Recomm Rep 2016;65:1–49. [DOI] [PubMed] [Google Scholar]
- [30].Drake K Quality of life for cancer patients. Nurs Manage 2012;43:20–25. doi: 10.1097/01.NUMA.0000410865.48922.18. [DOI] [PubMed] [Google Scholar]
- [31].Earnshaw VA, Chaudoir SR. From Conceptualizing to Measuring HIV Stigma: A Review of HIV Stigma Mechanism Measures. AIDS Behav 2009;13:1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Earnshaw VA, Quinn DM, Park CL. Anticipated stigma and quality of life among people living with chronic illnesses. Chronic Illn 2012;8:79–88. doi: 10.1177/1742395311429393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV Stigma Mechanisms and Well-Being among PLWH: A Test of the HIV Stigma Framework. AIDS Behav 2013;17:1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Earp JA, Ennett ST. Conceptual models for health education research and practice. Health Educ Res 1991;6:163–171. doi: 10.1093/her/6.2.163. [DOI] [PubMed] [Google Scholar]
- [35].El-Badri S, Mellsop G. Stigma and quality of life as experienced by people with mental illness. Australas Psychiatry 2007;15:195–200. doi: 10.1080/10398560701320089. [DOI] [PubMed] [Google Scholar]
- [36].Enzinger AC, Wright AA. Reduced Opioid Prescribing by Oncologists: Progress Made, or Ground Lost? JNCI J Natl Cancer Inst 2020. doi: 10.1093/jnci/djaa112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].ESMO Guidelines Committee, Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI, Committee EG. Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Ann Oncol 2018;29:iv166–iv191. doi: 10.1093/annonc/mdy152. [DOI] [PubMed] [Google Scholar]
- [38].Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Heal Soc Behav 2000;41:50–67. [PubMed] [Google Scholar]
- [39].Fischer MA, McKinlay JB, Katz JN, Gerstenberger E, Trachtenberg F, Marceau LD, Welch LC. Physician assessments of drug seeking behavior: A mixed methods study. PLoS One 2017;12. doi: 10.1371/journal.pone.0178690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Fox AB, Earnshaw VA, Taverna EC, Vogt D. Conceptualizing and Measuring Mental Illness Stigma: The Mental Illness Stigma Framework and Critical Review of Measures. Stigma Heal 2018;3:348–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Frontz AJ. Update on Oversight of Opioid Prescribing and Monitoring of Opioid Use: States Have Taken Action To Address the Opioid Epidemic. US Dep Heal Hum Serv Off Insp Gen; 2020. Available: https://oig.hhs.gov/oas/reports/region9/91801005.asp. [Google Scholar]
- [42].Bordage G, Caelleigh AS, Steinecke A, Bland CJ, Crandall SJ, McGaghie WC, Pangaro LN, Penn G, Regehr G, Shea JS JTF of AM and the G-RC. Review criteria for research manuscripts. Acad Med 2001;76:897–978. [PubMed] [Google Scholar]
- [43].Graczyk M, Borkowska A, Krajnik M. Why patients are afraid of opioid analgesics: A study on opioid perception in patients with chronic pain. Polish Arch Intern Med 2018;128:89–97. doi: 10.20452/pamw.4167. [DOI] [PubMed] [Google Scholar]
- [44].Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, Kalauokalani DA, Kaloukalani DA, Lasch KE, Myers C, Tait RC, Todd KH, Vallerand AH, Kalauokalani DA, Kaloukalani DA, Lasch KE, Myers C, Tait RC, Todd KH, Vallerand AH. The Unequal Burden of Pain: Confronting Racial and Ethnic Disparities in Pain. Pain Med 2003;4:277–294. Available: http://www.ncbi.nlm.nih.gov/pubmed/12974827. [DOI] [PubMed] [Google Scholar]
- [45].Green CR, Ndao-Brumblay SK, West B, Washington T. Differences in Prescription Opioid Analgesic Availability: Comparing Minority and White Pharmacies Across Michigan. J Pain 2005;6:689–699. doi: 10.1016/j.jpain.2005.06.002. [DOI] [PubMed] [Google Scholar]
- [46].Gronholm PC, Henderson C, Deb T, Thornicroft G. Interventions to reduce discrimination and stigma: the state of the art. Soc Psychiatry Psychiatr Epidemiol 2017;52:249–258. doi: 10.1007/s00127-017-1341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Hoffmann DE, Tarzian AJ. Achieving the Right Balance in Oversight of Physician Opioid Prescribing for Pain: The Role of State Medical Boards. J Law, Med Ethics 2003;31:21–40. [DOI] [PubMed] [Google Scholar]
- [48].Jairam V, Yang DX, Pasha S, Soulos PR, Gross CP, Yu JB, Park HS. Temporal Trends in Opioid Prescribing Patterns Among Oncologists in the Medicare Population. JNCI J Natl Cancer Inst 2020. doi: 10.1093/jnci/djaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Jovey RD. Opioids, pain and addiction – practical strategies. Br J Pain 2012;6:36–42. doi: 10.1177/2049463712439132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Joynt M, Train MK, Robbins BW, Halterman JS, Caiola E, Fortuna RJ. The impact of neighborhood socioeconomic status and race on the prescribing of opioids in emergency departments throughout the united states. J Gen Intern Med 2013;28:1604–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Keller CE, Ashrafioun L, Neumann AM, Van Klein J, Fox CH, Blondell RD. Practices, perceptions, and concerns of primary care physicians about opioid dependence associated with the treatment of chronic pain. Subst Abus 2012;33:103–113. [DOI] [PubMed] [Google Scholar]
- [52].Kinsler JJ, Wong MD, Sayles JN, Davis C, Cunningham WE. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDS 2007;21:584–592. doi: 10.1089/apc.2006.0202. [DOI] [PubMed] [Google Scholar]
- [53].Kroenke K, Alford DP, Argoff C, Canlas B, Covington E, Frank JW, Haake KJ, Hanling S, Hooten WM, Kertesz SG, Kravitz RL, Krebs EE, Stanos SP, Sullivan M. Challenges with Implementing the Centers for Disease Control and Prevention Opioid Guideline: A Consensus Panel Report. Pain Med 2019;20:724–735. doi: 10.1093/pm/pny307. [DOI] [PubMed] [Google Scholar]
- [54].Kwon JH. Overcoming barriers in cancer pain management. J Clin Oncol 2014;32:1727–1733. doi: 10.1200/JCO.2013.52.4827. [DOI] [PubMed] [Google Scholar]
- [55].Lavdaniti M, Tsitsis N. Definitions and Conceptual Models of Quality of Life in Cancer Patients. iMedPub, n.d. p. Available: http://journals.imedpub.com. Accessed 3 Feb 2021.
- [56].Lawrence RA, McLoone JK, Wakefield CE, Cohn RJ. Primary Care Physicians’ Perspectives of Their Role in Cancer Care: A Systematic Review. J Gen Intern Med 2016;31:1222–1236. doi: 10.1007/s11606-016-3746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Soc Sci Med 2010;71:2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- [58].Livingston JD, Milne T, Fang ML, Amari E. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction 2012;107:39–50. doi: 10.1111/j.1360-0443.2011.03601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Mayer DK, Travers D, Wyss A, Leak A, Waller A. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 2011;29:2683–2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Merrill JO, Rhodes LA, Deyo RA, Marlatt GA, Bradley KA. Mutual Mistrust in the Medical Care of Drug Users. The Keys to the “Narc” Cabinet. J Gen Intern Med 2002;17:327–333. doi: 10.1046/j.1525-1497.2002.10625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].National Academies of Sciences Engineering Medicine; Health and Medicine Division; Board on Health Sciences Policy; Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse. Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. Phillips JK, Ford MA, Bonnie RJ, editors Washington DC: National Academies Press (US), 2017. p. [PubMed] [Google Scholar]
- [62].National Cancer Institute. Cancer Statistics. 2020. Available: https://www.cancer.gov/about-cancer/understanding/statistics. Accessed 23 Nov 2020.
- [63].National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Adult Cancer Pain Version 2.2016. 2016. Available: https://oralcancerfoundation.org/wp-content/uploads/2016/09/pain.pdf. [DOI] [PubMed]
- [64].National Public Radio. White House Ad Campaign Aims To Prevent Youth Opioid Abuse. 2018. Available: https://www.npr.org/2018/06/07/617906373/with-real-life-stories-white-house-ad-campaign-aims-to-prevent-youth-opioid-abus. Accessed 29 Jan 2021.
- [65].O’Brien T, Kane CM. Pain services and palliative medicine – an integrated approach to pain management in the cancer patient. Br J Pain 2014;8:163–171. doi: 10.1177/2049463714548768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].O’Connor M, Weir J, Butcher I, Kleiboer A, Murray G, Sharma N, Thekkumpurath P, Walker J, Fallon M, Storey DJ, Sharpe M. Pain in Patients Attending a Specialist Cancer Service: Prevalence and Association With Emotional Distress. J Pain Symptom Manage 2012;43:29–38. doi: 10.1016/j.jpainsymman.2011.03.010. [DOI] [PubMed] [Google Scholar]
- [67].Page R, Blanchard E. Opioids and Cancer Pain: Patients’ Needs and Access Challenges. J Oncol Pract 2019;15:229–231. [DOI] [PubMed] [Google Scholar]
- [68].Paice JA. Cancer pain management and the opioid crisis in America: How to preserve hard-earned gains in improving the quality of cancer pain management. Cancer 2018;124:2491–2497. [DOI] [PubMed] [Google Scholar]
- [69].Paice JA, Portenoy R, Lacchetti C, Campbell T, Cheville A, Citron M, Constine LS, Cooper A, Glare P, Keefe F, Koyyalagunta L, Levy M, Miaskowski C, Otis-Green S, Sloan P, Bruera E. Management of Chronic Pain in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2016;34:3325–3345. doi: 10.1200/JCO.2016.68.5206. [DOI] [PubMed] [Google Scholar]
- [70].Paradies Y, Stevens M. Conceptual diagrams in public health research. J Epidemiol Community Health 2005;59:1012–1013. doi: 10.1136/jech.2005.036913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].PDQ Supportive and Palliative Care Editorial Board. Cancer Pain (PDQ(R)): Health Professional Version. PDQ Cancer Inf Summ; 2020. Available: https://www.ncbi.nlm.nih.gov/books/NBK65949/. [Google Scholar]
- [72].Penn TM, Overstreet DS, Aroke EN, Rumble DD, Sims AM, Kehrer C V, Michl AN, Hasan FN, Quinn TL, Long DL, Trost Z, Morris MC, Goodin BR. Perceived Injustice Helps Explain the Association Between Chronic Pain Stigma and Movement-Evoked Pain in Adults with Nonspecific Chronic Low Back Pain. Pain Med 2020;21:3161–3171. doi: 10.1093/pm/pnaa095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev 2015;16:319–326. doi: 10.1111/obr.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Quinlan J, Cox F. Acute pain management in patients with drug dependence syndrome. PAIN Reports 2017;2:e611. doi: 10.1097/PR9.0000000000000611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Rao D, Elshafei A, Nguyen M, Hatzenbuehler ML, Frey S, Go VF. A systematic review of multi-level stigma interventions: State of the science and future directions. BMC Med 2019;17:41. doi: 10.1186/s12916-018-1244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. Pain 2016;157:1607–1610. doi: 10.1097/j.pain.0000000000000512. [DOI] [PubMed] [Google Scholar]
- [77].Savage SR, Jamison RN. Assessment for addiction in pain-treatment settings. Clin J Pain 2002;18. doi: 10.1097/00002508-200207001-00004. [DOI] [PubMed] [Google Scholar]
- [78].Scarborough BM, Smith CB. Optimal pain management for patients with cancer in the modern era. CA Cancer J Clin 2018;68:182–196. doi: 10.3322/caac.21453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Schenker Y, Hamm M, Bulls H, Merlin J, Wasilko R, DAwdani A, Kenkre B, Belin S, Sabik L. ‘This is a different patient population’: oncologists’ views on challenges to safe and effective opioid prescribing for patients with cancer-related pain and recommendations for improvement. J Oncol Pr 2021;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Scott N, Crane M, Lafontaine M, Seale H, Currow D. Stigma as a barrier to diagnosis of lung cancer: patient and general practitioner perspectives. Prim Health Care Res Dev 2015;16:618–622. [DOI] [PubMed] [Google Scholar]
- [81].Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav 2011;15:1075–1087. doi: 10.1007/s10461-010-9847-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin 2021;71:7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- [83].Stangl AL, Earnshaw VA, Logie CH, Van Brakel W, Simbayi LC, Barré I, Dovidio JF. The Health Stigma and Discrimination Framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med 2019;17:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc 2013;16:18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Stephenson N, Dalton JA, Carlson J, Youngblood R, Bailey D. Racial and ethnic disparities in cancer pain management. J Natl Black Nurses Assoc 2009;20:11–18. Available: https://europepmc.org/article/med/19691179. Accessed 2 Mar 2021. [PubMed] [Google Scholar]
- [86].Tait RC, Chibnall JT, Kalauokalani D. Provider judgments of patients in pain: Seeking symptom certainty. Pain Med 2009;10:11–34. doi: 10.1111/j.1526-4637.2008.00527.x. [DOI] [PubMed] [Google Scholar]
- [87].The American Presidency Project. President Donald J. Trump’s Initiative to Stop Opioid Abuse and Reduce Drug Supply and Demand. 2018. Available: https://www.presidency.ucsb.edu/documents/president-donald-j-trumps-initiative-stop-opioid-abuse-and-reduce-drug-supply-and-demand. Accessed 29 Jan 2021.
- [88].Theobald DE. Cancer pain, fatigue, distress, and insomnia in cancer patients. Clin Cornerstone 2004;6 Suppl 1D:S15–21. [DOI] [PubMed] [Google Scholar]
- [89].Tsai AC, Kiang MV, Barnett ML, Beletsky L, Keyes KM, McGinty EE, Smith LR, Strathdee SA, Wakeman SE, Venkataramani AS. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PLoS Med 2019;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Tsang HWH, Ching SC, Tang KH, Lam HT, Law PYY, Wan CN. Therapeutic intervention for internalized stigma of severe mental illness: A systematic review and meta-analysis. Schizophr Res 2016;173:45–53. doi: 10.1016/j.schres.2016.02.013. [DOI] [PubMed] [Google Scholar]
- [91].Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing Mechanisms Linking HIV-Related Stigma, Adherence to Treatment, and Health Outcomes. Am J Public Heal 2017;107:863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Turan JM, Elafros MA, Logie CH, Banik S, Turan B, Crockett KB, Pescosolido B, Murray SM. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med 2019;17:7. doi: 10.1186/s12916-018-1246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].US Center for Disease Control and Prevention. CDC Advises Against Misapplication of the Guideline for Prescribing Opioids for Chronic Pain. n.d. Available: https://www.cdc.gov/media/releases/2019/s0424-advises-misapplication-guideline-prescribing-opioids.html. Accessed 20 Dec 2020.
- [94].US Centers for Medicare & Medicaid Services. Drug plan coverage rules. n.d. Available: https://www.medicare.gov/drug-coverage-part-d/what-medicare-part-d-drug-plans-cover/drug-plan-coverage-rules. Accessed 4 Feb 2021.
- [95].US Department of Health and Human Services. Draft Report on Pain Management Best Practices: Updates, Gaps, Inconsistencies, and Recommendations. 2018. Available: https://www.hhs.gov/ash/advisory-committees/pain/reports/2018-12-draft-report-on-updates-gaps-inconsistencies-recommendations/index.html#3.1-stigma.
- [96].Vadivelu N, Kai AM, Kodumudi V, Sramcik J, Kaye AD. The Opioid Crisis: a Comprehensive Overview. Curr Pain Headache Rep 2018;22:16. [DOI] [PubMed] [Google Scholar]
- [97].Varley AL, Lappan S, Jackson J, Goodin BR, Cherrington AL, Copes H, Hendricks PS. Understanding Barriers and Facilitators to the Uptake of Best Practices for the Treatment of Co-Occurring Chronic Pain and Opioid Use Disorder. J Dual Diagn 2020;16:239–249. doi: 10.1080/15504263.2019.1675920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Vayshenker BA, DeLuca J, Bustle T, Yanos P. “As soon as people hear that word…”: associative stigma among clinicians working with people with serious mental illness. J Public Ment Health 2018;17:20–28. [Google Scholar]
- [99].Verhaeghe M, Bracke P. Associative stigma among mental health professionals: Implications for professional and service user well-being. J Health Soc Behav 2012;53:17–32. doi: 10.1177/0022146512439453. [DOI] [PubMed] [Google Scholar]
- [100].Washington Medical Commission. WA Prescribing Rules Do Not Force Pain Patients Off Medication. 2019. Available: https://wmc.wa.gov/news/wa-prescribing-rules-do-not-force-pain-patients-medication. Accessed 4 Feb 2021.
- [101].Waugh OC, Byrne DG, Nicholas MK. Original Report Online Exclusive Internalized Stigma in People Living With Chronic Pain. 2014. doi: 10.1016/j.jpain.2014.02.001. [DOI] [PubMed] [Google Scholar]
- [102].Wiffen PJ, Wee B, Derry S, Bell RF, Moore RA. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev 2017;7:Cd012592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Williams ACDC. Defeating the stigma of chronic pain. Pain 2016;157:1581–1582. [DOI] [PubMed] [Google Scholar]
- [104].World Health Organization. Cancer Pain Management – Guiding Principles. 2018. Available: https://www.ncbi.nlm.nih.gov/books/NBK537483/. Accessed 3 Feb 2021.
- [105].Yanos PT, DeLuca JS, Salyers MP, Fischer MW, Song J, Caro J. Cross-sectional and prospective correlates of associative stigma among mental health service providers. Psychiatr Rehabil J 2020;43:85–90. doi: 10.1037/prj0000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Zallman L, Rubens SL, Saitz R, Samet JH, Lloyd-Travaglini C, Liebschutz J. Attitudinal barriers to analgesic use among patients with substance use disorders. Pain Res Treat 2012;2012. [DOI] [PMC free article] [PubMed] [Google Scholar]