INTRODUCTION
Physical inactivity is a leading cause of preventable morbidity and death in older adults. 27% of adults aged 65 to 74 years and 35% aged 75 years or older report no physical activity outside of work during the past month.1 Being physically active is a “gateway” for maintaining overall well-being, including preserving physical capability,2 prolonging independent living,3 enhancing social interaction,4 and contributing to a positive attitude and achievement.5 Visually impaired populations from several eye conditions demonstrate lower levels of total physical activity,6–8 and transitioning out of an active state to a sedentary state more quickly.9 These declines in physical activity are particularly substantial in people with visual field (VF) damage, i.e., glaucoma.9–11 which highlight the importance of identifying restrictions of physical activity and information to encourage safety behaviors in this high-risk population.
Physical activity occurs in a variety of locations and settings, and many interventions to improve physical activity focus on increasing activity in a specific location, such as at home or within an activity or fitness center.12 To optimize physical activity and safety, it is important to understand where persons with visual impairment perform their activities and also which activity locations are safest, guiding environmental modification of unsafe areas (especially when some activity is required in these locations), and maximization of activity in safe locations. Previous literature has assessed locations of physical activity using self-reported questionnaires,13,14 yet the rapid shift toward objective measures of physical activity and physical location allows researchers to examine location specific activity patterns using Global Positioning Systems (GPS).15 While the prior literature has reported associations between visual defects and overall physical activity levels, location-specific activity levels, such as at and away from home activity, remain less characterized.
Here, we studied participants from Falls in Glaucoma Study (FIGS), a well-established cohort of community-dwelling older people with glaucoma, to quantify and compare locations of physical activity across varying levels of VF damage, including: (1) away-from-home activity per day, (2) physical activity per out-of-home excursion, and (3) at home activity per day. We hypothesized that glaucoma patients with worse VF damage would demonstrate lower levels of away-from-home activity per day, physical activity per out-of-home excursion, and at home activity per day.
METHODS
Participants
Study participants were recruited into the FIGS study from the Johns Hopkins Wilmer Eye Institute between 2013 and 2015. FIGS study participants included individuals who met the following criteria: (1) 60 years or older by study completion, (2) living within 60 miles from the Wilmer Eye Institute, and (3) diagnosed with glaucoma or suspected glaucoma as judged by the treating glaucoma specialist.16 Participants were excluded if they had severe mobility restriction (i.e., wheelchair or bed-bound), had visual acuity worse than 20/40 because of illnesses other than glaucoma, or had undergone surgery (ocular or non-ocular) within the last two months or had been hospitalized in the last month.16 More detailed eligibility criteria are described elsewhere.9,16,17 The study was approved by the Johns Hopkins University Institutional Review Board (IRB number: CIR00041971), and informed consent was obtained from all participants. All research activities were conducted in adherence to the Declaration of Helsinki.
Vision Evaluation
Baseline visual acuity was assessed using a backlit ETDRS chart and transformed to log-MAR values. VF damage was examined using a Humphrey HFA-2 perimeter (Carl Zeiss Meditec, Carlsbad, California, USA). Pointwise sensitivities from left and right eye VF tests were combined to create a sensitivity at every spatial coordinate using the maximum sensitivity approach. Then, as previously described,16 each decibel sensitivity value was converted to a raw sensitivity and averaged across all points in whole VF, then converted back to decibel values to derive integrated VF (IVF) sensitivity. IVF sensitivity was further categorized into three groups: normal/mild (IVF >28 dB), moderate (IVF 23–28 dB), and severe (IVF <23 dB). People with normal VF had IVF in a range of 31 decibels or above, with lower IVF indicating worse VF damage.18
Location and physical activity assessment
Participants wore a waist-bound GPS tracker (QStarz, Inc, Taipei, Taiwan) for seven consecutive days after enrollment. The GPS tracker provided latitude and longitude on a minute-by-minute level. The home location was defined empirically by the overnight locates collected between 2 AM to 4 AM during the assessment. We used a distance of 50 meters to characterize an individual’s location as at home or away-from-home. The radius of 50 meters was used because: (i) it captured activity at home and surrounding the home (such as garden and garage), and (ii) 97% of 2–4 AM locations positioned the participant within this distance.19 Time spent at home or away from home per day was the sum of GPS minutes classified as at home or away from home. Away-from-home excursions were defined as the period spanning sequential space-time locations away from the home region.20
Physical activity was evaluated by waist-bound accelerometers (Actical, Respironics, Inc, Murrysville, PA) worn concurrently with the GPS device for seven days. Participants were instructed to wear the accelerometer and GPS tracker during all waking hours except swimming or bathing. To maximize compliance, participants also received two or more reminder calls during the week they wore their devices. Accelerometer data were used for participants who wore the device for at least eight hours/day and a minimum of four valid days.6,11 Steps occurring for each minute were categorized as home steps when an individual’s location for that minute was at home, away-from-home steps when the location was found away from home, or unknown when GPS data were missing or ambiguous (i.e. at the junction of home and away from home). Additionally, count data for each minute were utilized to classify activity level as sedentary, light, moderate or vigorous using the thresholds defined by Colley and Tremblay.21 Active minutes were calculated as the sum of light, moderate and vigorous minutes; Moderate and Vigorous Physical Activity (MVPA) minutes were identified as the sum of moderate and vigorous active minutes. Finally, physical activities per out-of-home excursion (including steps/excursion, active minutes/excursion and MVPA minutes/excursion) were derived for each participant.
Away-from-home MVPA was chosen as a primary outcome for this study because it was strongly associated with mobility measures based on preliminary findings in the same population. Other activity metrics, e.g., away-from-home active minutes and steps, and at home activities, were considered as secondary outcomes.
Covariate assessment
Demographic characteristics including age, sex, race, living arrangement, employment and education were assessed via questionnaires. Polypharmacy was defined as taking five or more prescription medications through a questionnaire or direct observation.22 Comorbid medical conditions were evaluated as the number of non-visual comorbidities from a list of 15 diseases described elsewhere.9 Cognitive function was assessed using Mini-Mental State Examination-Vision Impairment (maximum value of 22).23
Statistical analysis
Descriptive analyses were conducted using VF data obtained during the study. Pearson’s χ2 test and ANOVA test were used to assess the differences in demographic and health characteristics across the spectrum of VF damage. Away-from-home and home activity metrics were compared by VF damage using the ANOVA test for continuous variables.
Multivariable negative binomial regressions were used to examine Risk Ratios (RRs) for cross-sectional associations between IVF sensitivity and physical activity away from home, per away-from-home excursion and at home, adjusting for the following covariates: age, race, sex, living arrangement, employment, education, comorbidity, polypharmacy, and MMSE-VI. These covariates were considered based on their associations with physical activity shown in prior studies from the same clinical population.19 Locally weighted scatterplot smoothing (LOWESS) plots were fit to visualize physical activities per away-from-home excursion (MVPA minutes/excursion, active minutes/excursion and steps/excursion) across the severity of VF damage. Significance level was determined by two-tailed hypothesis testing with an alpha of 0.05. All analyses were performed using STATA 16.0 (StataCorp LP, College Station, Texas, USA).
RESULTS
Among the 229 study participants, mean age was 71 (Standard Deviation [SD]=8), 51% were men, 21% lived by themselves, 36% were employed, 71% had a bachelor’s degree or higher, 33% used at least five non-ocular prescription medications, 65% had more than one comorbidity condition, and the average Mini-Mental State Examination-Vision Impairment (maximum value: 22) was 20 (SD=2). Half of the participants had normal or mild VF damage (IVF >28 dB), while 40% and 10% were diagnosed with moderate (IVF: 23–28 dB) and severe VF damage (IVF <23 dB), respectively. People with severe VF damage were more likely to be African American and had higher (worse) logMAR visual acuity in the better seeing-eye than those with normal/mild and moderate VF damage (ANOVA p <0.01) (Table 1).
Table 1.
Participant demographics, health characteristics, and physical activity metrics by severity of visual field damage (N=229)
| Normal/Mild VF damage (IVF>28 dB) N = 115 | Moderate VF damage (IVF:23–28 dB) N = 91 | Severe VF damage (IVF<23 dB) N = 23 | P-value | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, mean (SD) | 69.10 (6.46) | 72.33 (8.88) | 70.17 (7.36) | 0.01 |
| Male, n (%) | 57 (50) | 49 (54) | 10 (44) | 0.64 |
| African American, n (%) | 27 (24) | 21 (23) | 15 (65) | <0.01 |
| Living alone, n (%) | 19 (17) | 20 (22) | 6 (26) | 0.44 |
| Employed, n (%) | 41 (36) | 36 (40) | 5 (22) | 0.28 |
| Education | 0.17 | |||
| ≤ High school, n (%) | 15 (13) | 15 (17) | 5 (22) | |
| Some college, n (%) | 14 (12) | 12 (13) | 5 (22) | |
| Bachelor, n(%) | 34 (30) | 18 (20) | 5 (22) | |
| ≥ Master, n (%) | 52 (45) | 46 (51) | 8 (35) | |
| Health characteristics | ||||
| Better-eye visual acuity-logMAR, mean(SD) | 0.04 (0.11) | 0.11 (0.12) | 0.31(0.38) | <0.01 |
| Polypharmacy, n (%) | 36 (31) | 30 (33) | 9 (39) | 0.76 |
| No. of comorbidities | 0.94 | |||
| ≤ 1, n (%) | 38 (33) | 34 (37) | 9 (39) | |
| 2–3, n (%) | 51 (44) | 40 (44) | 9 (39) | |
| 4–5, n (%) | 26 (23) | 17 (19) | 5 (22) | |
| MMSE-VI, mean (SD) | 20.32 (1.51) | 19.62 (2.21) | 19.83 (1.83) | 0.02 |
VF: vision field; SD: standard deviation; Polypharmacy: ≥ 5 systemic prescription medications without eye drops; MMSE-VI: Mini-Mental State Examination-Vision Impairment (maximum as 22); dB: decibels; IVF: integrated vision field. MVPA: moderate & vigorous physical activity.
Activity metrics by severity of VF damage
With regards to away-from-home activity measures, the number of MVPA minutes, active minutes and steps varied across persons with normal/mild, moderate and severe VF damage, with the lowest number of away-from-home MVPA minutes (ANOVA p=0.07) found in those with severe VF damage (Table 2). However, amount of time spent away from home per day, and excursions per week remained similar across the spectrum of VF damage (ANOVA p ≥0.19 for all). Over the observed range of glaucoma damage, fewer MVPA minutes per excursion (Figure 1A), fewer active minutes per excursion (Figure 1B), and fewer steps per excursion (Figure 1C) were observed with greater VF damage. In respect to at-home activity measures, active minutes and time spent at home per day varied across people with severe, moderate and normal/mild VF damage, with the lowest number of active minutes (ANOVA p=0.02) and highest number of time spent at home (ANOVA p=0.04) in people with severe VF damage; whereas the numbers of at-home MVPA minutes and steps per day were similar across three VF groups (ANOVA p ≥0.09 for all) (Table 2). Over the range of VF damage, participants had an average of four hours for missing GPS data mainly because of removing GPS devices during the overnight hours, and such missing pattern was not observed to vary by severity of VF damage (ANOVA p=0.11).
Table 2.
Participant activity metrics by severity of visual field damage (N=229)
| Normal/Mild VF damage (IVF>28 dB) N = 115 | Moderate VF damage (IVF:23–28 dB) N = 91 | Severe VF damage (IVF<23 dB) N = 23 | P-value | |
|---|---|---|---|---|
| Away home activity outcomes (per day) | ||||
| MVPA minutes, mean (SD) | 9.31 (12.76) | 6.77 (11.45) | 3.61 (6.08) | 0.07 |
| Active minutes, mean (SD) | 48.01 (32.43) | 39.53 (33.41) | 25.76 (23.42) | 0.01 |
| Time spent away-from-home (minutes), mean(SD) | 257.30 (158.22) | 252.52 (154.20) | 198.79 (178.64) | 0.27 |
| Steps, mean (SD) | 2196.44 (1228.01) | 1819.05 (1754.92) | 1077.44 (1004.18) | 0.01 |
| Excursions per week, mean (SD) | 7.15 (4.97) | 8.36 (7.17) | 6.25 (4.35) | 0.19 |
| At home activity outcomes (per day) | ||||
| MVPA minutes, mean (SD) | 1.96 (6.70) | 1 (3.45) | 0.77 (2.13) | 0.35 |
| Active minutes, mean (SD) | 67.45 (44.86) | 56.95 (40.61) | 43.60 (28.52) | 0.02 |
| Time spent at home (minutes), mean (SD) | 948.25 (310.43) | 896.28 (313.15) | 1082.77 (247.52) | 0.04 |
| Steps, mean (SD) | 1518.84 (1228.01) | 1295.73 (1102.14) | 985.46 (755.40) | 0.09 |
| Time period (minutes) for missing GPS data | 234.46 (299.95) | 291.21 (297.41) | 158.43 (147.76) | 0.11 |
VF: vision field; SD: standard deviation; MVPA: moderate & vigorous physical activity.
Note: the sum of time spent (minutes) at and away from home did not equal 1440 (24 hours) because we restricted each study minute to when both accelerometer and GPS data were available.
Figure 1A.
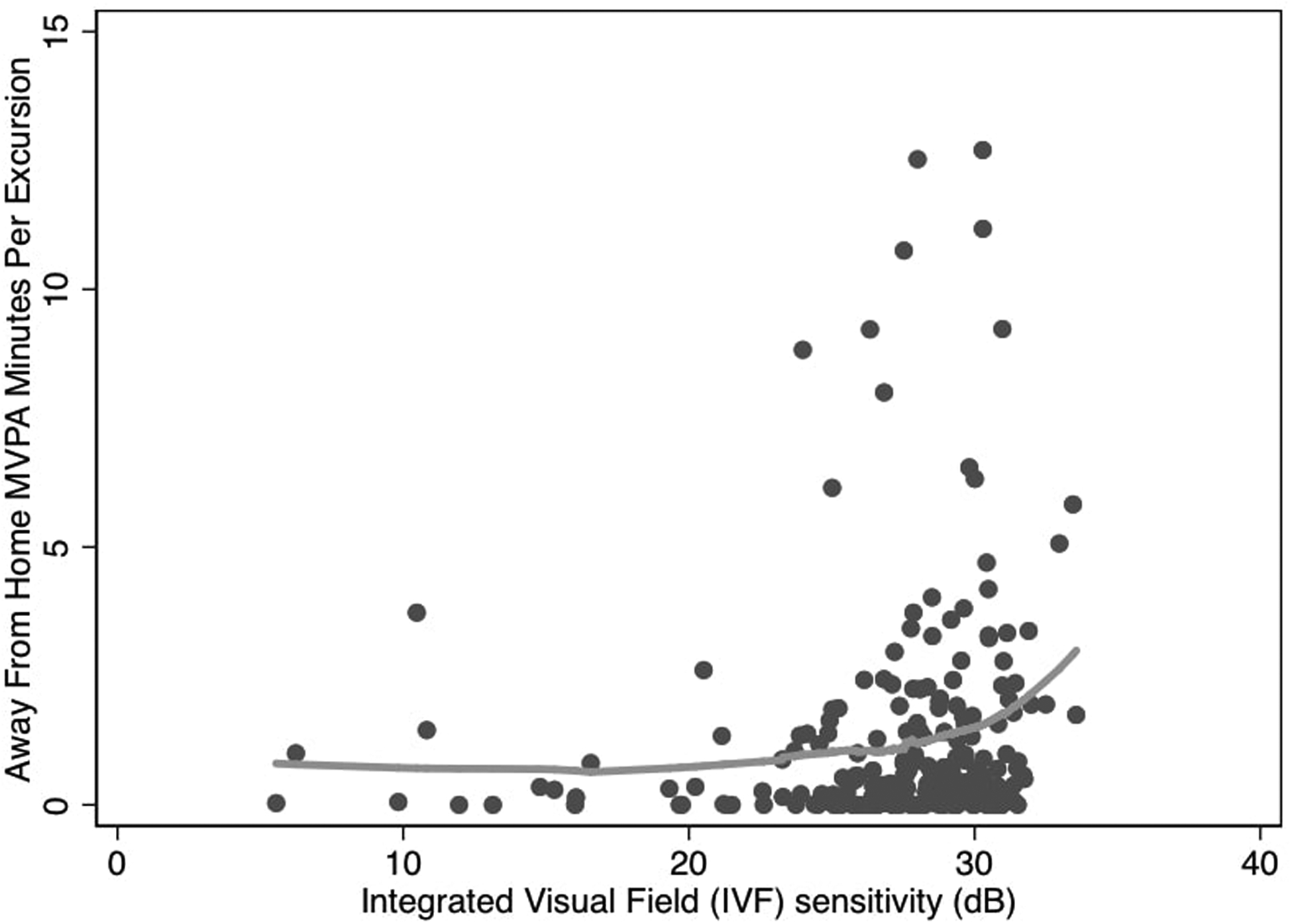
Away-from-home moderate & vigorous physical activity minutes per excursion and visual field damage
Figure 1B.
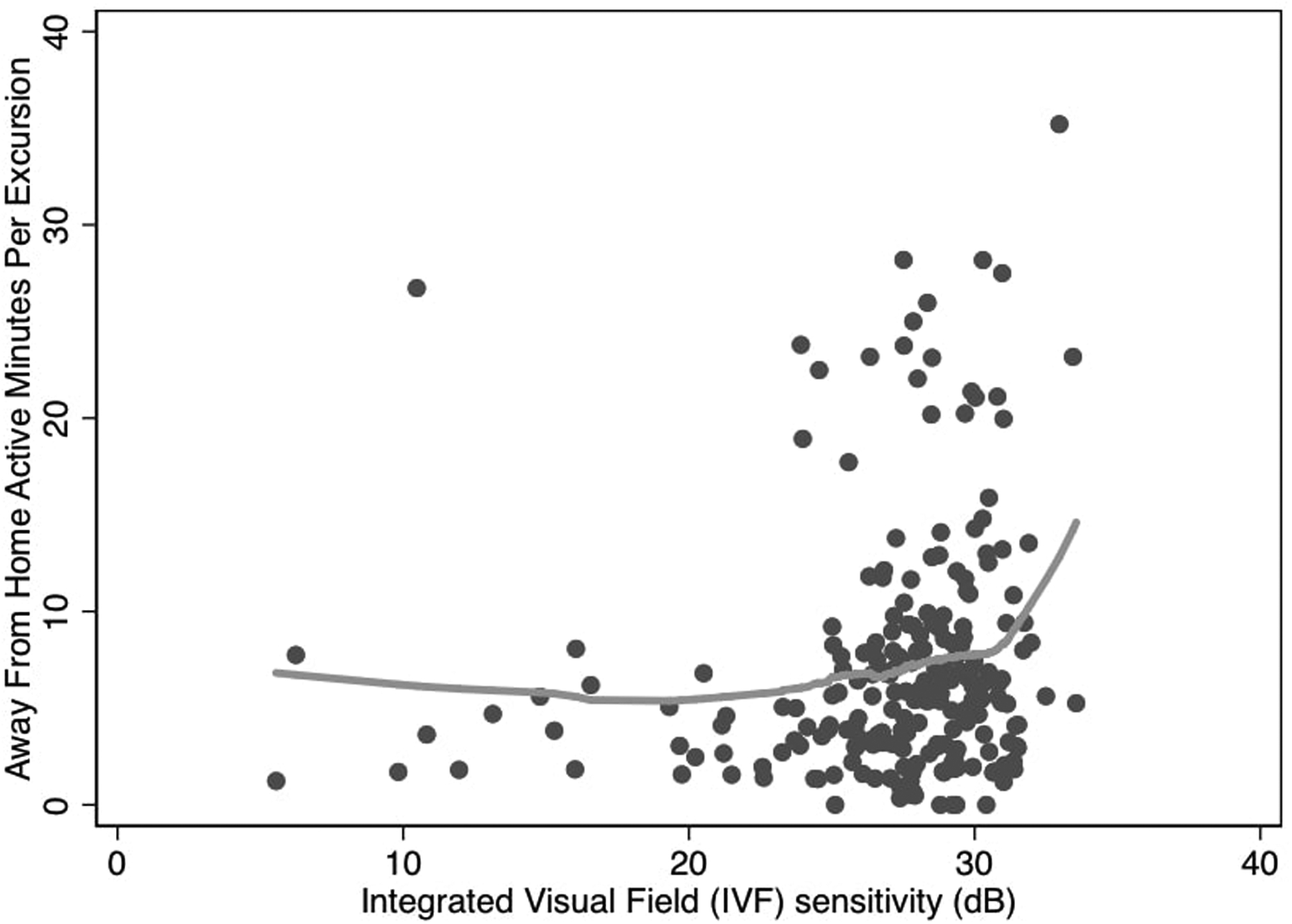
Away-from-home active minutes per excursion and visual field damage
Figure 1C.
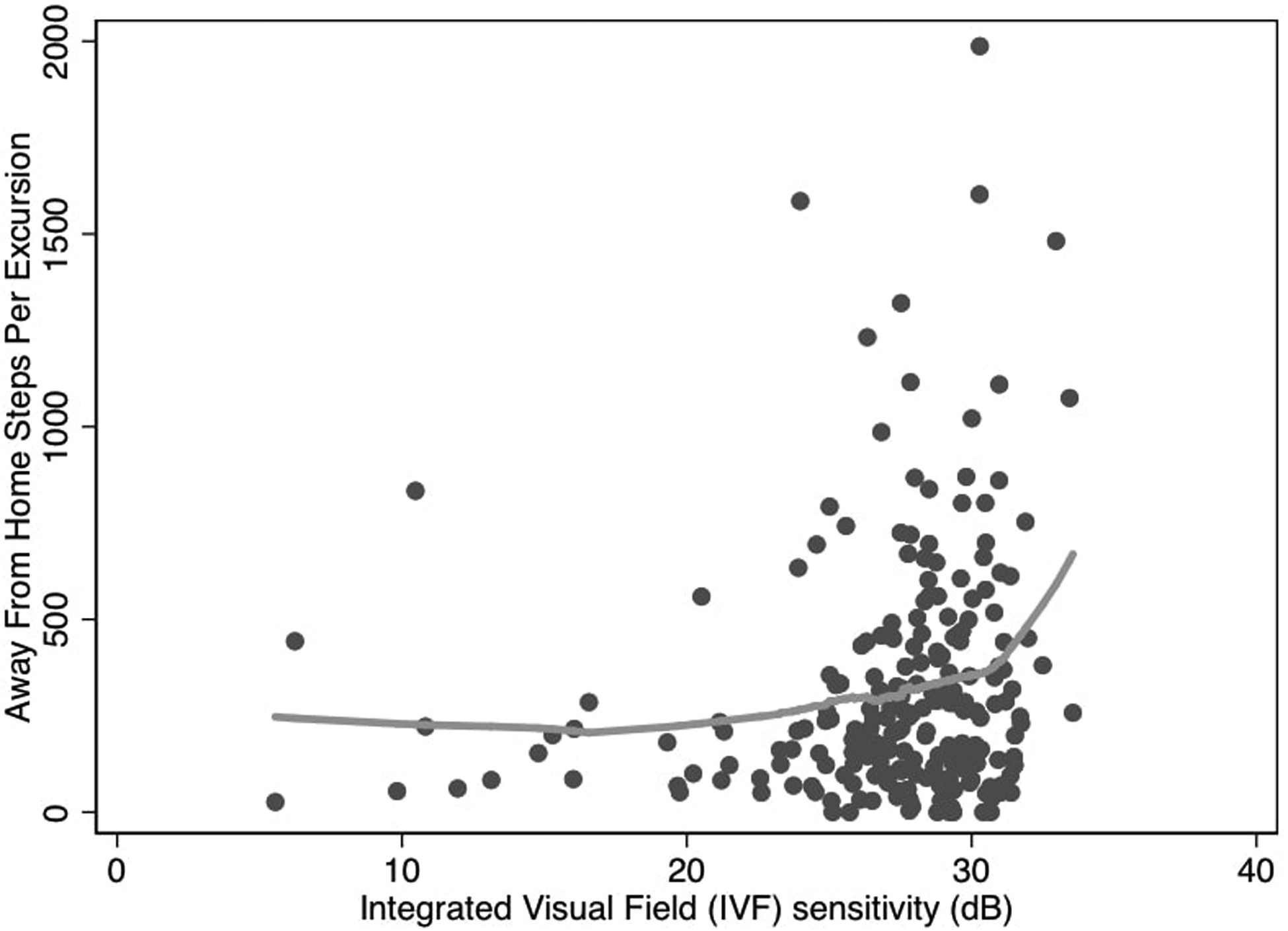
Away-from-home steps per excursion and visual field damage
Association of VF damage with away-from-home activity measures
In analyses considering VF damage as a continuous measure, after adjusting for age, race, sex, living arrangement, employment, education, comorbidity, polypharmacy, and MMSE-VI, each 5 dB decrement in IVF sensitivity was associated with less daily away-from-home activity [e.g.,18% less MVPA minutes/day (RR=0.82, 95% CI, 0.69 to 0.97)] (Table 3), and physical activities per away-from-home excursion [e.g., 20% less MVPA minutes/excursion (RR=0.80, 95 CI, 0.65 to 0.98)] (Table 4). Similar findings were noted for other away-from-home activity measures (including active minutes/steps per day, or active minutes/steps per excursion). No associations were noted between VF damage and time spent away-from-home per day (RR=0.91, 95% CI, 0.82 to 1.03), the number of excursions per week (RR=0.95, 95% CI, 0.86 to 1.05), and time spent away-from-home per excursion (RR=0.91, 95% CI, 0.80 to 1.04) (Table 3&4).
Table 3.
Associations between severity of glaucoma damage and away-from-home activity outcomes in multivariable models
| Variables | MVPA minutes per day, RR (95% CI) | Active minutes per day, RR (95% CI) | Time spent away-from-home (minutes) per day, RR (95% CI) | Steps per day, RR (95% CI) | Excursions per week, RR (95% CI) |
|---|---|---|---|---|---|
| 5-unit (dB) decrement in IVF sensitivitya | 0.82 (0.69, 0.97)* | 0.84 (0.75, 0.93)* | 0.91 (0.82, 1.03) | 0.83 (0.74, 0.93)* | 0.95 (0.86, 1.05) |
| VF damagea | |||||
| Normal/Mild | Reference | Reference | Reference | Reference | Reference |
| Moderate | 0.87 (0.61, 1.24) | 0.93 (0.78, 1.13) | 1.08 (0.90, 1.28) | 0.98 (0.77, 1.22) | 1.23 (0.99, 1.53) |
| Severe | 0.52 (0.27, 1.00)* | 0.54 (0.40, 0.72)* | 0.73 (0.51, 1.05) | 0.58 (0.41, 0.81)* | 0.95 (0.70, 1.29) |
Severity of VF damage on continuous and categorical scale were derived from different models, each containing the same covariates: age, race, sex, living arrangement, employment, education, comorbidity, polypharmacy, and cognitive function.
RR: Risk Ratio; MVPA: moderate & vigorous physical activity; VF: vision field; IVF: integrated vision field; dB: decibels; CI: confidence interval; Polypharmacy: ≥ 5 systemic prescription medications; Mini-Mental State Examination-Vision Impairment (maximum as 22).
p <0.05.
Table 4.
Associations between severity of glaucoma damage and away-from-home activity per excursion in multivariable models
| Variables | MVPA minutes per excursion, RR (95% CI) | Active minutes per excursion, RR (95% CI) | Time spent away home (minutes) per excursion, RR (95% CI) | Steps per excursion, RR (95% CI) |
|---|---|---|---|---|
| 5-unit (dB) decrement in IVF sensitivitya | 0.80 (0.65, 0.98)* | 0.81 (0.71, 0.92)* | 0.91 (0.80, 1.04) | 0.80 (0.72, 0.90)* |
| VF damagea | ||||
| Normal/Mild | Reference | Reference | Reference | Reference |
| Moderate | 0.71 (0.50, 1.09) | 0.77 (0.60, 1.00)* | 0.99 (0.78, 1.25) | 0.81 (0.62, 1.05) |
| Severe | 0.47 (0.23, 0.96)* | 0.48 (0.34, 0.67)* | 0.68 (0.48, 1.00) | 0.51 (0.35, 0.74)* |
Severity of VF damage on continuous and categorical scale were derived from different models, each containing the same covariates: age, race, sex, living arrangement, employment, education, comorbidity, polypharmacy, and cognitive function.
RR: Risk Ratio; MVPA: moderate & vigorous physical activity; VF: vision field; IVF: integrated vision field; dB: decibels; CI: confidence interval; Polypharmacy: ≥ 5 systemic prescription medications; Mini-Mental State Examination-Vision Impairment (maximum as 22).
p <0.05.
In comparisons across the levels of VF damage, participants with severe VF damage engaged in 48% fewer minutes of MVPA per day (RR=0.52, 95% CI, 0.27 to 1.00) and 53% fewer minutes of MVPA per excursion (RR=0.47, 95% CI, 0.23 to 0.96) compared to those with normal/mild VF damage, and similar findings were found for other away-from-home activity measures (including active minutes/steps per day, or active minutes/steps per excursion). However, those with severe VF damage had a similar amount of time spent away-from-home per day (RR=0.73, 95% CI, 0.51 to 1.05), excursion duration (RR=0.68, 95% CI, 0.48 to 1.00), and excursions per week (RR=0.95, 95% CI, 0.70 to 1.29) (Table 3&4). In comparison to people with normal/mild VF damage, those with moderate VF group did not show significant differences in any of away-from-home activity outcomes per day or per excursion (p>0.05 for all) (Table 3&4).
Associations of VF damage with at-home activity outcomes
After adjusting for age, race, sex, living arrangement, employment, education, comorbidity, polypharmacy, and MMSE-VI, each 5 dB decrement in IVF sensitivity was not associated with any measure of at-home activity, including MVPA minutes/day, active minutes/day, time spent at home, and steps/day (p>0.05 for all) (Table 5). When categorizing VF damage by severity, people with severe VF damage had significantly spent fewer at-home active minutes (RR=0.74, 95% CI, 0.57 to 0.97) and more time spent at home (RR=1.14, 95% CI, 1.03, 1.27) compared to those with normal/mild VF damage, but had similar number of MVPA minutes (RR=1.01, 95% CI, 0.28 to 3.66) and steps at home (RR=0.83, 95% CI, 0.59 to 1.16). Additionally, participants with moderate VF damage group had similar amounts of at-home activity outcomes compared to those with normal/mild VF damage (p>0.05 for all).
Table 5.
Associations between severity of glaucoma damage and at home activity outcomes in multivariable models
| Variables | MVPA minutes per day, RR (95% CI) | Active minutes per day, RR (95% CI) | Time spent at home (minutes) per day, RR (95% CI) | Steps per day, RR (95% CI) |
|---|---|---|---|---|
| 5-unit (dB) decrement in IVF sensitivitya | 0.83 (0.59, 1.17) | 0.92 (0.84, 1.01) | 1.03 (1.00, 1.07) | 0.92 (0.83, 1.02) |
| VF damagea | ||||
| Normal/Mild | Reference | Reference | Reference | Reference |
| Moderate | 0.63 (0.33, 1.20) | 0.90 (0.75, 1.08) | 0.95 (0.87, 1.04) | 0.90 (0.73, 1.10) |
| Severe | 1.01 (0.28, 3.66) | 0.74 (0.57, 0.97)* | 1.14 (1.03, 1.27)* | 0.83 (0.59, 1.16) |
Severity of VF damage on continuous and categorical scale were derived from different models, each containing the same covariates: age, race, sex, living arrangement, employment, education, comorbidity, polypharmacy, and cognitive function.
RR: Risk Ratio; MVPA: moderate & vigorous physical activity; VF: vision field; IVF: integrated vision field; dB: decibels; CI: confidence interval; Polypharmacy: ≥5 systemic prescription medications; Mini-Mental State Examination-Vision Impairment (maximum as 22).
p <0.05.
DISCUSSION
In this study, we examined the dependence of physical activity in different locations on visual ability in a group of glaucoma patients with a wide range of VF damage. Location was defined by GPS-tracking as either at-home or away-from-home. At more severe levels of VF damage, physical activity was lower outside the home, though at-home activity did not vary by levels of VF damage, indicating a specific lack of confidence for performing activity outside the home in more severe glaucoma patients. Our findings suggest that glaucoma patients with severe VF damage, especially those who report impaired mobility, may benefit from targeted strategies aimed at increasing the availability of activity-friendly environments outside the home, and encouraging the importance of activity, particulary higher intensity activity, outside the home. Our findings also highlight the importance of maintaining a safe home environment, where activity is not restricted with worse VF damage, which may subject the individuals to more frequent injury even when activity becomes restricted.
Previous research has investigated several aspects of mobility in visually impaired populations, i.e., the total amount of activity (steps or counts), intensity of activity,8,24,25 and activity fragmentation.9 Our study extends these findings by demonstrating how vision affects physical activity performed in various locations. Importantly, we found that people with worse VF damage conducted less activity away from home, mainly because they were less active each time they left home, and not because they left home less frequently. In addition, our results suggest that among the various measures of physical activity by GPS-tracked location (including MVPA, active minutes, and steps), only away-from-home MVPA was an independent factor of mobility measures. These findings indicate that some glaucoma people, i.e., those with less away-from-home MVPA due to worse VF damage, maybe a higher risk of worse mobility, possibly as a result of social isolation, depression, and difficulties of accessing health services outside the home.26
Activity outside the home has the potential to offer benefits not accrued by activity within the home. Although we do not know exactly where away-from-home activity occurred in the present study, activity in this region may have secondary benefits: for example, shopping could help older adults maintain independence, whereas visiting friends and attending social events are beneficial for mental and emotional wellness.27,28 Hence, expanding the activity conducted outside the home may indirectly enhance physical function and restore overall health. A growing body of literature suggests that exposure to nature and external home-environment has restorative health benefits, including recovery from surgery,29,30 maintaining mental health and improving the sense of well-being.26 Moreover, previous research also has found that participation in outdoor physical activity was associated with frequent interactions with others, lower levels of anger, confusion, and depression, and better ability to complete instrumental activities of daily living (such as transportation and shopping).26,31 Thus, there may be additional beneficial effects from performing MVPA in environments outside the home, and targeted strategies to improve MVPA outside the home in visually impared older adults may be warrented.
Previous studies have shown that visual impairment from irreversible ocular diseases such as glaucoma threatens their ability to live independently at home as a result of injuries (falls often occurring at home) and difficulties with tasks of daily living.11,32,33 The present study reported that people with greater VF damage were not observed to restrict their activity at home. In other words, a similar amount of at-home tasks related to daily living are conducted regardless of VF damage. Hence, it is important to maintain a safe home environment, such that this activity does not result in falls but enables people to adequately perform at-home functional tasks.34 Despite the fact that home modification led by occupational therapists is a Medicare-reimbursement service and part of vision care in some practices,34,35 most persons with low vision do not have access to these services or avail themselves of these services even when available, and physicians or eye care specialists may not be actively aware when to refer patients.36 Further research is warranted to study to what extent home hazard modification ensures safety activity in the visually impaired, and to what extent it helps preserve functionality and independence. Further research is needed to define specific environmental features which may improve safety and functionality in this population.37
Limitations of this study included a lack of generalizability as the study participants were recruited from a single center with one ocular disease, i.e., glaucoma. Moreover, there were a high proportion of highly educated and cognitively intact people in our study due to the demographics of the study population and willingness to participate in research, which may limit the ability to generalize the observed associations to other populations, particularly those of lower socioeconomic status and impaired cognition. Further, 65% of the severe VF damage group was African American as compared to that in moderate (23%) and normal/mild (24%) VF group, though no interaction was found between VF damage and race. Second, the cross-sectional study design limits the ability to examine the temporal relationship between severe VF damage and less away-from-home activity, which requires future studies with longitudinal analyses. Third, although the accelerometer and GPS device captures objective measures of physical activity at or away from home, GPS could not tell in what type of environment that activity takes place.38 Fourth, the accelerometer does not monitor upper body moments or some types of physical activity, such as bicycling and swimming. Fifth, we found an association between a 5 dB decrement on VF and away-from-home activity, but no difference was found when looking at the different stages except for advanced VF damage. It is likely that continuous measures typically have more power to detect differences across a range of values than categories, as some individuals with normal/mild vs. moderate glaucoma will not differ that much in their visual ability.
In conclusion, our study found that glaucoma patients with severe VF damage engage in a lower amount of away-from-home activity per day, or per away-from-home excursion. However, worse VF damage was not associated with measures of at-home activity, time spent at- or away-from-home, or out-of-home excursions per week. Our results suggest the restriction of physical activity in more severe glaucoma patients results mostly from activity restriction outside the home environment. These findings highlight the importance of maintaining a safe home environment (where activity is less restricted) and increasing confidence in performing activity when leaving the home.
Table of Contents Statement:
Severe glaucoma patients restrict their physical activity, particularly activity conducted outside the home environment.
Worse visual field damage is not associated with at-home activity or out-of-home excursions.
It is important to maintain a safe home environment and increase confidence in performing activity when leaving the home for visually impaired older people.
Funding/Support
The research was supported in part by National Institutes of Health Grant EY022976.
Biography

Jian-Yu E obtained his ScD from Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health. He was the recipient of the Gerontological Society of America (GSA) Research Award. He is currently a Postdoc Fellow at Wilmer Eye Institute, Johns Hopkins School of Medicine. His research interests include applying novel epidemiological methods in vision research, assessing physiological declines and improving overall well-being of visually impaired population.
Footnotes
Financial Disclosures
The following authors report no financial disclosures: Jian-Yu E, Aleksandra Mihailovic, MS, Catalina Garzon, Jennifer A. Schrack, Tianjing Li, Sheila K. West, David S. Friedman, Laura N. Gitlin, Pradeep Y. Ramulu.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
REFERENCE
- 1.Watson KB, Carlson SA, Gunn JP, et al. Physical inactivity among adults aged 50 years and older - United States, 2014. Morb. Mortal. Wkly. Rep 2016;65(36):954–958. [DOI] [PubMed] [Google Scholar]
- 2.West CG, Gildengorin G, Haegerstrom-Portnoy G, Schneck ME, Lott L, Brabyn JA. Is vision function related to physical functional ability in older adults? J Am Geriatr Soc. 2002;50(1):136–145. [DOI] [PubMed] [Google Scholar]
- 3.Sengupta S, van Landingham SW, Solomon SD, Do DV, Friedman DS, Ramulu PY. Driving habits in older patients with central vision loss. Ophthalmology. 2014;121(3):727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lindsay Smith G, Banting L, Eime R, O’Sullivan G, van Uffelen JGZ. The association between social support and physical activity in older adults: a systematic review. Int J Behav Nutr Phys Act. 2017;14(1):56–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Condello G, Capranica L, Stager J, et al. Physical activity and health perception in aging: do body mass and satisfaction matter? a three-path mediated link. PloS One. 2016;11(9):e0160805–e0160805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee MJ, Wang J, Friedman DS, Boland MV, De Moraes CG, Ramulu PY. Greater physical activity is associated with slower visual field loss in glaucoma. Ophthalmology. 2019;126(7):958–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ong SR, Crowston JG, Loprinzi PD, Ramulu PY. Physical activity, visual impairment, and eye disease. Eye (Lond). 2018;32(8):1296–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Landingham SW, Willis JR, Vitale S, Ramulu PY. Visual field loss and accelerometer-measured physical activity in the United States. Ophthalmology. 2012;119(12):2486–2492. [DOI] [PubMed] [Google Scholar]
- 9.E JY, Schrack JA, Mihailovic A, et al. Patterns of daily physical activity across the spectrum of visual field damage in glaucoma patients. Ophthalmology. 2021;128(1):70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.E JY, Mihailovic A, Kuo PL, et al. Characterizing the impact of fear of falling on activity and falls in older adults with glaucoma. J Am Geriatr Soc. 2020;68(8):1847–1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramulu PY, Maul E, Hochberg C, Chan ES, Ferrucci L, Friedman DS. Real-world assessment of physical activity in glaucoma using an accelerometer. Ophthalmology. 2012;119(6):1159–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ashworth NL, Chad KE, Harrison EL, Reeder BA, Marshall SC. Home versus center based physical activity programs in older adults. Cochrane Database Syst Rev. 2005;2005(1):CD004017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grow HM, Saelens BE, Kerr J, Durant NH, Norman GJ, Sallis JF. Where are youth active? Roles of proximity, active transport, and built environment. Med Sci Sports Exerc. 2008;40(12):2071–2079. [DOI] [PubMed] [Google Scholar]
- 14.Fan Y The built environment, activity space, and time allocation, University of North Carolina; at Chapel Hill; 2007. [Google Scholar]
- 15.Smith L, Foley L, Panter J. Activity spaces in studies of the environment and physical activity: A review and synthesis of implications for causality. Health & Place. 2019;58(7):102113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mihailovic A, Swenor BK, Friedman DS, West SK, Gitlin LN, Ramulu PY. Gait implications of visual field damage from glaucoma. Transl Vis Sci Technol. 2017;6(3):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sotimehin AE, Yonge AV, Mihailovic A, et al. Locations, circumstances, and outcomes of falls in patients with glaucoma. Am J Ophthalmol. 2018;192(8):131–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yonge AV, Swenor BK, Miller R, et al. Quantifying fall-related hazards in the homes of persons with glaucoma. Ophthalmology. 2017;124(4):562–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramulu PY, Mihailovic A, West SK, Gitlin LN, Friedman DS. Predictors of falls per step and falls per year at and away from home in glaucoma. Am J Ophthalmol. 2019;200(4):169–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Curriero FC, Pinchoff J, van Landingham SW, Ferrucci L, Friedman DS, Ramulu PY. Alteration of travel patterns with vision loss from glaucoma and macular degeneration. JAMA Ophthalmol. 2013;131(11):1420–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colley RC, Tremblay MS. Moderate and vigorous physical activity intensity cut-points for the Actical accelerometer. J Sports Sci. 2011;29(8):783–789. [DOI] [PubMed] [Google Scholar]
- 22.Gnjidic D, Hilmer SN, Blyth FM, et al. Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol. 2012;65(9):989–995. [DOI] [PubMed] [Google Scholar]
- 23.Busse A, Sonntag A, Bischkopf J, Matschinger H, Angermeyer MC. Adaptation of dementia screening for vision-impaired older persons: administration of the Mini-Mental State Examination (MMSE). J Clin Epidemiol. 2002;55(9):909–915. [DOI] [PubMed] [Google Scholar]
- 24.Ferguson T, Rowlands AV, Olds T, Maher C. The validity of consumer-level, activity monitors in healthy adults worn in free-living conditions: a cross-sectional study. Int J Behav Nutr Phys Act. 2015;12(3):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Willis JR, Vitale SE, Agrawal Y, Ramulu PY. Visual impairment, uncorrected refractive error, and objectively measured balance in the United States. JAMA Ophthalmol. 2013;131(8):1049–1056. [DOI] [PubMed] [Google Scholar]
- 26.Thompson Coon J, Boddy K, Stein K, Whear R, Barton J, Depledge MH. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ Sci Technol. 2011;45(5):1761–1772. [DOI] [PubMed] [Google Scholar]
- 27.Brenner AB, Clarke PJ. Difficulty and independence in shopping among older Americans: more than just leaving the house. Disabil Rehabil. 2019;41(2):191–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santini ZI, Jose PE, York Cornwell E, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5(1):e62–e70. [DOI] [PubMed] [Google Scholar]
- 29.Frumkin H Beyond toxicity: human health and the natural environment. Am J Prev Med. 2001;20(3):234–240. [DOI] [PubMed] [Google Scholar]
- 30.St Leger L Health and nature—new challenges for health promotion. Health Promot Int. 2003;18(3):173–175. [DOI] [PubMed] [Google Scholar]
- 31.Ćwirlej-Sozańska A, Wiśniowska-Szurlej A, Wilmowska-Pietruszyńska A, Sozański B. Determinants of ADL and IADL disability in older adults in southeastern Poland. BMC Geriatr. 2019;19(1):297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freeman EE, Muñoz B, Rubin G, West SK. Visual field loss increases the risk of falls in older adults: the Salisbury eye evaluation. Invest Ophthalmol Vis Sci. 2007;48(10):4445–4450. [DOI] [PubMed] [Google Scholar]
- 33.Lamoureux EL, Chong E, Wang JJ, et al. Visual impairment, causes of vision loss, and falls: the singapore malay eye study. Invest Ophthalmol Vis Sci. 2008;49(2):528–533. [DOI] [PubMed] [Google Scholar]
- 34.E JY, Li T, McInally L, et al. Environmental and behavioural interventions for reducing physical activity limitation and preventing falls in older people with visual impairment. Cochrane Database Syst Rev. 2020;9:Cd009233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Warren M Providing low vision rehabilitation services with occupational therapy and ophthalmology: a program description. Am J Occup Ther. 1995;49(9):877–883. [DOI] [PubMed] [Google Scholar]
- 36.National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Public Health Approaches to Reduce Vision Impairment and Promote Eye Health. Making eye health a population health imperative: vision for tomorrow. National Academies Press; (US: ); 2016. [Google Scholar]
- 37.Arbesman M, Lieberman D, Berlanstein DR. Methodology for the systematic reviews on occupational therapy interventions for older adults with low vision. Am J Occup Ther. 2013;67(3):272–278. [DOI] [PubMed] [Google Scholar]
- 38.Bowler DE, Buyung-Ali LM, Knight TM, Pullin AS. A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health. 2010;10(1):456. [DOI] [PMC free article] [PubMed] [Google Scholar]


