Abstract
Introduction
To describe a “triple” surgical procedure, which combined traumatic cataract extraction by phacoemulsification with gas endotamponade and cyclocryotherapy in the successful treatment of a traumatic cyclodialysis cleft.
Methods
A 44-year-old man who suffered severe left eye blunt trauma with an elastic band developed a 4-hour extent cyclodialysis cleft with consequent hypotony. After 7 weeks of persistent hypotonic maculopathy unresponsive to medical treatment, and with an evolving traumatic cataract, the patient underwent cataract surgery combined with intravitreal gas endotamponade (20% SF6) and cyclocryotherapy.
Results
Two weeks after the procedure the intraocular pressure increased to 12 mmHg and remained steady during the next 14 months of follow-up. Hypotonic maculopathy resolved and successful closure of the cyclodialysis cleft was confirmed by gonioscopy and ultrasound biomicroscopy.
Conclusion
Gas endotamponade and cyclocryotherapy constitute a promising option in the treatment of cyclodialysis clefts unresponsive to medical therapy. In our case, this minimally invasive technique was innovatively combined with cataract surgery. Despite early postoperative intraocular inflammation, a successful outcome was achieved.
Keywords: Cyclocryotherapy, Cyclodialysis Cleft, Gas Endotamponade, Hypotonic Maculopathy, Traumatic Cataract Surgery
Key Summary Points
| Cyclodialysis is a rare disorder that results from disinsertion of the longitudinal ciliary muscle fibers from the scleral spur, creating an alternative route for aqueous humor outflow, which may lead to severe hypotony. |
| Blunt ocular trauma is the most frequent cause of cyclodialysis cleft formation. |
| Closing a cyclodialysis cleft is a true therapeutic challenge. There are many treatment modalities (ranging from laser therapy to surgical interventions), but there is no obvious gold-standard technique. |
| We report a case of traumatic cyclodialysis cleft and cataract, successfully treated with gas endotamponade and cyclocryotherapy combined with phacoemulsification and intraocular lens (IOL) implantation. |
| To the best of our knowledge, this “triple” procedure is the first of its kind reported in the literature, with promising outcomes. |
Introduction
A cyclodialysis cleft formation is a rare clinical event that results from disinsertion of the longitudinal ciliary muscle fibers from the scleral spur, thus creating a direct communication between the anterior chamber and the suprachoroidal space [1]. The free outflow of aqueous humor through this alternative route may lead to chronic hypotony and secondary associated complications, such as refractive changes, cataract formation, flat anterior chamber, choroidal detachment, hypotonic maculopathy, and optic disc swelling [1, 2].
Before the advent of trabeculectomy, cyclodialysis was an accepted treatment strategy for glaucoma [3]. Nowadays, the deliberate creation of a cyclodialysis cleft is no longer performed, and the majority of cases occur inadvertently as a surgical complication or, more frequently, after blunt ocular trauma [1, 4]. Men are more frequently affected than women [1].
The presence of a cyclodialysis cleft should always be suspected in the setting of persistent hypotony after surgery or severe ocular contusion, especially when accompanied by other signs of anterior segment damage, such as hyphema and iris injuries, in the absence of an open globe injury [4].
Gonioscopy has traditionally been regarded as the gold-standard method for the diagnosis of cyclodialysis. Intracameral injection of a viscoelastic agent may be necessary to increase its effectiveness, since media opacity and globe hypotony can hamper the accurate identification of a cleft. Other noninvasive diagnostic techniques such as ultrasound biomicroscopy (UBM) are now an extremely valuable tool, as they not only increase the odds of cleft identification but also localize and measure the extent of the lesion, thus helping to delineate the best management plan [5].
Sealing a cyclodialysis cleft can be truly challenging. More than 20 different methods have been described in the literature, but no consensual standardized approach has been established [1, 2, 6]. Conservative medical treatment is usually used as a first-line option, but its success is limited to cases with small clefts. Therefore, more invasive techniques (ranging from laser-based to surgical interventions) are almost always necessary to restore normal ocular tonus [1, 2, 4, 5].
Here, we describe the case of a traumatic cataract and cyclodialysis cleft that were successfully treated with gas endotamponade, cyclocryotherapy, and phacoemulsification with intraocular lens (IOL) implantation. To the best of our knowledge, this “triple” procedure is the first of its kind reported in the literature.
Case Report
A 44-year-old Caucasian man presented to our emergency department with painful vision loss after blunt left eye trauma with an elastic band. On ophthalmic examination, the best-corrected visual acuity (BCVA) was 20/20 in his right eye (OD) and counting fingers at 30 cm in his left eye (OS). Left eye slit-lamp exam revealed exuberant eyelid ecchymosis, multiple conjunctival and corneal erosions, and significant corneal edema. A shallow anterior chamber, with a half-chamber hyphema and severe cellular and fibrinous reaction, was present. Fundoscopy was hampered by media opacity. Right eye biomicroscopy and fundoscopy were unremarkable. Intraocular pressure (IOP) was 12 mmHg OD and 5 mmHg OS. Pupillary evaluation and eye movements were normal. B-scan ultrasonography disclosed a small, flat peripheral choroidal detachment (Fig. 1). Orbital computed tomography (CT) was irrelevant.
Fig. 1.

B-scan ultrasonography of the patient’s left eye at presentation, revealing a small, flat, peripherical choroidal detachment (arrow)
The patient was prescribed cycloplegic drops, prednisolone/chloramphenicol ointment, topical hypotensive medication, and oral aminocaproic acid.
During subsequent follow-up visits, the hyphema and anterior chamber inflammatory reaction gradually resolved. Visual acuity improved to 20/50 and IOP remained consistently at 5 mmHg, even after discontinuation of hypotensive drops. Fundoscopy revealed radial star-shaped chorioretinal folds around the macula (Fig. 2a), as well as optic disc swelling (Fig. 2b). The choroidal detachment maintained its original extent and localization. Anterior displacement of the iris–lens diaphragm, with consequent shallowing of the anterior chamber, precluded accurate gonioscopy, but UBM showed a temporal cyclodialysis cleft and fluid in the suprachoroidal space (Fig. 3a–c). Topical steroids were tapered and the patient was maintained under conservative treatment with topical atropine 1% twice daily. However, after 7 weeks under cycloplegia, there was no improvement in IOP or fundoscopic findings. Also, the patient developed a subcapsular lens opacification, further reducing his visual acuity. At this stage, a triple surgical procedure, combining phacoemulsification and IOL implantation with gas endotamponade and subsequent cyclocryotherapy, was attempted under general anesthesia. Phacoemulsification was performed using a standard phaco-chop technique. Inferior-temporal zonular dehiscence was noted during cortical aspiration, which required a 13 mm capsular tension ring (CTR) implantation. In-the-bag IOL implantation was then successfully achieved. Afterward, the anterior chamber was filled with a viscoelastic agent, and direct gonioscopy revealed a cyclodialysis cleft, extending from the 12 to 4 o’clock positions. A single bubble (0.5 ml) of 20% sulfur hexafluoride–air mixture (SF6) was injected via pars plana, in the inferonasal quadrant, 3.5 mm behind the limbus. At this point of the surgery, the patient reacted to eye stimulation, and an unquantifiable part of the introduced gas was expelled. Transconjunctival cryotherapy was then performed using a 3 mm metal tip glaucoma probe (Fig. 4a), placed 1.5 mm behind the limbus. The cryoprobe was connected to a freezing console using nitrous oxide as a cryogen. Six contiguous applications, at a temperature of −80 ºC, with a duration of 20 s each, were applied to the sclera, covering the entire extension of the cleft (Fig. 4b).
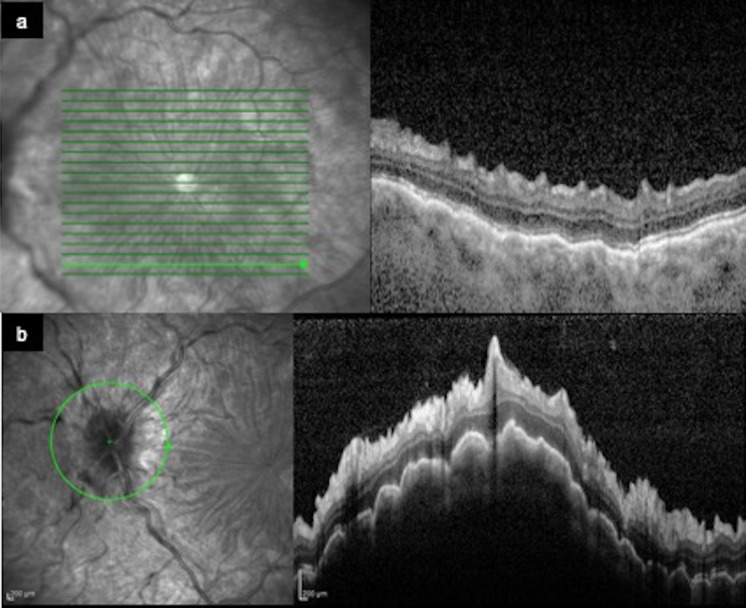
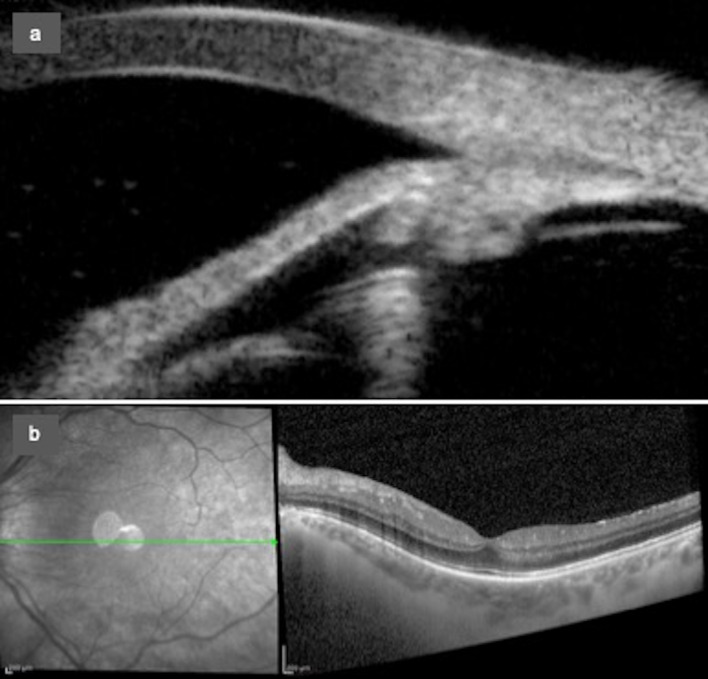
Fig. 2.
a, b Infrared images (left panel) and spectral-domain optical coherence tomography (OCT) scans (right panel) showing evident hypotonic maculopathy and optic disc swelling
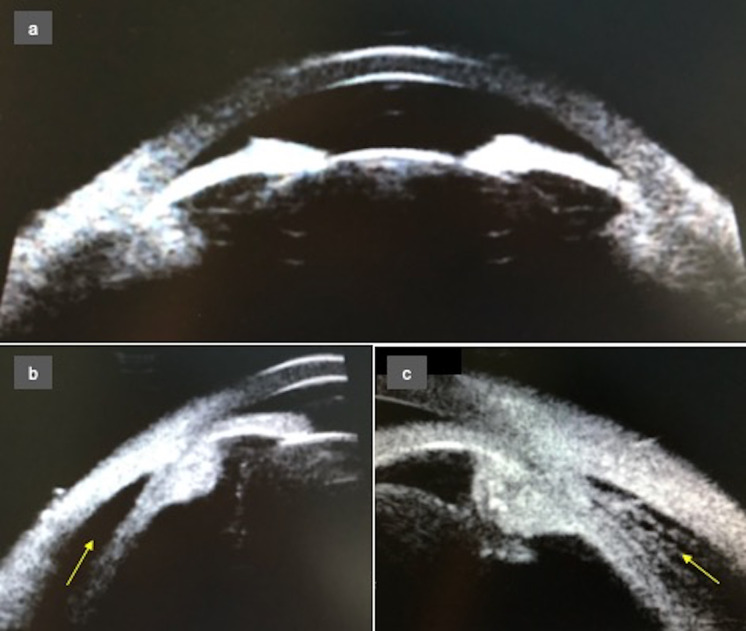
Fig. 3.
a High-resolution ultrasound biomicroscopy (UBM) of the left eye, showing anterior displacement of the iris–lens diaphragm and shallowing of the anterior chamber. b, c UBM radial section of the cyclodialysis cleft displaying the disinsertion of the longitudinal ciliary muscle fibers from the scleral spur, with fluid in the suprachoroidal space (arrows)
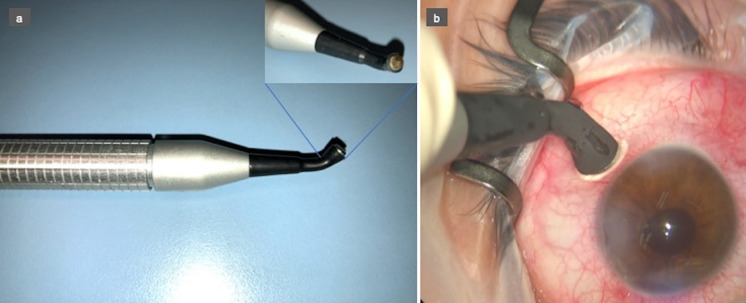
Fig. 4.
a Photograph of the glaucoma cryoprobe used in the procedure, and an inset of its 3-mm-diameter round metal tip. b Transconjunctival cryotherapy application, 1.5 mm behind the limbus, over the cyclodialysis cleft. A temperature of −80 °C is reached and an “ice ball” is formed at the tip of the probe, ensuring successful freezing. Each application was limited to 20 s duration
After the procedure, the patient was advised to rest on his right side for 1 week to guarantee a successful endotamponade. Topical levofloxacin, flurbiprofen, and dexamethasone were prescribed. Atropine 1% twice daily was re-introduced on the second postoperative day and maintained for 2.5 months.
During the early postoperative period, there was a severe anterior chamber inflammatory response (Fig. 5a), with considerable flare and cellular reaction, and a thin hypopyon layer. A small bubble of gas was present in the vitreous cavity for only 5 days (Fig. 5b) and, during that time, IOP increased to 7 mmHg. The inflammation gradually resolved with topical treatment, and 2 weeks after the procedure, the IOP increased to 12 mmHg. By the second postoperative month, successful closure of the cyclodialysis cleft was achieved, as proved by gonioscopy and UBM (Fig. 6a). Fundus examination no longer showed signs of hypotonic maculopathy (Fig. 6b) or choroidal detachment. Three months after the procedure, Nd:YAG laser capsulotomy was performed due to posterior capsular opacification, and the BCVA improved to 20/25. The IOP remained constant (12 mmHg) during the next 14 months of follow-up.
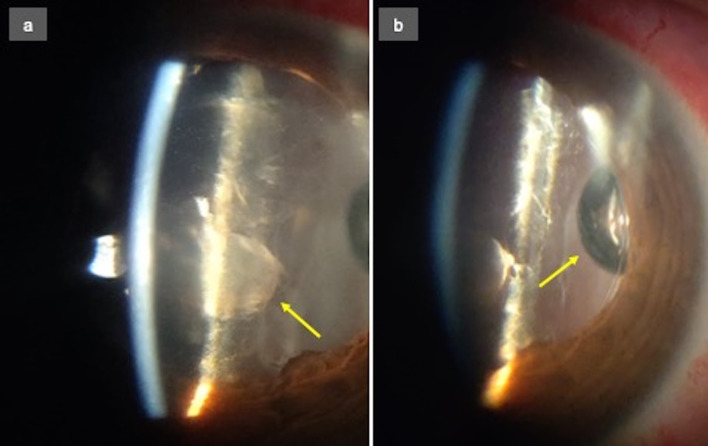
Fig. 5.
a Slit-lamp photograph of patient’s left eye by the second postoperative day. There is a marked anterior chamber inflammatory reaction, with cells and flare and a fibrinoid pupillary membrane (arrow). The hypopyon layer is not visible in this image. b The same image showing the small gas bubble present in the vitreous cavity (arrow)
Fig. 6.
a UBM radial scan 2 months after the procedure, demonstrating closure of the cyclodialysis cleft. b Infrared image (left panel) and OCT scan (right panel) showing resolution of the hypotonic maculopathy
This case report complies with the guidelines for human studies and was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The patient gave his consent to publish this report and all accompanying images.
Discussion
Treating a cyclodialysis cleft is a daunting task for any ophthalmologist. Due to the rarity of this disorder, and the consequent lack of strong scientific evidence, there are no established treatment guidelines [1, 6].
Medical treatment is consensually accepted as an adequate starting point for all patients. Theoretically, long-acting cycloplegics can close the clefts by relaxation of the ciliary muscle, thus facilitating its apposition to the sclera. However, the success rate of this conservative approach is disappointingly low, frequently creating the need to resort to more interventionist modalities [1, 4].
Laser-based treatments, such as ab interno argon laser photocoagulation and ab externo transscleral YAG or diode laser cyclophotocoagulation, act by generating a localized inflammatory reaction that stimulates cleft closure. However, the outcomes of these approaches can be unpredictable, and they are usually reserved for small clefts [1, 5].
Surgical modalities, namely direct cyclopexy, scleral buckling, vitrectomy (either alone or in combination with cryotherapy or endotamponade), and implantation of a CTR or IOL in the ciliary sulcus, are required for larger clefts, but they have all the inherent risks of invasive intraocular procedures [1, 4, 5].
Herein, we present the successful resolution of a traumatic cyclodialysis by gas endotamponade combined with cyclocryotherapy. This minimally invasive procedure takes advantage of the ability of gas to induce mechanical apposition between the ciliary body and the sclera, along with the inflammatory cicatricial reaction produced by cryotherapy.
Ceruti et al. reported a similar technique with a comparable good outcome [7], but in our case, simultaneous traumatic cataract surgery by phacoemulsification was performed. To the best of our knowledge, this “triple” procedure is the first of its kind to be described in the literature.
Our group previously published an analogous case, using a different type of gas (16% hexafluoroethane–air mixture–C2F6) [8]. This time, we elected the 20% sulfur hexafluoride–air mixture (SF6), hoping to lessen the potential effect of an excessive inflammatory reaction of both phacoemulsification and cryotherapy, on a rebound postoperative hypertensive spike.
There was no hypertensive spike, but the loss of a considerable amount of SF6 during eye injection due to accidental patient reaction might have contributed to that.
Additionally, considering the small amount of gas and the short period of time it remained in the vitreous cavity, it seems reasonable to admit that the inflammation induced by cryotherapy might have had a dominant effect in cleft closure and that eventually it might have sufficed. A review of the available literature suggests, however, that cryotherapy alone, without combined gas endotamponade or vitrectomy, has a minimal success rate [1].
The implantation of a CTR and/or IOL in the ciliary sulcus is another proposed option for cleft repair when a cataract is present [9, 10]. In our case, zonular damage and bag disinsertion precluded such a possibility.
Conclusion
Gas endotamponade followed by cyclocryotherapy is an advantageous alternative method for treating a cyclodialysis cleft. First of all, this is a minimally invasive technique free of the dangers associated with more invasive intraocular procedures. Secondly, it is technically simple and can therefore be executed without the need for a highly experienced surgeon. Lastly, our case demonstrated that it can be safely combined with other ocular procedures such as cataract surgery.
Although further studies are necessary to validate the outcomes and safety profile of such a technique, this is a promising option in the treatment of cyclodialysis clefts unresponsive to medical therapy.
Acknowledgements
The authors would like to thank the patient of this report.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Mariana Leuzinger-Dias, Mário Lima-Fontes, Paulo Freitas-Costa and António Benevides-Melo. The first draft of the manuscript was written by Mariana Leuzinger-Dias, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Compliance with Ethics Guidelines
This case report complies with the guidelines for human studies and was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The patient gave his consent to publish this report and all accompanying images.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed for this article.
References
- 1.González-Martín-Moro J, Contreras-Martín I, Muñoz-Negrete FJ, Gómez-Sanz F, Zarallo-Gallardo J. Cyclodialysis: an update. Int Ophthalmol. 2017;37(2):441–457. doi: 10.1007/s10792-016-0282-8. [DOI] [PubMed] [Google Scholar]
- 2.Selvan H, Gupta V, Gupta S. Cyclodialysis: an updated approach to surgical strategies. Acta Ophthalmol. 2019;97(8):744–751. doi: 10.1111/aos.14210. [DOI] [PubMed] [Google Scholar]
- 3.Shaffer RN, Weiss DI. Concerning cyclodialysis and hypotony. Arch Ophthalmol. 1962;68:25–31. doi: 10.1001/archopht.1962.00960030029006. [DOI] [PubMed] [Google Scholar]
- 4.Ioannidis AS, Barton K. Cyclodialysis cleft: causes and repair. Curr Opin Ophthalmol. 2010;21(2):150–154. doi: 10.1097/ICU.0b013e3283366a4d. [DOI] [PubMed] [Google Scholar]
- 5.Senthilkumar V, Rajendrababu S. Current concepts in the management of cyclodialysis. TNOA J Ophthalmic Sci Res. 2020;58(4):274–279. doi: 10.4103/tjosr.tjosr_77_20. [DOI] [Google Scholar]
- 6.Popovic M, Shareef S, Mura JJ, Valenzuela F, González Martín-Moro J, Schlenker MB, et al. Cyclodialysis cleft repair: a multi-centred, retrospective case series. Clin Exp Ophthalmol. 2019;47(2):201–211. doi: 10.1111/ceo.13378. [DOI] [PubMed] [Google Scholar]
- 7.Ceruti P, Tosi R, Marchini G. Gas tamponade and cyclocryotherapy of a chronic cyclodialysis cleft. Br J Ophthalmol. 2009;93(3):414–416. doi: 10.1136/bjo.2008.146266. [DOI] [PubMed] [Google Scholar]
- 8.Pinheiro-Costa J, Melo AB, Carneiro ÂM, Falcão-Reis F. Cyclodialysis cleft treatment using a minimally invasive technique. Case Rep Ophthalmol. 2015;6(1):66–70. doi: 10.1159/000375442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malandrini A, Balestrazzi A, Martone G, Tosi GM, Caporossi A. Diagnosis and management of traumatic cyclodialysis cleft. J Cataract Refract Surg. 2008;34(7):1213–1216. doi: 10.1016/j.jcrs.2008.02.038. [DOI] [PubMed] [Google Scholar]
- 10.Yuen NS, Hui SP, Woo DC. New method of surgical repair for 360-degree cyclodialysis. J Cataract Refract Surg. 2006;32(1):13–17. doi: 10.1016/j.jcrs.2005.05.035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed for this article.