Abstract
The influenza A non-structural protein 1 (NS1) is known for its ability to hinder the synthesis of type I interferon (IFN) during viral infection. Influenza viruses lacking NS1 (ΔNS1) are under clinical development as live attenuated human influenza virus vaccines and induce potent influenza virus-specific humoral and cellular adaptive immune responses. Attenuation of ΔNS1 influenza viruses is due to their high IFN inducing properties, that limit their replication in vivo. This study demonstrates that pre-treatment with a ΔNS1 virus results in an antiviral state which prevents subsequent replication of homologous and heterologous viruses, preventing disease from virus respiratory pathogens, including SARS-CoV-2. Our studies suggest that ΔNS1 influenza viruses could be used for the prophylaxis of influenza, SARS-CoV-2 and other human respiratory viral infections, and that an influenza virus vaccine based on ΔNS1 live attenuated viruses would confer broad protection against influenza virus infection from the moment of administration, first by non-specific innate immune induction, followed by specific adaptive immunity.
Subject terms: Microbiology, Vaccines, Live attenuated vaccines
Introduction
The type I interferon (IFN) response resulting from invading viral pathogens is considered as one of the first lines of antiviral defence mechanisms in higher organisms. The latter process takes place upon the detection of the pathogen associated molecular patterns (PAMPS) by the host pattern recognition receptors (PRRs). Secretion of interferons takes place in both paracrine and autocrine signalling mechanisms, mediated by the canonical JAK/STAT signal transduction pathway along with the transcriptional activation of a particular set of host genes as well as their corresponding promotors defined as IFN-stimulated response elements (ISREs)1. Subsequent activation of the downstream interferon stimulated genes (ISGs) lead to the transcriptional induction of a plethora of antiviral proteins, including dsRNA-activated protein kinase (PKR) leading to a halt of protein translation, dsRNA-activated oligoadenylate synthetases (OAS) which facilitate the degradation of RNA by activating RNAse L and Mx proteins which essentially sequester incoming viral components such as nucleocapsids2,3. Many studies have demonstrated that viruses have evolved to encode numerous mechanisms to prevent the host IFN-mediated antiviral response at different stages4. Viral non-structural proteins such as those of Toscana virus, dengue and HPV can sequester host factors to inhibit type I IFN response5–7, while viruses such as vaccinia, adeno and Ebola viruses secrete soluble ligands7,8, or encode miRNAs9,10 and other proteins to confer immune-evasion.
The influenza A virus (IAV) non-structural protein 1 (NS1) facilitates several functions ranging from inhibition of host mRNA polyadenylation and subsequent inhibition of their nuclear export as well as inhibition of pre-mRNA splicing11,12. A growing body of evidence to date has indicated that influenza NS1 protein has IFN antagonistic activity. It was initially shown that a recombinant influenza A virus that lacks the NS1 protein(ΔNS1) grew to a titer similar to that of WT virus in IFN deficient systems, albeit being markedly attenuated in IFN competent hosts13. This attenuated phenotype can be explained by the inability of the virus to prevent NS1 mediated IFN inhibition. The NS1 protein has been shown to bind to TRIM25 whereby the ubiquitination of the viral RNA sensor RIG-I is inhibited, which eventually results in the inhibition of IFN induction14,15. NS1 has also been shown to prevent IFN production by sequestering the cellular cleavage and polyadenylation specificity factor 30 (CPSF30) in order to halt the processing of host pre-mRNAs, resulting in accumulation of pre-mRNAs in the nucleus as well as the halt of cellular mRNA export to the cytoplasm16. This subsequently results in the inhibition of host protein production, including IFNs and proteins encoded by IFN inducible genes17,18 NS1 has also been shown to inhibit the antiviral activity of several IFN-stimulated genes, such as the 2′–5′- oligo A synthase (OAS)19.
Consistent with its function, deletion of NS1 in recombinant IAV results in a live attenuated and highly immunogenic IAV. As a result, IAV with impaired NS1 function are currently used as vaccines against swine influenza in pigs20 and they are under clinical consideration as live attenuated human influenza virus vaccines21–23.
Based on the growing body of evidence showing the IFN antagonistic properties of IAV NS1, we investigated the ability of the ΔNS1 viruses to induce an IFN response in vivo along with the biological antiviral consequences mediated by the type I IFN induction. Our results demonstrate that the ΔNS1 virus is an efficient inducer of IFN with antiviral properties in both mice and embryonated eggs. Our data indicates the suitability of ΔNS1 virus as a prophylactic agent to induce immediate mucosal antiviral responses with the aim of preventing acute respiratory infections caused by IFN sensitive viruses. ΔNS1 influenza viruses can provide first innate antiviral protection, followed by adaptive specific IAV protection.
Results
Recombinant influenza A virus lacking the NS1 gene (ΔNS1) induces higher levels of interferon than wild type viruses in embryonated chicken eggs
Previously, we demonstrated that tissue culture-based infections by ΔNS1 viruses induced the transactivation of an ISRE-containing reporter gene13, indicating that infection by ΔNS1 viruses induces higher levels of IFN in comparison to its wild type counterparts. To test whether ΔNS1induces IFN in 10-day old embryonated-chicken eggs, eggs were treated with 103 PFU of ΔNS1 or PR8-WT influenza viruses. Subsequently, the allantoic fluids were harvested 18 h post treatment to measure the levels of IFN by determining the highest dilution that inhibited the cytopathic effect mediated by vesicular stomatitis virus (VSV) in chicken embryo fibroblast (CEF) cells24,25. As indicated in the Supplementary Table 1, four hundred Uml−1 of IFN were detected in the allantoic fluid of eggs infected by ΔNS1 virus. However, allantoic fluids derived from WT-PR8 or mock infections indicated undetectable levels of IFN (< 16 Uml−1).
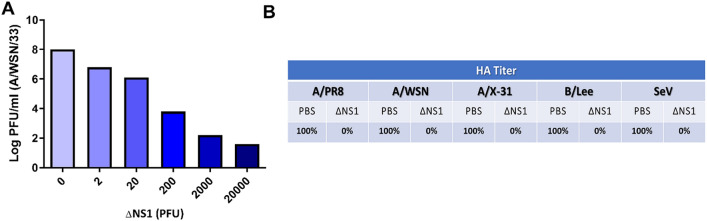
Pre-treatment with ΔNS1 influenza virus inhibits wild-type influenza virus replication in embryonated chicken eggs
We speculated that the ability of the ΔNS1 virus on inducing high titers of IFN in eggs facilitates an antiviral state that may prevent the replication of wild-type IAV. To evaluate this, increasing amounts of ΔNS1 virus were inoculated into eggs and 8 h post-treatment, the eggs were challenged with wild-type A/WSN/33 (WSN-WT) virus with a dose of 103 PFU. Two days post incubation extracted allantoic fluids were titrated via plaque assays. WSN viral titers decreased with ΔNS1 in a dose dependent manner. While the untreated allantoic fluids supported the growth of WSN virus to an approximate titer of 108 PFUml−1, administration of a dose as little as 2 × 104 PFUml−1 of ΔNS1 prevented the replication of WSN virus (less than 102 PFUml−1 of WSN were obtained in eggs). The titer of WSN virus was reduced by one log, by pre-treating allantoic fluids with as little as 2 PFU of ΔNS1 (Fig. 1A).
Figure 1.
Pre-incubation with ΔNS1 virus inhibits viral replication in embryonated chicken eggs. (A) 10-day-old embryonated chicken eggs (n = 2 per group) were inoculated with varying amounts of (PFU) of ΔNS1 virus in the allantoic cavity. Eight hours post infection at 37 °C, eggs were re-infected with 104 PFU of WT A/WSN/33 influenza virus and incubated at 37 °C for 40 h. Allantoic fluids were then titrated by plaque assay MDBK cells. (B) 10-day-old embryonated chicken eggs (n = 2 per group) were inoculated with 2 × 104 PFU of ΔNS1 virus or PBS (Untreated). 8 h post inoculation at 37 °C, the eggs were re-infected with 103 PFU of A/WSN/33 (WSN/H1N1), A/PR/8 (PR8/H1N1), A/X-31 (X-31/H3N2), B/Lee/40 (B-Lee influenza B) or Sendai Virus (Sendai). B-Lee infected eggs were incubated at 35 °C for additional 40 h. All other eggs were incubated at 37 °C for additional 40 h. Virus present in the allantoic fluid was titrated by hemagglutination assays. Maximum hemagglutination titers (100%) for each individual virus were 2048 (PR8), 1024 (X-31), 256 (B-Lee), 512 (Sendai).
Interestingly, treatment using ΔNS1 virus further inhibited the replication of other viruses, as depicted in Fig. 1B. Relative HA titers were obtained from eggs treated with 2 × 104 PFUml−1 of ΔNS1 virus followed by subsequent infection with wild-type Influenza A H1N1 strains WSN and PR8, H3N2 strain X-31, influenza B virus or Sendai virus (SeV; a paramyxovirus). In all cases, pre-treatment with ΔNS1 resulted in a two-log reduction of wild-type viral HA titers.
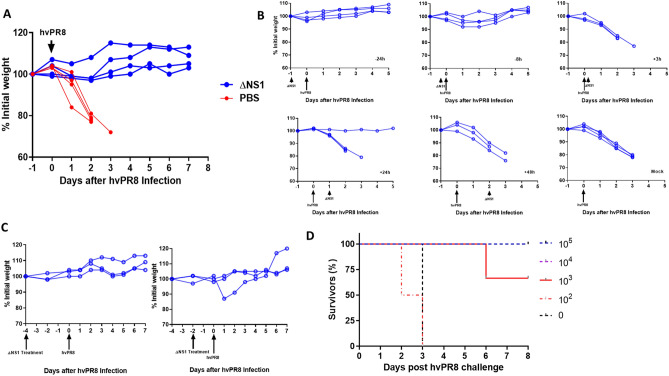
Severe disease and death caused by infection with the highly virulent PR8 virus (hvPR8) in A2G mice can be alleviated by ΔNS1 pre-treatment
In order to assess whether or not the administration of ΔNS1 virus inhibits replication of influenza viruses in mice, an inbred mouse strain that is homozygous for the gene which codes for the IFN induced full-length Mx1 protein, defined as C57BL/6-A2G (abbreviated as A2G) mice were used for this part of the study26,27. Previous studies have concluded that IFN administration was ineffective in preventing IAV replication in laboratory mice lacking a functional Mx1 gene28. In contrast, A2G mice which were administered IFN remained alive upon infection with the highly virulent hvPR8 IAV strain29. The presence of a functional Mx1 gene in A2G mice better mirrors the human situation, as Mx1 gene deficiencies in humans are rare. Here, A2G mice were intranasally infected with a dose of 5 × 105 PFUml−1 of ΔNS1 virus or PBS at − 24, − 8, + 3, + 24 and + 48 h. Mice were challenged at time 0 intranasally with 5 × 106 PFU of hvPR8 virus. Mice treated with ΔNS1 virus were protected from hvPR8 virus as measured by weight loss and death while the PBS treated mice succumbed to death (Fig. 2A).
Figure 2.
A single dose of ΔNS1 virus protects A2G mice against lethal infection by highly virulent hvPR8 influenza virus when given prior to virus challenge. (A) Treatment with ΔNS1 virus protects A2G mice against lethal infection by highly virulent hvPR8 influenza virus. Eight 6-week old A2G mice were intranasally infected with 5 × 106 PFU of highly virulent A/PR/8/34 (hvPR8) influenza virus. Half of the mice received a total of five intranasal treatments with 5 × 105 PFU of ΔNS1 virus at the following times with respect to the hvPR8 infection: − 24 h, − 8 h, + 3 h, + 24 h ad 48 h. The remaining four mice were treated with PBS and the bodyweight changes and survival was monitored. (B) A single dose of ΔNS1 virus protects A2G mice against lethal infection by highly virulent hvPR8 influenza virus when given prior to hvPR8 virus challenge. Groups of three A2G mice each were mock-treated or treated intranasally with 5 × 105 PFU of ΔNS1 at time points − 24 h, − 8 h, + 3 h, + 24 h, + 48 h relative to the intranasal infection by 5 × 106 hvPR8 influenza virus. (C) A single dose of ΔNS1 virus protects A2G mice against lethal infection by highly virulent hvPR8 influenza virus when given 2 and 4 days prior to hvPR8 virus administration Groups of three A2G mice were intranasally treated with 5 × 105 PFU of ΔNS1 virus 4 days or 2 days before infection by 5 × 106 hvPR8 influenza virus. Bodyweight changes and survival was monitored. All data points are from individual mice. (D) Determination of the minimal effective therapeutic dose of ΔNS1 to prevent lethal hvPR8 virus infection in A2G mice. Groups of three A2G mice were intranasally infected with 105, 104 or 103 PFU ΔNS1 influenza virus. Additionally, groups of two A2G mice were intranasally challenged with 102 of ΔNS1 virus or PBS. 24 h post inoculation, mice were challenged with by 5 × 106 hvPR8 influenza virus. The percentage of mice surviving the challenge is represented.
Subsequently, we examined whether all five ΔNS1 treatments were essential for the protective effect against hvPR8 infection in mice. Hence, a single dose of 5 × 106 PFU of ΔNS1 virus was given at various time points relative to the infection with hvPR8. Data indicated (Fig. 2B) that pre-treatment (hours 24 or 8 before hvPR8 challenge) but not post treatment (even 3 h post hvPR8 challenge) of ΔNS1 resulted in the prevention of weight loss disease and subsequent death. Additionally, ΔNS1 virus administered two or four days prior to hvPR8 challenge completely protected mice from disease (Fig. 2C).
Next, to obtain the effective dose 50 (ED50) of ΔNS1 virus to mediate protection against disease from hvPR8 infection, 2 × 105, 2 × 104, 2 × 103or 2 × 102 doses of ΔNS1 virus were intranasally administered to A2G mice 24 h prior to hvPR8 challenge. As shown in Fig. 2D, the ED50 of the ΔNS1 virus which conferred protection in A2G mice against hvPR8-induced death was approximately 103 PFU.
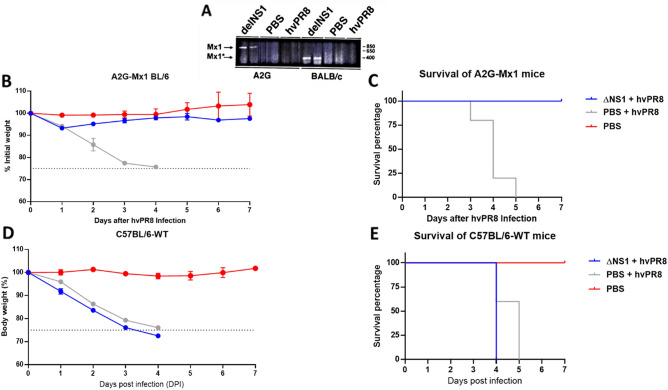
Induction of Mx1 specific mRNA in mice treated with ΔNS1 virus
To investigate whether ΔNS1 infection in mice resulted in induction of the Mx1 gene, an RT-PCR assay for Mx1 specific mRNA in infected animal lungs was developed. In parallel, infections were performed in BALB/c mice which have a non-functional Mx1 gene due to a large frameshift deletion28. As seen in Fig. 3A, treatment with ΔNS1 resulted in the early induction (24 h post infection) of Mx1 specific mRNA in both A2G and BALB/c mice. In contrast a very faint band was present in A2G mice infected with hvPR8 virus at the same time post infection and no specific mRNA was detected in mock infected mRNA.
Figure 3.
Dose dependent pre-treatment of ΔNS1 protects A2G-Mx1 mice but not wild-type C57BL/6 from a lethal hvPR8 virus challenge. (A) Induction of Mx1 specific mRNA expression in ΔNS1 virus infected mice. Groups of two A2G or BALB/c mice were intranasally treated with PBS or 2.5 × 105 PFU of ΔNS1 hvPR8 influenza viruses. 24 h post challenge, total RNA present in lung tissues were extracted and were used for RT-PCR reactions using Mx1 specific primers. PCR products were run in an agarose gel; the arrows indicate the predicted size of amplified cDNA from Mx1 genes pf A2G mice (Mx1) and BALB/c mice (Mx1*). (B, C, D, E) Sex matched 6 weeks old groups C57BL/6-A2G-Mx1 mice or C57BL/6-wild-type mice were either intranasally pre-treated with PR8-ΔNS1 (5 × 106 PFU; n = 5 per group), sterile PBS (n = 5) 12 h before a lethal challenge of hvPR8 (5 × 105 PFU; n = 5) or treated with only sterile PBS (n = 2). (B) Morbidity of C57Bl/6-A2G-Mx1 mice. (C). Survival of C57Bl/6-A2G-Mx1 mice. (D). Morbidity of C57Bl/6-wild-type mice. (E). Survival of C57Bl/6–6-wild-type mice.
ΔNS1 mediated protection from hvPR8 is Mx1-mediated
As the Mx1 protein is one of the most potent IFN inducible gene products with anti-influenza virus activity in mice, it is quite possible that the ΔNS1-mediated protection seen in A2G mice is Mx1-mediated. To test this hypothesis, we compared the antiviral activity of ΔNS1 in A2G mice and in C57BL/6 mice. C57BL/6 mice harbour a non-functional Mx1 gene due to a known deletion28 and were used as a back-cross genetic platform for the original A2G strain to generate the Mx1 positive A2G mice used in our experiments. A dose of PR8-ΔNS1 containing 5 × 106 PFU given 12H before a lethal hvPR8 challenge protected all A2G-Mx1 mice (n = 5) in both morbidity and mortality in comparison to the PBS pre-treated group (n = 5) (Figs. 3B,C). However, all five Mx1-deficient mice in the wild-type C57BL/6 group that were given the same dose of PR8-ΔNS1 succumbed to death by a lethal hvPR8 challenge. The morbidity data for these mice based on body weight was also consistent with lack of protection after ΔNS1 treatment from hvPR8 challenge, indicating that the antiviral effect on IAV induced in mice by ΔNS1 treatment is dependent on the IFN-inducible gene Mx1 w (Fig. 3D,E).
ΔNS1 viral treatment inhibits the replication of hvPR8 virus in A2G mice lungs
To better understand the ability of the ΔNS1 virus to inhibit replication of the hvPR8 virus in the lungs, A2G mice were intranasally treated with 2 × 105 PFU of ΔNS1 virus alone, 2 × 104 PFU of hvPR8 alone or treatment of 2 × 105 PFU of ΔNS1 virus 24 h before infecting them with 2 × 104 PFU of hvPR8 virus. Mice were sacrificed at three- and 6-days post infection and the lung homogenates were titrated in MDCK or Vero cells (Supplementary Table 2). A reduction of hvPR8 titers in lungs by fourfold was observed when mice were pre-treated with ΔNS1 virus. Furthermore, mice solely infected with ΔNS1 virus had titers below the detection limit (< 10 PFUml−1), while not showing any significant reduction of bodyweight. It was apparent that infection by hvPR8 virus without ΔNS1 administration resulted in the increase of lung weight by a factor of two or three in comparison to mice that were pre-treated with ΔNS1 virus. In the context of this study, increased lung weights are suggestive of lymphocytic infiltration and pulmonary disease during Influenza virus infection30,31.
Attenuated influenza viruses via a mutation in the Neuraminidase (NA) gene does not confer ΔNS1-like antiviral properties
Antiviral properties observed thus far in this study is from an attenuated influenza virus lacking the NS1 gene (ΔNS1). To confirm that the protective effects observed here are not due to the attenuation caused by the lack of a gene but specifically due to the lack of NS1, the antiviral property of ΔNS1 virus was compared to that of a the recombinant D2 influenza virus. The D2 virus contains a base-pair mutation in the dsRNA region formed by the non-coding sequences of its NA gene. This mutation is responsible for a tenfold reduction in the NA protein levels as well as a one-log reduction in viral titers within a multicycle growth curve32. The latter D2 strain has also been shown to be highly attenuated in mice with a LD50 of more than 106 PFU upon intranasal administration33. Identical doses (2.5 × 105 PFU) of D2 or ΔNS1 viruses were intranasally administered to A2G mice 4 h prior to challenge with 5 × 106 PFU of hvPR8. Although a prolonged survival was seen in one of the animals who received D2, pre-treatment with D2 was ineffective in protecting A2G mice from hvPR98 virus-induced disease and death (Fig. 4).
Figure 4.
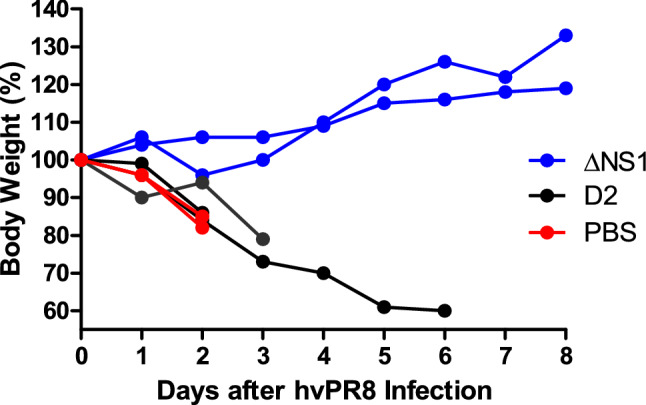
Comparison of the antiviral properties in A2G mice of recombinant influenza A viruses ΔNS1 and D2. A2G mice were intranasally treated with PBS or 2.5 × 105 PFU of ΔNS1 or D2 viruses for 24 h before infection with 5 × 106 PFU of hvPR8 influenza virus. Bodyweight changes and survival were monitored. Data shown are from individual mice.
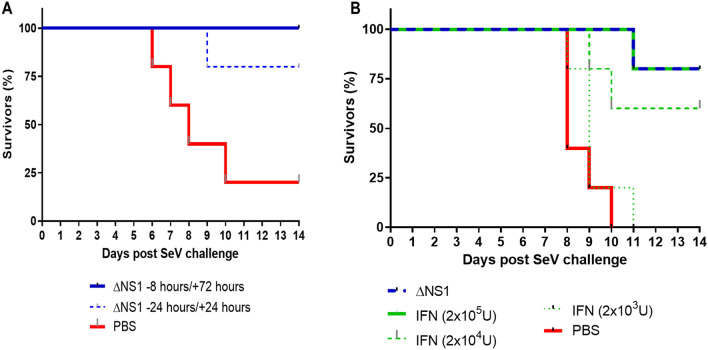
ΔNS1 viral treatment prevents death by Sendai virus (SeV) in C57BL/6 mice
Given the fact, that the antiviral effects against hvPR8 mediated by ΔNS1 viral are facilitated by an IFN mediated mechanism (Mx1 gene induction), we speculated that ΔNS1 treatment should protect mice from infections by other IFN sensitive viruses. Sendai virus was used in this study due to its pneumotropic nature and sensitivity to IFN in Mx1 deficient mice34,35. As seen in Fig. 1B, treatment with ΔNS1 inhibited Sendai viral replication in embryonated chicken eggs. Moreover, upon two intranasal administrations of 2.5 × 105 PFU of ΔNS1 virus to C57BL/6 mice at times − 24 and + 24 h or − 8 and + 72 h, mice infected with 5 × 105 PFU of Sendai virus were protected from death (Fig. 5A). The C57BL/6 mice used here are Mx1−/− and it is indicative that the mouse nuclear Mx1 protein does not have any antiviral activities against cytoplasmic viruses such as Sendai virus36. The efficacy of ΔNS1 treatment was compared against three doses of IFN-β using the Sendai virus challenge model. Treatment with the highest dose of IFN-β (2 × 105 U) protected mice from death induced by Sendai virus comparable to treatment with 2.5 × 105 PFU of ΔNS1 virus (Fig. 5B).
Figure 5.
Treatment with ΔNS1 influenza virus protects C57BL/6 mice against lethal infection with Sendai virus. All mice were challenged intranasally with a lethal dose of Sendai virus corresponding to (A) 5 × 105 PFU or (B) 1.5 × 105 PFU. The percentage of mice surviving the challenge is represented. (A) Groups of five mice were treated intranasally with 2.5 × 105 PFU of ΔNS1 virus at the indicated times. (B) Groups of five mice were intranasally treated at − 24 h and + 24 h with respect to the infection with Sendai virus with 2.5 × 105 PFU of ΔNS1 or with the indicated amounts of IFN-β.
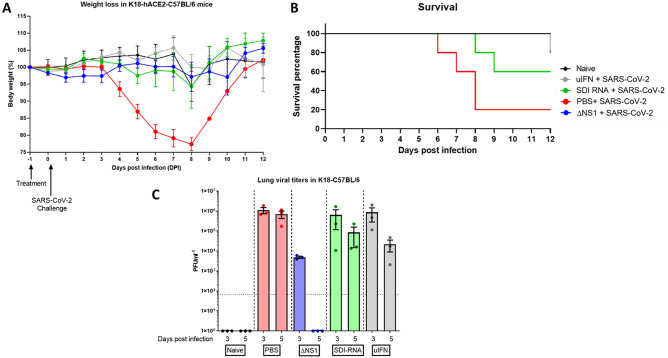
ΔNS1 virus treatment inhibits viral replication of SARS-CoV-2 virus in K18-hACE2-C57Bl/6 murine lungs
Given the emergence of the devastating COVID-19 pandemic, we assessed whether prophylactic treatment with ΔNS1 would hinder the replication of SARS-CoV-2. We used the transgenic mouse model that supports the replication of SARS-CoV2. As controls, we used universal IFN, and SeV defective RNA (SDI) which were previously shown to have an IFN inducing effect. Weight determination in all the treated groups showed no major loss in bodyweight, only one mouse each from the SDI treated group (day 8) and the uIFN treated group (day 12) reached below 75% bodyweight (Fig. 6A). Deaths (4 out of 5) in the mock treated group occurred between days 6–8 post infection. The SDI-RNA treated group lost 2 out of 5 animals on day 8 and 9 while the uIFN group lost one animal out of 5 at a later time point (D12; Fig. 6B). While both treatments resulted in reduction of viral titers day 3 and 5 post infection, mice that received ΔNS1 showed significant inhibition of SARS-CoV2 titers in lung homogenates and no detectable infectious viruses at day 5 post infection (Fig. 6C).
Figure 6.
Treatment with ΔNS1 influenza virus inhibits viral replication in the lungs of K18-hACE2 mice challenged with SARS-CoV-2. Mice were intranasally treated with 30 ul containing PBS, 2.5 × 106 PFU of ΔNS1, 1 μg defective interfering RNA from Sendai virus (SDI-RNA), 2.5 × 105 U of universal-interferon (uIFN) 24 h before intranasal challenge with 104 PFU of SARS-CoV-2/USA/WA1 isolate. (A) Weight-loss was monitored in mice (n = 11 for treated groups and n = 6 naïve) and (B) survival was monitored for 12 days. (C) Lungs were harvested at days three and five post infection (n = 3 per group per day) were homogenized and were titered in Vero-E6 cells using standard plaque assays.
Discussion
The NS1 protein of the influenza A virus has been shown to possess IFN antagonist activity whereby it is able to dampen the host innate immune response to provide a favourable environment for the virus to replicate. It has been demonstrated to be highly expressed in the host cytoplasm and nucleus upon viral infection, interacting with a plethora of host factors to inhibit the interferon response37. Data show the ability of NS1 to compete with innate immune sensors such as RLR to bind to dsRNA to avoid innate immune detection38. Additionally, NS1 has been shown to interact with other innate immune signalling components such as PKR39, TRIM2540 and CPSF16, resulting in lowering of the IFN mediated innate immunity41. For these reasons, influenza viruses with impaired NS1 function (and an increased innate immune response) have been under consideration for live attenuated influenza vaccines. There is an existing swine influenza vaccine based on NS1-deficient live attenuated viruses42, and clinical trials in humans using an intranasally administered live attenuated ΔNS1 virus have demonstrated potent immunogenicity and good safety profiles. Experimental evidence in mice indicates that the high IFN-inducing properties of ΔNS1 viruses are responsible for their superior immunogenicity as live vaccines43,44.
As ΔNS1 viruses are great IFN inducers, we reasoned that they might provide with innate protection against respiratory virus infection even before the development of an influenza virus specific adaptive immune response. Treatment with ΔNS1 virus inhibited the replication of both homologous and heterologous viruses in eggs (Fig. 1). Using the A2G-Mx1 mouse model, we demonstrated that the intranasal administration of the ΔNS1 virus induced an antiviral state, which prevented disease and death by a highly pathogenic influenza A virus (hvPR8) which is otherwise lethal45. Infection with ΔNS1 virus but not WT viruses yielded detectable levels of Mx1-specific mRNA levels in lungs 24 h post infection (Fig. 2). A large body of evidence has indicated that the protective impact of IFN against IAV infection in mice is mainly mediated by the IFN inducible antiviral Mx1 gene46–48. Consistently, we found that Mx1 was required for the ΔNS1 mediated protection against lethal hvPR8 challenge by comparing Mx1 competent A2G-C57BL/6 mice with Mx1 deficient WT-C57BL/6 mice.
Data depicted in Fig. 2C show that pre-treatment of A2G mice with ΔNS1 virus up to 4 days before the challenge with hvPR8 virus was effective in preventing disease. The Mx1 protein in mice is known to be stable for several days upon its induction and our observations are consistent with the half-life of the Mx1 protein described in mice49,50.
Given the inherently attenuated state of the ΔNS1 viruses, it was necessary to confirm that the antiviral state seen here is due to the specific attenuation of the ΔNS1 segment. We used a virus that is known to be attenuated due to its defective neuraminidase segment (D2 virus expressing a full-length NS1)33 to demonstrate that protection is not just mediated by any attenuated IAV (Fig. 4). ΔNS1 treated mice were also protected from lethal infection with an influenza-unrelated pneumotropic Sendai virus, suggesting that the IFN-mediated innate immune response induced by ΔNS1 has broad-antiviral effects, rather than being a pathogen-specific immune response. As anticipated for Sendai virus, the abovementioned protection was not Mx1 mediated and is most likely due to the activation of other ISGs such as OAS or PKR upon the ΔNS1-mediated IFN production51.
The feasibility of ΔNS1 virus as a prophylactic treatment to induce a type I interferon response to prevent acute respiratory infections from IFN sensitive viruses was demonstrated in the current study. Type I interferon administration has been used to treat a range of human diseases ranging from infections such as hepatitis B and C52,53 to other non-communicable diseases such as melanomas54 and hairy-cell leukaemia55. Although IFN has been promoted as a therapeutic agent, administration of exogenous interferon comes with a set of undesirable side effects56,57, arguably due to it causing major endocrine and metabolic changes in the host58. Therefore, various groups have attempted alternative ways to induce local type I IFN responses using different strategies. Some of these strategies were topical administration of plasmid DNA coding for IFNα1 in the mouse eye to protect against HSV-1 encephalitis59, liposomic intranasal treatment using dsRNA to induce IFN60 as well as recombinant viral vectors such as adenoviruses61 and hepatitis B viruses to express type I IFN to protect against infection and tumor regression61. Despite these experimental attempts to study the efficacy of IFN, it is still unclear whether virally induced IFN is more or less toxic efficient that IFN itself. This indicates that further work is needed to be done to ascertain the suitability of recombinant viruses as IFN inducers for therapeutic purposes. The physiological half-lives and binding affinities of different types of interferons are well studied and their half-lives can range from minutes to several hours, depending on the type of IFN62. Our data showed antiviral properties of ΔNS1 virus for up to 4 days before the viral challenge. While it is known that therapeutic properties and doses of different types of IFNs are highly variable due to their differential effects contributed by the ISGs, most therapeutic properties of type I interferons are yet to be completely understood63,64. In this instance, comparable prophylactic responses were obtained by the administration of either 2 × 105 U of IFN-β or 2 × 105 PFU of ΔNS1 virus (Fig. 5B). However, it is acknowledged that different subsets of IFN-regulated genes may differ in their relative transcriptional induction between treatments.
We also demonstrated that prophylactic treatment using ΔNS1 significantly inhibited viral replication in a relevant mouse model that can be infected with WT SARS-CoV-2 and is known to result in lethal infection65 (Fig. 6). This agrees with reports that state that SARS-CoV-2 is sensitive to IFN66. Interestingly, a similar level of reduction in viral titers was not seen upon intranasal inoculation of universal-IFN nor defective interfering RNA derived from SeV (SDE-RNA; a RIG-I agonist with known adjuvanting properties)67. While these treatments resulted in a better outcome in comparison to PBS pre-treatment, high amounts of viral titers were still observed day three and five post infection. Although weight loss and survival were best in the ΔNS1 group, the uIFN treated group showed a protective phenotype indicating that uIFN treatment was better than that provided by SDI-RNA. The difference observed here is likely due to the stimulation of multiple innate immune mechanisms by ΔNS1 which potentially primes cells to confer a broad antiviral phenotype. However, analysis of differentially expressed genes (particularly ISGs) via a technique such as bulk RNAseq would provide more insights in explaining the observed protective effects against COVID-19 in the K18 mouse model.
In conclusion, we report that prophylactic treatment with an attenuated influenza A virus lacking the NS1 gene induces an innate antiviral response which provides protection against IFN-sensitive viruses in both embryonated chicken eggs and mice. These in vivo data further validate previous observations showing the IFN-antagonistic properties of the NS1 protein of influenza A viruses13,68–70, while highlighting the role of NS1 in inhibiting IFN induction during influenza A virus infections. We also provide evidence for its potential as a prophylactic to protect against acute respiratory infections caused by IFN-sensitive viruses including the causative agent of COVID-19 pandemic. ΔNS1 viruses are being clinically developed as live attenuated influenza virus vaccines and in clinical trials they have shown to induce protective antibodies and no adverse responses in human volunteers21–23. Here we show that ΔNS1 viruses have the potential to induce immediate protection against viral infection prior to the induction of specific long-lasting protective adaptive immune responses71,72. Our results should encourage further research on the use of IFN-inducing, live attenuated virus vaccines, to confer innate and adaptive protection against virus pathogens. Further studies looking at the longitudinal changes in ISGs in the respiratory tract upon treatment to correlate with the level of protection from a lethal virus challenge via RNAseq would provide potential mechanistic insights to support the observations in this study and the potential application of this treatment system to prevent the transmission of interferon sensitive viruses.
Methods
Cells and viruses
Recombinant influenza A viruses were generated using reverse genetics as previously described13,32 A derivative of the A/PR/8/34 (PR8) defined as highly virulent PR8 (hvPR8) was kindly provided by O. Haller and J.L. Schulman. This variant of PR8 strain has been adapted to replicate efficiently in Mx1+ murine lungs owing to several mutations in all viral proteins including the HA and NA glycoproteins73. Strain 52 of Sendai virus was obtained from the ATCC. Vero cells, Madin-Darby bovine kidney (MDBK) cells, baby hamster kidney (BHK) cells or embryonated chicken eggs were used to propagate the following viruses as per standard protocols; Influenza A ΔNS1, hvPR8, PR8, A/WSN/33, A/X-31/H3N2, Influenza B/Lee/40, Sendai virus and vesicular stomatitis virus (VSV). Madin-Darby canine kidney (MDCK) cells or Vero cells were plated to obtain confluent monolayers and plaque assays were performed as previously described and an agar overlay in DMEM-F12 including 1 µgml−1 of trypsin was used. MDCK, Vero and BHK cells were cultured in DMEM (Corning 10013CV) in the presence of 10% FBS (PEAK; PS-FB03) and penicillin–streptomycin (Corning 30-0002-CL). The chicken embryo fibroblasts (CEF) purchased from ATCC was maintained in MEM as suggested by ATCC. Vero-E6 cells (ATCC® CRL-1586™, clone E6) were grown in DMEM containing 10% FBS, non-essential amino acids, HEPES and penicillin–streptomycin. SARS-CoV-2, isolate USA-WA1/2020 (BEI resources; NR-52281) was handled under BSL-3 containment in accordance with the biosafety protocols validated by the Icahn School of Medicine at Mount Sinai. Viral stocks were amplified in Vero-E6 cells in the above media containing 2% FBS for 3 days and were validated by whole-genome sequencing using the Oxford-MinION platform.
Animal studies
All animals used in the study were used at 6–10 weeks of age. The Institutional Animal Care and Use Committee (IACUC) of the Icahn School of Medicine at Mount Sinai (ISMMS) reviewed and approved the in vivo protocols included in this study. The animal work of this study is in accordance with the ARRIVE guidelines. A2G mice were kindly provided by Dr. Heinz Arnheiter while the BALB/c and C56BL/6 mice were purchased from Taconic Farms. Hemizygous female K18-hACE2 mice on the C57BL/6J genetic background (Jax strain 034860), were used to conduct studies with SARS-CoV-2 in BSL3 conditions. Anesthetized animals (Ketamine and Xylazine diluted in PBS administered via intraperitoneal injection) were intranasally infected using 30–50 µl of appropriately diluted viruses or PBS containing the indicated amounts of recombinant murine IFN-β (Calbiochem), universal-IFN (PBL assay science) SDI-RNA67. Afterwards, the animals were monitored daily for changes in body weight. All animal studies were done in accordance with the NIH guidelines as well as the guidelines devised by the Icahn School of Medicine with regards to the care and use of laboratory animals.
Measurement of interferon
Ten day old embryonated eggs were infected with 103 PFU in 100 µl containing either ΔNS1, PR8 viruses or PBS as mock. Next, the eggs were incubated at 37 °C and the allantoic fluids were extracted 18 h post infection. Viral inactivation of the allantoic fluids were conducted by dialysis against 0.1 M KCL–HCL buffer at pH 2 for 2 days at 4 °C. Later, the pH of the samples was adjusted to pH 7 by subsequent dialysis against Hank’s balanced sodium salt solution with 20 mM NA3PO4 for two more days as described previously24. The amount of IFN was titrated according to its ability to inhibit the growth of VSV74. In summary, CEF cells in 96-wells were treated with 100 µl of different dilutions of the respective samples in tissue culture media. Upon incubating for an hour at 37 °C, 200 TCID50 of VSV in 10 µl were added to the wells before incubating at 37 °C until complete lysis of untreated control cells was observed (approximately 2 days). As a standard control, recombinant chicken IFN donated by Drs. Peter Staeheli and Bernd Kaspers was used25.
Lung titration
Four A2G mice were intranasally challenged with 2 × 105 PFU of ΔNS1 at day-1. During day 0 mice were intranasally challenged with 2 × 104 PFU of hvPR8 virus. Alternatively, two other groups of four A2G mice were challenged with 2 × 105 PFU ΔNS1 or 2 × 104 PFU of hvPR8. Three days post infection, two animals from each group were humanely sacrificed while the rest of the animals were humanely sacrificed 6 days post infection. Lungs were weighed and homogenized in 2 ml of PBS. Resulting homogenates were clarified via centrifugation at 3000 rpm for 15 min at 4 °C and the acquired supernatants were tittered by plaque assays using MDCK or Vero cells. Lung homogenates derived from SARS-CoV-2 infected K18 mice were handled and titered in Vero-E6 cells as described previously75.
Detection of MX1 Specific mRNA in infected cells
A2G and BALB/c mice were intranasally challenged with 105 PFU of either ΔNS1 or hvPR8 or PBS. Afterwards, lungs were extracted 24 h post infection, snap frozen, homogenized, total RNA was extracted using TRIreagent (Sigma-Alderich). One microgram of total lung RNA was used to perform a RT reaction in a total volume of 20 µl using Mx1 specific primer. Two µl of the resulting RT product was used for PCR amplification using Mx1 specific primers under the following conditions (20 s at 95 °C, 30 s at 55 °C, 30 s at 72 °C for a total of 25 cycles). The sense and antisense primer sequences are as follows; 5′-CAGGACATCCAAGAGCAGCTGAGCCTCACT-3′ and 5′-GCAGTAGACAATCTGTTCCATCTGGAAGTG-3′. The PCR products were analysed using a 1.2% agarose gel. Correct size for the PCR products in A2G mice was 756 bp while it was 333 bp in BALB/c mice due to a deletion in the Mx1 gene between nucleotides 1120–154333.
Supplementary Information
Acknowledgements
The authors acknowledge members of AG-S and PP laboratories for their critical discussions. Technical assistance for the study was provided by Louis Ngyenvu and Richard Cadagan. We thank R. Albrecht for support with the BSL3 facility and procedures at the Icahn School of Medicine at Mount Sinai, New York. A2G mice were kindly provided by Dr. Heinz Arnheiter (NIH). hvPR8 virus was a generous gift from Drs. Otto Haller (University of Freiburg) and Jerome L. Schulman (Icahn School of Medicine). Recombinant Chicken IFN was a gift from Drs. Peter Staeheli (University of Freiburg) and Bernd Kaspers (University of Munich). This work was partly supported by the Centre for on Research for Influenza Pathogenesis, a Center of Excellence for Influenza Research and Surveillance supported by the National Institute of Allergy and Infectious Diseases (contract number HHSN272201400008C), CRIPT (Center for Research on Influenza Pathogenesis and Transmission) a Center of Excellence for Influenza Research and Response (CEIRR, NIAID contract number 75N93021C00014) by the NIAID funded Collaborative Influenza Vaccine Innovation Centers (contract number 75N93019C00051), by NIAID grants R01AI141226, R01AI145870 and P01AI097092, by DARPA grant HR0011-19-2-0020, and by the generous support of the JPB Foundation, the Open Philanthropy Project (research grant 2020-215611 (5384)), and anonymous donors to AG-S and PP.
Author contributions
A.G.-S., P.P., R.R., M.S. and T.M. conceived the project. R.R., M.S., H.Z., T.K., I.M. and S.J. conducted experiments while M.S., R.R. analysed the data and wrote the manuscript.
Competing interests
AG–S and PP are inventors in patents owned by the Icahn School of Medicine and licensed to Vivaldi Biosciences concerning the use of NS1 deficient viruses as human vaccines and to BI Vetmedica on the use of NS1 deficient viruses as veterinarian vaccines. The García-Sastre Laboratory has received research support from Pfizer, Senhwa Biosciences, 7Hills Pharma, Pharmamar, Blade Therapeutics, Avimex, Accurius, Dynavax, Kenall Manufacturing, ImmunityBio and Nanocomposix; and A.G.-S. has consulting agreements for the following companies involving cash and/or stock: Vivaldi Biosciences, Pagoda, Contrafect, Vaxalto, Accurius, 7Hills. The rest of the authors have no conflicts to declare.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-01780-8.
References
- 1.Taft J, Bogunovic D. The Goldilocks zone of Type I IFNs: Lessons from human genetics. J. Immunol. 2018;201:3479–3485. doi: 10.4049/jimmunol.1800764. [DOI] [PubMed] [Google Scholar]
- 2.Ivashkiv LB, Donlin LT. Regulation of type I interferon responses. Nat. Rev. Immunol. 2014;14:36. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schneider WM, Chevillotte MD, Rice CM. Interferon-stimulated genes: A complex web of host defenses. Annu. Rev. Immunol. 2014;32:513–545. doi: 10.1146/annurev-immunol-032713-120231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.García-Sastre AT. strategies of interferon evasion by viruses. Cell Host Microbe. 2017;22:176–184. doi: 10.1016/j.chom.2017.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gori-Savellini G, Valentini M, Cusi MG. Toscana virus NSs protein inhibits the induction of type I interferon by interacting with RIG-I. J. Virol. 2013;87:6660–6667. doi: 10.1128/JVI.03129-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan YK, Gack MU. A phosphomimetic-based mechanism of dengue virus to antagonize innate immunity. Nat. Immunol. 2016;17:523. doi: 10.1038/ni.3393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ronco LV, Karpova AY, Vidal M, Howley PM. Human papillomavirus 16 E6 oncoprotein binds to interferon regulatory factor-3 and inhibits its transcriptional activity. Genes Dev. 1998;12:2061–2072. doi: 10.1101/gad.12.13.2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith GL, Talbot-Cooper C, Lu Y. Advances in Virus Research. Elsevier; 2018. pp. 355–378. [DOI] [PubMed] [Google Scholar]
- 9.Edwards MR, et al. Differential regulation of interferon responses by Ebola and Marburg virus VP35 proteins. Cell Rep. 2016;14:1632–1640. doi: 10.1016/j.celrep.2016.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nidetz NF, Gallagher TM, Wiethoff CM. Inhibition of type I interferon responses by adenovirus serotype-dependent Gas6 binding. Virology. 2018;515:150–157. doi: 10.1016/j.virol.2017.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fortes P, Beloso A, Ortin J. Influenza virus NS1 protein inhibits pre-mRNA splicing and blocks mRNA nucleocytoplasmic transport. EMBO J. 1994;13:704–712. doi: 10.1002/j.1460-2075.1994.tb06310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qiu Y, Krug RM. The influenza virus NS1 protein is a poly(A)-binding protein that inhibits nuclear export of mRNAs containing poly(A) J. Virol. 1994;68:2425–2432. doi: 10.1128/jvi.68.4.2425-2432.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.García-Sastre A, et al. Influenza A virus lacking the NS1 gene replicates in interferon-deficient systems. Virology. 1998;252:324–330. doi: 10.1006/viro.1998.9508. [DOI] [PubMed] [Google Scholar]
- 14.Castanier C, et al. MAVS ubiquitination by the E3 ligase TRIM25 and degradation by the proteasome is involved in type I interferon production after activation of the antiviral RIG-I-like receptors. BMC Biol. 2012;10:44. doi: 10.1186/1741-7007-10-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koliopoulos MG, et al. Molecular mechanism of influenza A NS1-mediated TRIM25 recognition and inhibition. Nat. Commun. 2018;9:1820. doi: 10.1038/s41467-018-04214-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nemeroff ME, Barabino SM, Li Y, Keller W, Krug RM. Influenza virus NS1 protein interacts with the cellular 30 kDa subunit of CPSF and inhibits 3′ end formation of cellular pre-mRNAs. Mol. Cell. 1998;1:991–1000. doi: 10.1016/s1097-2765(00)80099-4. [DOI] [PubMed] [Google Scholar]
- 17.Kuo RL, et al. Role of N terminus-truncated NS1 proteins of influenza A virus in inhibiting IRF3 activation. J. Virol. 2016;90:4696–4705. doi: 10.1128/JVI.02843-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krug RM. Functions of the influenza A virus NS1 protein in antiviral defense. Curr. Opin. Virol. 2015;12:1–6. doi: 10.1016/j.coviro.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mibayashi M, et al. Inhibition of retinoic acid-inducible gene I-mediated induction of beta interferon by the NS1 protein of influenza A virus. J. Virol. 2007;81:514–524. doi: 10.1128/JVI.01265-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richt JA, et al. Vaccination of pigs against swine influenza viruses by using an NS1-truncated modified live-virus vaccine. J. Virol. 2006;80:11009–11018. doi: 10.1128/JVI.00787-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nicolodi C, et al. Safety and immunogenicity of a replication-deficient H5N1 influenza virus vaccine lacking NS1. Vaccine. 2019;37:3722–3729. doi: 10.1016/j.vaccine.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 22.Morokutti A, Muster T, Ferko B. Intranasal vaccination with a replication-deficient influenza virus induces heterosubtypic neutralising mucosal IgA antibodies in humans. Vaccine. 2014;32:1897–1900. doi: 10.1016/j.vaccine.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 23.Mössler C, et al. Phase I/II trial of a replication-deficient trivalent influenza virus vaccine lacking NS1. Vaccine. 2013;31:6194–6200. doi: 10.1016/j.vaccine.2013.10.061. [DOI] [PubMed] [Google Scholar]
- 24.Morahan PS, Grossberg SE. Age-related cellular resistance of the chicken embryo to viral infections. I. Interferon and natural resistance to myxoviruses and vesicular stomatitis virus. J. Infect. Dis. 1970;121:615–623. doi: 10.1093/infdis/121.6.615. [DOI] [PubMed] [Google Scholar]
- 25.Plachý J, et al. Protective effects of type I and type II interferons toward Rous sarcoma virus-induced tumors in chickens. Virology. 1999;256:85–91. doi: 10.1006/viro.1999.9602. [DOI] [PubMed] [Google Scholar]
- 26.Verhelst J, et al. Functional comparison of Mx1 from two different mouse species reveals the involvement of loop L4 in the antiviral activity against influenza A viruses. J. Virol. 2015;89:10879–10890. doi: 10.1128/JVI.01744-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haller O, Arnheiter H, Lindenmann J, Gresser I. Host gene influences sensitivity to interferon action selectively for influenza virus. Nature. 1980;283:660. doi: 10.1038/283660a0. [DOI] [PubMed] [Google Scholar]
- 28.Staeheli P, Grob R, Meier E, Sutcliffe JG, Haller O. Influenza virus-susceptible mice carry Mx genes with a large deletion or a nonsense mutation. Mol. Cell. Biol. 1988;8:4518–4523. doi: 10.1128/mcb.8.10.4518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haller, O., Arnheiter, H., Horisberger, M., Gresser, I. & Lindenmann, J. Genetic-control of antiviral activities of interferon in mice (EXPERIENTIA Ser. 37, BIRKHAUSER VERLAG AG PO BOX 133 KLOSTERBERG 23, CH-4010 BASEL, SWITZERLAND, 1981).
- 30.Guo L, et al. Pulmonary immune cells and inflammatory cytokine dysregulation are associated with mortality of IL-1R1 (−/−)mice infected with influenza virus (H1N1) Zool. Res. 2017;38:146–154. doi: 10.24272/j.issn.2095-8137.2017.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mizuta T, et al. Antisense oligonucleotides directed against the viral RNA polymerase gene enhance survival of mice infected with influenza A. Nat. Biotechnol. 1999;17:583. doi: 10.1038/9893. [DOI] [PubMed] [Google Scholar]
- 32.Fodor E, Palese P, Brownlee GG, Garcia-Sastre A. Attenuation of influenza A virus mRNA levels by promoter mutations. J. Virol. 1998;72:6283–6290. doi: 10.1128/jvi.72.8.6283-6290.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Solorzano A, et al. Reduced levels of neuraminidase of influenza A viruses correlate with attenuated phenotypes in mice. J. Gen. Virol. 2000;81:737–742. doi: 10.1099/0022-1317-81-3-737. [DOI] [PubMed] [Google Scholar]
- 34.Tashiro M, Homma M. Pneumotropism of Sendai virus in relation to protease-mediated activation in mouse lungs. Infect. Immun. 1983;39:879–888. doi: 10.1128/iai.39.2.879-888.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perler L, Pfister H, Schweizer M, Peterhans E, Jungi TW. A bioassay for interferon type I based on inhibition of Sendai virus growth. J. Immunol. Methods. 1999;222:189–196. doi: 10.1016/s0022-1759(98)00198-7. [DOI] [PubMed] [Google Scholar]
- 36.Pavlovic J, Zurcher T, Haller O, Staeheli P. Resistance to influenza virus and vesicular stomatitis virus conferred by expression of human MxA protein. J. Virol. 1990;64:3370–3375. doi: 10.1128/jvi.64.7.3370-3375.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hale BG, Albrecht RA, García-Sastre A. Innate immune evasion strategies of influenza viruses. Future Microbiol. 2010;5:23–41. doi: 10.2217/fmb.09.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Min J, Krug RM. The primary function of RNA binding by the influenza A virus NS1 protein in infected cells: Inhibiting the 2′-5′ oligo (A) synthetase/RNase L pathway. Proc. Natl. Acad. Sci. 2006;103:7100–7105. doi: 10.1073/pnas.0602184103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li S, Min J, Krug RM, Sen GC. Binding of the influenza A virus NS1 protein to PKR mediates the inhibition of its activation by either PACT or double-stranded RNA. Virology. 2006;349:13–21. doi: 10.1016/j.virol.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 40.Gack MU, et al. Influenza A virus NS1 targets the ubiquitin ligase TRIM25 to evade recognition by the host viral RNA sensor RIG-I. Cell Host Microbe. 2009;5:439–449. doi: 10.1016/j.chom.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Das K, Aramini JM, Ma L, Krug RM, Arnold E. Structures of influenza A proteins and insights into antiviral drug targets. Nat. Struct. Mol. Biol. 2010;17:530. doi: 10.1038/nsmb.1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vincent AL, et al. Efficacy of intranasal administration of a truncated NS1 modified live influenza virus vaccine in swine. Vaccine. 2007;25:7999–8009. doi: 10.1016/j.vaccine.2007.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mueller SN, Langley WA, Carnero E, Garcia-Sastre A, Ahmed R. Immunization with live attenuated influenza viruses that express altered NS1 proteins results in potent and protective memory CD8+ T-cell responses. J. Virol. 2010;84:1847–1855. doi: 10.1128/JVI.01317-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kochs G, et al. Strong interferon-inducing capacity of a highly virulent variant of influenza A virus strain PR8 with deletions in the NS1 gene. J. Gen. Virol. 2009;90:2990–2994. doi: 10.1099/vir.0.015727-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coch C, et al. RIG-I activation protects and rescues from lethal influenza virus infection and bacterial superinfection. Mol. Ther. 2017;25:2093–2103. doi: 10.1016/j.ymthe.2017.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ciancanelli MJ, Abel L, Zhang S, Casanova J. Host genetics of severe influenza: From mouse Mx1 to human IRF7. Curr. Opin. Immunol. 2016;38:109–120. doi: 10.1016/j.coi.2015.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Horisberger MA, Staeheli P, Haller O. Interferon induces a unique protein in mouse cells bearing a gene for resistance to influenza virus. Proc. Natl. Acad. Sci. USA. 1983;80:1910–1914. doi: 10.1073/pnas.80.7.1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Staeheli P, Haller O, Boll W, Lindenmann J, Weissmann C. Mx protein: Constitutive expression in 3T3 cells transformed with cloned Mx cDNA confers selective resistance to influenza virus. Cell. 1986;44:147–158. doi: 10.1016/0092-8674(86)90493-9. [DOI] [PubMed] [Google Scholar]
- 49.Horisberger M, Staritzky KD. Expression and stability of the Mx protein in different tissues of mice, in response to interferon inducers or to influenza virus infection. J. Interferon Res. 1989;9:583–590. doi: 10.1089/jir.1989.9.583. [DOI] [PubMed] [Google Scholar]
- 50.Pavlovic J, Haller O, Staeheli P. Human and mouse Mx proteins inhibit different steps of the influenza virus multiplication cycle. J. Virol. 1992;66:2564–2569. doi: 10.1128/jvi.66.4.2564-2569.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Basler CF, Garcia-Sastre A. Viruses and the type I interferon antiviral system: Induction and evasion. Int. Rev. Immunol. 2002;21:305–337. doi: 10.1080/08830180213277. [DOI] [PubMed] [Google Scholar]
- 52.Di Bisceglie AM, et al. Recombinant interferon alfa therapy for chronic hepatitis C. N. Engl. J. Med. 1989;321:1506–1510. doi: 10.1056/NEJM198911303212204. [DOI] [PubMed] [Google Scholar]
- 53.Kao J, Wu N, Chen P, Lai M, Chen D. Hepatitis B genotypes and the response to interferon therapy. J. Hepatol. 2000;33:998–1002. doi: 10.1016/s0168-8278(00)80135-x. [DOI] [PubMed] [Google Scholar]
- 54.Mocellin S, Pasquali S, Rossi CR, Nitti D. Interferon alpha adjuvant therapy in patients with high-risk melanoma: A systematic review and meta-analysis. J. Natl. Cancer Inst. 2010;102:493–501. doi: 10.1093/jnci/djq009. [DOI] [PubMed] [Google Scholar]
- 55.Bohn J, Gastl G, Steurer M. Long-term treatment of hairy cell leukemia with interferon-α: Still a viable therapeutic option. memo-Mag. Eur. Med. Oncol. 2016;9:63–65. doi: 10.1007/s12254-016-0269-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Valentine AD, Meyers CA, Kling MA, Richelson E, Hauser P. Mood and cognitive side effects of interferon-alpha therapy. Semin. Oncol. 1998;25:39–47. [PubMed] [Google Scholar]
- 57.Sleijfer S, Bannink M, Van Gool AR, Kruit WH, Stoter G. Side effects of interferon-α therapy. Pharm. World Sci. 2005;27:423. doi: 10.1007/s11096-005-1319-7. [DOI] [PubMed] [Google Scholar]
- 58.Corssmit E, et al. Endocrine and metabolic effects of interferon-alpha in humans. J. Clin. Endocrinol. Metab. 1996;81:3265–3269. doi: 10.1210/jcem.81.9.8784081. [DOI] [PubMed] [Google Scholar]
- 59.Noisakran S, Campbell IL, Carr DJ. Ectopic expression of DNA encoding IFN-alpha 1 in the cornea protects mice from herpes simplex virus type 1-induced encephalitis. J. Immunol. 1999;162:4184–4190. [PubMed] [Google Scholar]
- 60.Wong JP, et al. Liposome-mediated immunotherapy against respiratory influenza virus infection using double-stranded RNA poly ICLC. Vaccine. 1999;17:1788–1795. doi: 10.1016/s0264-410x(98)00439-3. [DOI] [PubMed] [Google Scholar]
- 61.Protzer U, Nassal M, Chiang PW, Kirschfink M, Schaller H. Interferon gene transfer by a hepatitis B virus vector efficiently suppresses wild-type virus infection. Proc. Natl. Acad. Sci. USA. 1999;96:10818–10823. doi: 10.1073/pnas.96.19.10818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Arnaud P. The interferons: Pharmacology, mechanism of action, tolerance and side effects. Rev. Med. Interne. 2002;23(Suppl 4):449s–458s. doi: 10.1016/s0248-8663(02)00659-8. [DOI] [PubMed] [Google Scholar]
- 63.Pfeffer LM, et al. Biological properties of recombinant alpha-interferons: 40th anniversary of the discovery of interferons. Cancer Res. 1998;58:2489–2499. [PubMed] [Google Scholar]
- 64.Vilcek J. Fifty years of interferon research: Aiming at a moving target. Immunity. 2006;25:343–348. doi: 10.1016/j.immuni.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 65.Oladunni FS, et al. Lethality of SARS-CoV-2 infection in K18 human angiotensin-converting enzyme 2 transgenic mice. Nat. Commun. 2020;11:1–17. doi: 10.1038/s41467-020-19891-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Miorin L, et al. SARS-CoV-2 Orf6 hijacks Nup98 to block STAT nuclear import and antagonize interferon signaling. Proc. Natl. Acad. Sci. USA. 2020;117:28344–28354. doi: 10.1073/pnas.2016650117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Martinez-Gil L, et al. A Sendai virus-derived RNA agonist of RIG-I as a virus vaccine adjuvant. J. Virol. 2013;87:1290–1300. doi: 10.1128/JVI.02338-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang X, et al. Influenza A virus NS1 protein prevents activation of NF-kappaB and induction of alpha/beta interferon. J. Virol. 2000;74:11566–11573. doi: 10.1128/jvi.74.24.11566-11573.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bergmann M, et al. Influenza virus NS1 protein counteracts PKR-mediated inhibition of replication. J. Virol. 2000;74:6203–6206. doi: 10.1128/jvi.74.13.6203-6206.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Talon J, et al. Activation of interferon regulatory factor 3 is inhibited by the influenza A virus NS1 protein. J. Virol. 2000;74:7989–7996. doi: 10.1128/jvi.74.17.7989-7996.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Romanova J, et al. Preclinical evaluation of a replication-deficient intranasal ΔNS1 H5N1 influenza vaccine. PLoS ONE. 2009;4:e5984. doi: 10.1371/journal.pone.0005984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wressnigg N, et al. Development of a live-attenuated influenza B ΔNS1 intranasal vaccine candidate. Vaccine. 2009;27:2851–2857. doi: 10.1016/j.vaccine.2009.02.087. [DOI] [PubMed] [Google Scholar]
- 73.Grimm D, et al. Replication fitness determines high virulence of influenza A virus in mice carrying functional Mx1 resistance gene. Proc. Natl. Acad. Sci. USA. 2007;104:6806–6811. doi: 10.1073/pnas.0701849104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lampson GP, Tytell AA, Field AK, Nemes MM, Hilleman MR. Inducers of interferon and host resistance. I. Double-stranded RNA from extracts of Penicillium funiculosum. Proc. Natl. Acad. Sci. USA. 1967;58:782–789. doi: 10.1073/pnas.58.2.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rathnasinghe R, et al. Comparison of transgenic and adenovirus hACE2 mouse models for SARS-CoV-2 infection. Emerg. Microbes Infect. 2020;9:2433–2445. doi: 10.1080/22221751.2020.1838955. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.