Abstract
Background: Sexual minority women may use contraception for various reasons but face notable barriers to contraceptive care, including stigma and discrimination. However, studies examining sexual orientation disparities in contraceptive care have largely relied on nonprobability samples of predominately White women and may thus not be generalizable to U.S. women overall or Black and Latina women in particular.
Materials and Methods: Using data from the 2006 to 2017 National Survey of Family Growth, a large national probability sample of U.S. women 15–44 years of age (N = 25,473), we used multivariable logistic regression to estimate adjusted odds ratios for receiving a contraceptive method or prescription and contraceptive counseling from a health care provider in the past year among sexual orientation identity and racial/ethnic subgroups of heterosexual, bisexual, and lesbian White, Black, and Latina women relative to White heterosexual women.
Results: Among women overall, 33.9% had received contraception and 18.3% had obtained contraceptive counseling. Black (odds ratio [OR] = 0.73, 95% confidence interval [CI]: 0.65–0.82) and Latina (OR = 0.73, 95% CI: 0.64–0.82) heterosexual women, White (OR = 0.80, 95% CI: 0.65–0.99) and Black (OR = 0.43, 95% CI: 0.32–0.58) bisexual women, and White (OR = 0.23, 95% CI: 0.13–0.43), Black (OR = 0.19, 95% CI: 0.09–0.40), and Latina (OR = 0.08, 95% CI: 0.03–0.22) lesbian women had significantly lower adjusted odds of receiving contraception compared with White heterosexual women. White (OR = 0.36, 95% CI: 0.15–0.85), Black (OR = 0.42, 95% CI: 0.18–0.98), and Latina (OR = 0.22, 95% CI: 0.09–0.53) lesbian women also had significantly lower adjusted odds of obtaining contraceptive counseling relative to White heterosexual women.
Conclusions: Policies, programs, and practices that facilitate access to person-centered contraceptive care among marginalized sexual orientation identity and racial/ethnic subgroups of U.S. women are needed to promote reproductive health equity.
Keywords: contraception, sexual orientation, race/ethnicity, health disparities, intersectionality
Introduction
Sexual minority cisgender women (SMW; i.e., individuals assigned female at birth [AFAB] who identify as women and identify as lesbian, bisexual, or queer, have female sexual partners, and/or have same-sex sexual attractions) may use contraception for various reasons. Indeed, contraception not only prevents pregnancy1 but can also help with the management of menses, acne, menstrual migraine, and polycystic ovarian syndrome.2 Moreover, contraception often provides an entry into other preventive health care, including cervical cancer screening and sexually transmitted infection (STI) testing, for cisgender women.3,4 As a result, contraception can provide reproductive and nonreproductive health benefits to cisgender women and other AFAB individuals, regardless of sexual orientation.
However, although findings are mixed, some studies indicate that SMW may be less likely to receive or use contraception compared with non-SMW (e.g., heterosexual women, women with only male sexual partners).5 For example, Charlton et al. found that lesbian and bisexual women 18–25 years of age were significantly less likely to report using hormonal contraception in the past year compared with their heterosexual counterparts with no same-sex lifetime sexual partners.3 Furthermore, Everett et al. found that women with both male and female sexual partners and women with only female sexual partners had significantly lower adjusted odds of using a long-acting reversible contraceptive compared with women with only male sexual partners.6 In addition, researchers have identified pronounced barriers to contraceptive care among SMW, including sexual orientation-related bias, stigma, and discrimination in health care settings and a lack of health care provider expertise in SMW's health.7,8
Studies examining access to and utilization of contraception among SMW have largely relied on nonprobability samples of predominately White U.S. women and may thus not be generalizable to U.S. women overall or Black and Latina U.S. women in particular.5 Indeed, research shows that pronounced racial/ethnic disparities exist in contraceptive use among U.S. women, with higher levels of contraceptive nonuse occurring among Black and Latina women relative to White women as a result of a lack of access to high-quality information, financial barriers to contraceptive care, contraceptive preferences, and/or medical mistrust rooted in a history of forced and coerced sterilization and medical experimentation, including in the development of the oral contraceptive pill.9–15 However, to our knowledge, no study has ascertained variation in contraceptive use in relation to both sexual orientation and race/ethnicity among U.S. women. Furthermore, no study we know of has assessed how sexual orientation and race/ethnicity simultaneously influence receipt of contraceptive counseling, an important component of contraceptive care during which patients can obtain information and guidance in meeting their contraceptive needs.16
Thus, to address these gaps in the scientific literature, we used intersectionality, an analytic framework rooted in Black feminist theory and praxis that addresses how multiple, intersecting, and mutually constitutive power relations (e.g., racism, sexism, classism, and heterosexism) linked to broader systems of oppression (e.g., white supremacy, capitalism, patriarchy, and colonialism) simultaneously shape the lives of marginalized groups,17,18 to examine disparities in receiving contraception and obtaining contraceptive counseling from a health care provider in the past year in relation to both sexual orientation and race/ethnicity in a large national probability sample of U.S. women. Furthermore, to contribute to intervention development, we also ascertained whether socioeconomic and health care factors may contribute to observed disparities among sexual orientation and racial/ethnic subgroups. Our study will help inform person-centered contraceptive care that is tailored to the unique needs and specific concerns of marginalized sexual orientation and racial/ethnic subgroups of U.S. women, including Black and Latina SMW whose lives and health care experiences are shaped by not only heterosexism but also racism.19
Materials and Methods
Study participants
We analyzed self-reported data from women who participated in the 2006–2010, 2011–2013, 2013–2015, and 2015–2017 waves (i.e., independent, repeated cross-sectional surveys) of the National Survey of Family Growth (NSFG). NSFG uses a complex, multistage sampling design to select a national probability sample of civilian, noninstitutionalized U.S. women.
Although the NSFG refers to participants as women or men, gender identity was not assessed as part of the survey. Indeed, only participants' sex assigned at birth was assessed in a binary manner by the interviewer using information provided by the screener informant during the screener interview only. Those for whom the screener informant responded “female” to the sex assigned at birth question on the screener interview were classified as “women,” and those for whom the informant responded “male” were classified as “men.” Therefore, it is possible that transgender men and nonbinary AFAB people were misclassified as “women” in the NSFG.
In 2006–2010 (n = 12,279; response rate: 78%), 2011–2013 (n = 5,601; response rate: 73.4%), and 2013–2015 (n = 5,699; response rate: 71.2%) only women 15–44 years of age were eligible to participate in the survey. In 2015–2017, participants included women 15–49 years of age (n = 5,554; response rate: 66.7%).20 Given the difference in age eligibility between the 2015–2017 and other NSFG waves, we restricted our analytic sample to women 15–44 years of age at the time of screening (N = 28,470).
Furthermore, women 15–44 years of age who were categorized by the NSFG as “multiracial or another race” (n = 2,546; 9.6%) were excluded from our sample owing to their heterogeneity, which precluded the generation of meaningful estimates and conclusions. In addition, women 15–44 years of age who responded “don't know” (n = 95; 0.31%), “something else” (n = 147; 0.51%), or otherwise did not provide data about their sexual orientation identity (n = 262; 0.60%) were excluded because of their small numbers, which precluded the estimation of reliable statistics in relation to both sexual orientation identity and race/ethnicity. Furthermore, women who did not report whether they had received a contraceptive method (n = 11; 0.02%) or contraceptive counseling (n = 11; 0.02%) in the past 12 months were excluded from our sample. Thus, our final analytic sample included White, Black, and Latina U.S. women 15–44 years of age who self-identified as heterosexual, bisexual, or lesbian (N = 25,473). The present study involved the analysis of publicly available, completely de-identified data and was thus not considered human subjects research.
Measures
Participants self-reported their Hispanic ethnicity followed by their race using one or more listed options. Based on these responses, NSFG staff categorized participants as follows: non-Hispanic White (hereafter, White), non-Hispanic Black (hereafter, Black), Hispanic (hereafter, Latina), or multiracial or another race/ethnicity (not included).
In 2006–2010, 2011–2013, and 2013–2015, sexual orientation identity was assessed using the following question: “Do you think of yourself as: heterosexual or straight; homosexual, gay, or lesbian; or bisexual?” During part of the 2006–2010 survey wave, response options also included “something else.” In 2015–2017, a random half of the sample received the aforementioned version of the sexual orientation identity question (with no “something else” option), whereas the other half was asked: “Which of the following best represents how you think of yourself?” Response options in all survey years included “lesbian or gay” (henceforth, lesbian), “straight, that is, not lesbian or gay” (henceforth, heterosexual), “bisexual,” and “something else” (not included). In all survey waves, participants could also respond “don't know” or refuse to answer to the sexual orientation identity question (not included).
Guided by intersectionality,17,18 we conceptualized race/ethnicity and sexual orientation identity as indicators of racism and heterosexism, respectively—which operate at both the interpersonal and structural level and simultaneously affect women's lives and health in social and historical context.
We examined two dichotomous outcomes of interest: (1) receiving contraception from a health care provider in the last 12 months (yes/no) and (2) receiving contraceptive counseling from a health care provider in the last 12 months (yes/no). Receiving contraception was measured by asking women: “In the past 12 months, have you received a method of birth control or a prescription for a method from a doctor or other medical care provider?” Receiving contraceptive counseling was assessed as follows: “In the past 12 months, have you received counseling or information about birth control from a doctor or other medical care provider?”
Covariates, selected a priori based on the scientific literature and shown along with their categorization in Table 1, included demographic factors (i.e., age, place of residence, nativity, and relationship status), which we conceptualized as potential confounders, and socioeconomic (i.e., educational attainment, household federal poverty level, and employment status) and health care (i.e., health insurance status, Pap test use in last 12 months, and STI test use in last 12 months) factors, which we conceptualized as potential mediators. NSFG staff imputed (using either multiple regression imputation or logical imputation in which NSFG staff examine related variables to assign a value consistent with those other variables20) any missing data for all covariates except for nativity (n = 4, 0.02%), Pap testing (n = 13, 0.05%), and STI testing (n = 49, 0.14%).
Table 1.
Age-Standardized Percent Distribution of Demographic, Socioeconomic, and Health Care Factors Among Sexual Orientation Identity and Racial/Ethnic Subgroups of U.S. Women 15–44 Years of Age (N = 25,473)
| Variable (%) | Total | White heterosexual (n = 12,148; 60.1%) | Black heterosexual (n = 5210; 14.1%) | Latina heterosexual (n = 6039; 19.0%) | White bisexual (n = 915; 3.6%) | Black bisexual (n = 349; 0.7%) | Latina bisexual (n = 338; 0.9%) | White lesbian (n = 237; 0.9%) | Black lesbian (n = 134; 0.3%) | Latina lesbian (n = 103; 0.3%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Age (at time of interview; years) | ||||||||||
| 15–19 | 16.1 | 14.8 | 16.8 | 17.2 | 22.4 | 24.0 | 36.1 | 16.3 | 18.1 | 23.3 |
| 20–29 | 34.2 | 32.8 | 35.3 | 34.6 | 46.1 | 41.7 | 35.6 | 40.5 | 39.9 | 39.1 |
| 30–45a | 49.7 | 52.4 | 47.9 | 48.2 | 31.5 | 34.3 | 28.3 | 43.2 | 42.0 | 37.6 |
| U.S. born: yes | 87.6 | 96.3 | 91.0 | 55.2 | 97.8 | 91.5 | 81.5 | 94.4 | 90.7 | 67.8 |
| Place of residence | ||||||||||
| MSA, central city | 32.9 | 24.9 | 50.8 | 43.0 | 31.0 | 61.0 | 45.1 | 34.7 | 58.4 | 55.6 |
| MSA, other | 49.4 | 52.5 | 37.5 | 49.5 | 48.9 | 34.0 | 44.4 | 51.2 | 33.1 | 39.7 |
| Non-MSA | 17.7 | 22.6 | 11.7 | 7.5 | 20.2 | 5.0 | 10.5 | 14.2 | 8.5 | 4.7 |
| Relationship status | ||||||||||
| Never married | 39.1 | 35.0 | 55.8 | 36.0 | 37.5 | 60.5 | 48.5 | 90.0 | 85.1 | 73.3 |
| Currently married to a male partner | 39.3 | 44.8 | 23.0 | 38.2 | 32.1 | 11.4 | 24.9 | 2.6 | 2.2 | 11.8 |
| Not married but living with a male partner | 12.8 | 12.5 | 10.0 | 16.2 | 16.7 | 13.3 | 15.7 | 1.5 | 3.8 | 0.4 |
| Separated, divorced, or widowed | 8.8 | 7.7 | 11.2 | 9.6 | 13.7 | 14.8 | 10.9 | 5.9 | 9.0 | 14.5 |
| Educational attainment | ||||||||||
| <High school degree | 21.7 | 16.4 | 24.3 | 36.8 | 21.1 | 32.3 | 29.5 | 14.1 | 25.9 | 14.9 |
| High school diploma/GED | 24.1 | 22.1 | 27.9 | 26.2 | 28.4 | 35.4 | 29.4 | 28.4 | 29.0 | 30.5 |
| Some college/associate's degree | 29.0 | 29.7 | 31.2 | 25.3 | 32.1 | 25.8 | 29.2 | 22.2 | 32.0 | 39.4 |
| Bachelor's degree or higher | 25.1 | 31.9 | 16.6 | 11.7 | 18.4 | 6.4 | 11.8 | 35.3 | 13.1 | 15.1 |
| Household federal poverty level (%) | ||||||||||
| <100 | 24.6 | 16.6 | 38.5 | 38.0 | 24.9 | 43.7 | 35.5 | 17.7 | 50.8 | 32.5 |
| 100–199 | 22.3 | 19.6 | 24.8 | 28.9 | 25.2 | 23.7 | 20.5 | 21.0 | 14.5 | 14.2 |
| 200–299 | 17.5 | 18.9 | 15.5 | 14.4 | 19.5 | 16.5 | 15.7 | 18.5 | 19.0 | 25.3 |
| ≥300 | 35.6 | 45.0 | 21.3 | 18.7 | 30.5 | 16.1 | 28.2 | 42.9 | 15.6 | 28.0 |
| Employment status | ||||||||||
| Working for pay | 67.2 | 70.5 | 64.9 | 60.0 | 64.7 | 51.2 | 61.5 | 76.7 | 68.2 | 61.9 |
| Not working for pay | 22.4 | 19.6 | 23.5 | 28.6 | 25.2 | 38.0 | 27.9 | 15.1 | 23.4 | 21.2 |
| Student | 10.4 | 9.8 | 11.6 | 11.4 | 10.1 | 10.8 | 10.7 | 8.2 | 8.4 | 17.0 |
| Health insurance status | ||||||||||
| Private | 61.4 | 72.3 | 48.1 | 41.3 | 49.0 | 37.0 | 48.8 | 65.1 | 45.9 | 50.6 |
| Public | 20.9 | 14.8 | 34.6 | 26.7 | 28.4 | 43.5 | 30.3 | 15.0 | 34.4 | 31.2 |
| Uninsured or underinsuredb | 17.7 | 12.9 | 17.3 | 32.0 | 22.6 | 19.5 | 20.9 | 19.9 | 19.7 | 18.3 |
| Pap test use in last 12 months: yes | 57.9 | 58.0 | 66.0 | 53.0 | 55.7 | 62.9 | 54.7 | 34.2 | 53.9 | 36.1 |
| STI test use in last 12 monthsc: yes | 22.0 | 18.6 | 32.6 | 22.4 | 30.1 | 43.8 | 26.4 | 17.5 | 33.3 | 18.0 |
All prevalence estimates account for the survey's complex sampling design and were directly age-standardized using the 2010 U.S. Census and may not add to 100.0% owing to rounding error.
Women in our analytic sample were 15–44 years of age at the time of screening, but some were 45 years of age at the time of interview.
Underinsured refers to individuals enrolled in a single service plan or Indian Health Service only.
In 2006–2010 and 2011–2013, STI testing was assessed by asking respondents, “In the past 12 months, have you received counseling for or been tested or treated for a sexually transmitted disease?” In 2013–2015 and 2015–2017, respondents were asked, “In the past 12 months, have you been tested for a sexually transmitted disease?”
GED, General Educational Development Test; MSA, metropolitan statistical area; STI, sexually transmitted infection.
Statistical analysis
We first assessed the age-standardized percent distribution of demographic, socioeconomic, and health care factors among U.S. women 15–44 years of age overall and across sexual orientation identity and racial/ethnic subgroups. Distributions were directly age standardized using the 2010 U.S. Census to account for the younger age of lesbian and bisexual women compared to heterosexual women in our analytic sample.21,22 We then ascertained the age-standardized distribution of receiving contraception and obtaining contraceptive counseling from a health care provider in the last 12 months across sexual orientation identity and racial/ethnic subgroups and tested for differences using the adjusted Wald test (α = 0.05).
In addition, we used multivariable logistic regression to assess differences in the odds of receiving contraception and obtaining contraceptive counseling from a health care provider in the past year across sexual orientation identity and racial/ethnic subgroups, first adjusting for demographic factors (Model 1), which we conceptualized as potential confounders, then adding socioeconomic and health care factors (Model 2), which we conceptualized as potential mediators (α = 0.05). All models were also adjusted for survey wave to account for time and the NSFG's complex sampling design (i.e., oversampling, stratification, and clustering) using Stata's svy option. In addition, we used Model 1 to estimate adjusted predicted probabilities of receiving contraception and obtaining contraceptive counseling from a health care provider in the past year and used adjusted Wald tests to assess differences across subgroups (α = 0.05). Stata 16 (College Station, TX) was used to conduct all analyses.
Results
The age-standardized distributions of demographic, socioeconomic, and health care factors among U.S. women 15–44 years of age overall and across sexual orientation identity and racial/ethnic subgroups are shown in Table 1. The distribution of covariates varied widely across sexual orientation identity and racial/ethnic subgroups of U.S. women. However, all subgroups were more likely to be <30 years of age, uninsured or underinsured, and living in a metropolitan statistical area, central city compared to White heterosexual women. In addition, relative to their White heterosexual counterparts, all subgroups were less likely to be currently married to a male partner, have a bachelor's degree or higher (except for White lesbian women), live at or >300% of the Federal Poverty Level, and working for pay (except for White lesbian women; Table 1).
Table 2 shows that, among U.S. women overall, 33.9% had received contraception and 18.3% had obtained contraceptive counseling from a health care provider in the last 12 months. White heterosexual women (37.0%) had the highest, whereas Latina lesbian women (6.2%) had the lowest age-standardized prevalence of receiving contraception from a health care provider in the past year. Moreover, Latina bisexual women (25.2%) had the highest, whereas Latina lesbian women (4.9%) had the lowest age-standardized prevalence of obtaining contraceptive counseling from a health care provider in the past year (Table 2).
Table 2.
Distribution of Receiving a Contraceptive Method or a Prescription for a Method and Receiving Contraceptive Counseling from a Health Care Provider in the Last 12 Months Among Sexual Orientation Identity and Racial/Ethnic Subgroups of U.S. Women 15–44 Years of Age (N = 25,473)
| Subgroup | Received contraception in last 12 months |
Received contraceptive counseling in last 12 months |
||
|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | |
| Total | 8641 | 33.9 (32.9–34.9) | 5039 | 18.3 (17.5–19.1) |
| White heterosexual (reference) | 4560 | 37.0 (35.8–38.4) | 2283 | 17.6 (16.5–18.7) |
| Black heterosexual | 1698 | 30.6 (28.7–32.6) | 1118 | 19.6 (18.1–21.2) |
| Latina heterosexual | 1821 | 29.5 (27.5–31.6) | 1255 | 19.6 (18.0–21.4) |
| White bisexual | 314 | 32.8 (28.4–37.5) | 194 | 20.0 (16.7–23.9) |
| Black bisexual | 96 | 21.1 (16.3–26.9) | 80 | 19.3 (13.7–26.6) |
| Latina bisexual | 99 | 31.2 (21.2–43.5) | 74 | 25.2 (16.8–35.9) |
| White lesbian | 28 | 12.8 (7.6–20.7) | 15 | 6.9 (3.3–14.0) |
| Black lesbian | 18 | 12.0 (6.2–21.7) | 11 | 9.1 (4.1–18.7) |
| Latina lesbian | 7 | 6.2 (2.3–15.6) | 9 | 4.9 (1.9–12.2) |
Prevalence estimates (%) account for the survey's complex sampling design and were directly age-standardized using the 2010 U.S. Census. Values in bold indicate p < 0.05 for comparisons using adjusted Wald tests.
CI, confidence interval.
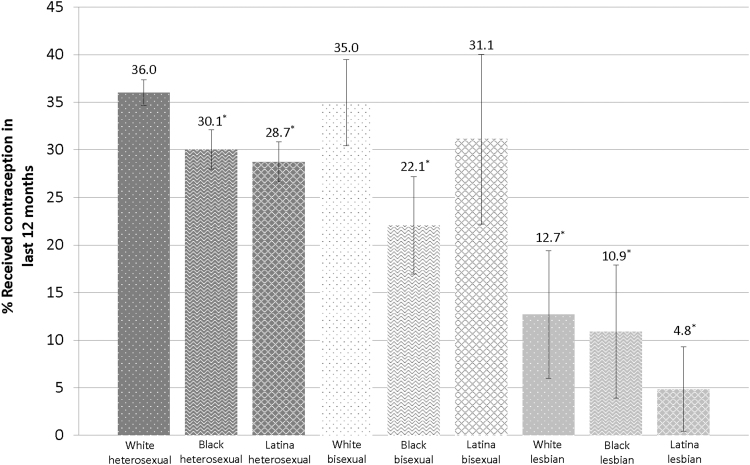
Table 3 indicates that, adjusting for demographic factors, Black (odds ratio [OR] = 0.73, 95% confidence interval [CI]: 0.65–0.82) and Latina (OR = 0.73, 95% CI: 0.64–0.82) heterosexual women, White (OR = 0.80, 95% CI: 0.65–0.99) and Black (OR = 0.43, 95% CI: 0.32–0.58) bisexual women, and White (OR = 0.23, 95% CI: 0.13–0.43), Black (OR = 0.19, 95% CI: 0.09–0.40), and Latina (OR = 0.08, 95% CI: 0.03–0.22) lesbian women had significantly lower odds of receiving contraception from a health care provider in the last 12 months relative to White heterosexual women (Model 1a). Predicted probabilities of receiving contraception from a provider in the past year, adjusting for demographic factors, are shown in Figure 1. Adding socioeconomic and health care factors to Model 1a magnified the observed disparity among Black heterosexual women (OR = 0.62, 95% CI: 0.54–0.71) and Black bisexual women (OR = 0.35; 95% CI: 0.26–0.49) compared to White heterosexual women (Model 2a). In contrast, including these factors in the model partially attenuated the disparity in receiving contraception between Latina and White heterosexual women (OR = 0.84; 95% CI: 0.73–0.96). The disparity among White bisexual women and White, Black, and Latina lesbian women compared with White heterosexual women did not change appreciably upon the addition of socioeconomic and health care factors to the model (Model 2a; Table 3).
Table 3.
Adjusted Odds of Receiving a Contraceptive Method or a Prescription for a Method and Receiving Contraceptive Counseling from a Health Care Provider in the Last 12 Months Among Sexual Orientation Identity and Racial/Ethnic Subgroups of U.S. Women 15–44 Years of Age (N = 25,473)
| |
Received contraception in last 12 months |
Received contraceptive counseling in last 12 months |
||
|---|---|---|---|---|
| Subgroup | Model 1a |
Model 2a |
Model 1b |
Model 2b |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| White heterosexual (reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Black heterosexual | 0.73 (0.65–0.82) | 0.62 (0.54–0.71) | 1.13 (0.99–1.29) | 0.98 (0.85–1.13) |
| Latina heterosexual | 0.73 (0.64–0.82) | 0.84 (0.73–0.96) | 1.01 (0.87–1.17) | 1.09 (0.93–1.27) |
| White bisexual | 0.80 (0.65–0.99) | 0.77 (0.61–0.98) | 1.24 (0.97–1.58) | 1.15 (0.88–1.49) |
| Black bisexual | 0.43 (0.32–0.58) | 0.35 (0.26–0.49) | 1.02 (0.72–1.46) | 0.84 (0.57–1.23) |
| Latina bisexual | 0.72 (0.47–1.10) | 0.88 (0.56–1.39) | 1.22 (0.78–1.90) | 1.40 (0.89–2.21) |
| White lesbian | 0.23 (0.13–0.43) | 0.29 (0.15–0.56) | 0.36 (0.15–0.85) | 0.46 (0.18–1.15) |
| Black lesbian | 0.19 (0.09–0.40) | 0.18 (0.08–0.39) | 0.42 (0.18–0.98) | 0.45 (0.19–1.07) |
| Latina lesbian | 0.08 (0.03–0.22) | 0.10 (0.03–0.28) | 0.22 (0.09–0.53) | 0.28 (0.11–0.68) |
Values in bold refer to ORs with 95% CIs that exclude 1. Model 1 is adjusted for demographic factors (i.e., age, place of residence, nativity, and relationship status) only. Model 2 adds socioeconomic (i.e., educational attainment, household federal poverty level, and employment status) and health care (i.e., health insurance status, Pap test use in last 12 months, STI test use in last 12 months) factors to Model 1. All models are adjusted for survey year and account for the survey's complex sampling design.
Note: Predicted probabilities are derived from the multivariable logistic regression model adjusted for demographic factors (Model 1a, Table 3). *p < 0.05 for comparisons using adjusted Wald tests (reference: White heterosexual).
OR, odds ratio.
FIG. 1.
Adjusted predicted probability of receiving a contraceptive method or a prescription for a method by a health care provider in the last 12 months among sexual orientation identity and racial/ethnic subgroups of U.S. women 15–44 years of age (N = 25,473).
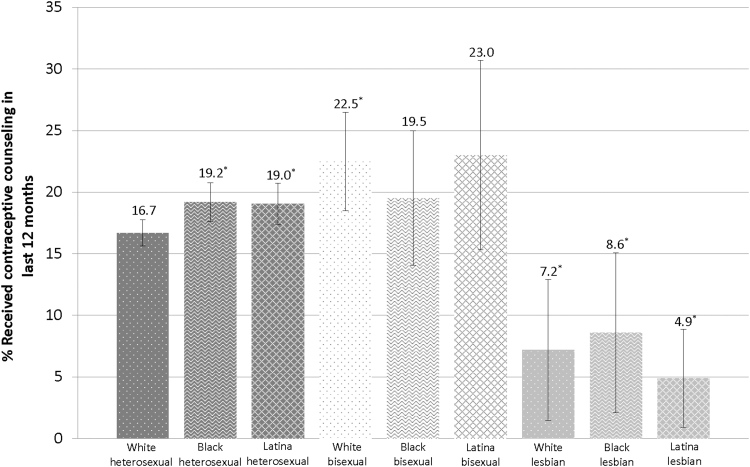
In addition, we found that White (OR = 0.36, 95%: 0.15–0.85), Black (OR = 0.42, 95% CI: 0.18–0.98), and Latina (OR = 0.22, 95% CI: 0.09–0.53) lesbian women had significantly lower adjusted odds of obtaining contraceptive counseling from a health care provider in the last 12 months relative to White heterosexual women (Model 1b; Table 3). Predicted probabilities of receiving contraceptive counseling from a provider in the past year, adjusting for demographic factors, are shown in Figure 2. Adding socioeconomic and health care factors to Model 1b completely attenuated the contraceptive counseling adjusted odds ratios comparing White (OR = 0.46, 95% CI: 0.18–1.15) and Black (OR = 0.45, 95% CI: 0.19–1.07) lesbian women and White heterosexual women (Model 2b). In contrast, the disparity between Latina lesbian and White heterosexual women persisted unchanged (Model 2b; Table 3).
FIG. 2.
Adjusted predicted probability of receiving contraceptive counseling by a health care provider in the last 12 months among sexual orientation identity and racial/ethnic subgroups of U.S. women 15–44 years of age (N = 25,473).
Discussion
Using nationally representative data, we identified previously unanalyzed disparities in receiving a contraceptive method or prescription for a method and obtaining contraceptive counseling from a health care provider in the past year in relation to both sexual orientation and race/ethnicity in a large national probability sample of U.S. women. Our study contributes to the small but growing literature on sexual orientation-related disparities in contraceptive use—which has largely relied on nonprobability samples of predominately White women and not presented findings in relation to race/ethnicity and racism,5 a key social and structural determinant of contraceptive care10—by providing estimates for and making comparisons among sexual orientation identity and racial/ethnic subgroups of U.S. women. Specifically, we found that, adjusting for demographic factors, Black and Latina heterosexual women, White and Black bisexual women, and White, Black, and Latina lesbian women had significantly lower odds of receiving contraception compared with White heterosexual women. Moreover, we also found that White, Black, and Latina lesbian women had significantly lower adjusted odds of obtaining contraceptive counseling relative to their White heterosexual counterparts.
Our analyses suggest that socioeconomic (i.e., educational attainment, household federal poverty level, and employment status) and health care (i.e., health insurance status, Pap test use in the past year, and STI test use in the past year) factors, which we conceptualized as potential mediators, may partially explain disparities in receiving contraception between Latina and White heterosexual women (who were just as likely to have received contraceptive counseling). Indeed, other research shows that socioeconomic23 and health care24 factors influence access to and utilization of contraception. Furthermore, studies indicate that as a result of structural and interpersonal racism,25–28 Latinx people are less likely to have a bachelor's degree, health insurance, and a regular source of care and are more likely to live below the federal poverty threshold and be unemployed compared with White individuals.29–31 In addition, our findings also suggest that socioeconomic and health care factors may completely explain disparities in obtaining contraceptive counseling between White and Black lesbian women and White heterosexual women. Indeed, as a result of structural and interpersonal heterosexism,32,33 lesbian women are less likely than heterosexual women to have access to income, employment, health insurance, and health care,34–36 all of which may influence access to contraceptive counseling by a health care provider.
Socioeconomic and health care factors only partially explained disparities in receiving contraception by a health care provider among Latina and White heterosexual women and did not explain contraception receipt disparities between Black heterosexual women, White and Black bisexual women, and White, Black, and Latina lesbian women relative to White heterosexual women or the disparity in obtaining contraceptive counseling from a health care provider between Latina lesbian women and White heterosexual women—suggesting that other societal factors may underlie these observed disparities. Of note, the disparity in receiving contraception among Latina heterosexual women and Black heterosexual and bisexual women (all of whom were just as likely to obtain contraceptive counseling as White heterosexual women) and Black and Latina lesbian women compared with their White heterosexual women may be due to the history of medical experimentation14,37,38 and forced and coerced sterilization12,15,39–41 as well as experiences of implicit pressure to choose a contraceptive method they may not want11 among Black and Latina women, which may in turn foster mistrust and decrease uptake of contraception provided by a health care provider among many women in these marginalized racial/ethnic groups.42–44
These observed disparities may also result from differences in contraceptive preferences between Black and Latina women, who may prefer nonhormonal contraceptive methods because of concerns about hormonal contraceptives' safety and interference with menstrual periods, and White women.13,45 In addition, the disparity in receiving contraception among White and Black bisexual women, who were just as likely as White heterosexual women to obtain contraceptive counseling, and White, Black, and Latina lesbian women relative to White heterosexual women may also be driven by high levels of condom, emergency contraception, and withdrawal use among bisexual and lesbian women from various racial/ethnic backgrounds.8,46 These patterns of contraceptive method use may be because of bisexual and lesbian women's (or their male sexual partners') contraceptive preferences, lack of access to tailored information about the full range of contraceptive options, mistrust of provider-administered contraceptive methods owing to experiences of heterosexism in the health care system, seeing hormonal contraception, which is often explicitly or implicitly branded as a heterosexual woman's issue, as being in conflict with a lesbian, bisexual, or queer sexual orientation identity, and/or a lack of male sexual partners in the past year.8,46
Lower observed levels of contraceptive counseling by a health care provider may also underlie disparities in receiving contraception between White, Black, and Latina lesbian women and White heterosexual women. Indeed, contraceptive counseling provides an important opportunity for raising lesbian women's awareness and knowledge of contraception, with which they may not be familiar because of the lack of inclusion of lesbians in sexuality education and reproductive health discourse8,47 but may nonetheless be relevant to them to some extent and at some point in their lives given that the vast majority of lesbian women have engaged in sexual activity with a man at some point in their lives.48 In addition, contraceptive counseling can also inform women of the nonreproductive uses of contraception, which are relevant to lesbian women with and without male sexual partners.2
Before discussing the implications of our study for practice and policy, we note several limitations that influence the interpretation of our research findings. First, all data were self-reported and cross-sectional, which may have affected the accuracy of prevalence estimates and precludes us from establishing causality among study variables. Second, neither bisexual nor lesbian women were oversampled in the NSFG; as such, it is possible that some disparities were not detected because of a lack of statistical power. Third, our study did not include measures of many potential mechanisms of observed disparities, including contraceptive preferences, awareness and knowledge of contraception, sex of sexual partners in the past year, pregnancy intentions, experiences of racism and heterosexism in the health care system, and medical mistrust. Future research that uses longitudinal data confirmed using medical records, oversamples lesbian and bisexual women from diverse racial/ethnic backgrounds, and includes data on potential mechanisms is needed. Furthermore, studies that use measures pertaining to the use of specific contraceptive methods, the content and quality of contraceptive counseling, and other dimensions of sexual orientation (e.g., sex of sexual partners in the past 12 months) are also warranted.
Despite these limitations, our research findings have important implications for both practice and policy. Given that socioeconomic and health care factors helped explain some of the observed disparities in receiving contraception (between Latina and White heterosexual women) and contraceptive counseling (between White and Black lesbian and White heterosexual women), policies and programs that promote access to income, education, employment, health insurance, and primary care may help address some contraceptive care disparities at the intersection of sexual orientation race/ethnicity among U.S. women. In addition, initiatives that decrease financial-, insurance-, and health care-related barriers to contraceptive care among women from marginalized sexual orientation and/or racial/ethnic backgrounds—including, making contraception available over the counter49 and at school-based health centers50 and eliminating cost-sharing for contraceptive care51,52—may also help address some of the observed disparities. Furthermore, programs and campaigns that promote trust between women from marginalized sexual orientation and/or racial/ethnic groups and reproductive health care providers, support access to sexuality education and information that is inclusive of lesbian and bisexual women and discusses the full range of contraceptive methods, and brand contraception as congruent with lesbian and bisexual sexual orientation identities may also help address disparities in contraceptive care across sexual orientation and racial/ethnic subgroups of U.S. women.8
Ultimately, all cisgender women and transgender and gender diverse AFAB people should have access to affordable, high-quality contraceptive care that is person-centered and free of discrimination and coercion, regardless of their sexual orientation, race/ethnicity, or other factors. In particular, reproductive health care providers should receive in-depth training on how to engage in contraceptive care and counseling that centers the experiences and preferences of diverse groups of cisgender women and transgender and gender-diverse AFAB people, including those from marginalized sexual orientation and/or racial/ethnic backgrounds, in social and historical context and ensure that all AFAB people have access to the information they need to make informed contraceptive decisions that meet their reproductive and nonreproductive needs.19,53–56 Of note, health care providers should also receive training in taking sexual histories that are inclusive of the diverse sexual experiences of bisexual and lesbian women with male and/or female sexual partners and providing tailored contraceptive care that addresses each person's specific reproductive and nonreproductive concerns as relevant throughout the life course.5,7,57
Health care providers' efforts to provide high-quality, person-centered contraceptive care to cisgender women and transgender and gender diverse AFAB people from marginalized sexual orientation and racial/ethnic backgrounds, including Black and Latina sexual minority cisgender women and transgender and gender diverse AFAB people, must be paired with institutional- and societal-level changes that promote reproductive health equity and reproductive justice, including the right to have children and raise children in healthy environments. Such initiatives should include policies, programs, and practices that address sexual orientation, racial/ethnic, and other forms of bias, stigma, and discrimination in health care organizations in particular and society in general and focus on meeting the reproductive health needs of Black and Latina sexual minority cisgender women and transgender and gender diverse AFAB people and other multiply marginalized groups, in health care, community-based, and policy settings. It is imperative that these efforts equitably involve community members throughout the development, implementation, and leadership process to ensure that they reflect the lived realities and meaningfully address the reproductive health needs, concerns, and preferences of multiply marginalized populations.19,54,55,57,58
Conclusion
Using a large national probability sample of U.S. women, this study provides novel information on disparities in receiving a contraceptive method or prescription and contraceptive counseling from a health care provider in relation to both sexual orientation and race/ethnicity. Of note, we found that several marginalized sexual orientation identity and racial/ethnic subgroups of U.S. women had significantly lower adjusted odds of receiving contraceptive care compared with White heterosexual women. In addition, our analyses suggest that socioeconomic and health care factors may help explain some of these observed disparities. Nonetheless, additional quantitative and qualitative research is needed to elucidate the individual-, interpersonal-, institutional-, community-, and structural-level determinants of contraceptive care disparities among diverse sexual orientation and racial/ethnic subgroups of cisgender women as well as transgender and gender-diverse AFAB people. In the meantime, equitable policies, programs, and practices that expand access to socioeconomic and health care resources, decrease social, economic, and health care barriers to contraceptive and other reproductive health care, and promote person-centered contraceptive care among multiply marginalized groups situated at the intersection of heterosexism, racism, and other forms of oppression are needed to help promote reproductive justice in the United States.19
Acknowledgments
The authors thank the Harvard Sexual Orientation and Gender Identity and Expression (SOGIE) Health Equity Research Collaborative and Alexa Solazzo, PhD for helpful feedback and advice on the analyses presented in this article. The authors also thank the National Center for Health Statistics and National Survey of Family Growth staff and participants for the data used in this study.
Disclaimer
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Disclosure Statement
None of the authors have any conflict of interest.
Funding Information
M.A. is supported by grant 1K01CA234226-01 from the National Cancer Institute. S.B.A. is supported by U.S. Maternal and Child Health Bureau grant T76 MC00001.
References
- 1. World Health Organization. Family planning/contraception methods. Available at: https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception Accessed October 13, 2020.
- 2. Maguire K, Westhoff C. The state of hormonal contraception today: Established and emerging noncontraceptive health benefits. Am J Obstetr Gynecol 2011;205(4, Suppl.):S4–S8. [DOI] [PubMed] [Google Scholar]
- 3. Charlton BM, Corliss HL, Missmer SA, et al. . Influence of hormonal contraceptive use and health beliefs on sexual orientation disparities in papanicolaou test use. Am J Public Health 2013;104:319–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Agénor M, Krieger N, Austin SB, Haneuse S, Gottlieb BR. Sexual orientation disparities in papanicolaou test use among US women: The role of sexual and reproductive health services. Am J Public Health 2014;104:e68–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stoffel C, Carpenter E, Everett B, Higgins J, Haider S. Family planning for sexual minority women. Semin Reprod Med 2017;35:460–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Everett BG, Sanders JN, Myers K, Geist C, Turok DK. One in three: Challenging heteronormative assumptions in family planning health centers. Contraception 2018;98:270–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Greene MZ, Carpenter E, Hendrick CE, Haider S, Everett BG, Higgins JA. Sexual minority women's experiences with sexual identity disclosure in contraceptive care. Obstet Gynecol 2019;133:1012–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Higgins JA, Carpenter E, Everett BG, Greene MZ, Haider S, Hendrick CE. Sexual minority women and contraceptive use: Complex pathways between sexual orientation and health outcomes. Am J Public Health 2019;109:1680–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rocca CH, Harper CC. Do racial and ethnic differences in contraceptive attitudes and knowledge explain disparities in method use? Perspect Sex Repro H 2012;44:150–158. [DOI] [PubMed] [Google Scholar]
- 10. Jackson AV, Wang L-F, Morse J. Racial and ethnic differences in contraception use and obstetric outcomes: A review. Semin Perinatol 2017;41:273–277. [DOI] [PubMed] [Google Scholar]
- 11. Gómez AM, Wapman M. Under (implicit) pressure: Young Black and Latina women's perceptions of contraceptive care. Contraception 2017;96:221–226. [DOI] [PubMed] [Google Scholar]
- 12. Roberts DE. Killing the Black Body: Race, Reproduction, and the Meaning of Liberty. New York, NY: Vintage Books, 1999. [Google Scholar]
- 13. Quinn DA, Sileanu FE, Zhao X, et al. . History of unintended pregnancy and patterns of contraceptive use among racial and ethnic minority women veterans. Am J Obstetr Gynecol 2020;223:564..e1–564.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Briggs L. Reproducing Empire: Race, Sex, Science, and U.S. Imperialism in Puerto Rico. Oakland, CA: University of California Press, 2002. [Google Scholar]
- 15. Gutiérrez ER. Fertile Matters the Politics of Mexican-Origin Women's Reproduction. Austin, TX: University of Texas Press, 2008. [Google Scholar]
- 16. Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: Best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol 2014;57:659–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bowleg L. The problem with the phrase women and minorities: Intersectionality—an important theoretical framework for public health. Am J Public Health 2012;102:1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Combahee River Collective. A Black feminist statement. In Hull GT, Scott PB, Smith B. (eds.): All the Women are White, all the Blacks are Men, but Some of us are Brave: Black Women's Studies. New York, NY: The Feminist Press at the City University of New York, 1982:13–22. [Google Scholar]
- 19. Agénor M. A reproductive justice approach to patient-centered, structurally competent contraceptive care among diverse sexual minority US women. Am J Public Health 2019;109:1626–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. National Center for Health Statistics. 2015–2017 National Survey of Family Growth User's Guide. 2018:50. Published December 2018. Hyattsville, MD: U.S. Department of Health and Human Services. Available at: https://www.cdc.gov/nchs/data/nsfg/NSFG_2015_2017_UserGuide_MainText.pdf. Accessed June 2021.
- 21. U.S. Census Bureau. Summary Population and Housing Characteristics: 2010. The United States Census Bureau. Available at: https://www.census.gov/library/publications/2012/dec/cph-1.html Accessed September 1, 2020.
- 22. Aschengrau A. Essentials of Epidemiology in Public Health, 3rd ed. Burlington, MA: Jones & Bartlett Learning, 2014. [Google Scholar]
- 23. Grindlay K, Grossman D. Prescription birth control access among U.S. women at risk of unintended pregnancy. J Womens Health 2016;25:249–254. [DOI] [PubMed] [Google Scholar]
- 24. Culwell KR, Feinglass J. The association of health insurance with use of prescription contraceptives. Perspect Sex Reprod Health 2007;39:226–230. [DOI] [PubMed] [Google Scholar]
- 25. Williams DR, Lawrence JA, Davis BA. Racism and health: Evidence and needed research. Annu Rev Public Health 2019;40:105–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: Evidence and interventions. Lancet 2017;389:1453–1463. [DOI] [PubMed] [Google Scholar]
- 27. Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: Structural racism, intersectionality theory, and immigrant health. SocSciMed 2012;75:2099–2106. [DOI] [PubMed] [Google Scholar]
- 28. Findling MG, Bleich SN, Casey LS, et al. . Discrimination in the United States: Experiences of Latinos. Health Serv Res 2019;54(S2):1409–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pew Research Center. Demographic trends and economic well-being. Pew Research Center's Social & Demographic Trends Project. Published June 27, 2016. Available at: https://www.pewsocialtrends.org/2016/06/27/1-demographic-trends-and-economic-well-being Accessed September 10, 2020.
- 30. Kaiser Family Foundation. Health and Health Care for Hispanics in the United States. Published May 10, 2019. Available at: https://www.kff.org/infographic/health-and-health-care-for-hispanics-in-the-united-states Accessed October 13, 2020.
- 31. Badgett MVL, Durso LE, Schneebaum A. New Patterns of Poverty in the Lesbian, Gay, and Bisexual Community. 2013. Available at: http://williamsinstitute.law.ucla.edu/wp-content/uploads/LGB-Poverty-Update-Jun-2013.pdf Accessed October 13, 2020.
- 32. NPR, Robert Wood Johnson Foundation, and Harvard T.H. Chan School of Public Health. Discrimination in America: Views and experiences of LGBTQ Americans. November, 2017. Available at: https://cdn1.sph.harvard.edu/wp-content/uploads/sites/94/2017/11/NPR-RWJF-HSPH-Discrimination-LGBTQ-Final-Report.pdf Accessed June 1, 2021.
- 33. Movement Advancement Project. Available at: https://www.lgbtmap.org/equality-maps Accessed November 6, 2020.
- 34. Badgett MVL, Choi SK, Wilson BDM. LGBT poverty in the United States: A study of differences between sexual orientation and gender identity groups. October 2018. Los Angeles, CA: The Williams Institute. Available at: https://williamsinstitute.law.ucla.edu/wp-content/uploads/National-LGBTPoverty-Oct-2019.pdf Accessed September 1, 2020.
- 35. Charlton BM, Gordon AR, Reisner SL, Sarda V, Samnaliev M, Austin SB. Sexual orientation-related disparities in employment, health insurance, healthcare access and health-related quality of life: A cohort study of US male and female adolescents and young adults. BMJ Open 2018;8:e020418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Diamant AL, Wold C, Spritzer K, Gelberg L. Health behaviors, health status, and access to and use of health care: A population-based study of lesbian, bisexual, and heterosexual women. Arch Fam Med 2000;9:1043–1051. [DOI] [PubMed] [Google Scholar]
- 37. Washington HA. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present, 1st ed. New York, NY: Doubleday, 2006. [Google Scholar]
- 38. Owens DC. Medical Bondage: Race, Gender, and the Origins of American Gynecology. Illustrated Edition. Athens, GA: University of Georgia Press, 2017. [Google Scholar]
- 39. Stern AM. Sterilized in the name of public health. Am J Public Health 2005;95:1128–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gutiérrez ER, Fuentes L. Population control by sterilization: The cases of Puerto Rican and Mexican-Origin women in the United States. Latino(a) Res Rev 2009;7:85–100. [Google Scholar]
- 41. Novak NL, Lira N, O'Connor KE, Harlow SD, Kardia SLR, Stern AM. Disproportionate sterilization of Latinos under california's eugenic sterilization program, 1920–1945. Am J Public Health 2018;108:611–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Prather C, Fuller TR, Jeffries WL, et al. . Racism, African American women, and their sexual and reproductive health: A review of historical and contemporary evidence and implications for health equity. Health Equity 2018;2:249–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Prather C, Fuller TR, Marshall KJ, Jeffries WL. The impact of racism on the sexual and reproductive health of African American women. J Womens Health (Larchmont, NY 2002) 2016;25:664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rosenthal L, Lobel M. Gendered racism and the sexual and reproductive health of Black and Latina Women. Ethnicity Health 2020;25:367–392. [DOI] [PubMed] [Google Scholar]
- 45. Jackson AV, Karasek D, Dehlendorf C, Foster DG. Racial and ethnic differences in women's preferences for features of contraceptive methods. Contraception 2016;93:406–411. [DOI] [PubMed] [Google Scholar]
- 46. Tornello SL, Riskind RG, Patterson CJ. Sexual orientation and sexual and reproductive health among adolescent young women in the United States. J Adolescent Health 2014;54:160–168. [DOI] [PubMed] [Google Scholar]
- 47. Power J, McNair R, Carr S. Absent sexual scripts: Lesbian and bisexual women's knowledge, attitudes, and action regarding safer sex and sexual health information. Cult Health Sex 2009;11:67–81. [DOI] [PubMed] [Google Scholar]
- 48. Diamant AL, Schuster MA, McGuigan K, Lever J. Lesbians' sexual history with men: Implications for taking a sexual history. Arch Intern Med 1999;159:2730–2736. [DOI] [PubMed] [Google Scholar]
- 49. Qato DM, Alexander GC, Guadamuz JS, Choi S, Trotzky-Sirr R, Lindau ST. Pharmacist-prescribed and over-the-counter hormonal contraception in Los Angeles County retail pharmacies. Health Affairs 2020;39:1219–1228. [DOI] [PubMed] [Google Scholar]
- 50. Bersamin M, Paschall MJ, Fisher DA. Oregon school-based health centers and sexual and contraceptive behaviors among adolescents. J School Nurs 2018;34:359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Carlin CS, Fertig AR, Dowd BE. Affordable Care Act's mandate eliminating contraceptive cost sharing influenced choices of women with employer coverage. Health Affairs 2016;35:1608–1615. [DOI] [PubMed] [Google Scholar]
- 52. Postlethwaite D, Trussell J, Zoolakis A, Shabear R, Petitti D. A comparison of contraceptive procurement pre- and post-benefit change. Contraception 2007;76:360–365. [DOI] [PubMed] [Google Scholar]
- 53. Levy K, Minnis AM, Lahiff M, Schmittdiel J, Dehlendorf C. Bringing patients' social context into the examination room: An investigation of the discussion of social influence during contraceptive counseling. Womens Health Issues 2015;25:13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Downey MM, Gómez AM. Structural competency and reproductive health. AMA J Ethics 2018;20:211–223. [DOI] [PubMed] [Google Scholar]
- 55. Holt K, Reed R, Crear-Perry J, Scott C, Wulf S, Dehlendorf C. Beyond same-day long-acting reversible contraceptive access: A person-centered framework for advancing high-quality, equitable contraceptive care. Am J Obstetr Gynecol 2019;222:S878..e1–S878.e6. [DOI] [PubMed] [Google Scholar]
- 56. Dehlendorf C, Fox E, Sobel L, Borrero S. Patient-centered contraceptive counseling: Evidence to inform practice. Curr Obstetr Gynecol Rep 2016;5:55–63. [Google Scholar]
- 57. Klein DA, Berry-Bibee EN, Keglovitz Baker K, Malcolm NM, Rollison JM, Frederiksen BN. Providing quality family planning services to LGBTQIA individuals: A systematic review. Contraception 2018;97:378–391. [DOI] [PubMed] [Google Scholar]
- 58. Luna Z, Luker K. Reproductive Justice. Ann Rev Law Soc Sci 2013;9:327–352. [Google Scholar]