Abstract
Introduction
In the race to deploy vaccines to prevent COVID-19, there is a need to understand factors influencing vaccine hesitancy. Secondary risk theory is a useful framework to explain this, accounting for concerns about vaccine efficacy and safety.
Methods
During the first week of July, 2020, participants (N = 216) evaluated one of three different hypothetical vaccine scenarios describing an FDA-approved vaccine becoming available “next week,” “in one year,” or “in two years.” Dependent variables were perceived vaccine efficacy, self-efficacy, perceived vaccine risk, and vaccination willingness. Covariates included vaccine conspiracy beliefs, science pessimism, media dependency, and perceived COVID-19 risk. Data analysis employed multiple analysis of covariance (MANCOVA).
Results
Perceived vaccine efficacy was lowest for the next-week vaccine (η2p = .045). Self-efficacy was higher for the two-year vaccine than the next-week vaccine (η2p = .029). Perceived vaccine risk was higher for the next-week vaccine than for the one-year vaccine (η2p = .032). Vaccination willingness did not differ among experimental treatments. In addition, vaccine conspiracy beliefs were negatively related to perceived vaccine efficacy (η2p = .142), self-efficacy (η2p = .031), and vaccination willingness (η2p = .143) and positively related to perceived vaccine risk (η2p = .216).
Conclusions
The rapid development of the COVID-19 vaccine may have heightened public concerns over efficacy, availability, and safety. However, the current findings showed a general willingness to take even the most rapidly developed vaccine. Nonetheless, there remains a need to communicate publicly and transparently about vaccine efficacy and safety and work to reduce vaccine conspiracy beliefs.
Keywords: Vaccine hesitancy, Secondary risk, Protection motivation, COVID-19 vaccine
1. Introduction
Shortly into the COVID-19 pandemic, scientists began working rapidly to develop a vaccine [15]. In the United States, these efforts were supported by Operation Warp Speed, a public–private partnership coordinating efforts for rapid vaccine development and deployment [53]. An ideal vaccine would evoke a lasting protective immune response while avoiding side effects such as vaccine-enhanced respiratory disease [13], [22]. On 21 July 2020, the United States House Committee on Energy and Commerce [54] held a hearing with representatives of major pharmaceutical companies. The committee heard statements concerning the development of a COVID-19 vaccine, focusing on availability, efficacy, and safety. The hearing addressed the capabilities to produce and distribute an ideal vaccine and challenges related to public vaccine hesitancy. On 11 December 2020, the U.S. Food and Drug Administration (2020) [52] issued emergency use authorization for the Pfizer-BioNTech COVID-19 vaccine and the first doses in the U.S. were administered four days later on 15 December [16]. This was in line with predictions of widespread availability of a vaccine by the end of 2020 or in early 2021 [15], [46]. In April 2021, the U.S. Centers for Disease Control and Prevention [51] reported that more than half of United States adults had received at least one dose and about one-third were fully vaccinated. While those numbers were promising, vaccine hesitancy may have been sapping momentum. On 23 April 2021, the Associated Press reported on waning demand for the vaccine in some parts of the U.S., quoting one individual’s concern over a vaccine “that was rushed in six, seven months” [57].
The current study focuses on the human dimension of vaccine uptake. Despite widespread availability of the COVID-19 vaccine, its effectiveness depends somewhat on public opinion and trust [10]. This echoes the conclusions of a World Health Organization [59] working group on the behavioural and social drivers of vaccination. Such motivation is often described in terms of vaccine hesitancy, which is both an attitudinal and behavioural rejection of vaccines [9]. Larson et al. [27] conducted a systematic review of research on vaccine hesitancy and identified contextual, vaccine-specific, and individual and group factors hindering or promoting vaccination. Among those factors were perceived risks and benefits, vaccine knowledge and awareness, and health-related beliefs and attitudes. Larson et al. [28] drew additional attention to communication and the media environment as sources of anti-vaccination beliefs. More recently, Shapiro et al. [47] developed a vaccine hesitancy scale in the context of parental vaccine decisions. That scale had two dimensions related to a lack of vaccine confidence and perceived risk.
Scholars have examined vaccine hesitancy in the context of a COVID-19 vaccine. Early polls suggested between 20% and 30% of Americans were unwilling to get a COVID-19 vaccine [6], [14]. Their willingness to vaccinate was relatively high compared with some countries, including the United Kingdom, and Russia, and relatively low compared with other countries, including South Korea, Brazil, and China (Lazarus et al., 2020) [30]. Fridman et al. [12] found that political ideology explained a shift in attitudes toward the COVID-19 vaccine over time, remaining relatively stable among Democrats and decreasing among Republicans. They found a similar trend in the perceived threat of COVID-19, where Republicans became more concerned over time. Another study showed vaccination willingness in the United States was related to the perceived severity of and susceptibility to COVID-19 and the perceived safety of the vaccine [49]. Respondents with vaccine hesitancy expressed concerns over the vaccine being too new, having potential side effects, and not being effective. Similarly, Guidry et al. [17] found perceived susceptibility to COVID-19, perceived vaccine efficacy, and vaccination self-efficacy positively predicted vaccine uptake intention. The conclusions of Tyson et al. [50] mirrored these findings, as did a survey of people in several European countries [40]. Most respondents in the latter study expressed a willingness to receive the vaccine, but those who were unwilling or unsure had concerns over safety and side effects. In Ireland and the United Kingdom, vaccine hesitancy was higher among females and youth [38]. That study included several psychometric variables to further characterize vaccine-hesitant individuals as self-interested, distrusting of experts, and impulsive.
Those findings generally align with secondary risk theory, which explains people’s intentions to engage in health-protective behaviours [7]. That model is based on protection motivation theory, which states that people form intentions to engage in a recommended risk response action when they perceive a likely and severe health risk, believe the recommended action will be effective to reduce the risk, and feel able to perform the action [44]. Extending that framework, secondary risk theory also states that people are hesitant to engage in the recommended action when they feel the action itself will expose them to a separate, or secondary, health risk. As the studies above suggest, COVID-19 vaccination hesitancy is related to perceived secondary risks, so secondary risk theory is a helpful framework to understand this human dimension.
The current study uses secondary risk theory as a framework for a simple research question: Does the rapid development of the COVID-19 vaccine make people more hesitant to take it? To answer that question, we conducted a between-subjects experiment in July 2020 in which participants evaluated three different timelines of vaccine availability, including next week, in one year, and in two years. Given the most immediate option, we expect lower perceived vaccine efficacy and vaccination self-efficacy, and higher perception of vaccine-related secondary risk. We also predict there will be lower willingness to take that vaccine or encourage others to take it. In addition to experimental effects, we examine several covariates, including age, sex, education, political orientation, vaccine conspiracy beliefs, science pessimism, and media dependency. Modelling these covariates can address some of the more socio-cultural aspects of vaccination willingness and hesitancy [2].
2. Methods
2.1. Sampling
The Institutional Review Board at Nanyang Technological University, Singapore, approved the study protocol, which included documented informed consent (IRB-2020–06-003). We opted to use a United States sample in anticipation of large variance in vaccine hesitancy against the backdrop of a presidential race that had politicized the issue [18], affecting public perceptions [39]. Indeed, recent work has linked perceptions of COVID-19 and vaccine hesitancy with political orientation [4], [11], [12], [50]. Admittedly, this phenomenon is not unique to the United States, but it is pronounced there.
The current study used an online research panel from Dynata, a panel provider commonly used in the social sciences. Their United States panel has more than 28 million members. Dynata sent invitations to 1792 individuals between July 1 and July 7, 2020. There were sampling quotas for age and sex. The age quota divided the sample into those aged 18–30 (30%), 31–50 (40%) and 51–80 (30%). The sex quota evenly split the sample between men and women with an allowance of ±5%. Of those invited, 216 completed an anonymous online survey, with a median completion time of 419 s. This was after removing 24 individuals who completed the study in under 150 s, which seemed too quick to have participated attentively.
2.2. Treatment
Each participant evaluated one of three vaccine scenarios, presented at random. The three scenarios concerned a hypothetical FDA-approved vaccine becoming available “next week,” “in one year,” or “in two years.” At the time of data collection, an approved vaccine was more than five months away, so it was possible for respondents to imagine one becoming available at the different time intervals. Had a vaccine already been approved, then it would not have been possible to test responses to these scenarios. The treatment involved a simple text-based manipulation. Prior to answering the dependent measures, participants saw the following text:
“Imagine the first FDA-approved COVID-19 vaccine became available [next week OR in one year OR in two years]. Please indicate how much you agree or disagree with the following statements.”
2.3. Measurement
We measured all items using five-point Likert scales from 1 (strongly disagree) to 5 (strongly agree), computed composite measures as item mean scores, and determined acceptable composite reliability as Cronbach’s alpha estimates of 0.70 and higher. Prior to creating composite measures, we assessed dimensionality using factor analysis in IBM SPSS Statistics 25 (hereafter, SPSS) with maximum likelihood estimation and oblique factor rotation. We retained items with strong loadings (λ > 0.70) on a single factor and weak loadings (λ < 0.40) on all other factors. Such item retention exhibits what many scholars call simple structure, which means that each item strongly indicates a single factor and does not have large residual variance associated with any other factor [60]. Table 1 contains the item wording and descriptive statistics. See Table 2 for a summary of the measured variables and their intercorrelations. Table S1 in the supplementary material shows the percent of respondents indicating each response option.
Table 1.
Measurement items wording and descriptive statistics.
| Scale/Item | M | SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Vaccine efficacy | ||||
| The vaccine would work to prevent infection by the virus. | 3.67 | 1.06 | −0.64 | 0.21 |
| If I got the vaccine, I would be less likely to get the virus. | 3.69 | 1.11 | −0.71 | 0.04 |
| Taking the vaccine would be an effective way of reducing the risk of infection. | 3.78 | 1.13 | −0.77 | −0.02 |
| Self-efficacy | ||||
| I would be able to get the vaccine if I wanted. | 3.66 | 0.95 | −0.36 | −0.03 |
| The vaccine would be easy for me to get. | 3.41 | 0.96 | −0.25 | −0.09 |
| It would be difficult for me to get vaccinated. (reverse-coded) | 3.54 | 1.09 | −0.28 | −0.62 |
| Vaccine risk | ||||
| If I received the vaccine, I would be at risk of getting side effects. | 3.22 | 1.00 | −0.34 | −0.05 |
| If I received the vaccine, my chance of getting side effects would be high. | 2.80 | 1.03 | 0.02 | −0.07 |
| If I received the vaccine, I would be more likely than other people of getting side effects. | 2.69 | 1.03 | −0.14 | −0.52 |
| The vaccine would cause serious illness. | 2.50 | 1.10 | 0.31 | −0.35 |
| Health effects of the vaccine would be severe. | 2.62 | 1.12 | 0.23 | −0.48 |
| Effects of the vaccine would affect my usual activities. | 2.73 | 1.01 | 0.06 | −0.13 |
| The vaccine would have considerable negative consequences. | 2.64 | 1.10 | 0.14 | −0.51 |
| Vaccination willingness | ||||
| I would be willing to take the vaccine. | 3.68 | 1.30 | −0.65 | −0.69 |
| I would avoid taking the vaccine. (reverse-coded) | 3.69 | 1.38 | −0.61 | −0.94 |
| I would encourage others to take the vaccine. | 3.52 | 1.25 | −0.46 | −0.64 |
| Scale/Item | M | SD | Skewness | Kurtosis |
| Vaccine conspiracy beliefs | ||||
| Vaccine safety data is often fabricated. | 2.42 | 1.25 | 0.51 | −0.72 |
| Immunizing children is harmful and this fact is covered up. | 2.05 | 1.23 | 0.89 | −0.31 |
| Pharmaceutical companies cover up the dangers of vaccines. | 2.67 | 1.31 | 0.21 | −1.01 |
| People are deceived about the effectiveness of vaccines. | 2.44 | 1.31 | 0.51 | −0.84 |
| Data on the effectiveness of vaccines is often fabricated. | 2.45 | 1.28 | 0.43 | −0.85 |
| People are deceived about vaccine safety. | 2.49 | 1.29 | 0.44 | −0.84 |
| The government is trying to cover up the link between vaccines and autism. | 2.24 | 1.23 | 0.53 | −0.75 |
| Science pessimism | ||||
| The world would be better without today’s technology. | 2.16 | 1.19 | 0.67 | −0.60 |
| Our leaders need to stop funding science research. | 1.95 | 1.17 | 1.06 | 0.14 |
| Science has created more problems in society than solutions. | 2.18 | 1.19 | 0.67 | −0.48 |
| Scientists purposefully hide the truth from the public. | 2.37 | 1.21 | 0.45 | −0.87 |
| Scientists don’t value my concerns when making decisions. | 2.51 | 1.19 | 0.34 | −0.77 |
| Scientists exaggerate the truth for their own personal gain. | 2.50 | 1.23 | 0.27 | −1.05 |
| Media dependency | ||||
| Information in the mainstream media helps me find out about COVID-19. | 3.70 | 1.05 | −0.80 | 0.23 |
| Information in the mainstream media helps me observe how others deal with COVID-19. | 3.57 | 1.05 | −0.67 | 0.14 |
| Information in the mainstream media gives me ideas about how to discuss the issue of COVID-19 with others. | 3.37 | 1.12 | −0.57 | −0.31 |
| Information in the mainstream media helps me figure out how I can deal with COVID-19. | 3.51 | 1.13 | −0.70 | −0.10 |
| Scale/Item | M | SD | Skewness | Kurtosis |
| COVID-19 susceptibility | ||||
| I am at risk of getting the virus. | 3.43 | 1.16 | −0.50 | −0.47 |
| My chance of getting the virus is high. | 2.99 | 1.10 | 0.02 | −0.51 |
| I am more likely than other people to get the virus. | 2.65 | 1.14 | 0.11 | −0.70 |
| COVID-19 severity | ||||
| The virus causes serious illness. | 4.19 | 0.98 | −1.14 | 0.83 |
| Health effects of the virus are severe. | 4.00 | 1.02 | −0.87 | 0.33 |
| Effects of the virus would affect my usual activities. | 3.98 | 1.07 | −1.00 | 0.56 |
| The virus has considerable negative consequences. | 4.08 | 1.06 | −1.19 | 1.02 |
Table 2.
Correlation/Covariance Matrix and Descriptive Statistics of the Measured Variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Vaccine conspiracy belief | 1.24 | 0.71 | −0.25 | −0.14 | −0.28 | −0.64 | −0.32 | 0.60 | −0.80 |
| 2. Science pessimism | 0.64 | 1.00 | −0.40 | −0.16 | −0.32 | −0.57 | −0.28 | 0.44 | −0.68 |
| 3. Media dependency | −0.24 | −0.42 | 0.92 | 0.32 | 0.35 | 0.44 | 0.16 | −0.19 | 0.50 |
| 4. COVID-19 susceptibility | −0.13 | −0.17 | 0.34 | 0.94 | 0.43 | 0.34 | 0.08 | 0.02 | 0.32 |
| 5. COVID-19 severity | −0.29 | −0.37 | 0.42 | 0.51 | 0.74 | 0.42 | 0.19 | −0.16 | 0.41 |
| 6. Vaccine efficacy | −0.58 | −0.57 | 0.47 | 0.36 | 0.49 | 0.99 | 0.31 | −0.50 | 0.91 |
| 7. Self-efficacy | −0.36 | −0.35 | 0.21 | 0.10 | 0.28 | 0.39 | 0.65 | −0.25 | 0.39 |
| 8. Vaccine risk | 0.63 | 0.52 | −0.23 | 0.03 | −0.22 | −0.58 | −0.36 | 0.74 | −0.61 |
| 9. Vaccination willingness | −0.59 | −0.56 | 0.43 | 0.27 | 0.39 | 0.75 | 0.39 | −0.59 | 1.49 |
| M | 2.39 | 2.28 | 3.54 | 3.02 | 4.06 | 3.71 | 3.54 | 2.74 | 3.63 |
| SD | 1.11 | 1.00 | 0.96 | 0.97 | 0.86 | 0.99 | 0.80 | 0.86 | 1.22 |
| t(215) | −8.02 | −10.61 | 8.26 | 0.35 ns | 18.07 | 10.53 | 9.79 | −4.41 | 7.55 |
Note. The diagonal (in bold typeface for ease of reference) shows variances. Numbers above the diagonal are covariances and numbers below the diagonal are correlations. Correlations with magnitudes of 0.13 and larger are significant (p < .05, two-tailed). M = unadjusted mean. SD = standard deviation of the mean. t(215) is the one-sample t-value with 215 degrees of freedom. The one-sample t-test compares mean scores against a test value of 3, which was the middle response option on the measurement items. ns = not significant. All other t-values are significant at p < .001 (two-tailed).
We measured efficacy beliefs using six items from prior research [7]. Three items measured vaccine efficacy, for example, “The vaccine would work to prevent infection by the virus” (Cronbach’s α = 0.89). Another three items measured self-efficacy, for example, “The vaccine would be easy for me to get” (Cronbach’s α = 0.72).
Consistent with secondary risk theory [7], we measured secondary risk susceptibility and severity. However, factor analysis suggested the items measured a single construct. Thus, seven items measured perceived vaccine risk. Examples of these items are, “If I received the vaccine, I would be at risk of getting side effects” and “The vaccine would cause serious illness” (Cronbach’s α = 0.91).
Three items measured willingness to take and encourage others to take the vaccine: “I would be willing to take the vaccine,” “I would avoid taking the vaccine” (reverse-coded), and “I would encourage others to take the vaccine” (Cronbach’s α = 0.92).
Prior to the experimental manipulation, participants responded to items measuring several covariates, including vaccine conspiracy beliefs, science pessimism, media dependency, and perceived COVID-19 risk. We measured vaccine conspiracy beliefs using the seven-item Vaccine Conspiracy Beliefs Scale, which researchers developed to explain vaccine hesitancy [47]. An example of these items is, “Immunizing children is harmful and this fact is covered up” (Cronbach’s α = 0.95). We measured science pessimism using six items from the Science and Technology Beliefs Scale, which has been validated by a work in progress. An example of these items is, “Our leaders need to stop funding science research” (Cronbach’s α = 0.91). We adapted four items from prior research on media dependency [21]. One study showed a positive relationship between social media dependency and H1N1 vaccination intention [32]. An example of these items is, “Information in the mainstream media helps me find out about COVID-19” (Cronbach’s α = 0.90). Finally, we measured perceived COVID-19 risk using seven items from prior research [7]. Three items measured perceived susceptibility, for example “I am at risk of getting the virus” (Cronbach’s α = 0.81). Another four items measured perceived severity, for example “The virus causes serious illness” (Cronbach’s α = 0.86).
2.4. Statistical analyses
We used multiple analysis of covariance (MANCOVA) in SPSS to estimate treatment effects on the dependent variables, controlling for vaccine conspiracy beliefs, science pessimism, media dependency, and perceived COVID-19 risk. Consistent with secondary risk theory, we modelled perceived COVID-19 risk as the conditional main effect of perceived susceptibility plus the conditional main effect of perceived severity plus the product term of perceived susceptibility and severity [7]. The model had initially included age, sex, education, political orientation, and estimated time to vaccine availability as covariates, but their effects were non-significant and we excluded them from the final analysis.
3. Results
3.1. Sample characteristics
The sample was 55% female and had a mean age of 45.67 (SD = 17.70). Participants identified their race as White (76%), Black or African American (11%), American Indian or Alaskan Native (<1%), Asian (9%), Native Hawaiian or Pacific Islander (1%), and Other (2%). Most participants (96%) identified as non-Hispanic. The median educational attainment was “Associate’s degree” and the mode was “Bachelor’s degree.” Participants indicated their political orientation as “extremely liberal” (6%), “very liberal” (9%), “somewhat liberal” (17%), “neither liberal nor conservative” (31%), “somewhat conservative” (17%), “very conservative” (12%), and “extremely conservative” (9%). The median and mode were both “Neither liberal nor conservative” and responses were normally distributed (M = 4.15, SD = 1.57). The normal distribution suggests we had good coverage of the political spectrum, despite not using quotas for political orientation.
We also asked participants roughly how long they think it will be until an FDA-approved vaccine becomes available. Responses were “One already exists” (1%), “One month or less” (1%), “More than one month and up to six months” (15%), “More than six months and up to a year” (43%), “More than a year and up to two years” (31%), “More than two years and up to three years” (3%), “More than three years” (2%), and “Never” (4%).
3.2. Sample and cell means
We begin the main analysis with some descriptive statistics. Table 3 shows marginal means, 95% confidence intervals of the means, and standard deviations of the means for each treatment group and the overall sample. It also shows one-sample t-tests comparing mean scores against a value of 3, which was the middle response option on the measurement items. Scores significantly above 3 indicate agreement with the measurement items, while those significantly below 3 indicate disagreement. Those t-tests show participants consistently reported high levels of perceived vaccine efficacy, self-efficacy, and vaccination willingness across the treatments, and generally low perceived vaccine risk. The only non-significant difference was for perceived vaccine risk in the next-week condition. In that condition, participants were in neither agreement nor disagreement about the likelihood and severity of side effects.
Table 3.
Marginal Means of Dependent Variables by Treatment.
| Vaccine Efficacy |
Self-Efficacy |
Vaccine Risk |
Vaccination Willingness |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment | n | M [95% CI] | SD | t(n–1) | M [95% CI] | SD | t(n–1) | M [95% CI] | SD | t(n–1) | M [95% CI] | SD | t(n–1) |
| Next week | 74 | 3.57 [3.42, 3.73] | 0.70 | 7.09 | 3.37 [3.20, 3.54] | 0.75 | 4.23 | 2.86 [2.70, 3.01] | 0.66 | −1.86 ns | 3.51 [3.30, 3.73] | 0.94 | 4.71 |
| One year | 68 | 3.92 [3.75, 4.09] | 0.71 | 10.71 | 3.43 [3.25, 3.62] | 0.77 | 4.67 | 2.58 [2.41, 2.74] | 0.67 | −5.18 | 3.70 [3.48, 3.93] | 0.95 | 6.10 |
| Two years | 74 | 3.80 [3.65, 3.96] | 0.69 | 10.08 | 3.66 [3.49, 3.83] | 0.74 | 7.63 | 2.68 [2.53, 2.83] | 0.65 | −4.26 | 3.70 [3.49, 3.91] | 0.92 | 6.52 |
| Overall | 216 | 3.76 [3.66, 3.86] | 0.75 | 14.90 | 3.49 [3.39, 3.60] | 0.80 | 9.01 | 2.71 [2.61, 2.80] | 0.71 | −6.04 | 3.64 [3.50, 3.77] | 0.99 | 9.46 |
Note. M = marginal mean controlling for covariates. SD = standard deviation of the mean. t(n–1) is the one-sample t-value with n-1 degrees of freedom. The one-sample t-test compares mean scores against a test value of 3, which was the middle response option on the measurement items. ns = not significant. All other t-values are significant at p < .001 (two-tailed).
3.3. Treatment effects
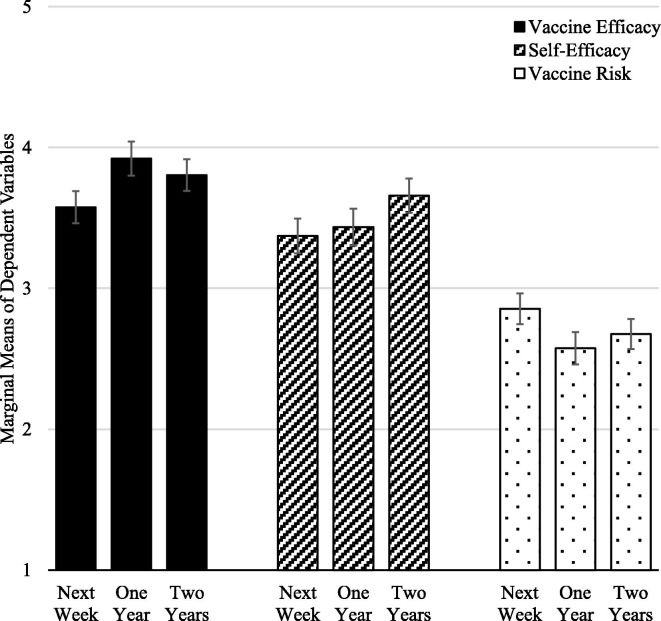
Next, we present the effects of the experimental treatment of the four dependent variables—perceived vaccine efficacy, self-efficacy, perceived vaccine risk, and vaccination willingness. These analyses pertain to our stated predictions. The multivariate tests for the treatment effect (p = .020, η2 p = .043) and covariate effects (all p < .05) were significant. Below we report the univariate tests, focusing on the treatment effects but also noting significant effects of covariates. Table 4 contains the unstandardized parameter estimates of pair-wise treatment effects and covariates. The parameter estimates for the between-treatment comparisons (e.g., “Next week vs. two years”) indicate the differences in mean scores between groups. Fig. 1 shows cell means with 84% confidence intervals, which allows for a visual comparison of mean differences roughly equivalent to p = .05 [42]. Put another way, visibly non-overlapping confidence intervals are significant at approximately p < .05.
Table 4.
Parameter Estimates from MANCOVA.
| Vaccine Efficacy R2 = 0.561 |
Self-Efficacy R2 = 0.218 |
Vaccine Risk R2 = 0.468 |
Vaccination Willingness R2 = 0.476 |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | B | SE | p | η2p | B | SE | p | η2p | B | SE | p | η2p | B | SE | p | η2p |
| Intercept | 4.09 | 0.29 | 0.000 | 0.499 | 3.71 | 0.30 | 0.000 | 0.411 | 1.77 | 0.27 | 0.000 | 0.170 | 4.15 | 0.38 | 0.000 | 0.362 |
| Next week vs. one year | −0.35 | 0.11 | 0.003 | 0.043 | −0.06 | 0.12 | 0.610 | 0.001 | 0.28 | 0.11 | 0.010 | 0.031 | −0.19 | 0.15 | 0.212 | 0.008 |
| Next week vs. two years | −0.23 | 0.11 | 0.041 | 0.020 | −0.29 | 0.12 | 0.018 | 0.027 | 0.18 | 0.11 | 0.092 | 0.014 | −0.18 | 0.15 | 0.217 | 0.007 |
| Vaccine conspiracy belief | −0.32 | 0.05 | 0.000 | 0.142 | −0.15 | 0.06 | 0.011 | 0.031 | 0.39 | 0.05 | 0.000 | 0.216 | −0.43 | 0.07 | 0.000 | 0.143 |
| Science pessimism | −0.19 | 0.06 | 0.004 | 0.039 | −0.10 | 0.07 | 0.152 | 0.010 | 0.15 | 0.06 | 0.016 | 0.028 | −0.22 | 0.09 | 0.012 | 0.030 |
| Media dependency | 0.19 | 0.06 | 0.001 | 0.049 | 0.07 | 0.06 | 0.255 | 0.006 | −0.05 | 0.05 | 0.330 | 0.005 | 0.25 | 0.08 | 0.001 | 0.049 |
| COVID-19 susceptibility | 0.15 | 0.06 | 0.006 | 0.036 | −0.06 | 0.06 | 0.322 | 0.005 | 0.14 | 0.05 | 0.009 | 0.033 | 0.10 | 0.07 | 0.170 | 0.009 |
| COVID-19 severity | 0.12 | 0.06 | 0.056 | 0.017 | 0.19 | 0.07 | 0.006 | 0.036 | −0.06 | 0.06 | 0.621 | 0.001 | 0.10 | 0.08 | 0.220 | 0.007 |
| Susceptibility × severity | −0.10 | 0.04 | 0.016 | 0.028 | 0.92 | 0.05 | 0.038 | 0.021 | 0.07 | 0.04 | 0.075 | 0.015 | −0.02 | 0.06 | 0.742 | 0.001 |
Note. The treatment is coded in two dummy variables with the next-week option as the reference category. R2 = explained variance. B = unstandardized parameter estimates. SE = standard error of the parameter estimate. p = two-tailed p-value. η2p = effect size, partial eta squared.
Fig. 1.
Marginal means of dependent variables showing treatment effects on perceived vaccine efficacy (black bars), self-efficacy (hashed bars), and perceived vaccine risk (dotted bars). All variables were on a scale of 1 to 5, where higher scores indicated higher levels of the measured concepts. Error bars show 84% confidence intervals for visual comparisons of mean differences at approximately p = .05.
First, perceived vaccine efficacy was different among the conditions, F(2,207) = 4.84, p = .009, η2 p = .045. It was lower for the next-week vaccine (M = 3.57, SD = 0.70) than the one-year vaccine (M = 3.92, SD = 0.71; p = .003) and two-year vaccine (M = 3.80, SD = 0.69; p = .041). This is consistent with our prediction. Further, perceived vaccine efficacy was negatively related to vaccine conspiracy beliefs and science pessimism and positively related to media dependency and perceived COVID-19 susceptibility. Also, the interaction of perceived COVID-19 susceptibility and severity was significant and negative. This interaction is not a key finding, but some readers may find it interesting, so we have included the Johnson-Neyman plot in the supplementary material (Figure S1).
Second, self-efficacy was different among the conditions, F(2,207) = 3.11, p = .047, η2 p = .029. It was lower for the next-week vaccine (M = 3.37, SD = 0.75) than the two-year vaccine (M = 3.66, SD = 0.74; p = .018), but not lower than the one-year vaccine (M = 3.43, SD = 0.77; p = .610). This is partly consistent with our prediction. Further, self-efficacy was negatively related to vaccine conspiracy beliefs and positively related to COVID-19 severity. Also, the interaction of perceived COVID-19 susceptibility and severity was significant and positive. Like the previous interaction, this not a key finding, but we have included the Johnson-Neyman plot in the supplementary material (Figure S2).
Third, perceived vaccine risk was different among the conditions, F(2,207) = 3.47, p = .033, η2 p = .032. It was higher for the next-week vaccine (M = 2.86, SD = 0.66) than the one-year vaccine (M = 2.58, SD = 0.67; p = .010), but not than the two-year vaccine (M = 2.68, SD = 0.65; p = .092). This is partly consistent with our prediction. Further, perceived vaccine risk was positively related to vaccine conspiracy beliefs, science pessimism, and perceived COVID-19 susceptibility.
Fourth, vaccination willingness did not differ among the next-week vaccine (M = 3.51, SD = 0.94), one-year vaccine (M = 3.70, SD = 0.95), and two-year vaccine (M = 3.70, SD = 0.92), F(2,207) = 1.04, p = .35. This is inconsistent with our prediction. Finally, vaccination willingness was negatively related to vaccine conspiracy beliefs and science pessimism and positively related to media dependency.
3.4. Post hoc analyses of age, sex, and political orientation
It is worth addressing the null findings regarding age, sex, education, and political orientation. None of them was a significant predictor of any dependent measure, which seems to diverge from prior research. The null findings may be due to the presence of covariates, which we can assess by conducting bivariate analyses, first with the dependent variables. Age was positively correlated with response efficacy (r = 0.18, p = .007) and vaccination willingness (r = 0.17, p = .012), and vaccination willingness was higher for males (M = 3.88, SD = 1.20) than for females (M = 3.42, SD = 1.20), F(1,214) = 11.51, p = .005. Those findings regarding age are consistent with Murphy et al. [38], who found vaccine hesitancy was higher among younger individuals and females. Among the dependent measures, education correlated only with self-efficacy (r = 0.15, p = .023). Political orientation had significant correlations with response efficacy (r = −0.19, p = .005) and vaccination willingness (r = −0.18, p = .007). Those correlations suggest the more conservative people are, the less effective they think a vaccine will be and the less willing they are to take it, which is consistent with Fridman et al. [12]. Next, we examined bivariate correlations with other covariates. The first analysis showed age was negatively related to vaccine conspiracy beliefs (r = −0.25, p < .001) and science pessimism (r = −0.16, p = .017), suggesting younger people are more likely to hold conspiracy beliefs and be pessimistic about science. Similarly, education was negatively related to vaccine conspiracy beliefs (r = −0.18, p = .005) and science pessimism (r = −0.19, p = .005), which is intuitive. Finally, political orientation also had significant correlations with science pessimism (r = 0.26, p < .001) and media dependency (r = −0.27, p < .001), suggesting the more conservative people are, the more pessimistic they are about science and the less they depend on media for information about COVID-19. Our full model controlled for vaccine conspiracy beliefs, science pessimism, and media dependency, which may explain why the effects of age, education, and political orientation on the dependent variables were non-significant.
4. Discussion
This discussion highlights five results. First, perceived COVID-19 risk was related to both perceived vaccine efficacy and self-efficacy. Although this is not a tenet of secondary risk theory, it is partly consistent with the extended parallel process model [58], a closely related framework. That model suggests fearful responses to perceived health threats can inhibit efficacy beliefs, reducing both the perceived effectiveness of a risk response action and the self-efficacy to perform it. This is called fear control. In contrast, when individuals have low or moderate levels of fear, they are more likely engage in activities aimed at reducing the threat directly, which is called danger control. Lithopoulos et al. [33] used this model to understand physical distancing in the context of COVID-19. They found individuals who perceived high threat and coping ability exhibited lower fear control and were more likely to practice physical distancing. In line with these and other findings, scholars often recommend that risk communicators avoid strong fear appeals and emphasize the effectiveness and ease of performing the recommended behaviour. Yet, it may be necessary to use targeted fear appeals to reach groups of people who underestimate their susceptibility to COVID-19 [5]. An important addition in contexts like COVID-19 is to highlight the safety of the recommended behaviour [40], [46]. This can allay concerns about secondary risks, which might otherwise be an extra source of fear. On that point, Wentzell and Racila [56] interviewed participants in the Pfizer-BioNTech clinical trial, who described their efforts to normalize vaccination by sharing their experiences, particularly with respect to the mildness or absence of side-effects. This highlights a special role of interpersonal communication about the COVID-19 vaccine that the current attention to media dependency fails to capture.
Second, there is an intuitive conflict between rapid vaccine development and ensuring safety [24]. Some recent qualitative findings attest to that idea and provide some triangulation of the current findings. Momplaisir et al. [36] conducted focus groups with Black Americans to understand their thoughts about the COVID-19 vaccine. Discussants expressed concerns about the speed of development, citing the usual multi-year timeline of vaccine trials. They were specifically concerned about potential side effects and too little testing. Latkin et al. [29] reported data from a survey about trust in the vaccine. Those who expressed distrust answered an open-ended question to explain their distrust. The most common theme, which appeared in nearly one-third of the comments, was concern over the vaccine being too new. Even Canadians expressed concerns over the rapid pace of vaccine development in the U.S., which Benham et al. [3] reported from focus groups with Alberta residents. One discussant expressed concern about how “the US is sidestepping their normal routines and their normal safety reviews to push through a new vaccine.” Those qualitative findings are consistent with the current quantitative findings that participants reported relatively low vaccine efficacy and high perceived risk for the next-week vaccine.
Third, despite the significant treatment effects, perceived vaccine efficacy and self-efficacy were generally high and perceived vaccine risk was generally low. This means the quickness of producing a vaccine did not incline participants away from the vaccine, but rather lessened their inclination toward it. Participants had an overall favourable impression of the vaccine, even for the next-week option. It is worth noting most participants (83%) expected a vaccine to become available after at least six months, and nearly all (98%) expected at least a one-month wait. This suggests the one-week option represented a sooner-than-expected vaccine to nearly all participants. Even so, the participants expressed a willingness to take the vaccine and encourage others to take it. This suggests that for many Americans, rapid vaccine development alone has not been a deterrent to them getting vaccinated. But that may apply only to individuals who had always planned to receive the vaccine.
Fourth, of all the model predictors, vaccine conspiracy beliefs had the largest effect on perceived vaccine efficacy, perceived vaccine risk, and vaccination willingness. This is consistent with other research using vaccine conspiracy beliefs to explain vaccination willingness and hesitancy [25], [47], [48]. Such beliefs may largely define the thoughts of individuals who will outright reject a vaccine regardless of the speed of development. Addressing those beliefs will likely require more than effective communication and may need to bolster public engagement and scientific literacy. However, recommending a specific strategy is beyond the scope of this article.
Fifth, media dependency was positively related to perceived vaccine efficacy and vaccination willingness, suggesting the mainstream media can be an effective communication channel to allay concerns about the vaccine and encourage uptake. However, that effectiveness may be hampered by newspapers and network news contributing to political polarization in their framing of COVID-19 severity [18], [37]. It is unclear if this polarization extends to coverage of the vaccine, but there is evidence that “balanced” reporting on vaccine risks and benefits can lead the public to perceive discord in the scientific community about vaccine safety [8]. And even if the mainstream media use consistent framing in their COVID-19 vaccine coverage, the effects on public vaccine hesitancy might not follow suit for a couple reasons. On the one hand, public understanding of scientific issues is not related to the use of any one type of media, but rather to the variety of sources people use [26]. On the other hand, regardless of the messaging appearing in the mainstream media, there will still be groups of people who distrust it [31]. Related, our post hoc analysis suggested more conservative individuals use the mainstream media less for information about COVID-19. Those same people may cluster, instead, around social media messages promoting vaccine conspiracy beliefs and hesitancy [1], [23] and form echo chambers that actively undermine competing viewpoints [41], [43]. Earlier we called for bolstering scientific literacy in public. In the same vein, there is a need to bolster media literacy in public [35], which can be an effective tool to reduce selective exposure to media messages [55]. This is pertinent in the context of social media, where viewpoints both consistent and inconsistent with scientific consensus are unfiltered by the gatekeepers of traditional media [45]. It is true the media are an important source of risk-related information the public can use to make decisions about advocated risk response actions. But the media are useful only insofar as the public has media literacy skills to search, access, and interpret that information.
This study has three notable limitations. First, the vaccines were hypothetical, and participants may have had different reactions when the first vaccine was approved. This limits external validity and is an inherent limitation when predicting how individuals will respond to a future scenario. Second, although our manipulations established timelines for vaccine development, our measure of vaccination willingness did not stipulate immediate vaccination. Loomba et al. [34] found individuals had lower vaccine hesitancy if they intended to wait for others to take the vaccine first. We have no way of knowing if such intentions affected our results. Third, despite efforts to capture a representative slice of the public, the small and non-random online sample means the results are not generalizable to the American public and further limits external validity. In particular, Hatch et al. [19] raised concern about selection bias when using online samples in epidemiological research but failed to find evidence of such bias. Admittedly, the current study is not epidemiological, bearing more resemblance to public opinion research. Public opinion researchers have concluded that online survey panels are problematic if researchers need precise estimates of the relationships between variables in a population and the sample deviates from the population on key variables [20]. The observed distribution of political orientation lends credence to the assumption that the current sample is representative of the population with respect to political views, which prior research has linked to vaccine conspiracy beliefs [11]. Despite that sliver of confidence, there is a need to replicate current findings using other samples and in other countries.
5. Conclusions
Although the speed of developing the COVID-19 vaccine was unprecedented, it did not mean compromising on efficacy and safety, a point that came up several times in the July 2020 hearing by the United States House Committee on Energy and Commerce [54]. Despite those assurances, it remained unclear how the public would react when the first vaccine became available. As of writing, the U.S. Centers for Disease Control and Prevention [51] report nearly 80% of people in the United States aged 12 and above have received at least one dose of the vaccine, which suggests a high degree of willingness among the public. At the same time, pockets of hesitancy remain [57]. That hesitancy is related to lingering concerns about efficacy and safety, which may stem from beliefs that vaccine development was too rapid. As vaccine efficacy and safety data continue to emerge, some of those concerns will allay. Along the way, it is important for governments and scientists to use the mainstream media to communicate transparently about vaccine development and undertake efforts to minimize vaccine conspiracy beliefs.
Funding
An internal grant (STAR Fund) from the Wee Kim Wee School of Communication and Information at Nanyang Technological University, Singapore, supported the data collection.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.11.014.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Allington D., Duffy B., Wessely S., Dhavan N., Rubin J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol Med. 2021;51(10):1763–1769. doi: 10.1017/S003329172000224X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bavel J.J.V., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4(5):460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- 3.Benham J.L., Lang R., Kovacs Burns K., MacKean G., Léveillé T., McCormack B., et al. Attitudes, current behaviours and barriers to public health measures that reduce COVID-19 transmission: a qualitative study to inform public health messaging. Plos One. 2021;16(2):e0246941. doi: 10.1371/journal.pone.0246941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calvillo D.P., Ross B.J., Garcia R.J.B., Smelter T.J., Rutchick A.M. Political ideology predicts perceptions of the threat of COVID-19 (and susceptibility to fake news about it) Soc Psychol Pers Sci. 2020;11(8):1119–1128. doi: 10.1177/1948550620940539. [DOI] [Google Scholar]
- 5.Chu H., Liu S. Integrating health behavior theories to predict American’s intention to receive a COVID-19 vaccine. Patient Educ Couns. 2021;104(8):1878–1886. doi: 10.1016/j.pec.2021.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cornwall W. Just 50% of Americans plan to get a COVID-19 vaccine. Here’s how to win over the rest. Science; 2020. https://www.sciencemag.org/news/2020/06/just-50-americans-plan-get-covid-19-vaccine-here-s-how-win-over-rest.
- 7.Cummings C.L., Rosenthal S., Kong W.Y. Secondary risk theory: validation of a novel model of protection motivation. Risk Anal. 2021;41(1):204–220. doi: 10.1111/risa:v41.110.1111/risa:13573. [DOI] [PubMed] [Google Scholar]
- 8.Dixon G.N., Clarke C.E. Heightening uncertainty around certain science: media coverage, false balance, and the autism-vaccine controversy. Sci Commun. 2012;35(3):358–382. doi: 10.1177/1075547012458290. [DOI] [Google Scholar]
- 9.Dubé E., Gagnon D., Ouakki M., Bettinger J.A., Guay M., Halperin S., et al. Understanding vaccine hesitancy in Canada: Results of a consultation study by the Canadian Immunization Research Network. Plos One. 2016;11(6):e0156118. doi: 10.1371/journal.pone.0156118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fadda M., Albanese E., Suggs L.S. When a COVID-19 vaccine is ready, will we all be ready for it? Int J Public Health. 2020;65(6):711–712. doi: 10.1007/s00038-020-01404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Featherstone J.D., Bell R.A., Ruiz J.B. Relationship of people’s sources of health information and political ideology with acceptance of conspiratorial beliefs about vaccines. Vaccine. 2019;37(23):2993–2997. doi: 10.1016/j.vaccine.2019.04.063. [DOI] [PubMed] [Google Scholar]
- 12.Fridman A., Gershon R., Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. Plos One. 2021;16(4):e0250123. doi: 10.1371/journal.pone.0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Funk C.D., Laferrière C., Ardakani A. A snapshot of the global race for vaccines targeting SARS-CoV-2 and the COVID-19 Pandemic [Review] Front Pharmacol. 2020;11(937) doi: 10.3389/fphar.2020.00937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldstein A., Clement S. Washington Post; 2020. 7 in 10 Americans would be likely to get a coronavirus vaccine, Post-ABC poll finds. [Google Scholar]
- 15.Graham B.S. Rapid COVID-19 vaccine development. Science. 2020;368(6494):945–946. doi: 10.1126/science.abb8923. [DOI] [PubMed] [Google Scholar]
- 16.Guarino B, Cha AE, Witte G. ‘The weapon that will end the war’: First coronavirus vaccine shots given outside trials in U.S. Washington Post; 2020. https://www.washingtonpost.com/nation/2020/12/14/first-covid-vaccines-new-york/.
- 17.Guidry J.P.D., Laestadius L.I., Vraga E.K., Miller C.A., Perrin P.B., Burton C.W., et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hart P.S., Chinn S., Soroka S. Politicization and polarization in COVID-19 news coverage. Sci Commun. 2020;42(5):679–697. doi: 10.1177/1075547020950735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hatch E.E., Hahn K.A., Wise L.A., Mikkelsen E.M., Kumar R., Fox M.P., et al. Evaluation of selection bias in an internet-based study of pregnancy planners. Epidemiology (Cambridge, Mass.) 2016;27(1):98–104. doi: 10.1097/EDE.0000000000000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hays R.D., Liu H., Kapteyn A. Use of internet panels to conduct surveys. Behav Res Methods. 2015;47(3):685–690. doi: 10.3758/s13428-015-0617-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ho S.S., Liao Y., Rosenthal S. Applying the theory of planned behavior and media dependency theory: predictors of public pro-environmental behavioral intentions in Singapore. Environ Commun. 2014;9(1):77–99. doi: 10.1080/17524032.2014.932819. [DOI] [Google Scholar]
- 22.Hotez P.J., Corry D.B., Strych U., Bottazzi M.E. COVID-19 vaccines: neutralizing antibodies and the alum advantage. Nat Rev Immunol. 2020;20(7):399–400. doi: 10.1038/s41577-020-0358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jamison A.M., Broniatowski D.A., Dredze M., Sangraula A., Smith M.C., Quinn S.C. Not just conspiracy theories: vaccine opponents and pro-ponents add to the COVID-19 ‘infodemic’ on Twitter. Harvard Kennedy School Misinf Rev. 2020;1(Special issue on COVID-19) doi: 10.37016/mr-2020-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang S. Don’t rush to deploy COVID-19 vaccines and drugs without sufficient safety guarantees. Nature. 2020;16 doi: 10.1038/d41586-020-00751-9. https://www.nature.com/articles/d41586-020-00751-9 [DOI] [PubMed] [Google Scholar]
- 25.Jolley D., Douglas K.M. The effects of anti-vaccine conspiracy theories on vaccination intentions. Plos One. 2014;9(2):e89177. doi: 10.1371/journal.pone.0089177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kahlor L., Rosenthal S. If we seek, do we learn? Predicting knowledge of global warming [Article] Sci Commun. 2009;30(3):380–414. doi: 10.1177/1075547008328798. [DOI] [Google Scholar]
- 27.Larson H.J., Jarrett C., Eckersberger E., Smith D.M.D., Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012 [Review] Vaccine. 2014;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 28.Larson H.J., Jarrett C., Schulz W.S., Chaudhuri M., Zhou Y., Dube E., et al. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33(34):4165–4175. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 29.Latkin C.A., Dayton L., Yi G., Konstantopoulos A., Boodram B. Trust in a COVID-19 vaccine in the U.S.: a social-ecological perspective. Soc Sci Med (1982) 2021;270:113684. doi: 10.1016/j.socscimed.2021.113684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee T., Hosam C. Fake news is real: the significance and sources of disbelief in mainstream media in Trump’s America. Sociol Forum. 2020;35(S1):996–1018. doi: 10.1111/socf.v35.s110.1111/socf.12603. [DOI] [Google Scholar]
- 32.Lin C.A., Xu X., Dam L. Information source dependence, presumed media influence, risk knowledge, and vaccination intention. Atlantic J Commun. 2021;29(2):53–64. doi: 10.1080/15456870.2020.1720022. [DOI] [Google Scholar]
- 33.Lithopoulos A., Liu S., Zhang C.-Q., Rhodes R.E. Predicting physical distancing in the context of COVID-19: a test of the extended parallel process model among Canadian adults. Canadian Psychol/Psychologie canadienne. 2021;62(1):56–64. doi: 10.1037/cap0000270. [DOI] [Google Scholar]
- 34.Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of exposure to COVID-19 vaccine misinformation on vaccine intent in the UK and US. medRxiv; 2020. 10.1101/2020.10.22.20217513. [DOI]
- 35.Mihailidis P. Civic media literacies: re-Imagining engagement for civic intentionality. Learn, Media Technol. 2018;43(2):152–164. doi: 10.1080/17439884.2018.1428623. [DOI] [Google Scholar]
- 36.Momplaisir F., Haynes N., Nkwihoreze H., Nelson M., Werner R.M., Jemmott J. Understanding drivers of coronavirus disease 2019 vaccine hesitancy among Blacks. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Motta M., Stecula D., Farhart C. How right-leaning media coverage of COVID-19 facilitated the spread of misinformation in the early stages of the pandemic in the U.S. Canadian J Polit Sci. 2020;53(2):335–342. doi: 10.1017/S0008423920000396. [DOI] [Google Scholar]
- 38.Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K., et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12(1) doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nagler R.H., Vogel R.I., Gollust S.E., Rothman A.J., Fowler E.F., Yzer M.C. Public perceptions of conflicting information surrounding COVID-19: Results from a nationally representative survey of U.S. adults. Plos One. 2020;15(10):e0240776. doi: 10.1371/journal.pone.0240776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21(7):977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nguyen C.T. Echo chambers and epistemic bubbles. Episteme. 2020;17(2):141–161. doi: 10.1017/epi.2018.32. [DOI] [Google Scholar]
- 42.Payton M.E., Greenstone M.H., Schenker N. Overlapping confidence intervals or standard error intervals: what do they mean in terms of statistical significance? J Insect Sci. 2003;3(34):1–6. doi: 10.1673/031.003.3401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Puri N., Coomes E.A., Haghbayan H., Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Human Vaccines Immunotherap. 2020;16(11):2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rogers R. Protection motivation theory of fear appeals and attitude-change [Article] J Psychol. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- 45.Rosenthal S. Media literacy, scientific literacy, and science videos on the internet. Front Commun. 2020 doi: 10.3389/fcomm.2020.581585. [DOI] [Google Scholar]
- 46.Schaffer DeRoo S., Pudalov N.J., Fu L.Y. Planning for a COVID-19 vaccination program. JAMA. 2020;323(24):2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- 47.Shapiro G.K., Holding A., Perez S., Amsel R., Rosberger Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2016;2:167–172. doi: 10.1016/j.pvr.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shapiro G.K., Tatar O., Dube E., Amsel R., Knauper B., Naz A., et al. The vaccine hesitancy scale: psychometric properties and validation. Vaccine. 2018;36(5):660–667. doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 49.Thunstrom L, Ashworth M, Finnoff D, Newbold S. Hesitancy towards a COVID-19 vaccine and prospects for herd immunity. SSRN (pre-publication); 2020. 10.2139/ssrn.3593098. [DOI] [PMC free article] [PubMed]
- 50.Tyson A, Johnson C, Funk C. U.S. public now divided over whether to get COVID-19 vaccine. Pew Research Center; 2020. https://www.pewresearch.org/science/wp-content/uploads/sites/16/2020/09/PS_2020.09.17_COVID-19-Vaccine_FINAL.pdf.
- 51.U.S. Centers for Disease Control and Prevention. COVID-19 vaccinations in the United States; 2021. Retrieved 26 April and 13 November from https://covid.cdc.gov/covid-data-tracker/#vaccinations.
- 52.U.S. Food and Drug Administration. FDA takes key action in fight against COVID-19 by issuing emergency use authorization for first COVID-19 vaccine; 2020. https://www.fda.gov/news-events/press-announcements/fda-takes-key-action-fight-against-covid-19-issuing-emergency-use-authorization-first-covid-19.
- 53.United States Department of Health and Human Services. Fact sheet: Explaining Operation Warp Speed; 2020. https://www.hhs.gov/about/news/2020/06/16/fact-sheet-explaining-operation-warp-speed.html.
- 54.United States House Committee on Energy and Commerce. Pathway to a vaccine: Efforts to develop a safe, effective and accessible COVID-19 vaccine; 2020. https://docs.house.gov/Committee/Calendar/ByEvent.aspx?EventID=110926.
- 55.Vraga E.K., Tully M. Engaging with the other side: Using news media literacy messages to reduce selective exposure and avoidance. J Inf Technol Polit. 2019;16(1):77–86. doi: 10.1080/19331681.2019.1572565. [DOI] [Google Scholar]
- 56.Wentzell E., Racila A.-M. The social experience of participation in a COVID-19 vaccine trial: Subjects’ motivations, others’ concerns, and insights for vaccine promotion. Vaccine. 2021;39(17):2445–2451. doi: 10.1016/j.vaccine.2021.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Willingham L, Hollingsworth H, Smith MR. US drop in vaccine demand has some places turning down doses. Associated Press; 2021. https://apnews.com/article/nm-state-wire-health-coronavirus-government-and-politics-108f1fd0813f0d2ecec1589fd137625d.
- 58.Witte K. Putting the fear back into fear appeals: the extended parallel process model. Commun Monogr. 1992;59(4):329–349. doi: 10.1080/03637759209376276. [DOI] [Google Scholar]
- 59.World Health Organization. Measuring behavioural and social drivers (BeSD) of vaccination working group; 2019. https://www.who.int/immunization/programmes_systems/Meeting_report_May2019.pdf?ua=1.
- 60.Yong A.G., Pearce S. A beginner’s guide to factor analysis: focusing on exploratory factor analysis. Tutor Quant Methods Psychol. 2013;9(2):79–94. doi: 10.20982/tqmp.09.2.p079. (IN FILE) [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.