Abstract
The Covid-19 crisis has led to a high demand and use of surgical masks worldwide, causing risks of shortages and pollution. Therefore, decontamination of surgical masks could be an opportunity to reduce these risks.
In our study, we applied dry heat to the masks for 15 min at different temperatures and studied the consequences of heat on surface chemistry and fiber morphology. We focus here on the effects of dry heat treatment on the masks and not on the verification of mask disinfection, which has been thoroughly studied in existing literature.
The masks that were heated to 70 °C, 100 °C, 130 °C, 140 °C, 150 °C did not show significant changes at the nanometric scale and the standard deviation of the surface temperature of the worn masks is similar to that of the unheated control mask. However we show a slight heating altered the hydrophobicity of the surface, and induced a significative modification of the wetting angle of water droplets. The mask heated to 157 °C has a higher surface temperature standard deviation and fused fibers are observed by scanning electron microscopy. The mask heated to 160 °C melted and then hardened as it cooled making it completely unusable.
Keywords: Covid-19, Pandemic, Face masks, Decontamination, Dry heat
1. Introduction
The significant impact of the Covid-19 outbreak paralyzed many countries in the world, forcing them to lockdown the population in order to stop the spread of the epidemic. The use of surgical masks helped to slow down the epidemic [1], [20]. In February 2020, single-use face mask production in China increased to 116 million per day [2].
Three major types of masks can be used: “Type I” masks, “Type II” and “Type IIR” masks. Type I masks filter 95% of the bacteria from an aerosol of average size 3 μm; type II masks filter 98% of the bacteria from an aerosol of average size 3 μm; type IIR filter the same as type II masks but are also splash resistant [3], [4]. A surgical mask can be either type. Type IIR masks are dedicated to the medical personnel.
Surgical masks are composed of non-woven polypropylene; they have three layers and three folders. The first and the third layer are the same and the second one is a filter. The filter is made of meltblown [5], [6] and is charged during the fabrication in order to increase the filtration capacity. Both the first and the third layer are made of 30 μm diameter fibers, the second one is made of 5 μm diameter fibers [7]. The daily use of the masks triggered a massive micro-plastic pollution [3]. According to the Oceanasia association, 1.56 billion face masks entered the oceans in 2020. Once in the oceans, these masks disintegrate into micro-particles which significantly disrupt the local ecosystem [8].
Thus, the reuse of surgical masks has been envisioned by many scientists. Various techniques have been tested: UV treatment [9], [10], [11], [12], [13], steam [14], [15], [13], [11], [9], dry heat [14], [13], [16], [9], [11], solvent [13], [11], [9]. According to the different studies, dry heat seems to be the easiest method to implement. It is known that the virus dies when exposed to a 63 °C environment for 4 min [17]. However, decontamination techniques can lead to a degradation and a loss of efficiency of the masks [18]. The origin of the loss of filtration efficiency is not systematically explained. Indeed, this degradation may be due to a modification of the microstructure and the surface chemistry of the masks.
The objective of this study is to focus on the possible degradation of masks (and the causes of this degradation) which have undergone a dry heat treatment.
2. Methods
Two face masks EN 14683/2019 were heated in an oven at temperatures of 70 °C, 100 °C, 130 °C, 140 °C, 150 °C, 157 °C and 160 ° C, for 15 min. Wetting angle measurements, thermal camera temperature measurements, and Scanning Electron Microscope (SEM) observations were then performed to assess the impact of dry heat on the mask structure at the micro and nanometric scale. For each heating temperature, a mask was used to perform thermal camera measurements and the other was used to perform both wetting angle and SEM measurements.
After being heated at 70 °C, 100 °C, 130 °C, 140 °C, 150 °C, 157 °C and 160 °C, the wetting angle of the masks, the surface temperature and the microstructure of the masks were observed.
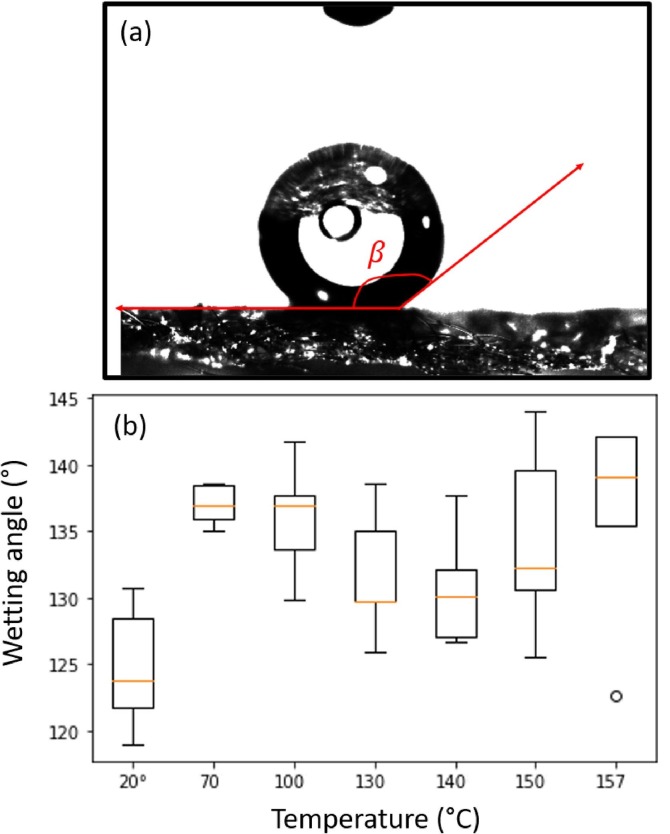
The wetting angle ( on Fig. 1 (a)) measurements were carried out with a tensiometer. Small squares of masks were cut (around 1 cm2) in each layer. The droplet had a constant volume of 1 μL except for the second layer where the droplet had to fall because of the high hydrophobia of the second layer. The measurements were repeated five times for each layer.
Fig. 1.
(a) Measurement of the wetting angle with a tensiometer, (b) statistic distribution of the wetting angle for each mask.
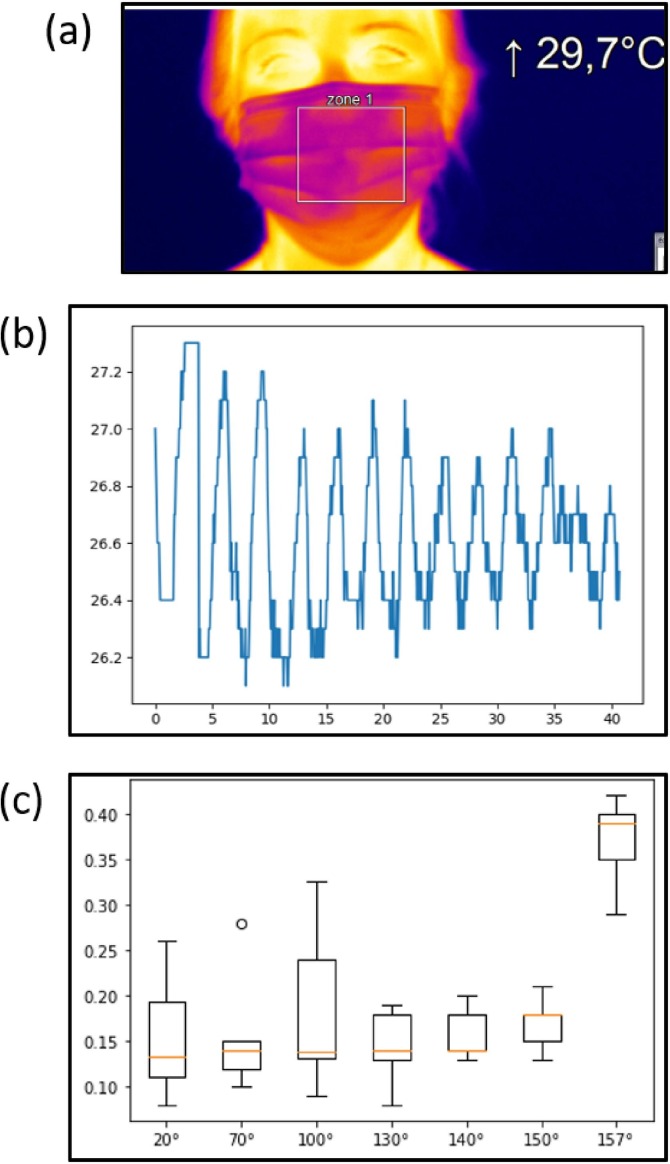
The InfraRed (IR) measurements were achieved with an iPi400 camera. A Region Of Interest (ROI) was chosen (the white square presented in Fig. 2 (a)) and the mean surface temperature of the ROI was measured during 40 s. This experiment was repeated 5 times for each mask with the same ROI and the same subject. Then, data were extracted and processed to extract the standard deviation of the temperature.
Fig. 2.
(a) ROI observed with the IR camera, (b) Evolution of the surface temperature of the mask heated at 70 °C as a function of time, (c) Statistic distribution of the Standard Deviation of the Surface Temperature (SDST) for each mask.
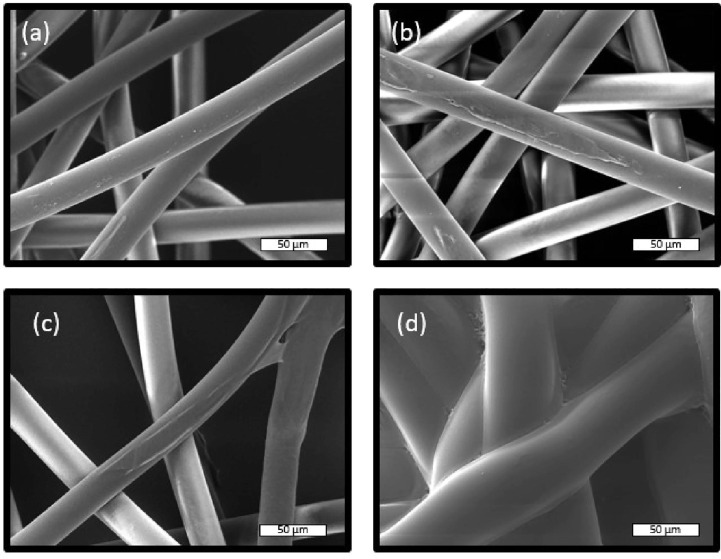
The SEM images were taken with a TESCAN MIRA3 microscope. Small squares of masks were cut (around 0.25 cm2) in each layer. The samples were placed on double-sided sticky carbon pads, which were sticked to an aluminum plane. The samples were then gold-coated by a sputtering device. The images were taken with an accelerating voltage of 10 kV.
3. Results
Fig. 1(a) shows a typical liquid droplet wetting on the mask surface and the corresponding wetting angle . The statistic distribution of the wetting angle is shown in Fig. 1 (b). The mean wetting angle increased going from 123°, with a standard deviation of 5° for the control sample to 137° and a standard deviation of 3° for the mask heated at 70 °C. A significant increase of the wetting angle was observed for each heated mask. It should be noted the contact angle values were not significantly altered by series of annealing performed at the same temperature.
Fig. 2(b) represents the average temperature of the ROI of the mask heated at 70 °C as a function of time. The maximum corresponds to the exhale of the subject and the minimum corresponds to the inhale of the subject. For the mask heated at 70 °C, the mean temperature was 29 °C and the standard deviation was 0.277 °C.
The statistic distribution of the standard deviation of the surface temperature (SDST) is represented in Fig. 2 (c). The SDST is stable for the temperatures until 157°, when it brutally increases. Indeed, for the control sample the SDST was 0.12 °C and it was 0.39 °C for the mask heated at 157 °C.
Fig. 3(a) and (b) show the first layer of the mask of the control sample and of the mask heated at 70 °C. Up to 155 °C no notable changes were observed, the fibers looked like the control sample. However, for the mask heated at 155 °C (Fig. 3 (c)) the fibers partially fused. For the mask heated at 160 °C, the temperature was so close to the fusion temperature that the fibers totally fused. All of the layers fused together, making the mask very hard and unwearable.
Fig. 3.
(a) Control sample, (b) mask heated at 70 °C, (c) mask heated at 155 °C, (d) mask heated at 160 °C. (The magnification is 1.12 k, all the images correspond to the first layer of the mask)
The restults are summarized in Table 1 (a = means no notable changes compared to the control sample, a + means an increase and a means that the measures could not be performed).
Table 1.
Table of results
| Mask | SDST (°C) | Wetting angle (°) | Visual aspect | SEM (fibers) |
|---|---|---|---|---|
| control sample | 0.12 | 130 | Normal | Intact |
| 70 °C | = | + | = | Intact |
| 100 °C | = | + | = | Intact |
| 130 °C | = | + | = | Intact |
| 140 °C | = | + | = | Intact |
| 150 °C | = | + | = | Intact |
| 157 °C | + | + | Blistered | Partly Fused |
| 160 °C | × | × | Fused | Totally fused |
4. Discussion
The masks heated at the highest temperatures were deeply damaged by the treatment. Indeed, the fibers fused. Regarding the mask heated at 157 °C, the fibers partially fused (Fig. 3 (c)), making breathing harder for the user (which could explain the higher air flow coming outside from the mask). The mask heated at 160 °C was unusable, as it had totally fused it was impossible to wear it. The increase in the airflow coming outside of the mask is not the only notable change.
The wetting angle increased significantly on the heated masks (even the one with the lowest temperature). This result can explain the source of the loss of filtration efficiency. Indeed, an increase in wetting angle means that the treated masks are more hydrophobic, which is important to prevent contaminated drops from reaching the user. However, this increase may be due to the loss of surface charges [18], that is likely to modify the surface’s chemical properties. Surface charges are useful, as they increase the filtration efficiency of the masks. Thus, the filtration efficiency might have decreased during the decontamination process. As the filtration efficiency was not measured, this loss cannot be quantified.
To conclude, when heated, the masks might loose a portion of their surface charges, making them more hydrophobic but less efficient. The only notable changes in airflow coming outside of the mask were visible on the masks heated at 157 °C and 160 °C. This variation is due to the partial (or total) fuse of the fibers. The impact of a dry heat on face mask seems to be limited to a slight modification of its hydrophobic properties. However other characterization should be performed to ensure the mask integrity.
Credit authorship contribution statement
Elise Sales: Investigation, Validation, Writing - original draft. Naïl Mulatier: Investigation, Validation, Writing - original draft. Louise Wittmann: Investigation, Validation, Writing - original draft. Antoine Fernandes: Investigation, Validation, Writing - original draft. Béatrice Vacher: Investigation. Jose Penuelas: Conceptualization, Supervision, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors thank the NanoLyon platform for access to the equipments. Isabel Nabeth, Thomas Gehin and Henri-Gabriel Glories are acknowledged for technical assistance.
References
- 1.O’Dowd, Kris, et al. Face Masks and Respirators in the Fight Against the COVID-19 Pandemic: A Review of Current Materials, Advances and Future Perspectives. Materials, vol. 13, no 15, january 2020, p. 3363. www.mdpi.com, doi:10.3390/ma13153363. [DOI] [PMC free article] [PubMed]
- 2.Aragaw, Tadele Assefa. Surgical Face Masks as a Potential Source for Microplastic Pollution in the COVID-19 Scenario. Marine Pollution Bulletin, vol. 159, october 2020, p. 111517. ScienceDirect, doi:10.1016/j.marpolbul.2020.111517. [DOI] [PMC free article] [PubMed]
- 3.Quesnel, Louis B. The Efficiency of Surgical Masks of Varying Design and Composition. BJS British Journal of Surgery, vol. 62, no 12, 1975, p. 936–40. Wiley Online Library, doi: 10.1002/bjs.1800621203. [DOI] [PMC free article] [PubMed]
- 4.An Overview of Filtration Efficiency through the Masks: Mechanisms of the Aerosols Penetration. Bioactive Materials, vol. 6, no 1, january 2021, p. 106–22. www.sciencedirect.com, doi:10.1016/j.bioactmat.2020.08.002. [DOI] [PMC free article] [PubMed]
- 5.Zuo, Feng, et al. Nanofibers from Melt Blown Fiber-in-Fiber Polymer Blends. ACS Macro Letters, vol. 2, no 4, April 2013, p. 301–05. DOI.org (Crossref), doi:10.1021/mz400053n. [DOI] [PubMed]
- 6.Chua, Ming Hui, et al. Face Masks in the New COVID-19 Normal: Materials, Testing, and Perspectives. Research, vol. 2020, august 2020. spj.sciencemag.org, doi:10.34133/2020/7286735. [DOI] [PMC free article] [PubMed]
- 7.Peeples, Lynne. Face Masks: What the Data Say. Nature, vol. 586, no 7828, october 2020, p. 186–89. www.nature.com, doi:10.1038/d41586-020-02801-8. [DOI] [PubMed]
- 8.Dybas, Cheryl. Surgical masks on the beach: COVID-19 and marine plastic pollution. Oceanography, vol. 34, no 1, March 2021. DOI.org (Crossref), doi:10.5670/oceanog.2021.105.
- 9.Evaluation of Decontamination Methods for Commercial and Alternative Respirator and Mask Materials – View from Filtration Aspect. Journal of Aerosol Science, vol. 150, december 2020, p. 105609. www.sciencedirect.com, doi:10.1016/j.jaerosci.2020.105609. [DOI] [PMC free article] [PubMed]
- 10.Health, Center for Devices and Radiological. UV Lights and Lamps: Ultraviolet-C Radiation, Disinfection, and Coronavirus. FDA, january 2021. www.fda.gov, https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/uv-lights-and-lamps-ultraviolet-c-radiation-disinfection-and-coronavirus.
- 11.Suen, C.Y., et al. Feasibility of Reusing Surgical Mask Under Different Disinfection Treatments. MedRxiv, May 2020, p. 2020.05.16.20102178. www.medrxiv.org, doi:10.1101/2020.05.16.20102178.
- 12.Kumar, Sumit, et al. Photoactive Antiviral Face Mask with Self-Sterilization and Reusability. Nano Letters, november 2020. ACS Publications, doi:10.1021/acs.nanolett.0c03725. [DOI] [PubMed]
- 13.Côrtes, Marina Farrel, et al. Decontamination and Re-Use of Surgical Masks and Respirators during the COVID-19 Pandemic. International Journal of Infectious Diseases, vol. 104, March 2021, p. 320–28. DOI.org (Crossref), doi:10.1016/j.ijid.2020.12.056. [DOI] [PMC free article] [PubMed]
- 14.Li, Daniel F., et al. It’s Not the Heat, It’s the Humidity: Effectiveness of a Rice Cooker-Steamer for Decontamination of Cloth and Surgical Face Masks and N95 Respirators. American Journal of Infection Control, vol. 48, no 7, July 2020, p. 854–55. ScienceDirect, doi:10.1016/j.ajic.2020.04.012. [DOI] [PMC free article] [PubMed]
- 15.Li, Daniel F., et al. Steam Treatment for Rapid Decontamination of N95 Respirators and Medical Face Masks. American Journal of Infection Control, vol. 48, no 7, July 2020, p. 855–57. ScienceDirect, doi:10.1016/j.ajic.2020.05.009. [DOI] [PMC free article] [PubMed]
- 16.Xiang, Yi, et al. Decontamination of Surgical Face Masks and N95 Respirators by Dry Heat Pasteurization for One Hour at 70C. American Journal of Infection Control, vol. 48, no 8, august 2020, p. 880–82. DOI.org (Crossref), doi:10.1016/j.ajic.2020.05.026. [DOI] [PMC free article] [PubMed]
- 17.Abraham, John P., et al. Using heat to kill SARS–CoV–2. Reviews in Medical Virology, July 2020, p. e2115. PubMed Central, doi:10.1002/rmv.2115. [DOI] [PMC free article] [PubMed]
- 18.Liao, Lei, et al. Can N95 Respirators Be Reused after Disinfection? How Many Times? ACS Nano, vol. 14, no 5, May 2020, p. 6348–56. ACS Publications, doi:10.1021/acsnano.0c03597. [DOI] [PubMed]
- 19.Evaluation of Decontamination Methods for Commercial and Alternative Respirator and Mask Materials – View from Filtration Aspect. Journal of Aerosol Science, vol. 150, december 2020, p. 105609. www.sciencedirect.com, doi:10.1016/j.jaerosci.2020.105609. [DOI] [PMC free article] [PubMed]
- 20.Cheng, Yafang, et al. Face Masks Effectively Limit the Probability of SARS-CoV-2 Transmission. Science, vol. 372, no 6549, June 2021, p. 1439–43. science.sciencemag.org, doi:10.1126/science.abg6296. [DOI] [PMC free article] [PubMed]