Abstract
Introduction
Cardiac rehabilitation (CR) is an effective tool for secondary prevention after acute coronary syndrome (ACS).
Aim
Aim of our study was to find the significant determinants of exercise capacity (evaluated with the six-minute walking test—6-MWT) and functional improvement in patients undergoing CR after an ACS.
Methods
The study group included 298 patients (mean age 61.6 ± 10.2 years; males 80.2%) who, after ACS, were enrolled in CR program at Niguarda Hospital in Milan from 2015 to 2018. For all patients, we collected anamnestic, clinical and instrumental cardiological data. All patients performed a 6-MWT at the beginning (6-MWT-1) and at the end (6-MWT-2) of CR program. Δ meters were used to represent functional improvement.
Results
Multiple linear regression models were carried out for 6-MWT-1, 6-MWT-2, Δ meters and % Δ meters. Standardized regression coefficients showed that age (β = − 0.237; p < 0.001), BMI (β = − 0.116; p = 0.006) and heart rate (β = − 0.082; p = 0.040) were determinants of exercise capacity (6MWT-1 and 2), whereas age (β = −.231; p = 0.004), sex (β = − 0.187; p = 0.008) and BMI (β = − 0.164; p = 0.022) were determinants of functional improvement (Δ meters).
Conclusions
Our data showed that functional improvement after CR in ACS patients is mainly related to non-cardiological variables. Instead it is related to intrinsic factors, both modifiable (BMI) and non-modifiable (age, sex).
Supplementary Information
The online version contains supplementary material available at 10.1007/s40292-021-00473-7.
Keywords: Cardiac rehabilitation, Acute coronary syndrome, Functional improvement
Introduction
Advances in the treatment of Acute Coronary Syndrome (ACS) achieved in the last decades led to an improvement in patient survival and, consequently, generated the need to intervene in terms of secondary prevention and Cardiac Rehabilitation (CR). Furthermore, since the duration of hospitalization is being reduced and the attention is more focused on the resolution of the acute problem, CR responds to the need to implement other types of intervention, such as health education and information, promotion of lifestyle changes, monitored physical activity, therapeutic optimization, risk stratification, functional and global evaluation [1]. CR health education interventions are particularly of interest to improve awareness of CV risk factors [2] and adherence to medical therapies [3]. CR participation after an ACS has demonstrated to be effective in reducing subsequent mortality [4].
Different and discordant associations between baseline characteristics of patients undergoing CR after ACS and their functional improvement could be found in literature. Lower exercise capacity at baseline, advanced age, higher lipids, female sex, and higher BMI have been found to be negative predictors of functional improvement after CR [5–11]. However also data showing that the improvement was not related to age, sex or left ventricular function [12, 13] have been published. Thus, the aim of our study was to define the determinants of functional improvement in patients undergoing CR after ACS. In order to quantify exercise capacity and functional improvement, patients performed a Six-Minute Walking Test (6-MWT) at the beginning and at the end of CR.
Methods
Study Population
A total of 410 consecutive patients were enrolled in the CR program of the Niguarda Hospital (Milan, Italy) institution from January 1st 2015 to December 31st 2018. Exclusion criteria were all non-ACS heart diseases (Chronic Coronary Sindrome, dilated or hypertrophic cardiomyopathy and peripheral artery disease) as well as neurological, pneumological or orthopaedic diseases impairing prolonged physical activity. Furthermore, individuals with a premature interruption of CR program were not considered in our study.
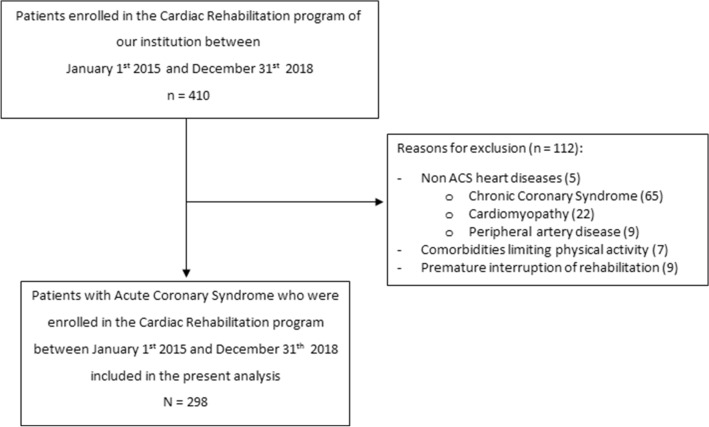
After application of exclusion criteria, 298 patients (239 men and 59 women) who were included in the CR program starting within two weeks after the index ACS were analysed (Fig. 1).
Fig. 1.
Study flow-chart of patients included in the analysis. ACS acute coronary syndrome
We collected data on medical history and physical examination at the beginning of the CR program, including age, body mass index (BMI), risk factors (hypertension, Diabetes Mellitus—DM—smoking habit and dyslipidaemia), pharmacotherapy (focusing on β-blockers, lipid-lowering, antiplatelet and antihypertensive drugs) and details on CV diseases, such as previous percutaneous or surgical revascularisation, number of critically occluded coronary vessels and maximum high-sensitivity cardiac troponin (hs-cTnT) and creatine kinase MB isoenzyme (CK-MB) values achieved during the event.
Moreover, we investigated the pharmacological history, in particular for the following classes of drugs: β-blockers, lipid-lowering, antiplatelet and antihypertensive drugs.
We also registered findings about blood pressure (BP), heart rate (HR) and left ventricular ejection fraction (LVEF) documented at the echocardiogram both at the beginning and at the end of the CR program, as we did with blood tests such as total-cholesterol, HDL-cholesterol, LDL-cholesterol, triglycerides, glucose and creatinine.
Cardiac Rehabilitation Program
The training program included 25 sessions with a total amount of 5 weeks of CR, which was performed in an outpatient setting in order to provide high intensity rehabilitation services and low intensity clinical care.
The daily aerobic physical exercise, which was the main activity of the program, was divided into 45 min of endurance training on the exercise bike and, after 15 min of resting time, 45 min of free-body exercises. Physical exercise intensity was modulated individually on functional capacity and effort tolerance.
Beside the cardiologist, who was the reference and coordinating figure, candidates related with a multidisciplinary team composed of nurses and physiotherapists. Moreover, CR program included a clinical dialogue with a psychologist—aiming to support the patient in changing lifestyle and in controlling emotional feelings—and dietology consultation in order to educate about nutritional habits.
Six-Minute Walking Test
Each candidate was submitted to a 6-MWT under standardized conditions, consisting in a 30 m, straight indoor hallway in accordance with the ATS guidelines [14]. Data registered on 6-MWT included vital signs (heart rate and oxygen saturation, detected at rest and at the end) and distance in meters.
The test was reproduced both at the beginning and at the end of the program, in order to obtain the functional improvement of the patient represented by the Δ meters, resulting from the mathematical subtraction of the distance covered at the end of CR and the one reached at the beginning. This indicator was also normalized for expected values, calculated using the following formula:
The tests were performed for all the patients at the two time point by a single trained physiotherapist.
The American Thoracic Society Guidelines suggest using absolute values when expressing the difference in distance travelled [15]; this recommendation is due to the lack of a definite indication about the use of the crude differences of the distance (m), its percentage or the values normalized for the expected one.
Statistical Analysis
Continuous and categorical variables were presented respectively as mean ± Standard Deviation (SD) and percentages. A Paired Samples T-Test was used to compare baseline and final factors for continuous variables, while a Chi-Square Tests was performed for categorical ones. Similarly, comparisons between subgroup (according to Δ meters and sex) were conducted using Independent Samples T-Test for continuous variables and Chi-Square Tests for categorical variables.
Pearson product-moment correlation coefficient or Spearman’s rank correlation coefficient was used to assess correlations among variables as appropriate. Multivariable linear regression models were performed considering the distance walked at 6-MWT at the beginning and at the end of CR and the relative Δ meters (which was also normalized for expected values) as the dependent variables, respectively; independent predictors were selected including the most clinically important baseline variables characterized by statistically significance Pearson correlation coefficients (see methods section).
Statistical analyses were performed using SPSS Statistics (IBM®). A p-value < 0.05 was considered to determine statistical significance.
Results
Population Characteristics
Table 1 shows population characteristics. 80.2% of the study population were male and mean age was 61.6 ± 10.2 years. Regarding CV risk factors BMI was 26.9 ± 3.7 kg/m2 so 57.7% of population were in overweight or obesity conditions, 16.1% were diabetic, 67.8% present dyslipidemia and 65.1% had arterial hypertension (with mean Systolic and Diastolic BP—SBP/DBP respectively—122.1 ± 15.4 and 74.8 ± 10.2 mmHg).
Table 1.
Population characteristics
| Number | 298 |
| Male (%) | 80.2% |
| Age (years) | 61.6 ± 10.2 |
| BMI (kg/m2) | 26.9 ± 3.7 |
| Overweight or obesity | 57.7% |
| Diabetes mellitus | 16.1% |
| Dyslipidaemia | 67.8% |
| Arterial hypertension | 65.1% |
| Smoking | 63.4% |
| Previous coronary revascularization | 18.8% |
| Atrial fibrillation | 7.0% |
| CK-MB max (ng/ml) | 91.2 ± 131.3 |
| TnT-hs max (ng/l) | 2344.4 ± 4057.2 |
| Number of coronary arteries treated with stenting during index ACS | |
| 1. Coronary artery | 52.7% |
| 2. Coronary arteries | 27.9% |
| 3. Coronary arteries | 14.4% |
BMI Body Mass Index, CK-MB creatine kinase MB fraction, TnT-hs troponin T high sensitive, LDL low density lipoprotein, HDL high density lipoprotein, SBP systolic blood pressure, DBP diastolic blood pressure, HR heart rate
18.8% had received a previous coronary revascularisation (prior to the recent ACS) while, regarding the acute CV events that lead to CR, maximum CK-MB and TnT-hs were 91.2 ± 131.3 mcg/l and 2344.4 ± 4057.2 ng/ml. 14.4% of subjects showed three critical coronary stenosis at the coronary angiography.
Baseline biochemical, echocardiographic and functional variables and their changes during CR were showed in Table 2. In the period between entry and discharge from CR, all patients improved the distance covered during the 6-MWT (474.7 ± 97.2 vs 590.6 ± 108.0 m; p < 0.001), configuring an average Δ meters of 115.8 ± 59.2. Patients also improved lipid profile: total-cholesterol from 177.3 ± 42.3 to 136.1 ± 28.9 mg/dl (p < 0.001); LDL-cholesterol from 110.3 ± 39.3 to 68.3 ± 22.7 mg/dl (p < 0.001); HDL-cholesterol from 43.6 ± 11.3 to 45.1 ± 12.3 mg/dl (p = 0.006); triglycerides from 129.2 ± 70.4 to 118.8 ± 64.9 mg/dl (p = 0.018). Furthermore, patients reduced BP (SBP from 122.1 ± 15.4 to 113.8 ± 11.0 mmHg, p < 0.001; DBP from 74.8 ± 10.2 to 66.1 ± 7.9 mmHg; p < 0.001) and HR (from 62.6 ± 7.6 to 60.6 ± 7.3 bpm; p < 0.001) and increased LVEF (from 54.5 ± 7.2 to 56.7 ± 6.0 %; p < 0.001).
Table 2.
Clinical data at the beginning and at the end of CR program
| Baseline | Final | p value | |
|---|---|---|---|
| Creatinine (mg/dl) | 1.04 ± 0.42 | 1.07 ± 0.49 | 0.093 |
| Total cholesterol (mg/dl) | 177.3 ± 42.3 | 136.1 ± 28.9 | < 0.001 |
| LDL cholesterol (mg/dl) | 110.3 ± 39.3 | 68.3 ± 22.7 | < 0.001 |
| HDL cholesterol (mg/dl) | 43.6 ± 11.3 | 45.1 ± 12.3 | 0.006 |
| Triglycerides (mg/dl) | 129.2 ± 70.4 | 118.8 ± 64.9 | 0.018 |
| Glycaemia (mg/dl) | 109.4 ± 27.0 | 108.1 ± 19.7 | 0.708 |
| SBP (mmHg) | 122.1 ± 15.4 | 113.8 ± 11.0 | < 0.001 |
| DBP (mmHg) | 74.8 ± 10.2 | 66.1 ± 7.9 | < 0.001 |
| HR (bpm) | 62.6 ± 7.6 | 60.6 ± 7.3 | < 0.001 |
| LVEF (%) | 54.5 ± 7.2 | 56.7 ± 6.0 | < 0.001 |
| 6-MWD (m) | 474.7 ± 97.2 | 590.6 ± 108.0 | < 0.001 |
LDL low density lipoprotein, HDL high density lipoprotein, SBP systolic blood pressure, DBP diastolic blood pressure, HR heart rate, LVEF left ventricular ejection fraction, 6-MWD 6-minute walk distance
Subgroup Analysis
When patients were divided according to their Δ meters median value (110 m), subjects whit lower functional improvement were older (63.4 ± 10.7 vs 59.8 ± 9.3 years; p = 0.004) and presented higher HR (64.2 ± 7.9 vs 61.1 ± 7.0 bpm; p = 0.003) as shown in Supplementary Table 1.
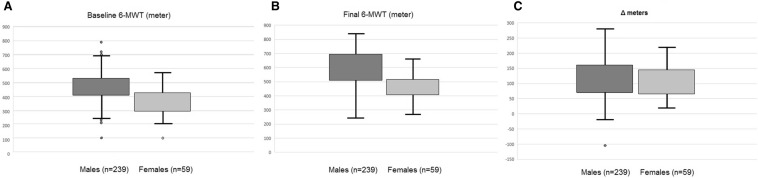
Supplementary Table 2 showed clinical data when patients were divided according to sex. Females presented significantly lower final 6-MWT (470.0 ± 92.4 vs 586.6 ± 110.8 m; p = 0.038, Fig. 2B) and BMI (26.4 ± 4.7 vs 27.3 ± 3.7 kg/m2; p = 0.015) in comparison to males, while they present a higher baseline LDL cholesterol (113.2 ± 47.3 vs 108.9 ± 37.4 mg/dl; p = 0.025). Furthermore, also a border-line lower Δ meters (101.2 ± 50.8 vs 119.6 ± 60.7; p = 0.061, Fig. 2C) was founded.
Fig. 2.
Boxplot continuous outcome variables referred as baseline 6-MWT (A), final 6-MWT (B) and ∆ meters (C). In boxplots the inner line indicates the median; the whiskers are located at the maximum and minimum observation (outside observations indicated with dots are those out of the 1.5 × interquartile range)
Correlations and Regression Analysis
Correlations for baseline and final 6-MWT distance and the relative Δ were showed in Table 3. Summarizing them, all the three variables correlates with age, baseline LDL cholesterol and baseline HR. The initial and the final covered distance both correlates with most of classical CV risk factors (BMI, arterial hypertension and baseline SBP, current or previous smoking habit) and diseases (previous coronary revascularisation and atrial fibrillation). Baseline 6-MWT distance also correlates with TnT peak (r = 0.129, p = 0.038) while final 6-MWT distance showed significant correlation also with DM (r = − 0.176; p = 0.003), reduction of LDL-cholesterol from the beginning to the end of CR (r = − 0.262; p < 0.001) and baseline glycaemia (r = − 0.147, p = 0.025). Finally, Δ meters showed correlations also with sex (r = − 0.125; p = 0.035), DM (r = − 0.155; p = 0.009), glycaemia (r = − 0.132; p = 0.045) and number of coronary arteries affected by critical stenosis (r = − 0.134; p = 0.024).
Table 3.
Correlations between clinical data and baseline 6-MWD, final 6-MWD and Δ meters.
| Baseline 6-MWD | Final 6-MWD | Δ meters | ||||
|---|---|---|---|---|---|---|
| r | p-value | r | p-value | r | p-value | |
| Age | − 0.488 | < 0.001 | − 0.511 | < 0.001 | − 0.194 | 0.001 |
| Male | – | – | – | – | − 0.125 | 0.035 |
| BMI | − 0.220 | < 0.001 | − 0.237 | < 0.001 | – | – |
| Diabetes mellitus | – | – | − 0.176 | 0.003 | − 0.155 | 0.009 |
| Arterial hypertension | − 0.226 | < 0.001 | − 0.258 | < 0.001 | – | – |
| Smoking | 0.163 | 0.005 | 0.147 | 0.013 | – | – |
| Previous coronary revascularisation | − 0.160 | 0.006 | − 0.126 | 0.033 | – | – |
| TnT-hs | 0.129 | 0.038 | – | – | – | – |
| Coronary vessels critical occlusion | – | – | – | – | − 0.134 | 0.024 |
| LDL cholesterol | 0.135 | 0.026 | 0.213 | <0.001 | 0.160 | 0.009 |
| LDL cholesterol | – | – | − 0.262 | < 0.001 | – | – |
| Baseline glycaemia | – | – | − 0.147 | 0.025 | − 0.132 | 0.045 |
| Baseline SBP | − 0.157 | 0.013 | − 0.175 | 0.007 | – | – |
| Baseline HR | − 0.168 | 0.009 | − 0.273 | < 0.001 | − 0.192 | 0.003 |
| Atrial Fibrillation | − 0.178 | 0.002 | − 0.187 | 0.001 | – | – |
BMI Body Mass Index, TnT-hs troponin T high sensitive, LDL low density lipoprotein, SBP systolic blood pressure, HR heart rate
Subsequently, linear regression analysis was performed (Table 4). In the model for baseline 6-MWT meter as dependent variables, age, sex, BMI, arterial hypertension, smoking, LDL-cholesterol, maximum peak of hs-cTnT, baseline SBP and HR and atrial fibrillation were used as covariates. With a total R2 of 0.335 the significant determinants were age (β = − 0.452; p < 0.001), BMI (β = − 0.199; p = 0.002) and HR (β = − 0.151; p = 0.013).
Table 4.
Determinants of exercise capacity and functional improvement
| β | p-value | |
|---|---|---|
| Baseline 6-MWD | ||
| Age | − 0.452 | < 0.001 |
| BMI | − 0.199 | 0.002 |
| Baseline HR | − 0.151 | 0.013 |
| Final 6-MWD | ||
| Baseline 6-MWD | 0.707 | < 0.001 |
| Age | − 0.237 | < 0.001 |
| BMI | − 0.116 | 0.006 |
| Baseline HR | − 0.082 | 0.040 |
| Δ meters | ||
| Age | − 0.231 | 0.004 |
| Male | − 0.187 | 0.008 |
| BMI | − 0.164 | 0.022 |
BMI Body Mass Index, HR heart rate, 6-MWD 6-minute walk distance
In the model for walked distance at final 6-MWT also DM and meters covered at baseline 6-MWT was inserted as covariates. With a total R2 of 0.791 the significant determinants were the baseline walked distance (β = 0.707; p < 0.001), age (β = − 0.237; p < 0.001), BMI (β = − 0.116; p = 0.006) and HR (β = − 0.082; p = 0.040).
Finally, model for ∆ meters present age, sex, BMI, DM, baseline LDL-cholesterol, glucose level, SBP, HR and the number of coronary arteries affected by critical stenosis as covariates. Whit a total R2 of 0.185 the significant determinants were age (β = − 0.231; p = 0.004), sex (β = − 0.187; p = 0.008) and BMI (β = − 0.164; p = 0.022). Similar results were also founded when ∆ meters was normalized for the expected values.
Discussion
The main result of our study was that the determinants of functional capacity (both at the beginning and at the end of CR) were age, BMI and HR. Furthermore, sex is implicated as a determinant of functional improvement (i.e. Δ meter) obtained during CR.
The relationship between older age and lower physical performance, both in terms of exercise capacity and functional improvement, is complex. First of all, age-related muscle change, which involves both skeletal muscle morphology and functionality, should be considered in older patients. Sarcopenia, the loss of muscle mass related to aging, physiologically occurs within the elderly population [5]. Furthermore, the interaction between older age and reduction of functional capacity can be confused with presence of comorbidities, which can negatively affect the execution of physical activity and the autonomy of the patient [5, 16]. Moreover, elderly patients are more vulnerable to adverse pharmacological events because of an increased risk of drugs interactions due to polypharmacotherapy and because of geriatric frailty [16]. This could be particularly the case of statins in which polypharmacotherapy interactions could increase the occurrence of muscle weakness or cramp leading to lower functional capacity. However, in our study, as well as in those published previously [11, 17], older patients showed a statistically significant functional improvement confirming the important role of CR also in this population.
The second most important finding to discuss is the sex implication [18]. In fact, females seemed to present lower functional improvement after CR. Nevertheless, as also founded in previous studies [5, 6, 9, 19], even female subjects increased appropriately their exercise capacity after CR course. Many reasons could explain these results. First of all, sex differences in diagnosis and treatment have been described. Women have smaller coronary arteries and less plaque burden but more apparent stenosis that is related to differences in remodelling [18], they present also a higher prevalence of spontaneous coronary dissection and myocardial infarction with no obstructive coronary atherosclerosis [20]. Women often present atypical symptoms, experience a smaller increase in cardiac enzymes and their CV risk is underestimated by traditional risk models resulting in diagnosis and treatment delays, and in higher rates of worse outcomes [21]. On the same issue, also personality traits and social roles traditionally ascribed to women could help explaining longer diagnosis and treatment delays in women [22]. Finally, women present also procedural technical aspects (such as an higher rate of radial artery spasm) that could leads to an increased risk of complications (access site bleeding and contrast induced nephropathy) and receive less frequently guideline-suggested treatments in comparison with men [21, 23].
Moreover, women low adherence to CR programs is a very important issue that may interfere with the overall functional improvement. It is widely known that men are more adherent to CR programs and that recruitment for women is often significantly delayed [24]. For women, the barriers to CR participation are multiple and complex and possible solutions such as community and home-based physical activity and women-only cardiac rehabilitation should be offered and are actually under evaluation [25].
Another important determinant founded in our analysis was BMI that was associated with lower functional capacity during 6-MWT as also reported by some previous studies [5, 9]. We didn’t collect discharge BMI and so we cannot relate it to the functional improvement, however, previous studies showed that obese patients who lost more than 5% of basal weight achieved a considerable improvement in exercise capacity, suggesting a possible association between the amount of weight loss and improvement in exercise capacity [9]. This result seems to suggest that an important effort to help patients reaching normal weight could be repaid by an increase in functional improvement. We must also say that weight loss often is a process longer than CR period and it is possible that what patients learn during CR could lead to further gain after CR itself.
In our study lower baseline HR was associated with higher functional capacity both before and after CR. Our findings are discordant with a previous study in which patients who initially showed evidence of the poorest state of fitness, with high rest HR, achieved a greater improvement after CR [26]. With regard to this, it is important to underline that HR value is strongly dependent on assumption of β-blockers. In our study all the patients took this drug class (principally bisoprolol) in order to reach a resting HR of 50–60 bpm. Patients with lower basal HR are those who better tolerate B-blockers and so who more benefit from their positive effects [27–29].
Previous studies also found that, despite a significant improvement of quality of life, weight loss and CV risk factors, diabetic subjects showed a significantly lower improvement in exercise capacity than non-diabetic subjects [10, 30]. We found that presence of DM and blood glucose values were associated with lower exercise capacity during 6-MWT and lower functional improvement after CR while these results were not confirmed at the multivariate analysis. However, DM prevalence in our population was low (16%) and this could be the reason why significant association was not found.
Finally, also anemia and hemoglobin level at baseline may have a relevant impact on functional capacity. Unfortunately, we were not able to collect hemoglobin level in our patients and so to test its association with functional improvement. However, it certainly have a role in ACS patients prognosis and their functional status. In fact, a drop in hemoglobin level (even in the absence of significant bleeding, have been identify as an independent predictor of 1-year mortality [31]. Furthermore, anemia was found to be very prevalent (75.2% of the population) in cardiac rehabilitation patients and to be related to their functional capacity [32, 33]
Another point of our study that needs to be discuss, i.e the confirmation of the efficacy regarding functional improvement and the optimization of cardiovascular risk factor (lipid profile, BP and HR) as well as improvement in LVEF. Besides the well-known effect of physical exercise [34], these improvement can be interpreted as the reflection of the efficacy of other aspects of the CR program such as therapeutic optimization, risk factors information, food education and promotion of a healthy lifestyle.
Our paper presents some limitations. Firstly, the low number of enrolled patients and the single-centre design of our study could limit the generalizability of the study. Furthermore, some subgroups (i.e. females, obese patients, diabetics) presented a low number of subjects. This sample size could limit our power to detect important associations or findings. Regarding obese patients, we did not registered weight change during CR, thus limiting our possibility to understand if subjects that lost weight had the greater gain in functional capacity. However, as already stated, weight loss is often a process longer than CR period. Furthermore, we did not collect HR during stress test or CR, limiting our power to detect if also this variable (i.e. the dynamic HR response to exercise) could be a significant predictor of functional capacity and improvement. Finally, although six-minute walk test is frequently used in cardiac rehabilitation [35], most of the studies concerning patients with coronary artery disease used other tools to measure exercise capacity and functional improvement, such as Metabolic Equivalents (METs) [7, 10, 13, 36] and maximum oxygen consumption (VO2max) [11, 19]; instead, in other types of cardiological populations, such as patients with heart failure, functional capacity is typically estimated by the distance travelled during a walking test [37]. It is easy to understand that the determination and the evaluation of the same functional parameter could lead to difficult comparisons and interpretations when using different tools.
Conclusions
In conclusion, our study showed that the determinants of exercise capacity were age, BMI and HR, whereas determinants of functional improvement in patients undergoing CR were age, sex and BMI. Therefore, determinants of functional improvement are not cardiological variables; they are intrinsic factors, both modifiable factors (BMI) and non-modifiable factors (age and sex).
These results suggest that a diversified or an intensified CR should be programmed for elderly, females or obese patients. However, how this could be translated into clinical practice is a matter of debate and focused studies are needed to answer these questions.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Funding
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement. This work was supported by the Italian Ministry of University and Research (MIUR)—Department of Excellence project PREMIA (PREcision MedIcine Approach: bringing biomarker research to clinic) and by the A. De Gasperis Cardiology and Cardiac Surgery Foundation.
Conflict of interest
The authors declares that there is no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the Institution involved.
Consent to participate
All participants provided informed written consent after being informed of its nature and purpose.
Consent for publication
Not applicable.
Availability of data and materials
On request to corresponding author.
Code availability
On request to corresponding author.
References
- 1.Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37(29):2315–2381. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conte M, Rozza F, Fucile I, D'Avino G, Sorvillo G, De Luca N, et al. Low awareness of cardiovascular risk factor among patients admitted in cardiac rehabilitation unit. High Blood Press Cardiovasc Prev. 2021;28(3):321–324. doi: 10.1007/s40292-021-00444-y. [DOI] [PubMed] [Google Scholar]
- 3.Greco A, Brugnera A, Adorni R, D'Addario M, Fattirolli F, Franzelli C, et al. Protein intake and physical activity in newly diagnosed patients with acute coronary syndrome: a 5-year longitudinal study. Nutrients. 2021;13(2):634. doi: 10.3390/nu13020634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salzwedel A, Jensen K, Rauch B, Doherty P, Metzendorf MI, Hackbusch M, et al. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: update of the Cardiac Rehabilitation Outcome Study (CROS-II) Eur J Prev Cardiol. 2020;27(16):1756–1774. doi: 10.1177/2047487320905719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bargehr J, Thomas CS, Oken KR, Thomas RJ, Lopez-Jimenez F, Trejo-Gutierrez JF. Predictors of suboptimal gain in exercise capacity after cardiac rehabilitation. Am J Cardiol. 2017;119(5):687–691. doi: 10.1016/j.amjcard.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Gaede-Illig C, Limbourg T, Jannowitz CVH. Predictors of exercise capacity improvement in patients after an acute coronary event during inpatient rehabilitation. Rehabilitation. 2014;53(5):341–345. doi: 10.1055/s-0034-1370983. [DOI] [PubMed] [Google Scholar]
- 7.Lavie CJMR. Patients with high baseline exercise capacity benefit from cardiac rehabilitation and exercise training programs. Am Heart J. 1994;128(6):1105–1109. doi: 10.1016/0002-8703(94)90740-4. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki Y, Ito K, Yamamoto K, Fukui N, Yanagi H, Kitagaki K, et al. Predictors of improvements in exercise capacity during cardiac rehabilitation in the recovery phase after coronary artery bypass graft surgery versus acute myocardial infarction. Heart Vessels. 2018;33(4):358–366. doi: 10.1007/s00380-017-1076-2. [DOI] [PubMed] [Google Scholar]
- 9.Lavie CJ, Milani RV. Effects of cardiac rehabilitation, exercise training, and weight reduction on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in obese coronary patients. Am J Cardiol. 1997;79(4):397–401. doi: 10.1016/S0002-9149(97)89239-9. [DOI] [PubMed] [Google Scholar]
- 10.Clair MS, Mehta H, Sacrinty M, Johnson DRK. Effects of cardiac rehabilitation in diabetic patients: both cardiac and noncardiac factors determine improvement in exercise capacity. Clin Cardiol. 2014;37(4):233–238. doi: 10.1002/clc.22245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ades PAGM. Cardiopulmonary exercise testing before and after conditioning in older coronary patients. Am Heart J. 1990;120(3):585–589. doi: 10.1016/0002-8703(90)90015-P. [DOI] [PubMed] [Google Scholar]
- 12.Peretti A, Maloberti A, Garatti L, Palazzini M, Triglione N, Occhi L, et al. Functional improvement after outpatient cardiac rehabilitation in acute coronary syndrome patients is not related to improvement in left ventricular ejection fraction. High Blood Press Cardiovasc Prev. 2020;27:225–230. doi: 10.1007/s40292-020-00374-1. [DOI] [PubMed] [Google Scholar]
- 13.Shiran A, Kornfeld S, Zur S, Laor A, Yafa K, Militianu A, Merdler ALB. Determinants of improvement in exercise capacity in patients undergoing cardiac rehabilitation. Cardiology. 1997;88(2):207–213. doi: 10.1159/000177331. [DOI] [PubMed] [Google Scholar]
- 14.Crapo RO, Enright PLZR. ATS statement: guidelines for the six- minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 15.Issues S, Test MW, Equipment R, Preparation P. ATS statement: guidelines for the six-minute walk test. Am Thorac Soc. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 16.Vigorito C, Abreu A, Ambrosetti M, Belardinelli R, Corrà U, Cupples M, et al. Frailty and cardiac rehabilitation: a call to action from the EAPC cardiac rehabilitation section. Eur J Prev Cardiol. 2017;24(6):577–590. doi: 10.1177/2047487316682579. [DOI] [PubMed] [Google Scholar]
- 17.Pratesi A, Baldasseroni S, Burgisser C, Orso F, Barucci R, Silverii MV, et al. Long-term functional outcomes after cardiac rehabilitation in older patients. Data from the Cardiac Rehabilitation in Advanced aGE: EXercise TRaining and Active follow-up (CR-AGE EXTRA) randomised study. Eur J Prev Cardiol. 2019;26(14):1470–1478. doi: 10.1177/2047487319854141. [DOI] [PubMed] [Google Scholar]
- 18.Spence JD, Pilote L. Importance of sex and gender in atherosclerosis and cardiovascular disease. Atherosclerosis. 2015;241(1):208–210. doi: 10.1016/j.atherosclerosis.2015.04.806. [DOI] [PubMed] [Google Scholar]
- 19.Ades PA, Waldmann ML, Polk DM. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. Am J Cardiol. 1992;69(17):1422–1425. doi: 10.1016/0002-9149(92)90894-5. [DOI] [PubMed] [Google Scholar]
- 20.Calabrò P, Niccoli G, Gragnano F, Grove EL, Vergallo R, Mikhailidis DP, Patti G, Working Group of Interventional Cardiology of the Italian Society of Cardiology et al. Are we ready for a gender-specific approach in interventional cardiology? Int J Cardiol. 2019;286:226–233. doi: 10.1016/j.ijcard.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 21.Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation. 2016;133(9):916–947. doi: 10.1161/CIR.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 22.Dsc KHH, Investigators G-P. Sex-related differences in access to care among patients with premature acute coronary syndrome. CMAJ. 2014;186(7):497–504. doi: 10.1503/cmaj.131450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spirito A, Gragnano F, Corpataux N, Vaisnora L, Galea R, Svab S, Gargiulo G, et al. Sex-based differences in bleeding risk after percutaneous coronary intervention and implications for the academic research consortium high bleeding risk criteria. J Am Heart Assoc. 2021;10(12):e021965. doi: 10.1161/JAHA.121.021965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.El-Missiri AM, Awadalla HM, Almoudi MM. Gender differences among ischemic heart disease patients enrolled in a cardiac rehabilitation program. Egypt Heart J. 2020;72(1):15. doi: 10.1186/s43044-020-00052-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Forsyth F, Deaton C. Women and cardiac rehabilitation: moving beyond barriers to solutions? Eur J Prev Cardiol. 2020:2047487320911843. [DOI] [PubMed]
- 26.Hammond HK, Kelly TL, Froelicher VF, Pewen W. Use of clinical data in predicting improvement in exercise capacity after cardiac rehabilitation. J Am Coll Cardiol. 1985;6(1):19–26. doi: 10.1016/S0735-1097(85)80246-1. [DOI] [PubMed] [Google Scholar]
- 27.Marian MEM, et al. Timolol-induced reduction in mortality and reinfarction in patients surviving acute myocardial infarction. N Engl J Med. 1974;306(13):802–805. doi: 10.1056/NEJM198104023041401. [DOI] [PubMed] [Google Scholar]
- 28.Freemantle N, Cleland J, Young P, Mason J, Harrison J. β Blockade after myocardial infarction: systematic review and meta regression analysis. Br Med J. 1999;318(7200):1730–1737. doi: 10.1136/bmj.318.7200.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steg PG, Ferrari R, Ford I, Greenlaw N, Tardif JC, Tendera M, et al. Heart rate and use of beta-blockers in stable outpatients with coronary artery disease. PLoS ONE. 2012;7(5):1–8. doi: 10.1371/journal.pone.0036284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Casale R, Symeonidou Z, Michail X. Improvement of exercise capacity in patients with type 2 diabetes mellitus during cardiac rehabilitation. Eur J Phys Rehabil Med. 2018;54(6):980–981. [Google Scholar]
- 31.Leonardi S, Gragnano F, Carrara G, Gargiulo G, Frigoli E, Vranckx P, Di Maio D, et al. Prognostic implications of declining hemoglobin content in patients hospitalized with acute coronary syndromes. J Am Coll Cardiol. 2021;77(4):375–388. doi: 10.1016/j.jacc.2020.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bellotto F, Palmisano P, Compostella L, Russo N, Zaccaria M, Guida P, Setzu T, Cati A, Maddalozzo A, Favale S, Iliceto S. Anemia does not preclude increments in cardiac performance during a short period of intensive, exercise-based cardiac rehabilitation. Eur J Cardiovasc Prev Rehabil. 2011;18(2):150–157. doi: 10.1177/1741826710389372. [DOI] [PubMed] [Google Scholar]
- 33.Tramarin R, Pistuddi V, Maresca L, Pavesi M, Castelvecchio S, Menicanti L, de Vincentiis C, Ranucci M, Surgical and Clinical Outcome Research (SCORE) Group Patterns and determinants of functional and absolute iron deficiency in patients undergoing cardiac rehabilitation following heart surgery. Eur J Prev Cardiol. 2017;24(8):799–807. doi: 10.1177/2047487317689975. [DOI] [PubMed] [Google Scholar]
- 34.Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, et al. Exercise-based cardiac rehabilitation for coronary heart disease cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67(1):1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 35.Harris KM, Anderson DR, Landers JDEC. Utility of walk tests in evaluating functional status among participants in an outpatient cardiac rehabilitation program. J Cardiopulm Rehabil Prev. 2017;37(5):329–333. doi: 10.1097/HCR.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 36.Lavie CJ, Milani RV. Effects of cardiac rehabilitation and exercise training on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in women. Am J Cardiol. 1995;75(5):340–343. doi: 10.1016/S0002-9149(99)80550-5. [DOI] [PubMed] [Google Scholar]
- 37.Sutherland N, Harrison A, Doherty P. Factors influencing change in walking ability in patients with heart failure undergoing exercise-based cardiac rehabilitation. Int J Cardiol. 2018;268:162–165. doi: 10.1016/j.ijcard.2018.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
On request to corresponding author.