Abstract
Lifestyle improvement is a cornerstone of cardiovascular disease prevention and has a relevant effect on blood pressure control. During the last decades the attention of the researcher has focused on low-salt diets as the lifestyle modification most effective in blood pressure reduction. Current international guidelines thus suggest to stress the importance of the implementation of the dietary approach to stop hypertension (DASH) diet and of a low-salt Mediterranean diet to achieve the best results in term of blood pressure decrease. However, salt reduction in diet could be not the only nor the main determinant of blood pressure reduction under dietary treatment. DASH and low-salt Mediterranean diet are also characterized by a high intake of vegetables (NO and polyphenol sources), whole grains, some low-fat dairy products, and low intake of red meat, sugar, and trans-hydrogenated fats. Lacto-ovo vegetarian diet are also per se associated to a significant improvement in blood pressure levels. Moreover, these diets are particularly effective when associated with a significant weight loss. Furthermore, blood pressure can also be lowered by some nutraceuticals (beetroot, magnesium, vitamin C, catechin-rich beverages, lycopene, etc). The aim of this narrative review is to critically resume the most recent evidence supporting a complete approach to dietary counseling for hypertension prevention and management.
Keywords: Diet, Blood pressure, Dietary supplements, Hypertension, Lifestyle
Introduction
Lifestyle improvement is a cornerstone of cardiovascular disease prevention and diet is one of the most effective strategy for attaining on blood pressure (BP) reduction and control [1].
During the last decades the attention of the researcher has focused on low-salt diets as the most effective lifestyle modification in BP reduction. In fact, from an epidemiological point of view is known that a daily intake of sodium > 5 g is associated with a proportional increase in systolic BP, both in children [2] and in adults [3], whereas it has been estimated (but not proven) that daily intake > 2 gr is associated to more than 1 of every 10 deaths from cardiovascular causes [4].
This could be mainly due to the fact that dietary sodium restriction has a significant BP-lowering effect. A very recent and huge meta-analysis of 85 trials, mainly carried out on hypertensive patients, with sodium intake ranging from 0.4 to 7.6 g/day and follow-up from 4 weeks to 36 months, showed an approximately linear relationship between sodium intake and increase in both systolic and diastolic BP across the entire range of dietary sodium exposure [5]. Another meta-analysis of 17 cohorts with 457 participants showed that salt restriction was associated with a significant reduction in augmentation index (9.3%) as well as central systolic BP and central pulse pressure [6]. Then, an average reduction in sodium intake of 89.3 mmol/day was associated with a 2.84% (95% CI 0.51–5.08) reduction in carotid-femoral pulse wave velocity [7].
On the other side, quick dietary sodium restriction has been associated with significant increase in serum renin, noradrenalin, adrenalin, and heart rate, and a mild but significant impairment in plasma lipid levels [8, 9]. For these reason, and in order to consent the patient adapation to the lower food sapidity, at the stage of hypertension diagnosis a mild and progressive reduction of salt intake should be suggested in spite of a quick and dramatic cut of salt assumption. The antihypertensive effect of sodium restriction is more pronounced in people of African descent, in older patients, and patients with diabetes, metabolic syndrome, or chronic kidney disease [10], but less pronounced in young overall health caucasians. Moreover, salt restriction could not be always easy, as often it is hidden in processed foods. Finally, it is not so evident that long-term dietary sodium restriction is associated to a significant reduction in cardiovascular disease risk [11].
In this context, there is a growing interest for implementation of whole dietary patterns or single nutrients other than sodium and nutraceuticals potentially improving BP control
Dietary Patterns Improving Blood Pressure Control
Different dietary pattern have proven an effective BP lowering effect (Fig. 1).
The dietary approach to stop hypertension (DASH) diet
Fig. 1.
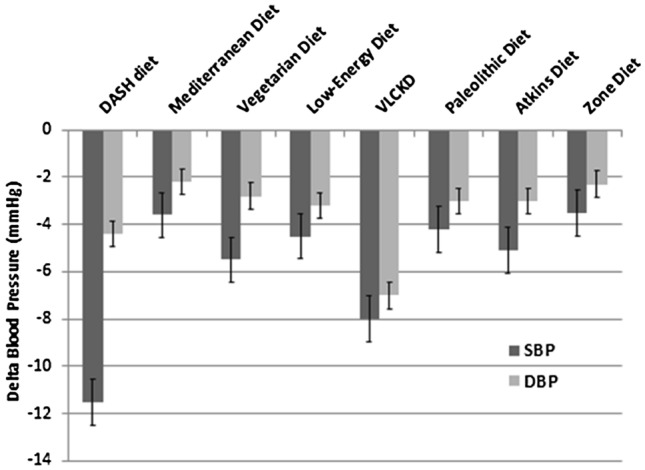
Mean (SEM) effect of different dietary pattern on BP levels from the most recent metanalyses of trials carried out on hypertensive subjects (derived by Ref. [1])
The DASH diet is an overall healthy low-salt diet high intake of vegetables, whole grains, some low-fat dairy products, and low intake of red meat, sugar, and trans-hydrogenated fats, when compared to a standard Western diet [12].
Compared to the typical North-American diet, the DASH one is associated with lower systolic BP independently from the sodium intake and with lower diastolic BP in subjects with intermediate-high sodium intake: the mean systolic BP falled by 7.1 mmHg in normotensive subjects, and by 11.5 mmHg in hypertensive patients [13].
A recent meta-analysis of 17 trials showed a significant preventive effect of DASH diet on mortality for different causes with hazard rations 0.95 (95% CI 0.94–0.96, I2 = 91.6%) for all-cause, 0.96 (95% CI 0.95–0.98, I2 = 82.4%) for cardiovascular diseases, 0.97 (95% CI 0.96–0.98, I2 = 0.00%) for stroke, and 0.97 (95% CI 0.95–0.98, I2 = 63.7%) for cancer mortality per each 5-point increment of adherence to the DASH diet [14]. DASH diet would also reduce the risk to develop type 2 diabetes (RR = 0.82; 95% CI 0.74–0.92) [15].
The Mediterranean diet
The Mediterranean diet is based on the traditional dietary pattern of old Greece and southern Italy, being rich in fruits, vegetables, legumes, cereals, dairy products (cheese, yogurt), fish, olive oil, and with small amount of wine and lean meats. The main differences with the DASH diet is related to the attention to the seasonality of fresh foods, the large number of polyphenos containing foods (in particular olives and extravirgin olive oil) and the use of vegetable oils in spite of animal oils, when compared with other traditional diets [16]. The Mediterranean diet has a less significant impact on BP than DASH-diet, probably because it is not strictly a low-salt diet. Another reason is related to the fact that a part of the available trials compared the effect of high adherence to low adherence to Mediterranean diet in Mediterranean countries (in particular Italy and Spain) where the low adherence is represented by a dietary pattern that is always healthier than the one in North-Europe or North-America [17]. This attenuate the measured effect of Mediterranean diet on BP. A recent umbrella meta-analysis of 57 trials involving 36,983 participants concluded that adherence to the Mediterranean diet is able to improve anthropometric measurements, BP, insulin-resistance, lipid pattern, liver transaminases and hepatic fat mass, systemic inflammation, flow-mediated dilatation and the risk of cardiovascular disease incidence (risk ratio = 0.61, 95% CI 0.42–0.80; I2 = 0%), and stroke (risk ratio = 0.67, 95% CI 0.35–0.98; I2 = 0%) [18]. However, the available evidence suggest that Mediterranean diet is associated to a mildly reduced risk of cardiovascular disease both in primary and secondary prevention setting, but the quality of the evidence is not so good and a definitive conclusion can not be currently drawn [19]. One more time, a part of the available trials compared the effect of high adherence to low adherence to Mediterranean diet in Mediterranean countries where the low adherence is represented by a dietary pattern that is always healthier than the one in North-Europe or North-America and where the baseline cardiovascular risk is meanly low, so that a risk reduction is less easily detectable. On the other side, adherence to the Mediterranean diet is associated to improved a significant reduction in the risk of all-cause mortality (relative risk for the study-specific highest/lowest and per 1sd MDS increment 0.79 (95% CI 0.77, 0.81, Ι2 = 42%) and 0.92 (95% CI 0.90, 0.94, Ι2 = 56 %), respectively) [20].
Vegetarian and vegan diets
A huge meta-analysis of long-term studies (n = 118,518; 2,936,359 person-years of follow-up) showed a positive association between meat (including poultry) and risk to develop hypertension, independently from fruit, vegetable, and whole grain intake [21]. On the contrary, a recent meta-analysis of 41 clinical trials (8416 participants) comparing different plant-based diet showed that lacto-ovo vegetarian diet has a significant BP effect lowering effect, while vegan not (systolic BP: − 5.47 mmHg (95% CI − 7.60, − 3.34) vs. 1.30 mmHg (95% CI − 3.90, 1.29). Similar effects were seen on diastolic BP, as well [22]. Vegetarian diets are also protective against the development of type 2 diabetes: odds ratio for diabetes in vegetarians vs. non-vegetarians was 0.73 (95% CI 0.61, 0.88) [23].
Vegetarian diets are associated with reduced risk of all-cause mortality, and in particular of mortality due to cardiovascular (0.92, 95% CI 0.85, 0.99; I2 = 0%) and coronary artery disease (0.76; 95% CI 0.68, 0.85; I2 = 35%) [24]. It has yet to be fully elucidated which subtype of vegetarian diet (vegan, lacto-vegetarian, lacto-ovo vegetarian, pesco-vegetarian) could have the best BP lowering and cardiovascular disease prevention effect.
On the other side, the vegetarian and vegan diet-related deficit of vitamin B12 intake could reduce their potential positive impact on cardiovascular disease prevention [25]. Then, compared with omnivores, vegetarians and vegans had lower BMD at the femoral neck and lumbar spine and vegans also had higher fracture rates [26]. Moreover, vegetarians show higher depression scores than non-vegetarians [27].
Low-energy diets
Increased body weight and obesity are the independent risk factors for hypertension [28].
A meta-analysis of 8 clinical trials involving 2100 patients showed a significant BP reduction in participants assigned to weight-loss diets as compared to controls: systolic BP: mean difference (MD) − 4.5 mm Hg (95% CI − 7.2 to − 1.8 mm Hg), and diastolic BP: MD − 3.2 mm Hg (95% CI − 4.8 to − 1.5 mm Hg) [29]. A further metanalysis showed that body weight loss is also associated to a significant reduction in heart rate (− 9 beats/min, 95% CI − 12 to − 6; p < 0.001), resting oxygen consumption (− 85 ml/min, 95% CI − 111 to − 60; p < 0.001) and mean pulmonary artery pressure (− 5 mm Hg, 95% CI − 8 to − 2; p = 0.001) [30].
Energy restriction could be obtained in different ways. In general, caloric restriction can lower both systolic BP and diastolic BP regardless of sex, ethnic group, BMI, presence of metabolic syndrome, or diabetes mellitus. BP-lowering effect may continue beyond the end of the fasting period. The greatest decrease takes place in patients with the highest baseline BP [31].
Alternate-day fasting has an increased popularity and is associated with an improvement of anthropometric measurements, glucose metabolism, lipid pattern and blood pressure [32].
Very low charbohydrate ketogenic diets (VLCKD) are associated with a quick and impressive reduction in body weight and BP (systolic BP − 8 mmHg, diastolic BP − 7 mmHg) [33]. The available studies are relatively short, but the most part of VLCKD protocols are of short duration and aim to train the subjects to a more healthy and balanced diet after some months of energy restriction. This approach could be more indicated in obese subjects resistant to previous dietary approaches [34].
Low-energy diets have been mainly tested in overweight-obese patients, so that it is not yet clear their potentially efficacy in lean hypertensive subjects, in particular when affected by insulin-resistance.
Other dietary patterns
Paleolithic type diet (nutrition of preagricultural hunter-gatherers including lean meat, fruits, vegetables, and nuts, while avoiding intake of grains, dairy products, processed foods, and added sugar and salt) led to the significant improvement of both systolic (WMD = − 4.24 mm Hg; 95% CI − 7.11, − 1.38 mm Hg) and diastolic (WMD = − 2.95 mm Hg; 95% CI − 4.72, − 1.18 mm Hg) BP, without relevant impact on body weight [35].
Among other popular diets, the Atkins (systolic BP—5.1 mm Hg, diastolic BP—3.3 mm Hg) and the Zone (systolic BP 3.5 mm Hg, and diastolic BP—2.3 mm Hg) also exerted a significant BP reduction effects [36]. Both diets are associated with body weight loss and have not studied on the long-term.
Nutraceuticals
Some single natural molecules are associated with a significant improvement in BP under controlled dietary conditions. In this context, recently, both the Italian [37] and the European Hypertension Societies [38] published statements related to the best available evidence of efficacy for some of them.
Both documents conclude that a sufficient clinical evidence of efficacy and safety exist for dietary supplementation with beetroot juice, magnesium, vitamin C, and catechin-rich beverages. Soy isoflavones could be suggested in perimenopausal women, resveratrol—in insulin-resistant patients, melatonin—in the subjects with noctural hypertension. Even if potassium is one of the most effective antihypertensive nutraceutical, warning on potassium intake is needed in patients with advanced chronic kidney failure and those assuming potassium-sparing diuretics/antialdosteronics. Pomegranate juice, karkadè tea and sesame effectiveness has been demonstrated in Middle-East people only [37, 38]. Lactotripeptides are effective only in Asian people [39], while polyunsaturated fatty acids from fish exert small effect on BP [40]. The possible additive effect of the combination of some of them is promising and under investigation [41].
Discussion
One of the first scientific attempt to manage heart failure and hypertension with diet is due to Kempner in the late 1930s. In fact he proposed to use a rice-based diet as a treatment for a patient with renal failure and congestive heart failure. He showed that this intervention led to the decrease of heart size according to the chest X-ray, normalization of ECG, and improvement of retinal conditions. Then, Kempner obtained similar results in ae cohort of hypertensive patients: rice and fruit diet helped them to significantly decrease their BP and heart size. Sadly, these findings did not receive enough attention from the scientific community [42].
The modern pre-pharmacological approach to prevention and management of hypertension should be multitarget, suggesting improvement of body weight, quality of diet and eventually inclusion of some dietary supplements.
The main international guidelines for the management of hypertension follows this approach (Table 1). Guidelines for the prevention, detection, evaluation, and management of high BP in adults, issued by American College of Cardiology/American Heart Association (2017) recommend a heart-healthy diet, that could be resumed in the DASH diet [43]. Guidelines for the management of arterial hypertension, issued by European Society of Cardiology/European Society of Hypertension (2018), support the suggestion of a low-salt Mediterranean-like diet [44]. On May 2020, the International Society of Hypertension issued Global Hypertension Practice Guidelines, which recommend a DASH-like diet, also highlighting the possible BP lowering effect of vegetables sources of nitrates like beetroot and leafy vegetables. Moreover, they also cited foods rich in calcium, magnesium, and potassium (avocados, nuts, seeds, legumes, and tofu) as having some antihypertensive benefits [45].
Table 1.
Nutritional recommendations of main guidelines on arterial hypertension
| Guidelines | Dietary recommendation |
|---|---|
| American College of Cardiology/American Heart Association (2017) | Low-salt diet high intake of vegetables, whole grains, some low-fat dairy products, and low intake of red meat, sugar, and trans-hydrogenated fats (DASH diet-like) |
| European Society of Cardiology/European Society of Hypertension (2018) | Healthy balanced diet containing vegetables, legumes, fresh fruits, low-fat dairy products, wholegrains, fish, and unsaturated fatty acids (especially olive oil); low consumption of red meat and saturated fatty acids (Mediterranean diet-like) |
| International Society of Hypertension (2020) | Diet rich in whole grains, fruits, vegetables (especially those sources of nitrates), low-fat dairy products, and foods rich in polyunsaturated fats (fish, nuts, seeds); low consumption of foods high in sugar, saturated fat and trans fats |
The dietary supplementation with beetroot juice, magnesium, vitamin C, and catechin-rich beverages could further improve BP control [46].
The antihypertensive effect observed with the above cited diet is sometime huge and similar to that achieved with the best pharmacological treatment, however the long-term compliance and consequently the long-term efficacy of these diet has yet to be rigorously quantified.
In conclusion, combining data derived by the available literature, we should propose a low-salt energy-restricted Mediterranean diet to the most part of our overweight hypertensive patients. In some cases (obese subjects apparently resistant to standard diets) VLCKD could be considered. Physical sactivity increase and smoking cessation should also always suggested [47]. This approach could prevent the use of antihypertensive drugs, reduce the dose or number of drugs employed, and improve the efficacy of the pharmacological treatment. Moreover, it would have a global positive impact on the cardiovascular risk profile both of patients in primary and secondary prevention for cardiovascular diseases.
Declarations
Funding
Open access funding provided by Alma Mater Studiorum -Università di Bologna within the CRUI-CARE Agreement.
Conflict of interest
No one.
Availability of data and material
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
References
- 1.Strilchuk L, Cincione RI, Fogacci F, Cicero AFG. Dietary interventions in blood pressure lowering: current evidence in 2020. Kardiol Pol. 2020;78(7–8):659–666. doi: 10.33963/KP.15468. [DOI] [PubMed] [Google Scholar]
- 2.Rios-Leyvraz M, Bloetzer C, Chatelan A, Bochud M, Burnier M, Santschi V, Paradis G, Tabin R, Bovet P, Chiolero A. Sodium intake and blood pressure in children with clinical conditions: a systematic review with meta-analysis. J Clin Hypertens. 2019;21(1):118–126. doi: 10.1111/jch.13436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whelton PK. Dietary sodium intake: scientific basis for public policy. Blood Purif. 2015;39(1–3):16–20. doi: 10.1159/000368975. [DOI] [PubMed] [Google Scholar]
- 4.Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, Lim S, Danaei G, Ezzati M, Powles J, Global Burden of Diseases Nutrition and Chronic Diseases Expert Group Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371(7):624–634. doi: 10.1056/NEJMoa1304127. [DOI] [PubMed] [Google Scholar]
- 5.Filippini T, Malavolti M, Whelton PK, Naska A, Orsini N, Vinceti M. Blood pressure effects of sodium reduction: dose–response meta-analysis of experimental studies. Circulation. 2021;143(16):1542–1567. doi: 10.1161/CIRCULATIONAHA.120.050371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Elia L, La Fata E, Giaquinto A, Strazzullo P, Galletti F. Effect of dietary salt restriction on central blood pressure: a systematic review and meta-analysis of the intervention studies. J Clin Hypertens. 2020;22(5):814–825. doi: 10.1111/jch.13852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D'Elia L, Galletti F, La Fata E, Sabino P, Strazzullo P. Effect of dietary sodium restriction on arterial stiffness: systematic review and meta-analysis of the randomized controlled trials. J Hypertens. 2018;36(4):734–743. doi: 10.1097/HJH.0000000000001604. [DOI] [PubMed] [Google Scholar]
- 8.Graudal NA, Hubeck-Graudal T, Jürgens G. Reduced dietary sodium intake increases heart rate. a meta-analysis of 63 randomized controlled trials including 72 study populations. Front Physiol. 2016;7:111. doi: 10.3389/fphys.2016.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2020;12(12):CD004022. doi: 10.1002/14651858.CD004022.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev. 2013;4:CD004937. doi: 10.1002/14651858.CD004937.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Adler AJ, Taylor F, Martin N, Gottlieb S, Taylor RS, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;2014(12):CD009217. doi: 10.1002/14651858.CD009217.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 13.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, 3rd, Simons-Morton DG, Karanja N, Lin PH, DASH-Sodium Collaborative Research Group Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 14.Soltani S, Arablou T, Jayedi A, Salehi-Abargouei A. Adherence to the dietary approaches to stop hypertension (DASH) diet in relation to all-cause and cause-specific mortality: a systematic review and dose–response meta-analysis of prospective cohort studies. Nutr J. 2020;19(1):37. doi: 10.1186/s12937-020-00554-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiavaroli L, Viguiliouk E, Nishi SK, Blanco Mejia S, Rahelić D, Kahleová H, Salas-Salvadó J, Kendall CW, Sievenpiper JL. DASH dietary pattern and cardiometabolic outcomes: an umbrella review of systematic reviews and meta-analyses. Nutrients. 2019;11(2):338. doi: 10.3390/nu11020338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, Trichopoulos D. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6 Suppl):1402S–1406S. doi: 10.1093/ajcn/61.6.1402S. [DOI] [PubMed] [Google Scholar]
- 17.Filippou CD, Thomopoulos CG, Kouremeti MM, Sotiropoulou LI, Nihoyannopoulos PI, Tousoulis DM, Tsioufis CP. Mediterranean diet and blood pressure reduction in adults with and without hypertension: a systematic review and meta-analysis of randomized controlled trials. Clin Nutr. 2021;40(5):3191–3200. doi: 10.1016/j.clnu.2021.01.030. [DOI] [PubMed] [Google Scholar]
- 18.Papadaki A, Nolen-Doerr E, Mantzoros CS. The effect of the Mediterranean diet on metabolic health: a systematic review and meta-analysis of controlled trials in adults. Nutrients. 2020;12(11):3342. doi: 10.3390/nu12113342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rees K, Takeda A, Martin N, Ellis L, Wijesekara D, Vepa A, Das A, Hartley L, Stranges S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2019;3(3):CD009825. doi: 10.1002/14651858.CD009825.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eleftheriou D, Benetou V, Trichopoulou A, La Vecchia C, Bamia C. Mediterranean diet and its components in relation to all-cause mortality: meta-analysis. Br J Nutr. 2018;120(10):1081–1097. doi: 10.1017/S0007114518002593. [DOI] [PubMed] [Google Scholar]
- 21.Borgi L, Curhan GC, Willett WC, Hu FB, Satija A, Forman JP. Long-term intake of animal flesh and risk of developing hypertension in three prospective cohort studies. J Hypertens. 2015;33(11):2231–2238. doi: 10.1097/HJH.0000000000000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gibbs J, Gaskin E, Ji C, Miller MA, Cappuccio FP. The effect of plant-based dietary patterns on blood pressure: a systematic review and meta-analysis of controlled intervention trials. J Hypertens. 2021;39(1):23–37. doi: 10.1097/HJH.0000000000002604. [DOI] [PubMed] [Google Scholar]
- 23.Lee Y, Park K. Adherence to a vegetarian diet and diabetes risk: a systematic review and meta-analysis of observational studies. Nutrients. 2017;9(6):603. doi: 10.3390/nu9060603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jafari S, Hezaveh E, Jalilpiran Y, Jayedi A, Wong A, Safaiyan A, Barzegar A. Plant-based diets and risk of disease mortality: a systematic review and meta-analysis of cohort studies. Crit Rev Food Sci Nutr. 2021 doi: 10.1080/10408398.2021.1918628. [DOI] [PubMed] [Google Scholar]
- 25.Pawlak R. Is vitamin B12 deficiency a risk factor for cardiovascular disease in vegetarians? Am J Prev Med. 2015;48(6):e11–26. doi: 10.1016/j.amepre.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 26.Iguacel I, Miguel-Berges ML, Gómez-Bruton A, Moreno LA, Julián C. Veganism, vegetarianism, bone mineral density, and fracture risk: a systematic review and meta-analysis. Nutr Rev. 2019;77(1):1–18. doi: 10.1093/nutrit/nuy045. [DOI] [PubMed] [Google Scholar]
- 27.Ocklenburg S, Borawski J. Vegetarian diet and depression scores: a meta-analysis. J Affect Disord. 2021;31(294):813–815. doi: 10.1016/j.jad.2021.07.098. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. Obesity and overweight. Fact sheet. 2018. https://www.who.int/mediacentre/factsheets/fs311/en/.
- 29.Semlitsch T, Krenn C, Jeitler K, Berghold A, Horvath K, Siebenhofer A. Long-term effects of weight-reducing diets in people with hypertension. Cochrane Database Syst Rev. 2021;2(2):CD008274. doi: 10.1002/14651858.CD008274.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reddy YNV, Anantha-Narayanan M, Obokata M, Koepp KE, Erwin P, Carter RE, Borlaug BA. Hemodynamic effects of weight loss in obesity: a systematic review and meta-analysis. JACC Heart Fail. 2019;7(8):678–687. doi: 10.1016/j.jchf.2019.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nicoll R, Henein MY. Caloric restriction and its effect on blood pressure, heart rate variability and arterial stiffness and dilatation: a review of the evidence. Int J Mol Sci. 2018;19(3):751. doi: 10.3390/ijms19030751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cui Y, Cai T, Zhou Z, Mu Y, Lu Y, Gao Z, Wu J, Zhang Y. Health effects of alternate-day fasting in adults: a systematic review and meta-analysis. Front Nutr. 2020;7:586036. doi: 10.3389/fnut.2020.586036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Castellana M, Conte E, Cignarelli A, Perrini S, Giustina A, Giovanella L, Giorgino F, Trimboli P. Efficacy and safety of very low calorie ketogenic diet (VLCKD) in patients with overweight and obesity: a systematic review and meta-analysis. Rev Endocr Metab Disord. 2020;21(1):5–16. doi: 10.1007/s11154-019-09514-y. [DOI] [PubMed] [Google Scholar]
- 34.Caprio M, Infante M, Moriconi E, Armani A, Fabbri A, Mantovani G, Mariani S, Lubrano C, Poggiogalle E, Migliaccio S, Donini LM, Basciani S, Cignarelli A, Conte E, Ceccarini G, Bogazzi F, Cimino L, Condorelli RA, La Vignera S, Calogero AE, Gambineri A, Vignozzi L, Prodam F, Aimaretti G, Linsalata G, Buralli S, Monzani F, Aversa A, Vettor R, Santini F, Vitti P, Gnessi L, Pagotto U, Giorgino F, Colao A, Lenzi A, Cardiovascular Endocrinology Club of the Italian Society of Endocrinology Very-low-calorie ketogenic diet (VLCKD) in the management of metabolic diseases: systematic review and consensus statement from the Italian Society of Endocrinology (SIE) J Endocrinol Invest. 2019;42(11):1365–1386. doi: 10.1007/s40618-019-01061-2. [DOI] [PubMed] [Google Scholar]
- 35.Ghaedi E, Mohammadi M, Mohammadi H, Ramezani-Jolfaie N, Malekzadeh J, Hosseinzadeh M, Salehi-Abargouei A. Effects of a paleolithic diet on cardiovascular disease risk factors: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2019;10(4):634–646. doi: 10.1093/advances/nmz007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ge L, Sadeghirad B, Ball GDC, da Costa BR, Hitchcock CL, Svendrovski A, Kiflen R, Quadri K, Kwon HY, Karamouzian M, Adams-Webber T, Ahmed W, Damanhoury S, Zeraatkar D, Nikolakopoulou A, Tsuyuki RT, Tian J, Yang K, Guyatt GH, Johnston BC. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ. 2020;369:m696. doi: 10.1136/bmj.m696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cicero AFG, Grassi D, Tocci G, Galletti F, Borghi C, Ferri C. Nutrients and nutraceuticals for the management of high normal blood pressure: an evidence-based consensus document. High Blood Press Cardiovasc Prev. 2019;26(1):9–25. doi: 10.1007/s40292-018-0296-6. [DOI] [PubMed] [Google Scholar]
- 38.Borghi C, Tsioufis K, Agabiti-Rosei E, Burnier M, Cicero AFG, Clement D, Coca A, Desideri G, Grassi G, Lovic D, Lurbe E, Kahan T, Kreutz R, Jelakovic B, Polonia J, Redon J, Van De Borne P, Mancia G. Nutraceuticals and blood pressure control: a European Society of Hypertension position document. J Hypertens. 2020;38(5):799–812. doi: 10.1097/HJH.0000000000002353. [DOI] [PubMed] [Google Scholar]
- 39.Cicero AF, Gerocarni B, Laghi L, Borghi C. Blood pressure lowering effect of lactotripeptides assumed as functional foods: a meta-analysis of current available clinical trials. J Hum Hypertens. 2011;25(7):425–436. doi: 10.1038/jhh.2010.85. [DOI] [PubMed] [Google Scholar]
- 40.Cicero AF, Ertek S, Borghi C. Omega-3 polyunsaturated fatty acids: their potential role in blood pressure prevention and management. Curr Vasc Pharmacol. 2009;7(3):330–337. doi: 10.2174/157016109788340659. [DOI] [PubMed] [Google Scholar]
- 41.Cicero AFG, Colletti A, Fogacci F, Bove M, Giovannini M, Borghi C. Is it possible to significantly modify blood pressure with a combined nutraceutical on top of a healthy diet? The results of a pilot clinical trial. High Blood Press Cardiovasc Prev. 2018;25(4):401–405. doi: 10.1007/s40292-018-0289-5. [DOI] [PubMed] [Google Scholar]
- 42.Klemmer P, Grim CE, Luft FC. Who and what drove Walter Kempner? The rice diet revisited. Hypertension. 2014;64(4):684–688. doi: 10.1161/HYPERTENSIONAHA.114.03946. [DOI] [PubMed] [Google Scholar]
- 43.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Sr, Williamson JD, Wright JT., Jr 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71(6):1269–1324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 44.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, ESC Scientific Document Group 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 45.Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M, Wainford RD, Williams B, Schutte AE. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–1357. doi: 10.1161/HYPERTENSIONAHA.120.15026. [DOI] [PubMed] [Google Scholar]
- 46.Borghi C, Cicero AF. Nutraceuticals with a clinically detectable blood pressure-lowering effect: a review of available randomized clinical trials and their meta-analyses. Br J Clin Pharmacol. 2017;83(1):163–171. doi: 10.1111/bcp.12902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cicero AFG, Fogacci F, Colletti A. Food and plant bioactives for reducing cardiometabolic disease risk: an evidence based approach. Food Funct. 2017;8(6):2076–2088. doi: 10.1039/c7fo00178a. [DOI] [PubMed] [Google Scholar]


