Abstract
Burnout is a response to sustained job stressors manifesting as a classic triad of emotional exhaustion, depersonalization, and a sense of reduced accomplishment. With 42% of physicians demonstrating some symptoms of burnout, this has already reached epidemic proportions. The COVID-19 pandemic has only worsened this phenomenon.
Physician burnout has physical and professional consequences which result in suboptimal patient health outcomes and increased healthcare costs. In response to the landmark report in 1999 from the National Academy of Medicine, ‘To Err is Human: Building a Safer Health System which focused on patient safety and wellbeing’, significant efforts and resources were directed in preventing these errors, making patient safety and quality care a priority.1 However, this needs to be priortized along with the well being of medical caregivers.
Caring for children and their families is the intrinsic motivation and primary driver for most child health clinicians. However, this has been eroded by the gradual conversion of the ‘art of medicine’ into a business associated with numerous regulatory, financial, and legal burdens. This evolution of medical practice has also stripped away the three pillars of intrinsic motivation: autonomy, competence, and relatedness. As Gagne and Deci very aptly stated: “In a misguided attempt to improve the medical system, health care reformers put into place various positive and negative extrinsic motivators, without realizing that they would actually erode and destroy intrinsic motivation, eventually leading to ‘amotivation’ — in other words, burnout.”2
This paper reviews the definition, causes, consequences and mitigation methods for this burnout epidemic. While burnout has been reported among all members of the care team, physician burnout has been the focus of most studies in this area.
Introduction
In recent years, numerous studies have shown that delivering safe, patient-centered, high-quality, and high-value health care requires a clinical workforce that is functioning at the highest level.3 However, two events threaten the well-being of our clinical workforce: COVID-19, the greatest infectious pandemic of the modern age – one which has revealed fundamental weaknesses in our healthcare system; and second, an epidemic of our own making – physician burnout. Rates of physician burnout have been at critical levels over the last few years, with the most recent annual Medscape survey finding 42% of physicians self-reported that they were burned out.4
Definition
Burnout is defined as a response to occupational stress associated with a classic triad of emotional exhaustion, depersonalization, and a sense of reduced accomplishment, which negatively impacts the physician's health, productivity and hence patient care.5 , 6 The Maslach Burnout Inventory (MBI), which uses 22 symptom questions to assess these three aspects of burnout, has long been considered the gold standard, but other simplified versions of this and other tools have been used.81 Recently, Li Sauerwine et al. found that a 2-question summative score correlated well with the score of the full inventory.7
Burnout is now recognized as a medical disorder, according to the International Classification of Diseases 10th Edition (ICD-10), associated with code Z73.0 (Burn-out state of vital exhaustion).
Burnout is often described as a chronic condition where perceived demands outweigh perceived resources.8 The strongest indicator of burnout is emotional exhaustion, which refers to feelings of being overextended and depleted of one's emotional and physical resources.9 Depersonalization is an indifferent detached attitude that manifests as cynical behaviors towards patients and their families, treating them as objects rather than human beings and a lack of empathy. This can make the demands of the job more manageable and can be another manifestation of emotional exhaustion. Reduced personal accomplishment implies feelings of incompetence and inefficiency in daily work. There is a tendency for negative self-appraisal and poor professional self-esteem. It is difficult to gain a sense of accomplishment when feeling exhausted or when helping people toward whom one is indifferent.10
Overall, burned out clinicians are frequently exhausted, angry, diminished in their ability to care, and feel as though their work makes little difference. The lack of efficacy arises from a lack of resources, whereas exhaustion and cynicism emerge from of work overload and lack of autonomy.11
Epidemiology
In a survey done by Medscape in 2021, 45% of pediatricians in the United States reported either experiencing symptoms of burnout/depression or complete burn out. This rate is consistent with pre-pandemic figures. 12% of pediatricians who were burned out admitted to suicidal thoughts and 1% of burned out or depressed pediatricians have made suicide attempts., which is similar percentage to physicians overall.12
In pediatrics, with the unique prevalence of women physicians, burnout rates are even higher; 64% of women pediatricians compared to 35% among all active physicians. Women physicians have consistently reported higher rates of burnout, often having the added responsibility for home and childcare.13
Moreover, an increasing number of students and postgraduate medical trainees are being affected as well. Data from medical students, residents and fellows when compared with population control samples have shown these groups to be more likely to exhibit symptoms of depression and both less likely to have suicidal ideation.14
Consequences
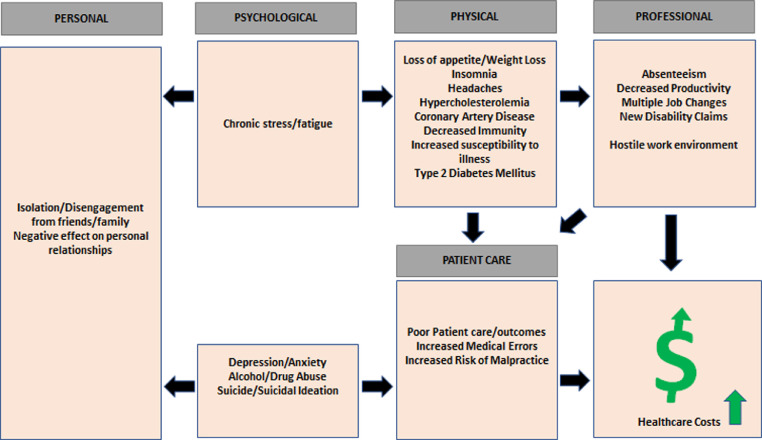
The consequences of clinician burnout can be far reaching. In addition to physical and psychological health, unaddressed burnout has both professional and patient care consequences. Clinicians suffering burnout are more likely to miss days at work, have decreased work hours, experience multiple job or specialty changes, and ultimately leave the profession altogether.15 Performance and productivity can both be negatively affected. Medical errors and patient safety events related to burnout can lead to poor patient outcomes and increased malpractice suits.16 The burned-out clinician often has negative interactions with co-workers, creating a hostile work environment and placing others at risk for burnout as well. All these factors together can drive up healthcare costs Fig. 1.17
Fig. 1.
Consequences of physician burnout.
Physical symptoms of burnout are varied, including headaches, insomnia, chronic gastrointestinal and respiratory problems, hypertension and heart disease.18 Depression and anxiety are not uncommon, as are alcohol and substance abuse and dependency. Physicians often do not seek help for mental health issues for fear of losing medical licensure and hospital credentialing, further driving up rates of self-medication.19
Suicide and suicidal ideation are more common in both genders as compared to the general population. However, in female physicians, the rate of completed suicide is 2.5–4 times higher than the general population, whereas attempted suicide rates are lower.
Alt-text: Unlabelled box
In male physicians, it is 1.41 times higher compared to males in the general population.20 (Figure)
Underlying causes
Part of the difficulty of preventing or treating burnout in physicians is that the underlying causes are diverse and include aspects central to our identity as physicians, how we relate to our colleagues, how we interact with our workplace environments, and the culture of medicine as a whole.
Organizational factors
The fact that nearly half of all U.S. physicians report symptoms of burnout suggests that this phenomenon has more to do with health care institutions and professional culture than it does personal characteristics of individual physicians. To this point, psychologist Christina Maslach, creator of the MBI, described
Burnout is not a problem of people, but of the social environment in which they work.
Alt-text: Unlabelled box
One of the more frequently identified factors in physician burnout is working long hours. Arigoni et al. found that doctors in Switzerland working over 50 h per week were at highest risk of having two of the three key features of burnout.22 Al-Dubai also found an association between burnout and working over 40 h per week.23 Beyond the total number of hours worked each week, the risk of burnout is significantly affected by the specific tasks being performed. Physicians who spent less than 20% of their time on the activity most meaningful to them had nearly double the rate of burnout.24
In the decade following enactment of the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009, health systems implemented electronic health record (EHR) systems at a rapid pace. While the benefits of widespread EHR adoption are numerous, there have been many unintended consequences. Medicine in the EHR era has led some clinicians to believe that they need to interact with the computer as much as, if not more than, the patient. This can ultimately compromise the patient-physician relationship.25 A time and motion study of ambulatory practice physicians found that physicians spent 53% of their time in the exam room directly interacting with their patients, but a noTable 37% on EHR and desk work.26 And the EHR responsibilities extend beyond the exam room, with Arndt et al. finding that during an average primary care physician day, over half of their time was spent on EHR tasks, including 1.4 h occurring outside of clinic hours. It has also been found that clinicians who self-reported burnout spent more time in the EHR after hours, as well as having lower rates of same day chart completion.27 , 28
Understanding why physicians dislike EHRs has been the subject of many opinion pieces, perhaps most notably Atul Gawande's New Yorker piece entitled tellingly “Why Doctors Hate Their Computers”.29 Some of these feelings are justified, but some may be displaced hostility resulting from factors unrelated to the EHR itself. In fact, implementations of an EHR from the same vendor, that in the US was viewed negatively, was met with satisfaction by clinicians in other countries who appreciated it as a tool to improve efficacy.30 This may be due to different demands and expectations for clinical documentation in those countries than in the US, where clinical notes are nearly four times longer on average than those in other countries. A recent study found that implementation of health information technology in hospitals in China did not increase stress but rather improved physicians’ feelings of meaning, autonomy, efficacy and impact.31 A large portion of the clinical documentation in the US is to support regulatory compliance and reimbursement, which is often viewed by physicians as low-value administrative data collected by unnecessary clicking. However, as the US moves towards value-based payment systems and as billing requirements become less onerous, this may not be as problematic. Though for many physicians who trained during this era of bloated documentation, it may be difficult to undo these habits and the feelings they engender.
Usability of EHRs is also a significant cause of frustration and burnout. US hospitals’ need for financial sustainability appeared to lead many EHR vendors to focus on financial and compliance features, often at the cost of usability.
The impact of EHRs on physician burnout is probably underestimated. In 2009, at the American Medical Informatics Annual Health Policy Meeting, informatics experts in the field of EHR implementation put forth predictions and recommendations regarding the potential unintended consequences of EHR implementation.32 In 2020, these predictions were reviewed by Starren et al. to assess whether those initial concerns were over- or underestimates. Predictions that addressed components of burnout, such as increased documentation, increased cognitive load, data overload and physicians taking early retirement, were all found to be worse than was anticipated 11 years earlier.33 However, when these informatics leaders were asked to quantify how much EHRs were contributing to the current burnout crisis, most of the respondents believed that EHRs contributed to half or less of the problem.
As described previously, increased working hours is associated with burnout. Not surprisingly, long working hours also often leads to decreased sleep. Almost one half of physicians surveyed reported that work schedules caused inadequate sleep.34 Inadequate sleep has been posited as a potential cause of burnout through two mechanisms: a chronic depletion of energy stores, and the activation of the hypothalamic-pituitary-adrenal axis leading to increased levels of stress.35 In individuals with burnout, sleep is less restorative than in those not experiencing significant burnout, potentially leading to a feedback loop of decreased restorative sleep, increased symptoms of burnout, and further decrease in quality of sleep.36
Unfortunately, the current medical ethos teaches trainees that sleep is dispensable and that surviving long shifts is a badge of honor, rather than potentially increasing the risk of medical errors or burnout.
Alt-text: Unlabelled box
The environment of practice is also an important contributor to burnout. Linzer et al. examined if adverse working conditions contributed to physician reactions and found that adverse workflow, such as a chaotic or time-pressured environment, low control over working conditions and decision making and an unfavorable organizational culture, were each strongly associated with low physician satisfaction, higher levels of stress, burnout and intent to leave.38
Medical culture
Factors contributing to burnout permeate medical culture. In addition to the “toughing it out” expectation in the face of sleep deprivation as mentioned previously, there exists a culture of presentee-ism, especially among trainees, where taking time off work is seen as letting their colleagues or even patients down. Illness, both physical and mental, is often treated as a weakness. In response, physicians continue to work at less than their full capacity or find other ways to hide their illness.
Some authors postulate that an increased focus on evidence-based medicine is a causative factor for burnout among more experienced physicians. With the recent intense focus on practicing only evidence-based medicine gleaned from careful review of the latest clinical research, physicians who rely on intuition and unsystematic clinical experience, often honed over years of practice, may be discredited as less valid or valuable.39
Interpersonal factors
In addition to the intrinsic pressures of medical practice, physicians often experience interpersonal stressors in the workplace. Medical culture has historically encouraged a “survival of the fittest” mentality, starting from medical school admissions through residency and beyond. This mentality engenders competitiveness which, though often subtle and benign, can progress to overt bullying. Both horizontal bullying (between people of the same rank) and vertical bullying (between people of different ranks) are commonplace, with 40% of doctors in a recent survey reporting experiencing bullying.82
Bullying more significantly impacts and marginalizes women and under-represented populations. Female clinicians are more likely to be humiliated or ridiculed in relation to their work, excluded from or ignored in conversations, have their work unrecognized or taken credit for by someone else, or have information withheld that affect their performance.41 The impact of these added stressors is reflected most starkly in the suicide statistics of female physicians. Although male physicians have a suicide rate 70% higher than men in the general population, a startling finding on its own, female physicians have a rate 250% higher than women in the general population.42 There is less known as to how significantly this affects pediatric providers, where 66% of physicians are female.43
Personal factors
The nature of medical training often selects for certain personality traits among aspiring physicians.
As described by Wong,39 pre-existing traits of perfectionism, altruism and responsibility for their patients can become pathologic and contribute to burnout.
Alt-text: Unlabelled box
Perfectionism can lead to micromanagement and an inability to delegate and severe self-criticism. This has been shown to be a risk factor for anxiety, burnout, and depression.44 , 45 46 Pathologic altruism may occur when to “go beyond the call of duty” leads a physician to make decisions that – while intended to promote the welfare of others – ultimately leads to negative consequences for the recipients and even the physician themselves.47
Adverse patient outcomes, whether expected or unexpected may result in second victim syndrome
Alt-text: Unlabelled box
first described by Wu in 2000, as the suffering of healthcare professionals related to an adverse outcome.48 Second victim syndrome includes physical manifestations such as fatigue, disordered sleep and elevated heart rate, as well as psychological and emotional distress. Scott et al. found that 30% of physicians experienced emotional issues related to a “bad outcome”, while Harrison et al. found that 76% of physicians whose patients had an adverse outcome or near miss had been affected personally or professionally.40 83
Preventive measures/mitigation
It may seem that the overabundance of risk factors for burnout has created an inescapable abyss that physicians cannot avoid. But the increasing recognition of burnout by national and international organizations raises hope that solutions can be developed to prevent or reverse symptoms of burnout in the physician workforce. It is important that these concepts of burnout prevention be introduced as early as possible in training. Lessons learned during early formative years can shape and color an entire career.49
Organizational interventions
Reducing stressors in the workplace is another important effort that should involve physicians at all levels of their careers, as well as allied health professionals, support staff and administrators. Over the years, administrative burden has become a significant source of frustration and stress for clinicians. Recently, the use of medical scribes has expanded to address this need. Although there has been little research on the use of scribes directly in relation to burnout, Mishra found that the use of scribes in primary care directly reduced time spent in the EHR by physicians and it improved efficiency and physician satisfaction.50 A recent qualitative study found that clinicians often “outsource certain tasks such as note-taking, computerized data entry and foraging the chart for information” to medical scribes.51 These tasks shared similar characteristics, including being time-consuming to perform, disruptive to clinical workflow, and adding no perceived value to direct patient care.
Similarly, it is important to reduce the amount of time spent on non-clinical tasks. This may involve re-distributing tasks to other team members, such as medical scribes, but also reducing the overall documentation burden. This emphasis on increasing time with patients aligns with the finding that physician satisfaction is associated with their relationship with patients, rather than compensation.52 Physicians who spend more than 20% of their time on the activity they deem most meaningful are least prone to burnout.53
In addition to reducing time spent on clerical tasks, an overall work-life balance shift would enable physicians time to recuperate and engage in self-care between and after shifts. Progress was made with duty hour limits imposed on residents in 2003 and those protections should be considered for physicians beyond their training years.54
Any intervention designed to reduce burnout must ultimately address known issues with EHR system design and usage, including documentation burden, inefficient or frustrating workflows, and the feeling of loss of autonomy.
The discipline of clinical informatics has a critical role in assisting clinicians be more efficient and help EHRs become a tool for efficiency and decrease its contribution to burnout. Health Information Technology is now a central theme in many institutional strategic plans and there is strong recognition that clinical informaticists are essential in the process to prevent burnout.
Documentation might be the most difficult to address. It requires government, payers and other external parties to adjust their expectations. It may also impact revenue generation. Recent changes to the documentation requirements for evaluation and management by Centers for Medicare and Medicaid Services that reduce the need for excessive and often unnecessary documentation is encouraging.55 There has also been strides towards improving usability of EHRs from the Office of the National Coordinator of Health Information Technology. However, changes must be made at the local level to align EHR workflows with local practices.56
Engaging physicians in the design and implementation of EHRs can provide some sense of control. Physician-led changes to EHR workflows has been shown to result in fewer clicks and more time with patients.84 57 In addition to making changes to the EHR, teaching clincians how to use the EHR better can improve efficiency and reduce burnout. Robinson and Kersey demonstrated a time savings of 4–5 min per hour and reduced feelings of burnout among physicians with an intensive three-day EHR education program.58 More recently, data from the KLAS Arch Collaborative found that physicians who reported their organization had done a “great job with EHR implementation, training, and support” were twice as likely to report lower burnout scores.59 Children's Hospital of Philadelphia created a more customized one-on-one training and efficiency program for their physicians and were able to reduce burnout rates from 32% to 23%.60
Beyond engagement and educational support, organizations can foster a culture that engenders resilience, compassion for ourselves and for each other as well as overall well-being. In a national survey of clinicians, supervisor scores in each of 12 leadership dimensions, as well as composite scores, strongly correlated with reduced burnout and improved satisfaction.61
Individual interventions
Promoting resilience – personal qualities that enable an individual to withstand, adapt or even thrive in the face of adversity and stress – can have a protective effect and reduce symptoms of burnout. Multiple studies have demonstrated that individuals with higher levels of resilience have reduced rates of burnout.62 63 West et al. found that physicians had higher levels of resilience compared with the general population. Despite this, nearly 30% of physicians with the highest resilience scores still experienced burnout. Interestingly, although pediatricians in this survey had lower resilience scores, previous studies have shown pediatricians to have lower rates of burnout compared to other physicians, which suggests the importance of environmental factors.63
Pediatric professional societies have been at the forefront of improving resilience. The American Academy of Pediatrics was one of the first medical societies to endorse a formal curriculum for building resilience in its trainees and clinicians with the AAP Resilience in the Face of Grief and Loss Curriculum.49 Initially created for educating trainees to understand grief and loss in children and better communicate with families regarding these difficult events, it was soon expanded to focus also on the impact these stressors had on the clinicians and how to promote personal wellness. The training materials for this curriculum are openly available.64 65
Mindfulness and self-compassion are two of the most effective strategies for increasing resilience.
Alt-text: Unlabelled box
Mindfulness is a mental state achieved by focusing one's awareness on the present moment, while calmly acknowledging and accepting one's feelings, thoughts, and bodily sensations. The goal is to be fully present, yet not be overwhelmed or be over-reactive to the situation. Originally developed by Jon Kabat-Zinn, mindfulness-based stress reduction courses have been associated with reduced rates of burnout in several studies. These courses often involve meditation techniques, simple yoga postures and discussion groups which focus on reflection, shared experiences, and small group learning.66,67
Self-compassion is the practice of treating oneself with the same kindness and care one would offer to a friend in the same circumstances.68 Many clinicians tend to be their own most severe critic. To counter this tendency, self-kindness encourages one to be kind to themselves when failing or feeling inadequate, paying attention to negative self-talk and replacing those statements with words one would offer to a co-worker or friend in the same circumstances. High levels of self-compassion are associated with greater emotional stability during stressful times and less brooding, rumination, anxiety or depression.69 70
Other self-care habits that have been suggested to reduce burnout often align with healthy coping mechanisms such as exercise, yoga and meditation. Adequate and quality sleep is also an important factor. Good sleep hygiene (removing electronics from sleeping areas, avoiding caffeine, maintaining a regular sleep schedule, etc.) is important to improving the quality of sleep, particularly given the often-chaotic schedules or shiftwork inherent in medical practice.71
Burnout in the age of COVID-19
It is impossible to discuss physician burnout in the current period without the mention of the COVID-19 pandemic. During the first year of the pandemic, Kaiser Health News and The Guardian counted 3607 US health care worker deaths related to the pandemic, including 291 physicians.72 Beyond deaths directly attributable to COVID-19, there is also the added emotional and mental health toll of caring for sick and often dying patients in unprecedented circumstances.
The pandemic has presented numerous challenges to clinicians– from frequently changing and often conflicting guidance, to a dearth of reliable testing and effective treatments early on, to the ever-present risk of getting infected oneself or of passing the infection on to a loved one.73 74 A systematic review by Kisely et al. looking at mental health effects of pandemics found that clinicians i in direct contact with affected patients had 1.7 times the incidence of acute or post-traumatic stress and 1.74 times the incidence of psychological distress than those not in direct contact.
Similar findings have been reported over the last year regarding COVID-19. Kannampallil found that physician trainees exposed to patients being tested for COVID-19 had higher levels of stress and burnout, while Dzau and colleagues noted moral distress, anxiety and suicide in healthcare workers early in the pandemic.75, 76 However, two studies showed higher rates of burnout in normal ward workers than in frontline workers.77, 78 This was posited to potentially be due to less familiarity with COVID precautions and protocols thereby causing greater anxiety about possible exposures. It should be noted that many of these studies do not have pre-pandemic baseline burnout data for comparison, so it may be difficult to gage the effect of the COVID-19 pandemic.
One positive aspect of this past year is the growing realization that the health of our healthcare workforce is critical to respond to global health threats. Many healthcare organizations have created Chief Wellness Officer roles or instituted well-being programs. Resources such as the Clinician Well-Being Knowledge Hub – https://nam.edu/clinicianwellbeing – and the Collaborative for Healing and Renewal in Medicine (CHARM) – https://www.im.org/resources/wellness-resiliency/charm – can aid organizations seeking to create their own wellness programs.
Conclusion
Burnout is an epidemic phenomenon among physicians, having an adverse effect not only on physician well-being, but also patient care, safety, and the larger health care ecosystem. It is, however, treatable, and preventable. The difficultly in doing so is that many of the changes needed to prevent burnout involve organizational culture and national policy. It is important to note that much of this research is done in non- pediatric groups, so not all the findings may be generalizable to our population.
In 2008, Dr. Berwick, a pediatrician and his colleagues introduced the concept of ‘The Triple Aim’. This is a widely accepted approach to optimize the health system performance, by simultaneously pursuing 3 aims: enhancing patient experience, improving population health, and reducing costs of performance.79
Despite adopting the patient centered Triple Aim, stress and burnout in clinicians has prevented successful achievement of this goal. In 2014, Bodenheimer and Sinsky recommended the “Quadruple Aim” framework, where the goal of improving clinician wellbeing directly contributes to better patient care and optimizes the performance of the healthcare system.80
Achieving this crucial fourth aim will not be easy, but it is certainly possible. It will require a partnership among clinicians, organizational leaders, government agencies, third-party payers, and many others. Clinicians must have input in determining workflows and strategic initiatives to ensure autonomy in the workplace and a feeling of being valued. Above all, the patient-clinician relationship must remain sacrosanct, and the value of clinician wellbeing in relation to patient care and operational priorities must be recognized, respected, and restored.
Declaration of Competing Interest
None of the authors have any conflict of interest to report
Funding Source
None, for all of the authors
References
- 1.Institute of Medicine (US) In: To Err is Human: Building a Safer Health System. Kohn LT, Corrigan JM, Donaldson MS, editors. National Academies Press (US); Washington (DC): 2000. Committee on Quality of Health Care in America. [PubMed] [Google Scholar]
- 2.Gagné M., Deci E.L. Self-determination theory and work motivation. J Organiz Behav. 2005;26:331–362. [Google Scholar]
- 3.National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine . Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. National Academies Press (US); Washington (DC): 2019. Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being. October 23. [PubMed] [Google Scholar]
- 4.'Death by 1000 Cuts': Medscape National Physician Burnout & Suicide Report 2021. https://www.medscape.com/slideshow/2021-lifestyle-burnout-6013456
- 5.Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal S.D., Pabo E., Rozenblum R., Sherritt K.M. Professional Dissonance and Burnout in Primary Care: a Qualitative Study. JAMA Intern Med. 2020;180(3):395–401. doi: 10.1001/jamainternmed.2019.6326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li-Sauerwine S., Rebillot K., Melamed M., Addo N., Lin M. A 2-Question Summative Score Correlates with the Maslach Burnout Inventory. West J Emerg Med. 2020;21(3):610–617. doi: 10.5811/westjem.2020.2.45139. Published 2020 Apr 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schaufeli W.B., Leiter M.P., Maslach C. Burnout: 35 years of research and practice. Career Dev Int. 2009;14:204–220. 3. [Google Scholar]
- 9.Patel R.S., Bachu R., Adikey A., Malik M., Shah M. Factors Related to Physician Burnout and Its Consequences: a Review. Behav Sci (Basel) 2018;8(11):98. doi: 10.3390/bs8110098. Published 2018 Oct 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 11.Portoghese I., Galletta M., Coppola R.C., Finco G., Campagna M. Burnout and workload among health care workers: the moderating role of job control. Saf Health Work. 2014;5(3):152–157. doi: 10.1016/j.shaw.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Medscape Pediatrician Lifestyle Happiness and Burnout Report. 2021 https://www.medscape.com/slideshow/2021-lifestyle-pediatrician-6013520 [Google Scholar]
- 13.Kumar G., Mezoff A. Physician Burnout at a Children's Hospital: incidence, Interventions, and Impact. Pediatr Qual Saf. 2020;5(5):e345. doi: 10.1097/pq9.0000000000000345. Published 2020 Sep 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dyrbye L., West C., Satele D. Burnout Among U.S. Medical Students, Residents, and Early Career Physicians Relative to the General U.S. Population. Academic Medicine. 2014;89:443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 15.Stehman C.R., Testo Z., Gershaw R.S., Burnout Kellogg AR., Out Drop. Suicide: physician Loss in Emergency Medicine, Part I [published correction appears. West J Emerg Med. 2019;20(5):840–841. doi: 10.5811/westjem.2019.4.40970. Aug 21]West J Emerg Med. 2019;20(3):485-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salyers M.P., Bonfils K.A., Luther L., et al. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: a Meta-Analysis. J Gen Intern Med. 2017;32(4):475–482. doi: 10.1007/s11606-016-3886-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.West C.P., Dyrbye L.N., Shanafelt T.D. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 18.Salvagioni D.A.J., Melanda F.N., Mesas A.E., González A.D., Gabani F.L., Andrade S.M. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS ONE. 2017;12(10) doi: 10.1371/journal.pone.0185781. Published 2017 Oct 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dyrbye L.N., West C.P., Sinsky C.A., Goeders L.E., Satele D.V., Shanafelt T.D. Medical Licensure Questions and Physician Reluctance to Seek Care for Mental Health Conditions. Mayo Clin Proc. 2017;92(10):1486–1493. doi: 10.1016/j.mayocp.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 20.Patel R.S., Bachu R., Adikey A., Malik M., Shah M. Factors Related to Physician Burnout and Its Consequences: a Review. Behav Sci (Basel) 2018;8(11):98. doi: 10.3390/bs8110098. Published 2018 Oct 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maslach C., Leiter M.P. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160–163. doi: 10.1080/0142159X.2016.1248918. [DOI] [PubMed] [Google Scholar]
- 22.Arigoni F., Bovier P.A., Mermillod B., Waltz P., Sappino A.P. Prevalence of burnout among Swiss cancer clinicians, paediatricians and general practitioners: who are most at risk? Support Care Cancer. 2009;17(1):75–81. doi: 10.1007/s00520-008-0465-6. [DOI] [PubMed] [Google Scholar]
- 23.Al-Dubai S.A., Rampal K.G. Prevalence and associated factors of burnout among doctors in Yemen. J Occup Health. 2010;52(1):58–65. doi: 10.1539/joh.o8030. [DOI] [PubMed] [Google Scholar]
- 24.Shanafelt T.D., West C.P., Sloan J.A., et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169(10):990–995. doi: 10.1001/archinternmed.2009.70. [DOI] [PubMed] [Google Scholar]
- 25.Asan O., Montague E. Physician interactions with electronic health records in primary care. Health Syst. 2012;1:96–103. doi: 10.1057/hs.2012.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sinsky C., Colligan L., Li L., et al. Allocation of Physician Time in Ambulatory Practice: a Time and Motion Study in 4 Specialties. Ann Intern Med. 2016;165(11):753–760. doi: 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]
- 27.Arndt B.G., Beasley J.W., Watkinson M.D., et al. Tethered to the EHR: primary Care Physician Workload Assessment Using EHR Event Log Data and Time-Motion Observations. Ann Fam Med. 2017;15(5):419–426. doi: 10.1370/afm.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peccoralo L.A., Kaplan C.A., Pietrzak R.H., Charney D.S., Ripp J.A. The impact of time spent on the electronic health record after work and of clerical work on burnout among clinical faculty. J Am Med Inform Assoc. 2021;28(5):938–947. doi: 10.1093/jamia/ocaa349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gawande A. Why Doctors Hate Their Computers. New Yorker. 2018 https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers Accessed June 23, 2020. [Google Scholar]
- 30.Downing N.L., Bates D.W., Longhurst C.A. Physician Burnout in the Electronic Health Record Era: are We Ignoring the Real Cause? Ann Intern Med. 2018;169(1):50–51. doi: 10.7326/M18-0139. [DOI] [PubMed] [Google Scholar]
- 31.Corrigendum to: journal of the American Medical Informatics Association, Volume 23, Issue 1, 1 January 2016, Pages 230-239. J Am Med Inform Assoc. 2018;25(9):1270–1271. doi: 10.1093/jamia/ocv100. doi:10.1093/jamia/ocy063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bloomrosen M., Starren J., Lorenzi N.M., Ash J.S., Patel V.L., Shortliffe E.H. Anticipating and addressing the unintended consequences of health IT and policy: a report from the AMIA 2009 Health Policy Meeting. J Am Med Inform Assoc. 2011;18(1):82–90. doi: 10.1136/jamia.2010.007567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Starren J.B., Tierney W.M., Williams M.S., et al. A retrospective look at the predictions and recommendations from the 2009 AMIA policy meeting: did we see EHR-related clinician burnout coming? J Am Med Inform Assoc. 2021;28(5):948–954. doi: 10.1093/jamia/ocaa320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American College of Chest Physicians. Most physicians sleep fewer hours than needed for peak performance, report says. ScienceDaily. March 5, 2008. www.sciencedaily.com/releases/2008/03/080304075723.htm. Accessed December 14, 2018.
- 35.Stewart N.H., Arora V.M. The Impact of Sleep and Circadian Disorders on Physician Burnout. Chest. 2019;156(5):1022–1030. doi: 10.1016/j.chest.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sonnenschein M., Sorbi M.J., van Doornen L.J., Schaufeli W.B., Maas C.J. Evidence that impaired sleep recovery may complicate burnout improvement independently of depressive mood. J Psychosom Res. 2007;62(4):487–494. doi: 10.1016/j.jpsychores.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 37.Peets A., Ayas N.T. Restricting resident work hours: the good, the bad, and the ugly. Crit Care Med. 2012;40(3):960–966. doi: 10.1097/CCM.0b013e3182413bc5. [DOI] [PubMed] [Google Scholar]
- 38.Linzer M., Manwell L.B., Williams E.S., et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151(1):28–W9. doi: 10.7326/0003-4819-151-1-200907070-00006. [DOI] [PubMed] [Google Scholar]
- 39.Wong A.M.F. Beyond burnout: looking deeply into physician distress. Can J Ophthalmol. 2020;55(3):7–16. doi: 10.1016/j.jcjo.2020.01.014. Suppl 1. [DOI] [PubMed] [Google Scholar]
- 40.Scott S.D., Hirschinger L.E., Cox K.R., et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010;36(5):233–240. doi: 10.1016/s1553-7250(10)36038-7. [DOI] [PubMed] [Google Scholar]
- 41.Rouse L.P., Gallagher-Garza S., Gebhard R.E., Harrison S.L., Wallace L.S. Workplace Bullying Among Family Physicians: a Gender Focused Study. J Womens Health (Larchmt) 2016;25(9):882–888. doi: 10.1089/jwh.2015.5577. [DOI] [PubMed] [Google Scholar]
- 42.Silverman M.M. In: The Handbook of Physician Health. Goldman LS, Myers M, Dickstein LJ, editors. American Medical Association; Chicago, IL: 2000. Physicians and suicide. editors. [Google Scholar]
- 43.General Pediatrician Age/Gender Distribution and Summary | The American Board of Pediatrics (abp.org)
- 44.Hamilton T.K., Schweitzer R.D. The cost of being perfect: perfectionism and suicide ideation in university students. Aust N Z J Psychiatry. 2000;34(5):829–835. doi: 10.1080/j.1440-1614.2000.00801.x. [DOI] [PubMed] [Google Scholar]
- 45.Beevers C.G., Miller I.W. Perfectionism, cognitive bias, and hopelessness as prospective predictors of suicidal ideation. Suicide Life Threat Behav. 2004;34(2):126–137. doi: 10.1521/suli.34.2.126.32791. [DOI] [PubMed] [Google Scholar]
- 46.Flett G.L., Hewitt P.L. American Psychological Association; Washington, DC: 2002. Perfectionism: Theory, Research, and Treatment. editors. [Google Scholar]
- 47.Oakley B., Knafo A., Madhavan G., Wilson D.S. Oxford Univeristy Press; New York: 2011. Pathological Altruism. editors. [Google Scholar]
- 48.Wu A.W. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ. 2000;320(7237):726–727. doi: 10.1136/bmj.320.7237.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Serwint J.R., Bostwick S., Burke A.E., et al. The AAP Resilience in the Face of Grief and Loss Curriculum. Pediatrics. 2016;138(5) doi: 10.1542/peds.2016-0791. [DOI] [PubMed] [Google Scholar]
- 50.Mishra P., Kiang J.C., Grant R.W. Association of Medical Scribes in Primary Care With Physician Workflow and Patient Experience. JAMA Intern Med. 2018;178(11):1467–1472. doi: 10.1001/jamainternmed.2018.3956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tran B.D., Rosenbaum K., Zheng K. An interview study with medical scribes on how their work may alleviate clinician burnout through delegated health IT tasks. J Am Med Inform Assoc. 2021;28(5):907–914. doi: 10.1093/jamia/ocaa345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Linzer M., Manwell L.B., Williams E.S., et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151(1):28–W9. doi: 10.7326/0003-4819-151-1-200907070-00006. [DOI] [PubMed] [Google Scholar]
- 53.Shanafelt T.D., West C.P., Sloan J.A., et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169(10):990–995. doi: 10.1001/archinternmed.2009.70. [DOI] [PubMed] [Google Scholar]
- 54.Philibert I., Friedmann P., Williams W.T. ACGME Work Group on Resident Duty Hours. AccreditationCouncil for Graduate Medical Education. New requirements for resident duty hours. JAMA. 2002;288(9):1112–1114. doi: 10.1001/jama.288.9.1112. [DOI] [PubMed] [Google Scholar]
- 55.Evaluation and Management Services Guide Booklet (cms.gov)
- 56.Usability and Provider Burden | HealthIT.gov
- 57.Collier R. Rethinking EHR interfaces to reduce click fatigue and physician burnout. CMAJ. 2018;190(33):E994–E995. doi: 10.1503/cmaj.109-5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Robinson K.E., Kersey J.A. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine (Baltimore) 2018;97(38):e12319. doi: 10.1097/MD.0000000000012319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eschenroeder H.C., Manzione L.C., Adler-Milstein J., et al. Associations of physician burnout with organizational electronic health record support and after-hours charting. J Am Med Inform Assoc. 2021;28(5):960–966. doi: 10.1093/jamia/ocab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lourie E.M., Utidjian L.H., Ricci M.F., Webster L., Young C., Grenfell S.M. Reducing electronic health record-related burnout in providers through a personalized efficiency improvement program. J Am Med Inform Assoc. 2021;28(5):931–937. doi: 10.1093/jamia/ocaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shanafelt T.D., Gorringe G., Menaker R., et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432–440. doi: 10.1016/j.mayocp.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 62.Rushton C.H., Batcheller J., Schroeder K., Donohue P. Burnout and Resilience Among Nurses Practicing in High-Intensity Settings. Am J Crit Care. 2015;24(5):412–420. doi: 10.4037/ajcc2015291. [DOI] [PubMed] [Google Scholar]
- 63.West C.P., Dyrbye L.N., Sinsky C., et al. Resilience and Burnout Among Physicians and the General US Working Population. JAMA Netw Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.9385. Published 2020 Jul 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Resilience Curriculum: resilience in the face of grief and loss (aap.org). https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/hospice-palliative-care/Pages/Resilience-Curriculum.aspx [DOI] [PubMed]
- 65.Pediatric Resident Burnout-Resilience Study Consortium – PRBRSC (pedsresresilience.com)
- 66.Crane R.S., Brewer J., Feldman C., et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med. 2017;47(6):990–999. doi: 10.1017/S0033291716003317. [DOI] [PubMed] [Google Scholar]
- 67.Shapiro S.L., Astin J.A., Bishop S.R., Cordova M. Mindfulness-Based Stress Reduction for Health Care Professionals: results From a Randomized Trial. Int J Stress Manag. 2005;12(2):164–176. doi: 10.1037/1072-5245.12.2.164. [DOI] [Google Scholar]
- 68.Neff K. William Morrow; New York, NY: 2011. Self-Compassion. [Google Scholar]
- 69.Raes F. Rumination and worry as mediators of the relationship between self-compassion and depression and anxiety. Pers Individ Dif. 2010;48:757–761. [Google Scholar]
- 70.Leary M.R., Tate E.B., Adams C.E., Allen A.B., Hancock J. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Pers Soc Psychol. 2007;92(5):887–904. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- 71.The Role of Sleep Hygiene in Promoting Public Health: A Review of Empirical Evidence (nih.gov) [DOI] [PMC free article] [PubMed]
- 72.Lost on the frontline: US healthcare workers who died fighting Covid-19. The Guardian Accessed: Nov 3, 2021. https://www.theguardian.com/us-news/ng-interactive/2020/aug/11/lost-on-the-frontline-covid-19-coronavirus-us-healthcare-workers-deaths-database
- 73.Shanafelt T., Ripp J., Trockel M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. JAMA. 2020;323(21):2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 74.Cai H., Tu B., Ma J., et al. Psychological Impact and Coping Strategies of Frontline Medical Staff in Hunan Between January and March 2020 During the Outbreak of Coronavirus Disease 2019 (COVID‑19) in Hubei, China. Med Sci Monit. 2020;26 doi: 10.12659/MSM.924171. Published 2020 Apr 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kannampallil T.G., Goss C.W., Evanoff B.A., Strickland J.R., McAlister R.P., Duncan J. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS ONE. 2020;15(8) doi: 10.1371/journal.pone.0237301. Published 2020 Aug 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dzau V.J., Kirch D., Nasca T. Preventing a Parallel Pandemic - A National Strategy to Protect Clinicians' Well-Being. N Engl J Med. 2020;383(6):513–515. doi: 10.1056/NEJMp2011027. [DOI] [PubMed] [Google Scholar]
- 77.Wu Y., Wang J., Luo C., et al. A Comparison of Burnout Frequency Among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. J Pain Symptom Manage. 2020;60(1):e60–e65. doi: 10.1016/j.jpainsymman.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dimitriu M.C.T., Pantea-Stoian A., Smaranda A.C., et al. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses. 2020;144 doi: 10.1016/j.mehy.2020.109972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Berwick D.M., Nolan T.W., Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 80.Bodenheimer T., Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Maslach Christina, Jackson Susan, Leiter Michael. Evaluating stress: A book of resources. Scarecrow Education; 1997. Maslach Burnout Inventory: Third edition; pp. 191–218. In press. [Google Scholar]
- 82.British Medical Association - Caring, supportive, collaborative? Doctors' views on working in the NHS, 2018. [Accessed 03 November 2021].
- 83.Harrison Reema, Lawton Rebecca, Stewart Kevin. Doctors’ experiences of adverse events in secondary care: the professional and personal impact. Clinical Medicine. 2014;14(6):585–590. doi: 10.7861/clinmedicine.14-6-585. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Guo Uta, Chen Lu, Mehta Parag. Electronic health record innovations: Helping physicians – One less click at a time. Health Information Management Journal. 2017;46(3):140–144. doi: 10.1177/1833358316689481. In press. [DOI] [PubMed] [Google Scholar]