Abstract
Introduction
Little is known about COVID-19 vaccination intent among people experiencing homelessness. This study assesses surveyed COVID-19 vaccination intent among adult homeless shelter residents and staff and identifies factors associated with vaccine deliberation (responded “undecided”) and reluctance (responded “no”), including time trends.
Methods
From 11/1/2020–2/28/21, we conducted repeated cross-sectional surveys at nine shelters in King County, WA as part of ongoing community-based SARS-CoV-2 surveillance. We used a multinomial model to identify characteristics associated with vaccine deliberation and reluctance.
Results
A total of 969 unique staff (n = 297) and residents (n = 672) participated and provided 3966 survey responses. Among residents, 53.7% (n = 361) were vaccine accepting, 28.1% reluctant, 17.6% deliberative, and 0.6% already vaccinated, whereas among staff 56.2% were vaccine accepting, 14.1% were reluctant, 16.5% were deliberative, and 13.1% already vaccinated at their last survey. We observed higher odds of vaccine deliberation or reluctance among Black/African American individuals, those who did not receive a seasonal influenza vaccine, and those with lower educational attainment. There was no significant trend towards vaccine acceptance.
Conclusions
Strong disparities in vaccine intent based on race, education, and prior vaccine history were observed. Increased vaccine intent over the study period was not detected. An intersectional, person-centered approach to addressing health inequities by public health authorities planning vaccination campaigns in shelters is recommended.
Clinical Trial Registry Number: NCT04141917.
Keywords: COVID-19, SARS-CoV-2, Shelter, Homeless, Vaccination, Health inequities
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has caused significant morbidity and mortality and highlighted socioeconomic and racial disparities. People experiencing homelessness (PEH) and the staff who work in homeless shelters are at high-risk for acquiring respiratory viral infections due to difficulty maintaining physical distance, shelter overcrowding, and sharing of hygiene facilities [1], [2], [3]. In the United States (U.S.), approximately 61% of 580,000 PEH reside in sheltered locations [4] and are disproportionately affected by underlying medical conditions associated with severe illness from COVID-19 [5]. Therefore, addressing access and barriers to care in this population is a public health priority.
Challenges to reduce severe outcomes related to COVID-19 include access to COVID-19 vaccination [6], [7], [8] and a history of disproportionately low vaccine intent among PEH [7], [9], [10]. An understanding of vaccination intent—defined here as planning to get the COVID-19 vaccine—is important to tailor vaccine campaign strategies to maximize improvements in socio-culturally informed vaccine uptake. Available vaccines report high efficacy and safety [11], [12], and the U.S. population has had an overall increase in COVID-19 vaccine intent over the last year [13]. While many studies have examined the continuum of vaccination intent and related sociodemographic and racial disparities [13], [14], [15], [16], little is known about COVID-19 vaccination intent among PEH or homeless shelter staff. In this study, we assessed adult homeless shelter residents’ and staffs’ intent to receive COVID-19 vaccination and identified factors associated with vaccine deliberation and reluctance. We also evaluated how vaccination intent changed over a four-month study period that preceded vaccine eligibility for those in congregate settings where PEH live or access services in King County, Washington.
2. Methods
2.1. Study design and population
Our study used a repeated cross-sectional design to describe and identify factors associated with COVID-19 vaccine deliberation and reluctance among shelter residents and staff before vaccine eligibility. This analysis was a sub-study of community-based severe acute respiratory syndrome coronavirus (SARS-CoV-2) surveillance in homeless shelters in King County, Washington [17]. In brief, the surveillance occurred in-person six days/week using self-collected mid-turbinate nasal swabs and corresponding surveys to assess SARS-CoV-2 infection burden and associated risk factors among residents and staff. Persons aged ≥3 months whose primary residence or place of employment was at one of nine shelters were eligible for participation up to once/week. During the study period, two of the nine shelters relocated staff and residents to new facilities that enabled improved adherence to COVID-19 infection and prevention control measures. Research activities immediately recommenced following these relocations. Participant recruitment relied on consistent on-site presence of research staff and in-person messaging that regular testing was an important strategy for keeping oneself and their community safe from COVID-19 disease. Sites included a mix of adult, family, and young adult shelters, strategically selected to be sociodemographically representative of King County’s sheltered PEH (Supplemental Table 1) [17]. Survey responses collected between 11/1/2020 through 2/28/2021 from participants aged ≥18 years were included in this analysis. All survey data were collected electronically in Research Electronic Data Capture (REDCap) on tablets; additional study details have been previously described [17]. This study was approved by the Human Subjects Division of the University of Washington Institutional Review Board (STUDY00007800).
2.2. Measures
The primary outcome of this study was the intention to be vaccinated against COVID-19 before and early in the vaccine rollout. All participants were posed the question “Once a vaccine against COVID-19 becomes available to you, do you plan to get it?” Responses were categorized as vaccine accepting (“yes”); vaccine deliberative [18] (“undecided”); or vaccine reluctant (“no”). Participants who indicated that they already received any COVID-19 vaccine doses were also considered vaccine accepting.
Survey data included participant sex, date of birth (DOB), race, ethnicity (Hispanic or Latino vs. non-Hispanic or Latino), seasonal influenza vaccine receipt, underlying medical conditions, status as shelter staff versus resident, level of highest education (a proxy for health literacy) [19], health insurance status, employment status, receipt of any COVID-19 vaccine doses, and primary reason for COVID-19 vaccination deliberation or reluctance. Influenza vaccine status was determined by self-reported receipt of the vaccine since 7/1/2020. All variables were determined by self-report, including having ever tested positive for SARS-CoV-2 (through this surveillance or another testing platform). Duration of homelessness was captured among shelter residents, with chronic homelessness defined as duration ≥1 year. Enrollments per unique participant was defined as the number of survey responses collected from the same participant over the study period.
2.3. Statistical analysis
This study allowed individuals to enroll and complete the survey multiple times (Supplemental Fig. 1). Surveys from the same participant were linked and assigned a unique identifier using name, DOB, and sex. Incongruous name spelling due to clerical error was addressed using a function of the Levenshtein distance, a metric used to measure the differences between two character strings [20]. Survey records were manually assigned to the same individual if the two names fell above a pre-specified value of similarity (>0.8 in the interval [0,1]) and had the same DOB and sex. If two survey records had the same name and sex but one-digit discrepancy in the DOB, the same unique identifier was assigned.
We used descriptive statistics to evaluate the sociodemographic and health characteristics associated with intent to receive COVID-19 vaccine using each unique participant’s last survey response, as it is most relevant to public health decision-making for continuing COVID-19 vaccine implementation efforts. For categorical variables, we used a Chi-square test for independence (or a Fisher’s exact test when cells had less than 10 observations) of participant characteristics and vaccine intent, separately among shelter residents and shelter staff; a one-way ANOVA test was used for continuous variables.
To identify factors associated with COVID-19 vaccine deliberation and reluctance, we conducted a multivariate multinomial logistic regression model to calculate adjusted odds ratios (aOR) based on the last survey response. This model compares two nonordered outcome categories to a reference category. We estimated the “odds” (here, the ratio of two probabilities) a participant would be deliberative about COVID-19 vaccination, compared to vaccine accepting (i.e., intending to be or already vaccinated). We simultaneously estimated the odds a participant would be reluctant to vaccination, compared to vaccine accepting. Model covariates included age, race, ethnicity, sex, status as shelter staff versus resident, highest education level, employment status, ≥1 underlying medical condition, enrollments per unique participant, self-reported prior SARS-CoV-2 positive test result, and seasonal influenza vaccination status. Only completed surveys were included; if a subject responded “Prefer not to say” for any covariates included, they were removed as an observation from the final fitted model. We explored models for residents and staff separately; however, finding that several independent variables had fewer than 10 cases in each stratum, we decided to present a single model with a covariate for resident or staff to avoid over-parameterization. We also explored a multivariable mutinomial model without influenza vaccination history in case inclusion of this variable concealed other covariates’ association with COVID-19 vaccine intent due to collinearity. Coefficient and p-value results were very comparable to the original model, however, so we chose not to present the results from this sensitivity analysis.
When examining population-level change in vaccination intent over time, we overlaid events of interest that preceded widespread vaccine eligibility (Table 1 ) to see if they appeared to correspond with temporal trends in intent to receive COVID-19 vaccine.
Table 1.
Events of interest related to COVID-19 vaccine confidence in Washington State.
| Event Description | Date Implemented | |
|---|---|---|
| 1 | Institution of Washington (WA) statewide restrictions on openings and public gatherings | 16 November 2020 |
| 2 | Emergency Use Authorization for the BNT162b2 mRNA (Pfizer) COVID-19 vaccine by the U.S. Food and Drug Administration | 11 December 2020 |
| 3 | Initiation of Phase 1A Tier 1 COVID-19 vaccination in WA*, extending eligibility to:
|
14 December 2020 |
| 4 | Initiation of Phase 1B Tier 1 COVID-19 vaccination in WA, extending eligibility to:
|
18 January 2021 |
| 5 | First discovery of the SARS-CoV-2 variant B.1.1.7 in WA | 23 January 2021 |
COVID-19 Vaccine Response Team, Meehan K, Hanewall B. COVID-19 Vaccine Prioritization Guidance and Allocation Framework.; 2021. https://www.doh.wa.gov/Portals/1/Documents/1600/coronavirus/820–112-VaccineAllocationPrioritization.pdf.
To evaluate within-person change in vaccination intent over time, we filtered our data to include only unique participants with two or more survey responses and compared their first and last survey responses. Participants who received any COVID-19 vaccine prior to their first survey were excluded. To test whether there was a significant change in intent over the study period, we fit an unadjusted multinomial logistic model predicting self-reported receipt of or intent to receive a COVID-19 vaccine at last survey response (outcome), based on first survey response. All analyses were performed using R Statistical Software Version 4.0.3.
3. Results
3.1. Participant characteristics
From 11/1/2020 through 02/28/2021, a total of 969 unique adult shelter residents (n = 672) and staff (n = 297) in nine shelters in King County, Washington participated and completed 3966 surveys (Table 2 ). Each participant completed a median of two surveys over the four-month study period, with interquartile ranges (IQR) of [1.00–5.00] and [1.00–6.00], among residents and staff, respectively. The median number of days between participants’ first and last survey was 53 (Supplemental Fig. 2). The median date of first survey was 11/14/2020 (IQR: 11/05/2020–12/12/2020). The median date of last survey was 02/03/2021 (IQR: 12/28/2020–02/22/2021). A greater proportion of residents reported previously testing positive for SARS-CoV-2 than staff (10.4% vs. 5.1%).
Table 2.
Last survey responses for COVID-19 vaccine uptake, when it becomes available, from unique participants.*
| Intent to Be Vaccinated, n (%)† |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resident |
Staff |
|||||||||||
| No n = 189 (28.1%) |
Yes n = 361 (53.7%) |
Undecided n = 118 (17.6%) |
Received vaccine n = 4 (0.6%) |
Total n = 672 |
P-value | No n = 42 (14.1%) |
Yes n = 167 (56.2%) |
Undecided n = 49 (16.5%) |
Received vaccine n = 39 (13.1%) |
Total n = 297 |
P-value | |
| Median age [Range] | 36.0 [18.0, 80.0] | 45.0 [18.0, 85.0] | 38.0 [18.0, 72.0] | 48.5 [41.0, 51.0] | 41.0 [18.0, 85.0] | <0.001 | 38.5 [20.0, 68.0] | 29.0 [18.0, 78.0] | 40.0 [21.0, 71.0] | 31.0 [21.0, 81.0] | 33.0 [18.0, 81.0] | 0.004 |
| Age group | ||||||||||||
| 18–49 y | 142 (31.8%) | 212 (47.4%) | 90 (20.1) | 3 (0.7%) | 447 (66.5%) | 0.001 | 35 (14.5%) | 139 (57.7%) | 37 (15.4%) | 30 (12.4%) | 241 (81.1%) | 0.33 |
| 50–64 y | 35 (20%) | 118 (67.4%) | 21 (12%) | 1 (0.6%) | 175 (26.0%) | 6 (13.3%) | 23 (51.1%) | 11 (24.4%) | 5 (11.1%) | 45 (15.2%) | ||
| ≥65 y | 12 (24%) | 31 (62%) | 7 (14%) | 0 (0%) | 50 (7.44%) | 1 (9.1%) | 5 (45.5%) | 1 (9.1%) | 4 (36.4%) | 11 (3.70%) | ||
| Race | ||||||||||||
| American Indian/ Alaska Native | 9 (34.6%) | 11 (42.3%) | 5 (19.2%) | 1 (3.8%) | 26 (4.50%) | 0.001 | 1 (25.0%) | 1 (25.0%) | 2 (50.0%) | 0 (0.0%) | 4 (1.44%) | <0.001 |
| Asian | 2 (11.1%) | 15 (83.3%) | 1 (5.6%) | 0 (0.0%) | 18 (3.11%) | 3 (10.3%) | 19 (65.5%) | 3 (10.3%) | 4 (13.8%) | 29 (10.4%) | ||
| Black/African American | 75 (34.7%) | 100 (46.3%) | 39 (18.1%) | 2 (0.9%) | 216 (37.4%) | 29 (39.7%) | 16 (21.9%) | 20 (27.4%) | 8 (11.0%) | 73 (26.3%) | ||
| Multiple | 21 (44.7%) | 19 (40.4%) | 7 (14.9%) | 0 (0.0%) | 47 (8.13%) | 0 (0.0%) | 11 (64.7%) | 2 (11.8%) | 4 (23.5%) | 17 (6.12%) | ||
| Native Hawaiian/ Pacific Islander | 14 (37.8%) | 17 (45.9%) | 6 (16.2%) | 0 (0.0%) | 37 (6.40%) | 0 (0.0%) | 2 (28.6%) | 4 (57.1%) | 1 (14.3%) | 7 (2.52%) | ||
| White | 46 (19.7%) | 145 (62.0%) | 43 (18.4%) | 0 (0.0%) | 234 (40.5%) | 7 (4.7%) | 108 (73.0%) | 11 (7.4%) | 22 (14.9%) | 148 (53.2%) | ||
| Hispanic or Latino | 19 (19.0%) | 61 (61.0%) | 20 (20.0%) | 0 (0%) | 100 (15.2%) | 0.12 | 1 (3.4%) | 17 (58.6%) | 8 (27.6%) | 3 (10.3%) | 29 (9.90%) | 0.13 |
| Male | 113 (27.4%) | 244 (59.2%) | 54 (13.1%) | 1 (0.2%) | 412 (63.6%) | <0.001 | 10 (9.4%) | 70 (66.0%) | 13 (12.3%) | 13 (12.3%) | 106 (36.4%) | 0.06 |
| Duration of homelessness | ||||||||||||
| ≤6 months | 60 (32.8%) | 87 (47.5%) | 35 (19.1%) | 1 (0.5%) | 183 (28.7%) | 0.24 | NA | NA | NA | NA | NA | NA |
| 7–12 months | 34 (35.8%) | 46 (48.4%) | 15 (15.8%) | 0 (0.0%) | 95 (14.9%) | NA | NA | NA | NA | NA | ||
| 13–24 months | 20 (27.4%) | 42 (57.5%) | 10 (13.7%) | 1 (1.4%) | 73 (11.4%) | NA | NA | NA | NA | NA | ||
| ≥24 months | 68 (23.7%) | 171 (59.6%) | 46 (16.0%) | 2 (0.7%) | 287 (45.0%) | NA | NA | NA | NA | NA | ||
| Highest education | ||||||||||||
| Less than high school | 42 (30.0%) | 75 (53.6%) | 23 (16.4%) | 0 (0.0%) | 140 (21.6%) | 0.02 | 1 (12.5%) | 4 (50.0%) | 3 (37.5%) | 0 (0.0%) | 8 (2.70%) | <0.001 |
| High school / GED | 74 (27.4%) | 139 (51.5%) | 55 (20.4%) | 2 (0.7%) | 270 (41.6%) | 18 (30.0%) | 25 (41.7%) | 14 (23.3%) | 3 (5.0%) | 60 (20.3%) | ||
| Some college | 55 (28.1%) | 112 (57.1%) | 29 (14.8%) | 0 (0.0%) | 196 (30.2%) | 14 (19.7%) | 33 (46.5%) | 20 (28.2%) | 4 (5.6%) | 71 (24.0%) | ||
| Bachelors or higher | 9 (20.9%) | 28 (65.1%) | 4 (9.3%) | 2 (4.7%) | 43 (6.63%) | 9 (5.7%) | 105 (66.9%) | 11 (7.0%) | 32 (20.4%) | 157 (53.0%) | ||
| Employed | 35 (32.1%) | 51 (46.8%) | 23 (21.1%) | 0 (0.0%) | 109 (16.2%) | 0.30 | 41 (14.7%) | 150 (54.0%) | 49 (17.6%) | 38 (13.7%) | 278 (93.6%) | 0.02 |
| Health insurance | 148 (26.9%) | 305 (55.4%) | 95 (17.2%) | 3 (0.5%) | 551 (85.2%) | 0.20 | 40 (14.3%) | 157 (56.1%) | 45 (16.1%) | 38 (13.6%) | 280 (95.6%) | 0.99 |
| Underlying medical conditions (≥1)‡ | 40 (20.6%) | 111 (57.2%) | 40 (20.6%) | 3 (1.5%) | 194 (28.9%) | 0.01 | 7 (11.1%) | 38 (60.3%) | 12 (19.0%) | 6 (9.5%) | 63 (21.2%) | 0.64 |
| Median enrollments per unique participant [Range] | 2.00 [1.00, 31.0] | 2.00 [1.00, 27.0] | 2.00 [1.00, 25.0] | 12.0 [3.00, 16.0] | 2.00 [1.00, 31.0] | 0.05 | 1.50 [1.00, 15.0] | 2.00 [1.00, 15.0] | 2.00 [1.00, 20.0] | 6.00 [1.00, 16.0] | 2.00 [1.00, 20.0] | <0.001 |
| Ever tested SARS-CoV-2 positive | 13 (19.7%) | 40 (60.6%) | 12 (18.2%) | 1 (1.5%) | 66 (10.4%) | 0.25 | 3 (21.4%) | 6 (42.9%) | 1 (7.1%) | 4 (28.6%) | 14 (5.05%) | 0.20 |
| Reason for no COVID-19 vaccine | ||||||||||||
| Concerns about vaccine safety | 60 (72.3%) | NA | 23 (27.7%) | NA | 83 (29.4%) | <0.001 | 14 (38.9%) | NA | 22 (61.1%) | NA | 36 (41.9%) | 0.005 |
| Need more information | 21 (28.8%) | NA | 52 (71.2%) | NA | 73 (25.9%) | 6 (26.1%) | NA | 17 (73.9%) | NA | 23 (26.7%) | ||
| Not worried about COVID-19 | 8 (72.7%) | NA | 3 (27.3%) | NA | 11 (3.90%) | 1 (50.0%) | NA | 1 (50.0%) | NA | 2 (2.33%) | ||
| Not enough time | 1 (50.0%) | NA | 1 (50.0%) | NA | 2 (0.71%) | 0 (0.0%) | NA | 0 (0.0%) | NA | 0 (0.0%) | ||
| Already had COVID-19 | 3 (100.0%) | NA | 0 (0.0%) | NA | 3 (1.06%) | 1 (100.0%) | NA | 0 (0.0%) | NA | 1 (1.16%) | ||
| Want to prioritize high-risk persons | 1 (100.0%) | NA | 0 (0.0%) | NA | 1 (0.35%) | 1 (33.3%) | NA | 2 (66.7%) | NA | 3 (3.49%) | ||
| Unlisted reason | 81 (74.3%) | NA | 28 (25.7%) | NA | 109 (38.7%) | 18 (72.0%) | NA | 7 (28.0%) | NA | 21 (24.4%) | ||
| Received this season's flu vaccine | 56 (19.2%) | 196 (67.4%) | 37 (12.7%) | 2 (0.7%) | 291 (45.0%) | <0.001 | 9 (5.4%) | 107 (63.7%) | 20 (11.9%) | 32 (19.0%) | 168 (57.5%) | <0.001 |
| Reason for no flu vaccine | ||||||||||||
| Concerns about vaccine safety | 32 (51.6%) | 18 (29.0%) | 12 (19.4%) | 0 (0.0%) | 62 (19.4%) | <0.001 | 4 (50.0%) | 1 (12.5%) | 2 (25.0%) | 1 (12.5%) | 8 (7.02%) | 0.02 |
| Not worried about flu | 10 (35.7%) | 8 (28.6%) | 10 (35.7%) | 0 (0.0%) | 28 (8.78%) | 8 (50.0%) | 3 (18.8%) | 4 (25.0%) | 1 (6.2%) | 16 (14.0%) | ||
| I plan to get the flu vaccine | 6 (12.8%) | 26 (55.3%) | 15 (31.9%) | 0 (0.0%) | 47 (14.7%) | 2 (6.9%) | 21 (72.4%) | 4 (13.8%) | 2 (6.9%) | 29 (25.4%) | ||
| Other reason§ | 72 (39.6%) | 83 (45.6%) | 26 (14.3%) | 1 (0.5%) | 182 (57.1%) | 16 (26.2%) | 27 (44.3%) | 15 (24.6%) | 3 (4.9%) |
|
||
Excludes participants that responded “Prefer not to say” when asked about vaccination intent.
All columns apart from “Total” have calculated row percentages; “Total” column percentages calculated exclude missing responses.
Underlying conditions include asthma, blood disorders, cancer, chronic obstructive pulmonary disease or emphysema, immunosuppression, liver disease, heart disease, diabetes, neurologic conditions or aspirin therapy.
Aggregated responses: “Do not have the time to get vaccinated” (n = 29); “Not required for work or school” (n = 2); “Not recommended by a doctor or healthcare worker” (n = 2); “Not covered by health insurance” (n = 3); “Not offered at a convenient location” (n = 12); “None of the above” (n = 195).
The median age of shelter residents and staff was 41 years (range: 18–85 years) and 33 years (range: 18–81 years), respectively. Most participants identified as White (40.5% residents, 53.2% staff) or Black/African American (37.4% residents, 26.3% staff). The majority of residents (63.6%) were male compared to 36.4% of staff. Among residents and staff, 78.4% and 97.3% indicated that they had a high school education or higher, respectively. The majority (56.4%) of residents reported chronic homelessness, and 83.2% were unemployed; 28.9% had one or more underlying medical conditions. At their last survey response, 45.0% of residents and 57.5% of staff reported receiving influenza vaccine for the 2020–2021 influenza season. Prior to widespread COVID-19 vaccine eligibility within this population, four (0.6%) residents had received at least one COVID-19 vaccine dose as of their last survey response compared to 39 (13.1%) staff (Table 2).
3.2. COVID-19 vaccination intent
Among residents, 53.7% (n = 361) were vaccine accepting, 28.1% (n = 189) reluctant, 17.6% (n = 118) deliberative, and 0.6% (n = 4) already vaccinated, whereas among staff, 56.2% (n = 167) were vaccine accepting, 14.1% (n = 42) reluctant, 16.5% (n = 49) deliberative, and 13.1% (n = 39) already vaccinated at last survey (Table 2). The majority of participants who were COVID-19 vaccine accepting were White (62.0% residents, 87.8% staff) and Hispanic or Latino (61.0% residents, 69.0% staff). Among those with a high school education and above (n = 821), vaccine acceptance increased with each level of educational attainment (51.5% to 65.1% among residents, 41.7% to 66.9% among staff). Of the residents who previously tested positive for SARS-CoV-2 (n = 66), 60.6% reported COVID-19 vaccine acceptance, compared to 53.6% among those who did not (n = 567). Of the residents who reported receiving influenza vaccine (n = 291), 67.4% reported COVID-19 vaccine acceptance, compared to 43.4% among those who did not report influenza vaccination (n = 355).
3.3. Reasons for COVID-19 vaccine deliberation or reluctance
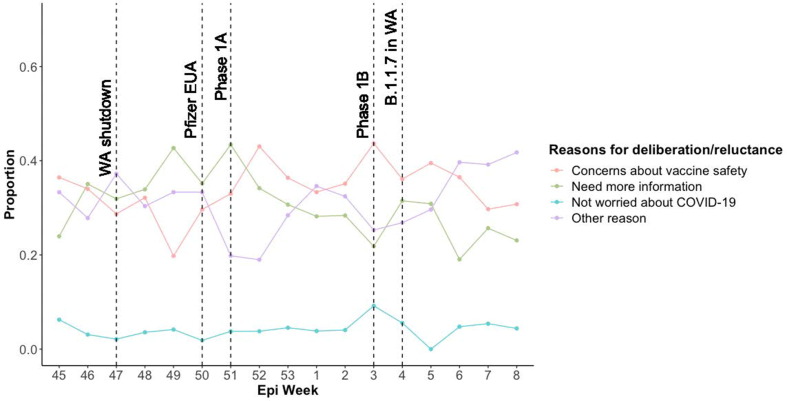
Among residents who were vaccine deliberative at last survey (n = 118), the most common primary reason reported was that they needed more information (48.6%), whereas vaccine deliberative staff were most commonly concerned about vaccine safety (46.8%; Table 2). Among those who were COVID-19 vaccine reluctant, “Other reason” (n = 140) was the most common reason given (49.1% residents, 46.2% staff), followed by concerns about vaccine safety (34.3% residents, 35.9% staff). The following reasons were aggregated into the singular “Other reason” category due to low number of responses: “Do not have time to get vaccinated” (n = 2); “Want to make sure high-risk individuals get it first” (n = 4); “I’ve already had COVID-19 and don’t think I need the vaccine” (n = 4); and “None of the above” (n = 130). Of the aggregated “Other reason” responses, 92.9% cited “None of the above” as their primary reason for COVID-19 vaccine deliberation or reluctance (Fig. 1b).
Fig. 1b.
Proportion of survey responses citing primary reason for COVID-19 vaccine deliberation or reluctance, by CDC Epidemiological Week (N = 1476)*. (*Overlaid key events are detailed in Supplemental Table 1 in chronological order; Does not include responses from those already vaccinated (n = 75) or those that answered “yes” (n = 2293); Overall proportion of responses that were included as “Other reason”: “Do not have time to get vaccinated” (0.3%); “Want to make sure high-risk individuals get it first” (1.2%); “I’ve already had COVID-19 and don’t think I need the vaccine” (2.3%); “None of the above” (27.2%).)
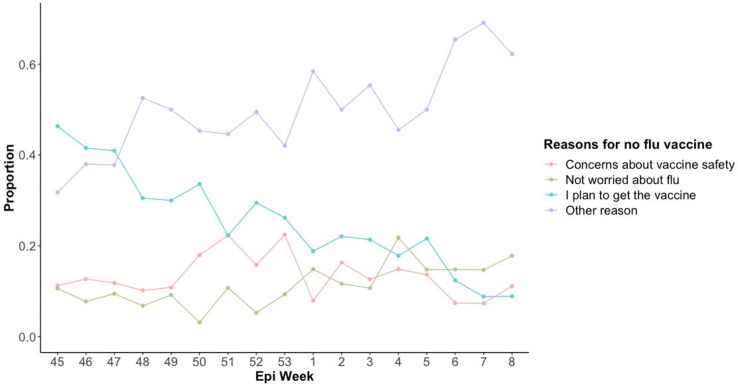
The most common primary reason for not receiving influenza vaccination was “Other reason” (n = 243), among both residents (57.1%) and staff (53.5%). The following reasons were aggregated into the singular “Other reason” category due to low number of responses: “Do not have the time to get vaccinated” (n = 29); “Not required for work or school” (n = 2); “Not recommended by a doctor or healthcare worker” (n = 2); “Not covered by health insurance” (n = 3); “Not offered at a convenient location” (n = 12); “None of the above” (n = 195). Of the aggregated “Other reason” responses, 80.2% cited “None of the above.” Among residents, 19.4% had concerns about influenza vaccine safety and 8.8% were not worried about influenza. Among staff, 14.0% were not worried about influenza compared to 7.0% concerned about vaccine safety.
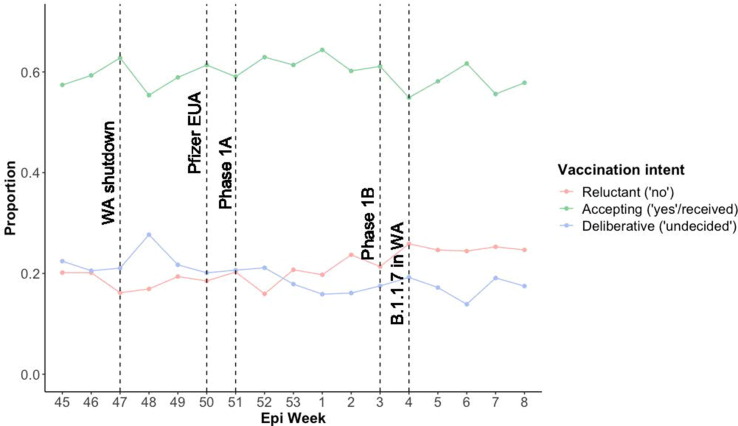
3.4. COVID-19 vaccination intent over time
When examining population-level changes in vaccination intent and uptake by week, we observed no evident temporal trend of COVID-19 vaccine intent corresponding with events of interest (Fig. 1a ). We observed a slight increase in vaccine reluctance as the proportion of vaccine deliberation decreased over the study period. Generally, we did not observe changes in reasons for vaccine deliberation or reluctance that corresponded with events of interest (Fig. 1b). However, there was a peak in the proportion of those indicating a need for more information the week following the Emergency Use Authorization (EUA) for the BNT162b2 mRNA (Pfizer) COVID-19 vaccine (43.4%, 95% CI 0.34–0.53), with a downward trend through the end of the study period. The proportion of those indicating “Other reason” was highest in the study’s final week (41.8%, 95% CI 0.32–0.53). Of the aggregated survey responses across the study period, 27.2% cited “None of the above” as the primary reason for COVID-19 vaccine deliberation or reluctance, which remained consistent over time.
Fig. 1a.
Proportion of survey responses for COVID-19 vaccine uptake when it becomes available, by Centers for Disease Control & Prevention (CDC) Epidemiological Week (N = 3966)*. (*Overlaid key events are detailed in Supplemental Table 1 in chronological order.)
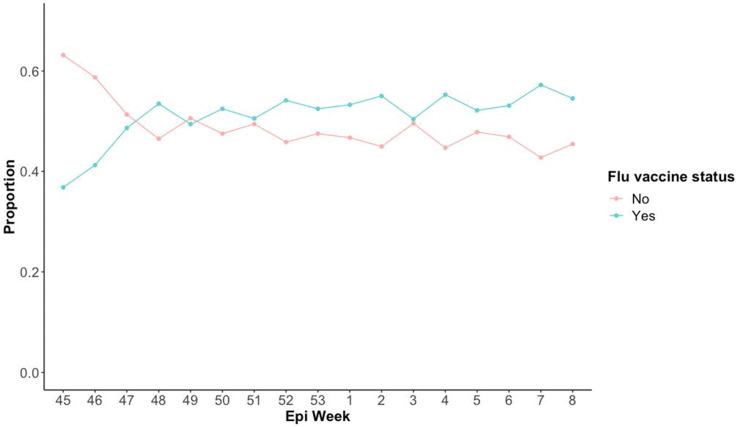
The proportion of survey responses indicating seasonal influenza vaccine receipt first surpassed those that did not in Epidemiological Week 48 (Fig. 1c ). Among 1768 (44.6%) survey responses from participants who had not already received their influenza vaccine, we observed a decrease in those still planning to receive it and an increase in “Other reasons” for no influenza vaccination (Fig. 1d ).
Fig. 1c.
Proportion of survey responses for seasonal flu vaccine uptake, by CDC Epidemiological Week (N = 3889)*. (*Does not include responses from those that answered “Prefer not to say” when asked about seasonal influenza vaccine status (n = 77).)
Fig. 1d.
Proportion of survey responses citing primary reason for not receiving seasonal flu vaccine, by CDC Epidemiological Week (N = 1768)*. (*Does not include responses from those already vaccinated against seasonal flu (n = 1977) or those that answered “prefer not to say” (n = 144), Overall proportion of responses that were included as “Other reason”: “Do not have the time to get vaccinated” (4.2%); “Not required for work or school” (0.4%); “Not recommended by a doctor or healthcare worker” (0.2%); “Not covered by health insurance” (0.4%); “Not offered at a convenient location” (2.9%); “None of the above” (40%).)
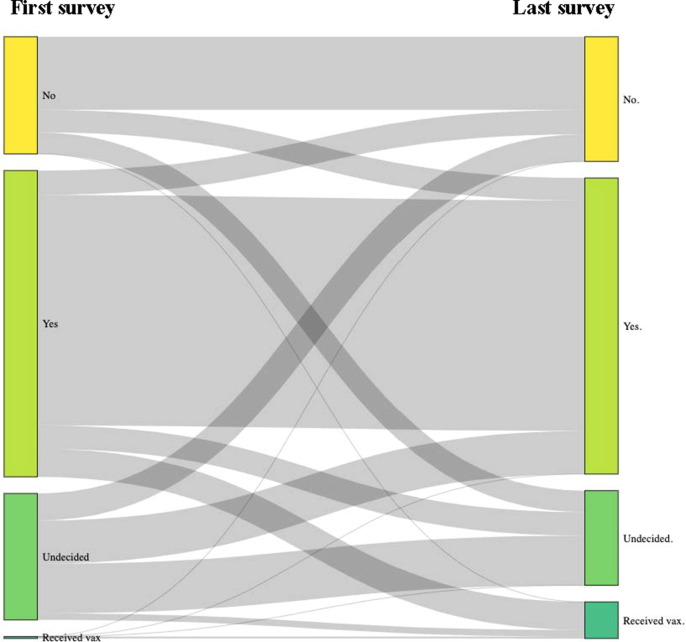
Of the 589 unique participants who completed at least two surveys over the study period, 173 (29.4%) changed their intent to receive a COVID-19 vaccine between first and last response (Fig. 2 ; Supplemental Fig. 1). Of the 135 participants who were vaccine deliberative in their first survey, 60 (44.4%) remained deliberative, 46 (34.1%) became vaccine accepting and 29 (21.5%) vaccine reluctant by their last survey. Among the 125 who were initially vaccine reluctant, 78 (62.4%) remained reluctant, 23 (18.4%) became deliberative, and 24 (19.2%) became vaccine accepting. Of the 329 who were initially vaccine accepting, 25 (7.6%) became deliberative and 26 (7.9%) became reluctant.
Fig. 2.
Sankey diagrams of COVID-19 vaccination intent vacillation, based on first and last survey response (N = 589).
Initial vaccine deliberation compared to initial vaccine acceptance was associated with increased odds of final vaccine deliberation (aOR = 11.34, 95% CI 6.41–20.05) and final vaccine reluctance (aOR = 5.96, 95% CI 3.22–11.04), as compared to final vaccine acceptance. Initial vaccine reluctance compared to initial vaccine acceptance was associated with increased odds of final vaccine deliberation (aOR = 9.43, 95% CI 4.66–19.08) and final vaccine reluctance compared to final vaccine acceptance (aOR = 30.75, 95% CI 16.70–56.62) (Table 3 ). Therefore, initial vaccine deliberation and reluctance was highly associated with remaining deliberative or reluctant.
Table 3.
Multinomial logistic model predicting intent to receive COVID-19 vaccine at last survey response based on first response (N = 587).*
| Last Survey (ref = vaccine accepting) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Vaccine deliberative |
Vaccine reluctant |
Received at least one vaccine dose |
|||||||
| First Survey (ref. = vaccine accepting) | aOR† | 95% CI | P-value | aOR | 95% CI | P-value | aOR | 95% CI | P-value |
| Vaccine deliberative | 11.34 | 6.41–20.05 | <0.001 | 5.96 | 3.22–11.04 | <0.001 | 1.25 | 0.52–3.01 | 0.622 |
| Vaccine reluctant | 9.43 | 4.66–19.08 | <0.001 | 30.75 | 16.70–56.62 | <0.001 | NA | NA | NA |
Excludes participants vaccinated at first response.
aOR = adjusted odds ratio.
3.5. Factors associated with COVID-19 vaccine deliberation or reluctance
Based on unique participants’ last survey (n = 752), our multivariate multinomial model showed that no prior influenza vaccination during the 2020–2021 season, Black/African American race, and education level lower than bachelor’s degree were significantly associated with COVID-19 vaccine deliberation or reluctance as distinct vaccine attitude categories (Table 4 ). Adjusting for other variables, participants who had received that season’s influenza vaccine had a 57% (aOR = 0.43, 95% CI 0.27–0.67) lower odds of COVID-19 vaccine deliberation and a 64% (aOR = 0.36, 95% CI 0.24–0.53) lower odds of COVID-19 vaccine reluctance compared with those who had not received influenza vaccine. Black/African American race was associated with a nearly 2.5-times higher odds of COVID-19 vaccine reluctance (aOR = 2.47, 95% CI 1.57–3.88) and 1.7-times higher odds of COVID-19 vaccine deliberation compared to those identifying as White. Having attended some college, high school, and less than high school were each associated with higher odds of deliberation and reluctance compared to those with a bachelor’s degree or higher.
Table 4.
Multivariate predictors of vaccine deliberation or vaccine reluctance regarding intent to be vaccinated, according to multinomial model, based on last survey response (N = 752).*
| Vaccine deliberative (“undecided” vs. “yes/received”) |
Vaccine reluctant (“no” vs. “yes/received”) |
|||||
|---|---|---|---|---|---|---|
| Characteristic | aOR† | 95% CI | P-value | aOR | 95% CI | P-value |
| Age group | ||||||
| 18–49 y | 1.03 | 0.41–2.62 | 0.947 | 1.75 | 0.72–4.24 | 0.215 |
| 50–64 y | 0.72 | 0.26–1.94 | 0.511 | 0.90 | 0.34–2.33 | 0.824 |
| ≥ 65 y | Reference | Reference | ||||
| Race | ||||||
| American Indian/ Alaska Native | 1.98 | 0.61–6.49 | 0.257 | 3.20 | 1.13–9.02 | 0.028 |
| Asian | 0.34 | 0.08–1.52 | 0.157 | 0.63 | 0.20–1.94 | 0.418 |
| Black/African American | 1.69 | 1.02–2.78 | 0.040 | 2.47 | 1.57–3.88 | <0.001 |
| Multiple | 0.94 | 0.36–2.41 | 0.892 | 2.41 | 1.17–4.96 | 0.017 |
| Native Hawaiian/ Pacific Islander | 1.01 | 0.35–2.88 | 0.987 | 1.32 | 0.54–3.25 | 0.540 |
| White | Reference | Reference | ||||
| Ethnicity | ||||||
| Hispanic or Latino | 1.29 | 0.59–2.82 | 0.524 | 0.50 | 0.21–1.20 | 0.120 |
| Non-Hispanic or Latino | Reference | Reference | ||||
| Sex | ||||||
| Female | 2.26 | 1.42–3.60 | 0.001 | 1.45 | 0.96–2.17 | 0.076 |
| Male | Reference | Reference | ||||
| Participant type | ||||||
| Resident | 1.41 | 0.68–2.91 | 0.358 | 1.96 | 1.00–3.83 | 0.048 |
| Staff | Reference | Reference | ||||
| Highest education level | ||||||
| Less than high school | 3.90 | 1.46–10.36 | 0.006 | 3.51 | 1.54–8.03 | 0.003 |
| High school / GED | 4.69 | 2.06–10.69 | <0.001 | 3.34 | 1.63–6.86 | 0.001 |
| Some college | 4.56 | 2.03–10.27 | <0.001 | 3.38 | 1.66–6.90 | 0.001 |
| Bachelors or higher | Reference | Reference | ||||
| Employed | ||||||
| Yes | 1.43 | 0.76–2.68 | 0.269 | 1.11 | 0.63–1.93 | 0.723 |
| No | Reference | Reference | ||||
| Underlying medical conditions (≥1)‡ | ||||||
| Yes | 1.36 | 0.84–2.21 | 0.211 | 0.77 | 0.48–1.23 | 0.268 |
| No | Reference | Reference | ||||
| Enrollments per unique participant | ||||||
| 2 | 0.79 | 0.40–1.56 | 0.496 | 0.54 | 0.29–0.99 | 0.045 |
| 3–5 | 1.02 | 0.57–1.83 | 0.949 | 1.05 | 0.64–1.71 | 0.846 |
| ≥6 | 1.23 | 0.69–2.18 | 0.488 | 0.76 | 0.45–1.28 | 0.304 |
| 1 | Reference | Reference | ||||
| Prior SARS-CoV-2 positive test | ||||||
| Yes | 0.63 | 0.29–1.36 | 0.242 | 0.50 | 0.25–1.00 | 0.049 |
| No | Reference | Reference | ||||
| Received flu vaccine | ||||||
| Yes | 0.43 | 0.27–0.67 | <0.001 | 0.36 | 0.24–0.53 | <0.001 |
| No | Reference | Reference | ||||
Based on complete case responses (N = 752); responses “yes” or “received vaccine” combined is the reference group for the outcome.
aOR = adjusted odds ratio.
Underlying conditions include asthma, blood disorders, cancer, chronic obstructive pulmonary disease or emphysema, immunosuppression, liver disease, heart disease, diabetes, neurologic conditions or aspirin therapy.
Females were more likely to be vaccine deliberative compared to males (aOR = 2.26, 95% CI 1.42–3.60), however female sex was not significantly associated with greater vaccine reluctance. Factors associated with vaccine reluctance, but not vaccine deliberation, included identifying with multiple races (aOR = 2.41, 95% CI 1.17–4.96) compared to White race and being a shelter resident (aOR = 1.96, 95% CI 1.00–3.83) compared to staff. American Indian and Alaska Native (AIAN) race was also identified with a significant association, however the validity of this finding is undermined by the small sample size of AIAN respondents.
4. Discussion
Intent to be vaccinated against COVID-19 was low and similar among homeless shelter residents and staff in this community-based study conducted over four months prior to widespread vaccine availability in the Seattle metropolitan area. Overall, 54% of shelter residents and 56% of staff were vaccine accepting, compared with 74% of adults in the Seattle metropolitan area as of early February 2021 [21]. A survey conducted among PEH in Los Angeles between December 2020 and February 2021 reported 48% of respondents being vaccine hesitant (defined as having refused, or intending to refuse, a vaccine when offered), however change in attitude over time was not assessed [22]. Studies regarding PEH acceptance of vaccines against other pathogens were also lower when compared to the general population [7], [23], [24]. The substantial discrepancy in vaccine intent between our study population and the general population suggests the importance of tailored interventions by regional housing coordination bodies and homeless service providers to engage shelter residents and staff regarding COVID-19 vaccines.
Factors most strongly associated with COVID-19 vaccine deliberation or reluctance in our study included Black/African American race; lower educational attainment; and not having received seasonal influenza vaccine. Race as a factor associated with low COVID-19 vaccine intent is a consistent finding [25], [26], and has been contextualized as a symptom of underlying structural racism [18]. A study conducted among U.S. adults found 21% higher COVID-19 vaccine hesitancy among those who experienced racial discrimination compared to those who had not [27]. Racial disparities have also been persistent in influenza vaccination coverage among U.S. adults [28], [29]. Higher hesitancy (42.9%) among adults without a college degree [16] and lower hesitancy among those who received an influenza vaccine (94% lower odds) [26] were also observed in nationally representative surveys. These two factors could be useful in prioritizing messaging and outreach at shelters. We were not able to conclude that racial and educational inequities are more strongly associated with vaccine deliberation/reluctance than unhoused status due to small sample sizes for several independent variables. However, we explored separate unadjusted regression models and found comparable associations among residents and staf. This suggests a need for PEH vaccine campaigns to address these factors concurrently.
Our study highlights changes in shelter residents and staff intent to be vaccinated against COVID-19 over the study period before widespread vaccine availability. Overall fluctuation of COVID-19 vaccine acceptance prior to availability has similarly been documented in the general U.S. population (71% in May 2020, 51% in September 2020, and 69% in February 2021), with demographic and socioeconomic divides [13]. In another nationally representative study that did not detect this fluctation, the largest increase in COVID-19 vaccine acceptance was observed among Hispanic and Black respondents, while acceptance remained low among those with lower educational status [15], [16]. However, we did not observe discrepancies when we explored changes in vaccine intent between subgroups in our study population. Contrary to our initial hypothesis, we did not observe an increase in vaccination intent and decrease in “need for more information” as time since EUA of COVID-19 vaccines and state-wide eligibility increased. This suggests that risk perception of COVID-19 disease may be an important unmeasured factor associated with vaccine intent, as observed in other populations [30]. For example, a study in France provides evidence that vaccination refusal is strongly associated with a lower perceived risk of severe COVID-19 and that overall intention is likely dependent on available vaccine characteristics [31], while another study in Italy found that vaccine acceptance increased as COVID-19 risk perception increased during lockdowns [32]. This suggests that temporal trends in vaccine intent are not unique to PEH or shelter staff, and may reflect larger behavioral trends, including documented fluidity of vaccine intent [15], [16].
These findings are subject to several limitations. First, the study employed a repeated cross-sectional design and thus surveys were not conducted on the same calendar dates, but rather when the participant first and last enrolled. Challenges in linking survey records (e.g., due to participants providing inconsistent identifiable information) likely resulted in an overestimation of unique participants. Data were collected during the beginning of public COVID-19 vaccine rollout and may not reflect current vaccination intent. Results may also be subject to selection bias as vaccine intent among those willing to accept SARS-CoV-2 testing and interact with study staff may not reflect the intention of those unwilling to be tested. Furthermore, information bias may be present due to self-report, as well as social desirability bias and changes in comfort with study staff over time. Nondifferential misclassification of underlying medical conditions associated with severe COVID-19 disease may also contribute to attenuation of true associations as high blood pressure and obesity were not captured by the survey. Due to small sample size, we were not able to assess interaction terms in our multinomial multivariate model for potential effect modification. The increasing proportion of participants citing “Other reason” (specifically “None of the above”) for why they are vaccine deliberative or reluctant may reflect the limited scope of our categorical responses, which did not extend to referencing past negative experience and diminished trust in healthcare systems. It may also represent survey fatigue, as this response was similarly high among those unvaccinated against influenza. Despite including options of “Prefer not to say” and assurances that data would not be shared with shelter administration, there may have been a tendency to respond favorably among residents due to fear of losing access to shelter services. Finally, these findings may not be representative of all King County shelters or generalizable to PEH in other locations and do not allow us to examine factors associated with deliberation or reluctance by resident versus staff.
4.1. Investigator positionality statement
In the spirit of reflexivity, we acknowledge the role that our socioeconomic positions and experiences may contribute to data presentation and interpretation. Co-authors have extensive experience conducting vaccine research and public health practice to improve health equity in Seattle-King County. Among co-authors, there is some familial and personal lived experience of homelessness.
5. Public health implications
This study provides critical data on low COVID-19 vaccination intent among residents and staff in homeless shelters, with no increase in vaccination intent between November 2020 and February 2021. Strong disparities in vaccination intent associated with education and race suggest that these factors should be considered as part of an intersectional approach to address health inequities by public health authorities planning vaccination campaigns in shelters. Suggested interventions include: (1) partnering with trusted organizations and those with lived experience to build relationships and deliver transparent health messaging between the community and medical institutions; (2) mobile units and community vaccination events for equitable vaccine distribution; (3) favoring person-to-person practices over reliance on web-based technology; (4) trauma-informed engagement strategies attuned to racial and socioeconomic disparities; and (5) offering flexible, non-punitive sick leave options (e.g., paid sick leave) for employees to get vaccinated and for those with symptoms after vaccination [18]. Evidence of these approaches’ success are seen in their deployment by tribal communities and Urban Indian organizations [33], [34]. More studies, specifically employing qualitative methodologies, are needed to evaluate the role of structural racism and low health literacy on vaccine attitudes among shelter residents and staff. Our findings support a need for continued dialogue and a person-centered approach to understanding the sociocultural complexities and dynamism of vaccine attitudes at shelters so that residents and staff may feel more receptive to make informed choices about the risks and benefits of vaccination.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: [Helen Y. Chu reports financial support was provided by Centers for Disease Control and Prevention. James P. Hughes reports a relationship with National Institutes of Health that includes: funding grants. Michael L. Jackson, Janet A. Englund, Helen Y. Chu reports a relationship with Sanofi Pasteur that includes: consulting or advisory and funding grants. Michael Boeckh reports a relationship with Moderna Therapeutics Inc that includes: consulting or advisory. Michael Boeckh reports a relationship with VirBio that includes: consulting or advisory and funding grants. Michael Boeckh, Janet A. Englund, Helen Y. Chu reports a relationship with Merck & Co Inc that includes: consulting or advisory and funding grants. Michael Boeckh reports a relationship with Regeneron Pharmaceuticals Inc that includes: funding grants. Michael Boeckh reports a relationship with Ridgeback Biotherapeutics L.P. that includes: funding grants. Michael Boeckh, Helen Y. Chu reports a relationship with Bill and Melinda Gates Foundation that includes: consulting or advisory and funding grants. Janet A. Englund reports a relationship with AstraZeneca that includes: consulting or advisory and funding grants. Janet A. Englund, Helen Y. Chu reports a relationship with GlaxoSmithKline that includes: consulting or advisory and funding grants. Janet A. Englund reports a relationship with Novavax Inc that includes: funding grants. Janet A. Englund, Helen Y. Chu reports a relationship with Pfizer Inc that includes: consulting or advisory and funding grants. Janet A. Englund reports a relationship with Meissa Vaccines that includes: consulting or advisory. Helen Y. Chu reports a relationship with Ellumen Inc that includes: consulting or advisory and funding grants. Helen Y. Chu reports a relationship with Gates Ventures that includes: funding grants. Helen Y. Chu reports a relationship with Cepheid that includes: funding grants.].
Acknowledgments
Acknowledgements
We thank the shelter staff and program managers for their cooperation and collaboration throughout the participant recruitment process. A special thanks to all participants and the research assistants who assisted with data collection.
All authors attest they meet the ICMJE criteria for authorship.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.11.026.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Kuehn B.M. Homeless Shelters Face High COVID-19 Risks. JAMA - J Am Med Assoc. 2020;323(22):2240. doi: 10.1001/jama.2020.8854. [DOI] [PubMed] [Google Scholar]
- 2.Imbert E., Kinley P.M., Scarborough A., et al. Coronavirus Disease 2019 Outbreak in a San Francisco Homeless Shelter. Clin Infect Dis. 2020;(Aug) doi: 10.1093/cid/ciaa1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leung C.S., Ho M.M., Kiss A., Gundlapalli A.V., Hwang S.W. Homelessness and the response to emerging infectious disease outbreaks: Lessons from SARS. J Urban Heal. 2008;85(3):402–410. doi: 10.1007/s11524-008-9270-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henry M, de Soussa T, Roddey C, Gaywen S, Bednar TJ. The 2020 Annual Homeless Assessment Report (AHAR) to Congress. Washington, D.C.; 2021. https://www.huduser.gov/portal/sites/default/files/pdf/2020-AHAR-Part-1.pdf.
- 5.Sutherland H, Rosenoff E. Individuals Experiencing Homelessness Are Likely to Have Medical Conditions Associated with Severe Illness from COVID-19 Issue Brief. Washington, D.C. https://aspe.hhs.gov/basic-report/individuals-experiencing-homelessness-are-likely-have-medical-conditions-associated-severe-illness-covid-19-issue-brief.
- 6.Liu C.Y., Chai S.J., Watt J.P. Communicable Disease among People Experiencing Homelessness in California. Epidemiol Infect. 2020;148(e85) doi: 10.1017/S0950268820000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buechler Connor R., Ukani Anita, Elsharawi Radwa, Gable Jessica, Petersen Anneliese, Franklin Michael, et al. Barriers, beliefs, and practices regarding hygiene and vaccination among the homeless during a hepatitis A outbreak in Detroit, MI. Heliyon. 2020;6(3):e03474. doi: 10.1016/j.heliyon.2020.e03474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coady M.H., Galea S., Blaney S., Ompad D.C., Sisco S., Vlahov D. Project VIVA: A multilevel community-based intervention to increase influenza vaccination rates among hard-to-reach populations in New York City. Am J Public Health. 2008;98(7):1314–1321. doi: 10.2105/AJPH.2007.119586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beers L., Filter M., McFarland M. Increasing influenza vaccination acceptance in the homeless: a quality improvement project. Nurse Pract. 2019;44(11):48–54. doi: 10.1097/01.NPR.0000586012.31046.c9. [DOI] [PubMed] [Google Scholar]
- 10.Story A., Aldridge R.W., Gray T., Burridge S., Hayward A.C. Influenza vaccination, inverse care and homelessness: cross-sectional survey of eligibility and uptake during the 2011/12 season in London. BMC Public Health. 2014;14(1) doi: 10.1186/1471-2458-14-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polack Fernando P., Thomas Stephen J., Kitchin Nicholas, Absalon Judith, Gurtman Alejandra, Lockhart Stephen, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baden Lindsey R., El Sahly Hana M., Essink Brandon, Kotloff Karen, Frey Sharon, Novak Rick, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Funk C, Tyson A. Growing Share of Americans Say They Plan to Get a COVID-19 Vaccine - or Already Have. Washington, D.C.; 2021. https://www.pewresearch.org/science/2021/03/05/growing-share-of-americans-say-they-plan-to-get-a-covid-19-vaccine-or-already-have/.
- 14.Malik A.A., McFadden S.A.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Does the Public Want To Get a COVID-19 Vaccine? When?; 2021. https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard/.
- 16.Daly M., Jones A., Robinson E. Public Trust and Willingness to Vaccinate Against COVID-19 in the US From October 14, 2020, to March 29, 2021. Jama. 2021 doi: 10.1001/jama.2021.8246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rogers Julia H., Link Amy C., McCulloch Denise, Brandstetter Elisabeth, Newman Kira L., Jackson Michael L., et al. Characteristics of COVID-19 in homeless shelters: a community-based surveillance study. Ann Intern Med. 2021;174(1):42–49. doi: 10.7326/M20-3799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corbie-Smith G. Vaccine Hesitancy Is a Scapegoat for Structural Racism. JAMA Heal Forum. 2021;2(3):e210434. doi: 10.1001/jamahealthforum.2021.0434. [DOI] [PubMed] [Google Scholar]
- 19.Paasche-Orlow M.K., Parker R.M., Gazmararian J.A., Nielsen-Bohlman L.T., Rudd R.R. The prevalence of limited health literacy. J Gen Intern Med. 2005;20(2):175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sariyar M, Borg A. RecordLinkage: Record Linkage Functions for Linking and Deduplicating Data Sets; 2020.
- 21.Week 24 Household Pulse Survey: February 3 - February 15. Washington, D.C.; 2021 https://www.census.gov/data/tables/2021/demo/hhp/hhp24.html.
- 22.Kuhn R, Henwood B, Lawton A, et al. COVID-19 vaccine access and attitudes among people experiencing homelessness from pilot mobile phone survey in Los Angeles, CA. medRxiv. January 2021:2021.03.23.21254146. 10.1101/2021.03.23.21254146. [DOI] [PMC free article] [PubMed]
- 23.People at High Risk For Flu Complications. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/highrisk/index.htm.
- 24.Adult Immunization: Shots to Save Lives. Washington, D.C.; 2010.
- 25.Nguyen K.H., Srivastav A., Razzaghi H., et al. COVID-19 Vaccination Intent, Perceptions, and Reasons for Not Vaccinating Among Groups Prioritized for Early Vaccination — United States, September and December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(6):217–222. doi: 10.15585/mmwr.mm7006e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann Intern Med. 2020;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Savoia E, Piltch-Loeb R, Goldberg B, et al. Predictors of COVID-19 Vaccine Hesitancy: Socio-demographics, Co-Morbidity and Past Experience of Racial Discrimination. medRxiv. January 2021:2021.01.12.21249152. 10.1101/2021.01.12.21249152. [DOI] [PMC free article] [PubMed]
- 28.Lu P, Hung M, Srivastav A, Grohskopf LA. Surveillance of Vaccination Coverage Among Adult Populations — United States, 2018. MMWR Surveill Summ. 2021;70(No.SS-3):1–26. 10.15585/mmwr.ss7003a1. [DOI] [PMC free article] [PubMed]
- 29.Flu Vaccination Coverage, United States, 2019-20 Influenza Season. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/fluvaxview/coverage-1920estimates.htm?web=1&wdLOR=cED5032D9-F784-4A45-A837-F9A1C117E375. Published 2020.
- 30.Lin C., Tu P., Beitsch L.M. Confidence and receptivity for covid-19 vaccines: a rapid systematic review. Vaccines. 2021;9(1):1–32. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Heal. 2021;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Caserotti M., Girardi P., Rubaltelli E., Tasso A., Lotto L., Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. 2021;272 doi: 10.1016/j.socscimed.2021.113688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Summary of COVID Vaccination among King County Residents. Seattle, WA; 2021. https://kingcounty.gov/depts/health/covid-19/data/vaccination.aspx.
- 34.Brown A. Indian Country Reaches 1M Vaccine Dosesss.; 2021. https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2021/04/06/indian-country-reaches-1m-vaccine-doses.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.