Abstract
Background: Since 2003, the University of Mississippi Medical Center has operated a robust telehealth emergency department (ED) network, TelEmergency, which enhances access to emergency medicine-trained physicians at participating rural hospitals. TelEmergency was developed as a cost-control measure for financially constrained rural hospitals to improve access to quality, emergency care. However, the literature remains unclear as to whether ED telehealth services can be provided at lower costs compared with traditional in-person ED services.
Introduction: Our objective was to empirically determine whether TelEmergency was associated with lower ED costs at rural hospitals when compared with similar hospitals without TelEmergency between 2010 and 2017.
Materials and Methods: A panel of data for 2010–2017 was constructed at the hospital level. Hospitals with TelEmergency (n = 14 hospitals; 112 hospital-years) were compared with similar hospitals that did not use TelEmergency from Arkansas, Georgia, Mississippi, and South Carolina (n = 102; 766 hospital-years), matched using Coarsened Exact Matching. The relationship between total ED costs and treatment (e.g., participation in TelEmergency) was predicted using generalized estimating equations with a Poisson distribution, a log link, an exchangeable error term, and robust standard errors.
Results: After controlling for ownership type, critical access hospital status, year, and size, TelEmergency was associated with an estimated 31.4% lower total annual ED costs compared with similar matched hospitals that did not provide TelEmergency.
Conclusions: TelEmergency utilization was associated with significantly lower total annual ED costs compared with similarly matched hospitals that did not utilize TelEmergency. These findings suggest that access to quality ED care in rural communities can occur at lower costs.
Keywords: TelEmergency, emergency medicine, rural health, rural hospital finances, telemedicine, telehealth
Introduction and Background
A lack of access to local emergency medical services is a life-threatening concern for a growing number of rural Americans. For many rural residents, emergency care is not available within the local community. Local emergency care is particularly important for time-sensitive, emergent conditions like heart attack, stroke, seizures, asthma, and chronic obstructive pulmonary disease, for which increased travel time can negatively impact health outcomes.1–3 With limited or no local access to emergency care, many rural Americans may forego care or travel farther distances to receive care.
Farther distance to care is associated with a host of adverse consequences. As distance to care increases, patients become less likely to receive care.4–6 Increased distance to care has also been associated with worsening of certain disease prognoses, worse quality of life, and ultimately, poorer health outcomes.5 These consequences are important for rural Americans needing emergency care because of the relatively large distances they must travel to receive care, and the transportation obstacles they face.4,6 For rural Americans, these problems have increased in recent years due, in part, to increasing rural hospital closures, resulting in growing health disparities. Compared with nonrural Americans, rural Americans have shorter life expectancies and generally worse health outcomes—and those disparities have worsened in recent decades.7
Rural hospitals aim to deliver high-quality access to emergency services, but are often limited in the scope of services that can be provided within the community. These hospitals serve a population that accounts for only 17% of the U.S. population, but are distributed across 97% of the U.S. land mass.8 Compared with nonrural hospitals, low patient volumes, poor payer mix, and isolation from specialist consulting services4,9,10 can make it difficult for rural hospitals to survive. Since 2010, over 130 rural hospitals in the United States have closed,11 and over a third of all rural hospitals are currently at risk of closure.12 Such an environment can make it difficult for many rural hospitals to continue providing emergency services. Telehealth for emergency care may be one cost-effective alternative for rural hospitals to continue providing access to local emergency care, while also improving one dimension of financial performance (e.g., reducing costs).13–17
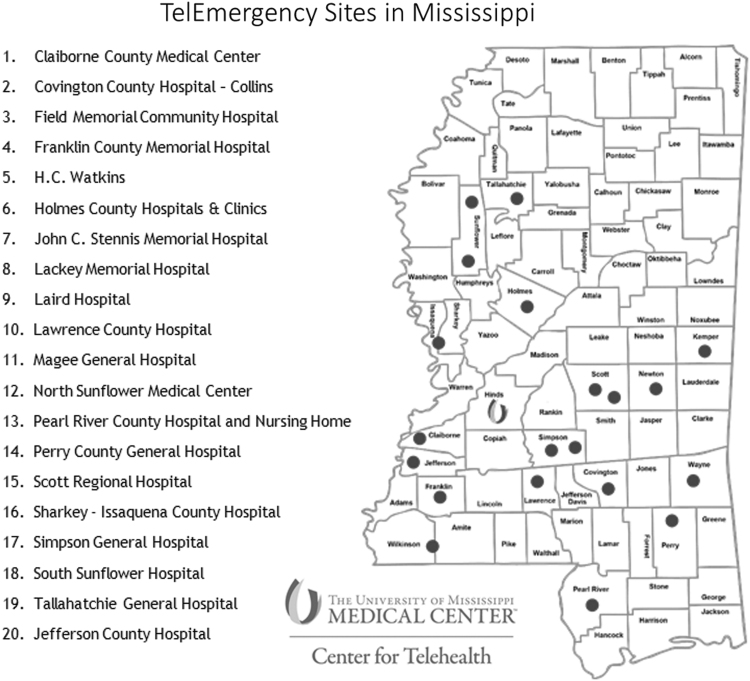
In an effort to stabilize financial performance at many financially fragile rural Mississippi (MS) hospitals and enhance local access to quality emergency care within those communities, the University of Mississippi Medical Center (UMMC) developed a telehealth program, TelEmergency, for use in rural and critical access hospital (CAH) emergency departments (EDs). Beginning in 2003 with one remote site, this hub-and-spoke model has grown to 20 remote rural hospital sites (Fig. 1). As the only academic medical center and Level-1 trauma center in MS, UMMC operates a high-volume ED and staffs emergency medicine (EM)-trained, board-certified physicians (e.g., the hub). Each remote ED site (e.g., the spokes) is staffed by nurse practitioners (NPs), who have completed additional training in EM through the hub.18 Further detail on the TelEmergency model has been described in previous work.18–20
Fig. 1.
The U-shaped emblem represents the location of the UMMC hub hospital in Jackson, MS. Dots with numbers represent the name and location of the 20 spoke hospitals using TelEmergency. UMMC, University of Mississippi Medical Center.
UMMC executives were motivated to create and expand this unique TelEmergency delivery system across rural MS for four key reasons, outlined in Table 1. First, UMMC leaders were motivated to maintain or expand access to EM care within rural MS communities. Second, they wanted to ensure that the highest quality of EM was provided. Third, they wanted to stabilize financially distressed rural MS hospitals. Fourth, they wanted to mitigate the cost and financial risk to UMMC while achieving these objectives.
Table 1.
University of Mississippi Medical Center TelEmergency Motives and Benefits
| TELEMERGENCY | |||
|---|---|---|---|
| MOTIVES | BENEFITS | BARRIERS | SOLUTIONS |
| 1. Maintain or bolster access to ED care within rural communities | Local ED care remained in all communities using TelEmergency without a reduction in the volume of care provided. | Scope of NPs previously limited to physician oversight within 15 miles. | UMMC obtained a waiver of this requirement for TelEmergency from relevant MS oversight authorities. |
| 2. Enhance quality of ED care provided within rural communities | Increased access to EM-trained, board-certified physicians and specially trained NPs. | ||
| Achieved a high-degree of satisfaction from patients and hospital administrators.18 | |||
| 3. Stabilize financial performance at financially fragile rural MS hospitals | None of the hospitals using TelEmergency closed. | Historically, telehealth reimbursement was restrictive, particularly for ED care. | A 2013 MS state-level telehealth parity law expanded telehealth reimbursement across all payers. |
| a. Cut rural ED expenses (e.g., physician staffing, inventory management) | By coordinating ED care through the hub, fewer physicians were staffed. | ||
| The TelEmergency inventory protocols decreased unnecessary inventory held. | |||
| b. Concerns for cuts to CAH reimbursement | Improving the profitability of one service line, emergency care, eases concerns for CAH reimbursement changes. | ||
| 4. Mitigate financial investment by UMMC to achieve prior objectives | Stabilizing access to ED care through TelEmergency was one reason UMMC did not have to make substantial capital investments to acquire those rural hospitals, which may have otherwise closed. | ||
| Led to better downstream population health management. | |||
CAH, critical access hospital; ED, emergency department; EM, emergency medicine; MS, Mississippi; NP, nurse practitioner; UMMC, University of Mississippi Medical Center.
TelEmergency provides a number of benefits for participating rural hospitals related to quality, access, and costs. While rural hospitals historically experience difficulty employing EM-trained, board-certified physicians, and at times, any physicians to staff the ED, TelEmergency has delivered consistent 24-h access to specialty-trained physicians.18 This quality improvement has been supplemented by achieving high levels of satisfaction for patients and administrators.18
Several financial improvements at rural hospitals related to TelEmergency were recognized as well. By coordinating EM care through the hub location, fewer physicians were necessary to provide care to all spoke sites, reducing staff costs. Additionally, the TelEmergency inventory protocols decreased unnecessary inventory held at rural hospitals, decreasing inventory costs. For example, these protocols reduced the supply of otoscopes and stethoscopes, medications, and various sizes of medical equipment stocked at each rural hospital (G. Hall, pers. comm.).
To address inconsistent reimbursement policies for tele-emergency services compared with in-person services,21 the state of MS adopted a telemedicine parity law in 201322 that requires all private and public payers to cover all telehealth services deemed medically necessary. This expanded reimbursement for telehealth across all payers. While these cost reductions and revenue benefits have been observed anecdotally, they have not been tested or quantified empirically.
The objective of this study was to empirically determine whether TelEmergency utilization was associated with lower ED costs at rural hospitals when compared with similar hospitals without TelEmergency between 2010 and 2017. We hypothesize that TelEmergency utilization lowers ED costs at rural hospitals. We expect this to occur because of the specific initiatives previously described in Table 1, as well as structural changes in the local community health system related to providing telehealth services.23 The results of this study may benefit a variety of stakeholders. Policymakers may benefit when considering the impact of existing legislation on the financial viability of rural hospitals to continue providing access to ED care within those communities, including long-term telehealth reimbursement, CMS CAH reimbursement, as well as Stark and Anti-kickback laws on hospital mergers and affiliations. Rural hospital decisionmakers may benefit when deciding whether the investment in tele-emergency care is a financially prudent decision to provide ED care. Furthermore, most importantly, rural community members may benefit from hospital leaders and policymakers using this research for informed decision making that may improve access to and the quality of ED care through telehealth.
Materials and Methods
Data Sources
A panel of data was constructed at the hospital level for 2010–2017 using two data sources. The identification of the names and implementation dates of TelEmergency were derived from internal UMMC data. Data for all analyses came from the CMS Hospital Cost Report Information System files' “cost reports.”24 Cost reports are a widely adopted source of hospital financial information because all hospitals are required to file these with CMS annually to receive Medicare reimbursement. While widely accepted, cost reports have been shown to report certain data inconsistently.25 Still, the accessibility of financial data for all hospitals receiving CMS-based reimbursement makes cost reports a commonly accepted source of hospital financial data.
Sample
To define the sample, we combined TelEmergency participation status with hospital cost reports from 2003 to 2017. We determined there were 20 rural hospitals using TelEmergency. We limited our treatment group to the 16 of those that began TelEmergency before or during the sample period. We limited the comparison group to similar southern states: Arkansas (AR), Georgia (GA), MS, and South Carolina (SC). Preliminary analysis led us to discover inconsistencies in the key outcome variable for some of the treatment hospitals before 2010. Therefore, we limited our analysis to the years 2010 through 2017. Next, we limited the sample to hospitals that reported the cost outcome variable in every year and matched treatment hospitals to similar comparison hospitals using a process subsequently described in the “Study Design” section. Our final sample comprised 14 hospitals using TelEmergency (112 hospital-years, with a hospital-year defined as each year for which we had data for a particular hospital) and 102 comparison hospitals (766 hospital-years) that did not offer TelEmergency from AR, GA, MS, and SC.
Study Variables
Dependent variable
The key outcome measure was total annual ED costs, which was analyzed using a log link because of the extreme right-skewed nature of its distribution. This measure came from cost report Worksheet B, Part 1, row 91, Column 26.
Key independent variable
The key explanatory measure was a binary measure for whether a hospital provided TelEmergency.
Additional independent variables
Other factors evaluated in the generalized estimating equations (GEE) were ownership type, whether a hospital was a CAH,i total operating expenses, number of beds, and year. Ownership was categorized as private for-profit, private not-for-profit, and government-owned, which controlled for differing financial objectives.26 CAH-status accounted for Medicare cost-based reimbursement and differences in meaningful use incentive/penalty guidelines.27 Total operating expenses and the number of beds controlled for hospital size. Repeated measures of hospital over years were controlled for in the analysis.
Study Design
The relationship between total annual ED costs and treatment (e.g., participation in TelEmergency) was fitted using GEE with a Poisson distribution and robust standard errors28; including a log link and an exchangeable error term for repeated observations that accounted for time-invariant unobserved hospital-specific characteristics affecting treatment. Hospital-years were included in the analysis if no missing values were present, using complete case analysis. Extreme values were Winsorized at the one percent tails of each variable's distribution.29,30 Descriptive bivariate differences between treatment and comparison hospitals were tested using Pearson's chi-square (categorical variables) and t-tests (continuous variables). The threshold for statistical significance was set a priori at p < 0.10. A one-to-many31 Coarsened Exact Match32,33 was applied to address suspected selection bias around which rural hospitals participated in TelEmergency. Matching was based on CAH-status (exact match), beds, and ownership. While some statistical differences remained between most variables of interest after matching (Table 2), balance improved notably between groups when compared with the nonmatched descriptive results (Appendix Table A1), and the matching methods used in the study design further decreased the likelihood of misspecification.
Table 2.
Descriptive Statistics by TelEmergency Participation
| ALL HOSPITAL YEARS | TELEMERGENCY |
NO TELEMERGENCY |
p | |
|---|---|---|---|---|
| (N = 112) | (N = 766) | |||
| Total ED costs (scaled by $1,000s) | $2,305 | $1,626 | $2,405 | <0.001*** |
| Ownership | <0.001*** | |||
| Not for profit | 30% | 19% | 31% | |
| For profit | 8% | 5% | 8% | |
| Government | 63% | 76% | 61% | |
| CAH status | <0.001*** | |||
| Non-CAH | 24% | 14% | 26% | |
| CAH | 76% | 86% | 74% | |
| Total operating expenses (scaled by $1,000s) | $20,955 | $18,651 | $21,291 | <0.001*** |
| Beds | 28 | 22 | 29 | <0.001*** |
p < 0.001.
p-values by t-test for continuous variables and χ2 test for binary/categorical variables.
Results
Descriptive Statistics
In Table 2, matched descriptive statistics are presented for hospital-years in the sample. The first column depicts averages for all hospitals, the second column displays the treatment group averages, and the third column displays the comparison group averages. The average total annual ED cost for hospitals participating in TelEmergency was $1.6M, which was significantly less than the comparison group average of $2.4M (p < 0.001). Compared with nonparticipating hospitals, hospitals using TelEmergency were more likely to be government owned (76% vs. 61%; p < 0.001), CAHs (86% vs. 74%; p < 0.001), and had lower average beds (22 vs. 29; p < 0.001) and operating expenses ($19M vs. $21M; p < 0.001). TelEmergency ED costs accounted for 9% ($1.626M/$18.651M) of total operating expenses at treatment hospitals.
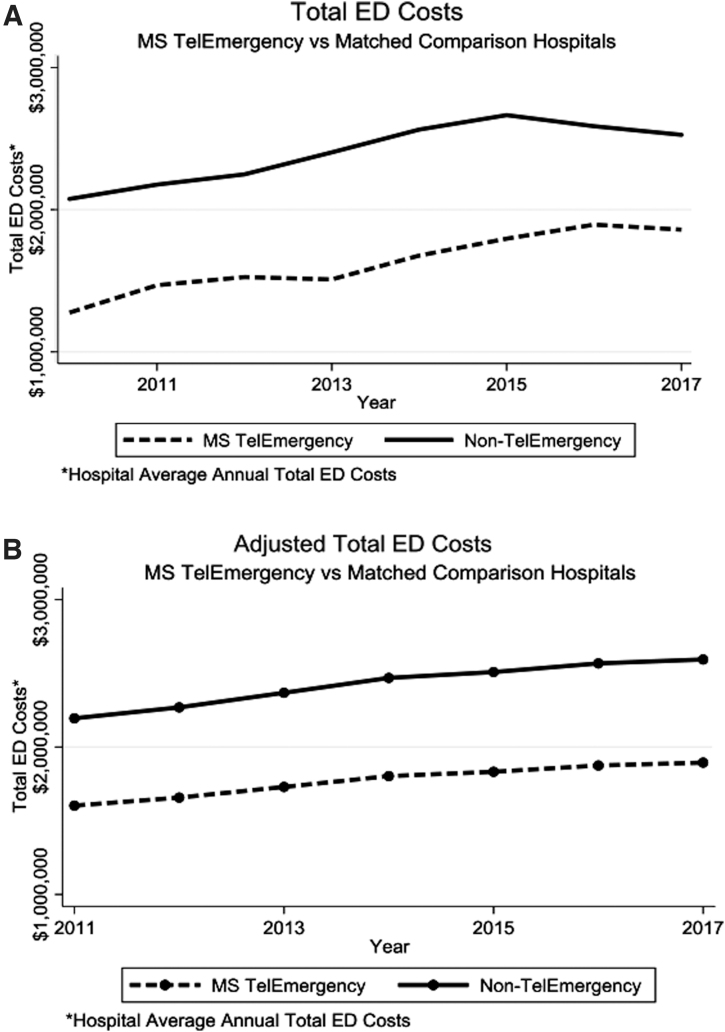
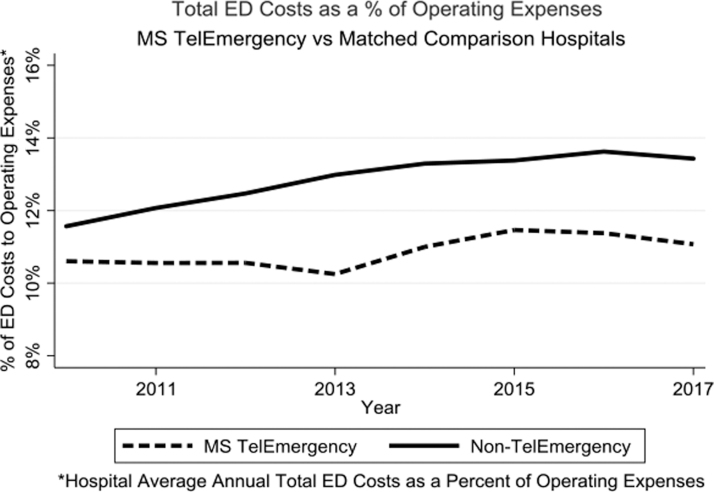
In Figure 2A, unadjusted average annual hospital ED costs by treatment are shown to describe changes over time. Each year, hospitals utilizing TelEmergency spent less in annual averaged ED costs. To account for the potential that hospital size impacted total ED costs, we calculated the average annual total hospital ED costs as a percent of total operating expenses by treatment (Appendix Fig. A1). In every study year, hospitals utilizing TelEmergency spent less on ED costs as a percentage of total operating expenses. In 2010, hospitals with TelEmergency spent more similar proportions of ED to total operating costs. That difference increased in more recent years as hospitals without TelEmergency increased their proportional ED to total operating spending, whereas hospitals using TelEmergency remained relatively stable, around 11%.
Fig. 2.
(A) Total ED costs—MS TelEmergency versus matched comparison hospitals. (B) Adjusted total ED costs—MS TelEmergency versus matched comparison hospitals. ED, emergency department; MS, Mississippi.
Adjusted Regression Results
In Table 3, adjusted results for the impact of TelEmergency on annual total hospital ED costs are presented. After controlling for ownership type, CAH-status, year, and size, and compared with similar matched hospitals in AR, GA, SC, and MS that did not provide TelEmergency, TelEmergency usage was associated with an estimated 31.4% lower total annual ED costs (p = 0.073). Hospital size, measured by operating expenses and beds, and year were associated with higher ED costs. Ownership type and CAH-status were not associated with statistically significant impact on ED costs.
Table 3.
Adjusted Estimates for the Impact of TelEmergency on Annual Total Hospital Emergency Department Costs
| VARIABLE | ESTIMATE [90% CI] | VARIABLE | ESTIMATE [90% CI] |
|---|---|---|---|
| Treatment (TelEmergency participation) | −0.314* | Year (referent: 2010) | [0 to 0] |
| [−0.603 to −0.026] | 2011 | 0.0427*** | |
| Ownership (referent: not for profit) | [0.025 to 0.061] | ||
| For profit | −0.097 | 2012 | 0.076*** |
| [−0.254 to 0.061] | [0.050 to 0.102] | ||
| Government | −0.028 | 2013 | 0.119*** |
| [−0.115 to 0.059] | [0.088 to 0.149] | ||
| CAH status (referent: non-CAH) | 2014 | 0.160*** | |
| CAH | 0.175 | [0.122 to 0.199] | |
| [−0.013 to 0.363] | 2015 | 0.176*** | |
| Total operating expenses (logged) | 0.455*** | [0.139 to 0.214] | |
| [0.373 to 0.537] | 2016 | 0.199*** | |
| Beds | 0.015** | [0.158 to 0.241] | |
| [0.007 to 0.022] | 2017 | 0.210*** | |
| [0.170 to 0.249] | |||
| Constant | 6.400*** | ||
p < 0.10, **p < 0.01, ***p < 0.001.
CI, confidence interval.
90% CIs reported.
In Figure 2B, adjusted average annual ED costs are shown that control for the factors described in Table 3 and present average hospital ED costs by treatment annually. After adjustments, estimates are similar to the unadjusted results of Figure 2A, with hospitals that utilize TelEmergency spending less in the ED.
Rural MS Hospital Closures by Telemergency Use
Because one of the largest goals of improving access to EM care was to avoid rural hospital closure, closures were evaluated at the state level using data from the University of North Carolina Sheps Center.11 Six rural MS hospitals were identified that closed between 2005 and 2020. During that time, there were ∼70 rural MS hospitals,34 with 20 of those hospitals using TelEmergency. Over the period of the program, none of the rural hospitals using TelEmergency closed, whereas 6 out of the ∼50 rural hospitals (12%) closed.
Discussion
The objective of this study was to empirically determine whether TelEmergency usage was associated with lower ED costs at rural hospitals when compared with similar hospitals without TelEmergency. We hypothesized that TelEmergency utilization lowered overall ED costs. Our main finding confirmed this hypothesis and quantified that, after adjusting for other factors and when compared with similar, matched hospitals, the use of TelEmergency was associated with an estimated ∼30% lower total annual ED costs. We expect that lower costs associated with TelEmergency are due directly to specific initiatives previously described (e.g., scaling services like physician labor and enhanced inventory management across sites)35 and indirectly associated with structural changes in the local community health system related to the provision of telehealth services.23
Additionally, we found that lower ED costs associated with TelEmergency use were not simply due to the relatively smaller size of the hospitals using TelEmergency. We accounted for size differences in multiple ways. We matched hospitals based on number of beds and CAH-status. Then, in regression-adjusted results, we controlled for size with two measures—bed size and operating expenses. We expected operating expenses to correlate with size relatively well in these hospitals, particularly because 17 hospitals using TelEmergency were CAHs. Under the CAH-designation, CMS reimbursement is directly associated with reasonable expenses under a cost-based model,27,36 rather than the more common prospective payment reimbursement system.
Importantly, our results suggest that TelEmergency utilization potentially prevented some financially distressed rural hospitals from closing, a key objective in the development of the TelEmergency program. The core strategic goal for UMMC's deployment of TelEmergency was to maintain or improve access to and the quality of ED care in rural MS communities, while also stabilizing the financial health of rural hospitals. While a growing body of evidence suggests myriad health outcomes can benefit from ED telehealth,13–15 ours is the first known study to quantify two key aspects related to rural hospital financial health and access—the magnitude of lower costs and the potential avoidance of rural hospital closures.
Implications
Taken together, our findings advance the literature related to the costs associated with the provision of ED telehealth in several meaningful ways, and several stakeholders may benefit from this research.
Policymakers at all levels of government may benefit from this research when considering various provisions directly or indirectly impacting the delivery of ED care remotely. Two key state-specific legislative changes contributed to the financial savings related to TelEmergency. First, negotiating waivers to expand NP scope of practice beyond 15 miles for TelEmergency delivery created cost savings. Second, MS state telemedicine parity law vastly increased reimbursable telehealth services, and did so across all payers.18 The COVID-19-induced March 2020 temporary expansion of both scope of practice for NPs and reimbursable telehealth services at the federal level may have created an environment, where hospitals in states other than MS could benefit from some existing TelEmergency practices. When policymakers determine whether provisions such as these should continue, our research may highlight one nuanced impact, particularly for financially fragile rural hospitals. These findings may benefit policymakers and grantees of the Federal Office of Rural Health Policy's Evidence-Based Tele-Emergency Network Grant Program.
Our findings may also inform hospital executives and board members, particularly at financially constrained rural hospitals, who may benefit from this research when deciding whether ED telehealth fits within their overall organizational mission. Additionally, our results could be used to augment budgeting projections related to ED telehealth. Concerns for changes to or the elimination of the CAH designation37 were one motive UMMC leaders reported for deploying TelEmergency. Since CAH reimbursement is directly tied to costs, lowering costs through the use of TelEmergency may reduce some reliance of participating CAHs on this reimbursement methodology and prepare them for shifts toward value-based care models.
Finally, administrators at larger hospitals who are considering the creation of an ED telehealth network, for which their hospital would be a hub, may benefit from our findings when deciding how to improve care coordination for outlying communities in their market without acquiring those hospitals. Large tertiary/quaternary health systems are increasingly merging with rural hospitals38 within their outlying market. Those mergers, at least in part, are motivated by a need to manage the more complex care of patients in those outlying markets.39 Doing so becomes increasingly important as a greater proportion of care is reimbursed under value-based models, shifting population health management risk to the hospital. However, merging requires significant upfront and ongoing capital spending at the larger hospital,40 and ties it to the overall financial health of the smaller, merged hospitals. Our findings suggest it is possible that an ED-based telehealth similar to TelEmergency could achieve similar objectives of improving access to quality care and coordinating complex care while stabilize outlying rural hospitals and keeping them open, without the costs and assumed risks of a merger.
Limitations
While we believe our findings offer compelling evidence that hospitals using TelEmergency had lower ED costs, we acknowledge some important limitations. First, our outcome measure was total annual ED costs, not a bottom-line profitability measure. We considered many alternatives and believed ED costs was most directly tied to the intervention. Second, while we knew the comparison hospitals were not part of TelEmergency, we could not determine whether any of those hospitals provided any other form of ED telehealth. This concern was at least partially mitigated because TelEmergency is one of the nation's most robust ED telehealth networks and there was no other known ED telehealth network nearly as robust by comparison in the other comparator states. If comparison hospitals had a form of ED telehealth, it would likely skew the results in favor of no difference between the groups. Third, the generalizability of our study is limited to the evaluation of only one ED telehealth program, TelEmergency, and compared with hospitals in four southern states (AR, GA, MS, and SC). We are cautious to not generalize our results beyond those groups and states.
Conclusion
TelEmergency utilization was associated with significantly lower total annual ED costs compared with similarly matched hospitals that did not utilize TelEmergency. These findings suggest that access to quality ED care in rural communities can occur at lower costs.
Appendix
Appendix Fig. A1. Total ED costs as a percent of total operating expenses—MS TelEmergency versus matched comparison hospitals. ED, emergency department; MS, Mississippi.
Appendix Table A1. Non-matched Descriptive Statistics by TelEmergency Participation
| ALL HOSPITAL YEARS | TELEMERGENCY |
NO TELEMERGENCY |
p | |
|---|---|---|---|---|
| (N = 112) | (N = 2,376) | |||
| Total ED costs (scaled by $1,000s) | $6,3121 | $1,626 | $6,533 | <0.001*** |
| Ownership | <0.001*** | |||
| Not for profit | 43% | 19% | 44% | |
| For profit | 21% | 5% | 22% | |
| Government | 36% | 76% | 35% | |
| CAH status | <0.001*** | |||
| Non-CAH | 73% | 14% | 76% | |
| CAH | 27% | 86% | 24% | |
| Total operating expenses (scaled by $1,000s) | $1.3e+05 | $18,651 | $1.4e+05 | <0.001*** |
| Beds | 140 | 22 | 145 | <0.001*** |
p < 0.001.
CAH, critical access hospital; ED, emergency department.
p-values by t-test for continuous variables and χ2 test for binary/categorical variables.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure Statement
No competing financial interests exist.
Funding Information
This publication was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of the National Telehealth Center of Excellence Awards (U66 RH31458—MUSC; U66RH31459—UMMC). This publication was also partially supported by the South Carolina Clinical & Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, through NIH - NCATS Grant Number UL1 TR001450. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. Dr. Sterling is partially supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award No. 1U54GM115428.
Hospitals must meet certain criteria to be eligible for the Critical Access designation. Most hospitals must be located in a rural area, be more than a 35-mile drive to the next hospital, and maintain no more than 25 inpatient beds (with certain allowable exceptions).36
References
- 1. De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: Every minute of delay counts. Circulation 2004;109:1223–1225. [DOI] [PubMed] [Google Scholar]
- 2. Newgard CD, Meier EN, Bulger EM, et al. Revisiting the “golden hour”: An evaluation of out-of-hospital time in shock and traumatic brain injury. Ann Emerg Med 2015;6630–41, 41.e31–e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better outcome: The NINDS rt-PA stroke study. Neurology 2000;55:1649–1655. [DOI] [PubMed] [Google Scholar]
- 4. Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res 2005;40:135–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ambroggi M, Biasini C, Del Giovane C, Fornari F, Cavanna L. Distance as a barrier to cancer diagnosis and treatment: Review of the literature. Oncologist 2015;20:1378–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Syed ST, Gerber BS, Sharp LK. Traveling towards disease: Transportation barriers to health care access. J Community Health 2013;38:976–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969–2009. Am J Prev Med 2014;46:e19–e29. [DOI] [PubMed] [Google Scholar]
- 8. What is Rural America? Available at https://www.census.gov/library/stories/2017/08/rural-america.html (last accessed April 11, 2020).
- 9. Gamm L, Van Nostrand JF. Rural healthy people 2010: A companion document to healthy people 2010. College Station, TX: Texas A & M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003. [Google Scholar]
- 10. Hilsenrath P FK. Economic transformation in health care: Implications for rural communities. J Rural Health 2013;29:337–338. [DOI] [PubMed] [Google Scholar]
- 11. North Carolina Rural Health Research Program Tracking of Rural Hospital Closures. 2018. Available at www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/ (last accessed February 13, 2018).
- 12. iVantage_Health_Analytics. Rural Relevance - Vulnerability to Value 2016. A Hospital Strength INDEX® Study. Available at https://www.chartis.com/resources/files/INDEX_2016_Rural_Relevance_Study_FINAL_Formatted_02_08_16.pdf (last accessed April 11, 2020).
- 13. Natafgi N, Mohr NM, Wittrock A, Bell A, Ward MM. The association between telemedicine and emergency department (ED) disposition: A stepped wedge design of an ED-based telemedicine program in critical access hospitals. J Rural Health 2020;36:360–370. [DOI] [PubMed] [Google Scholar]
- 14. Swanson MB, Miller AC, Ward MM, Ullrich F, Merchant KA, Mohr NM. Emergency department telemedicine consults decrease time to interpret computed tomography of the head in a multi-network cohort. J Telemed Telecare 2019;1357633X19877746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mohr NM, Campbell KD, Swanson MB, Ullrich F, Merchant KA, Ward MM. Provider-to-provider telemedicine improves adherence to sepsis bundle care in community emergency departments. J Telemed Telecare 2020;1357633X19896667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Natafgi N, Shane DM, Ullrich F, MacKinney AC, Bell A, Ward MM. Using tele-emergency to avoid patient transfers in rural emergency departments: An assessment of costs and benefits. J Telemed Telecare 2018;24:193–201. [DOI] [PubMed] [Google Scholar]
- 17. MacKinney AC, Ward MM, Ullrich F, Ayyagari P, Bell AL, Mueller KJ. The business case for tele-emergency. Telemed J E Health 2015;21:1005–1011. [DOI] [PubMed] [Google Scholar]
- 18. Galli R, Keith JC, McKenzie K, Hall GS, Henderson K. TelEmergency: A novel system for delivering emergency care to rural hospitals. Ann Emerg Med 2008;51:275–284. [DOI] [PubMed] [Google Scholar]
- 19. Sterling SA, Seals SR, Jones AE, et al. The impact of the TelEmergency program on rural emergency care: An implementation study. J Telemed Telecare 2017;23:588–594. [DOI] [PubMed] [Google Scholar]
- 20. Galli R. Innovation possibilities for prehospital providers. Prehosp Emerg Care 2006;10:317–319. [DOI] [PubMed] [Google Scholar]
- 21. Mueller KJ, Potter AJ, MacKinney AC, Ward MM. Lessons from tele-emergency: Improving care quality and health outcomes by expanding support for rural care systems. Health Aff (Millwood) 2014;33:228–234. [DOI] [PubMed] [Google Scholar]
- 22. Mississippi Code Title 83. Insurance § 83-9-351. Accident, health and medicare supplement insurance coverage for telemedicine services. Available at https://law.justia.com/codes/mississippi/2014/title-83/chapter-9/coverage-for-telemedicine-services/section-83-9-351/#:~:text=FOR%20TELEMEDICINE%20SERVICES-,%C2%A7%2083%2D9%2D351%20%2D%20Health%20insurance%20plans%20in%20Mississippi,coverage%20for%20telemedicine%20services%3B%20definitions&text=(d)%20%22Telemedicine%22%20means,video%2C%20or%20other%20electronic%20media (last accessed April 11, 2020).
- 23. Simpson A, Harvey J, DiLembo S, et al. Population Health Indicators Associated with a Statewide Telestroke Program. Telemed J E Health 2020;26:1126–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. CMS. Hospital Cost Report Information System (HCRIS) Medicare Cost Reports (Cost Reports). 2020. Available at https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Cost-Reports (last accessed April 11, 2020).
- 25. Ozmeral AB, Reiter KL, Holmes GM, Pink GH. A comparative study of financial data sources for critical access hospitals: Audited financial statements, the Medicare cost report, and the internal revenue service form 990. J Rural Health 2012;28:416–424. [DOI] [PubMed] [Google Scholar]
- 26. Horwitz JR, Nichols A. Rural hospital ownership: Medical service provision, market mix, and spillover effects. Health Serv Res 2011;46:1452–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Eligible Hospital And Critical Access Hospital Meaningful Use Core Measures. 2013. Available at https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/9_Clinical_Quality_Measures.pdf (last accessed December 18, 2019).
- 28. Ballinger GA. Using generalized estimating equations for longitudinal data analysis. Organizational Res Methods 2004;7:127–150. [Google Scholar]
- 29. Rivest LP. Statistical properties of Winsorized means for skewed distributions. Biometrika 1994;81:373–383. [Google Scholar]
- 30. Williams Jr. D, Holmes GM, Song PH, Reiter KL, Pink GH.. For rural hospitals that merged, inpatient charges decreased and outpatient charges increased: A pre-/post-comparison of rural hospitals that merged and rural hospitals that did not merge between 2005 and 2015. J Rural Health 2020. [Epub ahead of print]; DOI: 10.1111/jrh.12461. [DOI] [PubMed] [Google Scholar]
- 31. Schuur JD, Baker O, Freshman J, Wilson M, Cutler DM. Where do freestanding emergency departments choose to locate? A national inventory and geographic analysis in three states. Ann Emerg Med 2017;69:383–392.5. [DOI] [PubMed] [Google Scholar]
- 32. Blackwell M, Iacus S, King G, Porro G. CEM: Coarsened exact matching in Stata. Stata J 2009;9:524–546. [Google Scholar]
- 33. Stuart EA. Matching methods for causal inference: A review and a look forward. Stat Sci 2010;25:1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Author's analysis of Medicare Cost Report data for relevant years. [Google Scholar]
- 35. Greg Hall M. Interview with Greg Hall, MD, University of Mississippi Medical Center. In: Dunc Williams J, ed. 2020. [Google Scholar]
- 36. CMS. Critical access hospital fact sheet. 2016. Available at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/CritAccessHospfctsht.pdf (last accessed April 11, 2020).
- 37. Holmes GM, Pink GH, Friedman SA. The financial performance of rural hospitals and implications for elimination of the critical access hospital program. J Rural Health 2013;29:140–149. [DOI] [PubMed] [Google Scholar]
- 38. Williams D, Thomas SR, Howard HA, Pink G. Rural hospital mergers from 2005 through 2016. Findings brief for the federal office of rural health policy. NC Rural Health Research Program. 2018. Available at https://www.shepscenter.unc.edu/wp-content/uploads/dlm_uploads/2018/08/Rural-Hospital-Mergers.pdf (last accessed April 11, 2020).
- 39. Nakamura S, Capps C, Dranove D. Patient admission patterns and acquisitions of “feeder” hospitals. J Econ Manage Strategy 2007;16:995–1030. [Google Scholar]
- 40. Williams Jr D, Pink G, Song PH, Reiter KL, Holmes GM. Capital expenditures increased at rural hospitals that merged between 2012 and 2015. J Healthcare Manage 2020;65:346–364. [DOI] [PubMed] [Google Scholar]