Abstract
Introduction
Inconsistent reporting practices in third trimester ultrasound, the choice of reference charts in particular, have the potential to misdiagnose abnormal fetal growth. But this may lead to unnecessary anxiety and confusion amongst patients and clinicians and ultimately influence clinical management. Therefore, we sought to determine the extent of variability in choice of fetal biometry and Doppler reference charts and reporting practices in Australia and New Zealand.
Methods
Clinicians performing and/or reporting obstetric ultrasound were invited to answer questions about fetal biometry and Doppler charts in a web‐based survey.
Results
At least four population‐based charts are in current use. The majority of respondents (78%) report the percentile for known gestational age (GA) alongside measurements and 63% using a cut‐off of estimated fetal weight (EFW) < 10th percentile when reporting small for gestational age (SGA) and/or fetal growth restriction (FGR). The thresholds for the use of fetal and maternal Doppler in third trimester ultrasound varied in terms of the GA, EFW cut‐off, and how measures were reported. The majority of respondents were not sure of which Doppler charts were used in their practice.
Conclusion
This survey revealed inconsistencies in choice of reference chart and reporting practices. The potential for misdiagnosis of abnormal fetal growth remains a significant issue.
Keywords: obstetric ultrasound, fetal measurement, reference charts, biometry, Doppler
Introduction
Abnormal fetal growth and fetal growth restriction (FGR), in particular, are associated with increased risk of adverse perinatal outcomes. 1 , 2 Prenatal identification allows for increased fetal monitoring to inform clinical decisions regarding delivery and has been shown to improve perinatal outcomes. 3
The role of ultrasound in the measurement of fetal biometry and estimation of fetal weight is well established, with the identification of abnormal growth based on comparison with expected measurements for a given gestational age derived from a reference chart. However, a large number of reference charts exist and population bias or heterogeneity in chart methodologies means percentiles for a given measurement may vary considerably. Indeed, comparison of three fetal measurement reference charts has demonstrated a six‐fold increase in measurements classified as being below the 5th percentile. 4 The calculated estimated fetal weight (EFW) can vary according to the choice of formula, with some models better suited to estimating weight in the small fetus and other models performing better in the large fetus. 5 , 6 The calculated EFW may be compared to one of several birthweight charts or ultrasound‐based EFW charts, with the potential for considerable differences in assigned percentile. 7 This situation leads to unnecessary anxiety and confusion amongst patients and clinicians, particularly if the same fetus is examined at different centres using different reference charts.
Fetal Doppler assessment, namely umbilical artery (UA), middle cerebral artery (MCA) and their ratio, the cerebroplacental ratio (CPR), are increasingly being used in the surveillance of suspected FGR fetuses. Abnormal Doppler indices are associated with adverse pregnancy outcomes, 8 and there is growing evidence this may also apply to fetuses of normal size. 9 , 10 Similar to fetal biometry reference charts, there is significant heterogeneity between different Doppler reference charts, 11 with the potential to influence management, namely induction of labour, in 30% of cases. 12
The choice of reference chart has been a contentious issue in Australian and New Zealand ultrasound practices for the past two decades. Despite the 2001 recommendation from Australasian Society for Ultrasound in Medicine (ASUM) for use of the Westerway charts formulated from an Australian population, 13 there were at least eight fetal growth charts in clinical use in Australia and New Zealand in 2013. 14 Variation in the choice of umbilical artery Doppler index and reference chart has also been reported 15 ; however, reporting practices involving other Doppler parameters are unknown. The aim of this study is to establish which fetal biometry and Doppler reference charts are currently used in Australian and New Zealand practice and how these parameters are reported.
Materials and Methods
Clinicians performing and/or reporting obstetric ultrasound were invited to answer questions about fetal biometry and Doppler charts in a web‐based survey (Qualtrics, Provo, UT). The survey text is provided as supporting information ([Link], [Link]).
Questions were based on a pilot survey conducted in 2017 within four ultrasound practices and semi‐structured interviews with four clinicians. Further question refinement followed expert panel review. The survey instrument was designed to be used on either a desktop or mobile device, utilising drop‐down menus for responses where possible and conditional questioning via skip and/or display logic. Two rating scale questions investigated factors influencing the choice of reference chart, and one open text question invited comment about how third trimester ultrasound is performed and reported. The survey was approved by the Australian National University Human Research Ethics Committee 2017/418 and Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) continuing professional development committee.
The intended survey recipients included obstetricians performing obstetric ultrasound as part of their clinical practice, obstetricians with ultrasound subspecialty qualifications, radiologists, and other medical specialists with ultrasound qualifications. To reach these groups, applications were made to the representative professional bodies RANZCOG, Royal Australian and New Zealand College of Radiologists (RANZCR) and ASUM for the survey link to be distributed to their members.
Letters inviting participation and links to the electronic survey were distributed to members of RANZCOG via email on 16/9/2019 with one reminder email two weeks later. Links were distributed to members of the RANZCR Obstetrics and Gynaecology Special Interest Group 15/8/2019 via social media and again on 24/2/2020 via email. Survey links were advertised in the ASUM member electronic newsletter on 7/11/2019 and the ASUM Diploma of Diagnostic Ultrasound (DDU) newsletter on 20/2/2020.
Analysis was performed for responses recorded up to and including the 'Third trimester Doppler' section of the electronic survey.
Data were analysed using Microsoft Excel (2016) and IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, NY, USA).
Results
A total of 230 responses were received: 204 following RANZCOG distribution of the survey link, 13 following RANZCR distribution of the survey link and 13 following ASUM distribution of the survey link. The estimated response rate from RANZCOG members was 15%, based on membership numbers reported in the 2018–2019 RANZCOG Annual Report 16 and the estimated number of clinicians fulfilling the pre‐condition of performing/reporting obstetric ultrasound. 14 The response rate from obstetric subspecialists was 29%.
The survey link was distributed to the 73 members of the RANZCR Obstetrics and Gynaecology Special Interest Group (Fitzpatrick, personal communication) with an 18% response rate.
There are approximately 650 medical members of ASUM 17 ; however, information on the specialty area(s) practised by ASUM medical members is not collected. The target medical members for this survey were also likely to be RANZCOG or RANZCR members, further confounding estimation of a response rate from this cohort.
Of the 230 returned surveys, 86 were excluded from analysis as shown in Figure 1. Of the remaining 144 responses, 125 were complete for both biometry and Doppler sections.
Figure 1.
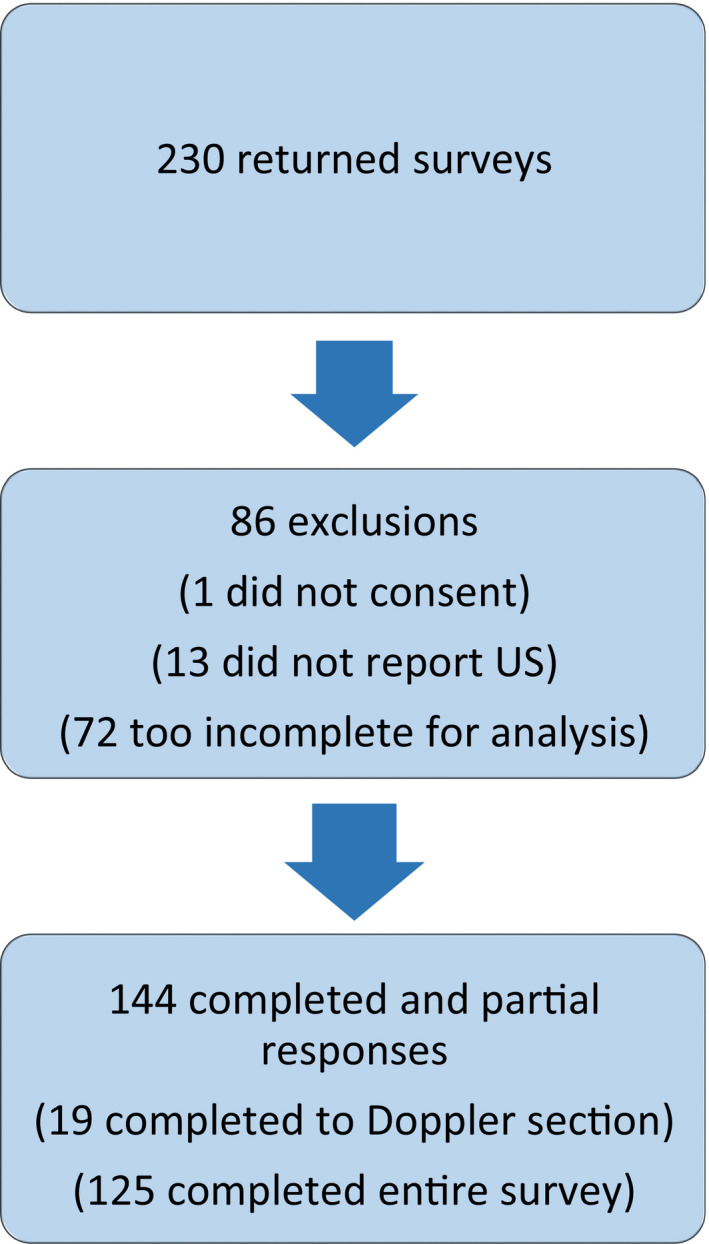
Summary of returned surveys used in analysis.
Most respondents (80%) practised in Australia. All states and territories were represented with 70% of responses from major cities as defined by the Australian Bureau of statistics Australian Statistical Geography Standard. 18 Responses from New Zealand were from major urban centres as defined by Statistics New Zealand Urban Rural Indicator 2018 V1.0.0 19 from seven of the twenty district health boards. 20
The majority (127 or 88%) of respondents were 62 (52%) were generalists with no additional qualification in ultrasound, and obstetricians or obstetric registrars; 32 (27%) were subspecialists with certification in obstetric and gynaecological ultrasound (COGU) or maternal fetal medicine (CMFM). Many subspecialists had completed the ASUM Diploma in Diagnostic Ultrasound (DDU); however, 27 (19%) of respondents with a DDU were not subspecialists. No radiologists had additional ultrasound qualifications, and only a small number (4) of respondents were other medical specialists with a DDU. The majority (72%) had greater than five years’ experience in performing/reporting obstetric ultrasound with 47% indicating more than ten years’ experience. Public and private practice was fairly evenly represented with 40% working in obstetric public practice, 38% in obstetric private practice, 9% in radiology public practice and 6% in radiology private practice.
Charts for fetal biometry
Table 1 lists charts in current use in Australia and New Zealand for the standard fetal biometry measures of bi‐parietal diameter (BPD), head circumference (HC), abdominal circumference (AC) and femur length (FL) (note 2/144 respondents did not provide geographic information). The Westerway 13 charts (commonly referred to as ASUM charts) and Hadlock 21 , 22 , 23 , 24 charts were used by 35% and 26% of respondents, respectively. None reported using Intergrowth 21st (IG21), 25 Schluter, 26 , 27 Snijders 28 or Jeanty 29 , 30 charts. Fourteen respondents were unsure of which charts were used, and fifteen indicated a combination of charts were used for standard fetal biometry measures. In‐house charts based on the Western Australian Raine Cohort (Newnham, personal communication) were used by a minority of respondents, but none outside of Western Australia.
Table 1.
Reporting practices for fetal biometry.
|
Obstetric practice AU a N |
Obstetric practice NZ b N |
Radiology practice AU N |
Radiology practice NZ N |
Total N (%) |
|
|---|---|---|---|---|---|
| Chart used 142/142 | |||||
| ASUM 13 (BPD c ,HC d ,AC e ,FL f ) | 28 | 11 | 6 | 7 | 50 (35) |
| Chitty 31 , 32 , 33 (BPD,HC,AC,FL) | 16 | 0 | 0 | 0 | 16 (11) |
| Hadlock 21 , 22 , 23 , 24 (BPD,HC,AC,FL) | 30 | 6 | 1 | 0 | 37 (26) |
| GROW 34 (BPD,HC,AC,FL) | 1 | 2 | 0 | 0 | 3 (2) |
| Unsure (BPD,HC,AC,FL) | 13 | 0 | 1 | 0 | 14 (10) |
| Raine unpublished data (BPD,HC,AC,FL) | 6 | 0 | 1 | 0 | 7 (5) |
| Combination of charts | 13 | 0 | 2 | 0 | 15 (11) |
| Reported alongside 142/142 | |||||
| Percentile for known GA g | 69 | 12 | 4 | 7 | 92 (65) |
| Equivalent weeks and days | 13 | 1 | 1 | 0 | 15 (11) |
| Reference range | 1 | 1 | 0 | 0 | 2 (1) |
| Equivalent weeks and days & percentile | 13 | 0 | 3 | 0 | 16 (11) |
| Plotted on chart | 4 | 2 | 1 | 0 | 7 (5) |
| Nothing | 3 | 1 | 0 | 0 | 4 (3) |
| Other | 3 | 2 | 0 | 1 | 6 (4) |
Australia.
New Zealand.
Bi‐parietal diameter.
Head circumference.
Abdominal circumference.
Femur length.
Gestational age.
Reporting fetal measurements
A clear trend emerged in the way measurements were reported with a majority (78%) reporting the percentile for known gestational age (GA) alongside measurements. Some respondents (13%) co‐reported percentiles with equivalent weeks and days, with 11% only reporting equivalent weeks and days for each parameter. A minority (5%) indicated measurements were plotted directly onto charts. No respondents reported the z‐score alongside measurements. Most (63%) did not cite the reference chart in the report.
The report page generated by the ultrasound machine was typically used by clinicians reporting fetal measurements (74% of respondents). Most (75%) indicated all machines in their department were configured with the same fetal measurement charts; however, 21% were unsure, and 4% indicated machines in their department were not configured with the same fetal measurement charts.
Digital reporting packages were used by 16% of respondents.
Estimated Fetal Weight
Table 2 lists reporting practices for EFW (note 2/144 respondents did not provide geographic information). Hadlock 35 , 36 (BPD, HC, AC, FL) was the most commonly used algorithm for calculating EFW used by 69% of respondents, typically reported alongside the percentile for the known GA according to fetal weight charts, 37 rather than birthweight (BW) charts. 38 , 39 , 40 A minority (6%) used in‐house BW charts, 41 and 14% used customised EFW charts. 34 , 42
Table 2.
Reporting practices for Estimated Fetal Weight (EFW).
|
Obstetric practice AU a N |
Obstetric practice NZ b N |
Radiology practice AU N |
Radiology practice NZ N |
Total N (%) |
|
|---|---|---|---|---|---|
| EFW c algorithm 142/142 | |||||
| Hadlock 35 , 36 (BPD d ‐HC e ‐AC f ‐FL g ) | 69 | 16 | 7 | 7 | 99 (70) |
| Hadlock 35 , 36 (HC‐AC‐FL) | 18 | 1 | 1 | 0 | 20 (14) |
| Hadlock 35 , 36 (BPD‐AC‐FL) | 7 | 0 | 0 | 0 | 7 (5) |
| Unsure | 13 | 1 | 1 | 0 | 15 (11) |
| Other | 0 | 1 | 0 | 0 | 1 (1) |
| Reported alongside 141/142 | |||||
| Percentile for known GA h | 74 | 10 | 4 | 1 | 89 (63) |
| Error as % | 9 | 1 | 0 | 1 | 11 (8) |
| Error in grams | 6 | 1 | 1 | 0 | 8 (6) |
| Nothing | 6 | 2 | 1 | 0 | 9 (6) |
| Percentile & error (%) | 3 | 0 | 1 | 4 | 8 (6) |
| Percentile & error (g) | 5 | 0 | 2 | 0 | 7 (5) |
| Plotted onto customised chart | 0 | 3 | 0 | 0 | 3 (2) |
| Other | 3 | 2 | 0 | 1 | 6 (4) |
| Chart used 139/142 | |||||
| Roberts 38 (birthweight) | 5 | 0 | 0 | 0 | 5 (4) |
| Hadlock 37 (fetal weight) | 55 | 3 | 7 | 4 | 69 (50) |
| WHO 39 (fetal weight) | 2 | 0 | 0 | 0 | 2 (1) |
| Dobbins 40 (birthweight) | 6 | 0 | 0 | 0 | 6 (4) |
| NZ customised 34 (GROW, fetal weight) | 0 | 13 | 0 | 3 | 16 (12) |
| NZ WHO 42 (birthweight) | 0 | 1 | 0 | 0 | 1 (1) |
| Unsure | 23 | 2 | 2 | 1 | 28 (20) |
| GROW 34 (Australian, fetal weight) | 2 | 0 | 0 | 0 | 2 (2) |
| Mercy 41 (in‐house, population‐customised) | 6 | 0 | 0 | 0 | 6 (4) |
| Raine (unpublished, in‐house) | 2 | 0 | 0 | 0 | 2 (2) |
| Other | 2 | 0 | 0 | 0 | 2 (2) |
Australia.
New Zealand.
Estimated fetal weight.
Bi‐parietal diameter.
Head circumference.
Abdominal circumference.
Femur length.
Gestational age.
Reporting Small for Gestational Age (SGA) and/or Fetal Growth Restriction (FGR)
Thresholds for reporting SGA and/or FGR were variable. The majority of respondents (63%) used a cut‐off of EFW < 10th percentile for GA; however, most also considered the AC percentile (<10th percentile by 36% and <5th percentile by 11%). A small number of respondents (3%) indicated they did not comment on SGA or FGR, and 12% indicated other factors were taken into account, for example, interval growth and asymmetric growth.
Third trimester Doppler
Tables 3 and 4 summarise third trimester UA and MCA Doppler practices from the 125 respondents that completed the entire survey. UA Doppler was performed in all third trimester ultrasound examinations by 61% of respondents and when EFW <5th or 10th percentile by 31%. Most (75%) reported the pulsatility index (PI) either as the only index (59%) or alongside other indices (16%).
Table 3.
Reporting practices for Umbilical Artery Doppler.
|
Obstetric practice AU a N |
Obstetric practice NZ b N |
Radiology practice AU N |
Radiology practice NZ N |
Total N (%) |
|
|---|---|---|---|---|---|
| UA c Doppler performed: 123/123 | |||||
| In all third trimester scans | 65 | 3 | 7 | 0 | 75 (61) |
| At specific GA d | 2 | 0 | 0 | 0 | 2 (2) |
| Never performed | 4 | 0 | 1 | 0 | 5 (4) |
| When EFW e <10th percentile | 12 | 13 | 0 | 7 | 32 (26) |
| When EFW<5th percentile | 3 | 1 | 0 | 0 | 4 (3) |
| Other | 5 | 0 | 0 | 0 | 5 (4) |
| Doppler index/indices reported: 118/118 (5 never performed UA Doppler) | |||||
| SD f | 18 | 1 | 1 | 0 | 20 (17) |
| PI g | 45 | 15 | 2 | 7 | 69 (58) |
| SD&PI | 8 | 1 | 3 | 0 | 12 (10) |
| SD,PI & RI h | 8 | 0 | 0 | 0 | 8 (7) |
| PI & RI | 3 | 0 | 0 | 0 | 3 (3) |
| RI | 2 | 0 | 0 | 0 | 2 (2) |
| SD & RI | 3 | 0 | 1 | 0 | 4 (3) |
| UA Doppler chart used: 118/118 | |||||
| Unsure | 54 | 9 | 4 | 2 | 69 (58) |
| Acharya 43 | 12 | 2 | 2 | 0 | 14 (12) |
| Ebbing 44 | 5 | 5 | 0 | 5 | 15 (13) |
| Trudinger 45 , 46 | 5 | 0 | 0 | 0 | 5 (4) |
| Baschat 47 | 3 | 1 | 0 | 0 | 4 (3) |
| Schaffer (unpublished) | 3 | 0 | 0 | 0 | 3 (3) |
| Medina Castro 48 | 1 | 0 | 0 | 0 | 1 (1) |
| Parra Cordero 49 | 1 | 0 | 0 | 0 | 1 (1) |
| Arduini 50 | 1 | 0 | 1 | 0 | 2 (2) |
| Other | 2 | 0 | 0 | 0 | 2 (2) |
Australia.
New Zealand.
Umbilical artery.
Gestational age.
Estimated fetal weight.
Systolic diastolic ratio.
Pulsatility index.
Resistive index.
Table 4.
Reporting practices for Middle Cerebral Artery Doppler.
|
Obstetric practice AU a N |
Obstetric practice NZ b N |
Radiology practice AU N |
Radiology practice NZ N |
Total N (%) |
|
|---|---|---|---|---|---|
| MCA c Doppler performed: 123/123 | |||||
| In all third trimester scans | 28 | 0 | 1 | 0 | 29 (24) |
| All scans above 34w GA d | 1 | 0 | 0 | 0 | 1 (1) |
| All scans above 28w GA | 1 | 0 | 0 | 0 | 1 (1) |
| Never performed | 15 | 0 | 2 | 0 | 17 (14) |
| When EFW e <10th percentile | 8 | 4 | 0 | 2 | 14 (11) |
| When UA f Doppler abnormal | 11 | 2 | 1 | 2 | 16 (13) |
| Both EFW<10th percentile & abnormal UA Doppler | 14 | 8 | 1 | 2 | 25 (20) |
| Suspected fetal anaemia | 9 | 2 | 3 | 1 | 15 (12) |
| Other | 2 | 0 | 0 | 0 | 2 (2) |
| Doppler index/indices reported: 106/106 (17 never performed MCA Doppler) | |||||
| SD g | 3 | 0 | 0 | 0 | 3 (3) |
| PI h | 37 | 10 | 0 | 5 | 52 (49) |
| RI i | 3 | 0 | 0 | 0 | 3 (3) |
| PSV j | 2 | 1 | 0 | 0 | 3 (3) |
| PI&PSV | 23 | 6 | 5 | 2 | 36 (34) |
| Other co‐reporting combinations | 8 | 0 | 1 | 0 | 9 (8) |
| MCA Doppler chart used: 105/106 | |||||
| Unsure | 47 | 9 | 3 | 2 | 61 (58) |
| Ebbing 44 | 13 | 6 | 3 | 5 | 27 (25) |
| Schaffer (unpublished) | 5 | 1 | 0 | 0 | 6 (6) |
| Baschat 47 | 7 | 1 | 0 | 0 | 8 (8) |
| Medina Castro 48 | 1 | 0 | 0 | 0 | 1 (1) |
| Ayoola 51 | 1 | 0 | 0 | 0 | 1 (1) |
| Arduini 50 | 1 | 0 | 0 | 0 | 1 (1) |
| CPR l reported: 106/106 | |||||
| Always when MCA performed | 34 | 16 | 1 | 7 | 58 (55) |
| Never reported | 42 | 1 | 5 | 0 | 48 (45) |
| Cut‐off used for abnormal CPR: 58/58 (42 never reported CPR) | |||||
| <10th percentile for GA | 1 | 0 | 0 | 0 | 1 |
| <5th percentile for GA | 23 | 15 | 1 | 7 | 46 |
| Ratio < 1 | 6 | 0 | 0 | 0 | 6 |
| Other | 4 | 1 | 0 | 0 | 5 |
| CPR chart used: 58/58 | |||||
| Unsure | 8 | 8 | 1 | 2 | 19 (33) |
| Ebbing 44 | 12 | 7 | 0 | 5 | 24 (41) |
| Baschat 47 | 4 | 1 | 0 | 0 | 5 (9) |
| No chart (ratio) | 6 | 0 | 0 | 0 | 5 (9) |
| Morales Rosello 52 | 3 | 0 | 0 | 0 | 3 (5) |
| Fetal Medicine Foundation online calculator 53 | 1 | 0 | 0 | 0 | 1 (1) |
Australia.
New Zealand.
Middle cerebral artery.
Gestational age.
Estimated fetal weight.
Umbilical artery.
Systolic diastolic ratio.
Pulsatility index.
Resistive index.
Peak systolic velocity.
Cerebroplacental ratio.
Middle cerebral artery Doppler was performed for indications including EFW<10th percentile, abnormal umbilical artery Doppler and suspected fetal anaemia; however, 24% performed middle cerebral artery Doppler in all third trimester ultrasound. Most (52%) reported the pulsatility index (PI) with 36% indicating the peak systolic velocity was also reported. When middle cerebral artery Doppler was performed, the cerebroplacental ratio (CPR) was always reported in 55% of cases with 80% of respondents using <5th percentile for GA as the cut‐off for an abnormal CPR.
Third trimester ductus venosus Doppler practices varied. Although performed by 75% of respondents, indications for doing so differed in terms of GA cut‐off, EFW threshold, umbilical artery and middle cerebral artery Doppler parameters, and combinations of these factors. The (PI) was the most commonly reported index (27%), followed by the pulsatility index for veins (PVIV) (20%). Positivity/negativity of the A‐wave was reported by 21%. Half of the respondents did not perform uterine artery Doppler in the third trimester, and for those that did, indications included EFW<5th or 10th percentile (15% of responses) and a history of FGR (8% of responses). Most (65%) reported the pulsatility index. Details for ductus venosus and uterine artery Doppler practices are provided as supporting information.
The majority of respondents were not sure of which Doppler charts were used in their practice, and when charts were named, it was evident a wide variety of charts were used; 42% could name UA Doppler charts and while charts by Acharya 43 and Ebbing 44 were most popular; this only accounted for 12% and 13% of responses, respectively. A similar pattern was observed for additional Doppler measurements.
Choice of reference chart
Responses (125/125) to questions on the choice of reference chart are illustrated in Figure 2. Recommendations and guidelines of professional bodies and chart methodologies were the most important considerations in the choice of reference chart.
Figure 2.
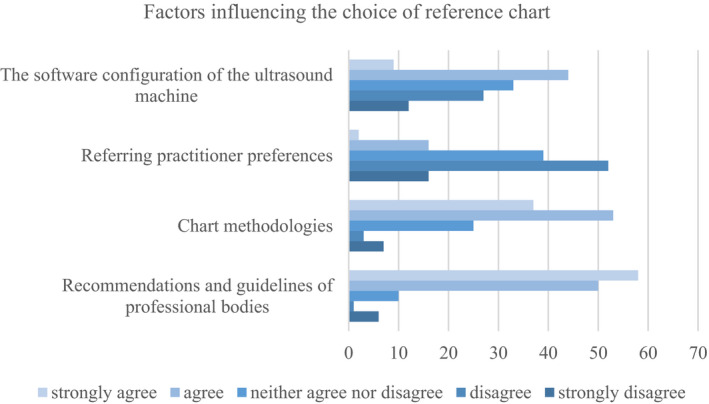
Factors influencing chart choice.
There were 32 comments made in response to ‘Is there anything you would like to add about how third trimester growth is performed and reported?’ A consistent theme emerging from the free text comments highlighted the need for national standardisation of reference charts used in third trimester ultrasound and standardised reporting (34%). Other comments included poor performance of ASUM FL percentiles (9%), a need for standardisation in reporting interval growth (13%), standardisation in reporting the amniotic fluid index (9%) and that changing reference charts would present difficulties (6%).
Discussion
This survey revealed inconsistent reporting practices with four population‐based charts for fetal biometry in current use: ASUM, 13 Hadlock, 21 , 22 , 23 , 24 Chitty 31 , 32 , 33 and Raine (Newnham, personal communication). Variation in choice of reference chart is comparable to a recent survey on fetal growth chart use in Italy. 54 There is diversity in Doppler practices, including when Doppler is performed, how it is reported and the choice of reference charts.
The use of charts derived from different populations for different biometry measures was another finding of this study. Although numbers were small (n = 10), Chitty 33 charts were used by some respondents for FL while ASUM 13 or Hadlock 21 , 22 , 23 charts were used for other measures. Older charts typically overestimate the FL; as ultrasound technology has improved over the past two decades, narrower beamwidth and higher scan‐line density have improved lateral resolution such that a FL measured with new equipment at mid‐trimester is shorter by 1mm on average than a FL measured with pre‐1998 equipment. 55 But this does not fully explain why these respondents favoured Chitty 33 (published in 1994) over more recently published charts. Interestingly, none in this group commented on ‘poor performance’ of ASUM 13 FL percentiles in the open text question.
The survey revealed the extent to which customised charts for EFW have been adopted (14% of respondents). However, a majority of respondents from New Zealand (73%) either report EFW percentiles using customised charts or include advice to plot measurements on a GROW 34 chart in the ultrasound report. Customisation takes into account maternal and fetal characteristics which may impact growth, namely maternal height and weight, parity, ethnic origin and fetal sex. GROW 34 software calculates an adjusted optimal fetal weight at 40 weeks GA and generates a proportionality curve based on the Hadlock 37 EFW curve. In addition to this individualised approach, population‐customised EFW curves may be produced 56 and formed the basis for charts used by a further 4% of respondents. 41 An additional 2% of respondents reported using EFW charts derived from the Raine Cohort (Newnham, personal communication), but did not specify if these were population‐customised. 57
The thresholds for the use of fetal and maternal Doppler in third trimester ultrasound varied in terms of the GA performed, EFW cut‐off and how measures were reported. While some respondents indicated certain Doppler measures were performed in all third trimester ultrasounds, no respondents performed umbilical artery, middle cerebral artery, ductus venosus and uterine artery, Doppler in every examination. Of the 22% of respondents reporting multiple indices for umbilical artery Doppler, the majority (70%) did not use a digital reporting package, suggesting deliberate co‐reporting of indices.
Comments made by respondents raised concerns regarding the lack of standardisation in how third trimester ultrasound is performed and the potential for diagnostic error:
‘Non uniformity makes ultrasound a potentially dangerous tool in my public hospital clinic. Standard reporting and reference ranges would be enormously useful.’
Some of these concerns may have since been addressed by the reporting template for third trimester fetal growth scans endorsed by ASUM, RANZCOG and RANZCR 58 in March 2019.
Study strengths and weaknesses
A weakness of this survey is the lower than expected response rate, even when the general decline in response rates in health research and the low reported response rates typical of medical specialists 59 is considered. The impact of this on interpretation of these findings is unclear as it has been shown response rate is not always predictive of nonresponse bias when the target population is relatively homogenous, as is the case with clinicans. 60 Mode of administration may have also contributed to the low response rate. It has been recently reported that the mode of survey administration does not affect the response rate from clinicians; however, emails inviting survey participation may be easily overlooked when the volume of emails is high. 61 Participant interest in the survey topic is another important factor influencing survey response rates, 59 and perhaps this topic of research only appealed to a small cohort. It was disappointing general radiologists were not part of this survey. Most radiologists in Australia and New Zealand are generalists, 92% are involved in reporting ultrasound, 62 and most obstetric ultrasounds are performed at generalist radiology practices. 63 Responses from this cohort may have provided valuable insights.
When compared to Australian and New Zealand surveys in 2013, 14 , 15 this study has shown there is more consistency in biometry charts used in current practice and a greater awareness of which chart is used. The way measurements are reported appears to be unchanged with most respondents using percentile for known GA and none using the z‐score. Awareness of which UA Doppler chart is used is unchanged with 58% of respondents indicating they were unsure. There was, however, a change in reporting practice for UA Doppler evidenced by the decline in the use of the SD ratio favour of the PI. More respondents (72%) indicated using a fetal weight chart for EFW rather than a birthweight chart, which differs from the 2011 study by Gibbons et al., 64 although these researchers acknowledged a degree of confusion exists amongst practitioners as to differences between population‐based birthweight charts, customised birthweight charts and fetal weight charts.
This change may be due to greater engagement with practice guidelines; notably, most New Zealand respondents reported using customised EFW charts and demonstrated consistent Doppler practices, in keeping with national guidelines. 65 , 66 , 67 There is also evidence of adherence to local institutional guidelines with the use of in‐house charts; Raine (Newnham, personal communication) and Mercy. 41 However, the ASUM Normal Ultrasonic Fetal Measurements Standard guideline updated in 2018 68 recommending the Hadlock 35 , 36 (HC‐AC‐FL) algorithm for EFW has yet to make an impact on reporting practices with 70% of respondents using the Hadlock 35 , 36 (BPD‐HC‐AC‐FL) algorithm to calculate EFW.
Conclusion
Inconsistent reporting practices still continue for third trimester ultrasound; however, this appears to be to a lesser extent than previously reported in 2013. 14 There appears to be a greater awareness of which reference chart is used for fetal biometry and EFW, but this is not true for Doppler charts. Overall, the use of Doppler in the third trimester is inconsistent, and with the exception of the UA and MCA, there is wide variation in the Doppler index reported. The potential for false‐positive and false‐negative diagnosis of FGR exists, and it remains possible for a fetus to have conflicting diagnoses based on the providers’ choice of reference chart. This situation will not change until there is consensus on which reference charts should be used. This could be achieved by an Australian and New Zealand collaboration to establish new charts constructed using best research practice.
Funding
No funding information is provided.
Disclosure
Debra Paoletti is a member of the ASUM board of directors, the ASUM DMU board of examiners and an associate editor of AJUM.
Author contributions
Debra Paoletti: Conceptualization (lead); Data curation (lead); Formal analysis (lead); Investigation (lead); Methodology (lead); Project administration (lead); Writing‐original draft (lead); Writing‐review & editing (lead). Lillian Smyth: Conceptualization (equal); Data curation (equal); Formal analysis (supporting); Methodology (equal); Supervision (equal); Writing‐review & editing (equal). Susan Campbell Westerway: Conceptualization (equal); Data curation (equal); Formal analysis (supporting); Methodology (equal); Supervision (equal); Writing‐review & editing (equal). Jon Hyett: Conceptualization (equal); Methodology (equal); Supervision (equal); Writing‐review & editing (equal). Ritu Mogra: Conceptualization (equal); Methodology (equal); Project administration (equal); Writing‐review & editing (equal). Stephen Haslett: Conceptualization (equal); Methodology (equal); Supervision (equal). Michael John Peek: Conceptualization (equal); Formal analysis (supporting); Methodology (equal); Supervision (lead); Writing‐review & editing (equal).
Supporting information
Table S1 Reporting practices for additional Doppler measures.
Appendix S1 Third trimester ultrasound and fetal measurements questionnaire.
Acknowledgements
The authors would like to thank RANZCOG, RANZCR and ASUM for assistance in distribution of the survey link and all those who took part in the survey.
References
- 1. Gardosi J, Madurasinghe V, Williams M, Malik A, Francis A. Maternal and fetal risk factors for stillbirth: population based study. BMJ 2013; 346: f108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Platz E, Newman R. Diagnosis of IUGR: traditional biometry. Semin Perinatol 2008; 32(3): 140–7. [DOI] [PubMed] [Google Scholar]
- 3. Hugh O, Williams M, Turner S, Gardosi J. Reduction of stillbirths in England according to uptake of the Growth Assessment Protocol, 2008‐2017: 10 year population based cohort study. Ultrasound Obstet Gynecol 2021; 57:401–8. [DOI] [PubMed] [Google Scholar]
- 4. Salomon LJ, Bernard JP, Duyme M, Buvat I, Ville Y. The impact of choice of reference charts and equations on the assessment of fetal biometry. Ultrasound in Obstetrics Gynecol 2005; 25(6): 559–65. [DOI] [PubMed] [Google Scholar]
- 5. Westerway SC. Estimating fetal weight for best clinical outcome. Australasian J Ultrasound Med. 2012; 15(1): 13–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hammami A, Mazer Zumaeta A, Syngelaki A, Akolekar R, Nicolaides KH. Ultrasonographic estimation of fetal weight: development of new model and assessment of performance of previous models. Ultrasound Obstet Gynecol 2018; 52(1): 35–43. [DOI] [PubMed] [Google Scholar]
- 7. Choi SKY, Gordon A, Hilder L, Henry A, Hyett JA, Brew BK, et al. Performance of six birthweight and estimated fetal weight standards for predicting adverse perinatal outcomes: a 10‐year nationwide population‐based study. Ultrasound Obst Gynecol 2021;58(2):264–77. [DOI] [PubMed] [Google Scholar]
- 8. Alfirevic Z, Stampalija T, Dowswell T. Fetal and umbilical Doppler ultrasound in high‐risk pregnancies. Cochrane Database Syst Rev 2017(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khalil A, Thilaganathan B. Role of uteroplacental and fetal Doppler in identifying fetal growth restriction at term. Best Practice Res Clin Obst Gynaecol. 2017; 38: 38–47. [DOI] [PubMed] [Google Scholar]
- 10. Khalil AA, Morales‐Rosello J, Morlando M, Hannan H, Bhide A, Papageorghiou A, et al. Is fetal cerebroplacental ratio an independent predictor of intrapartum fetal compromise and neonatal unit admission? Am J Obstet Gynecol 2015; 213(1): 54.e1–10. [DOI] [PubMed] [Google Scholar]
- 11. Oros D, Ruiz‐Martinez S, Staines‐Urias E, Conde‐Agudelo A, Villar J, Fabre E, et al. Reference ranges for Doppler indices of umbilical and fetal middle cerebral arteries and cerebroplacental ratio: systematic review. Ultrasound Obstet Gynecol 2019; 53(4): 454–64. [DOI] [PubMed] [Google Scholar]
- 12. Ruiz‐Martinez S, Papageorghiou AT, Staines‐Urias E, Villar J, Gonzalez De Agüero R, Oros D. Clinical impact of Doppler reference charts on management of small‐for‐gestational‐age fetuses: need for standardization. Ultrasound Obstet Gynecol 2020; 56(2): 166–72. [DOI] [PubMed] [Google Scholar]
- 13. Westerway SC, Davison A, Cowell S. Ultrasonic fetal measurements: new Australian standards for the new millennium. Aust N Z J Obstet Gynaecol 2000; 40(3): 297–302. [DOI] [PubMed] [Google Scholar]
- 14. McCarthy EA, Shub A, Walker SP. Is that femur really short? A survey of current and best practice in fetal biometry. Aust N Z J Obstet Gynaecol 2013; 53(2): 203–6. [DOI] [PubMed] [Google Scholar]
- 15. McCarthy EA, Walker SP, Shub A. Umbilical artery Doppler flow: an examination of current and best practice. Australian New Zealand J Obst Gynaecol. 2013; 53(4): 403–7. [DOI] [PubMed] [Google Scholar]
- 16. RANZCOG 2018‐2019 RANZCOG Annual Report [internet]; 2019. Available from: https://ranzcog.edu.au/ [cited 2020 July 10].
- 17. ASUM Annual Report 2017/2018 [internet]; 2018. Available from: https://www.asum.com.au/about‐the‐australasian‐society‐for‐ultrasound‐in‐medicine/governance/ [cited 2020 10 July].
- 18. Australian Bureau of Statistics 1270.0.55.004 – Australian Statistical Geography Standard (ASGS): Volume 4 – Significant Urban Areas, Urban Centres and Localities, Section of State. July 2016 [internet]; 2016. Available from: https://www.abs.gov.au [updated 9 October 2017; cited 2020 7 March].
- 19. Stats NZ Urban Rural Indicator 2018 V1.0.0 [internet]; 2017. Available from: http://aria.stats.govt.nz/aria/ [cited 2020 March 7].
- 20. Ministry of Health, District Health Board Code Table [internet]; 2015. Available from: https://www.health.govt.nz/ [updated 27 March 2015; cited 2020 June 7].
- 21. Hadlock FP, Deter RL, Harrist RB, Park SK. Fetal biparietal diameter: a critical re‐evaluation of the relation to menstrual age by means of real‐time ultrasound. J Ultrasound Med 1982; 1(3): 97–104. [DOI] [PubMed] [Google Scholar]
- 22. Hadlock FP, Deter RL, Harrist RB, Park SK. Fetal head circumference: relation to menstrual age. Am J Roentgenol 1982; 138(4): 649–53. [DOI] [PubMed] [Google Scholar]
- 23. Hadlock FP, Deter RL, Harrist RB, Park SK. Fetal abdominal circumference as a predictor of menstrual age. AJR Am J Roentgenol 1982; 139(2): 367–70. [DOI] [PubMed] [Google Scholar]
- 24. Hadlock FP, Harrist RB, Deter RL, Park SK. Fetal femur length as a predictor of menstrual age: sonographically measured. AJR Am J Roentgenol 1982; 138(5): 875–8. [DOI] [PubMed] [Google Scholar]
- 25. Papageorghiou AT, Ohuma EO, Altman DG, Todros T, Ismail LC, Lambert A, et al. International standards for fetal growth based on serial ultrasound measurements: the Fetal Growth Longitudinal Study of the INTERGROWTH‐21st Project. Lancet (London, England). 2014; 384(9946): 869–79. [DOI] [PubMed] [Google Scholar]
- 26. Schluter PJ, Pritchard G, Gill MA. Ultrasonic fetal size measurements in Brisbane, Australia. Australasian Radiol 2004; 48(4): 480–6. [DOI] [PubMed] [Google Scholar]
- 27. Schluter PJ, Pritchard G, Gill MA. Using ultrasonic fetal size measurements to estimate gestational age in Brisbane, Australia. Australasian Radiol 2007; 51(1): 46–52. [DOI] [PubMed] [Google Scholar]
- 28. Snijders RJM, Nicolaides KH. Fetal biometry at 14–40 weeks' gestation. Ultrasound Obstet Gynecol 1994; 4(1): 34–48. [DOI] [PubMed] [Google Scholar]
- 29. Jeanty P, Cousaert E, Hobbins JC, Tack B, Bracken M, Cantraine F. A longitudinal study of fetal head biometry. Am J Perinatol 1984; 1(2): 118–28. [DOI] [PubMed] [Google Scholar]
- 30. Jeanty P. Fetal limb biometry. Radiology 1983; 147(2): 601–2. [DOI] [PubMed] [Google Scholar]
- 31. Chitty LS, Altman DG, Henderson A, Campbell S. Charts of fetal size: 2. Head measurements. Br J Obstet Gynaecol 1994; 101(1): 35–43. [DOI] [PubMed] [Google Scholar]
- 32. Chitty LS, Altman DG, Henderson A, Campbell S. Charts of fetal size: 3. Abdominal measurements. BJOG Int J Obst Gynaecol. 1994; 101(2): 125–31. [DOI] [PubMed] [Google Scholar]
- 33. Chitty LS, Altman DG, Henderson A, Campbell S. Charts of fetal size: 4. Femur length. BJOG Int J Obst Gynaecol. 1994; 101(2): 132–5. [DOI] [PubMed] [Google Scholar]
- 34. Perinatal Institute . Gestation Network [internet]; 2020. Available from: https://www.gestation.net/index.htm [updated 2020; cited 2020 13 September].
- 35. Hadlock FP, Harrist RB, Carpenter RJ, Deter RL, Park SK. Sonographic estimation of fetal weight. The value of femur length in addition to head and abdomen measurements. Radiology 1984; 150(2): 535–40. [DOI] [PubMed] [Google Scholar]
- 36. Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK. Estimation of fetal weight with the use of head, body, and femur measurements–a prospective study. Am J Obstet Gynecol 1985; 151(3): 333–7. [DOI] [PubMed] [Google Scholar]
- 37. Hadlock FP, Harrist RB, Martinez‐Poyer J. In utero analysis of fetal growth: a sonographic weight standard. Radiology 1991; 181(1): 129–33. [DOI] [PubMed] [Google Scholar]
- 38. Roberts CL, Lancaster PA. Australian national birthweight percentiles by gestational age. Med J Aust 1999; 170(3): 114–8. [DOI] [PubMed] [Google Scholar]
- 39. WHO Fetal Growth Calculator [internet]; 2018. Available from: http://srhr.org/fetalgrowthcalculator/ [cited 2020 22 August].
- 40. Dobbins TA, Sullivan EA, Roberts CL, Simpson JM. Australian national birthweight percentiles by sex and gestational age, 1998–2007. Med J Aust 2012; 197(5): 291–4. [DOI] [PubMed] [Google Scholar]
- 41. Mercy Perinatal Antenatal Toolkit [internet]. Available from: https://mercyperinatal.com/toolkit [cited 2020 22 August].
- 42. Calculator for customised birth weight at term and optimal fetal weight according to gestation. New Zealand population [internet]; 2015. Available from: http://www.hutchon.net/CESDIcalcNZ.htm [updated 2015; cited 2020 22 September].
- 43. Acharya G, Wilsgaard T, Berntsen GKR, Maltau JM, Kiserud T. Reference ranges for serial measurements of umbilical artery Doppler indices in the second half of pregnancy. Am J Obstet Gynecol 2005; 192(3): 937–44. [DOI] [PubMed] [Google Scholar]
- 44. Ebbing C, Rasmussen S, Kiserud T. Middle cerebral artery blood flow velocities and pulsatility index and the cerebroplacental pulsatility ratio: longitudinal reference ranges and terms for serial measurements. Ultrasound Obstet Gynecol 2007; 30(3): 287–96. [DOI] [PubMed] [Google Scholar]
- 45. Trudinger BJ, Giles WB, Cook CM. Flow velocity waveforms in the maternal uteroplacental and fetal umbilical placental circulations. Am J Obstet Gynecol 1985; 152(2): 155–63. [DOI] [PubMed] [Google Scholar]
- 46. Trudinger BJ, Giles WB, Cook CM, Bombardieri J, Collins L. Fetal umbilical artery flow velocity waveforms and placental resistance: clinical significance. Br J Obstet Gynaecol 1985; 92(1): 23–30. [DOI] [PubMed] [Google Scholar]
- 47. Baschat AA, Gembruch U. The cerebroplacental Doppler ratio revisited. Ultrasound Obstet Gynecol 2003; 21(2): 124–7. [DOI] [PubMed] [Google Scholar]
- 48. Castro NM, Diesel HF, Huerta MG, Andrade EH. Normal reference values of the pulsatility index from the uterine and umbilical arteries during pregnancy. Ginecol Obstet Mex 2006; 74(10): 509–15. [PubMed] [Google Scholar]
- 49. Parra‐Cordero M, Lees C, Missfelder‐Lobos H, Seed P, Harris C. Fetal arterial and venous Doppler pulsatility index and time averaged velocity ranges. Prenat Diagn 2007; 27(13): 1251–7. [DOI] [PubMed] [Google Scholar]
- 50. Arduini D, Rizzo G. Normal values of Pulsatility Index front fetal vessels: A cross‐sectional study on 1556 healthy fetuses. J Perinatal Med. 1990; 18(3): 165–72. [DOI] [PubMed] [Google Scholar]
- 51. Ayoola OO, Bulus P, Loto OM, Idowu BM. Normogram of umbilical artery Doppler indices in singleton pregnancies in south‐western Nigerian women. J Obst Gynaecol Res. 2016; 42(12): 1694–8. [DOI] [PubMed] [Google Scholar]
- 52. Morales‐Roselló J, Khalil A, Morlando M, Hervás‐Marín D, Perales‐Marín A. Doppler reference values of the fetal vertebral and middle cerebral arteries, at 19–41 weeks gestation. J Maternal‐Fetal Neonatal Med. 2015; 28(3): 338–43. [DOI] [PubMed] [Google Scholar]
- 53. The Fetal Medicine Foundation Fetal Doppler Calculator [internet]; 2021. Available from: https://fetalmedicine.org/research/doppler
- 54. Stampalija T, Ghi T, Rosolen V, Rizzo G, Ferrazzi EM, Prefumo F, et al. Current use and performance of the different fetal growth charts in the Italian population. Eur J Obst Gynecol Reprod Biol. 2020; 252: 323–9. [DOI] [PubMed] [Google Scholar]
- 55. Okland I, Bjastad TG, Johansen TF, Gjessing HK, Grottum P, Eik‐Nes SH. Narrowed beam width in newer ultrasound machines shortens measurements in the lateral direction: fetal measurement charts may be obsolete. Ultrasound Obst Gynecol. 2011; 38(1): 82–7. [DOI] [PubMed] [Google Scholar]
- 56. Mikolajczyk RT, Zhang J, Betran AP, Souza JP, Mori R, Gülmezoglu AM, et al. A global reference for fetal‐weight and birthweight percentiles. Lancet 2011; 377(9780): 1855–61. [DOI] [PubMed] [Google Scholar]
- 57. White SW, Marsh JA, Lye SJ, Briollais L, Newnham JP, Pennell CE. Improving customized fetal biometry by longitudinal modelling. J Maternal‐fetal Neonatal Med. 2016; 29(12): 1888–94. [DOI] [PubMed] [Google Scholar]
- 58. The Third Trimester Fetal Growth Scans Reporting Template, endorsed by ASUM, RANZCOG (Royal Australian and New Zealand College of Obstetricians and Gynaecologists) and RANZCR (Royal Australian and New Zealand College of Radiologists) [internet]; 2019. Available from: https://www.asum.com.au/standards‐of‐practice/obstetrics‐and‐gynaecology/ [cited 2020 9 September]
- 59. Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, et al. Exploring physician specialist response rates to web‐based surveys. BMC Med Res Methodol 2015; 15(1): 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Taylor T, Scott A. Do physicians prefer to complete online or mail surveys? Findings from a national longitudinal survey. Eval Health Prof 2018; 42(1): 41–70. [DOI] [PubMed] [Google Scholar]
- 61. Weaver L, Beebe TJ, Rockwood T. The impact of survey mode on the response rate in a survey of the factors that influence Minnesota physicians’ disclosure practices. BMC Med Res Methodol 2019; 19(1): 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. 2016 RANZCR Clinical Radiology Workforce Census Report Australia [internet]; 2018. Available from: https://www.ranzcr.com/college/document‐library/2016‐clinical‐radiology‐workforce‐census‐report‐australia [cited 2020 Aug 28].
- 63. King K, Foo J, Hazelton K, Henry A. Selective versus universal third trimester ultrasound: Time for a rethink? An audit of current practices at a metropolitan Sydney hospital. Australasian. J Ultrasound Med 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gibbons K, Beckmann M, Flenady V, Rossouw D, Gardener G, Mahomed K, et al. A survey of policies for the monitoring of fetal growth in Australian and New Zealand hospitals. Australian New Zealand J Obst Gynaecol. 2011; 51(6): 493–8. [DOI] [PubMed] [Google Scholar]
- 65. New Zealand Maternal Fetal Medicine Network SGA guideline [internet]; 2014. Available from: https://www.healthpoint.co.nz/public/new‐zealand‐maternal‐fetal‐medicine‐network/ [updated 2014; cited 2020 9 September].
- 66. New Zealand Fetal Medicine Network Obstetric Doppler Guideline; 2014. Available from: https://www.healthpoint.co.nz/public/new‐zealand‐maternal‐fetal‐medicine‐network/?solo=otherList&index=5
- 67. Ministry of Health New Zealand Obstetric Ultrasound Guidelines. Wellington: Ministry of Health; 2019. Available from: https://www.health.govt.nz/publication/new‐zealand‐obstetric‐ultrasound‐guidelines [updated 2019; cited 2021 20 June]. [Google Scholar]
- 68. ASUM Normal Ultrasonic Fetal Measurements Standard 1991. Available from: https://www.asum.com.au/standards‐of‐practice/obstetrics‐and‐gynaecology/ [updated 2018; cited 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Reporting practices for additional Doppler measures.
Appendix S1 Third trimester ultrasound and fetal measurements questionnaire.


