Abstract
Background:
Understanding sexual partnerships of HIV-positive persons, particularly at the dyad level, can help in quantifying HIV transmission risk. We described sexual partnerships among HIV-positive men who have sex with men (MSM), including partnerships with a high risk for sexual HIV transmission.
Setting:
The Medical Monitoring Project is an annual, cross-sectional study that reports representative estimates on U.S. HIV-positive adults.
Methods:
During 2015–2019, we assessed sexual behaviors by interview, and viral load results from medical records. Among sexually active HIV-positive MSM (n = 4923), we described prevalence of high-risk sex, defined as: (1) not having sustained viral suppression, and (2) having condomless sex with an HIV-negative partner not known to be taking pre-exposure prophylaxis or an HIV-unknown partner. We described sexual partnerships among HIV-positive MSM (n = 13,024 partnerships among 4923 MSM). For HIV-discordant partnerships (n = 7768), we reported the proportion involved in high-risk sex, and associations with high-risk sex using prevalence ratios with predicted marginal means, controlling for age of the HIV-positive partner (P < 0.05).
Results:
More than half (66%) of sexually active HIV-positive MSM had condomless sex; 11% had high-risk sex. Blacks were more likely to have detectable viral loads, but less likely to have condomless sex, making prevalence of high-risk sex comparable between racial/ethnic groups. Dyad-level analyses among HIV-discordant partnerships indicated that prevalence of high-risk sex was higher among partnerships with HIV-positive white MSM, which was not observed using person-level data alone.
Conclusions:
In the context of ending the HIV epidemic, behavioral and clinical surveillance data can help monitor HIV transmission risk and target prevention efforts to reduce transmission among populations at disproportionate risk.
Keywords: men who have sex with men, high-risk sex, HIV, pre-exposure prophylaxis, race/ethnicity
INTRODUCTION
During 2017, 70% of diagnosed HIV infections in the United States were attributed to male-to-male sexual contact.1 Disparities in HIV diagnoses within selected populations of men who have sex with men (MSM) exist, particularly by race/ethnicity. For example, during 2014, the rate of new HIV diagnoses among black MSM were over 5 times as high compared with that among white MSM; these racial/ethnic disparities have persisted over time.2,3
Sexual HIV transmission risk is a function of sexual behaviors and viral load.4 Use of prevention strategies, such as pre-exposure prophylaxis (PrEP) and condom use, have been shown to decrease sexual HIV transmission risk.5–7 In addition, multiple studies have shown that persons with HIV who are virally suppressed have effectively no risk of transmitting HIV to sexual partners,8–10 leading to the development of the undetectable equals untransmittable (U = U) campaign in 2016.10 Because of the availability of multiple HIV prevention strategies and their relevance across partnerships with varying levels of sexual risk, estimating sexual HIV transmission risk and targeting interventions to reduce risk have become increasingly complex. In addition to clinical HIV surveillance data on HIV viral load, behavioral surveillance data describing the characteristics of sexual partnerships, including sexual behaviors within partnerships, are essential for monitoring patterns of high-risk sex associated with HIV transmission risk. These data can also help to target prevention efforts for reducing HIV transmission among populations with disproportionate HIV risk.
In addition to person-level data, using dyad-level data can provide more granular detail for assessing partnership characteristics, including components of high-risk sex associated with HIV transmission. Although previous studies have assessed sexual HIV transmission risk among MSM, these analyses have mostly focused on smaller populations or on persons at risk for HIV (i.e., from a risk acquisition standpoint), or have been restricted to persons currently in HIV care or certain geographic areas.3,11–15 In this analysis, we used nationally representative person-level and dyad-level data to describe characteristics of sexual partnerships of MSM with diagnosed HIV. We described high-risk sex within HIV-serodiscordant partnerships among MSM, overall and by selected characteristics, including race/ethnicity.
METHODS
Population
The Medical Monitoring Project (MMP) is an annual cross-sectional survey designed to produce nationally representative estimates of behavioral and clinical characteristics among adults with diagnosed HIV in the United States. Persons with diagnosed HIV are interviewed about sexual behaviors and HIV prevention practices, such as condom use, sex with HIV-concordant and HIV-discordant partners, and PrEP use in sexual partnerships, for the last 5 sexual partnerships reported in the previous 12 months. MMP provides a unique opportunity to use geographically diverse data from a probability sample of persons with diagnosed HIV in the United States (US) to examine sexual behaviors and use of single and combination HIV prevention strategies among MSM using person-level and sexual dyad data.
During 2015–2019, MMP used a two-stage sampling method, in which during the first stage, 16 states and 1 territory were sampled from all states in the US, the District of Columbia, and Puerto Rico. Areas were sampled with probability proportional to size based on AIDS prevalence at the end of 2002. In the second stage, for each jurisdiction, a simple random sample of persons aged ≥18 years with diagnosed HIV was sampled annually from the National HIV Surveillance System (NHSS), a census of persons with diagnosed HIV in the US. Data on demographic, behavioral, and clinical characteristics were collected through face-to-face or phone interviews, and medical record data were abstracted for all interviewed participants who received primary HIV care during the previous 2 years. Because MMP is conducted as a part of routine public health surveillance, it is deemed to be nonresearch. Participating jurisdictions obtained institutional review board approval for data collection as needed and informed consent was obtained from all participants.
All sampled jurisdictions participated in MMP, and included California (including the separately funded jurisdictions of Los Angeles County and San Francisco), Delaware, Florida, Georgia, Illinois (including Chicago), Indiana, Michigan, Mississippi, New Jersey, New York (including New York City), North Carolina, Oregon, Pennsylvania (including Philadelphia), Puerto Rico, Texas (including Houston), Virginia, and Washington. For each data cycle of MMP included in the analysis (2015, 2016, 2017, 2018), data were collected from June to May of the following year; national response rates for sampled persons by data cycle ranged from 40% to 45%.
Measures
Adults with diagnosed HIV were interviewed about demographic characteristics, such as age, race/ethnicity, gender, and sexual orientation, and sexual behaviors in the past 12 months, including condomless sex, sex in exchange for money or goods, and the total number of anal and vaginal sex partners. Detailed information was also collected about the last 5 reported sex partners, including HIV status, race/ethnicity, and gender of each partner; commitment level of each relationship; condom use with each partner; and whether each partner was known to be using PrEP. Viral load test results from the past year were abstracted from available medical records.
For this analysis, race and ethnicity were categorized as non-Hispanic white (henceforth referred to as white), non-Hispanic black/African American (henceforth referred to as black), Hispanic/Latino, and other (including multiracial). Data on PrEP use at the time of the last sexual encounter were collected from MMP participants for all HIV-negative partners. If participants either did not know whether their HIV-negative partner was using PrEP during the last sexual encounter or refused to answer questions regarding the partner’s PrEP use, we assumed that these HIV-negative partners were not using PrEP. Information on PrEP use among partners with an HIV-unknown status was not ascertained; these partners were assumed to not be using PrEP. Sustained viral suppression was defined as all viral loads being undetectable (<200 copies/mL) during the past 12 months.
We constructed a measure of high-risk sex associated with HIV transmission, hereafter referred to as high-risk sex, which was defined as the HIV-positive person: (1) not having sustained viral suppression (i.e., having ≥1 detectable viral load in the past 12 months), and (2) having condomless sex with an HIV-negative partner not known to be using PrEP or an HIV-unknown partner. This composite measure was intended to capture the proportion of persons and partnerships at risk for sexual HIV transmission.
Analysis
Person-Level Analysis
We analyzed pooled cross-sectional data collected during 2015–2019 and restricted the analysis to men with diagnosed HIV aged ≥18 years who reported having sex with at least one other male (MSM) in the past 12 months and reported detailed information on at least one partnership (n = 4923). Transgender men were excluded from the analysis because of limited sample size. Among sexually active MSM with diagnosed HIV, we described demographic characteristics, sexual behaviors, and components of high-risk sex associated with HIV transmission, including having: (1) an unsuppressed viral load, (2) condomless sex, (3) sex with an HIV-negative or HIV-unknown partner, and (4) sex with an HIV-negative partner not known to be using PrEP or an HIV-unknown partner, overall and by race/ethnicity. We also described the composite measure of high-risk sex as defined above. We reported components of high-risk sex among all sexually active MSM and among sexually active MSM who did not have sustained viral suppression (n = 1527). Rao–Scott χ2 tests were used to assess statistical differences between groups, where α = 0.05 determined statistical significance.
Dyad-Level Analysis
Next, among the 5 most recent sexual partnerships reported by MSM with diagnosed HIV in the past 12 months (n = 13,024 partnerships among 4923 MSM), we described partnerships by race/ethnicity, gender, level of commitment, sexual behaviors, and components of high-risk sex, overall and by HIV status of both partners. Transgender partners were excluded from the analysis because of limited sample size and instability of estimates among partnerships with transgender persons. Among HIV-discordant partnerships (n = 7768), in which HIV-positive MMP participants reported an HIV-negative or HIV-unknown partner, we reported the proportion of partnerships that involved high-risk sex, overall and by racial/ethnic partnerships, gender within partnerships, and level of partnership commitment. We examined associations with high-risk sex using prevalence ratios (PRs) with predicted marginal means, controlling for age of the HIV-positive participant. Age of the HIV-positive participant was presumed to be a potential confounder of the association between other characteristics of MSM and high-risk sex. In all dyad-level analyses, each partnership was assigned the weight of the MMP participant who reported the partnership such that weighted estimates represented sexual partnerships of MSM with diagnosed HIV in the U.S.
We reported weighted percentages and corresponding 95% confidence intervals (CIs) for all person-level and dyad-level estimates. Data were weighted on the basis of known probabilities of selection at state or territory and person levels. In addition, data were weighted to adjust for person nonresponse and poststratified to known population totals by age, race/ethnicity, and gender from NHSS. All analyses were conducted using survey procedures in SAS and SAS-callable SUDAAN.
RESULTS
Person-Level Analysis
Demographic Characteristics and Sexual Behaviors
Among MSM with diagnosed HIV who had vaginal or anal sex in the past 12 months, 38% were white, 29% were black, and 26% were Hispanic/Latino (Table 1). Overall, 84% self-identified as gay, but there were differences in sexual orientation by race/ethnicity (P < 0.0001), with 74% of black MSM identifying as homosexual or gay, compared with 89% of white and 87% of Hispanic/Latino MSM. The median number of sex partners in the past 12 months was 2 (min: 1, max: 960) and 3% of MSM exchanged sex for money or goods. Most (95%) persons had only male partners, but gender of sex partners differed significantly by race/ethnicity (P < 0.0001); 92% of black MSM had only male partners, compared with 98% of white and 95% of Hispanic/Latino MSM.
TABLE 1.
Demographic Characteristics and Sexual Behaviors Among Sexually Active Men Who Have Sex With Men With Diagnosed HIV, Overall and by Race/Ethnicity—MMP, 2015–2019 (n = 4923 Persons)*
| Overall |
White† |
Black† |
Hispanic/Latino† |
||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Weighted Col % (95% CI) | n | Weighted Col % (95% CI) | n | Weighted Col % (95% CI) | n | Weighted Col % (95% CI) | P | |
| Total persons (row %) | 4923 | 1918 | 38.0 (34.5 to 41.5) | 1474 | 29.1 (24.8 to 33.4) | 1182 | 25.5 (22.2 to 28.8) | ||
| Demographic characteristics | |||||||||
| Age, in yrs | <0.0001 | ||||||||
| 18–29 | 736 | 15.6 (13.9 to 17.3) | 101 | 7.1 (5.5 to 8.6) | 408 | 28.4 (25.3 to 31.5) | 174 | 13.3 (11.0 to 15.7) | |
| 30–39 | 1181 | 24.7 (23.2 to 26.2) | 332 | 17.5 (15.6 to 19.4) | 420 | 28.4 (25.5 to 31.4) | 340 | 29.2 (25.6 to 32.8) | |
| 40–49 | 1311 | 26.3 (24.6 to 28.1) | 537 | 26.7 (24.1 to 29.3) | 314 | 21.8 (19.4 to 24.1) | 359 | 31.2 (27.4 to 34.9) | |
| ≥50 | 1695 | 33.4 (31.3 to 35.5) | 948 | 48.8 (45.7 to 51.9) | 332 | 21.4 (18.0 to 24.7) | 309 | 26.3 (22.1 to 30.5) | |
| Sexual orientation | <0.0001 | ||||||||
| Gay | 4043 | 83.8 (82.1 to 85.5) | 1702 | 89.1 (87.2 to 91.0) | 1037 | 73.6 (70.6 to 76.7) | 1019 | 86.9 (84.5 to 89.3) | |
| Heterosexual or straight | 224 | 4.9 (3.9 to 5.8) | 81 | 4.6 (3.3 to 5.8) | 101 | 7.7 (6.0 to 9.5) | 31 | 2.6 (1.6 to 3.6) | |
| Bisexual | 534 | 11.3 (10.1 to 12.6) | 105 | 6.3 (4.8 to 7.8) | 272 | 18.7 (16.3 to 21.0) | 118 | 10.5 (8.2 to 12.7) | |
| Sexual behaviors in the past 12 mo | |||||||||
| Total number of sex partners, median [min–max] [IQR] | 2 [1–960] | 1 to 4 | 2 [1–600] | 1 to 5 | 2 [1–120] | 1 to 3 | 2 [1–960] | 1 to 4 | |
| No. of male sex partners, median [min–max] [IQR] | 2 [1–960] | 1 to 4 | 2 [1–600] | 1 to 5 | 2 [1–120] | 1 to 3 | 1 [1–960] | 1 to 4 | |
| Number of female sex partners, median [min–max] [IQR] | 0 [0–20] | 0 to 0 | 0 [0–15] | 0 to 0 | 0 [0–15] | 0 to 0 | 0 [0–20] | 0 to 0 | |
| No. of HIV-positive partners, median [min–max] [IQR] | 0 [0–255] | 0 to 1 | 0 [0–255] | 0 to 1 | 0 [0–95] | 0 to 1 | 0 [0–163] | 0 to 1 | |
| No. of HIV-negative/ unknown partners, median [min–max] [IQR] | 1 [0–956] | 0 to 3 | 1 [0–600] | 0 to 3 | 1 [0–80] | 0 to 2 | 1 [0–956] | 0 to 3 | |
| Gender of sex partners | <0.0001 | ||||||||
| Only males | 4677 | 95.1 (94.3 to 95.8) | 1876 | 98.0 (97.4 to 98.6) | 1355 | 91.6 (89.8 to 93.3) | 1116 | 94.7 (93.1 to 96.2) | |
| Males and females | 246 | 4.9 (4.2 to 5.7) | 42 | 2.0 (1.4 to 2.6) | 119 | 8.4 (6.7 to 10.2) | 66 | 5.3 (3.8 to 6.9) | |
| Sex exchanged for money or goods | 0.028 | ||||||||
| Yes | 167 | 3.4 (2.8 to 4.0) | 55 | 2.6 (1.8 to 3.5) | 44 | 3.0 (2.0 to 4.0) | 51 | 4.7 (3.0 to 6.5) | |
| No | 4753 | 96.6 (96.0 to 97.2) | 1862 | 97.4 (96.5 to 98.2) | 1429 | 97.0 (96.0 to 98.0) | 1131 | 95.3 (93.5 to 97.0) | |
Categories for some variables may not sum to total because of missing values.
Racial/ethnic categories are mutually exclusive. Hispanics/Latinos can be of any race. Other racial/ethnic groups excluded because of limited sample size.
Components of High-Risk Sex Among Sexually Active MSM
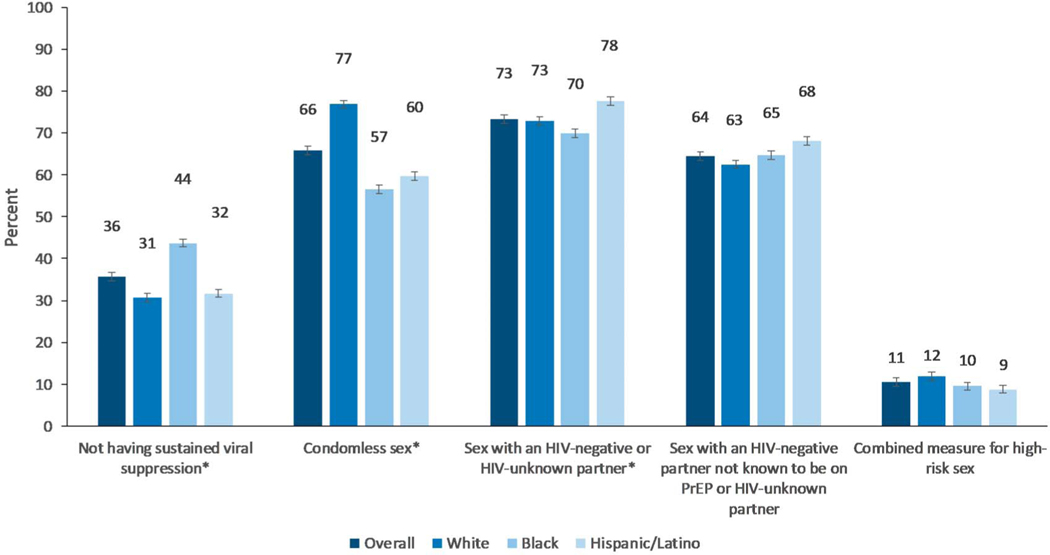
Among sexually active MSM, 36% did not have sustained viral suppression, 66% had condomless sex, 73% had sex with an HIV-negative or HIV-unknown partner, 64% had sex with an HIV-negative partner not known to be using PrEP or an HIV-unknown partner, and 11% engaged in high-risk sex (Fig. 1). There were significant differences in sustained viral suppression by race/ethnicity (P < 0.0001); specifically, 44% of blacks had a detectable viral load in the past 12 months, compared with 31% of whites and 32% of Hispanics/Latinos. There were also differences in condomless sex by race/ethnicity (P < 0.0001); 77% of whites had condomless sex, compared with 57% of blacks and 60% of Hispanics/Latinos. Overall, 73% had sex with an HIV-negative or HIV-unknown partner; estimates differed by race/ethnicity (P = 0.0014) (whites: 73%; blacks: 70%; Hispanics/Latinos: 78%). There were no significant differences in high-risk sex by race/ethnicity.
FIGURE 1.
Characteristics of high-risk sex among sexually active MSM with diagnosed HIV—Medical Monitoring Project, 2015–2019 (n = 4923 persons).
*Statistically significant differences at P<.05.
Note: Racial/ethnic categories are mutually exclusive. Hispanics/Latinos can be of any race. Sustained viral suppression was defined as having all undetectable (<200 copies/mL) viral loads in the past 12 months. Pre-exposure prophylaxis (PrEP) use was only measured for HIV-negative partners and was reported by the HIV- positive MMP participant. HIV-unknown partners were assumed to not be on PrEP. High-risk sex was defined as the HIV-positive MMP participant: (1) not having sustained viral suppression (i.e., having ≥1 detectable viral load in the past 12 months), and (2) having condomless sex with an HIV-negative partner not known to be using PrEP or HIV-unknown partner.
Components of High-Risk Sex Among Sexually Active MSM Who Were Not Virally Suppressed
Among MSM with diagnosed HIV who were not virally suppressed, 66% had condomless sex, 71% had sex with an HIV-negative or HIV-unknown partner, 62% had sex with an HIV-negative partner not known to be using PrEP or an HIV-unknown partner, and 30% engaged in high-risk sex (Fig. 2). There were significant differences in condomless sex by race/ethnicity among persons who did not have sustained viral suppression (P < 0.0001), where 56% of blacks had condomless sex, compared with 80% of whites and 64% of Hispanics/Latinos. In addition, the prevalence of high-risk sex varied by race/ethnicity (P < 0.0001), with 22% of blacks engaging in high-risk sex, compared with 39% of whites and 28% of Hispanics/Latinos.
FIGURE 2.
Characteristics of high-risk sex among sexually active MSM with diagnosed HIV who did not have sustained viral suppression in the past 12 months—Medical Monitoring Project, 2015–2019 (n = 1527 persons).
*Statistically significant differences at P<.05.
Note: Racial/ethnic categories are mutually exclusive. Hispanics/Latinos can be of any race. Sustained viral suppression was defined as having all undetectable (<200 copies/mL) viral loads in the past 12 months. Pre-exposure prophylaxis (PrEP) use was only measured for HIV-negative partners and was reported by the HIV- positive MMP participant. HIV-unknown partners were assumed to not be on PrEP. High-risk sex was defined as the HIV-positive MMP participant: (1) not having sustained viral suppression (i.e., having ≥1 detectable viral load in the past 12 months), and (2) having condomless sex with an HIV-negative partner not known to be using PrEP or HIV-unknown partner.
Prevalence of different combinations of the high-risk sex components among sexually active HIV-positive MSM are also presented in Appendix Table 1, Supplemental Digital Content, http://links.lww.com/QAI/B471.
Dyad-Level Analysis
Overall, 61% of partnerships in the past 12 months among HIV-positive MSM were HIV-discordant, of which 53% included an HIV-negative partner and 47% included an HIV-unknown partner (Table 2). Racial/ethnic partnerships were diverse, although racial/ethnic assortativity was more common among black MSM (73%) compared with white (61%) or Hispanic/Latino (58%) MSM. Most partnerships were male/male (98%). Among HIV-discordant partnerships, 67% included an HIV-positive person who did not have sustained viral suppression, 45% involved condomless sex, and 82% involved sex with an HIV-negative partner not known to be using PrEP or an HIV-unknown partner. Nine percent of HIV-discordant partnerships involved high-risk sex in the past 12 months.
TABLE 2.
Characteristics of Sexual Partnerships Among Men Who Have Sex With Men With Diagnosed HIV, Overall and by HIV Status Within Partnerships—MMP, 2015–2019 (n = 13,024 Partnerships)*
| Overall |
HIV-Discordant Partnerships |
HIV-Concordant Partnerships |
||||
|---|---|---|---|---|---|---|
| n | Weighted Col % (95% CI) | n | Weighted Col % (95% CI) | n | Weighted Col % (95% CI) | |
| Total partnerships (row %) | 13,024 | 7768 | 60.7 (59.1 to 62.3) | 5256 | 39.3 (37.7 to 40.9) | |
| HIV partnerships | ||||||
| HIV-positive/HIV-positive | 5256 | 39.3 (37.7 to 40.9) | — | 5256 | 100 | |
| HIV-positive/HIV-negative | 4113 | 32.3 (30.8 to 33.9) | 4113 | 53.3 (50.9 to 55.6) | — | |
| HIV-positive/HIV-unknown | 3655 | 28.4 (26.7 to 30.0) | 3655 | 46.7 (44.4 to 49.1) | — | |
| Race/ethnicity partnerships† | ||||||
| White HIV-positive person with white partner | 2988 | 23.5 (20.4 to 26.6) | 1666 | 22.3 (19.0 to 25.6) | 1322 | 25.4 (22.2 to 28.6) |
| White HIV-positive person with non-white partner | 2057 | 15.1 (13.9 to 16.3) | 1157 | 14.4 (13.1 to 15.8) | 900 | 16.1 (14.3 to 17.9) |
| Black HIV-positive person with black partner | 2752 | 21.0 (17.3 to 24.7) | 1590 | 20.0 (16.4 to 23.7) | 1162 | 22.5 (18.2 to 26.8) |
| Black HIV-positive person with non-black partner | 953 | 7.8 (6.6 to 8.9) | 567 | 7.8 (6.5 to 9.2) | 386 | 7.7 (6.5 to 9.0) |
| Hispanic/Latino HIV-positive person with Hispanic/Latino partner | 1632 | 14.5 (11.4 to 17.5) | 1170 | 17.3 (13.3 to 21.3) | 462 | 10.2 (8.1 to 12.2) |
| Hispanic/Latino HIV-positive person with non-Hispanic/Latino partner | 1383 | 10.7 (9.7 to 11.6) | 845 | 10.8 (9.7 to 12.0) | 538 | 10.4 (8.9 to 12.0) |
| Others | 935 | 7.4 (6.1 to 8.7) | 538 | 7.3 (5.9 to 8.7) | 397 | 7.7 (6.0 to 9.3) |
| Race/ethnicity partnerships† | ||||||
| White HIV-positive person | 5223 | 39.0 (35.2 to 42.8) | 2942 | 37.2 (33.3 to 41.1) | 2281 | 41.8 (37.5 to 46.0) |
| White partner | 2988 | 60.9 (58.1 to 63.7) | 1666 | 60.7 (57.1 to 64.3) | 1322 | 61.2 (57.9 to 64.4) |
| Non-white partner | 2057 | 39.1 (36.3 to 41.9) | 1157 | 39.3 (35.7 to 42.9) | 900 | 38.8 (35.6 to 42.1) |
| Black HIV-positive person | 3750 | 28.4 (24.1 to 32.8) | 2187 | 27.4 (23.1 to 31.7) | 1563 | 30.1 (25.1 to 35.0) |
| Black partner | 2752 | 73.0 (69.7 to 76.3) | 1590 | 72.0 (67.9 to 76.0) | 1162 | 74.5 (70.8 to 78.2) |
| Non-Black partner | 953 | 27.0 (23.7 to 30.3) | 567 | 28.0 (24.0 to 32.1) | 386 | 25.5 (21.8 to 29.2) |
| Hispanic/Latino HIV-positive person | 3096 | 25.1 (21.9 to 28.4) | 2086 | 28.1 (24.0 to 32.2) | 1010 | 20.5 (17.6 to 23.4) |
| Hispanic/Latino partner | 1632 | 57.5 (52.2 to 62.9) | 1170 | 61.5 (55.6 to 67.4) | 462 | 49.3 (43.9 to 54.7) |
| Non-Hispanic/Latino partner | 1383 | 42.5 (37.1 to 47.8) | 845 | 38.5 (32.6 to 44.4) | 538 | 50.7 (45.3 to 56.1) |
| Gender partnerships | ||||||
| Male/Male | 12,676 | 97.5 (97.0 to 98.0) | 7461 | 96.5 (95.8 to 97.1) | 5215 | 99.1 (98.7 to 99.5) |
| Male/Female | 315 | 2.5 (2.0 to 3.0) | 274 | 3.5 (2.9 to 4.2) | 41 | 0.9 (0.5 to 1.3) |
| Level of commitment in partnership | ||||||
| Not committed to very committed | 11,425 | 88.3 (87.5 to 89.1) | 6913 | 90.0 (89.1 to 90.9) | 4512 | 85.6 (84.3 to 87.0) |
| Committed to above and beyond anyone else | 1466 | 11.7 (10.9 to 12.5) | 746 | 10.0 (9.1 to 10.9) | 720 | 14.4 (13.0 to 15.7) |
| Components of high-risk sex | ||||||
| Did not have sustained viral suppression‡ | ||||||
| Yes | 9015 | 64.8 (62.3 to 67.2) | 5528 | 66.5 (63.7 to 69.3) | 3487 | 62.0 (58.8 to 65.2) |
| No | 4009 | 35.2 (32.8 to 37.7) | 2240 | 33.5 (30.7 to 36.3) | 1769 | 38.0 (34.8 to 41.2) |
| Had condomless sex | ||||||
| Yes | 7351 | 56.9 (54.3 to 59.5) | 3417 | 44.8 (41.8 to 47.7) | 3934 | 75.4 (72.8 to 78.0) |
| No | 5144 | 43.1 (40.5 to 45.7) | 3972 | 55.2 (52.3 to 58.2) | 1172 | 24.6 (22.0 to 27.2) |
| Had sex with an HIV-negative/unknown partner | ||||||
| Yes | 7768 | 60.7 (59.1 to 62.3) | 7768 | 100 | 0 | 0 |
| No | 5256 | 39.3 (37.7 to 40.9) | 0 | 0 | 5256 | 100 |
| Had sex with an HIV-negative partner not known to be on PrEP or an HIV-unknown partner§ | ||||||
| Yes | 6264 | 49.5 (47.7 to 51.2) | 6264 | 81.5 (79.9 to 83.1) | 0 | 0 |
| No | 6760 | 50.5 (48.8 to 52.3) | 1504 | 18.5 (16.9 to 20.1) | 5256 | 100 |
| Had high-risk sex∥ | ||||||
| Yes | 590 | 5.9 (4.8 to 7.0) | 590 | 8.7 (7.1 to 10.3) | — | |
| No | 10,879 | 94.1 (93.0 to 95.2) | 6997 | 91.3 (89.7 to 92.9) | — | |
Categories for some variables may not sum to total because of missing values. HIV-discordant partnerships were defined as including one HIV-positive person and one HIV-negative or HIV-unknown person. HIV-concordant partnerships were defined as including 2 HIV-positive persons.
Racial/ethnic categories are mutually exclusive. Hispanics/Latinos can be of any race.
Sustained viral suppression was defined as having all undetectable (<200 copies/mL) viral loads in the past 12 months.
Pre-exposure prophylaxis (PrEP) use was only measured for HIV-negative partners and was reported by the HIV-positive MMP participant. HIV-unknown partners were assumed to not be on PrEP.
High-risk sex was defined as the HIV-positive MMP participant: (1) not having sustained viral suppression (ie, having ≥1 detectable viral load in the past 12 months), and (2) having condomless sex with an HIV-negative partner not known to be using PrEP or an HIV-unknown partner.
Table 3 presents factors associated with high-risk sex in HIV-discordant partnerships, controlling for age of the HIV-positive participant. Although we did not find significant differences in high-risk sex by race/ethnicity in person-level analyses, we did observe differences by racial/ethnic partnerships in dyad-level analyses. Specifically, partnerships with a white HIV-positive participant had a higher prevalence of high-risk sex compared with those with black [aPR: 0.56 (95% CI: 0.39 to 0.80)] or Hispanic/Latino [aPR: 0.46 (95% CI: 0.31 to 0.68)] HIV-positive participants.
TABLE 3.
High-Risk Sex Among HIV-Discordant Sexual Partnerships of Men Who Have Sex With Men With Diagnosed HIV, Overall and by Selected Characteristics—MMP, 2015–2019 (n = 7768 Partnerships)*
| High-risk sex† |
||||||||
|---|---|---|---|---|---|---|---|---|
| Yes |
No |
|||||||
| n | Weighted Row % (95% CI) | n | Weighted Row % (95% CI) | Unadjusted PR‡ (95% CI) | P | Adjusted PR‡ (95% CI) | P | |
| Total partnerships | 590 | 8.7 (7.1 to 10.3) | 6999 | 91.3 (89.7 to 92.9) | ||||
| Age, in yrs | ||||||||
| 18–29 | 113 | 11.7 (7.4 to 15.9) | 1268 | 88.3 (84.1 to 92.5) | 1.33 (0.88 to 2.03) | 0.182 | ||
| 30–39 | 144 | 7.0 (4.9 to 9.0) | 1799 | 93.0 (91.0 to 95.1) | 0.80 (0.54 to 1.18) | 0.260 | ||
| 40–49 | 147 | 8.3 (5.8 to 10.8) | 1793 | 91.7 (89.2 to 94.2) | 0.95 (0.66 to 1.37) | 0.788 | ||
| ≥50 | 186 | 8.7 (6.5 to 11.0) | 2139 | 91.3 (89.0 to 93.5) | Reference | |||
| Race/ethnicity within partnerships§ | ||||||||
| White HIV-positive person with white partner | 141 | 11.3 (7.6 to 15.0) | 1501 | 88.7 (85.0 to 92.4) | Reference | Reference | ||
| White HIV-positive person with non-white partner | 118 | 11.7 (8.3 to 15.0) | 1024 | 88.3 (85.0 to 91.7) | 1.03 (0.71 to 1.51) | 0.869 | 1.04 (0.73 to 1.50) | 0.823 |
| Black HIV-positive person with black partner | 116 | 7.4 (5.1 to 9.7) | 1428 | 92.6 (90.3 to 94.9) | 0.65 (0.44 to 0.98) | 0.040 | 0.57 (0.37 to 0.90) | 0.016 |
| Black HIV-positive person with non-black partner | 36 | 7.5 (4.2 to 10.7) | 513 | 92.5 (89.3 to 95.8) | 0.66 (0.39 to 1.12) | 0.125 | 0.60 (0.35 to 1.03) | 0.061 |
| Hispanic/Latino HIV-positive person with Hispanic/Latino partner | 63 | 6.1 (3.8 to 8.3) | 1098 | 93.9 (91.7 to 96.2) | 0.54 (0.33 to 0.87) | 0.012 | 0.52 (0.32 to 0.85) | 0.010 |
| Hispanic/Latino HIV-positive person with non-Hispanic/Latino partner | 47 | 4.8 (2.8 to 6.9) | 787 | 95.2 (93.1 to 97.2) | 0.43 (0.25 to 0.72) | 0.002 | 0.41 (0.24 to 0.71) | 0.002 |
| Others | 52 | 11.1 (6.5 to 15.7) | 472 | 88.9 (84.3 to 93.5) | 0.98 (0.60 to 1.61) | 0.933 | 0.93 (0.56 to 1.56) | 0.783 |
| Race/ethnicity of HIV-positive person§ | ||||||||
| White | 272 | 11.6 (8.7 to 14.4) | 2617 | 88.4 (85.6 to 91.3) | Reference | Reference | ||
| Black | 154 | 7.4 (5.4 to 9.5) | 1956 | 92.6 (90.5 to 94.6) | 0.64 (0.46 to 0.89) | 0.009 | 0.56 (0.39 to 0.80) | 0.002 |
| Hispanic/Latino | 111 | 5.5 (3.8 to 7.2) | 1941 | 94.5 (92.8 to 96.2) | 0.48 (0.33 to 0.70) | ,0.001 | 0.46 (0.31 to 0.68) | ,0.001 |
| Other | 53 | 11.0 (6.5 to 15.5) | 485 | 89.0 (84.5 to 93.5) | 0.95 (0.61 to 1.47) | 0.815 | 0.90 (0.57 to 1.41) | 0.644 |
| Race/ethnicity of HIV-negative/unknown partner§ | ||||||||
| White | 210 | 9.7 (7.2 to 12.3) | 2433 | 90.3 (87.7 to 92.8) | Reference | Reference | ||
| Black | 201 | 8.5 (6.3 to 10.7) | 2106 | 91.5 (89.3 to 93.7) | 0.87 (0.65 to 1.18) | 0.386 | 0.83 (0.60 to 1.17) | 0.290 |
| Hispanic/Latino | 147 | 8.1 (6.1 to 10.0) | 1964 | 91.9 (90.0 to 93.9) | 0.83 (0.60 to 1.14) | 0.247 | 0.83 (0.60 to 1.14) | 0.243 |
| Gender partnerships | ||||||||
| Male/Male | 578 | 8.9 (7.3 to 10.5) | 6725 | 91.1 (89.5 to 92.7) | 2.53 (1.25 to 5.13) | 0.009 | 2.52 (1.24 to 5.11) | 0.009 |
| Male/Female | 12 | 3.5 (1.0 to 6.0)*,¶ | 258 | 96.5 (94.0 to 99.0) | Reference | Reference | ||
| Level of commitment in partnership | ||||||||
| Not committed to very committed | 515 | 8.3 (6.7 to 10.0) | 6261 | 91.7 (90.0 to 93.3) | Reference | Reference | ||
| Committed to above and beyond anyone else | 74 | 12.0 (8.8 to 15.3) | 665 | 88.0 (84.7 to 91.2) | 1.44 (1.06 to 1.97) | 0.022 | 1.45 (1.06 to 1.97) | 0.02 |
Categories for some variables may not sum to total because of missing values. HIV-discordant partnerships were defined as including one HIV-positive person and one HIV-negative or HIV-unknown person.
High-risk sex was defined as the HIV-positive MMP participant: (1) not having sustained viral suppression (ie, having ≥1 detectable viral load in the past 12 months), and (2) having condomless sex with an HIV-negative partner not known to be using PrEP or an HIV-unknown partner.
PRs were adjusted for age.
Racial/ethnic categories are mutually exclusive. Hispanics/Latinos can be of any race.
Estimates with a coefficient of variation $0.30 should be interpreted with caution.
DISCUSSION
This is the first analysis to present nationally representative estimates of characteristics of sexual partnerships among MSM with diagnosed HIV, including a composite measure describing high-risk sex. This comprehensive measure of high-risk sex builds on previously published work using national surveillance data to describe components of sexual risk.12,16,17 Specifically, this analysis incorporated PrEP use among sexual partners of HIV-positive MMP participants, and analyzed sexual risk at the dyad level, which had not been done previously. We showed that most sexually active MSM had condomless sex in the past 12 months. However, when accounting for a combination of sustained viral suppression and risk reduction strategies, only 11% of sexually active MSM with diagnosed HIV engaged in high-risk sex, thereby illustrating the importance of PrEP, condom use, and HIV treatment as HIV prevention strategies. Although a higher proportion of blacks had detectable viral loads compared with other racial/ethnic groups, fewer blacks had condomless sex, and thus, the proportion of MSM with diagnosed HIV engaging in high-risk sex was comparable between racial/ethnic groups. Of all partnerships among HIV-positive MSM, 61% were HIV-discordant, of which 9% involved high-risk sex. Although person-level analyses did not show racial/ethnic differences in high-risk sex, dyad-level analyses among HIV-discordant partnerships demonstrated that high-risk sex varied by race/ethnicity of the HIV-positive partner, with partnerships of white HIV-positive MSM engaging in more high-risk sex compared with other partnerships.
We demonstrated that 64% of sexually active MSM had sustained viral suppression, and thus, had negligible risk of transmitting HIV to sexual partners. However, among persons who did not have sustained viral suppression, about a third of persons had condomless sex with an HIV-negative or HIV-unknown partner not known to be using PrEP, and thus were engaging in behaviors associated with HIV transmission to sexual partners. White MSM were more likely to engage in high-risk sexual behaviors compared with other MSM. Although PrEP is now recommended for use in populations at high risk for HIV, PrEP use has been shown to be significantly higher among white versus black MSM.10,18 Interventions aimed to increase availability and provision of PrEP among populations at high risk for HIV may help reduce HIV transmission. Further, medical providers could help HIV patients develop strategies to reduce HIV transmission risk to sexual partners, including achieving and maintaining viral suppression and consistent condom use, particularly for those with sexual partners who are HIV-negative or have an unknown HIV status.
Dyad-level data showed that high-risk sex was more prevalent in partnerships with white HIV-positive MSM. These results may seem counterintuitive, because HIV prevalence and incidence are higher among black MSM.2,3 Previous studies have explored potential reasons for the discrepancy in patterns of sexual HIV transmission risk and HIV burden by race/ethnicity.11,13,15,19–25 For instance, some studies demonstrated that black MSM represent a smaller total population but also a higher proportion of the HIV-positive population, and that black MSM have higher levels of racial/ethnic assortativity, compared with white MSM. Therefore, despite engaging in fewer high-risk sexual behaviors, HIV-negative black MSM may be more likely to encounter persons with HIV, which may partially contribute to higher HIV incidence and prevalence among black MSM.15,20,21 We observed similar patterns, with black MSM having higher levels of racial/ethnic assortativity in partnerships compared with white MSM, but also higher levels of condom use. However, racial/ethnic sexual assortativity may not alone explain disparities in HIV incidence and prevalence, and social determinants of health, including stigma and previous history of trauma, may also contribute to racial/ethnic differences in HIV incidence and prevalence.11,13 In addition, because HIV disproportionately affects younger black MSM compared with white MSM, and younger persons generally are more likely to engage in high-risk sex compared with older persons, age may confound the association between race/ethnicity and high-risk sex.1 However, even when we controlled for age of the HIV-positive participant, differences in high-risk sex by race/ethnicity remained. Future studies should continue to explore the role of all of these factors on HIV transmission by race/ethnicity.
Although HIV-discordant partnerships that include HIV-positive persons with undetectable viral loads have negligible risk for sexual HIV transmission, condom use is still important for the prevention of sexually transmitted infections (STIs). Condom use is particularly relevant among MSM, among whom a substantial proportion of STI diagnoses in the U.S. occur compared with other populations.5,8–10,26 Prevalence of STI diagnoses have also been shown to be higher among black MSM compared with white MSM.25,27 Presence of STIs can also increase viral shedding of HIV, thus increasing transmission risk to sexual partners.28,29 Recurrent history of STI diagnoses can also increase risk of acquiring HIV infection.30 Given recent increases in diagnoses of syphilis, gonorrhea, and chlamydia among men, promoting condom-protected sex is important for prevention of STIs, regardless of HIV status, viral load, or PrEP use.7,26
There were some limitations in this analysis. Data collected on sexual partners, including race/ethnicity and HIV status, were self-reported and only reflected the perspective of the HIV-positive MMP person. Because HIV-discordant partnerships included partners with unknown HIV status, estimates of high-risk sex were highly influenced by our inclusion of partners with unknown HIV status, and our assumption that partners with unknown HIV status were not taking PrEP. Thus, we conducted a sensitivity analysis in which we examined high-risk sex by selected characteristics among HIV-discordant partners, excluding those with unknown HIV status, to provide a lower bound for our estimates of high-risk sex (see Appendix Table 2, Supplemental Digital Content, http://links.lww.com/QAI/B471). Even in the sensitivity analysis, differences in high-risk sex by race/ethnicity remained. Estimates on dyad-level analyses were representative of the last 5 sex partners of MMP participants in the past 12 months, and not all partners. Approximately 20% of sexually active HIV-positive MSM had more than 5 sex partners in the past 12 months. Also, despite adjustment for nonresponse using standard methodology,31 nonresponse bias may remain to some extent. Even with suboptimal response rates, however, there is still value in results obtained from unbiased sampling methods.32 Finally, although we were able to incorporate both viral load and sexual behaviors into estimates for high-risk sex, we were not able to account for the timing of unsuppressed viral loads with respect to condomless sex with an HIV-negative or unknown partner.
To our knowledge, these are the first nationally representative estimates describing the sexual partnerships of HIV-positive MSM using person and dyad-level data. We used a comprehensive measure of high-risk sex that builds on previously published work using national surveillance data to describe sexual risk behaviors. We demonstrated that most sexually active HIV-positive MSM had sustained viral suppression, although there is room for improvement to reach the national prevention goal of viral suppression among at least 90% of persons with diagnosed HIV.33 This has implications for the U = U campaign, which has been instrumental in communicating that people with HIV can live long, healthy lives without risk of transmission to others, and thus, has the potential to reduce HIV-related stigma. Given the importance of viral suppression in both reducing HIV transmission risk and improving health outcomes, providers should address barriers to maintaining viral suppression among patients, and continue talking with patients about HIV prevention strategies, including U = U.
We also reported that the prevalence of high-risk sex among sexually active HIV-positive MSM was 11%, and was 9% among HIV-discordant partnerships. However, among persons who were not virally suppressed, 30% were engaging in high-risk sex. Dyad-level analyses demonstrated that the prevalence of high-risk sex was higher among partnerships with white HIV-positive MSM compared with other partnerships, which was not observed using person-level data alone. Recently, the Ending the HIV Epidemic initiative was announced, in which the primary goal was to reduce new HIV infections by 90% in 10 years; reaching this goal will require increasing promotion of various risk reduction strategies, including viral suppression, condom use, sexual HIV concordance, and PrEP use. These findings demonstrate the use of MMP data in monitoring patterns in HIV transmission risk, which is key to targeting prevention efforts to reduce HIV transmission among populations at disproportionate risk.
Supplementary Material
ACKNOWLEDGMENTS
The authors acknowledge MMP project areas and participants for their contributions.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Footnotes
The authors have no conflicts of interest to disclose. CDC funded data collection and other activities related to the Medical Monitoring Project.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.jaids.com).
REFERENCES
- 1.CDC. HIV Surveillance Report: Diagnoses of HIV Infection in the United States and Dependent Areas, 2017. CDC; Vol 28; 2018. Available at: https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. [Google Scholar]
- 2.Purcell DW, Johnson CH, Lansky A, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS J. 2012;6:98–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenberg ES, Purcell DW, Grey JA, et al. Rates of prevalent and new HIV diagnoses by race and ethnicity among men who have sex with men, U.S. States, 2013–2014. Ann Epidemiol. 2018;28:865–873. [DOI] [PubMed] [Google Scholar]
- 4.Patel P, Borkowf CB, Brooks JT, et al. Estimating per-act HIV transmission risk: a systematic review. AIDS. 2014;28:1509–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316:171–181. [DOI] [PubMed] [Google Scholar]
- 6.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010; 363:2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CDC U. Preexposure Prophylaxis for the Prevention of HIV Infection in the United States-2017 Update: A Clinical Practice Guideline. CDC; 2018. Available at: https://www.cdc.gov/hiv/guidelines/preventing.html. [Google Scholar]
- 8.Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375:830–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Risk of Sexual Transmission of HIV from a Person Living with HIV Who Has an Undetectable Viral Load. Available at: https://www.preventionaccess.org/consensus. Accessed March 1, 2020.
- 11.Goodreau SM, Rosenberg ES, Jenness SM, et al. Sources of racial disparities in HIV prevalence in men who have sex with men in atlanta, Ga, USA: a modelling study. Lancet HIV. 2017;4:e311–e320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mattson CL, Freedman M, Fagan JL, et al. Sexual risk behaviour and viral suppression among HIV-infected adults receiving medical care in the United States. AIDS. 2014;28:1203–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mustanski B, Morgan E, D’Aquila R, et al. Individual and network factors associated with racial disparities in HIV among young men who have sex with men: results from the radar cohort study. J Acquir Immune Defic Syndr. 2018;80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beer L, Oster AM, Mattson CL, et al. Disparities in HIV transmission risk among HIV-infected black and white men who have sex with men, United States, 2009. AIDS. 2014;28:105–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenberg ES, Millett GA, Sullivan PS, et al. Understanding the HIV disparities between black and white men who have sex with men in the USA using the HIV care continuum: a modeling study. Lancet HIV. 2014;1:e112–e118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hall HI, Holtgrave DR, Tang T, et al. HIV transmission in the United States: considerations of viral load, risk behavior, and health disparities. AIDS Behav. 2013;17:1632–1636. [DOI] [PubMed] [Google Scholar]
- 17.Holtgrave DR, Hall HI, Des Jarlais DC, et al. Estimating number of diagnosed persons living with HIV in the United States engaged in unprotected serodiscordant risk behavior with unsuppressed viral load. J Acquir Immune Defic Syndr. 2014;65:e125–128. [DOI] [PubMed] [Google Scholar]
- 18.Hoots BE, Finlayson T, Nerlander L, et al. , National HIVBSSG. Willingness to take, use of, and indications for pre-exposure prophylaxis among men who have sex with men-20 Us cities, 2014. Clin Infect Dis. 2016;63:672–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelley CF, Rosenberg ES, O’Hara BM, et al. Measuring population transmission risk for HIV: an alternative metric of exposure risk in men who have sex with men (MSM) in the us. PLoS One. 2012;7:e53284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raymond HF, McFarland W. Racial mixing and HIV risk among men who have sex with men. AIDS Behav. 2009;13:630–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Janulis P, Phillips G, Birkett M, et al. Sexual networks of racially diverse young MSM differ in racial homophily but not concurrency. J Acquir Immune Defic Syndr. 2018;77:459–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Millett GA, Flores SA, Peterson JL, et al. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–2091. [DOI] [PubMed] [Google Scholar]
- 23.Maulsby C, Millett G, Lindsey K, et al. HIV among black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18:10–25. [DOI] [PubMed] [Google Scholar]
- 24.Magnus M, Kuo I, Phillips G II, et al. Elevated HIV prevalence despite lower rates of sexual risk behaviors among black men in the District of Columbia who have sex with men. AIDS Patient Care STDS. 2010;24:615–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380:341–348. [DOI] [PubMed] [Google Scholar]
- 26.CDC. Sexually Transmitted Disease Surveillance 2017. CDC; 2018. Available at: https://www.cdc.gov/nchhstp/newsroom/2018/2017-STD-surveillance-report.html. [Google Scholar]
- 27.Grey JA, Bernstein KT, Sullivan PS, et al. Rates of primary and secondary syphilis among white and black non-hispanic men who have sex with men, United States, 2014. J Acquir Immune Defic Syndr. 2017; 76:e65–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson LF, Lewis DA. The effect of genital tract infections on HIV-1 shedding in the genital tract: a systematic review and meta-analysis. Sex Transm Dis. 2008;35:946–959. [DOI] [PubMed] [Google Scholar]
- 29.Kelley CF, Vaughan AS, Luisi N, et al. The effect of high rates of bacterial sexually transmitted infections on HIV incidence in a cohort of black and white men who have sex with men in atlanta, Georgia. AIDS Res Hum Retroviruses. 2015;31:587–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bernstein KT, Marcus JL, Nieri G, et al. Rectal gonorrhea and Chlamydia reinfection is associated with increased risk of HIV seroconversion. J Acquir Immune Defic Syndr. 2010;53:537–543. [DOI] [PubMed] [Google Scholar]
- 31.Iachan R, Johnson CH, Harding RL, et al. Design and weighting methods for a nationally representative sample of HIV-infected adults receiving medical care in the United States-medical monitoring project. Open AIDS J. 2016;10:164–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opin Q. 2006;70:646–675. [Google Scholar]
- 33.What Is “Ending the HIV Epidemic: A Plan for America”? Available at: https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview. Accessed March 1, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.