Abstract
Background
Correct mask use can prevent the spread of COVID-19 and hospitals require correct mask use. Despite this, there is variation in mask use among health care workers (HCW). Incorrect mask use may lead to increased infections and decreased feelings of safety. The purpose of this study was to determine variation in mask use among HCW as well as feelings of safety from exposure to COVID-19 when around colleagues before and after COVID-19 vaccine roll out.
Methods
This study used direct observation to assess mask use in patient-facing areas before and after COVID-19 vaccine. A staff survey was used to assess feelings of safety.
Results
Over 1,600 mask observations showed increased compliance from 94.6% to 97.5% (P = .001). Three hundred survey responses showed significantly increased feelings of safety (P < .001) after vaccine roll out, and 203 free-text responses with respondant reasoning were categorized into 6 themes.
Discussion
Understanding mask use behaviors and safety attitudes of HCW can help improve policies, workplace culture, and reduce HCW to HCW infections.
Conclusions
Correct mask use was a highly adopted habit in patient-facing areas. The COVID-19 vaccine led to significantly increased feelings of safety among HCW, though the diverging narratives seen in the survey may be helpful to consider when crafting safety interventions.
Key Words: Infection prevention, Narrative medicine, Hang hygiene, Workplace culture, Healthcare, Behavior change
The COVID-19 pandemic created an unprecedented challenge for health care. Correct mask use, defined as covering the nose and mouth, has been shown to help prevent the spread of COVID-191 and the CDC continues to recommend mask use in health care facilities. Despite continued education and signage about masking requirements, there is variation in mask use among health care workers (HCW). Incorrect mask use, even if rare, may lead to increased infections and decreased feelings of safety at work. All incoming staff and visitors at our 304-bed community teaching hospital in Michigan, USA, are given a mask but the rate of correct mask use is not known. Impact of incorrect mask use on HCW feelings of safety is also unknown.
The goal of this study is to determine the rate of correct mask use among HCW before and after COVID-19 vaccine roll out at our institution. A secondary aim is to determine how safe HCW felt from exposure to COVID-19 when around their colleagues before and after vaccine roll out and the factors that influenced their perceived safety.
The hospital received its first COVID-19 patient on March 14, 2020. The hospital serves an elderly population, and according to internal records, act as the primary emergency response hospital for approximately 141 facilities (skilled nursing, assisted living, independent living, and senior apartments) and 39 group homes. Data from our infection prevention team show that from March to June 2020 the hospital treated a total of 1,504 COVID-19 patients, with an average of 40-60 confirmed and suspected COVID-19 patients daily with a peak of 151 patients on April 9, 2020. During that time, 209 patients passed away from COVID-19, a case fatality rate of 13.8 per 100 hospitalized patients.
Caring for patients suspected or confirmed to have COVID-19 and the worry of spreading the virus to family and friends may manifest as emotional fatigue and anxiety in frontline staff.2 While initial shortages of masks and isolation gowns were mitigated, changes in protocols, long hours spent in personal protective equipment (PPE), complex patient care, high mortality, and unknowns about transmission, has anecdotally contributed to fear and exhaustion among HCW at the hospital.
In the first months of the pandemic, education at the hospital was disseminated electronically from twice daily COVID-19 huddles, followed by the addition of nursing educators and signage demonstrating correct mask use and donning and doffing procedures. The hospital continues to provide up-to-date guidance to staff on PPE and safe COVID-19 patient care.3 , 4
Few studies have used direct observation to assess variation in mask use among HCW in the hospital setting since the start of the pandemic. One observational study from Uttarakhand, India5 showed 54.1%-75.6% correct mask use among HCW, where correct mask use was defined as wearing a medical, non-cloth mask over the nose, mouth, and chin. A study from Zehejiang, China6 showed 73.8% correct mask use, defined as a surgical mask “worn correctly” per their Infection Prevention Department. Incorrect mask use in this study was described as “pulled downwards.” Another study from Canada7 conducted after a facility-wide outbreak of COVID-19, showed that having an observer, or “dofficer,” monitor PPE compliance and provide intervention resulted in a reduction of errors in donning and doffing from 9.81% to 2.88%.
Despite knowledge of masking efficacy in preventing the spread of COVID-191 there is still variation in compliance. One study of Americans and Canadians found that reported mask compliance among the general public was 84%. The 16% who did not wear masks did so because of beliefs that masks were ineffective and/or had an aversion to being forced to wear masks.8
In addition to masking as a means of COVID-19 prevention, many HCW have received COVID-19 vaccines. HCW were prioritized in the initial mRNA COVID-19 vaccine roll out in December 2020. One study of 609 HCW in California, USA, explored attitudes towards the upcoming COVID-19 vaccine.9 They found that 46.9% of respondents felt that the vaccine would protect them from COVID-19, with 65.5% planning to delay vaccination after it became available. Those who planned to delay vaccination cited a desire to “wait and see” how the vaccine affected others (49.9%), and 1.30% indicated they never planned to receive the vaccine.
These studies demonstrate variation in mask use in the health care setting, variation in attitudes towards mask use and vaccination as well as the emotional burden carried by HCW during the pandemic. Our study aims to explore objective mask use among HCW before and after vaccine roll out, as well as their subjective feelings of safety at work while around their colleagues.
Methods
This was a single center Institutional Review Board approved quality improvement study. The safety intervention was defined as the COVID-19 vaccine roll out at our institution, with pre- and post-assessments of HCW mask use and feelings of safety. Similar to how hand hygiene has been studied,10 , 11 , 12 mask use data was collected by non-intrusive, direct observation of HCW. Observations occurred over two 5-day, Monday through Friday, periods. The first mask observation period was conducted in November 2020. COVID-19 vaccination at the hospital began on December 24, 2020. The second observation period as well as a staff survey occurred in February 2021 to give adequate time for staff to receive both doses of the mRNA vaccine. Direct observation was completed by a group of volunteers HCW and health professional students who were trained to use a standardized data collection sheet. Observations occurred between 6am-6pm in patient-facing areas and were not recorded if a HCW was eating or drinking. No observation was done in private offices or staff break rooms. Location was limited to non-COVID-19 general medicine floors and the hospital's main Atrium to limit COVID-19 exposure. Mask compliance was recorded as 1 of 4 discrete options: Covers nose and mouth; Below nose; Below mouth; and No mask.
The survey was sent to HCW on the main hospital campus by their department leaders. Staff were given 2 weeks to complete the survey on our secure hospital network and all data was collected in REDCap. The survey asked respondents to rate their feelings of safety from exposure to COVID-19 when around their colleagues at work before and after COVID-19 vaccine roll out. Staff were given the option to share their role and primary work location from a dropdown menu, as well as an optional text box to explain why they rated their pre-vaccine feelings of safety as they did.
Descriptive statistics were used to analyze mask observation and survey data. Distribution of mask use across time points and by role was analyzed as categorical and ordinal data using chi-square and Wilcoxon-Mann-Whitney tests respectively. Because survey data are paired data, feelings of safety across time points and by role was analyzed as categorical and ordinal data role using McNemar and Wilcoxon Signed Rank tests respectively. The free-text data from respondents explaining their pre-vaccine feelings of safety were scored into 6 categories. Categories were determined by a research team member, author LO, who reviewed all free-text responses and identified common sentiments. These common sentiments were coded with a number, 1 through 6, to represent each category. Comments that indicated no opinion or lacked reasoning, such as “N/A” or “no change” were excluded.
Results
A total of 1,016 mask observations were collected over the 5-day period in November 2020 and correct mask use was observed in 961 (94.59%) HCW. A total of 594 mask observations were collected over the 5-day period in February 2021 and correct mask use was observed in 579 (97.5%) HCW (Table 1 ). There was significant (P = .001) improvement in ordinal compliance across time points. This difference was driven mainly by the decrease in wearing masks below the nose (P = .004) and increase in correct mask use (P = .005) (Table 1). Most groups maintained or improved their mask compliance, though the change was not statistically significant for any group (Table 1).
Table 1.
Mask use before and after vaccine roll out - overall and by role
| Variable | Label | Pre (N = 1,016) | Post (N = 594) | P value |
|---|---|---|---|---|
| Mask use (categorical) | ||||
| Mask covers nose and mouth | 961 (94.59%) | 579 (97.47%) | .005 | |
| Mask below nose | 27 (2.66%) | 4 (0.67%) | .004 | |
| Mask below mouth | 15 (1.48%) | 9 (1.52%) | >.999 | |
| No mask | 13 (1.28%) | 2 (0.34%) | .063 | |
| Mask use (ordinal) | 1.09 (0.44) | 1.05 (0.31) | .001 |
| Mask use by role (Ordinal) | Pre | Post | P Value | |
|---|---|---|---|---|
| Doctor | 1.1 (0.49) | 1.04 (0.26) | .248 | |
| Food service | 1.08 (0.28) | 1 (0) | .327 | |
| Nurse | 1.1 (0.48) | 1.05 (0.34) | .110 | |
| Patient care assistant | 1.13 (0.44) | 1.05 (0.32) | .215 | |
| Phlebotomist | 1 (0) | 1 (0) | NA | |
| Physical therapist | 1 (0) | 1.08 (0.4) | .250 | |
| Respiratory therapist | 1 (0) | 1 (0) | NA | |
| Social worker/case manager | 1.38 (1.06) | 1.29 (0.76) | >.999 | |
| Transport | 1.03 (0.16) | 1 (0) | .516 | |
| Other | 1.08 (0.39) | 1.05 (0.29) | .209 | |
NOTE. P values come from chi-square tests for categorical data and Wilcoxon-Mann-Whitney tests for ordinal data. For the ordinal coding of mask use, a value of 1 is defined as “Mask covers nose and mouth,” and a value of 4 is defined as “No mask”. Values between 1 and 4 indicate a gradient from correct mask use to no mask use.
The distribution of observations by role was relatively consistent across time points (Table 2 ). The only group with significantly different representation between time points was patient care assistants who made up 11.71% in the pre-period and 6.73% in the post-period (P = .002) (Table 2). There was a significant difference in the distribution of observations from the General Medicine floors relative to the Atrium, with the proportion of Atrium observations making up a larger share of the sample in the postperiod (83.5%) compared to the pre-period (62.7%) (P < 0.001) (Table 2).
Table 2.
Mask observation demographics
| Distribution of role |
|||
|---|---|---|---|
| Role | Pre (N = 1,016) | Post (N = 594) | P value |
| Doctor | 189 (18.6%) | 131 (22.05%) | .107 |
| Food service | 37 (3.64%) | 12 (2.02%) | .093 |
| Nurse | 337 (33.17%) | 203 (34.18%) | .721 |
| Patient care assistant | 119 (11.71%) | 40 (6.73%) | .002 |
| Phlebotomist | 9 (0.89%) | 4 (0.67%) | .864 |
| Physical therapist | 35 (3.44%) | 25 (4.21%) | .519 |
| Respiratory therapist | 5 (0.49%) | 6 (1.01%) | .366 |
| Social worker/case manager | 8 (0.79%) | 7 (1.18%) | .604 |
| Transport | 38 (3.74%) | 18 (3.03%) | .542 |
| Other | 239 (23.52%) | 148 (24.92%) | .568 |
| Relative distribution of location |
|||
|---|---|---|---|
| Location | Pre (N=1016) | Post (N=594) | |
| General Medicine floors | 379 (37.3%) | 98 (16.5%) | <.001 |
| Atrium | 637 (62.7%) | 496 (83.5%) | |
NOTE. P values come from chi-square tests.
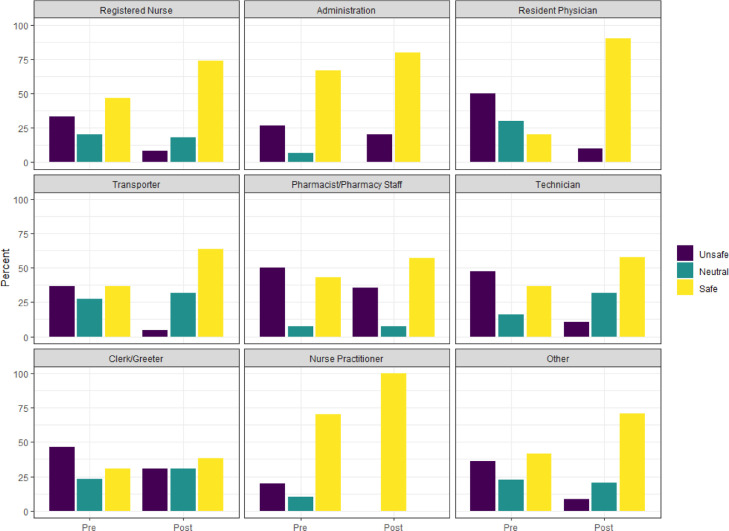
The staff survey received 300 responses. It demonstrated that feelings of safety around colleagues at work increased significantly after the COVID-19 vaccine roll out in December 2020 (P < 0.001) (Table 3 and Fig 1 ). Response options consisted of a 5-point Likert Scale ranging from 1 = very unsafe to 5 = very safe. There was a significant improvement in feelings of safety for all roles other than Administration and Clerk/Greeter, which showed non-significant improvements. Staff were given the option to share their primary role and primary work location (Table 4 ).
Table 3.
Feeling of safety before and after vaccine roll out – overall and by role
| Variable | Label | Before (N = 300) | After (N = 300) | P value |
|---|---|---|---|---|
| Safety (categorical) | ||||
| very unsafe | 28 (9.33%) | 4 (1.33%) | <.001 | |
| moderately unsafe | 79 (26.33%) | 28 (9.33%) | <.001 | |
| neutral | 61 (20.33%) | 56 (18.67%) | .920 | |
| moderately safe | 90 (30%) | 131 (43.67%) | <.001 | |
| very safe | 42 (14%) | 81 (27%) | <.001 | |
| Safety (ordinal) | 3.13 (1.22) | 3.86 (0.97) | <.001 |
| Role | Before | After | P value | |
|---|---|---|---|---|
| Registered Nurse | 3.23 (1.19) | 3.94 (0.92) | <.001 | |
| Administration | 3.53 (1.55) | 4.13 (1.19) | .298 | |
| Resident Physician | 2.7 (0.82) | 3.9 (0.74) | .018 | |
| Transporter | 3.09 (1.02) | 3.77 (0.81) | .003 | |
| Pharmacist/Pharmacy Staff | 2.64 (1.5) | 3.21 (1.19) | .305 | |
| Technician | 3.05 (1.43) | 3.74 (0.99) | .014 | |
| Clerk/Greeter | 2.77 (1.24) | 3.15 (1.21) | .298 | |
| Nurse Practitioner | 3.5 (0.85) | 4.3 (0.48) | .031 | |
| Other | 3.02 (1.24) | 3.91 (0.98) | <.001 | |
NOTE. P values come from McNemar tests for categorical data and Wilcoxon Signed Rank tests for ordinal data. For the ordinal coding of safety data, a value of 1 is defined as “very unsafe” and a value of 5 is defined as “very safe.”
Fig 1.
Note. Distribution of responses to feelings of safety question by primary role in the pre- and post-period. Values of 1 and 2 are collapsed into a single “unsafe” category, and values of 4 and 5 are collapsed into a single “safe” category.
Table 4.
Survey demographics
| Role | N = 300 | |
|---|---|---|
| Administration | 15 (5%) | |
| Clerk/Greeter | 13 (4.33%) | |
| Nurse Practitioner | 10 (3.33%) | |
| Pharmacist/Pharmacy Staff | 14 (4.67%) | |
| Registered Nurse | 133 (44.33%) | |
| Resident Physician | 10 (3.33%) | |
| Technician | 19 (6.33%) | |
| Transporter | 22 (7.33%) | |
| Other | 58 (19.33%) | |
| Missing | 6 (2%) | |
| Location | N = 300 | |
| General Medicine Floors | 44 (14.67%) | |
| Emergency Department | 38 (12.67%) | |
| Mobile service/floater/general inpatient | 16 (5.33%) | |
| Operating/procedure room | 12 (4%) | |
| Outpatient clinics | 19 (6.33%) | |
| Pre and Post-Operative space | 12 (4%) | |
| Radiology suite | 11 (3.67%) | |
| Shared administrative space | 11 (3.67%) | |
| Other | 119 (39.67%) | |
| Missing | 18 (6%) | |
NOTE. Staff were given the option to provide their primary role and work location from a dropdown menu.
The survey included the optional question: “Why did you rate your feelings of safety before vaccination started as you did?” This question received 203 (67.7%) free-text responses that fell into 6 categories. Categories and representative examples are shown in Table 5a . While a majority of responses (125/203, 61.6%) fell into a category that described feeling less safe prior to the vaccine, free-text responses helped highlight broad and often diverging safety narratives as highlighted in Table 5b .
Table 5a.
Select survey responses representing 6 categories of prevaccine feelings of safety
| Category | Responses (N = 203) | % Total | Quote | Role | Safety pre | Safety post |
|---|---|---|---|---|---|---|
| Unsafe due to workspace proximity and poor adherence to social distancing and PPE by colleagues | 61 | 30.0% | “Colleagues traveling, having gatherings with family and friends, poor adherence to masking policy.” | RN | Moderately Unsafe | Moderately Safe |
| Safe due to adherence to PPE and safety guidelines by themselves and their colleagues | 58 | 28.6% | “Colleagues were very good at wearing masks, utilizing hand sanitizer, keeping distance. Most people were great role models” | PA | Moderately Safe | Very Safe |
| Unsafe due to a general high concern about COVID-19 | 47 | 23.2% | “I felt afraid because there were a lot of unknown facts about the virus.” | Role not provided | Neutral | Moderately Safe |
| Safe due to a general low concern about COVID-19 | 20 | 9.9% | “I was not concerned of getting exposed from a colleague. I assume they won't come to work if they feel ill.” | RN | Moderately Safe | Moderately Safe |
| Unsafe due to hospital policy implementation | 10 | 4.9% | “Visitors are NOT wearing masks in patient rooms… hardly any staff members are enforcing this rule (or even aware of this rule)…” | RN | Very Unsafe | Moderately Unsafe |
| Unsafe due to the vaccine | 7 | 3.4% | “…Staff think they will not get COVID if they are vaccinated and may not maintain the social distancing and mask wearing consistently.” | Role not provided | Very Safe | Neutral |
Table 5b.
Selected responses representing diverging narratives of safety
| Quote | Role | Safety pre | Safety post |
|---|---|---|---|
| “I don't think we should have to wear masks anymore.” | RN | Very Safe | Very Safe |
| “I don't feel safe from COVID anywhere, except my home.” | Clerk | Very Unsafe | Very Unsafe |
| “I knew I could get it from co-workers, but also that severe symptoms, hospitalization, death, etc. was very low, so I was not scared.” | Role Not Provided | Neutral | Moderately Safe |
| “With certain colleagues, I didn't feel like they were taking precautions against the virus as seriously as I was. My dad has COPD so I have been very anxious and worried, and trying hard to keep him safe.” | RN | Moderately Unsafe | Neutral |
| “99% + survival rate” | RN | Moderately Safe | Moderately Safe |
| “Because I am a very bad asthmatic and I'm also considered obese, and I've gotten very bad lung infections in the past, I felt if I got COVID-19, I would not have made it. I would have died.” | Clerk | Very Unsafe | Neutral |
Another theme that emerged across categories was “see something, say something.” These responses were from HCW who took it upon themselves to “say something” to colleagues or bring up policy issues to hospital administration. Some responses made it apparent that they were tired of this role and felt they were not being heard. One representative response from a respiratory therapist who felt moderately safe before and after vaccination reads: “I don't feel that we ALL took it seriously, therefore it required frequent reminders to staff to mask-up, wear proper PPE, etc. All of which gets tiring.” Another response from a nurse who went from feeling very unsafe to moderately unsafe reads: “I don't feel we are doing everything we can to protect ourselves or the patients. I have tried to bring attention to the fact that we are not enforcing many of the new COIVD policies that are in place. So far, the issues I have voiced concern about have not changed.”
Discussion
There was a very high rate of correct mask use in patient-facing areas at both time points. There are many possible reasons for the increase in correct mask use from 94.6% in November 2020 to 97.5% in February 2021. Possible contributing factors include the vaccine roll out in December 2020, additional time reinforcing the habit of masking, and/or as a response to the surge of COVID-19 cases in Michigan in November 2020.13 It was unlikely due to inpatient cases as the infection prevention team reported an average of 43 COVID-19 inpatients per day in November compared to an average of 16 inpatients per day in February. It is important not to overstate the significance of the improvement in mask use over time. Despite statistical significance, the magnitude of change was small and our study faced limitations which make direct comparison between time points difficult. Outside of vaccine roll out, our study was not designed to account for the rapidly changing landscape of the COVID-19 pandemic including case numbers and attitudes towards PPE. Another limitation was the variation in the location and number of observations between time points. Despite these limitations, high rates of correct mask use in patient-facing areas indicate that masking is a highly adopted practice among HCW at the hospital.
The survey data showed a significant increase in feelings of safety after vaccine roll out, but respondents’ free text explanations of their pre-vaccine feelings of safety showed a striking divergence in the lived experience of the pandemic and perceived risk of exposure from colleagues (Table 5b). Notably, we did not conduct mask observations in private offices or break rooms where staff spend time eating and drinking together, activities where masks are typically off. This may help account for the discrepancy between the high rates of mask use in patient-facing areas and relatively low feelings of safety among staff when around their colleagues.
Continued vaccination is encouraging, but herd immunity appears less likely in the US due to vaccine hesitancy.14 COVID-19 is likely to be with us for some time due to new mutations and possibly as an annual virus.15 The health care community will have to continue improving and adapting safety measures and success will require buy in from HCW. For these reasons, it is important to understand these safety narratives and account for them in the design and implementation of safety interventions.
One way to interpret safety behaviors during the pandemic is through an understanding of attribution bias and naïve realism. Attribution bias is the tendency to attribute others’ behaviors to their character rather than their circumstances.16 , 17 Attribution bias stems from naïve realism, which is a tendency to believe that we see the world rationally and objectively, and those who behave otherwise must be mis-informed or irrational.18 Variation in a community's safety behaviors and an individual's interpretation of them exists because it is informed by that individual's personal experience and risk tolerance. Similar to how those driving slower on the freeway seem overly cautious and those driving faster seem reckless, those wearing a N95 at all times may seem overly cautious, while a colleague who pulls down their mask to speak can seem reckless.
This data shows that there is variation in how safe HCW feel while around their colleagues at work during the pandemic. Patient safety is a unifying goal which has motivated advances in infection control and quality improvement. COVID-19 has posed an additional unique challenge to HCW safety. Organizational awareness of these issues and a focus on “provider wellbeing” may go a long way to normalize these new concerns. Leadership's ability to reach out to vaccine hesitant or non-compliant sub-groups will also play a key role in continuing to provide a safe environment in health care.
There are many challenges in the pursuit of objective and subjective safety. One challenge is that behavior change is difficult, and its difficulty is exacerbated by the fact that HCW are mentally and emotionally fatigued.2 In addition, when the pandemic began, masking was not as common of a habit in the US as it was in some countries, and faced the added handicap of mixed messaging early on about masking effectiveness.19 , 20
One historic example that can be used to understand mask compliance is hand hygiene. The benefits of hand washing for infection control have been known for hundreds of years, and yet, hospitals still require reminders and interventions in our effort to reach 100% compliance.21 A common model is appointing a hand hygiene champion whose role it is to educate, encourage and monitor for proper hand hygiene.22 Our survey demonstrates that staff have taken it upon themselves to point out lapses in masking and have grown fatigued. Masking champions or “dofficers”7 may be able to lift this burden from staff and provide regular and accurate feedback. Healthcare leadership may consider looking at models for hand hygiene and other infection control practices at their institution to draw inspiration for increasing mask compliance.
The challenges posed by the diverging narratives seen in the survey need to be explored in our current crisis, but also for reasons beyond the COVID-19 pandemic. There will be future challenges in health care that require a unified response from HCW. More importantly, it is always a good time to improve our culture of safety. HCW need to be able to respectfully point out lapses to a co-worker to keep our patients and each other safe. Implementing mask use and social distancing have put this practice to the test, in our communities and at work.
Conclusion
This study showed that mask use is a highly adopted practice among HCW in patient-facing areas, with correct mask use accounting for >94% of over 1,600 staff observations. HCW reported significant improvement in feelings of safety from exposure to COVID-19 when around their colleagues after vaccine roll out. Narrative reports of pre-vaccine feelings of safety exposed a divergent and conflicting experience of the pandemic. Understanding these narratives may be helpful when crafting COVID-19 safety interventions. The health care community has made tremendous progress in PPE availability and ubiquity, and we have seen its ability to keep HCW safe when used properly. This data can help build on the progress already made in patient and HCW safety during the COVID-19 pandemic. Better understanding of the lived experience of HCW during the pandemic can help to implement effective practices now, next season, and in the next safety challenge.
Acknowledgments
Special acknowledgement to Methods Consultants for assistance with statistical analysis; Laurie McHugh for assistance with project coordination; and Luna Nasry, Christina Lui, and Matthew Chuang for assistance with data collection.
Footnotes
Conflicts of Interest: None to report.
References
- 1.Howard J, Huang A, Li Z, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci U S A. 2021;118:2–8. doi: 10.1073/pnas.2014564118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirkman J. Depressive symptoms, perceived risk of infection,and emotional fatigue among COVID-19 frontline medical personnel. Psychosociol Issues Human Resour Manage. 2021;9:49–53. [Google Scholar]
- 3.Interim Public Health Recommendations for Fully Vaccinated People. In: Control CfD, editor. cdc.gov 2021.
- 4.Updated Healthcare Infection Prevention and Control Recommendations in Response to COVID-19 Vaccination. In: Control CfD, editor. cdc.gov 2021.
- 5.Supehia S, Singh V, Sharma T, Khapre M, Gupta PK. Rational use of face mask in a tertiary care hospital setting during COVID-19 pandemic: an observational study. Indian J Public Health. 2020;64(Supplement) doi: 10.4103/ijph.IJPH_493_20. S225-S7. [DOI] [PubMed] [Google Scholar]
- 6.Xu C, Jin J, Song J, et al. Application of refined management in prevention and control of the coronavirus disease 2019 epidemic in non-isolated areas of a general hospital. Int J Nurs Sci. 2020;7:143–147. doi: 10.1016/j.ijnss.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Picard C, Edlund M, Keddie C, et al. The effects of trained observers (dofficers) and audits during a facility-wide COVID-19 outbreak: a mixed-methods quality improvement analysis. Am J Infect Control. 2021;49:1136–1141. doi: 10.1016/j.ajic.2021.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor S, Asmundson GJG. Negative attitudes about facemasks during the COVID-19 pandemic: the dual importance of perceived ineffectiveness and psychological reactance. PLoS One. 2021;16 doi: 10.1371/journal.pone.0246317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gadoth A, Halbrook M, Martin-Blais R, et al. Cross-sectional assessment of COVID-19 vaccine acceptance among health care workers in Los Angeles. Ann Intern Med. 2021;174:882–885. doi: 10.7326/M20-7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.King D, Vlaev I, Everett-Thomas R, Fitzpatrick M, Darzi A, Birnbach DJ. Priming" hand hygiene compliance in clinical environments. Health Psychol. 2016;35:96–101. doi: 10.1037/hea0000239. [DOI] [PubMed] [Google Scholar]
- 11.Derde LPG, Cooper BS, Goossens H, et al. Interventions to reduce colonisation and transmission of antimicrobial-resistant bacteria in intensive care units: an interrupted time series study and cluster randomised trial. Lancet Infect Dis. 2014;14:31–39. doi: 10.1016/S1473-3099(13)70295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diegel-Vacek L, Ryan C. Promoting hand hygiene with a lighting prompt. HERD. 2016;10:65–75. doi: 10.1177/1937586716651967. [DOI] [PubMed] [Google Scholar]
- 13.Coronavirus: Michigan Data michigan.gov2021 Accessed May 17, 2021. https://www.michigan.gov/coronavirus/
- 14.Amin DP, Palter JS. COVID-19 vaccination hesitancy among healthcare personnel in the emergency department deserves continued attention. Am J Emerg Med. 2021;48:372–373. doi: 10.1016/j.ajem.2021.01.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahase E. Covid-19: booster dose will be needed in autumn to avoid winter surge, says government adviser. BMJ. 2021;372:n664. doi: 10.1136/bmj.n664. [DOI] [PubMed] [Google Scholar]
- 16.Robinson J. Exploring attribution theory and bias. Commun Teacher. 2017;31:209–213. [Google Scholar]
- 17.Chaiyachati K, Kangovi S. Inappropriate ED visits: patient responsibility or an attribution bias? BMJ Qual Saf. 2020;29:441–442. doi: 10.1136/bmjqs-2019-009729. [DOI] [PubMed] [Google Scholar]
- 18.Nasie M, Bar-Tal D, Pliskin R, Nahhas E, Halperin E. Overcoming the barrier of narrative adherence in conflicts through awareness of the psychological bias of naive realism. Pers Soc Psychol Bull. 2014;40:1543–1556. doi: 10.1177/0146167214551153. [DOI] [PubMed] [Google Scholar]
- 19.Lang J, Erickson WW, Jing-Schmidt Z. #MaskOn! #MaskOff! Digital polarization of mask-wearing in the United States during COVID-19. PLoS One. 2021;16 doi: 10.1371/journal.pone.0250817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen A. Dis/avowing masks: culture, race, and public health between the United States and Taiwan. Med Anthropol Theory. 2021;8:2–8. [Google Scholar]
- 21.Gould DJ, Moralejo D, Drey N, Chudleigh JH, Taljaard M. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev. 2017;9 doi: 10.1002/14651858.CD005186.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goedken CC, Livorsi DJ, Sauder M, et al. The role as a champion is to not only monitor but to speak out and to educate": the contradictory roles of hand hygiene champions. Implement Sci. 2019;14:110. doi: 10.1186/s13012-019-0943-x. [DOI] [PMC free article] [PubMed] [Google Scholar]