Abstract
Background
Selective serotonin reuptake inhibitors (SSRIs) might theoretically reduce post‐stroke disability by direct effects on the brain. This Cochrane Review was first published in 2012 and last updated in 2019.
Objectives
To determine if SSRIs are more effective than placebo or usual care at improving outcomes in people less than 12 months post‐stroke, and to determine whether treatment with SSRIs is associated with adverse effects.
Search methods
We searched the Cochrane Stroke Group Trials Register (last searched 7 January 2021), Cochrane Controlled Trials Register (CENTRAL, Issue 7 of 12, 7 January 2021), MEDLINE (1946 to 7 January 2021), Embase (1974 to 7 January 2021), CINAHL (1982 to 7 January 2021), PsycINFO (1985 to 7 January 2021), and AMED (1985 to 7 January 2021). PsycBITE had previously been searched (16 July 2018). We searched clinical trials registers.
Selection criteria
We included randomised controlled trials (RCTs) recruiting stroke survivors within the first year. The intervention was any SSRI, at any dose, for any period, and for any indication. The comparator was usual care or placebo. Studies reporting at least one of our primary (disability score or independence) or secondary outcomes (impairments, depression, anxiety, quality of life, fatigue, cognition, healthcare cost, death, adverse events and leaving the study early) were included in the meta‐analysis. The primary analysis included studies at low risk of bias.
Data collection and analysis
We extracted data on demographics, stroke type and, our pre‐specified outcomes, and bias sources. Two review authors independently extracted data. We used mean difference (MD) or standardised mean differences (SMDs) for continuous variables, and risk ratios (RRs) for dichotomous variables, with 95% confidence intervals (CIs). We assessed bias risks and applied GRADE criteria.
Main results
We identified 76 eligible studies (13,029 participants); 75 provided data at end of treatment, and of these two provided data at follow‐up. Thirty‐eight required participants to have depression to enter. The duration, drug, and dose varied. Six studies were at low risk of bias across all domains; all six studies did not need participants to have depression to enter, and all used fluoxetine. Of these six studies, there was little to no difference in disability between groups SMD ‐0.0; 95% CI ‐0.05 to 0.05; 5 studies, 5436 participants, high‐quality evidence) or in independence (RR 0.98; 95% CI 0.93 to 1.03; 5 studies, 5926 participants; high‐quality evidence) at the end of treatment.
In the studies at low risk of bias across all domains, SSRIs slightly reduced the average depression score (SMD 0.14 lower, 95% CI 0.19 lower to 0.08 lower; 4 studies; 5356 participants, high‐quality evidence) and there was a slight reduction in the proportion with depression (RR 0.75, 95% CI 0.65 to 0.86; 3 studies, 5907 participants, high‐quality evidence).
Cognition was slightly better in the control group (MD ‐1.22, 95% CI ‐2.37 to ‐0.07; 4 studies, 5373 participants, moderate‐quality evidence).
Only one study (n = 30) reported neurological deficit score (SMD ‐0.39, 95% CI ‐1.12 to 0.33; low‐quality evidence).
SSRIs resulted in little to no difference in motor deficit (SMD 0.03, ‐0.02 to 0.08; 6 studies, 5518 participants, moderate‐quality evidence).
SSRIs slightly increased the proportion leaving the study early (RR 1.57, 95% CI 1.03 to 2.40; 6 studies, 6090 participants, high‐quality evidence).
SSRIs slightly increased the outcome of a seizure (RR 1.40, 95% CI 1.00 to 1.98; 6 studies, 6080 participants, moderate‐quality evidence) and a bone fracture (RR 2.35, 95% CI 1.62 to 3.41; 6 studies, 6080 participants, high‐quality evidence).
One study at low risk of bias across all domains reported gastrointestinal side effects (RR 1.71, 95% CI 0.33, to 8.83; 1 study, 30 participants).
There was no difference in the total number of deaths between SSRI and placebo (RR 1.01, 95% CI 0.82 to 1.24; 6 studies, 6090 participants, moderate quality evidence).
SSRIs probably result in little to no difference in fatigue (MD ‐0.06; 95% CI ‐1.24 to 1.11; 4 studies, 5524 participants, moderate‐quality of evidence), nor in quality of life (MD 0.00; 95% CI ‐0.02 to 0.02, 3 studies, 5482 participants, high‐quality evidence).
When all studies, irrespective of risk of bias, were included, SSRIs reduced disability scores but not the proportion independent.
There was insufficient data to perform a meta‐analysis of outcomes at end of follow‐up.
Several small ongoing studies are unlikely to alter conclusions.
Authors' conclusions
There is high‐quality evidence that SSRIs do not make a difference to disability or independence after stroke compared to placebo or usual care, reduced the risk of future depression, increased bone fractures and probably increased seizure risk.
Plain language summary
Selective serotonin reuptake inhibitors for stroke recovery
Review question What are the effects of selective serotonin uptake inhibitor (SSRI) drugs on recovery from stroke?
Background Stroke is a major cause of disability. Stroke‐related disability can include difficulty with daily tasks such as toileting, washing, and walking. Sometimes disability is so severe that a person becomes dependent on others for performing basic activities (this is known as 'dependence'). We previously published an update of this Cochrane Review which aimed to find out whether SSRIs (a class of drug usually used to treat mood problems, which work by changing the level of chemicals in the brain) might improve recovery after stroke.
Since the update in 2019, two large studies have now been completed and so it is necessary to perform a further update of this review. In our main analyses we included only high‐quality trials, that is those which used rigorous methods to avoid biases (such as the person assessing outcome being aware of whether the stroke survivor received the active drug or placebo). We refer to these studies as 'low risk of bias' studies.
We also wanted to find out whether SSRIs had other benefits, for example improving the severity of any arm or leg weakness, mood, anxiety, cognition, quality of life, and whether SSRIs were associated with side effects such as bleeding or seizures.
Study characteristics In total we found 76 studies recruiting 13,029 stroke survivors within one year of their stroke. There was a wide age range. About half the studies required participants to have depression to enter the trial. The duration, drug, and dose varied between studies. However, only six of these studies were at low risk of bias; the participants in these studies did not have to be depressed to enter the study, and they were all recruited soon after their stroke.
Key results When we combined data from these six studies at low risk of bias, SSRIs did not reduce disability or dependency. SSRIs reduced the risk of future depression by about a quarter, but led to a slight increase in the risk of seizures and also increased the risk of bone fractures. The evidence is current until January 2021.
Quality of the evidence We are very confident that the results are reliable for the effect on disability, dependency and bone fractures, and moderately confident about the effect on seizure risk.
Summary of findings
Summary of findings 1. Fluoxetine versus control at end of treatment, for stroke recovery, using data from high quality trials only.
| Fluoxetine versus control at end of treatment, by SSRI, for stroke recovery* | ||||||
|
Patient or population: people with stroke recovery
Settings: hospital
Intervention: fluoxetine versus control at end of treatment *Summary of findings table based on studies with low risk of bias. | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Fluoxetine versus control at end of treatment | |||||
| Disability (primary analysis) | SMD 0.0 (‐0.05, 0.05) | 5436 (5 studies) | ⊕⊕⊕⊕ High | ‐ | ||
| Independent on modified Rankin score (mRS 0 to 2) (primary analysis) | Study population | RR 0.98
(0.93 to 1.03) |
5926 (5 studies) | ⊕⊕⊕⊕ High | ‐ | |
| 1541/2971 (i.e. 52 per hundred) | 1498/2955 (i.e. 51 per hundred) |
|||||
| Neurological deficit score | SMD ‐0.39 (95% CI (‐1.12 to 0.33) | 30 participants, one study | ⊕⊕⊝⊝ Lowa |
This is a small effect (based on the 'rule‐of‐thumb' method for interpreting SMD) | ||
| Depression (continuous data) | SMD ‐0.14 (‐0.19 to ‐0.08) | 5356 (4 studies) | ⊕⊕⊕⊕ High | This is a small effect (based on the 'rule‐of‐thumb' method for interpreting SMD) | ||
| Death | Study population | RR 1.01 (0.82 to 1.24) | 6090 (6 studies) | ⊕⊕⊕⊝ Moderate | ‐ | |
| 168/3029 (i.e. 55 per thousand) | 170/3061 (i.e. 56 per thousand) |
|||||
| Number of seizures | Study population | RR 1.40 (1.00 to 1.98) | 6080 (6 studies) | ⊕⊕⊕⊝ Moderatec |
‐ | |
| 54/3024 (i.e. 18 per thousand) | 76/3056 (i.e. 25 per thousand) | |||||
| Bone fractures | Study population | RR 2.35 (1.62 to 3.41) | 6080 (6 studies) | ⊕⊕⊕ ⊕ High | ‐ | |
| 40/3024 (i.e. 13 per thousand) |
93/3056 (i.e. 30 per thousand) |
|||||
| *The basis for the assumed risk (e.g. the mean control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aNeurological deficit from only one trial of 30 people so we have downgraded for imprecision (GRADE 2013).
bDeath downgraded for imprecision.
cSeizures downgraded for imprecision.
Note that because we included only the low risk of bias studies in our review, none of the evidence was downgraded because of study quality.
A range of different outcome scales were used for disability (including Barthel Index and daily activities subscale of the Stroke Impact Scale), and depression (including emotional role function of the Stroke Impact Scale).
Background
Description of the condition
Worldwide, stroke is the second leading cause of death, the third leading cause of disability (Johnson 2016), and results in 6.5 million years being lived with disability (GBD 2015). Although major advances in the early reperfusion of ischaemic stroke have been achieved in recent years (e.g. by intravenous thrombolysis, thrombectomy), and more is known about prevention of recurrent stroke), effective, safe and widely accessible and affordable treatments that facilitate early and sustained recovery after stroke are urgently needed to further reduce the burdens of disability and dependency after stroke.
Description of the intervention
Selective serotonin reuptake inhibitors (SSRIs) are drugs that have been available for many years. There are several different SSRIs which all increase brain serotonin levels by preventing its reuptake by the presynaptic neurons. They are widely used to treat mood disorders, including those that occur after stroke, such as depression and emotional lability (i.e. emotional behaviour that is outside normal control and that occurs in situations that previously would not have provoked such behaviour) (Allida 2019). SSRIs are sometimes used to manage anxiety.
Small studies have suggested that fluoxetine, one of the SSRIs, might have a favourable effect on motor recovery after stroke (Chollet 2011; Yi 2010), even in people without mood disorders. Our 2019 Cochrane Review of SSRI for stroke recovery included 63 studies of SSRIs recruiting 9168 stroke survivors within one year of their stroke, where SSRIs were used in people with or without depression (Legg 2019). Combining the studies suggested a benefit on recovery but this benefit was not apparent when low‐quality studies were excluded from the meta‐analysis.
How the intervention might work
In animal studies, multiple potentially beneficial effects of SSRIs have been demonstrated in both normal and diseased brains. First, SSRIs have a neurotrophic effect. Neurotrophins are a family of proteins that are involved in embryogenesis (formulation of an embryo) and organogenesis (development of organs). They control neural plasticity (ability to change, or easily changed or shaped) in adults, regulate synaptic activity and neurotransmitter synthesis, and are essential for the regeneration of nerves (Lang 2004). The development of new nerve cells in adults is generally restricted to specific areas of the brain, namely the subependymal cells of the ventricular system and the subgranular zone of the dentate gyrus in the hippocampus (Ming 2005). SSRIs increase neurogenesis and expression of neurotrophic or growth factors in the adult hippocampus (Schmidt 2007), and this is likely to account for the behavioural benefits of antidepressants in animals (Santarelli 2003). Importantly, several studies have shown that migration of new neurones to damaged areas of brain may occur (Wiltrout 2007), and that neurogenesis can also occur within areas of damaged brain, for example in people with Alzheimer's disease and in animal models of Alzheimer's disease (Taupin 2006).
Second, fluoxetine may have a neuroprotective effect (i.e. protect nerve cells when the brain is damaged, e.g. by a stroke). In animals, there may be several mechanisms for neuroprotective effects of SSRIs, such as reducing inflammation (e.g. repression of microglia activation) (Lim 2009), and by enhancement of specific protein expression (hypoxia inducible factor–1 alpha, heme oxygenase‐1) (Shin 2009).
Third, SSRIs can indirectly affect an important hormonal system in the body, the adrenergic system, through up‐regulation (i.e. increase a cellular component of a cell, such as ribonucleic acid (RNA) or protein, in response to an external variable) of beta1 receptors (Pälvimäki 1994).
In healthy humans, functional magnetic resonance imaging (fMRI) studies have demonstrated that fluoxetine can modulate cerebral motor activity (Loubinoux 1999). For example, in eight chronic stroke participants in (Zittel 2008) , a single dose of citalopram 40 mg led to improvements in dexterity. A 2017 review paper discussed the hypothesis that SSRI might modulate inhibitory pathways, and that this modulation might enhances reorganisation and reestablishment of excitatory‐inhibitory control, and thus promote motor recovery after stroke (Pinto 2017).
SSRIs may also improve recovery after stroke simply through their effect on preventing or treating depression and anxiety, and through improving sleep and alertness.
Why it is important to do this review
Our 2012 Cochrane Review of SSRIs for stroke recovery showed that SSRIs appeared to reduce dependence, disability, neurological impairment, anxiety, and depression after stroke, even in participants without depression, but when we included only those studies at low risk of bias, effect sizes were much smaller (Mead 2012). The review generated the hypothesis that SSRIs might promote recovery after stroke.
SSRIs interact with platelet function and clotting, and therefore may have adverse effects in people with stroke, particularly those with haemorrhagic stroke, and these adverse effects might outweigh any potential benefits.
Three large collaborative studies (AFFINITY 2020; EFFECTS 2020; FOCUS 2019), were designed based on the results of the 2012 Cochrane Review (Mead 2012), to test the hypothesis that fluoxetine given early after stroke would improve recovery, or in other words, lead to less dependency and less disability at follow‐up. The 2019 Cochrane review Legg 2019 included the results of FOCUS 2019, which recruited over 3000 participants; in the 2019 update, meta‐analysis of the studies at low risk of bias indicated that SSRIs did not improve recovery from stroke. There were improvements in disability only when studies at high risk of bias were included.
Cochrane Reviews should be updated regularly (ideally every two years when substantial new evidence becomes available). In 2020, the results of two large studies (AFFINITY 2020; EFFECTS 2020) were published and therefore we decided to update this review.
Objectives
To determine if selective serotonin reuptake inhibitors (SSRIs) are more effective than placebo or usual care at improving outcomes in people less than 12 months post‐stroke, and to determine whether treatment with SSRIs is associated with adverse effects.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomised controlled trials (RCTs) in people with a clinical diagnosis of stroke (Hatano 1976), where an SSRI had been given within the first year of stroke onset i.e. 1) studies had to state that participants were recruited within 12 months of stroke onset, or 2) studies where the mean (or median) time since stroke was less than 12 months. Studies had to have reported at least one of our outcomes of interest in order to be included in the meta‐analysis. For those studies which did not report data in a form that we could use, we attempted to get the raw data from the authors, and if this was not possible, we retained the studies in the list of included studies, even though they could not be included in the meta‐analysis .
We included studies:
with more than two arms (e.g. SSRI versus another active treatment versus placebo). We included data from the SSRI arm and the placebo arm (or usual‐care arm if a placebo was not used), and discarded data from the other active treatment arms;
in all languages.
We excluded studies:
using a quasi‐experimental design (i.e. where investigators describe a non‐random component in the sequence generation process, such as date of admission);
using a cross‐over design.
There was no restriction on the eligibility of RCTs on the basis of sample size or duration of follow‐up.
Types of participants
We included studies that had recruited survivors of a stroke, defined as a sudden‐onset focal neurological disturbance, assumed to be vascular in origin, and lasting more than 24 hours (Hatano 1976). Studies had to recruit participants within 12 months of stroke onset, or the mean/median time since stroke had to be less than 12 months. We intended to include studies in subarachnoid haemorrhage and perform a subgroup analysis but we did not find any such studies. We intended to exclude trials of mixed populations (e.g. stroke and head injury) unless separate results for those with stroke were available, but we found no such studies.
Types of interventions
We included any drug classified as a SSRI (e.g. fluvoxamine, fluoxetine, sertraline, citalopram and paroxetine). We included any dose or mode of delivery, given for any duration and for any reason (e.g. to aid neurological recovery, to treat depression or anxiety or emotionalism, or to prevent depression or anxiety or other mood disorders). We did not include drugs that have mixed effects that include SSRI actions.
The comparator arm could include usual care or a placebo.
We excluded studies in which an SSRI was compared with another active intervention (e.g. another type of drug or herb or acupuncture). We also excluded studies that combined an SSRI with another active treatment and compared with the active treatment alone, because of the potential for interaction between the SSRI and other active treatment.
If studies had two SSRI arms, we combined these and compared with control.
Types of outcome measures
We included several outcomes.
Primary outcomes
We had two co‐primary outcomes:
independence at end of treatment. In stroke trials this is typically measured using the modified Rankin Scale (mRS), with a score of 0 to 2 conventionally considered to represent independence;
disability score at the end of treatment. Measures included, but were not limited to, Barthel index (BI) or Functional Independence Measure (FIM). If FIM or Barthel was not measured, we included an outcome reported in the trial that reported a construct as similar as possible to FIM or Barthel. For the trials which reported the Stroke Impact Scale, we used the daily activities subscale as a measure of disability.
Although disability scores and independence (or not) are arguably measuring the same concept, disability scores provide a more detailed description of functional outcome than simply using a dichotomous outcome such as independence. In other words, we were interested in performance in personal activities of daily living (ADL)/disability (measured using disability scores) and also independence in performance in personal ADL/disability measured using dichotomous outcome (independent or not).
Note that 'end of treatment' depends on the duration of treatment, and so the outcome might be measured at different time points in different studies. But we justified this approach because we were interested in whether an SSRI, given for any duration, led to better outcomes immediately after completing the course of the SSRI. However, to be included, the outcome measure had to be assessed at the same time in the control and SRRI group.
Secondary outcomes
Impairments (which can include neurological deficit scores such as the National Institute of Health Score, Motor deficit scores‐such as the Fugl‐Meyer motor score). If the total score was reported, and also motor deficit alone, we performed two separate meta‐analyses. For the trials which reported Stroke Impact Scale, we elected to use the self‐reported 'strength' domain for motor deficit.
Depression. We accepted any depression score. We did not decide which score to prioritise as we anticipated that trials would use only one depression score. W e included both continuous and dichotomous scores and analysed these separately.
Anxiety. We intended to accept any anxiety score. We intended to include both continuous and dichotomous scores and analyse these separately.
Quality of life. We accepted any score.
Fatigue. This could include any fatigue score, or the vitality component of the SF‐36 ( Short Form Survey).
Healthcare cost.
Death
Adverse events including gastrointestinal (GI) side effects, bleeding, seizures, and any other side effect. For this update, there were sufficient data on fractures to include this as an additional analysis, and so we included this as an additional Forest plot.
Cognition‐this could include self report or directly measured cognition. We would have prioritised directly measured cognition if these data had been available. In the previous update no trials reported this‐but the new trials included in this update did include cognition.
Leaving the trial early (for reasons other than death).
We anticipated that most studies would assess these at the end of treatment and possibly at one or more time points. We did not stipulate a minimum follow‐up time. We did not stipulate in advance precisely how multiple time points would be handled (if they had been found).
In the previous update we stated that we would also analyse change in depression scores over time. For this update, we made the decision just to analyse depression score at the end of the studies, as change in scores were not reported by the new included trials.
Search methods for identification of studies
See the methods for the Cochrane Stroke Group Specialised register. We searched for studies in all languages and arranged for the translation of trials where necessary.
Electronic searches
We developed the MEDLINE search strategy with the help of the Cochrane Stroke Group Information Specialist and adapted it for the other databases.
We searched the following electronic bibliographic databases.
Cochrane Stroke Group Trials Register (7 January 2021)
Cochrane Central Register of Controlled Trials (CENTRAL; 2021, Issue 1) in the Cochrane Library (searched 7 January 2021) (Appendix 1)
MEDLINE (from 1948 to 7 January 2021) (Appendix 2)
Embase Ovid (from 1980 to 7 January 2021) (Appendix 3)
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature ; 1982 to 7 January 2021) (Appendix 4)
AMED Ovid (Allied and Complementary Medicine) (from 1985 to 7 January 2021) (Appendix 5)
PsycINFO Ovid (from 1967 to 7 January 2021) (Appendix 6)
PsycBITE Psychological Database for Brain Impairment Treatment Efficacy (www.psycbite.com/) (16 July 2018)
In addition, we searched the following ongoing trials registers (Appendix 7).
Stroke Trials Registry (www.strokecenter.org/trials) (26 June 2018)
US National Institutes of Health ongoing Trials Register ClinicalTrials.gov (www.ClinicalTrials.gov) (7 January 2021)
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (apps.who.int/trialsearch/) (7 September 2020)
Evidence for this update included search results from the previous version of this review), combined with results from the above searches. In Mead 2012 there had been no date limits and searches had been applied from inception of databases.
Following editorial review, one review author (GM) searched the WHO ICTRP using the term 'stroke' on 8 August 2021 to identify any new trials registered after 7 July 2020 i.e. > 1 year since last search.
Searching other resources
In an effort to identify further published, unpublished and ongoing studies, we:
searched reference lists of included trials and relevant reviews when full texts were retrieved for detailed scrutiny;
contacted researchers in the field.
Data collection and analysis
Selection of studies
Joshua Cheyne (Cochrane Stroke Group Information Specialist), ran the searches of CENTRAL, MEDLINE, Embase, CINAHL, AMED, and PsycINFO, and downloaded the resulting references into Reference Manager. These were imported into Covidence, which automatically removed some, but not all, of the duplicates.
Any two review authors (from GM, EL, LAL, MK, SW, RT, A‐SR, LL,C‐FH, MH or XH) independently scrutinised the resulting titles and abstracts and excluded obviously irrelevant reports and duplicates. We obtained full texts of potentially eligible studies. Any two review authors (from GM, AB, EL, LAL, MK, SW, RT, A‐SR, LL C‐FH or XH) independently applied inclusion and exclusion criteria; if there was lack of consensus, a third review author (usually GM unless she had already scrutinised the paper) also applied inclusion and exclusion criteria.
We include a flow diagram that includes the number of unique references identified by the searches, the number of records excluded after preliminary screening of titles and abstracts, the number of records retrieved in full text, and the number of studies fulfilling our inclusion criteria (Figure 1).
1.
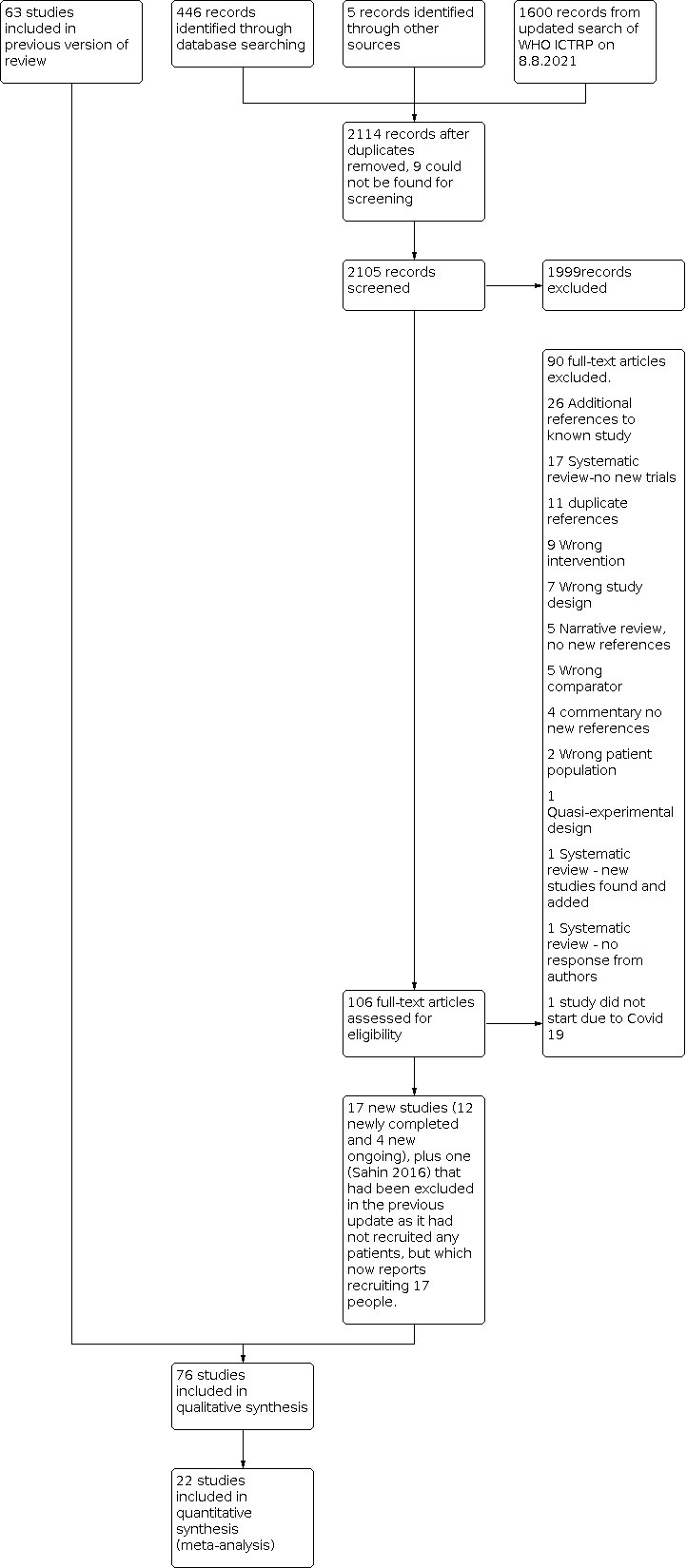
PRISMA flow diagram for this update
Data extraction and management
For the new eligible studies that we had identified, any two review authors (from GM, EL, LAL, MK, MH, SW, RT, LL, A‐SR, LL, C‐FH or XH) independently extracted data from each new study.
We extracted the following data:
the report: author, year and source of publication;
the study: sample characteristics, social demography;
the participants: stroke sequence (first‐ever versus recurrent), social situation, time since stroke onset, prior history of psychiatric illness, current neurological status, stroke severity, whether people with aphasia were recruited, the proportion with depression at baseline (if recorded by trialists), we did not extract information on location or size of lesion as this was unlikely to have been recorded by the trialists, and brain imaging often does not show a visible infarct in people with minor strokes;
the research design and features: adherence, non‐response and length of follow‐up;
the intervention: type, duration, dose, timing and mode of delivery;
the effect size: sample size, nature of outcome, estimate and standard deviation (SD) (or standard error (SE));
source of funding.
Methods in previous versions were broadly similar and are fully reported in previous versions (Legg 2019; Mead 2012)
Assessment of risk of bias in included studies
We assessed risks of bias using the Cochrane 'Risk of bias' tool (Higgins 2017). We assessed the methods used in each study to control for the following potential sources of bias: sequence generation (selection bias); allocation concealment (selection bias); blinding of participants, personnel and outcome assessors (performance and detection bias); incomplete outcome data (attrition bias); selective outcome reporting (reporting bias); and other potential threats to validity.
Where there was a disagreement between the two review authors on risk of bias, a third review author (LAL, GM) reviewed the data and reached a consensus in discussion with the first two review authors.
For incomplete outcome data, we categorised as 'low risk' if missing data were imputed using appropriate methods or if missing outcome data overall were less than 5%. For this update, we decided to categorise studies as low risk of bias if more than 5% of data were missing providing the number of participants with missing data was balanced between groups and the reasons for missing data were unrelated to treatment allocation.
We extracted data on source of funding, and listed this under 'Other sources of bias'. If the source of funding was not given, or if there were links with the pharmaceutical industry and no explicit statement that the funder had no input into the design or analysis of the study, we classified this as 'unclear risk'. We also recorded any other potential threats to validity.
We also extracted data on how adverse effects were reported, and listed these in the descriptions of the studies.
If a study author was also one of the review authors, a review author who was not involved in the study extracted data and assessed quality.
For this 2021 update, we contacted study authors to obtain more information to enable us to make judgements about risk of bias if this was unclear from the paper, AND if this was going to influence whether a study was categorised as low risk of bias across all seven domains i.e. changing a judgement of 'uncertain' to 'low risk' of bias.
Measures of treatment effect
For dichotomous data, we reported risk ratios (RRs). For ordinal scales, where there was a well‐recognised cut‐point in the scale (e.g. mRS) we analysed the data as a dichotomous outcome (dependent or independent).
For ordinal scales with no recognised cut‐point, we analysed the data as continuous data. The data required for meta‐analyses of continuous data in Review Manager 5 are means and standard deviations (SDs) (Review Manager 2014). When extracting continuous data from the study reports, we checked whether trials reported the SD or the standard error (SE). We had planned to use the SE or 95% confidence interval (CI) to compute the SD when SDs were missing, but this was not needed as all the trials reported SDs.
For ordinal scales and continuous data, we calculated standardised mean differences (SMDs), because different scales were used for the same outcomes (e.g. Barthel Index (BI) and Funtional Independence Measure (FIM) for disability score, the Beck Depression Inventory (BDI) or the Hamilton Rating Scale for Depression (HAMD) for depression). The SMD does not correct for differences in the direction of the scale. Some scales increase with disease severity and others decrease, so we multiplied the mean value from one set of trials by −1. For example, in the National Institute of Health Stroke Scale (NIHSS), a low score indicates a less severe stroke, whilst a low score in the Scandinavian Stroke Scale (SSS) indicates a more severe stroke.
If there was more than one outcome measure in the same domain (e.g. two different depression scales), we made a post‐hoc decision to select the one with the most complete data.
Unit of analysis issues
The number of observations in the analysis should match the number of 'units' that were randomised. We considered outcomes measured at the end of treatment and at the end of follow‐up in separate analyses. For side effects, we considered the number of participants developing a specified side effect rather than the total number of side effects in each group.
Dealing with missing data
For this update, we contacted authors of new trials to obtain any data that we needed for our meta‐analysis that had not been included in a published full‐text article or an abstract.
Note that for some analyses, the sample size is slightly different for different outcomes, this is because of the missing responses for some outcomes.
Assessment of heterogeneity
We assessed whether there was evidence of inconsistency in our results by considering possible clinical, methodological, and statistical heterogeneity. We assessed clinical and methodological heterogeneity by comparing similarities in our included studies between study designs, participants, interventions, and outcomes.
We quantified the effect of heterogeneity using the I2 statistic. We assessed statistical heterogeneity by visually examining forest plots. Thresholds for the interpretation of the I2 statistic can be misleading, since the importance of inconsistency depends on several factors. A rough guide to interpretation in the context of meta‐analyses of randomised trials is as follows: (Section 9.5.2; Deeks 2021):
0% to 40% is not considered important;
30% to 60% suggests moderate heterogeneity;
50% to 90% suggests substantial heterogeneity;
75% to 100% is considerable heterogeneity.
Assessment of reporting biases
We searched clinical trials registers to identify published protocols for each of our included studies. We checked for selective reporting of results by comparing the published protocol with the published full‐text article and by scrutinising the aims and methods of the trials and comparing these with outcomes reported. We found several papers by the same authors, and contacted the authors to check whether the publications were duplicates or to check if the included study populations were unique. If it was not possible to determine whether different publications reported overlapping groups of participants, we included just one of the papers and listed the others as awaiting assessment.
If we had identified a sufficient number of included studies at low risk of bias (i.e. more than 10 studies (Sterne 2017), we would have generated a funnel plot of low risk of bias studies, to assess risk of publication bias, an asymmetrical funnel plot might have suggested publication of only positive results (Egger 1997). We made a post‐hoc decision to perform a funnel plot for all studies, irrespective of risk of bias, for the co‐primary outcome of disability.
We deployed a comprehensive search strategy in an effort to avoid reporting biases in our review methodology. See Search methods for identification of studies.
We tried to avoid language bias by including all trials, irrespective of language: we sought translation where needed.
Data synthesis
We completed meta‐analysis of outcomes for which we had comparable effect measures from more than one study, and when measures of heterogeneity indicated that pooling of results was appropriate. We used the statistical calculator provided in Review Manager 5 to perform meta‐analysis (Review Manager 2014).
We used a fixed‐effect model (Mantel 1959), rather than a random‐effects model because of the dominance of the three largest trials (AFFINITY 2020, EFFECTS 2020; FOCUS 2019); random effects would have given too much weight to the smaller trials. The dominance of the three large trials makes a fixed‐effect model a more reliable indicator of the effect than the average across the smaller trials. We assessed the robustness of the results to choice of model using a sensitivity analysis for our primary outcomes.
In the initial 2012 review, we had performed multiple meta‐analyses of all the primary and secondary outcomes, included all trials irrespective of risk of bias, and then explored the influence of each aspect of bias on estimates of effects in a series of sensitivity analyses.
In the 2019 review we limited our analyses of all outcome measures to studies at low risk of bias (Higgins 2017), as we wanted reliable data, not confounded by bias, to find out whether SSRIs were more effective than placebo or usual care at improving a range of important outcomes. Also, had we included all studies, irrespective or risk of bias, for all available outcomes, the number of analyses would have become unmanageable within the resources we had. However, in the 2019 review, we performed a sensitivity analysis by using data on our two primary outcomes (disability and independence) from all trials, irrespective of risk of bias. For this current update, we use the same approach.
We reached decisions on overall risk of bias by study by consideration of six risk of bias domains: sequence generation, allocation concealment, blinding of participants and trial personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and other risk of bias. We required a study to have a judgement of low risk of bias in all domains in order to categorise it as having an overall low risk of bias.
Subgroup analysis and investigation of heterogeneity
If there had been at least two studies at low risk of bias across all six domains of risk of bias, we would have explored variability in the participants, interventions, and outcomes among studies using the following subgroups.
Type of SSRI.
Studies with depression at baseline as an inclusion criterion and those where depression was not an inclusion criterion.
Time since stroke at recruitment. We categorised these as less than three months (0 ‐ 90 days), three to six months (91 to 108 days), six to nine months (181 to 271 days) or nine to 12 months (272 to 365 days).
Finding high statistical heterogeneity (I2 > 50%) would not have prevented us from performing a subgroup analysis, rather we would have considered the reason for this heterogeneity.
We did not perform subgroup analyses by type of SSRI or time since stroke as all studies included in the main analyses were similar with regard to these characteristics.
Sensitivity analysis
We explored the potential effects of decisions made as part of the review process as follows.
We included all studies regardless of risk of bias judgement for our primary outcomes of disability score and independence.
We conducted meta‐analysis using the alternate meta‐analytical effects model (fixed‐effect or random‐effects) for just those studies at low risk of bias across all six domains.
We intended to conduct a meta‐analysis using the alternate 'last available follow‐up' time point if studies had reported more than one follow‐up after the end of treatment, but none of the included studies did this.
We compared effect estimates from the above results with effect estimates from the main analysis. We reported differences that altered the interpretation of effects.
Summary of findings and assessment of the quality of the evidence
We created a summary of findings table using the following outcomes: disability; dependent according to the mRS; neurological deficit score; depression (continuous data); death; seizures; and gastrointestinal side effects (Table 1). We chose these outcomes as they are of high clinical relevance. We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence as it relates to the studies that contribute data to the meta‐analyses for the prespecified outcomes (Atkins 2004). We used methods and recommendations described in Chapter 11 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2017), using GRADEproGDT software (GRADEproGDT 2015). We justified all decisions to downgrade the quality of studies using footnotes, and made comments to aid the reader's understanding of the review where necessary.
Summary of findings and assessment of the certainty of the evidence
We created a 'Summary of findings' table using the following outcomes: disability; dependent according to the mRS; neurological deficit score; depression (continuous data); death; seizures; and gastrointestinal side effects (Table 1). We chose these outcomes as they are of high clinical relevance. We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence as it relates to the studies that contribute data to the meta‐analyses for the prespecified outcomes (Atkins 2004). We used methods and recommendations described in Chapter 11 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2017), using GRADEproGDT software (GRADEproGDT 2015). We justified all decisions to downgrade the quality of studies using footnotes, and made comments to aid the reader's understanding of the review where necessary.
Results
Description of studies
For substantive descriptions of studies see: Characteristics of included studies, Characteristics of excluded studies, Studies awaiting classification, and Characteristics of ongoing studies.
Results of the search
For this update, we screened 221 references from database searches and accessed the available full‐text reports for 10 6 studies. This included a systematic review from which we identified five new studies from China (Chen 2015; Hu 2018; Li 2007; Li 2017; Wang 2009).
As a final check for new studies, WHO ICTRP was searched by one review author (GM) on 8 August 2021 and 1600 citations screened.
The flow diagram is shown in Figure 1. This includes the results of the August 2021 search of the WHO ICTRP.
The 2019 version of this review (Legg 2019), identified 63 completed studies recruiting 9168 stroke survivors within one year of their stroke; and 16 ongoing studies (AFFINITY 2020; Asadollahi 2018; Bembenek 2020; Dike 2019; EFFECTS 2020; EudraCT 2005‐005266‐37; Bonin Pinto 2019 ; IRCT201112228490N1; IRCT2012101011062N1; IRCT2017041720258N37; NCT02386475; NCT02737930; NCT02767999; NCT02865642; NCT03448159; NCT03826875).
Of these 16 previously ongoing studies, six have now been published (AFFINITY 2020; Asadollahi 2018; Bembenek 2020; Dike 2019; EFFECTS 2020; Bonin Pinto 2019); we excluded one of these at it recruited patients within two years (not one year) of stroke (Bonin Pinto 2019). One trial which we had previously listed as 'excluded' has been moved to our list of included studies; this study recruited only 17 patients and was terminated due to slow recruitment and lack of funding to expand to other sites (NCT02737930).
Based on information provided in trials registers: we found the following.
Five of these previously ongoing studies are still ongoing: EudraCT 2005‐005266‐37, NCT02767999, NCT02865642, NCT03448159, NCT03826875.
There are no results for IRCT201112228490N1; the authors were contacted on 20 April 2021 but no response was received; this trial is also listed as ongoing.
Three studies are completed but the results are not yet available; these are still listed as ongoing (IRCT2012101011062N1; IRCT2017041720258N37; NCT02386475).
Our January 2021 searches identified two new completed studies (Cao 2020; Gong 2020) and three new ongoing studies (ChiCTR1800019467; CTRI/2018/12/016568; TCTR20181216001). An additional study identified in the January 2021 searches did not start due to the COVID 19 pandemic (ACTRN12619000573156).
The flow of search results for the previous version of the review are reported in Legg 2019. We report details of the search for this update in a PRISMA flow chart (Figure 1). This includes our additional searches of WHO ICTRP on 8 August 2021, to identify any new ongoing studies, where we used the broad search term 'STROKE' which identified 1600 records, of which two records which were scrutinised in detail; one of these is now included as an ongoing study (IRCT20210307050617N1).
Included studies
In the previous version of the review (Legg 2019), there were 63 included studies recruiting a total of 9168 randomised participants. One study had previously been included in the list of excluded studies, but for this review we included it in our list of included studies as it now reports having recruited 17 participants although the results are not available (NCT02737930).
For the current 2021 update, we identified a further 12 completed studies providing data for meta‐analysis and recruiting a total of 3845 more participants (AFFINITY 2020; Asadollahi 2018; Bembenek 2020; Cao 2020; Chen 2015; Dike 2019; EFFECTS 2020; Gong 2020; Hu 2018; Li 2007; Li 2017; Wang 2009). Five of these studies (Chen 2015; Hu 2018; Li 2007; Li 2017; Wang 2009), were identified from the reference list of a 2020 systematic review (Li 2020). For Cao 2020, there are two reports (one reporting 97 participants and the other reporting 100 participants, with overlapping periods for recruitment, almost identical stroke subtypes in the control and citalopram groups, the same funding source, and identical text in some sections of the papers); the author did not respond to our request for clarification, and the editors of the journals in which they were published also did not receive a response from the authors, so to avoid the possibility of double‐counting the same participants, we included just one paper reporting 100 participants.
Overall, we now have a total of 76 included studies recruiting 13,029 participants (Figure 1). Of these, 22 contributed to the quantitative syntheses; the remaining studies were not of sufficiently high quality to be included in the main analyses, or did not report our co‐primary outcomes of disability, or independence, or did not report any results .
Of the 76 included studies:
38 studies used fluoxetine (AFFINITY 2020; Bembenek 2020; Birchenall 2019; Brown 1998; Chen 2001; Cheng 2003; Chollet 2011; Dam 1996; Dike 2019; EFFECTS 2020; Feng 2004; FOCUS 2019; Fruehwald 2003; Gong 2020; He 2004; He 2016; Hu 2002; Huang 2002; Kong 2007; Li 2004a; Li 2004b; Li 2008; Marquez Romero 2013; NCT01674868; NCT02737930; Pariente 2001; Razazian 2014; Restifo 2001; Robinson 2000a; Robinson 2000b; Shah 2016; Song 2006; Wang 2003; Wen 2006; Wiart 2000; Xu 2001; Zhao 2011; Zhou 2008);
eight studies used sertraline (Almeida 2006; Burns 1999; Guo 2009; Meara 1998; Murray 2005; NCT00177424; Rasmussen 2003; Xie 2005);
13 studies used paroxetine (Chen 2002; Chen 2005b; GlaxoSmithKline 1998; He 2005; Lai 2006; Li 2005; Li 2007; Pan 2018; Wang 2009; Xu 2006; Yang 2002; Yang 2011; Ye 2004);
nine studies used citalopram (Acler 2009; Andersen 1994; Andersen 2013; Chen 2015; Gao 2017; Li 2006; Liu 2006; Miao 2004; Savadi Oskouie 2012)
five studies used escitalopram (Cao 2020; Hu 2018; Kim 2017; Li 2017; Robinson 2008);
one study used either sertraline or fluoxetine (Jia 2005);
two studies used citalopram or fluoxetine (Chen 2005a; Asadollahi 2018).
Baseline sociodemographic and clinical characteristics
The mean age of participants ranged from 51 ± 7 years (Song 2006), to 75.6 years (Wang 2003), with most studies recruiting participants in their 60s. There are more men than women. Patients with ischaemic stroke and/or primary intracerebral haemorrhage were included.
Mean time since stroke
Of the 76 included studies: (numbers below add up to 76 not 75).
Forty‐four studies report recruiting participants between 0 and 90 days after stroke onset (AFFINITY 2020; Acler 2009; Almeida 2006; Andersen 1994; Andersen 2013; Bembenek 2020; Birchenall 2019; Chen 2001; Chen 2005b; Cheng 2003; Chollet 2011; Dike 2019; EFFECTS 2020; Feng 2004; FOCUS 2019; Fruehwald 2003; Gao 2017; Gong 2020; He 2004; He 2016; Hu 2002; Huang 2002; Asadollahi 2018; Kim 2017; Kong 2007; Li 2004a; Li 2004b; Li 2008; Marquez Romero 2013; Pan 2018; Rasmussen 2003; Robinson 2008; Savadi Oskouie 2012; Shah 2016; Song 2006; Wen 2006; Wiart 2000; Xie 2005; Xu 2001; Xu 2006; Yang 2011; Ye 2004; Zhao 2011; Zhou 2008).
Five studies described participants as having an 'acute stroke'; so we have included these in the zero‐to‐three‐month group (Cao 2020; He 2005; Lai 2006; Li 2006; NCT02737930).
Two further studies reported that the mean time since stroke was between five and 16 weeks, so we included these in the zero‐to three‐month group (Robinson 2000a; Robinson 2000b).
One study, which did not recruit any participants, had an inclusion criterion of less than 15 days before stroke (NCT01674868).
Four studies report recruiting participants three to six months (91 to 108 days) after stroke onset: Dam 1996 (described as participants being one to six months), Miao 2004, Murray 2005, and Yang 2002 ('recovery phase of stroke' two to six months).
Two studies report recruiting participants at six to nine months (181 to 271 days) after stroke onset (Guo 2009; Li 2006).
No study reported recruiting participants between nine and 12 months after stroke.
One study reported the experimental and control group being median 10.5 months and 5.5 months after stroke, respectively (Burns 1999).
Seventeen studies did not report the precise time (Brown 1998; Chen 2002; Chen 2005a; Chen 2015; GlaxoSmithKline 1998; Hu 2018; Jia 2005; Li 2005; Li 2007; Li 2017; Meara 1998; NCT00177424; Pariente 2001; Razazian 2014; Restifo 2001; Wang 2003; Wang 2009).
Depression as an inclusion criterion
Thirty‐seven studies included participants affected by depression (i.e. depression used as an inclusion criterion) (Andersen 1994; Chen 2001; Chen 2002; Chen 2005a; Chen 2005b; Chen 2015; Cheng 2003; Feng 2004; Fruehwald 2003; GlaxoSmithKline 1998; Guo 2009; He 2005; Hu 2002; Hu 2018; Huang 2002; Jia 2005; Lai 2006; Li 2004a; Li 2004b; Li 2005; Li 2006; Li 2008; Li 2017; Liu 2006; Meara 1998; Miao 2004; Murray 2005; Robinson 2000a; Song 2006; Wang 2003; Wang 2009; Wiart 2000; Xie 2005; Xu 2001; Yang 2002; Yang 2011; Ye 2004).
Thirty‐nine studies did not use depression as an inclusion criterion (Acler 2009; AFFINITY 2020; Almeida 2006; Andersen 2013; Bembenek 2020; Birchenall 2019; Brown 1998; Burns 1999; Cao 2020; Chollet 2011; Dam 1996; Dike 2019; EFFECTS 2020; FOCUS 2019; Gao 2017; Gong 2020; He 2004; He 2016; Asadollahi 2018; Kim 2017; Kong 2007; Li 2007; Marquez Romero 2013; NCT00177424; NCT01674868; NCT02737930; Pan 2018; Pariente 2001; Rasmussen 2003; Razazian 2014; Restifo 2001; Robinson 2000b; Robinson 2008; Savadi Oskouie 2012; Shah 2016; Wen 2006; Xu 2006; Zhao 2011; Zhou 2008).
The criteria for diagnosing depression varied between studies.
Excluded studies
Our table of excluded studies is as brief as possible and does not list studies that obviously do not fulfil the inclusion criteria. There are a total of 28 excluded studies.
We describe a total of 28 studies in our table of excluded studies (ACTRN12619000573156; Andersen 1993; Andersen 2012; Anderson 2002; Anonymous 2012a; Anonymous 2012b; Berends 2009; Chen 2019; Choi Kwon 2008; Finkenzeller 2009; Foster 2019; Bonin Pinto 2019; Gourab 2015; Graffagnino 2002; Ji 2000; Kitago 2020; Li 2002; Liang 2003; Liu 2004; Liu 2020; Mosarrezaii 2018; NCT01963832; Robinson 2011; Sitzer 2002; Sun 2015; Vogel 2020; Xu 2007; Zhou 2003). Eight of these studies were excluded during this update (ACTRN12619000573156; Chen 2019; Foster 2019; Bonin Pinto 2019; Kitago 2020; Liu 2020; Mosarrezaii 2018; Vogel 2020).
Ongoing studies
The following studies are either ongoing or are completed but have not yet published results (ChiCTR1800019467; CTRI/2018/12/016568; EudraCT 2005‐005266‐37; IRCT201112228490N1; IRCT2012101011062N1; IRCT2017041720258N37; IRCT20210307050617N1; NCT02386475; NCT02767999; NCT02865642; NCT03448159; NCT03826875; TCTR20181216001). See Characteristics of ongoing studies.
Studies awaiting classification
The same studies that were listed as 'awaiting classification' in the previous version of the review of Legg 2019 continue to be listed as 'awaiting classification' as no new information is available to change these classification (Guo 2016; He 2018; Jurcau 2016; NCT00967408). See Characteristics of studies awaiting classification.
Risk of bias in included studies
All 76 studies were randomised controlled trials (RCTs). We could not assess risk of bias in one study as there are no published data, just information on a trials register (NCT02737930). Thirty‐two studies were at low risk of bias for random sequence generation and 44 at unclear risk. See Figure 2 and Figure 3.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.

'Risk of bias' graph: review authors' judgements about each 'risk of bias' item presented as percentages across all included studies.
Allocation
For allocation concealment, we assessed 21 studies to be at low risk of bias and 55 studies to be at unclear risk. Figure 2 and Figure 3 demonstrate selection bias.
Blinding
For performance bias, we assessed 26 studies to be at low risk of bias, 23 studies to be at unclear risk of bias, and 26 studies to be at high risk of bias for blinding of participants.
For blinding of outcome we assessed 25 studies to be a low risk of bias, 48 studies to be at unclear risk of bias, and two studies to be at high risk of bias. Figure 2 and Figure 3 demonstrate blinding.
Incomplete outcome data
For incomplete outcome data we assessed 28 studies to be at low risk of bias, 20 studies to be at unclear risk of bias, and 27 studies to be at high risk of bias. Figure 2 and Figure 3 demonstrate attrition bias.
Selective reporting
We assessed 20 studies to be at low risk of bias, 46 studies to be at unclear risk of bias, and nine studies to be a high risk of bias for selective outcome reporting. Figure 2 and Figure 3 demonstrate reporting bias.
Other potential sources of bias
Other sources of bias
These are shown in the final column of Figure 2 and Figure 3. There were 23 studies at low risk of bias, seven at high risk, and the rest were at unclear risk.
Low risk of bias across all domains
Six trials were at low risk of bias across all domains (AFFINITY 2020; Asadollahi 2018; Bembenek 2020; EFFECTS 2020; FOCUS 2019; Marquez Romero 2013) (Figure 2; Figure 3). For two of these trials, the final judgement was made after obtaining further information from the trialists (Asadollahi 2018; Bembenek 2020).
Following editorial review, one trial that had been included as low risk of bias across all domains in the previous review was re‐categorised as unclear risk of bias for 'other sources of bias' as there were baseline differences in motor scores (Chollet 2011).
Publication bias
We performed a funnel plot for the outcome of disability, for all trials irrespective of risk of bias (Figure 4). This suggests publication bias, with a cluster of studies in the upper left portion of the graph.
4.

Funnel plot, all studies irrespective or risk of bias, for disability at end of treatment.
Effects of interventions
See: Table 1
Primary outcomes (low risk of bias trials only)
Disability score at the end of treatment
Of the six studies at low risk of bias in all seven domains, two reported Barthel score as median and interquartile range (QR) (Bembenek 2020; Marquez Romero 2013). For one study (Marquez Romero 2013), we converted the median Barthel score and IQR to mean and standard deviation (SD) using a method described in Wan 2014.
For Bembenek 2020, AFFINITY 2020, EFFECTS 2020, and FOCUS 2019 the authors supplied the mean and SD of the activities of daily living score (five questions about activities done during a typical day) of the Stroke Impact Scale.
One did not report disability or independence and so is not included in the analyses of disability and independence (Asadollahi 2018).
There was no difference in measures of disability between selective serotonin reuptake inhibitors (SSRIs) and placebo (Analysis 1.1): the standard mean difference (SMD) with a fixed‐effect model (SMD −0.00, 95% CI −0.05 to 0.05; P = 0.98; 5 studies, 5436 participants; high‐quality evidence) with no heterogeneity (I2 = 0%).
1.1. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 1: Disability (primary outcome). Studies at low risk of bias
Independent on modified Rankin score (mRS 0 to 2) at the end of treatment
We combined data from the five studies at low risk of bias across all seven domains for the outcome of independent on mRS 0 to 2 using a risk ratio with a fixed‐effect model (RR 0.98, 95% CI 0.93 to 1.03; P = 0.37; 5 studies, 5926 participants, high‐quality evidence). The I2 was 32%, moderate heterogeneity (Analysis 1.2).
1.2. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 2: Independent on modified Rankin score (mRS 0 to 2) (primary outcome). Studies at low risk of bias
Secondary outcomes (low risk of bias trials only)
Impairments: neurological deficit score at the end of treatment
One study (30 participants) of high quality reported neurological deficit scores. The study authors reported no difference in neurological score for participants who received and SSRI compared with those who received a placebo (Analysis 1.3).
1.3. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 3: Neurological deficit score (studies at low risk of bias)
Impairments: motor deficits at end of treatment
We combined data for the six low risk of bias studies that reported motor deficits, using the SMD with a fixed‐effect model. The analysis found no difference between SSRI and placebo (SMD 0.03, 95% CI −0.02 to 0.08; P = 0.23; 6 studies, 5518 participants, I2 = 75%, substantial heterogeneity, moderate‐quality evidence) (Analysis 1.4).
1.4. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 4: Motor deficits (studies at low risk of bias)
We downgraded the evidence to 'moderate' as the data from several trials were by self‐report rather than by an objective assessment of deficits. Note that data from Marquez Romero 2013 are means and SDs estimated from reported medians and interquartile ranges using a method described in Wan 2014.
Depression severity at end of treatment (continuous data)
We combined data from the four studies with an overall low risk of bias for the outcome of depression severity using the SMD with a fixed‐effect model (SMD −0.14, 95% CI −0.19 to −0.08; P < 0.01; 4 studies, 5356 participants; high‐quality evidence). Participants who received fluoxetine had significantly lower end‐of‐treatment scores on measures of depression than those participants receiving placebo (Analysis 1.5) with moderate heterogeneity (I2 = 36%, P < 0.01).
1.5. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 5: Depression, continuous data (studies at low risk of bias)
Depression at the end of treatment (dichotomous data)
Data were available for three studies at low risk of bias (Analysis 1.6). Risk of depression was lower in the SSRI group (RR 0.75, 95% CI 0.65 to 0.86; 3 studies, 5907 participants, P < 0.01 ), with no important heterogeneity (I2 = 0%). This was assessed as high‐quality evidence.
1.6. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 6: Depression, dichotomous data (studies at low risk of bias)
Anxiety severity at end of treatment (continuous data)
No studies at low risk of bias reported measures of anxiety.
Anxiety severity at end of treatment (dichotomous data)
No studies at low risk of bias reported number of diagnoses of anxiety.
Death at end of treatment
We combined data for the six studies with an overall low risk of bias for the outcome of death, using a risk ratio with a fixed‐effect model. The analysis found no difference in the total number of deaths between SSRI and placebo (RR 1.01, 95% CI 0.82 to 1.24; P = 0.98; 6 studies, 6090 participants, moderate quality evidence), with no evidence of heterogeneity (I2 = 0%) (Analysis 1.7).
1.7. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 7: Death (trials at low risk of bias)
Side effects: seizures at end of treatment
We combined data for the six studies with an overall low risk of bias for the outcome of seizures, using a risk ratio with a fixed‐effect model. The analysis showed more patients had seizures in the SSRI than control group (RR 1.40, 95% CI 1.00 to 1.98; P = 0.05; 6 studies, 6080 participants, moderate‐quality evidence because wide confidence intervals), with moderate heterogeneity (I2 = 45%) (Analysis 1.8).
1.8. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 8: Seizures (studies at low risk of bias)
Gastrointestinal side effects at end of treatment
One study (30 participants) of high quality reported 'gastrointestinal side effects' at the end of treatment. The study authors reported no difference in 'gastrointestinal side effects' for participants who received and SSRI compared with those who received a placebo (Analysis 1.9).
1.9. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 9: Gastrointestinal side effects (studies at low risk of bias)
Side effects: bleeding at end of treatment
We combined data from the six studies at low risk of bias using a risk ratio with fixed‐effects model (Analysis 1.10). The risk ratio was 1.08 (95% CI 0.69 to 1.70; P = 0.73, 6 trials, 6088 participants, high‐quality evidence). There was no important heterogeneity I2 = 0%).
1.10. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 10: Bleeding (studies at low risk of bias)
Side effects: fractures at end of treatment
We combined data from the six studies at low risk of bias. SSRIs were associated with higher risk of fractures (RR 2.35, 95% 1.62 to 3.41, 6 studies, 6080 participants, high‐quality evidence, P < 0.01, I2 = 0%, no important heterogeneity) (Analysis 1.11).
1.11. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 11: Fractures (studies at low risk of only)
Cognition at end of treatment (continuous data)
Of the six studies at low risk of bias, four studies reported the memory domain of the Stroke Impact Scale (AFFINITY 2020; Bembenek 2020; EFFECTS 2020; FOCUS 2019). MD was ‐1.22 (95% CI ‐2.37 to ‐0.07) in favour of control, 4 trials, 5373 participants, I2 72%, P = 0.04 (Analysis 1.12). There was substantial heterogeneity. We downgraded to moderate‐quality evidence because the cognition outcomes were self‐reported, not directly measured. Note that the size of the mean difference between treatment and placebo is very small.
1.12. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 12: Cognition (trials at low risk of bias)
Leaving the study early (before the end of scheduled follow‐up) for reasons other than death
We combined data for studies with an overall low risk of bias for the outcome of leaving the study before the end of scheduled follow‐up, using a risk ratio with a fixed‐effect model. The analysis suggested a slight excess of people leaving early in the SSRI group with no evidence of heterogeneity (RR 1.57, 95% CI 1.03 to 2.40, P = 0. 04, 6 studies, 6090 participants; I2 = 0%, no important heterogeneity, high‐quality evidence) (Analysis 1.13).
1.13. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 13: Leaving the study before the end of scheduled follow‐up for reasons other than death (trials at low risk of bias)
Fatigue
Four trials reported SF36 Vitality score as a measure of fatigue (AFFINITY 2020; EFFECTS 2020; Bembenek 2020; FOCUS 2019). The mean difference between groups was ‐0.06 (95% CI ‐1.24 to 1.11; 5524 participants, P = 0.92, I2 = 0, no important heterogeneity, moderate‐quality evidence). We downgraded quality because of wide confidence intervals (Analysis 1.14).
1.14. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 14: Fatigue at end of treatment (studies at low risk of bias only)
Quality of life
Three trials used EQ5 5DL and reported mean and standard deviation in each group which enabled us to perform a meta‐analysis. (FOCUS 2019; AFFINITY 2020; EFFECTS 2020 ). The mean difference between groups was ‐0.00 (95% CI ‐0.02 to 0.02), 5482 participants, P = 0. 93 ; I2 = 0, no important heterogeneity, high ‐ quality of evidence) (Analysis 1.15).
1.15. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 15: Quality of life at end of treatment (studies at low risk of bias)
Healthcare costs
No trial reported healthcare costs.
Outcomes at the end of follow‐up
We repeated the analyses above for all outcomes reported at the end of follow‐up for the studies at low risk of bias across all domains. Four studies collected data on outcomes 12 months after completing the intervention and so we selected this time point for our analyses (AFFINITY 2020; Bembenek 2020; EFFECTS 2020; FOCUS 2019). Two studies have not yet published their 12‐month data and so are not included in this meta‐analysis (AFFINITY 2020; EFFECTS 2020). We analysed available data for other two studies (Bembenek 2020; FOCUS 2019).
These analyses are shown in Analysis 2.1 to Analysis 2.10. There was no clear evidence of differences between SSRI and control for any outcome.
2.1. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 1: Disability (studies at low risk of bias only)
2.10. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 10: Independent on mRS (0‐2) all studies irrespective of risk of bias
Subgroup analyses by intervention characteristics and subsets of participant
We did not perform preplanned subgroup analyses by intervention characteristics and subsets of participant (including with or without depression) of the studies at low risk of bias, because they all used fluoxetine and all did not require participants to have depression to enter the trial.
Sensitivity analysis
Inclusion of all studies regardless of 'Risk of bias' judgement for the co‐primary outcomes
We included all studies reporting disability, regardless of 'Risk of bias' judgement for the co‐primary outcome of disability at the end of treatment using a SMD and a fixed‐effect model.
For disability, participants who received an SSRI intervention had significantly lower end‐of‐treatment scores than those participants receiving placebo or standard care/practice (SMD ‐0.18, 95% CI ‐0.23 to ‐0.14; P < 0.00001; 32 studies, 7667 participants) with considerable heterogeneity (I2 = 94% ) (Analysis 1.16). Our post‐hoc analysis (Funnel plot, Figure 4) demonstrated an absence of studies in the right hand side of the plot, consistent with publication bias.
1.16. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 16: Disability (all studies regardless of risk of bias)
We included all studies regardless of risk of bias judgement for the co‐primary outcome of independence.
Note that previously Andersen 2013 had the mRS data entered as a continuous variable for disability; for this update we have entered it only as dichotomous data for mRS.
The mRS 0 to 2 at the end of treatment was similar in the two groups (RR 0.97, 95% CI 0.93 to 1.01; P = 0.18, I2 = 59%, 8 studies, 6792 participants) (Analysis 1.17).
1.17. Analysis.

Comparison 1: SSRI versus control at end of treatment, by SSRI, Outcome 17: Independent on modified Rankin score (mRS 0 to 2) (all studies regardless of risk of bias)
Meta‐analysis using the alternate meta‐analytical effects model (fixed‐effect or random‐effects) for the primary outcomes from the high‐quality studies
We re‐analysed the data for our primary outcomes (disability score and independence (0‐2 on mRS) using the random‐effects analysis for the high‐quality studies. This made no difference to the results (Table 2).
1. Sensitivity analysis for co‐primary outcomes depending on the method of analysis.
| mRS (RR and 95% CI) | Disability (SMD and 95% CI) | |
| Fixed‐effect | 0.98 (0.93, 1.03) | ‐0.0 (‐0.05, 0.05) |
| Random‐effects | 0.98 (0.92, 1.04) | ‐0.00 (‐0.05, 0.05) |
CI: confidence interval mRS: modified Rankin Scale RR: risk ratio SMD: standardised mean difference
Discussion
Summary of main results
For this update we included 76 studies with 13,029 participants, of which 38 used fluoxetine and the remaining studies used other selective serotonin reuptake inhibitors (SSRIs) . Data from our co‐primary outcomes (disability, independence) were not collected in many of the studies.
Six studies were at low risk of bias across all key domains; these all recruited participants who were less than 90 days after stroke onset, none used depression as an inclusion criterion; and they all compared fluoxetine with placebo. Comparing fluoxetine to placebo in these trials, we found high‐quality evidence of no beneficial effects of fluoxetine on our co‐primary outcomes (disability and independence) at end of treatment. We found high‐quality evidence that fluoxetine reduced the severity of depression evaluated using a continuous outcome and the number of participants with depression at end of treatment. We found an excess of participants having seizures and bone fractures amongst those allocated to fluoxetine. Cognition was lower at the end of treatment in the SSRI group. As we included only high‐quality studies in our main analyses, we did not downgrade for quality of trials; the main reason for downgrading quality was because of imprecision.
There are data on outcomes at end of follow‐up for two trials (Bembenek 2020; FOCUS 2019); follow‐up data will be available for two other studies in due course (AFFINITY 2020; EFFECTS 2020).
When we performed a meta‐analysis of disability for all studies irrespective of risk of bias, we found a small beneficial effect of SSRI but with high heterogeneity. There was no difference in the proportion of participants independent at follow‐up; for this outcome there was evidence of publication bias on our funnel plot.
Overall completeness and applicability of evidence
This review includes studies from different settings (e.g. countries; high‐, middle‐ and low‐income settings; healthcare systems), with different criteria for selecting participants (e.g. methods of pre‐randomisation diagnosis and investigation, inclusion and exclusion criteria), that may reflect differences between the trial protocol and routine clinical practice (e.g. inclusion of participants based on a diagnosis of stroke made using brain imaging: brain imaging is unlikely to be either available or affordable in routine clinical care in many low‐ and middle‐income country settings); and different characteristics of randomised participants (e.g. baseline demographic and clinical characteristics, stroke severity, time since stroke onset, presence or absence of depression, severity of depression). These study characteristics may in part explain the heterogeneity of results, but we know from our previous review that the most probable cause of heterogeneity is study quality.
There is a discordance between the results for disability (one of our co‐primary outcomes) between the studies at low risk of bias, which showed no effect, and all studies irrespective of bias (a positive effect). This is because trials at high risk of bias tended to be positive.
The results of the meta‐analysis of the seven studies at low risk of bias are applicable to clinical practice throughout the world, for both ischaemic and haemorrhagic stroke.
There is a theoretical risk that SSRIs might carry particular risks in people with haemorrhagic stroke, due to their effects on platelet aggregation and bleeding, but there was no evidence of this based on data from the individual studies; to explore this further we are planning an individual patient meta‐analysis (EFFECTS 2020; FOCUS 2019). We noted that those allocated control had better cognition at the end of treatment, although the effect size was very small, and of uncertain clinical relevance. According to the NHS in the UK, confusion is a rare side effect of SSRIs (NHS 2021 , but on the other hand, there is also systematic review evidence that fluoxetine might improve cognition in people with dementia (Xie 2019). Our finding might also have been due to chance. We plan to explore in more detail the impact of fluoxetine on cognition when we perform our individual patient data meta‐analysis from the three large studies.
There were no data on anxiety from the studies, even though anxiety is a common problem after stroke.
We were unable to explore the influence of the type of SSRI, as all the high‐quality trials used fluoxetine.
The full searches were last performed in January 2021; the lead review author (GM) searched WHO ICTRP in August 2021 and did not find any further new eligible studies. We are not aware of any other new studies published since January 2021 that are likely to change the results of the review.
We have data on follow‐up after treatment end for only two studies (Bembenek 2020; FOCUS 2019). Two large studies have unpublished data for outcome six months after treatment end (12 months after randomisation) (AFFINITY 2020; EFFECTS 2020); these data will be incorporated into an individual patient data meta‐analysis in due course (Mead 2020).
We did not include studies which combined an SSRI with another active treatment (either drugs or another type of intervention), and either compared with control or the active treatment alone. It is possible that SSRIS could modify (either enhance or reduce) training‐induced brain plasticity and hence functional recovery. Thus, the absence of an effect of SSRIs on disability might have been because the SSRI was not coupled with a domain‐specific behavioural rehabilitation intervention. In the future, a systematic review of SSRIs plus training would be of interest.
Quality of the evidence
For the evaluation of quality of the evidence, we contacted authors of primary studies as yet unpublished for data on outcomes. For studies which we thought would fall into the category of being at low risk of bias across all the domains, but where some of the methodology was not reported in sufficient detail to enable us to make a final judgement, we contacted authors to clarify methodology. We also contacted authors of primary studies when it appeared that the same (or similar) group of patients had been described in more than one publication, in order to avoid double counting participants, and for one study, we also contacted the editors of the respective journals.
We used the Cochrane risk of bias tool to assess study methods. As in the previous update (Legg 2019), we restricted our meta‐analyses to studies at low risk of bias, because in the first review, Mead 2011, there was evidence that the apparently beneficial effects of SSRI on recovery was due to methodological limitations of the included trials. This observation was confirmed by the sensitivity analyses that we performed for these two previous reviews.
The meta‐analysis of the high‐quality studies is dominated by three trials (AFFINITY 2020; EFFECTS 2020; FOCUS 2019). All three of these trials were neutral for their primary outcome (modified Rankin score (mRS) at six months).
We performed sensitivity analyses of our two co‐primary outcomes (disability and independence) by including all the available outcome data, irrespective of risk of bias. Like our initial (hypothesis‐generating) Cochrane Review (Mead 2011), we found that SSRIs reduced disability at the end of treatment. However, it is highly likely that this positive effect is due to biases in trial quality. Publication bias might also be a problem, as suggested by the funnel plot (Figure 4).
We also performed sensitivity analyses to explore whether a random‐effects model would make any difference to outcome, but it did not (Table 2).
Potential biases in the review process
We conducted the review using robust Cochrane methodology, with two review authors independently assessing studies for eligibility, extracting data, and carrying out risk of bias assessment. As five review authors (MD, GEM, EL, GH, MH) were also authors of the AFFINITY 2020, FOCUS 2019, and EFFECTS 2020 trials, we ensured that assessment of risk of bias and data extraction for these trials was not performed by these review authors; except for unpublished data on mean (SD) for the Stroke Impact Scale scores, fatigue and quality of life, which were provided by the trial statisticians and entered into forest plots by one review author (GEM).
Our searches identified one systematic review that included several trials from China that we had not identified in the previous review (Li 2020). These trials are now included. Thus, it is possible, though unlikely, that there are other trials that have been published since the Li 2020 review that our searches might not have identified.
After editorial review in July 2021, we decided to perform a final check of the WHO ICTRP (that had last been searched about a year previously) to check for any new ongoing studies. This search was done by one review author only (GEM) and so it is possible, though very unlikely, that new studies were missed.
Agreements and disagreements with other studies or reviews
This review has demonstrated that SSRIs do not improve recovery after stroke. This is in contrast with several other meta‐analyses which showed that SSRIs might improve recovery, but these meta‐analyses did not include two recently published large high‐quality trials which were both neutral (AFFINITY 2020; EFFECTS 2020). In this meta‐analysis, we were also able to explore the influence of SSRIs on other important outcomes, that previous reviews had not done, because there had previously been insufficient data.
Authors' conclusions
Implications for practice.
Based on our meta‐analysis of the studies at low risk of bias, most of which provided selective serotonin reuptake inhibitors (SSRIs) early after stroke and did not require participants to have depression, there is currently no indication for the routine prescription of SSRIs in order to reduce disability and increase independence after stroke. Fluoxetine, which was the most commonly used SSRI and used in the three largest trials, reduces the risk of depression and the severity of depression, but this is probably not a sufficiently strong rationale to give all people with stroke a six‐month course of the drug, particularly as there is an increased risk of seizures and fractures. As the studies at low risk of bias all did not require patients to have depression at entry, we do not know for certain whether SSRIs might reduce disability in people who do have depression after stroke. Also, we do not know what effect SSRIs other than fluoxetine might have on recovery after stroke.
Implications for research.
This review found high‐quality evidence that SSRIs do not improve recovery after stroke and provided reliable evidence about their risks, though this conclusion is based mainly on evidence about fluoxetine. Thus, further trials of SSRI for stroke recovery are almost certainly not needed, unless they are designed only to include people with depression. This is because all the studies in this review which were at low risk of bias did not require participants to have depression at entry.
We have published a protocol for an individual patient data meta‐analysis of the three largest studies included in this review, all of which were of high quality (AFFINITY 2020; EFFECTS 2020; FOCUS 2019). This individual patient data meta‐analysis may provide more precise estimates of treatment effects and may be able to identify any differences in outcome related to country or ethnicity. We are also planning to publish a series of other papers, using these data, which we have already described (Mead 2020).
We have carefully considered whether to update this review again. Currently there are several small ongoing studies but, because they are small, the results will not make a material difference to the results of this review. Thus, we think that it is unlikely that further updates of this Cochrane Review will be needed. However, if further large studies are established in the future, we will reconsider this decision.
What's new
| Date | Event | Description |
|---|---|---|
| 7 January 2021 | New citation required and conclusions have changed | The conclusions are now more certain than in the previous version. |
| 7 January 2021 | New search has been performed | We updated the searches. We identified and included 13 new studies. There are now 76 included studies involving 13,029 participants. We have created a funnel plot and entered data on SF36 vitality, quality of life, and fractures. |
History
Protocol first published: Issue 11, 2011 Review first published: Issue 11, 2012
| Date | Event | Description |
|---|---|---|
| 14 March 2019 | New citation required and conclusions have changed | We include 2 new high‐quality trials. Meta‐analysis of all the high‐quality trials shows no effect on either of the co‐primary outcomes of independence and disability. Meta‐analysis of all trials irrespective of trial quality showed that SSRIs reduced disability at the end of treatment. |
| 14 March 2019 | New search has been performed | We have clarified that there are 2 primary outcomes: independence and disability. For modified Rankin Score (mRS) in advance of starting this update, we decided to report the proportion of independent participants compared with the proportion dead or dependent which is the usual convention in stroke trials. In the previous version we had reported the proportion dependent and had excluded the dead participants from the analysis. We checked the total number of participants included in the 2012 review. We had stated that the trials included 4060 participants; there were errors in the arithmetic (due to counting number allocated rather than those recruited, and omitting to count data from 2 small trials). When we recalculated the figures, there were 4109 recruited. We excluded 7 of these trials (439 participants) which had combined an SSRI with another active intervention and compared it to the active treatment alone or where there was a non‐random component to sequence generation process (see list of excluded studies in text). We added 14 new completed trials, recruiting 5498 participants. There are now a total of 63 trials recruiting a total of 9168 participants. We decided to restrict our primary analyses only to those trials at low risk of bias. We did this because we wished to provide a clear answer about the risks and benefits of SSRIs, which was not influenced by trial quality and because it would have been impractical, given the resources for this update, to perform analyses including all the low‐quality trials. We made this decision before we knew the results of the largest trial in this review (FOCUS). We have, however, performed a sensitivity analysis for dependence and disability (our primary outcomes) using data from all trials; as in the first version of the review, this sensitivity analysis showed that when low‐quality trials are included, results tend to be in favour of SSRIs. We adhered to the MECIR standards for conduct and reporting. We shortened our list of excluded studies in line with the Cochrane Handbook, by not listing those studies that obviously did not fulfil inclusion criteria, including those studies which clearly had an ineligible comparator, intervention or study design. |
| 26 August 2013 | Amended | The review authors identified minor errors following publication of the previous version. These errors have now been corrected and have resulted in very minor changes in SMD for disability and some I2 values. The changes have not materially changed the results or conclusions of the review. Changes made: (1) the total number of participants has been changed from 4059 to 4060; (2) Almeida 2006 recruited people without depression; this has been corrected in the 'Characteristics of included studies' table, and data have been moved to 'did not have to have depression' in the relevant subgroup analyses; (3) disability data for Acler 2009 had been entered incorrectly; this has now been corrected. |
Acknowledgements
For this update, we are grateful to the following people.
Joshua Cheyne, Cochrane Stroke Information Specialist, ran the literature searches.
Maureen Harding obtained articles for full‐text review.
Dr Jan Bembenek and Professor Anna Czlonkowska provided further unpublished information about FOCUS‐Poland, and additional data on SIS.
Dr Qilong Yi provided additional data for means (SD) of SIS, SF‐36 vitality and quality of life from AFFINITY.
Professor Osvaldo Almeida provided additional information about Almeida 2006
Dr Per Näsman provided data for means (SD) of SIS, SF‐36 vitality and quality of life from AFFINITY.
Dr Ehsan Karimi provided further information about Asadollahi 2018.
Bernhard Sabel (Editor in Chief of Restorative Neurology and Neuroscience) and Dr. João Pereira Leite, Editor of Brazilian Journal of Medical and Biological Research, wrote to the authors of the two publications relating to Cao 2020; these papers were very similar. No response was received; the two editors kindly checked the text of the two papers and decided that it was likely that the two papers described overlapping groups of patients.
We are also grateful to the peer reviewers and editors in Cochrane Stroke for their comments.
This updated review was funded by the National Institute for Health Research (NIHR) [NIHR Cochrane Review Incentive Scheme 2020 (NIHR133254)]. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Appendices
Appendix 1. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
[1] The CENTRAL search strategy looks different to the one I have stored. Please see below the correct strategy and add it into your appendices. #1 MeSH descriptor: [Cerebrovascular Disorders] this term only #2 MeSH descriptor: [Basal Ganglia Cerebrovascular Disease] explode all trees #3 MeSH descriptor: [Brain Ischemia] explode all trees #4 MeSH descriptor: [Carotid Artery Diseases] explode all trees #5 MeSH descriptor: [Intracranial Arterial Diseases] explode all trees #6 MeSH descriptor: [Intracranial Embolism and Thrombosis] explode all trees #7 MeSH descriptor: [Intracranial Hemorrhages] explode all trees #8 MeSH descriptor: [Stroke] explode all trees #9 MeSH descriptor: [Brain Infarction] explode all trees #10 MeSH descriptor: [Vertebral Artery Dissection] this term only #11 (stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc* or cva* or apoplex* or SAH):ti,ab,kw (Word variations have been searched) #12 ((brain* or cerebr* or cerebell* or intracran* or intracerebral) near/5 (isch?emi* or infarct* or thrombo* or emboli* or occlus*)):ti,ab,kw (Word variations have been searched) #13 ((brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid) near/5 (haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed*)):ti,ab,kw (Word variations have been searched) #14 MeSH descriptor: [Hemiplegia] this term only #15 MeSH descriptor: [Paresis] explode all trees #16 (hemipleg* or hemipar* or paresis or paretic):ti,ab,kw (Word variations have been searched) #17 MeSH descriptor: [Gait Disorders, Neurologic] explode all trees #18 {or #1‐#17} #19 MeSH descriptor: [Serotonin Uptake Inhibitors] explode all trees #20 ((serotonin or 5‐HT or 5 HT or 5‐hydroxytryptamine or 5 hydroxytryptamine) near/5 (uptake or reuptake or re‐uptake) near/5 inhib*):ti,ab,kw (Word variations have been searched) #21 SSRI*:ti,ab,kw (Word variations have been searched) #22 (alaproclat* or cericlamin* or citalopram or clomipramin* or dapoxetin* or etoperidon* or escitalopram or femoxetin* or fenfluramin* or fluoxetin* or fluvoxamin* or nonfenfluramin* or paroxetin* or sertralin$ or trazodone or vilazodone or zimelidine):ti,ab,kw (Word variations have been searched) #23 (Celexa or Cipramil or Cipram or Recital or Emocal or Dalsan or Sepram or Seropram or Citox or Priligy or Lexapro or Cipralex or Seroplex or Esertia or Prozac or Fontex or Seromex or Seronil or Sarafem or Ladose or Motivest or Fluctin or fluox or Lovan or Luvox or Fevarin or Faverin or Favoxil or Movox or Paxil or Seroxat or Sereupin or Aropax or Deroxat or Divarius or Rexetin or Xetanor or Paroxat or Loxamine or Zoloft or Lustral or Serlain or Asentra):ti,ab,kw (Word variations have been searched) #24 {or #19‐#23}
Appendix 2. MEDLINE (Ovid) search strategy
1. cerebrovascular disorders/ or exp basal ganglia cerebrovascular disease/ or exp brain ischemia/ or exp carotid artery diseases/ or exp intracranial arterial diseases/ or exp "intracranial embolism and thrombosis"/ or exp intracranial hemorrhages/ or stroke/ or exp brain infarction/ or vertebral artery dissection/ 2. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw. 3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 5. hemiplegia/ or exp paresis/ 6. (hemipleg$ or hemipar$ or paresis or paretic).tw. 7. exp Gait Disorders, Neurologic/ 8. or/1‐7 9. exp Serotonin Uptake Inhibitors/ 10. ((serotonin or 5‐HT or 5 HT or 5‐hydroxytryptamine or 5 hydroxytryptamine) adj5 (uptake or reuptake or re‐uptake) adj5 inhib$).tw. 11. SSRI$1.tw. 12. (alaproclat$ or cericlamin$ or citalopram or dapoxetin$ or escitalopram or femoxetin$ or fluoxetin$ or fluvoxamin$ or paroxetin$ or sertralin$ or trazodone or vilazodone or zimelidine).tw,nm. 13. (Celexa or Cipramil or Cipram or Recital or Emocal or Dalsan or Sepram or Seropram or Citox or Priligy or Lexapro or Cipralex or Seroplex or Esertia or Prozac or Fontex or Seromex or Seronil or Sarafem or Ladose or Motivest or Fluctin or fluox or Lovan or Luvox or Fevarin or Faverin or Favoxil or Movox or Paxil or Seroxat or Sereupin or Aropax or Deroxat or Divarius or Rexetin or Xetanor or Paroxat or Loxamine or Zoloft or Lustral or Serlain or Asentra).tw,nm. 14. 9 or 10 or 11 or 12 or 13 15. 8 and 14 16. exp animals/ not humans.sh. 17. 15 not 16 18. Randomized Controlled Trials as Topic/ 19. random allocation/ 20. Controlled Clinical Trials as Topic/ 21. control groups/ 22. clinical trials as topic/ or clinical trials, phase i as topic/ or clinical trials, phase ii as topic/ or clinical trials, phase iii as topic/ or clinical trials, phase iv as topic/ 23. Clinical Trials Data Monitoring Committees/ 24. double‐blind method/ 25. single‐blind method/ 26. Placebos/ 27. placebo effect/ 28. cross‐over studies/ 29. Multicenter Studies as Topic/ 30. Therapies, Investigational/ 31. Drug Evaluation/ 32. Research Design/ 33. Program Evaluation/ 34. evaluation studies as topic/ 35. randomized controlled trial.pt. 36. controlled clinical trial.pt. 37. (clinical trial or clinical trial phase i or clinical trial phase ii or clinical trial phase iii or clinical trial phase iv).pt. 38. multicenter study.pt. 39. (evaluation studies or comparative study).pt. 40. meta analysis.pt. 41. meta‐analysis as topic/ 42. random$.tw. 43. (controlled adj5 (trial$ or stud$)).tw. 44. (clinical$ adj5 trial$).tw. 45. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 46. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 47. ((multicenter or multicentre or therapeutic) adj5 (trial$ or stud$)).tw. 48. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw. 49. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 50. (coin adj5 (flip or flipped or toss$)).tw. 51. latin square.tw. 52. versus.tw. 53. (cross‐over or cross over or crossover).tw. 54. placebo$.tw. 55. sham.tw. 56. (assign$ or alternate or allocat$ or counterbalance$ or multiple baseline).tw. 57. controls.tw. 58. (treatment$ adj6 order).tw. 59. (meta‐analy$ or metaanaly$ or meta analy$ or systematic review or systematic overview).tw. 60. or/18‐59 61. 17 and 60
Appendix 3. Embase (Ovid) search strategy
1. cerebrovascular disease/ or basal ganglion hemorrhage/ or exp brain hematoma/ or exp brain hemorrhage/ or exp brain infarction/ or exp brain ischemia/ or exp carotid artery disease/ or cerebral artery disease/ or cerebrovascular accident/ or exp intracranial aneurysm/ or exp occlusive cerebrovascular disease/ or stroke/ 2. stroke unit/ or stroke patient/ 3. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 5. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 6. hemiparesis/ or hemiplegia/ or paresis/ 7. (hemipleg$ or hemipar$ or paresis or paretic).tw. 8. or/1‐7 9. exp serotonin uptake inhibitor/ 10. ((serotonin or 5‐HT or 5 HT or 5‐hydroxytryptamine or 5 hydroxytryptamine) adj5 (uptake or reuptake or re‐uptake) adj5 inhib$).tw. 11. SSRI$1.tw. 12. (alaproclat$ or cericlamin$ or citalopram or dapoxetin$ or escitalopram or femoxetin$ or fluoxetin$ or fluvoxamin$ or paroxetin$ or sertralin$ or trazodone or vilazodone or zimelidine).tw. 13. (Celexa or Cipramil or Cipram or Recital or Emocal or Dalsan or Sepram or Seropram or Citox or Priligy or Lexapro or Cipralex or Seroplex or Esertia or Prozac or Fontex or Seromex or Seronil or Sarafem or Ladose or Motivest or Fluctin or fluox or Lovan or Luvox or Fevarin or Faverin or Favoxil or Movox or Paxil or Seroxat or Sereupin or Aropax or Deroxat or Divarius or Rexetin or Xetanor or Paroxat or Loxamine or Zoloft or Lustral or Serlain or Asentra).tw,tn. 14. 9 or 10 or 11 or 12 or 13 15. 8 and 14 16. limit 15 to human 17. Randomized Controlled Trial/ 18. Randomization/ 19. Controlled Study/ 20. control group/ 21. clinical trial/ or phase 1 clinical trial/ or phase 2 clinical trial/ or phase 3 clinical trial/ or phase 4 clinical trial/ or controlled clinical trial/ 22. Double Blind Procedure/ 23. Single Blind Procedure/ or triple blind procedure/ 24. placebo/ 25. "types of study"/ 26. research subject/ 27. random$.tw. 28. (controlled adj5 (trial$ or stud$)).tw. 29. (clinical$ adj5 trial$).tw. 30. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw. 31. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw. 32. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw. 33. (coin adj5 (flip or flipped or toss$)).tw. 34. versus.tw. 35. placebo$.tw. 36. controls.tw. 37. or/17‐36 38. 16 and 37
Appendix 4. CINAHL (Ebsco) search strategy
S23. S12 and S22 S22. S13 or S17 or S18 or S19 or S20 or S21 S21. AB Celexa or Cipramil or Cipram or Recital or Emocal or Dalsan or Sepram or Seropram or Citox or Priligy or Lexapro or Cipralex or Seroplex or Esertia or Prozac or Fontex or Seromex or Seronil or Sarafem or Ladose or Motivest or Fluctin or fluox or Lovan or Luvox or Fevarin or Faverin or Favoxil or Movox or Paxil or Seroxat or Sereupin or Aropax or Deroxat or Divarius or Rexetin or Xetanor or Paroxat or Loxamine or Zoloft or Lustral or Serlain or Asentra S20. TI Celexa or Cipramil or Cipram or Recital or Emocal or Dalsan or Sepram or Seropram or Citox or Priligy or Lexapro or Cipralex or Seroplex or Esertia or Prozac or Fontex or Seromex or Seronil or Sarafem or Ladose or Motivest or Fluctin or fluox or Lovan or Luvox or Fevarin or Faverin or Favoxil or Movox or Paxil or Seroxat or Sereupin or Aropax or Deroxat or Divarius or Rexetin or Xetanor or Paroxat or Loxamine or Zoloft or Lustral or Serlain or Asentra S19. TI ( alaproclat* or cericlamin* or citalopram or dapoxetin* or escitalopram or femoxetin* or fluoxetin* or fluvoxamin* or paroxetin* or sertralin* or trazodone or vilazodone or zimelidine ) OR AB ( alaproclat* or cericlamin* or citalopram or dapoxetin* or escitalopram or femoxetin* or fluoxetin* or fluvoxamin* or paroxetin* or sertralin* or trazodone or vilazodone or zimelidine ) S18. TI SSRI* OR AB SSRI* S17. S14 and S15 and S16 S16. TI inhib* OR AB inhib* S15. TI ( uptake or reuptake or re‐uptake ) OR AB ( uptake or reuptake or re‐uptake ) S14. TI ( serotonin or 5‐HT or 5 HT or 5‐hydroxytryptamine or 5 hydroxytryptamine ) OR AB ( serotonin or 5‐HT or 5 HT or 5‐hydroxytryptamine or 5 hydroxytryptamine ) S13. (MH "Serotonin Uptake Inhibitors+") S12. S1 or S2 or S3 or S6 or S9 or S10 or S11 S11. TI ( hemipleg* or hemipar* or paresis or paretic ) or AB ( hemipleg* or hemipar* or paresis or paretic ) S10. (MH "Hemiplegia") S9. S7 and S8 S8. TI ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* ) or AB ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* ) S7. TI ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid ) or AB ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid ) S6. S4 and S5 S5. TI ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* ) or AB ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* ) S4. TI ( brain* or cerebr* or cerebell* or intracran* or intracerebral ) or AB ( brain* or cerebr* or cerebell* or intracran* or intracerebral ) S3. TI ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH ) or AB ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH ) S2. (MH "Stroke Patients") OR (MH "Stroke Units") S1. (MH "Cerebrovascular Disorders") OR (MH "Basal Ganglia Cerebrovascular Disease+") OR (MH "Carotid Artery Diseases+") OR (MH "Cerebral Ischemia+") OR (MH "Cerebral Vasospasm") OR (MH "Intracranial Arterial Diseases+") OR (MH "Intracranial Embolism and Thrombosis") OR (MH "Intracranial Hemorrhage+") OR (MH "Stroke") OR (MH "Vertebral Artery Dissections")
Appendix 5. AMED (Ovid) search strategy
1. cerebrovascular disorders/ or cerebral hemorrhage/ or cerebral infarction/ or cerebral ischemia/ or cerebrovascular accident/ or stroke/ 2. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw. 3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 5. hemiplegia/ 6. (hemipleg$ or hemipar$ or paresis or paretic).tw. 7. or/1‐6 8. antidepressive agents/ 9. ((serotonin or 5‐HT or 5 HT or 5‐hydroxytryptamine or 5 hydroxytryptamine) adj5 (uptake or reuptake or re‐uptake) adj5 inhib$).tw. 10. SSRI$1.tw. 11. (alaproclat$ or cericlamin$ or citalopram or dapoxetin$ or escitalopram or femoxetin$ or fluoxetin$ or fluvoxamin$ or paroxetin$ or sertralin$ or trazodone or vilazodone or zimelidine).tw. 12. (Celexa or Cipramil or Cipram or Recital or Emocal or Dalsan or Sepram or Seropram or Citox or Priligy or Lexapro or Cipralex or Seroplex or Esertia or Prozac or Fontex or Seromex or Seronil or Sarafem or Ladose or Motivest or Fluctin or fluox or Lovan or Luvox or Fevarin or Faverin or Favoxil or Movox or Paxil or Seroxat or Sereupin or Aropax or Deroxat or Divarius or Rexetin or Xetanor or Paroxat or Loxamine or Zoloft or Lustral or Serlain or Asentra).tw. 13. 8 or 9 or 10 or 11 or 12 14. 7 and 13
Appendix 6. PsycINFO (Ovid) search strategy
1. cerebrovascular disorders/ or cerebral hemorrhage/ or exp cerebral ischemia/ or cerebral small vessel disease/ or cerebrovascular accidents/ or subarachnoid hemorrhage/ 2. (stroke or poststroke or post‐stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw. 3. ((brain$ or cerebr$ or cerebell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. 4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. 5. (hemipleg$ or hemipar$ or paresis or paretic).tw. 6. hemiparesis/ or hemiplegia/ 7. or/1‐6 8. exp serotonin reuptake inhibitors/ 9. ((serotonin or 5‐HT or 5 HT or 5‐hydroxytryptamine or 5 hydroxytryptamine) adj5 (uptake or reuptake or re‐uptake) adj5 inhib$).tw. 10. SSRI$1.tw. 11. (alaproclat$ or cericlamin$ or citalopram or dapoxetin$ or escitalopram or femoxetin$ or fluoxetin$ or fluvoxamin$ or paroxetin$ or sertralin$ or trazodone or vilazodone or zimelidine).tw. 12. (Celexa or Cipramil or Cipram or Recital or Emocal or Dalsan or Sepram or Seropram or Citox or Priligy or Lexapro or Cipralex or Seroplex or Esertia or Prozac or Fontex or Seromex or Seronil or Sarafem or Ladose or Motivest or Fluctin or fluox or Lovan or Luvox or Fevarin or Faverin or Favoxil or Movox or Paxil or Seroxat or Sereupin or Aropax or Deroxat or Divarius or Rexetin or Xetanor or Paroxat or Loxamine or Zoloft or Lustral or Serlain or Asentra).tw. 13. 8 or 9 or 10 or 11 or 12 14. 7 and 13
Appendix 7. Search strategy for the trial registers
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch;search strategy) 1. Basic search: CEREBR* AND selective serotonin OR CEREBR* AND alaproclate OR CEREBR* AND cericlamine OR CEREBR* AND citalopram OR CEREBR* AND clomipramine OR CEREBR* AND dapoxetine OR CEREBR* AND etoperidone OR CEREBR* AND escitalopram OR CEREBR* AND femoxetine OR CEREBR* AND fenfluramine OR CEREBR* AND fluoxetine OR CEREBR* AND fluvoxamine OR CEREBR* AND norfenfluramine OR CEREBR* AND paroxetine OR CEREBR* AND sertraline OR CEREBR* AND trazodone OR CEREBR* AND vilazodone OR CEREBR* AND zimelidine 2. Basic search: STROKE AND selective serotonin OR STROKE AND alaproclate OR STROKE AND cericlamine OR STROKE AND citalopram OR STROKE AND clomipramine OR STROKE AND dapoxetine OR STROKE AND etoperidone OR STROKE AND escitalopram OR STROKE AND femoxetine OR STROKE AND fenfluramine OR STROKE AND fluoxetine OR STROKE AND fluvoxamine OR STROKE AND norfenfluramine OR STROKE AND paroxetine OR STROKE AND sertraline OR STROKE AND trazodone OR STROKE AND vilazodone OR STROKE AND zimelidine US National Institutes of Health Trials Register (ClinicalTrials.gov) search strategy ( “selective serotonin” OR alaproclate OR cericlamine OR citalopram OR clomipramine OR dapoxetine OR etoperidone OR escitalopram OR femoxetine OR fenfluramine OR fluoxetine OR fluvoxamine OR norfenfluramine OR paroxetine OR sertraline OR trazodone OR vilazodone OR zimelidine ) AND EXACT "Interventional" [STUDY‐TYPES] AND Stroke [DISEASE]
Data and analyses
Comparison 1. SSRI versus control at end of treatment, by SSRI.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Disability (primary outcome). Studies at low risk of bias | 5 | 5436 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.00 [‐0.05, 0.05] |
| 1.1.1 Fluoxetine | 5 | 5436 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.00 [‐0.05, 0.05] |
| 1.2 Independent on modified Rankin score (mRS 0 to 2) (primary outcome). Studies at low risk of bias | 5 | 5926 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.93, 1.03] |
| 1.3 Neurological deficit score (studies at low risk of bias) | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.39 [‐1.12, 0.33] |
| 1.3.1 Fluoxetine | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.39 [‐1.12, 0.33] |
| 1.4 Motor deficits (studies at low risk of bias) | 6 | 5518 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.02, 0.08] |
| 1.4.1 Fluoxetine | 6 | 5518 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.02, 0.08] |
| 1.5 Depression, continuous data (studies at low risk of bias) | 4 | 5356 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.19, ‐0.08] |
| 1.5.1 Fluoxetine | 4 | 5356 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.19, ‐0.08] |
| 1.6 Depression, dichotomous data (studies at low risk of bias) | 3 | 5907 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.65, 0.86] |
| 1.6.1 Fluoxetine | 3 | 5907 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.65, 0.86] |
| 1.7 Death (trials at low risk of bias) | 6 | 6090 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.82, 1.24] |
| 1.7.1 Fluoxetine | 6 | 6090 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.82, 1.24] |
| 1.8 Seizures (studies at low risk of bias) | 6 | 6080 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [1.00, 1.98] |
| 1.8.1 Fluoxetine | 6 | 6080 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [1.00, 1.98] |
| 1.9 Gastrointestinal side effects (studies at low risk of bias) | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.71 [0.33, 8.83] |
| 1.9.1 Fluoxetine | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.71 [0.33, 8.83] |
| 1.10 Bleeding (studies at low risk of bias) | 6 | 6088 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.69, 1.70] |
| 1.10.1 Fluoxetine (except for Asadollahi 2018) | 6 | 6088 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.69, 1.70] |
| 1.11 Fractures (studies at low risk of only) | 6 | 6080 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.35 [1.62, 3.41] |
| 1.12 Cognition (trials at low risk of bias) | 4 | 5373 | Mean Difference (IV, Fixed, 95% CI) | ‐1.22 [‐2.37, ‐0.07] |
| 1.13 Leaving the study before the end of scheduled follow‐up for reasons other than death (trials at low risk of bias) | 6 | 6090 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [1.03, 2.40] |
| 1.13.1 Fluoxetine | 6 | 6090 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [1.03, 2.40] |
| 1.14 Fatigue at end of treatment (studies at low risk of bias only) | 4 | 5524 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐1.24, 1.11] |
| 1.15 Quality of life at end of treatment (studies at low risk of bias) | 3 | 5482 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐0.02, 0.02] |
| 1.16 Disability (all studies regardless of risk of bias) | 32 | 7667 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.23, ‐0.14] |
| 1.16.1 Fluoxetine | 19 | 6590 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.13, ‐0.04] |
| 1.16.2 Sertraline | 1 | 130 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.38 [‐1.76, ‐0.99] |
| 1.16.3 Paroxetine | 5 | 293 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.29 [‐1.55, ‐1.03] |
| 1.16.4 Citalopram | 5 | 446 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.68 [‐0.88, ‐0.48] |
| 1.16.5 Escitalopram | 2 | 208 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.00, ‐0.34] |
| 1.17 Independent on modified Rankin score (mRS 0 to 2) (all studies regardless of risk of bias) | 8 | 6792 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.93, 1.01] |
| 1.17.1 Fluoxetine | 6 | 6039 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.94, 1.03] |
| 1.17.2 Sertraline | 1 | 111 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.97, 1.04] |
| 1.17.3 Citalopram | 1 | 642 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.82, 0.98] |
Comparison 2. SSRI versus control at end of follow up, by SSRI.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Disability (studies at low risk of bias only) | 2 | 2591 | Mean Difference (IV, Fixed, 95% CI) | ‐0.24 [‐2.59, 2.11] |
| 2.2 Independent on modified rankin score (0‐2) (studies at low risk of bias only) | 2 | 3137 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.89, 1.19] |
| 2.3 Depression, continuous data (studies at low risk of bias only) | 2 | 2684 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.36, 0.44] |
| 2.4 Depression, dichotomous (studies at low risk of bias only) | 1 | 3083 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.73, 1.04] |
| 2.5 Motor deficits (studies at low risk of bias only) | 2 | 2688 | Mean Difference (IV, Fixed, 95% CI) | ‐0.77 [‐3.00, 1.46] |
| 2.6 Cognition (studies at low risk of bias only) | 2 | 2689 | Mean Difference (IV, Fixed, 95% CI) | ‐0.35 [‐2.32, 1.62] |
| 2.7 Death (studies at low risk of bias only) | 2 | 3144 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.77, 1.12] |
| 2.8 Leaving the trial before the end of follow‐up, for reasons other than death ( studies at low risk of bias) | 2 | 3188 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.54, 1.51] |
| 2.9 Disability, all studies irrespective of risk of bias | 2 | 2691 | Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐2.56, 2.06] |
| 2.10 Independent on mRS (0‐2) all studies irrespective of risk of bias | 2 | 3134 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.89, 1.19] |
2.2. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 2: Independent on modified rankin score (0‐2) (studies at low risk of bias only)
2.3. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 3: Depression, continuous data (studies at low risk of bias only)
2.4. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 4: Depression, dichotomous (studies at low risk of bias only)
2.5. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 5: Motor deficits (studies at low risk of bias only)
2.6. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 6: Cognition (studies at low risk of bias only)
2.7. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 7: Death (studies at low risk of bias only)
2.8. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 8: Leaving the trial before the end of follow‐up, for reasons other than death ( studies at low risk of bias)
2.9. Analysis.

Comparison 2: SSRI versus control at end of follow up, by SSRI, Outcome 9: Disability, all studies irrespective of risk of bias
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Acler 2009.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Intervention model: parallel assignment Primary purpose: treatment |
|
| Participants | 20 participants Location: Italy Setting: inpatient Inclusion criteria: first‐ever ischaemic stroke, CT or MRI documenting a single monohemispheric lesion, age below 80 years, within 3 months of onset Exclusion criteria: major affective disorders, alcohol abuse and dementia leading to un‐cooperative behaviour, pacemakers, metal in the head, concomitant neuropathies, systemic vasculopathies, major affective disorders Treatment: 10 people, mean age 68 ± 7 years, 6 men Control: 10 people, mean age 65 ± 7 years, 6 men |
|
| Interventions | Citalopram 10 mg daily Placebo: identical pill daily Duration of treatment: at least 4 months Duration of follow‐up: not stated |
|
| Outcomes | Motor cortex excitability NIHSS Lindmark Scale BI HDRS BDI No data on death, GI upset, bleeds or seizures |
|
| Funding source | Source of funding not stated; unclear whether or not a drug company was involved in the study | |
| Notes | Dates of study not stated. Any conflicts of interest not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Stated blinded, placebo was 'an identical pill' |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Stated blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is not stated whether data from all recruited participants are reported |
| Selective reporting (reporting bias) | High risk | Side effects were not reported although they were assessed |
| Other bias | Unclear risk | − |
AFFINITY 2020.
| Study characteristics | ||
| Methods | Multicentre Study type: interventional (clinical trial) Allocation: randomised Intervention model: parallel assignment Masking: quadruple (participant, care provider, investigator, outcomes assessor) Primary purpose: treatment |
|
| Participants | 1280 participants Country: Australia (n = 532), New Zealand (n = 42), and Vietnam (n = 706) Setting: inpatient At randomisation number allocated: N = 1280: fluoxetine (n = 642); placebo (n = 638) % male: fluoxetine (64%); placebo (62%) Age: mean age: fluoxetine = 63.5± 12.5; placebo = 64.6 ± 12.2 Subtype of stroke
Inclusion criteria
Exclusion criteria:
|
|
| Interventions | Fluoxetine 20 mg once daily or matching placebo capsules for 6 months | |
| Outcomes | Primary outcome
Secondary outcomes at 180 and 365 days after randomisation
|
|
| Funding source | The AFFINITY trial was funded by the Australian NHMRC Project Grant 1059094. The minimisation algorithm was provided by The Stroke Research Group, Division of Clinical Neuroscience, University of Edinburgh, Edinburgh, UK | |
| Notes | ACTRN12611000774921Recruitment January 11, 2013, and June 30, 2019. GJH has received grants from the NHMRC of Australia, Vetenskapsrådet (The Swedish Research Council), and UK National Institute for Health Research Technology, during the conduct of the study; and personal fees from the American Heart Association, outside of the submitted work. MLH, CE‐B, LB, and TL have received grants from the NHMRC of Australia during the conduct of the study. CSA has received grants from the NHMRC of Australia, and grants and personal fees from Takeda, outside of the submitted work. All other members of the writing group declare no competing interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " The patient’s clinician entered the patient’s baseline data into a secure, password‐protected, centralised, web‐based randomisation system that checked the data for completeness and consistency and generated a unique study identification number and treatment pack number corresponding to fluoxetine or placebo in a 1:1 ratio." |
| Allocation concealment (selection bias) | Low risk | Quote: " All patients, carers, investigators, and outcome assessors were masked to the allocated treatment by use of placebo capsules that were visually identical to the fluoxetine capsules even when broken open. Success of masking was not assessed." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All patients, carers, investigators, and outcome assessors were masked to the allocated treatment by use of placebo capsules that were visually identical to the fluoxetine capsules even when broken open. Success of masking was not assessed." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All patients, carers, investigators, and outcome assessors were masked to the allocated treatment by use of placebo capsules that were visually identical to the fluoxetine capsules even when broken open. Success of masking was not assessed." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 5% dropped out or died and there is no compelling evidence of a difference between the 2 groups |
| Selective reporting (reporting bias) | Low risk | All outcomes in protocol were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Almeida 2006.
| Study characteristics | ||
| Methods | Parallel design Analysis: ITT (last observation carried forward), withdrawn owing to becoming depressed, AE, treating practitioner started antidepressant, medical advice, no reason given, not contactable ‐ numbers not included |
|
| Participants | Location: Australia Setting: inpatient Treatment: 55 people, mean ± SD age 68 ± 13 years, 67% men Control: 56 people, mean ± SD age 67 ± 13 years, 62% men Stroke criteria: acute ischaemic or haemorrhagic stroke, diagnosis by clinical signs (ICD‐10) and CT (100% imaged, 10/111 CT scan did not show acute ischaemia); stroke on average < 2 weeks prior to randomisation Not depressed (HADS‐D had to be over 7) Other entry criteria: not stated Comparability of treatment groups: more participants in treatment group with previous heart attack and stroke, also higher levels of hypertension Exclusion criteria: severe communication difficulties, unstable medical condition, severe cognitive impairment and depression (MMSE < 10), taking antidepressants within 4 weeks of stroke, contraindication to sertraline, previous reaction to sertraline, could not speak English |
|
| Interventions | Treatment: sertraline 50 mg daily (night) Control: matched placebo Duration: treatment continued for 24 weeks Duration of follow‐up (post‐treatment to study end): 28 weeks |
|
| Outcomes | Depression: change in scores from baseline to end of treatment on HDRS, proportion depressed Change in MMSE scores mRS Death Leaving the trial early Check list of possible AEs read out to participant by a research nurse |
|
| Funding source | Funded by an unrestricted grant from Rotary Health Research Fund | |
| Notes | Recruitment June 2004 to June 2006 Conflicts of interest not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Centralised |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Stated in paper, matched placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated in paper |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Performed last observation carried forward |
| Selective reporting (reporting bias) | Low risk | Trial protocol published on www.strokecentre.org/trials . This weblink is no longer available so we have been unable to check whether all the outcomes were reported. We have contacted the author to check this‐who confirm that all endpoints were reported |
| Other bias | Low risk | No other obvious biases |
Andersen 1994.
| Study characteristics | ||
| Methods | Parallel design Analysis (ITT) last observation carried forward and per protocol: death (1 treatment, 1 control) withdrawn owing to AE (6 treatment, 1 control), all excluded from analysis |
|
| Participants | Location: Denmark Setting: mixed Treatment: 33 people, mean ± SD age 68 ± 4 years, 36% men Control: 33 people, mean ± SD age 66 ± 9 years, 66% men Stroke criteria: ischaemic stroke and PICH; diagnosis via clinical signs and CT (100%); stroke 2 to 52 weeks prior to randomisation (average time 12 weeks) Depression criteria: HDRS score > 12 (score transformed to appropriate DSM‐III‐R criteria) Other entry criteria: none stated Comparability of treatment groups: balanced Exclusion criteria: depression within last year, receiving current treatment for depression, severe dementia or communication problems, degenerative or expansive neurological disease, decreased consciousness |
|
| Interventions | Experimental: citalopram 10 mg in participants > 66 years, 20 mg in participants < 67 years daily; dose doubled if no response to treatment within 3 weeks Comparator: matched placebo Duration: treatment continued for 6 weeks Duration of follow‐up (post‐treatment to study end): 0 Note that although the protocol on www.strokecentre.org/trials states that mood scores were measured up to 1 year post‐stroke, this probably refers to the time since stroke at the time of randomisation |
|
| Outcomes | Depression: change in scores from baseline to end of treatment on HDRS Melancholia scale Proportion no longer meeting entry criteria (< 13 on HDRS) 50% reduction in HDRS score Additional: leaving the study early Death AEs (unwanted drug effects were registered and evaluated at the same intervals using a side effect scale) Unable to use: BI, Social Activities Index, MMSE (data not presented) |
|
| Funding source | Funded by Lundbeck Foundation, Medical Research Foundation for North Jutland County, The Aalgorg Diocese Research Foundation, Consultant Otorhinolaryngologist Kopp's Foundation and Stine and Martinus Sorensen's Foundation. Lundbeck Pharma A/S provided the citalopram and placebo; thus we have classified this as 'unclear risk'. | |
| Notes | Recruitment 1 February 1991 to 29 February 1992. Conflicts of interest not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Blocks of 4 used |
| Allocation concealment (selection bias) | Low risk | Centralised opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Matched placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Those who were blinded were not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Although there were dropouts, analysis performed both per protocol and using last observation carried forward |
| Selective reporting (reporting bias) | High risk | Trial published on www.strokecentre.org/trials The primary outcome was reported. We have been unable to access this record on 28 September 2021, the paper also describes the social activities index in the list of outcomes but this was not reported in the results so we have changed this to high risk of bias for this 2021 update |
| Other bias | Unclear risk | − |
Andersen 2013.
| Study characteristics | ||
| Methods | Multicentre Study type: interventional (clinical trial) Intervention model: parallel assignment Primary purpose: treatment |
|
| Participants | 642 participants Country: Denmark Setting: inpatient At randomisation number allocated: citalopram n = 319; placebo n = 323 % male at baseline: citalopram n = 199/319 (62%); placebo n = 222/323 (69%) Age at baseline: mean age, citalopram 68 ± 13 (n = 319); placebo 68 ± 13 (n = 323) Subtype of stroke at baseline: not available Severity of stroke at baseline: NIHSS, citalopram 5.3 ± 5.6; placebo 4.8 ± 4.8 Time since stroke onset: mean time from last known 'well' to first treatment 1.7 days (median 1, IQR 0 to 6) Inclusion criteria:
Exclusion Criteria
|
|
| Interventions | Experimental: citalopram 20 mg (10 mg if aged ≥ 65 years or having reduced liver/kidney function) or placebo once daily for 6 months Comparator: ½ to 2 tablets with no intrinsic drug activity per day for 6 months |
|
| Outcomes | Primary outcomes
Secondary outcomes within or at 6 months
|
|
| Funding source | TrygFonden, the Danish Council for Independent Research, the Regional Medicine Fund, and the Aarhus University Research Foundation | |
| Notes | Dates study conducted: September 2013 to December 2016 Declarations of Interest: Dr Kraglund received speaker honoraria from Bristol‐Meyers Squibb and Pfizer. Dr Iversen received speaker honoraria from Boehringer Ingelheim, Bristol‐Myers Squibb, Bayer, AstraZeneca, and Pfizer and has previously participated in advisory board meetings for Boehringer Ingelheim, Bristol‐Myers Squibb, Pfizer, Bayer, AstraZeneca, and Amgen. Dr Grove has received speaker honoraria from AstraZeneca, Baxter, Bayer, Boehringer Ingelheim, Bristol‐Myers Squibb, MSD, and Pfizer and has previously participated in advisory board meetings for AstraZeneca, Bayer, Boehringer Ingelheim, and Bristol‐Myers Squibb. Dr Andersen reports other from MSD, personal fees from AstraZeneca, outside the submitted work |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated randomization code was used to randomize patients in blocks of 10." |
| Allocation concealment (selection bias) | Low risk | Quote: "Citalopram was commercially available (Sandoz, Denmark) and production of the placebo and randomization was prepared by a pharmacy independently of the investigators (Glostrup Pharmacy, Denmark). The tablets were indistinguishable and were supplied in numbered containers." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participant, care provider, and investigator assured and unlikely that the blinding could have been broken |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome assessor assured and unlikely that the blinding could have been broken |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition/exclusions reported with reasons provided (including did not start on study medication, consent withdrawn, side effects, indication for open label, other reasons (no detail provided)). At < 31 days of study medication, twice as many participants in the citalopram group withdrew consent (n = 29/318 (9%)) compared to the placebo group (n = 14/320 (4%)). However, at < 31 days twice as many participants in the placebo group (n = 12/318(4%)) compared to the citalopram group (n = 6/320 (2%) were switched to open label. Attrition/exclusions: 51/319 (16%) in the citalopram group and 39/319 (11%) in the placebo group. The investigators use LOCF in their intention‐to‐treat analysis. LOCF assumes that missing values are missing completely at random and ignores improvements or deteriorations in the participants condition since dropout and therefore stops improvements or declines in outcome measures. LOCF introduces risk of false or biased conclusions (Molnar 2008) |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all of the study's prespecified (primary and secondary) outcomes that are of interest to the review have been reported in the prespecified way |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Asadollahi 2018.
| Study characteristics | ||
| Methods | RCT Study type: interventional (clinical trial) Allocation: randomised Intervention model: parallel assignment Masking: double (participant, outcomes assessor) Primary purpose: treatment |
|
| Participants | 90 participants Country: Iran Setting: inpatient At randomisation number allocated: N = 90: citalopram (n = 30); fluoxetine (n = 30); placebo (n = 30) % male: citalopram (60%) fluoxetine (50%); placebo (56.6%) Age: mean age: citalopram = 61.7 ± 9.6; fluoxetine = 60.2 ± 8.52; placebo = 58.7 ± 8.56 Inclusion criteria
Exclusion criteria
|
|
| Interventions | Participants were randomly allocated to 1 of 3 groups: Group A received 20 mg orally of fluoxetine daily, Group B received 20 mg orally of citalopram daily, and Group C received a placebo orally. The duration of the therapy was 90 days. In addition to the medications, all of the participants received physiotherapy | |
| Outcomes | FMMS | |
| Funding source | No financial support received | |
| Notes | IRCT20141116019971N3. Recruitment January 2015 to January 2016. Authors declared no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated schedule was used by investigators to assign the patients into one of three groups by block randomization: Group A—20mg P.O. daily of citalopram, Group B—20mg P.O. daily of fluoxetine, and Group C—a placebo (microcrystalline cellulose)." |
| Allocation concealment (selection bias) | Low risk | Computer‐generated schedule confirmed with authors |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All of the drugs for each group of subjects were over‐encapsulated by a pharmacist." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Three evaluators were used in our study, namely, neurology residents who were blind to the interventions." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5/90 discontinued medication due to moving away‐but this would not have introduced because the reasons for missing data are unlikely to be related to the true outcome (Quote: "The main reason for participants leaving the study was noncompliance in terms of taking their drugs regularly (10 subjects stopped taking the treatment but completed their follow‐up), while five participants intentionally failed to attend follow‐up after two months because they were resident in other cities distant from the location of the study.") |
| Selective reporting (reporting bias) | Low risk | There was just one outcome measure planned (see reference on Iranian clinical trials register) and this was reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Bembenek 2020.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Actual enrolment 61 Allocation: randomised Intervention model: parallel assignment Masking: double (participant, care provider) Primary purpose: treatment |
|
| Participants | 61 participants Country: Poland Setting: inpatient At randomisation number allocated: N = 61: fluoxetine (n = 30); placebo (n = 31) % male: fluoxetine (73.3%); placebo (58.1%) Age: mean age: fluoxetine = 66.6 ± 12.6; placebo = 66.35 ± 12.46 Subtype of stroke
Severity of stroke: NIHSS, Median (IQR) fluoxetine (5 (3 to 8)); placebo (6 (4 to 8)) Inclusion criteria
Exclusion criteria
|
|
| Interventions | Fluoxetine 20 mg daily (1 capsule) for 6 months (180 capsules) vs placebo | |
| Outcomes | The primary outcomes at 6 months
Secondary endpoints
|
|
| Funding source | POLPHARMA S.A. manufactured and donated fluoxetine and placebo for this study. Anna Członkowska, Jan Bembenek, and Katarzyna Kurczych were supported by statutory activity of the Institute of Psychiatry and Neurology, Warsaw, Poland | |
| Notes | Recruitment 19 December 2014 and 13 March 201 8. Authors declared no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomly assigned in a 1:1 ratio to receive either fluoxetine or a placebo, by use of a computer‐based permuted block randomisation |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed (further information obtained from the study author Jan Bembenek to confirm this) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Clinicians involved in randomisation and outcome assessments, the patients, and their families, were all masked so as to be unaware of treatment allocation. The placebo capsules were visually identical to the fluoxetine capsules, even when broken open." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Clinicians involved in randomisation and outcome assessments, the patients, and their families, were all masked so as to be unaware of treatment allocation" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5 withdrew consent (8%) before 6 months but the withdrawals are balanced between groups (3 in the fluoxetine group and 2 in the control group) From personal communication with the author: a further 2 patients dropped out between 6 and 12 months |
| Selective reporting (reporting bias) | Low risk | Trial was registered and all outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Birchenall 2019.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Intervention model: parallel assignment Primary Purpose: treatment |
|
| Participants | 6 participants Country: France Setting: inpatient At randomisation number allocated: 6 although unclear as to which group % male: not available Age: not available Subtype of stroke: not available Severity of stroke: not available Time since stroke onset: not available Inclusion criteria
Exclusion criteria
Withdrawal criteria: not stated |
|
| Interventions | Experimental: fluoxetine; 1 pill of 20 mg/day, during 3 months Comparator: placebo of fluoxetine; 1 pill of 20 mg/day, during 3 months |
|
| Outcomes | Primary outcome
Secondary outcomes recorded at 3 and 6 months
|
|
| Funding source | Not stated | |
| Notes | No published data, unpublished data say 6 patients, none of whom died, so we have used this information Dates study conducted: February 2014 to August 2015 Declarations of Interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information available |
| Allocation concealment (selection bias) | Unclear risk | No information available |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information available |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information available |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information available |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Unclear risk | No information available |
Brown 1998.
| Study characteristics | ||
| Methods | Parallel design Analysis: per protocol: 1 withdrawn (treatment), excluded from analysis |
|
| Participants | Diagnosis: stroke, time from stroke to randomisation not reported Randomised 10 to treatment and 10 to control Treatment: 9 completed treatment, mean ± SD age 61.4 ± 8.6 years, 55% men Control: 10 people completed placebo, mean ± SD age 63.7 ± 5.4 years, 60% men Emotionalism criteria: emotionalism of at least 4 weeks' duration assessed during semi‐structured interview using a modified Lawson and MacLeod rating scale, in addition to frequency of outbursts Exclusion criteria: cognitive impairment, dysphasia, major depressive disorder |
|
| Interventions | Treatment: fluoxetine 20 mg daily Control: matched placebo Duration: 10 days Duration of follow‐up: (end of treatment to end of study) 0 |
|
| Outcomes | Used leaving the study early Unable to use data from HDRS, Lawson and MacLeod Scale, self‐rating scales (mean and SD not presented) Also reported emotional outbursts; we have not used these in our analyses AEs: not presented |
|
| Funding source | Funder not stated | |
| Notes | Dates of study not stated; conflicts of interest not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not stated |
| Allocation concealment (selection bias) | Unclear risk | Randomised by independent statistician |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | States blinding of patients and nursing staff, matched placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | States blinding of rating clinicians |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 1 withdrawn (5% of participants); we categorised this as low risk |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make judgement |
| Other bias | Low risk | No other obvious biases, baseline balanced |
Burns 1999.
| Study characteristics | ||
| Methods | Parallel design Analysis: ITT: 2 withdrawn and 1 death (treatment), 1 death (placebo), last value carried forward |
|
| Participants | Diagnosis: stroke. Months from stroke: median (range) 10.5 months (1 ± 156) in sertraline group and 5.5 months (1.5 ± 48) in the control group Treatment: 14 people Control: 14 people Exclusion criteria: less than 1 month since stroke, depression or dementia using the DSM III‐R criteria |
|
| Interventions | Treatment: sertraline 50 mg daily Control: matched placebo Duration: treatment continued for 8 weeks Duration of follow‐up: 2 weeks off treatment. All scores became non‐significant (though data not reported so could not be used in the analysis) |
|
| Outcomes | Able to use
Method of collecting AEs was not stated Unable to use: MADRS, BI, MMSE (data not presented) |
|
| Funding source | Funded by an unrestricted personal grant from Pfizer, the manufacturers of sertraline | |
| Notes | Dates of study not stated, conflicts of interest not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Blocks of 4 using list produced by medical statistics department |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Matched placebo, both active drug and placebo were packed in gelatine capsules with an identical appearance |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Run‐out was single‐blind, treatment was double‐blind, but unclear whether outcome assessors were blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analysis: ITT, LOCF 4/28 did not complete the study (14%) |
| Selective reporting (reporting bias) | Low risk | Trial details published on www.strokecentre.org/trials, although unable to use data from MADRS Given that the main aim was to explore effect on emotionalism, this is unlikely to have biased results |
| Other bias | Unclear risk | Placebo group younger, uncertain influence on bias Statistical analysis was carried out independently by the Applied Statistics Research Unit in Canterbury |
Cao 2020.
| Study characteristics | ||
| Methods | RCT Study type: interventional (clinical trial) Primary purpose: prevention |
|
| Participants | 100 participants January 2013 to April 2016 Country: China Setting: inpatient At randomisation number allocated: N = 99: escitalopram (n = 52); usual care (n = 47) % male: escitalopram (%); usual care (%) Inclusion criteria
Exclusion criteria
|
|
| Interventions | Experimental: prophylactic escitalopram in addition to the basic therapies. Started with 5 mg and gradually titrated to 10 mg/d, oral administration in the morning for 90 days Comparator: usual care. Secondary prevention of cerebral infarction, brain protection therapy and rehabilitation, without any antidepressants. People with difficulty sleeping could receive Zolpidem or benzodiazepines for a short period of time |
|
| Outcomes | Primary and secondary outcome measures not stated
|
|
| Funding source | ||
| Notes | No trial registration information Dates study conducted: All patients were hospitalised patients treated for acute ischaemic stroke from January 2013 to April 2016 Declarations of Interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available to permit a judgement of ‘low risk’ or ‘high risk’. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Control group did not receive a placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Treatment evaluation conducted by a physician blind to patient’s clinical data, but it does not state whether the physician was blind to treatment allocation. So the judgement was that the risk of bias was unclear |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There are two publications‐the numbers initially included in the two papers do not match; also two patients out of 49 randomised to escitalopram dropped out. Given the inconsistency in the numbers reported, we judge that there is the potential for high risk of bias |
| Selective reporting (reporting bias) | Unclear risk | No protocol is available |
| Other bias | Unclear risk | The authors did not reply to questions and so we have graded this as unclear |
Chen 2001.
| Study characteristics | ||
| Methods | Randomised trial Aim: to observe effects of integrative Chinese herb YuLeShu and fluoxetine on the depressive symptoms and rehabilitation of neurological impairment in patients with post‐stroke depression |
|
| Participants | Country: China Setting: not described Participants: internal carotid system cerebral infarction or haemorrhage within previous 2 months Fluoxetine: 19 people, mean age 61.71 ± 8.13 years, 8 men Control: 18 people, mean age 62.85 ± 7.32 years, 7 men Depression: diagnosis of depression according to DSM‐IV Inclusion criteria: HDRS ≥ 20 but < 35 and/or Zung SDS ≥ 41 Exclusion criteria: HDRS > 35, previous depression, aphasia, severe cardiac, pulmonary, hepatic and renal diseases, previous stroke |
|
| Interventions | 3 groups: fluoxetine plus usual care versus YuLeShu plus usual care versus usual care. We are using the fluoxetine plus usual care versus usual care alone in the comparison | |
| Outcomes | HDRS Zung SDS BI Scandinavian Neurological Stroke Scale (also known as CSS) Stated no side effects, but not clear which side effects were sought, or how they were sought. They were reported at 4, 8 and 12 weeks after treatment |
|
| Funding source | Funded by a local scientific academic fund, drug company not involved | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "using a computer", but method not described. Insufficient information about the sequence generation process available to permit a judgement of ‘low risk’ or ‘high risk' |
| Allocation concealment (selection bias) | Unclear risk | The method of concealment is not described or not described in sufficient detail to allow a definite judgement of ‘low risk’ or ‘high risk’ |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information about blinding of outcome assessment available to permit a judgement of ‘low risk’ or ‘high risk’ |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropouts: 2 people dropped out of the fluoxetine group, 1 dropped out of the YuLeShu group and 2 dropped out of the control group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not published. Insufficient information available to permit a judgement of ‘low risk’ or ‘high risk’ |
| Other bias | Unclear risk | Reported that of the people who completed the tests, there were no differences in baseline No comment on whether there were differences in baseline for the entire group |
Chen 2002.
| Study characteristics | ||
| Methods | Parallel group (3 groups: doxepin, paroxetine, placebo; we used the paroxetine and placebo data in our review) Aim: treat depression and determine effect on neurological function |
|
| Participants | Country: China Setting: unclear Stroke diagnosis: diagnostic criteria of the 4th National Meeting of the Cerebrovascular Diseases proved by CT or MRI Time since stroke: not known Depression diagnosis: Classification and Diagnosis of Psychosis in China (2nd edition) Treatment: 24 people, age and gender not given Control: 24 people, age and gender not given Exclusion: pre‐stroke mental disease, cognition disorder (MMSE < 24), marked deterioration in depression during treatment (HAMD > 24) or suicide mood, intolerance to drug |
|
| Interventions | Treatment: paroxetine 20 mg 3 times per day Control: placebo guvitamine once per day Duration of treatment: 8 weeks Duration of follow‐up (post‐treatment to study end): unclear: follow‐up is performed 'after treatment' so we assume this is at 8 weeks (so post‐treatment to study end = 0) |
|
| Outcomes | HAMD BI CSS Death/side effects/leaving the trial early Method of reporting side effects not stated |
|
| Funding source | Funder not stated, unclear if there was drug company involvement | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information about the sequence generation process available to permit a judgement of ‘low risk’ or ‘high risk’ |
| Allocation concealment (selection bias) | Unclear risk | The method of concealment is not described to allow a definite judgement of ‘low risk’ or ‘high risk’ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information available to permit a judgement of ‘low risk’ or ‘high risk’ |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information about blinding of outcome assessment available to permit a judgement of ‘low risk’ or ‘high risk’ |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropouts: 4 in placebo and 0 in paroxetine |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available to permit a judgement of ‘low risk’ or ‘high risk’ |
| Other bias | Unclear risk | Demographic data not provided, so we cannot determine whether the baseline was balanced |
Chen 2005a.
| Study characteristics | ||
| Methods | To observe the changes of neurotransmitter in people with post‐stroke depression by using encephalofluctuography technology, and observe the effect of antidepression treatment on the activity of neurotransmitter | |
| Participants | 48 participants with post‐stroke depression | |
| Interventions | Treatment: 24 people received citalopram 20 mg plus usual care, or fluoxetine if side effects such as nausea, emesis Control: 24 people usual care alone |
|
| Outcomes | Encephalofluctuography technology Level of sympathin and 5‐hydroxytryptamine at 4 weeks and 3 months after treatment started |
|
| Funding source | Not stated | |
| Notes | No data from our endpoints of interest, so data not included in a meta‐analysis Recruitment March 2001 to December 2001 Conflicts of interest not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomly divided" but method not stated. Insufficient information about the sequence generation process available to permit a judgement of ‘low risk’ or ‘high risk’ |
| Allocation concealment (selection bias) | Unclear risk | The method of concealment is not described or not described in sufficient detail to allow a definite judgement of ‘low risk’ or ‘high risk’ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Unclear risk | Unclear |
Chen 2005b.
| Study characteristics | ||
| Methods | Parallel group Analysis: according to allocated treatment group |
|
| Participants | Country: China Setting: inpatient Stroke criteria: first ever stroke, onset time ≤ 7 days, haemorrhagic and ischaemic, clinical diagnosis plus confirmation by imaging (though not clear whether a stroke lesion had to be present), at least 1 limb with muscle power grade 3 or less, BI ≤ 50, no consciousness disturbance Mood criteria: HAMD > 16 Treatment: 40 people, mean age 63.5 years, 29 men Control: 38 people, mean age 65.8 years, 25 men No difference in baseline depression and BI between treatment and control group Excluded: severe cardiac, hepatic and renal organic diseases, psychiatric disorders |
|
| Interventions | Treatment: paroxetine 20 mg daily plus routine stroke medication, nerve nutritional agents, acupuncture and rehabilitation Control: routine stroke medication, nerve nutritional agents, acupuncture and rehabilitation Duration of treatment: 12 weeks Duration of follow‐up (post‐treatment to study end): 0 weeks |
|
| Outcomes | HAMD BI Death Number completing the trial AEs not reported |
|
| Funding source | No description of funding | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts: none |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | No obvious risks, baseline similar |
Chen 2015.
| Study characteristics | ||
| Methods | To investigate the effect of early antidepressant intervention on the acute depression and rehabilitation of neurological function after stroke | |
| Participants | 96 acute depression patients after stroke were selected and randomly divided into study group and control group. Stroke diagnosed according to the diagnostic criteria of stroke by the 4th Congress of Chinese Cerebrovascular Diseases, which requires both clinical and imaging criteria to be met. HAMD ≥ 17. Excluded patients with mental disorders. Range of disease: 2‐9 months | |
| Interventions | The study group orally took the antidepressant ( citalopram) and the control group took placebo for 8 weeks | |
| Outcomes | Depression (HAMD), neurological function (NIHSS), ADL (BI). Substance P and neuropeptide Y | |
| Funding source | No information regarding funding | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Information not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Information not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | information not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | information not provided |
| Selective reporting (reporting bias) | Unclear risk | Information not provided |
| Other bias | Unclear risk | No information provided e.g. on source of funding |
Cheng 2003.
| Study characteristics | ||
| Methods | Parallel design Aim: to treat depression and augment rehabilitation Analysis: according to allocated treatment group |
|
| Participants | Location: China Setting: inpatient Treatment: 25 people Control: 32 people Whole group (including non‐depression group, depression control group and depression treatment group): 132 (mean age 62 ± 12 years, 79 men) Stroke: ischaemic stroke or PICH, clinical diagnosis plus confirmation on brain imaging (not clear that a stroke lesion had to be present), clear consciousness Depression diagnosis (at 2 weeks after stroke onset): psychiatric interview, DSM IV criteria Excluded: major psychological trauma history in previous 1 year, severe mental retardation, severe impairment of lingual expression or comprehension, major complicated medical event in previous 1 year |
|
| Interventions | Treatment: fluoxetine 20 mg daily Control: no fluoxetine Duration of treatment: 6 months Duration of follow‐up (post‐treatment to study end): 6 months |
|
| Outcomes | SSS ADL HAMD Zung SDS Zung SAS No deaths, none left trial early No data on AEs |
|
| Funding source | No description of funding | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 59 participants were diagnosed to have depression by symptoms but only 57 were included in the results table |
| Selective reporting (reporting bias) | High risk | No protocol, no report of the results of the self‐rating anxiety scale |
| Other bias | Unclear risk | No clear description of differences between the treatment and control group |
Chollet 2011.
| Study characteristics | ||
| Methods | Randomised parallel‐group trial | |
| Participants | Location: France Setting: stroke units Inclusion criteria: aged 18 to 85 years with FMMS of 55 or less, acute ischaemic stroke with hemiparesis or hemiplegia, 5 to 10 days after stroke onset, unclear if there had to be a visible lesion on brain imaging Treatment: 59 people, mean ± SD age 66.4 ± 11.7 years; 63% men Control: 59 people, mean ± SD age 62.9 ± 13.4 years; 59% men Comparability of treatment groups: total FMMS score fluoxetine 17.1 compared with 13.4 in placebo Previous stroke more common in the fluoxetine group; fluoxetine group had more diabetes Exclusions: clinical depression or treatment with antidepressants, MADRS > 19, aphasia severe enough to mask detection/assessment of depression, pregnancy, patient on neuroleptics/benzodiazepines, owing to undergo carotid endarterectomy, other major diseases that would prevent follow‐up |
|
| Interventions | Treatment: fluoxetine 20 mg daily for 90 days Control: identical capsules to active drug Duration of treatment: 90 days Duration of follow‐up (treatment end to study end): 0 days |
|
| Outcomes | Primary outcome: the mean change of FMMS score between inclusion (day 0) and day 90 after the start of the study drug Secondary endpoints were NIHSS, mRS and MADRS measured at days 0, 30 and 90 |
|
| Funding source | Funded by French national programme for clinical research: the sponsor had no involvement in study design, data collection, data analysis, data interpretation or writing the report | |
| Notes | Recruitment 14 March 2005 to 9 June 2009. Authors state "no conflicts of interest" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Balanced by centre with an allocation based on a block size of 4 generated with a computer random‐number generator |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Identical capsules for control arm |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All study site investigators and all investigators were masked to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts: 2 participants died (1 in each group) and 3 dropped out; not stated how missing outcome data were dealt with |
| Selective reporting (reporting bias) | Low risk | Trial protocol published on www.strokecentre.org/trials, all outcomes were reported |
| Other bias | Unclear risk | Note difference in baseline; particularly for the total FMMS score (17.1 in fluoxetine and 13.4 in the placebo): it is not clear what effect this had on results, so we have classified this as 'unclear risk' |
Dam 1996.
| Study characteristics | ||
| Methods | Parallel design Analysis: per protocol: withdrawn because of AEs (2 treatment), all excluded from analysis |
|
| Participants | Location: Italy Setting: unclear Treatment: 18 people, mean ± SD age 68 ± 9 years, 44% men Control: 17 people, mean ± SD age 68 ± 5.5 years, 44% men Stroke criteria: ischaemic, unilateral MCA territory stroke, diagnosis via clinical signs and CT (100%), stroke 1 to 6 months prior to randomisation (average time 3 months) Other inclusion criteria: unable to walk Comparability of treatment groups: balanced Exclusion: history of major affective disorders; alcohol abuse; or a history or evidence or both of severe heart, lung, kidney or liver diseases or mental deterioration |
|
| Interventions | Treatment: fluoxetine 20 mg daily Control: matched placebo Duration: treatment continued on average 74 ± 6 days, duration not reported for control group Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | Depression: change in scores from baseline to end of treatment on HDRS Additional: graded neurological scale (HSS), BI Leaving the study early Death AEs including seizures ‐ unclear if these were reported systematically |
|
| Funding source | Funding source not stated | |
| Notes | Dates of recruitment and conflicts of interest not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Examining neurologists blind to treatment". Comment: Unclear if this refers to outcome assessors or the neurologist caring for the participant. However, placebo was 'matched' so this is low risk as the treating physician and the participants would have been blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | See above |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2/35 dropouts (5.7%), per‐protocol analysis |
| Selective reporting (reporting bias) | Low risk | Trial available, including results on www.strokecentre.org/trials: all specified outcome measures were reported |
| Other bias | Low risk | Baseline characteristics similar in the 2 groups |
Dike 2019.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Allocation: randomised Intervention model: parallel assignment Masking: single (investigator) Primary purpose: treatment |
|
| Participants | 60 participants Country: Nigeria Setting: inpatient At randomisation number allocated: N = 1500: fluoxetine (n = 750 ); placebo (n = 750 ) % male: fluoxetine (53.3%); placebo (43.3%) Age: mean age: fluoxetine = 59 ± 11; placebo = 62 ± 9 Inclusion criteria
Exclusion criteria
|
|
| Interventions | Experimental: 20 mg fluoxetine for 30 days plus standard treatment Comparator: standard treatment |
|
| Outcomes | Primary outcome
Secondary outcomes
|
|
| Funding source | N o funding | |
| Notes | PACTR201412000967245. Recruitment between January 2015 and May 2016. All authors declare no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Block randomization was used in the assignment of study participants. Permuted blocks of six (6) for two groups were drawn up. A random selection of possibilities was done using a list of random numbers generated with STATA 12." |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation concealment was done using sequentially numbered envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "This was a single‐blind randomized controlled trial that compared motor recovery between 2 groups of stroke patients: those on fluoxetine 20mg daily + standard therapy; and the control group who received standard therapy only." Thus the participants would have known their treatment allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 22/60 lost to follow‐up (presumably including the 7 in the intervention group and the 8 in the control group who died). 6 in fluoxetine group stopped treatment but were still included in the analysis. It is unclear what effect this would have had, hence the judgement about unclear risk of bias |
| Selective reporting (reporting bias) | Low risk | All the prespecified outcomes were reported |
| Other bias | Unclear risk | Insufficient information to to assess whether an important risk of bias exists |
EFFECTS 2020.
| Study characteristics | ||
| Methods | Multicentre RCT Study type: interventional (clinical trial) Allocation: randomised Intervention model: parallel assignment Masking: quadruple (participant, care provider, investigator, outcomes assessor) Primary purpose: treatment |
|
| Participants | 1500 participants Country: Sweden Setting: inpatient At randomisation number allocated: N = 1500: fluoxetine (n = 750 ); placebo (n = 750 ) % male: fluoxetine (62%); placebo (62%) Age: mean age: fluoxetine = 70.6 ± 11.3; placebo = 71.0± 10.5 Subtype of stroke
Inclusion criteria
Exclusion criteria
|
|
| Interventions | Fluoxetine (20 mg once daily) for 6 months with oral capsules | |
| Outcomes | Outcomes collected at 6 months and 12 months Primary outcome
Secondary outcomes
|
|
| Funding source | The Swedish Research Council, the Swedish Heart‐Lung Foundation, the Swedish Brain Foundation, the Swedish Society of Medicine, King Gustav V and Queen Victoria’s Foundation of Freemasons, and the Swedish Stroke Association (STROKE‐Riksförbundet) | |
| Notes | clinicaltrials.gov/ct2/show/NCT02683213. Recruitment between Oct 20, 2014, and June 28, 2019 BN has received honoraria for data monitoring committee work in the SOCRATES and THALES trials (AstraZeneca) and the NAVIGATE‐ESUS trial (Bayer). HW has received grants from the Swedish Medical Research Council (Vetenskapsrådet) during the conduct of the study; the grant was for the study that is presented inthe submitted manuscript. GJH has received grants from the National Health and Medical Research Council (NHMRC) of Australia, Vetenskapsrådet, and UK National Institute for Health Research Technology, during the conduct of the study; and personal fees from American Heart Association, outside of the submitted work. MD reports that the University of Edinburgh received some funding from the grants for EFFECTS (Vetenskapsrådet) in relation to its provision of a randomisation system. MLH has received grants from the NHMRC of Australia, outside of the submitted work. All other authors declare no competing interests |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A physician or nurse entered patients’ baseline data into a secure web‐based randomisation system. The system checked the data for completeness and consistency and allocated each patient an identification number and a treatment number. Patients were randomly assigned in a 1:1 ratio to either oral fluoxetine 20 mg once daily or placebo for 6 months." |
| Allocation concealment (selection bias) | Low risk | Quote: "secure web‐based randomisation system" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Patients, their families, health‐care personnel, investigators, outcomes assessors, and staff in the coordinating centre (Karolinska Institutet, Department of Clinical Sciences Danderyd Hospital, Stockholm, Sweden), and the pharmacy were masked to treatment allocation. The placebo capsules were visually identical to the fluoxetine capsules, even when broken open. The success of the masking procedure was not assessed. An emergency unmasking system was available but was designed so that the coordinating centre and staff doing follow‐up continued to be masked throughout the study." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Patients, their families, health‐care personnel, investigators, outcomes assessors, and staff in the coordinating centre (Karolinska Institutet, Department of Clinical Sciences Danderyd Hospital, Stockholm, Sweden), and the pharmacy were masked to treatment allocation" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 11 dropped out; 2 crossed over; the rest were included in the analysis |
| Selective reporting (reporting bias) | Low risk | All outcomes that were prespecified were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Feng 2004.
| Study characteristics | ||
| Methods | Aim: to study the influence of Jieyu Huoxue decoction on rehabilitation of patients with depression after cerebral infarction | |
| Participants | Country: China 4 groups: fluoxetine plus usual care, Jieyu Huoxue decoction plus usual care, usual care in people with depression, usual care in people with no depression We are using data from 'fluoxetine plus usual care' versus 'usual care in people with depression' Setting: mixed inpatient and outpatient Stroke criteria: ischaemic stroke within 1 month of stroke onset, clinical diagnosis plus confirmation by imaging. Did not state whether a visible lesion was needed to make a diagnosis Depression: psychiatric interview using DSM IV, Zung SDS ≥ 41 Included those with no previous psychiatric history 54 participants with post‐stroke depression were randomised 18 received fluoxetine plus usual care, 18 received usual care only and 18 received Jieyu Huoxue decoction Of the 54 participants with depression randomised, mean age: 71.5 ± 6.7 years, 24 men Excluded: previous stroke, previous depression, and severe cardiac, pulmonary, hepatic and renal diseases |
|
| Interventions | Treatment: fluoxetine 20 mg daily plus usual stroke care Control: usual stroke care Duration of treatment: 60 days Duration of follow‐up (post‐treatment to study end): 0 weeks |
|
| Outcomes | Zung SDS ADL: although score not referenced, so not used in analysis MESSS Reported side effects in fluoxetine group but not in the control group Unclear how side effects were collected |
|
| Funding source | Funding source not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 8 participants dropped out (2 in fluoxetine group, 2 in the depression control group, 1 in the Jieyu Huoxue decoction, 3 in no‐depression control) |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Baseline balanced |
FOCUS 2019.
| Study characteristics | ||
| Methods | Multicentre RCT Study type: interventional (clinical trial) Primary purpose: treatment |
|
| Participants | 3127 participants Country: UK Setting: inpatient At randomisation number allocated: N = 3127: fluoxetine (n = 1564); placebo (n = 1563) % male: fluoxetine (62%); placebo (61%) Age: mean age: fluoxetine = 71·2 ± 12.4; placebo = 71·5 ± 12.1 Subtype of stroke
Severity of stroke: NIHSS, Median (IQR) fluoxetine (6 (3 to 11)); placebo (6 (3 to 11)) Time since stroke onset: mean days: fluoxetine 6.9 ± 3.6; placebo 7.0 ± 3.6 Inclusion criteria
Exclusion criteria
|
|
| Interventions | Experimental: 20 mg orally once daily for 6 months Comparator: matching placebo orally once daily for 6 months |
|
| Outcomes | Primary outcome
Secondary outcome measures
|
|
| Funding source | MHRA approval granted. Start‐up phase funded by The Stroke Association. Main phase funded by NIHR | |
| Notes | ISRCTN83290762. Recruitment 10 September 2012 to 31 March 2017. Authors declared no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly assigned in a 1:1 ratio to receive fluoxetine or placebo, by use of a centralised randomization system." |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomly assigned in a 1:1 ratio to receive fluoxetine or placebo, by use of a centralised randomization system." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Patients, their families, and the health‐care team including the pharmacist, staff in the coordinating centre, and anyone involved in outcome assessments were all masked to treatment allocation by use of a placebo capsule that was visually identical to the fluoxetine capsules even when broken open." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Patients, their families, and the health‐care team including the pharmacist, staff in the coordinating centre, and anyone involved in outcome assessments were all masked to treatment allocation by use of a placebo capsule that was visually identical to the fluoxetine capsules even when broken open." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | For the primary outcome of mRS at 6 months data were available for fluoxetine n = 1553/1564 (99.3%) and placebo n = 1553/1563 (99.3%) |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all of the study's prespecified (primary and secondary) outcomes that are of interest in the review have been reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Fruehwald 2003.
| Study characteristics | ||
| Methods | Parallel design Analysis: per protocol Withdrawals: death (1 treatment), withdrawn owing to AEs (1 treatment, 2 control), all excluded from analysis |
|
| Participants | Location: Austria Setting: inpatients Treatment: 28 people, mean ± SD age 65 ± 14 years, 46% men Control: 26 people, mean ± SD age 64 ± 14 years, 71% men Stroke criteria: ischaemic stroke and PICH; diagnosis via clinical signs and CT (100%); stroke on average 11 days prior to randomisation Depression criteria: psychiatric interviews, HDRS score > 15 Other entry criteria: not stated Comparability of treatment groups: non‐significant trend towards more women and right‐sided strokes in treatment group Exclusion criteria: MMSE < 20, more than mild communication deficit, diseases of the central nervous system and previous neurodegenerative or expansive neurological disorders |
|
| Interventions | Treatment: fluoxetine 20 mg daily, dose escalation at 4 weeks if HDRS score > 13 Control: matched placebo Duration of treatment: 12 weeks Duration of follow‐up (end of treatment to study end): 15 months |
|
| Outcomes | Depression: change in scores from baseline to end of treatment of HDRS, BDI, and CGI (item 1) Proportion of responders (< 13 HDRS) Additional: SSS Death AEs (selected data) Unable to use: RS, BI, MMSE (data not presented at follow‐up) AEs data on dizziness, nausea and cephalalgia (data not presented by group) |
|
| Funding source | The medication was supplied by Lannacher Heilmittel, Lannach, Austria | |
| Notes | Recruitment 1 June 1998 to 31 Decmeber 1998. Conflicts of interest not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation, using random permutated block design |
| Allocation concealment (selection bias) | Low risk | Centralised concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | States blinded, used matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | States blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4/54, per protocol analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Baseline balanced All participants were randomly assigned to either fluoxetine or placebo treatment by the drug company independently of the research teams and the study centres |
Gao 2017.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Primary purpose: treatment |
|
| Participants | 274 participants Country: China Setting: outpatient At randomisation number allocated: N = 274, citalopram (n = 91); placebo (n = 91); cognitive behavioural therapy (n = 92) % male: 51.8% Age: mean age, citalopram 66.0 ± 7.3 (n = 91); placebo 67.2 ± 9.6 (n = 91); cognitive behavioural therapy 64.9 ± 8.0 (n = 92) Subtype of stroke: not available Severity of stroke: not available Time since stroke onset: acute ischaemic stroke within the previous 7 days Inclusion criteria
Exclusion criteria
|
|
| Interventions | Experimental: citalopram 20 mg per day for a minimum of 3 months + general discussions Comparator 1: placebo + general discussions Comparator 2: placebo + cognitive behavioural therapy |
|
| Outcomes |
|
|
| Funding source | Natural Science Foundation of China [81100243, 81171131, 81272564, 81272795, 81100893, 81172197, and 81372484], the Natural Science Foundation of Liaoning Province in China [No. L2013296], and Liaoning Science and Technology Plan Projects [No. 2011225020] | |
| Notes | This trial was particular in that recruitment happened at 4 different time points: at 0 months, 3 months, 6 months, and 9 months from discharge. Inclusion criteria required that participants suffered from post‐stroke depression. Participants were invited to complete the BDI and those with a score > 10 were included, provided other criteria were met Group 'placebo + general discussions' and 'citalopram + general discussions were included. No significant differences observed in the 2 included groups Dates study conducted: participants enrolled between October 2011 and June 2013 Declarations of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization into one of three intervention groups was undertaken by an independent researcher using computer‐generated random number sequences ..." |
| Allocation concealment (selection bias) | Low risk | Quote: "... that were prepared in advance and placed in consecutively numbered, sealed, opaque envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Study described as "single blind" Quote: "The researcher successively opened the envelopes corresponding to different time periods and determined the intervention by patient number." Quote: "The study therapists acted as clinical evaluators." Quote: "The study therapists were asked not to divulge any treatment information to their patients." Comment: Care providers, investigator and outcome assessors were all aware of allocation |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "The study therapists acted as clinical evaluators." Quote: "The study therapists were asked not to divulge any treatment information to their patients." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "in Group A [placebo + general discussions], one patient violated protocol in the second time period, one could no longer be reached, and one left the study owing to stroke recurrence in the third time period; in Group B [citalopram + general discussions], persistent side‐effects from the drugs led five patients to leave the study (two owing to orthostatic dizziness, one owing to palpitation, and two owing to constipation)" Comment: Attrition reported for each intervention group and reasons given Group A (placebo + general discussions) 3/91 = 3% attrition Group B (citalopram + general discussions) 5/91 = 5% attrition Overall = 4% attrition |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol available. Therefore insufficient information to judge high or low |
| Other bias | Low risk | The study appears to be free from other sources of bias |
GlaxoSmithKline 1998.
| Study characteristics | ||
| Methods | Parallel group Analysis: according to treatment group |
|
| Participants | Location: not stated Setting: not stated Stroke criteria: "documented diagnosis of stroke within 12 months prior to screening" Mood: MADRS score > 17 Treatment: 112 people, age 64.3 ± 11.4 years, 61 men Control: 117 people, 65.6 ± 10.5 years, 64 men Excluded: concurrent psychiatric disorders, concurrent psychotropic pharmacotherapy, patients who posed a suicidal risk, patients with substance abuse/dependence, concurrent psychotropic pharmacotherapy, MMSE < 24, participating in another clinical trial, serious medical condition or clinically significant finding on screening or baseline evaluation that would preclude the administration of paroxetine and an intolerance to paroxetine |
|
| Interventions | Treatment: paroxetine 20 to 50 mg daily Control: placebo (not stated whether matching) Duration of treatment: 8 weeks Duration of follow‐up (treatment to study end): 0 weeks |
|
| Outcomes | Change from baseline to endpoint in MADRS Proportion of participants scoring < 8 on the MADRS total score at the endpoint (we used this in our analysis) Changes from baseline to endpoint on the BI Change from baseline to endpoint on RS score Change from baseline to endpoint on the Clinical Global Improvement Severity of Illness Score (CGI‐S Proportion of responders based on CGI‐Global Improvement (CGI‐G) score (score of < 4) at endpoint GI side effects reported, but unclear whether these are 'events' or 'participants', so we cannot use these data. It is not clear how the side effects were collected Withdrawal from study |
|
| Funding source | Source of funding not stated, but we assume it was funded by GlaxoSmithKline | |
| Notes | Study period 29 August 1998 to 15 October 1999. Conflicts of interest not stated. Study number PAR625. Date updated: 11 March 2005 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not described |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment: not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding not described, used placebo but not stated whether identical |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 20 in each group dropped out |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Insufficient information to make clear judgement |
Gong 2020.
| Study characteristics | ||
| Methods | RCT Study type: interventional (clinical trial) Allocation: randomised Intervention model: parallel assignment Masking: double (participant, outcomes assessor) Primary purpose: treatment The study was designed as a double‐blind, randomized clinical trial in order to obtain evidence for using Shu‐Gan‐JieYu capsule as an integrative, anti‐depressive treatment for motor recovery in post‐stroke patients |
|
| Participants | 254 participants Country: China Setting: inpatient At randomisation number allocated: N = 254: Group A (Shu‐Gan‐Jie‐Yu only (n = 64), Group B (fluoxetine n = 64), Group C (Shu‐Gan‐Jie‐Yu and fluoxetine (n = 64)), and Group D (placebo (n = 62)) % male: Group A (Shu‐Gan‐Jie‐Yu only (n = 68.5%), Group B (fluoxetine n = 64.2%), Group C (Shu‐Gan‐Jie‐Yu and fluoxetine (n = 67.3%)), and Group D (placebo (n = 61.0%)) Age: mean age: Group A (Shu‐Gan‐Jie‐Yu only (58.36 ± 15.28), Group B (fluoxetine 56.68 ± 17.59), Group C (Shu‐Gan‐Jie‐Yu and fluoxetine (55.95 ± 19.66), and Group D (placebo (57.79 ± 17.54) Inclusion criteria
Exclusion criteria
|
|
| Interventions | Group A (Shu‐Gan‐Jie‐Yu only), Group B (fluoxetine), Group C (Shu‐Gan‐Jie‐Yu and fluoxetine), and Group D (placebo) | |
| Outcomes | mRS: categorised as (0&1), (2&3), (> 4) Fugl‐Meyer: continuous |
|
| Funding source | Supported by a grant from The National Natural Science Foundation of China (81373619) and the Plateau Discipline of Neurology of Integrated Traditional Chinese and Western Medicine in Pudong New Area (PDZY‐2018‐0606) | |
| Notes | No trila registration number. Recruitment from July 2015 to December 2018. The authors declare that they have no conflicts of interest Please note: final per protocol number stated as 222, but Table 2 baseline only includes 219; Table 2 mRS n=291; Table 3 30 & 90 days n=222 Denominators change for each outcome – even different for mRS 90 day and Fugel‐Meyer 90 day |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Simple randomization method … computer‐generated schedule to assign the patients who met the criteria into one of four groups by block randomization, in a ratio of 1:1:1:1, without stratification" |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment is not described to allow a definite judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All capsules looked identical ... in order to guarantee the consistency of capsule appearance. All of the patients were told the effects of the drugs ... could improve motor recovery even if they did not have a depressive disorder." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Three neurology residents who were blinded to the interventions served as eva‐ luators in the study. The evaluators obtained the patients’ FMMS and mRS scores at enrollment and follow‐up on day 30 and day 90 after the start of the intervention. They also recorded any adverse events observed during the study." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Final per protocol number stated as 222, but Table 2 baseline only includes 219; Table 2 mRS n = 291; Table 3 30 and 90 days n = 222. Denominators change for each outcome – and are different for mRS 90 day and Fugel‐Meyer 90 day |
| Selective reporting (reporting bias) | Unclear risk | No published protocol to cross check for selective reporting |
| Other bias | High risk | Non‐standard analysis of outcomes |
Guo 2009.
| Study characteristics | ||
| Methods | Parallel group, 3‐arm trial, comparing sertraline plus routine care versus routine care versus acupuncture plus routine care. We are using the sertraline plus routine care versus routine care in this review Aim: to treat depression Analysis: according to allocated treatment |
|
| Participants | Country: China Setting: unknown Stroke criteria: first ever stroke, clinical diagnosis plus relevant lesion on imaging, age ≥ 60 years old Depression criteria: HAMD score ≥ 8, no depression prior to stroke Treatment: 40 people, mean age 67.6 ± 12.43 years, 23 men Control: 40 people, mean age 64.5 ± 12.07 years, 22 men Exclusions: psychiatric disorders or family psychiatric disorders, severe cognitive impairment, global aphasia, sensory aphasia, apraxia, severe cardiac, hepatic, renal, lung or other severe somatic disorder, consciousness disturbance, severe deafness, family or patient unable to comply |
|
| Interventions | Treatment: sertraline 50 mg daily plus stroke care (acute, secondary prevention, rehabilitation and psychotherapy) Control: stroke care (acute, secondary prevention, rehabilitation and psychotherapy) Duration of treatment: 6 weeks Duration of follow‐up: (treatment end to study end): 6 months |
|
| Outcomes | HAMD NIHSS FIM (reported cognition and mobility scores only) SF‐36 AEs not reported |
|
| Funding source | Funded by a local scientific academic fund | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐number table |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts, analysed by allocated treatment |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Low risk | No obvious risk, balance baseline |
He 2004.
| Study characteristics | ||
| Methods | Parallel group Analysis: according to treatment allocation |
|
| Participants | Location: China Setting: inpatient Inclusion criteria: all pathological types of stroke, clinical diagnosis plus confirmation by imaging (did not state that a visible lesion was needed to make the diagnosis), first ever stroke Depression diagnosis: 'HAMD scores'. Translation of paper: did not have to have depression at recruitment Treatment: 36 people, mean age 70.8 ± 6.7 years, 25 men Control: 35 people, mean age 70.4 ± 6.8 years, 23 men Exclusion: psychiatric disorders, dysphasia, consciousness disturbance, agnosia, severe dementia |
|
| Interventions | Treatment: fluoxetine 20 mg daily plus usual stroke care Control: usual stroke care Duration of treatment: 8 weeks Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | HAMD SSS No description of how side effects were collected |
|
| Funding source | Funded by local scientific academic fund | |
| Notes | Reported that there were no AEs, so we have assumed no seizures or GI side effects | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Outcome assessors blind" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 13 dropped out after randomisation |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Low risk | Balanced baseline, no obvious risks |
He 2005.
| Study characteristics | ||
| Methods | Parallel design. 3 groups: paroxetine, paroxetine plus psychotherapy, control. We are using paroxetine and control data in this review Analysis: according to treatment group |
|
| Participants | Location: China Setting: inpatient Stroke criteria: first ever stroke; ischaemic and haemorrhagic, timing: "acute", clinical diagnosis plus confirmation by imaging (though not clear whether a stroke lesion had to be present or not) Mood criteria: meets ICD‐10 organic depression and organic anxiety diagnostic criteria on psychiatric interview, HAMD score ≥ 17 and HAMA score ≥ 14 Treatment: 27 people, mean age 62.4 ± 6.1 years, 14 men Control: 27 people, mean age 63.2 ± 5.7 years, 16 men Exclusion: previous psychiatric disorder, antidepressants and "nerve block agents" in recent 3 months, severe cognitive impairment, aphasia, severe cardiac, hepatic and renal function impairment, allergy to paroxetine, severe suicidal behaviour |
|
| Interventions | Treatment: paroxetine 20 mg plus routine stroke treatment Control: routine stroke treatment Duration of treatment: 6 weeks Duration of follow‐up: end of treatment to study end: 0 |
|
| Outcomes | SSS BI HAMD HAMA TESS Also reported GI upset and dizziness. They did not list any seizures in the list of AEs, so we are assuming no seizures in either groups Unclear how side effects were collected |
|
| Funding source | Funded by a local scientific academic fund | |
| Notes | The authors mentioned using the SDS and the SAS for evaluation, but they did not report the results of SDS and SAS | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts, analysed according to treatment group |
| Selective reporting (reporting bias) | High risk | No protocol, the authors mentioned using the SDS and the SAS for evaluation but they did not report the results |
| Other bias | Low risk | Balanced baseline |
He 2016.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Primary purpose: prevention |
|
| Participants | 374 participants Country: China Setting: inpatient At randomisation numbers allocated: N = 300 Experimental group 1: fluoxetine immediately after enrolment n = 100; comparator group 1: fluoxetine 7 days after enrolment n = 100; comparator group 2: no fluoxetine n = 100 % male: unclear Age: experimental, unclear; comparator 1, unclear; comparator 2, unclear Subtype of stroke: unclear Severity of stroke NIHSS score at baseline: unclear Experimental: unclear Comparator 1: unclear Comparator 2: unclear Time from stroke onset: within 1 week after onset of cerebral infarction Inclusion criteria
Exclusion criteria
Withdrawal criteria
|
|
| Interventions | Experimental: 20 mg of fluoxetine a day for 90 days and conventional therapy Comparator: conventional therapy |
|
| Outcomes | Primary outcome at days 15, 90 and 180
Secondary outcome at days 90 and 180
|
|
| Funding source | This study was funded by Science and Technology Department of Guangdong, China (grant number: 2011B031800130), Science and Technology Innovation Committee of Shenzhen, China (grant number: 201101020), and Health and Family Planning Committee of Shenzhen, China (grant number: 201501009). It was registered on the Chinese Clinical Trial Registry (number: ChiCTR‐TRC‐12002078) | |
| Notes | Dates study conducted: unclear. Either from June 2011 to December 2012 (ChiCTR‐TRC‐12002078) or from December 2015 to June 2016 (ChiCTR‐IPR ‐ 15007658) Declarations of Interest: none reported Trial registration detail (ChiCTR‐TRC‐12002078) does not match but rather matches ChiCTR‐IPR ‐ 15007658. Baseline demographic and clinical characteristics for each group not presented, but rather the baseline demographic and clinical characteristics for those completing the trial (i.e. a subset of all those randomised at baseline) are presented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information on method of allocation concealment to judge high or low |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement of high or low |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The evaluator was banned from participation in the treatment or from querying of the randomisation data." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | For the primary outcome of NIHSS score at 15, 90 and 180 days there was 8/187 (4%) lost to follow‐up in the experimental group; 16/187 (15%) in the comparator group. Twice as many participants in the comparator group (16/187(9%)) compared to the fluoxetine group (8/187 (4%)) were lost to follow‐up. Attrition and exclusions were not fully reported > 5% lost to follow‐up |
| Selective reporting (reporting bias) | High risk | The trial registration number/protocol does not match the study design presented, but rather matches ChiCTR‐IPR ‐ 15007658 |
| Other bias | High risk | The baseline data presented in table 1: comparison of data at baseline between control group and the treatment group are not true baseline characteristics (i.e. at randomisation). The data presented in table 1 are the baseline characteristics of all those completing the trial which is a subgroup of all participants randomised. We cannot tell if there is whether there was any baseline imbalance in important demographic or clinical characteristics |
Hu 2002.
| Study characteristics | ||
| Methods | Parallel design Aim: to study effect of antidepressants on depressive symptoms and nervous function |
|
| Participants | Country: China Setting: inpatient Stroke criteria: all pathological stroke types, clinical diagnosis plus confirmation by imaging (though unclear whether a relevant lesion had to be visible), onset of stroke 0.5 to 2 months, no obvious aphasia Depression: according to CCMD‐II‐R Treatment: 42 people, mean age 61.4 ± 3.6 years, 32 men Control: 30 people, mean age 60 ± 4.8 years, 23 men |
|
| Interventions | Treatment: fluoxetine 20 mg daily Control: no other antidepressant Duration of treatment: 8 weeks Duration of follow‐up (end of treatment to study end): 0 |
|
| Outcomes | HAMD MESSS However, these data were not usable, as they were reported as proportions above or below "decrement levels" Reported side effects but unclear how this was done None left the trial early |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Balanced baseline, no other obvious risks |
Hu 2018.
| Study characteristics | ||
| Methods | Aim: to explore the effect of escitalopram on the neural function and cognitive function of patients with post‐stroke depression RCT |
|
| Participants | 82 stroke patients selected who were in hospital from October 2016 to October 2017. Met diagnostic criteria for stroke. Both haemorrhagic and ischaemic stroke included. Patients also met the diagnostic criteria of depression in Chinese classification of mental disorders; Patients did not take other antidepressants before; HAMD Score > 18 Exclusions: 1) patients with transient cerebral ischaemia, secondary cerebral ischaemia and cerebral infarction; 2) patients with haematological diseases, coagulation dysfunction, arteriovenous malformations; 3) patients with severe organ diseases, respiratory failure; 4) patients taking other antidepressants recently; 5) patients with severe depression and cognitive impairment; 6) patients allergic to the study drugs, and dropped out of the study |
|
| Interventions | Both groups were given usual medical care, the treatment group was given escitalopram oxalate tablets (H20103327, Shandong Jingwei Pharmaceutical Co., Ltd. 10mg*7 tablets) 10mg, once per day, for 12 weeks | |
| Outcomes | HAMD score NIHSS score MMSE score FIM score | |
| Funding source | Scientific research program of Shandong Provincial Department of Health (Funding number: 2012ws1783) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table method |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | No protocol available to check |
| Other bias | Unclear risk | Not described |
Huang 2002.
| Study characteristics | ||
| Methods | Parallel design Aim: efficacy and tolerance of fluoxetine in early post‐stroke depression Analysis: according to treatment group |
|
| Participants | Country: China Setting: inpatient Stroke criteria: first ever stroke, with single unilateral lesion, clinical diagnosis with imaging consistent with stroke, both ischaemic and haemorrhagic, recruited 2 weeks after stroke onset Depression criteria: CCMD II‐R depression diagnosis Treatment: 40 people, age and gender not stated Control: 40 people, age and gender not stated Participants in the treatment and control groups were selected from a group of 168 first‐ever acute stroke patients with average age of 62 ± 8.1 years, 76 men |
|
| Interventions | Treatment: fluoxetine 20 mg daily Control: placebo Duration of treatment: 4 weeks Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | HAMD CSS Did not report death Unclear how AEs were reported: no obvious AEs were found, but they did not specifically report seizures |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated |
| Allocation concealment (selection bias) | Unclear risk | Method not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Placebo used, but unclear if identical |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts, analysed according to treatment group |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | No description of the differences between treatment and control group in baseline characteristics |
Jia 2005.
| Study characteristics | ||
| Methods | Parallel design Aim: to determine the effect of early intervention for post stroke depression on movement after 3 months of stroke |
|
| Participants | Country: China Setting: inpatient Inclusion: aged 40 to 75 years, all pathological types of stroke, clinical diagnosis plus confirmation by imaging (did not state whether a relevant lesion had to be present to make a diagnosis), able to give informed consent Depression diagnosis: Zung SDS > 41 for screening for depression, HDRS for evaluation of the depression severity level Treatment: 92 people randomised, 90 accepted allocation, mean age 55.6 ± 6.5 years, 60 men Control: 92 people randomised, 90 accepted allocation, mean age 55.1 ± 6.8, 55 men Excluded: organic psychiatric disorders such as Alzheimer's disease or degenerative disease, functional disorders such as schizophrenia and affective disorders |
|
| Interventions | Treatment: either fluoxetine or sertraline (given sertraline if also had anxiety) plus routine stroke care Control: routine stroke care Duration of treatment: 3 months Duration of follow‐up: 3 years but the authors did not describe the extent of neurological function damage and HAMD scores in the third year |
|
| Outcomes | HAMD Extent of neurological damage Recurrent stroke Death Did not report AEs |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts: 6 in treatment group (2 refused allocation), 4 in control group (2 refused allocation) |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Balanced baseline |
Kim 2017.
| Study characteristics | ||
| Methods | Multicentre Study type: interventional (clinical trial) Intervention model: parallel assignment Primary purpose: prevention |
|
| Participants | 478 participants Country: South Korea Setting: inpatient. at neurology departments in 17 university hospitals throughout South Korea At randomisation number allocated: N = 478, escitalopram (n = 241); placebo (n = 237) % male at baseline: unclear Age at baseline: unclear Subtype of stroke at baseline: unclear Severity of stroke at baseline: unclear Time since stroke onset: acute ischaemic stroke or intracerebral haemorrhage within the previous 21 days Inclusion criteria
Exclusion criteria
Withdrawal criteria: not stated |
|
| Interventions | Experimental: escitalopram: first week 5 mg, 2nd week ~ 12 week: 10 mg Comparator: "sugar pill". First week 5 mg, 2nd week ~ 12 week: 10 mg |
|
| Outcomes | Primary outcomes collected at 3 months
Secondary outcomes
|
|
| Funding source | Dong‐A Pharmaceutical Company, grants from the Ministry for Health, Welfare, and Family Affairs, South Korea | |
| Notes |
NCT01278498 Baseline demographic and clinical characteristics for each group not presented, but rather the baseline demographic and clinical characteristics for those completing the trial (i.e., a subset of all those randomised at baseline) are presented Dates study conducted: January 2011 to December 2015 Declarations of Interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible patients were enrolled by investigators at each centre, and randomly assigned in a 1:1 ratio using a web‐based system to the escitalopram group or the placebo group after being assigned a subject number. Randomisation was done with random permuted blocks of sizes four to six, and was stratified by centre. The placebo was identical in appearance to escitalopram" |
| Allocation concealment (selection bias) | Low risk | Quote: "Eligible patients were enrolled by investigators at each centre, and randomly assigned in a 1:1 ratio using a web‐based system to the escitalopram group or the placebo group after being assigned a subject number. Randomisation was done with random permuted blocks of sizes four to six, and was stratified by centre" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The placebo was identical in appearance to escitalopram" Quote: "The individual treatment code was stored separately by the main medical statistician (E‐JL) and two designated statisticians. All investigators including interviewers and assessors of the outcome, participants, and care providers were masked to treatment assignment throughout the study. The code could be unblinded only with the approval of the steering committee." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All investigators including interviewers and assessors of the outcome, participants, and care providers were masked to treatment assignment throughout the study. The code could be unblinded only with the approval of the steering committee." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The following participants were excluded from the 'full analysis set' post‐randomisation from both escitalopram group and placebo group:
Reasons for attrition were reported (withdrew consent, violated protocol, considered for treatment for depression, death). Numbers were similar in both groups At 12 weeks, escitalopram group 67/241 (28%) attrition and placebo 73/237(31%) attrition Attrition much greater than 5% It is not clear how missing data were imputed for the intention‐to‐treat analysis; Quote: "we used latest available records for analysis." |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all the study's prespecified (primary outcomes and secondary outcomes) that are of interest in the review have been reported in the prespecified way. |
| Other bias | High risk | The baseline data presented in table 1: comparison of data at baseline between control group and the treatment group are not true baseline characteristics (i.e. at randomisation). The data presented in table 1 are the baseline characteristics of all those completing the trial which is a subgroup of all participants randomised. We cannot tell if there is whether there was any baseline imbalance in important demographic or clinical characteristics |
Kong 2007.
| Study characteristics | ||
| Methods | Parallel Aim: to study whether fluoxetine could prevent post‐stroke depression and improve neurological function |
|
| Participants | Country: China Setting: inpatient Stroke: met diagnostic criteria of various cerebrovascular diseases formulated in the 4th National Cerebrovascular Disease conference and confirmed as stroke by CT or MRI, all hemiplegic, within 7 days of onset HAMD score of no depression Treatment: 48 people, mean age 64 ± 7 years, 60% men Control: 42 people, mean age 62 ± 7 years, 57% men Exclusion: major depression, current antidepressants, allergy to fluoxetine, substance abuse, bipolar disorder, schizophrenia, MMSE ≤ 23/30, substance abuse, obvious liver and renal deficit |
|
| Interventions | Treatment: fluoxetine 20 mg daily Control: matching placebo capsules Duration of treatment: 8 weeks Duration of follow‐up (end of treatment to end of study): 0 |
|
| Outcomes | HAMD BI NIHSS Reported "somatic side effects and hyponatraemia" but not death or other side effects Authors state that "side effect rating was assessed at each visit" but unclear how this was done |
|
| Funding source | Source of funding not stated. Fluoxetine and placebo were supplied by Lilly Pharmaceutical Company | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated table of random digits |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Identical capsules, participants blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | States that researchers were blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 17/90 dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Balanced baseline |
Lai 2006.
| Study characteristics | ||
| Methods | Parallel design Analysis: analysed according to allocated treatment groups |
|
| Participants | Location China Setting: inpatients Treatment: 40 people Control: 40 people Total: mean age 60 ± 14 years, 43 men Stroke criteria: unclear stroke types, clinical diagnosis plus brain imaging (though not clear that stroke lesion had to be present), acute stroke Depression criteria: HAMD at least 7, or Zung SDS > 53, but no clear description about using which scale for inclusion criteria Other entry criteria: none stated Comparability of treatment groups: unclear Exclusion criteria: unclear |
|
| Interventions | Treatment: paroxetine 20 mg daily Control: placebo Duration: treatment continued for 2 months Duration of follow‐up (end of treatment to end of study): 0 |
|
| Outcomes | Depression: HAMD, Zung SDS (abnormal if the score is > 53) Additional: Zung SAS (abnormal is the score is > 50) Death The author described that they recorded AEs but they did not report any AEs |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Placebo used, not stated if matching |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant dropped out |
| Selective reporting (reporting bias) | High risk | No protocol, stated that they would evaluate side effects but these were not reported |
| Other bias | Unclear risk | Demographic details at baseline not described |
Li 2004a.
| Study characteristics | ||
| Methods | Parallel group Aim: to study effects of fluoxetine on neurological impairment and post‐stroke depression |
|
| Participants | Location: China Setting: inpatient Stroke: inclusion: all pathological types, clinical diagnosis plus confirmation by imaging that relevant lesion visible, CSS 16 to 30 Depression criteria: HAMD scores ≥ 17 and DSM IV diagnostic criteria Treatment: 33 people, mean age 60.33 years, 24 men Control: 34 people, mean age 60.44 years, 23 men Excluded severe psychiatric disorders, severe cardiac, pulmonary, hepatic and renal disease |
|
| Interventions | Treatment: fluoxetine 20 mg daily plus routine acute stroke care Control: routine acute stroke care Duration of treatment: 4 weeks Duration of follow‐up (end of treatment to end of study): 0 |
|
| Outcomes | CSS Depression incidence Laboratory monitoring parameters AEs (method of reporting not stated) |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random numbers |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Low risk | Balanced baseline |
Li 2004b.
| Study characteristics | ||
| Methods | Parallel design Aim: to treat depression |
|
| Participants | Country: China Setting: inpatient Stroke criteria: ischaemic stroke, clinical diagnosis plus imaging confirmation (though not clear that a relevant lesion had to be seen), stroke onset time ≤ 7 days Depression criteria: HAMD score ≥ 8 Treatment: 37 people, age 48 to 87 years, 17 men Control: 36 people, age 53 to 82 years, 15 men Exclusion: previous depression or psychiatric interview, dementia (according to MMSE scores), aphasia, severe cardiac, pulmonary, hepatic, renal function impairment, consciousness disturbance |
|
| Interventions | Treatment: fluoxetine 20 mg daily plus usual stroke care Control: usual stroke care Duration: 8 weeks Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | HAMD CSS (cannot use as reported as a categorical variable) MMSE (reported as a dichotomous variable) BI (reported as a dichotomous variable) Data for continuous variables not provided Death reported Side effects in treatment group only reported, not control group. Method of reporting side effects not stated |
|
| Funding source | Source of funding not stated | |
| Notes | Note that the sum of numbers in each category of HAMD at 8 weeks in the control group adds up to 30, not 32 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Method not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropouts: 6 in treatment and 4 in control group. Total dropouts = 10/73 (14%) |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Baseline balanced |
Li 2005.
| Study characteristics | ||
| Methods | Parallel design Improvement of post‐stroke depression and augmentation of rehabilitation |
|
| Participants | Country: China Setting: inpatient Stroke criteria: all stroke, clinical diagnosis plus confirmation on imaging (though not clear whether a relevant lesion had to be present) Depression according to CCMD‐II‐R Treatment: 74 participants Control: 74 participants Participaients in the treatment and control groups were selected from a group of 368 stroke patients with an average age of 57 ± 11.8 years, age range 33 to 84 years, 240 men Excluded: previous psychiatric disorders, severe dementia, aphasia, consciousness disturbance |
|
| Interventions | Treatment: paroxetine 20 mg daily plus routine stroke treatment Control: routine stroke treatment Duration of treatment: 4 weeks Duration of follow‐up (end of treatment to study end): 0 |
|
| Outcomes | HAMD SSS Deaths Side effects not recorded |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not described |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated whether blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analysed according to allocated treatment group, no participant dropped out |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | No description of differences between treatment and control group |
Li 2006.
| Study characteristics | ||
| Methods | Parallel group | |
| Participants | All pathological types of stroke, CT or MRI needed for diagnosis Inclusion criteria: depression diagnosed by Chinese Classification of Mental Disorders 3 and HAMD ≥ 18, no previous organic brain disorder, and no previous psychiatric history, clear consciousness, no comprehension problems, normal language, first acute stroke, first episode of depression Treatment: 52 people, mean ± SD age 61.12 ± 10.25, 32 men Control: 53 people, mean ± SD age 60.89 ± 9.12, 35 men |
|
| Interventions | Treatment: citalopram 20 mg daily plus usual care Control: usual care Duration of treatment: 12 weeks Duration of follow‐up (end of treatment to end of study): 0 |
|
| Outcomes | HDRS (also known as HAMD) BI CSS MMSE Side effects reported according to the participant's complaints and observation, no description of who recorded AEs; and reported only for the treatment group |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 dropouts in treatment group, 4 in control group. 1 in treatment group died, and 2 in the control group died (i.e. > 5%) |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Low risk | Baseline balanced |
Li 2007.
| Study characteristics | ||
| Methods | Aim: to investigate the efficacy and safety of paroxetine in the treatment of post‐stroke depression. Patients randomly divided into two groups | |
| Participants | Stroke diagnosis: 4th Congress of Chinese Cerebrovascular Diseases, with brain CT or MRI to confirm the diagnosis. 30 cases of ischemic stroke and 14 cases of hemorrhagic stroke in the treatment group, and 31 cases of ischemic stroke and 11 cases of hemorrhagic stroke in the control group. Patients with prior depression, anxiety and schizophrenia were excluded HAMD Score ≥ 18 |
|
| Interventions | Both groups were given usual medical care, the treatment group was give paroxetine tablets (Zhejiang Huahai Pharmaceutical Co., Ltd.,), 20mg, once per day orally in the morning for 8 weeks; the control group was given the placebo, dose not reported, once per day orally in the morning for 8 weeks | |
| Outcomes | Depression score at treatment of 2‐week, 4‐week and 8‐week Neurological deficiency score at treatment of 2‐week, 4‐week and 8‐week |
|
| Funding source | Unclear | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Other bias | Unclear risk | No information provided |
Li 2008.
| Study characteristics | ||
| Methods | Parallel trial, 3 (fluoxetine versus "free and easy wandering" versus placebo), we are using the fluoxetine versus placebo comparison in this review | |
| Participants | Country: China Setting: unclear Stroke criteria: by neuroimaging, ischaemic or PICH Depression diagnosis: "each patient was evaluated by a psychiatrist", HAMD > 20 included Fluoxetine group: 60 people, mean age 69.2 ± 3.5 years, men 41.6% Control: 30 people, mean age 67.8 ± 3.9 years, men 56.7% Excluded psychiatric illness other than depression, antidepressants within previous 2 weeks, MMSE < 23, severe aphasia |
|
| Interventions | Treatment: fluoxetine 20 to 40 mg daily Control: placebo Duration of treatment: 8 weeks Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | HAMD BI Description of why participants left the trial early AEs (reported by participant or observed/elicited by physician at each visit) |
|
| Funding source | Funded by the Natural Science Foundation of Shandong Province, People's Republic of China. None of authors had financial ties with the companies producing the medications in this study | |
| Notes | Note twice as many in fluoxetine as in control group Study conducted between March 2006 to September 2007. None of the authors or departments involved in the study had financial ties with the companies producing the medications used in this study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Paper states blinded, used placebo (though unclear if matching, thus unclear (had a matching placebo been used then it would have been low) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 4/90 dropped out (< 5%) |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Low risk | Balanced baseline |
Li 2017.
| Study characteristics | ||
| Methods | Aim: to investigate the effect of escitalopram oxalate in the early treatment of post‐stroke depression, cognition and neurological function | |
| Participants | The diagnosis of ischaemic stroke was based on the Chinese guidelines for the diagnosis and treatment of acute ischaemic stroke (2010), and the diagnosis of haemorrhagic stroke was based on the Chinese diagnostic criteria for adult spontaneous cerebral haemorrhage (2010). Patient met the Chinese diagnostic criteria for mental disorders and depression, with HAMD ≥ 17 points. MMSE was used to screen the patients with post‐stroke cognitive impairment The patients with unstable vital signs, severe cognitive impairment, severe depression, severe aphasia and unconsciousness were excluded |
|
| Interventions | Both groups received routine medicine and rehabilitation exercise. The treatment group was additionally treated with escitalopram oxalate tablets (Lexpro, produced by Lingbei pharmaceutical factory of Denmark, Xi'an Janssen Pharmaceutical sub package), 10 mg orally after breakfast every day for 24 weeks; the control group was additionally treated with placebo, 1 tablet each time, orally after breakfast for 24 weeks | |
| Outcomes | HAMD, MMSE, NIHSS and FIM were used to evaluate depression, cognitive function, neurological deficit and the patients' ability to live independently respectively, by 2 psychiatrists and 2 neurologists who were uninformed of the treatment. Above scales were respectively before treatment, 4 weeks and 24 weeks after treatment | |
| Funding source | Unclear | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessed by 2 neurologist and 2 pyschiatrists unaware of treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | No information |
Liu 2006.
| Study characteristics | ||
| Methods | Parallel design Aim: to study effect of citalopram on post‐stroke depression and neurological functional rehabilitation |
|
| Participants | Country: China Setting: inpatient Stroke criteria: stroke during "recovery phase" at 6 to 9 months, NIHSS score ≥ 13, HAMD score ≥ 17 60 people randomised, of whom 38 were men, mean age 60.7 ± 8.6 years. Demographics for treatment and control groups were not provided Treatment: 30 people, age and gender not stated Control: 30 people, age and gender not stated Exclusion criteria: previous psychiatric disorder, dementia, aphasia, consciousness disturbance |
|
| Interventions | Treatment: citalopram 20 mg daily plus routine stroke care Control: routine stroke care Duration of treatment: 6 weeks Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | HAMD NIHSS BI Death |
|
| Funding source | Source of funding not stated | |
| Notes | AEs not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Baseline balance reported by authors |
Marquez Romero 2013.
| Study characteristics | ||
| Methods | Multicentre Study type: interventional (clinical trial) Primary purpose: supportive care |
|
| Participants | 32 participants Country: Mexico Setting: inpatient At randomisation number allocated: N = 32: fluoxetine (n = 15); placebo (n = 17) % men: 50% Age: mean age 55.1 ± 12.2 Subtype of stroke: not available Severity of stroke: NIHSS, Median (IQR): fluoxetine (12 (5)); placebo (14 (5)) Time since stroke onset: within 10 days Inclusion criteria
Exclusion criteria
Withdrawal criteria
|
|
| Interventions | Experimental: fluoxetine 20 mg orally once daily for 90 days Comparator: matching placebo orally once daily for 90 days |
|
| Outcomes | Primary outcome
Secondary outcomes
|
|
| Funding source | Psicofarma S.A. de C.V. | |
| Notes |
NCT01737541 Terminated (study recruitment was suspended due to lack of funding) Dates study conducted: November 2012 to August 2014 Declarations of Interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A pharmaceutical laboratory (Psicofarma™ S.A. de C.V.) will be responsible for the manufacture and randomization of the investigational product, which will be achieved using a web‐based randomization program. This program will be set to assign participants equally to each site at a ratio of 1:1." |
| Allocation concealment (selection bias) | Low risk | Quote: "Each of the sites will be assigned 22 participants. The manufacturer will then deliver the pre‐randomized bottles containing the investigational product to each recruiting center. Study subjects who satisfy the eligibility criteria at each recruiting center will receive the investigational product corresponding to a consecutive number assigned according to their entrance to the study." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Fluoxetine and placebo tablets will be identical in form, color, odor and packaging." "Both the investigator and the subject will be blinded to the assignment of the study drugs. The manufacturer of the tablets will label the investigational drugs by the randomization code number. The labeled experimental products will be provided to the recruiting centers by the manufacturer. An envelope containing all randomization codes will be delivered to the principal investigator and will be kept sealed until the conclusion of the trial." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of participants and key study personnel ensured, and unlikely that blinding could have been broken |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Aimed to recruit 44 per group (total of 88) 35 in each group + 20% to allow for predicted 20% loss to follow‐up Actual enrolment N = 32. Quote: "Two patients (one in each group) did not take any medication returning the unopened bottles at visit 1 and had to be excluded from analysis.". We judged that this is unlikely to have influenced bias, as there is one missing from each group and this represents a similar proportion in each group Comment: report includes data from 30 participants (14 participants in the fluoxetine group and 16 in the placebo group) |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all of the study's prespecified (primary and secondary) outcomes that are of interest in the review have been reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Meara 1998.
| Study characteristics | ||
| Methods | Parallel design Analysis: unclear | |
| Participants | Location: Wales, UK Setting: inpatient Treatment: unclear Control: unclear Stroke criteria: ischaemic stroke > 11 weeks prior to randomisation Depression criteria: GDS (15‐item) score > 4 Other entry criteria: not stated Exclusion criteria: moderate to severe dementia, severe aphasia, communication difficulties, poorly controlled epilepsy |
|
| Interventions | Treatment: sertraline 50 mg daily, dose escalation to 100 mg for non‐responders at 2 weeks Control: matched placebo Duration: treatment continued for 6 weeks |
|
| Outcomes | Depression: change in scores from baseline to end of treatment on GDS Unable to use GDS, BI, MMSE, FAI, FAST Leaving trial early Death AEs |
|
| Funding source | Source of funding not stated | |
| Notes | Contacted author for more details but no response We could not use the data in our meta‐analysis Dates of study not stated. Conflicts not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blind reported, those who were blind not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Double‐blind reported, those who were blind not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | Insufficient data to make a judgement |
| Other bias | Unclear risk | Insufficient data to make a judgement |
Miao 2004.
| Study characteristics | ||
| Methods | Parallel group 9 not allocated (5 in treatment group refused allocation, 4 in the control group refused allocation) |
|
| Participants | Country: China Setting: mixed inpatient and outpatient All stroke pathological types, clinical diagnosis plus confirmation by imaging that a relevant lesion was visible, 2 to 8 months after stroke, clear consciousness, no comprehension problem, 1 lesion in 1 hemisphere, normal language comprehension Mood: depression after stroke onset, HAMD score ≥ 20 Participants: 90 randomised, 34 in each group at treatment end Treatment: 34 people, age 58.16 ± 8.49 years, 19 men Control: 34 people, age 62.45 ± 8.24 years, 18 men Exclusion criteria: other organic brain disorders and other aetiologies‐related depression |
|
| Interventions | Treatment: citalopram 20 mg daily plus usual stroke care Control: usual stroke care Duration of treatment: 6 weeks Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | HAMD SDS Efficacy Death AEs (only in the citalopram group) Method of recording AEs was not stated |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Simple random sampling" Comment: no further description given |
| Allocation concealment (selection bias) | Unclear risk | Allocation not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 9 not allocated after randomisation, 13 dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Baseline balanced |
Murray 2005.
| Study characteristics | ||
| Methods | Parallel design Analysis: ITT (last observation carried forward) and per‐protocol: death (2 control), no efficacy (16 treatment, 22 control), withdrawn owing to AE (8 treatment, 5 control), withdrew consent (1 control), all excluded from analysis |
|
| Participants | Location: Sweden Setting: mixed Treatment: 62 people, mean ± SD age 71 ± 10 years, 52% men Control: 61 people, mean ± SD age 71 ± 10 years, 44% men Stroke criteria: all subtypes, diagnosis by WHO criteria and CT (100%); stroke 3 to 367 days prior to randomisation (average time 128 days) Depression criteria: psychiatric interview (DSM‐IV, major and minor) and MADRS > 9 Other entry criteria: > 17 years of age, stroke within the previous 12 months Comparability of treatment groups: significant trend towards more left‐hemisphere lesion strokes in treatment group Exclusion criteria: under 18 years of age, severely impaired communication, apparent difficulties adhering to study protocol, acute myocardial infarction, other psychiatric illnesses other than depression, significant risk of suicide, antidepressants during the month after randomisation, current use of psychotropic medication or opiate analgesic drugs Participants with < 20% reduction in MADRS score at 6 weeks were excluded |
|
| Interventions | Treatment: sertraline 50 mg daily; possible dose escalation to 100 mg after 4 weeks Control: matching placebo Duration of treatment: 26 weeks Duration of follow‐up: (treatment end to study end): 0 |
|
| Outcomes | Depression: change in scores from baseline to end of treatment on MADRS Additional: leaving the study early Death Unable to use: Scandinavian Supervision Stroke Scale, BI, Stroke Unit Mental Status, Examination social performance, treatment costs, mortality, relative's situation, neuropsychological performance, neurological recovery (data not presented) AEs (selected data presented) using a modified version of the Udvalg for Kliniske Undersogelser side effect rating scale |
|
| Funding source | Funded by an unrestricted grant, study drug and placebo from Pfizer AG Sweden and grants from the AFA Insurances and Marianne and Marcus Wallenberg Foundation | |
| Notes | Recruitment September 1998 to January 2001. Conflicts stated; some of the authors have received grants from pharmaceutical companies | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation |
| Allocation concealment (selection bias) | Low risk | Centralised randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | States blinding and used matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | States blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 123 enrolled. 69 completed. Last observation carried forward |
| Selective reporting (reporting bias) | High risk | No protocol, paper stated that ADL data and SSS data were collected, but these were not reported |
| Other bias | Unclear risk | Balanced baseline except that more participants had left hemisphere brain lesion in sertraline group than in placebo group (statistically significant) |
NCT00177424.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Primary purpose: prevention |
|
| Participants | Number of participants: unclear Country: USA Setting: inpatient At randomisation number allocated: unclear % male: unclear Age: unclear Subtype of stroke: unclear Severity of stroke: unclear Time since stroke onset: unclear Inclusion criteria
Exclusion criteria
|
|
| Interventions | Experimental: sertraline 12.5 mg/d for 3 days, increased to 25 mg/d for 4 days, then 50 mg/day for 7 days, then increased to 75 mg/day. Target dose = 75 mg per day for the remainder of participation in the study Comparator: matched placebo |
|
| Outcomes | Primary outcome collected at 12 months
Secondary outcomes collected at 12 months:
|
|
| Funding source | None stated | |
| Notes | Terminated (recruitment goals could not be met). Last update 27 June 27 2014 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
NCT01674868.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Intervention model: parallel assignment Primary purpose: treatment |
|
| Participants | 0 participants (aimed to recruit 25 participants) Country: USA Setting: inpatient At randomisation number allocated: 0 % male: not available Age: not available Subtype of stroke: not available Severity of stroke: not available Time since stroke onset: not available Inclusion criteria
Exclusion criteria
|
|
| Interventions | Experimental: fluoxetine 20 mg daily for 90 days starting day 5 to10 after stroke Comparator: placebo participants will take 1 placebo pill daily for 90 days |
|
| Outcomes | Primary outcome measure
Secondary outcome measures
|
|
| Funding source | Not stated | |
| Notes |
NCT01674868 Withdrawn: unable to find patients meeting inclusion/exclusion criteria Dates study conducted: April 2013 to December 2015 (estimated completion date) Declarations of Interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Withdrawn: unable to find patients meeting inclusion/exclusion criteria |
| Allocation concealment (selection bias) | Unclear risk | Withdrawn: unable to find patients meeting inclusion/exclusion criteria |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Withdrawn: unable to find patients meeting inclusion/exclusion criteria |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Withdrawn: unable to find patients meeting inclusion/exclusion criteria |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Withdrawn: unable to find patients meeting inclusion/exclusion criteria |
| Selective reporting (reporting bias) | Unclear risk | Withdrawn: unable to find patients meeting inclusion/exclusion criteria |
| Other bias | Unclear risk | Withdrawn: unable to find patients meeting inclusion/exclusion criteria |
NCT02737930.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Acute stroke 18 Years to 85 years MRI‐confirmed acute ischaemic stroke resulting in an isolated homonymous visual field loss 17 enrolled up to August 2020. No results published |
|
| Interventions | Fluoxetine 20mg for 90 days or matching placebo | |
| Outcomes | Improvement in size of visual field deficit (degrees) (primary outcome) Secondary outcomes: improvement in size of visual field deficit (square degrees), Improvement in parametric mean deviation Functional field score Visual Function Questionnaire‐25 score Patient Health Questionnaire‐9 score mRS score Post‐stroke changes in cortical visual representation as measured by functional MRI Post‐stroke changes in retinal nerve fibre layer thickness |
|
| Funding source | Bogachan Sahin | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No published data |
| Allocation concealment (selection bias) | Unclear risk | No published data |
Pan 2018.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Primary purpose: treatment |
|
| Participants | 170 participants Country: China Setting: inpatient At randomisation number allocated: 170, paroxetine (n = 85); usual care (n = 85) % male: paroxetine (71.8); usual care (unclear) Age: mean age paroxetine = 65.6 ± 7.56; placebo = unclear Subtype of stroke: not stated. Severity of stroke: NIHSS, Median (IQR): paroxetine 8 (6 – 10); usual care (unclear) Time since stroke onset: within 1 week Inclusion criteria
Exclusion criteria
Withdrawal criteria: not stated |
|
| Interventions | Experimental: orally administrated paroxetine at dosages of 10 mg/day during week 1 and 20 mg/day thereafter, for a total treatment duration of 3 months Comparator: usual care |
|
| Outcomes | Outcomes were collected at 15, 90 and 180 days
|
|
| Funding source | No grant funding from any grant funding agency, commercial or not‐for‐profit organisations | |
| Notes | There is no study protocol/trial register reference Baseline sociodemographic and clinical characteristics are provided only for those who completed the study The authors state that one of the inclusion criteria is MOCA score of < 26 points. In the Results section they state that there were "72 cases of cognitive impairment" (i.e. a MoCA score of < 26 points) in the comparator group and 82 in the experimental group at days 15, 90 and 180. This suggests that either that the inclusion criteria were not strictly adhered to or if 100% of participants had a MoCA score of < 26 points at baseline then 10/82 participants in the comparator group and 3/85 in the experimental group have improved on the MoCA between days 0 and 15 Dates study conducted: participants recruited between January 2012 and June 2014 Declarations of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random number table" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to judge high or low |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to judge high or low |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All scale evaluators were trained and tested by the main investigator and were blind to the group assignment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data available for all participants in the experimental group (n = 85/85) and data available for (n = 82/85) participants in the comparison group for the Fugl–Meyer Motor Scale and the HAMD score For the MoCA (see 'Other bias' below) < 5% overall loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol/trial register reference, so insufficient information to judge high or low |
| Other bias | High risk | The authors state that one of the inclusion criteria is Montreal Cognitive Assessment (MoCA) score of < 26 points. In the Results section they state that there were "72 cases of cognitive impairment" (i.e., a MoCA score of < 26 points) in the comparator group and 82 in the experimental group at days 15, 90 and 180. This suggests that either that the inclusion criteria were not strictly adhered to or, if 100% of participants had a MoCA score of < 26 points at baseline then 10/82 participants in the comparator group and 3/85 in the experimental group have improved on the MoCA between days 0 and 15. The results 'Comparison of MoCA scores' and table 3 suggests otherwise |
Pariente 2001.
| Study characteristics | ||
| Methods | Prospective double‐blind cross‐over placebo‐controlled study of 8 people with pure motor hemiparesis | |
| Participants | Lacunar ischaemic stroke, assessed by brain CT Quote: "Early phase of recovery" |
|
| Interventions | Single dose of fluoxetine | |
| Outcomes | fMRI (raw data provided) Finger tapping (presented as a graph, no raw data) NIHSS, motricity index, BI, trunk control test, Ashworth Scale, somatosensory scale (no data) |
|
| Funding source | Source of funding not stated | |
| Notes | We could not use these data in our meta‐analyses. The authors reported that fluoxetine led to hyperactivation in the ipsi‐lesional (i.e. on the same side as the stroke lesion) primary motor cortex during a motor task; moreover, fluoxetine significantly improved motor skills of the affected side Dates of recruitment not given. Conflicts not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation code kept at the centre and broken at the end of the study |
| Allocation concealment (selection bias) | Low risk | Randomisation code kept at the centre and broken at the end of the study |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, placebo given |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data on fMRI appears complete |
| Selective reporting (reporting bias) | Unclear risk | Data on clinical outcomes were not reported |
| Other bias | Low risk | Balanced baseline |
Rasmussen 2003.
| Study characteristics | ||
| Methods | Parallel design Analysis: ITT (last observation carried forward) and per‐protocol: details of those excluded from analyses (35 treatment, 35 control) unclear |
|
| Participants | Location: Denmark Setting: unclear Treatment: 70 people, mean ± SD age 72 ± 9, 50% men Control: 67 people, mean ± SD age 68 ± 11, 51% men Stroke criteria: ischaemic and PICH; diagnosis by clinical signs and symptoms; stroke 0 to 4 weeks prior to randomisation Other entry criteria: not stated Comparability of treatment groups: participants in treatment group older on average |
|
| Interventions | Treatment: sertraline 50 mg daily; at any time after 2 weeks dose could be increased in 50 mg increments up to 150 mg daily; average dose 62.9 mg daily Control: matched placebo Duration of treatment: 12 months Duration of follow‐up (end of treatment to end of study): 0 |
|
| Outcomes | Depression: change in scores from baseline to end of treatment on HDRS Proportion scoring > 2 on the CGI or > 16 on the GDS at end of treatment Additional: leaving the study early. Did not report death Unable to use: HDRS, GDS, aphasia severity rating scale, European Stroke Scale, MMSE, Cambridge Cognitive Examination, SF‐36, BI (data not presented) AEs (detailed data not presented) evaluated by using the Udvalg for Kliniske Undersogelser Side Effect Rating Scale Did not report death |
|
| Funding source | Funding from Pfizer A/S, Gert Jorgensen legat and the Brain Cause. It is unclear whether the drug companies had input into the design and analysis of the study | |
| Notes | Recruitment January 1996 to May 1998. Conflicts not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated |
| Allocation concealment (selection bias) | Unclear risk | Method not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Matched placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No data on patients who dropped out. Used ITT analysis and last observation carried forward |
| Selective reporting (reporting bias) | Low risk | Trial details published on www.strokecentre.org/trials |
| Other bias | Unclear risk | Those given sertraline were slightly older (by 4 years) but this is unlikely to introduce bias There was no significant difference between groups |
Razazian 2014.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Primary purpose: treatment |
|
| Participants | 172 participants Country: Iran (Islamic Republic of) Setting: inpatient At randomisation number allocated: fluoxetine n = 86; placebo n = 86 % male: unclear Age: fluoxetine group = unclear; placebo = unclear Subtype of stroke: not available Severity of stroke: not available Time since stroke onset: not available Inclusion criteria
Exclusion criteria
Withdrawal criteria: not stated |
|
| Interventions | Experimental: fluoxetine, 20 mg once a day for 90 days Comparator: placebo fluoxetine for 90 days All participants received 30 sessions of routine physiotherapy during the rehabilitation period |
|
| Outcomes | Primary outcomes collected at day 45 and day 90
|
|
| Funding source | Kermanshah University of Medical Sciences | |
| Notes | IRCT201312088323N7 Baseline demographic and clinical characteristics for each group not presented, but rather the baseline demographic and clinical characteristics for those completing the trial (i.e. a subset of all those randomised at baseline) are presented Dates study conducted: participants recruited between June 2013 and September 2014 Declarations of Interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "random permuted blocks" Comment: insufficient information about the block randomisation to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of high or low |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "placebo that was identical to the active drug in appearance and packaging" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement of high or low |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 13% attrition at 90 days. 13% (n = 11/86) from the experimental group and 13% (n = 11/86) from the comparator group were excluded form the full set analysis at 90 days follow‐up. Reasons for attrition reported |
| Selective reporting (reporting bias) | Low risk | Protocol available and all the study's prespecified outcomes that are of interest to the review have been reported in a prespecified way |
| Other bias | High risk | The baseline data presented in table 1: patients demographic characteristics and risk factors and not true baseline characteristics (i.e. at randomisation). The data presented in table 1 are the characteristics of the full analysis set which is a subgroup of all participants randomised. We cannot tell if there is whether there was any baseline imbalance in important demographic or clinical characteristics |
Restifo 2001.
| Study characteristics | ||
| Methods | Double‐blind study | |
| Participants | 10 participants with disabling hemiplegia owing to hemispheric ischaemic stroke in territory of left MCA | |
| Interventions | Treatment: fluoxetine 20 mg daily for 3 months plus usual care (including Bobath rehabilitation) Control: usual care including Bobath rehabilitation |
|
| Outcomes | Transmagnetic stimulation to establish motor reorganisation The authors reported that fluoxetine might modulate the primary motor cortex reorganisation |
|
| Funding source | Source of funding not stated | |
| Notes | Abstract only, full paper could not be found by our searches. Dates of study and conflicts of interest not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Random allocation"; method not described |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Random allocation"; method not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | A placebo was used, not clear if it was matching |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear from abstract |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear from abstract |
| Selective reporting (reporting bias) | Unclear risk | Unclear from abstract |
| Other bias | Unclear risk | Unclear from abstract |
Robinson 2000a.
| Study characteristics | ||
| Methods | Parallel design Comparison of fluoxetine, nortriptyline and placebo. We are using the fluoxetine and placebo data Analysis: per protocol, number excluded from analyses varied Data provided for depressed and non‐depressed separately. We are labelling the depressed group as Robinson 2000a (this trial), and the non‐depressed group as Robinson 2000b |
|
| Participants | Location: USA and Argentina Setting: mixed Treatment: 23 people with depression, mean ± SD age 65 ± 14 years; 17 men Control: 17 people with depression, mean ± SD age 73 ± 10 years; 9 men Stroke criteria: all subtypes, diagnosis by clinical signs and CT (100%), stroke within 6 months of recruitment, 18 to 85 years of age Stroke on average 16 weeks (fluoxetine) and 6 weeks (placebo) prior to randomisation Exclusion criteria: other significant medical illness, severe comprehension deficit, prior history of head injury, prior history of other brain disease (with the exception of stroke), participants on antidepressants (other than fluoxetine) were allowed to stop their antidepressant for a 2‐week washout period |
|
| Interventions | Treatment: fluoxetine 10 mg daily (3 weeks), 20 mg daily (3 weeks), 30 mg daily (3 weeks), 40 mg daily (3 weeks) Control: matched placebo Duration: treatment continued for 12 weeks Duration of follow‐up (end of treatment to end of study): 0 |
|
| Outcomes | Depression: change in scores from baseline to end of treatment on HDRS Additional: MMSE, JHFI Death AEs (method of reporting these was not stated) |
|
| Funding source | Funded by NIMH grants and grants from the Raul Carrea Institute of Neurological Research and Fundacion Perez Companc. Eli Lilly and company supplied the fluoxetine and placebo | |
| Notes | Note difference in time since stroke between treatment groups Dates of recruitment not stated. Conflicts not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐number table |
| Allocation concealment (selection bias) | Low risk | Concealment held by independent person |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Matched placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Per‐protocol and ITT analyses |
| Selective reporting (reporting bias) | Low risk | Protocol published www.strokecentre.org/trials |
| Other bias | Unclear risk | Imbalance in treatment groups for time since stroke and gender |
Robinson 2000b.
| Study characteristics | ||
| Methods | Parallel design Comparison of fluoxetine, nortriptyline and placebo. We are using the fluoxetine and placebo data Analysis: per protocol, number excluded from analyses varies Data provided for depressed and non‐depressed separately. We are labelling the depressed group as Robinson 2000a, and the non‐depressed group as Robinson 2000b (this trial) |
|
| Participants | Location: USA and Argentina Setting: mixed Treatment: 17 non‐depressed people, mean ± SD age 66 ± 13 years, 15 men Control: 16 non‐depressed people, mean ± SD age 67 9 years, 12 men Stroke criteria: all subtypes, diagnosis by clinical signs and CT (100%), stroke within 6 months of recruitment, aged 18 to 85 years of age Stroke on average 8 weeks (treatment) and 5 weeks (control) prior to randomisation Comparability of treatment groups: unclear Exclusion criteria: other significant medical illness, severe comprehension deficit, prior history of head injury, prior history of other brain disease (with the exception of stroke), participants on antidepressants (other than fluoxetine) were allowed to stop their antidepressant for a 2‐week washout period |
|
| Interventions | Treatment: fluoxetine 10 mg daily (3 weeks), 20 mg daily (3 weeks), 30 mg daily (3 weeks), 40 mg daily (3 weeks) Control: matched placebo Duration: treatment continued for 12 weeks Duration of follow‐up (end of treatment to end of study): 0 |
|
| Outcomes | Depression: change in scores from baseline to end of treatment on HDRS Additional: MMSE, JHFI Death AEs (method of reporting these was not stated) |
|
| Funding source | Funded by NIMH grants and grants from the Raul Carrea Institute of Neurological Research and Fundacion Perez Companc. Eli Lilly and company supplied the fluoxetine and placebo | |
| Notes | Note difference in time since stroke between groups Dates of recruitment not stated. Conflicts of interest not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐number table |
| Allocation concealment (selection bias) | Low risk | Concealment held by independent person |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Matched placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT and per‐protocol |
| Selective reporting (reporting bias) | Low risk | Trial on www.strokecentre.org/trials |
| Other bias | Unclear risk | Note imbalance in time since stroke and in gender |
Robinson 2008.
| Study characteristics | ||
| Methods | Parallel group, 3‐arm (escitalopram, placebo, problem‐solving therapy group). We are using the escitalopram versus placebo arm in this review Analysis: ITT |
|
| Participants | Country: USA Setting: mixed: neurology department and newspaper advertisements Stroke criteria: ischaemic or haemorrhagic stroke not because of complications of intracranial aneurysm or intracranial vascular malformation; within 3 months of index stroke Mood: excluded if DSM IV for major or minor depression or HAMD > 17 Treatment (escitalopram): 59 people, mean ± SD age 61.2 ± 13.7, 38 men Control (matched placebo): 58 people, mean ± SD age 63.9 ± 11.1, 37 men Exclusion: acute coronary syndrome, neurodegenerative disorders, DSM IV criteria for alcohol or substance abuse |
|
| Interventions | Treatment: escitalopram 5 mg to 10 mg (depending on age ‐ lower dose given to > 65 years old) Control: matched placebo Duration of treatment: 12 months Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | Diagnosis of depression HAMD (dichotomised) FIM (though no raw data provided in the paper for meta‐analysis) Social functioning examination Repeatable Battery for Neuropyschological Status The Iowa subset provided detailed information about cognition Participants, family members and primary care physicians were asked about AEs at 3 monthly intervals or sooner if an individual reported an AE using a standardised checklist |
|
| Funding source | The initial report states that "This work was supported solely by National Institute of Mental Health Grant RO1MH‐65134. All the study medications were purchased using NIMH grant funds." In a subsequent letter to the Journal, the authors disclosed honoraria and expenses from pharmaceutical companies, and that 1 of the authors owned Pfizer stock. However, the authors stated that the design and analysis of any of the expenses of the study were supported by monies, materials or any intellectual input from Forest Laboratories | |
| Notes | The escitalopram group had significantly more diabetes than the placebo group Financial disclosures: see above Recruitment: 9 July 2003 to 1 October 2007 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised blocks of 3, 6, and 9 |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Identical placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analyses, all participants used in analysis Dropouts: 5 in placebo and 7 drop‐outs in escitalopram |
| Selective reporting (reporting bias) | Low risk | All specified outcome data reported. Trial published on www.strokecentre.org/trials |
| Other bias | Unclear risk | There was more diabetes in the escitalopram group than placebo group |
Savadi Oskouie 2012.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Primary purpose: treatment |
|
| Participants | 144 participants Country: Islamic Republic of Iran Setting: inpatient At randomisation number allocated: N = 144; citalopram (n = 72); placebo (n = 72) % male at baseline: citalopram n = unclear; placebo n = unclear Age at baseline: citalopram (n = unclear); placebo (n = unclear) Subtype of stroke at baseline: unclear Severity of stroke at baseline: unclear Time since stroke onset: within 7 days Inclusion criteria
Exclusion criteria
Withdrawal criteria: not stated |
|
| Interventions | Experimental: oral citalopram 20 mg once daily Comparator: placebo |
|
| Outcomes | Primary outcome
Secondary outcome
|
|
| Funding source | Neurosciences Research Center (NSRC) of Tabriz University of Medical Sciences | |
| Notes | IRCT201203192150N2 Baseline demographic and clinical characteristics for each group not presented, rather the baseline demographic and clinical characteristics for those completing the trial (i.e. a subset of all those randomised at baseline) are presented Dates study conducted: May 2012 to January 2014 Declarations of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A total of 144 patients were randomized through an allocation sequence based on 2 blocks with size of 72, generated with a computer random number generator." |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation was concealed using the sequentially numbered black envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not explicitly stated that key study personnel and care providers were blinded, although implied by: Quote: "The blinding code remained confidential until the end of the study." Quote: "placebo of the same shape and full packaging during the first day after hospital admission." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not explicitly stated that outcome assessors were blinded, although perhaps implied by the fact: Quote: "The blinding code remained confidential until the end of the study." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Primary outcome data were available for 58 (81%) of the citalopram group and 50 (69%) of the placebo group. Reasons for attrition are reported but there are differences between groups: number of participants in the placebo group (n = 11) dead compared to the citalopram group (n = 4). 3 times the number of participants in the placebo group were depressed (n = 6) compared to the citalopram group (n = 2). Did not want to continue (placebo group (n = 5), citalopram group (n = 8) Intention‐to‐treat analyses were carried out (suppl table) assuming that 1. those lost to follow‐up had a poor outcome (i.e. did not improve their NIHSS scores from baseline) and 2. those participants in the placebo group who did not want to continue had a good outcome Overall loss of > 5% |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all the study's prespecified (primary outcomes and secondary outcomes) that are of interest in the review have been reported in the prespecified way |
| Other bias | High risk | The baseline data presented in table 1: comparison of demographic and baseline variables and not true baseline characteristics (i.e. at randomisation). The data presented in table 1 are the characteristics of the full analysis set at 3 months which is a subgroup of all participants randomised. We cannot tell if there is whether there were any baseline imbalance in important demographic or clinical characteristics. However, given that approximately 3 times the number of participants in the placebo group (n = 11) died compared to the citalopram (n = 4) and 3 times the number of participants in the placebo group were depressed (n = 6) compared to the citalopram group (n = 2), this suggests that there may have been important group differences in clinical characteristics at baseline |
Shah 2016.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Primary purpose: supportive care |
|
| Participants | 89 participants Country: India Setting: inpatient At randomisation number allocated: N = 89: fluoxetine (n = 45); placebo (n = 44) % male: unclear Age: unclear Subtype of stroke: unclear Severity of stroke: unclear Time since stroke onset: within 5 to 10 days Inclusion criteria
Exclusion criteria
Withdrawal criteria: not stated |
|
| Interventions | Experimental: fluoxetine 20 mg orally once daily for 90 days Comparator: matching placebo orally once daily for 90 days |
|
| Outcomes | Primary outcome
|
|
| Funding source | Not stated | |
| Notes | Baseline demographic and clinical characteristics for each group not presented, rather the baseline demographic and clinical characteristics for those completing the trial (i.e. a subset of all those randomised at baseline) are presented Dates study conducted: January 2014 to January 2015 Declarations of Interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information about the sequence generation process to permit judgement of high or low |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information about the method of allocation concealment to permit judgement of high or low |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Patients, attendants, study staff and investigators were masked to treatment allocation." However, "matching was done on a 1:1 basis for age, sex, severity of stroke", which suggests that some key study personnel were not blinded and this non‐blinding is likely to introduce bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement of high or low |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3/45 (7%) participants in the fluoxetine and 2/44 (5%) in the placebo group were lost to follow‐up. Reasons for attrition/exclusion not reported. 6% lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. Insufficient information to permit judgement of high or low |
| Other bias | High risk | The use of matching suggests a matched case control design rather than an RCT design We cannot tell whether there was any baseline imbalance in important demographic or clinical characteristics |
Song 2006.
| Study characteristics | ||
| Methods | Aim: to evaluate changes in depression and cognitive impairment in people with post‐stroke depression treated with fluoxetine Parallel trial |
|
| Participants | Country: China Setting: inpatient Stroke diagnosed by clinical criteria and "proved on CT" (though not clear if lesion had to be visible) Depression: diagnosed in accordance with the CCMD‐II‐R Treatment: 41 people, mean age 51 ± 7 years, 25 men), time since stroke: 3.5 days Control: 41 people, mean age 50 ± 8 years, 24 men), time since stroke: 3.7 days Excluded: previous mental disorders, previous "neurological disorder", if other psychiatric drugs had been taken, these had to be stopped for 1 week before fluoxetine was administered |
|
| Interventions | Treatment: fluoxetine 20 mg daily Control: placebo (although not stated whether this was identical to fluoxetine) Duration of treatment: 6 weeks Duration of follow‐up (treatment end to study end): 0 Side effects not reported |
|
| Outcomes | SDS P300 (an event‐related potential) Although the stated aim was to assess cognitive impairment, it is not clear how this was measured |
|
| Funding source | Source of funding not stated | |
| Notes | Recruitment: December 1999 to June 2003. Conflicts of interest not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Placebo, but not clear whether identical |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Unclear risk | Balanced baseline |
Wang 2003.
| Study characteristics | ||
| Methods | Parallel design 3‐arm trial: routine care, fluoxetine plus routine care, amitriptyline plus routine care. We are using the routine care and fluoxetine plus routine care in this analysis Aim: to observe effects of antidepressant therapy on post‐stroke and neurological rehabilitation in the elderly |
|
| Participants | Country: China Setting: inpatient Stroke criteria: ischaemic stroke, clinical diagnosis plus confirmation by imaging (although not clear whether a stroke lesion had to be present) Depression diagnosed according to CCMD‐II‐R diagnostic criteria, HAMD ≥ 18 Treatment: 64 people, mean age 75.6 ± 19.7 years, 39 men Control: 56 people, mean age 74.9 ± 20.8 years, 29 men Excluded: psychiatric disorder history, severe cardiac, pulmonary, hepatic and renal diseases |
|
| Interventions | Treatment: fluoxetine 20 mg to 80 mg daily (start at 20 mg/day, increase dosage at 3 weeks if poor therapeutic effect and no AE), plus usual stroke care Control: usual stroke care Duration of treatment: 12 to 24 weeks Duration of follow‐up (treatment end to study end): 6 to 9 months |
|
| Outcomes | HAMD Neurological function impairment score BI AEs not recorded |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 13 dropped out of fluoxetine group, and 9 dropped out of control group |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Baseline appeared balanced but no statistical comparison between groups |
Wang 2009.
| Study characteristics | ||
| Methods | Aim: to investigate the efficacy of paroxetine in the treatment of post‐stroke depression Parallel RCT design. Placebo‐same appearance as paroxetine |
|
| Participants | Diagnosis of stroke: all patients underwent CT or MRI examination, and the diagnosis was in accordance with the Chinese diagnostic criteria formulated by the Second National Conference of Cerebrovascular Disease in 1986; Depression diagnosis: HAMD ≥ 18, SDS (self‐rating depression scale) ≥ 50 Excluded: patients with medical history of mental illness, aphasia, epilepsy, glaucoma and drug allergy before stroke or used other antipsychotics or antidepressants in the past 2 weeks |
|
| Interventions | The treatment group was given paroxetine 20mg/day in the morning, which could be increased to 40 mg/day according to the condition, for a total of 2 months; the control group was given placebo with the same appearance. No other antipsychotics were used during the study period and benzodiazepines were given to patients with severe insomnia | |
| Outcomes | HAMD AEs |
|
| Funding source | Unclear | |
| Notes | The data in Table 2 were different to the data in the Results section. Possibly the data of treatment group were mistakenly listed for the control group. Thus there is a high risk of incorrect data reporting | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Other bias | Unclear risk | No information provided |
Wen 2006.
| Study characteristics | ||
| Methods | Parallel trial Aim: to explore effects of prophylactic anti‐depression therapy on nerve functional rehabilitation after stroke Analysis: according to treatment group |
|
| Participants | Country: China Setting: inpatient Stroke criteria: acute stroke of all pathological subtypes, clinical diagnosis plus confirmation by imaging (although not clear whether a stroke lesion had to be present) Treatment: 42 people, mean age 56.8 years, men 19 Control: 42 people, mean age 57.2 years, men 16 Excluded those with primary psychiatric impairment and premorbid mood disorders, pre‐existing neurological disease causing confusion, severe systematic diseases and pulmonary, hepatic and renal failure |
|
| Interventions | Treatment: fluoxetine 20 mg daily plus routine stroke care Control: routine stroke care Duration of treatment: 8 weeks Duration of follow‐up (end of treatment to end of study): 0 |
|
| Outcomes | HAMD MESSS AEs (method of obtaining data not stated) Death |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analysed according to treatment group, no dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Balanced baseline |
Wiart 2000.
| Study characteristics | ||
| Methods | Purpose: to treat early depression Parallel design Analysis: ITT (last observation carried forward), withdrawn owing to AE (1 treatment), protocol violation (1 treatment) |
|
| Participants | Location: France Setting: unclear Treatment: 16 people, mean ± SD age 66 ± 7 years, 65% men Control: 15 people, mean ± SD age 66 ± 12 years, 40% men Stroke criteria: ischaemic stroke and PICH, diagnosis by clinical signs and CT (100%); stroke on average 47 ± 22 days (treatment group) and 48 ± 20 days (control group) Depression criteria: psychiatric interview (ICD‐10 criteria) and MADRS score > 19 Other entry criteria: all antidepressant or neuroleptic drugs stopped 10 days prior to enrolment Comparability of treatment groups: balanced Exclusion criteria: severe psychiatric problems which required hospitalisation, severe aphasia, previous stroke, severe cognitive impairment, chronic alcoholism, chronic associated handicapping pathology, contraindication to fluoxetine |
|
| Interventions | Treatment: fluoxetine 20 mg daily Control: matched placebo Duration of treatment: 45 days Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | Depression: change in scores from baseline to end of treatment of MADRS, 50% reduction in MADRS score Additional: FIMs MMSE Motricity Index Leaving the study early Death AEs ("evaluated qualitatively and quantitatively". Complete blood count, liver test and renal function test were carried out at each assessment visit) |
|
| Funding source | Lilly France Laboratory provided methodological and financial support | |
| Notes | Dates of recruitment not stated. Conflicts of interest not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not stated |
| Allocation concealment (selection bias) | Unclear risk | Method not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Identical white capsules" given |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Method of blinding not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Used last observation carried forward; 2/31 (both in fluoxetine group) dropped out. This is > 5% |
| Selective reporting (reporting bias) | Low risk | Trial published on www.strokecentre.org/trials. The primary outcome was reported |
| Other bias | Unclear risk | Baseline balanced |
Xie 2005.
| Study characteristics | ||
| Methods | Aim: to study the effect of treatment with sertraline in elderly patients with post‐stroke depression Parallel study |
|
| Participants | Country: China Setting: unclear Recruitedquote: "clinically stable stroke patients with post‐stroke depression" No other inclusion and exclusion criteria given Mood: Zung SDS score ≥ 40 or GDS score 5 to 10 Treatment: 65 people, mean age 69.8 years, 29 men Control: 65 people, mean age 70.7 years, 27 men Time since stroke: mean 87.8 days, range 48 to 142 days |
|
| Interventions | Treatment: sertraline 50 mg/day plus usual stroke care Control: usual stroke care Duration of treatment: 12 weeks Duration of follow‐up: 0 |
|
| Outcomes | Zung SDS, GDS, ADL score AEs were not reported |
|
| Funding source | Local scientific academic fund funded the study | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | No clear description between treatment and control |
Xu 2001.
| Study characteristics | ||
| Methods | Parallel Aim: to study the effect of fluoxetine on depression in early recovery stage of cerebral infarction |
|
| Participants | Country: China Setting: outpatient in rehabilitation clinic Stroke: first acute cerebral infarction, no description of the diagnostic criteria and the need for imaging confirmation, excluded large cerebral infarction or lacunar infarction (clinical condition too severe or too mild); onset to recruitment time mean 30 days Zung SDS ≥ 40 Treatment: 32 people Control: 31 people (no details of participant characteristics) Excluded if previous antidepressants |
|
| Interventions | Treatment: fluoxetine 20 mg daily plus usual stroke care Control: usual stroke care Duration of treatment: 8 weeks Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | Zung SDS ADL (BI) Neural function deficient Death AEs not reported |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 10/62 dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | No clear description of stroke criteria and imaging |
Xu 2006.
| Study characteristics | ||
| Methods | Parallel group Aim: to test whether early prophylactic antidepressant treatment by paroxetine has any beneficial influence on the rate of post‐stroke depression and rehabilitation |
|
| Participants | Country: China Setting: inpatient Stroke criteria: stroke onset time ≤ 3 days, age ≤ 75 years old, no previous psychiatric disorders, no obvious cognitive impairment or aphasia Depression diagnosis was not mentioned as an inclusion criteria, so we assumed that patients did not have to have depression to enter the trial Treatment: 32 people, mean age 65 ± 12 years, 17 men Control: 32 people, mean age 63 ± 11 years, 16 men Exclusion: no severe hepatic or renal impairment, DSM IV depression not stated as an inclusion, but none met criteria for depression initially |
|
| Interventions | Treatment: paroxetine 20 mg daily Control: placebo Duration of treatment: 12 weeks Duration of follow‐up (treatment end to study end): 0 |
|
| Outcomes | MESSS ADL Post‐stroke diagnosis incidence of depression according to DSM IV AEs not recorded |
|
| Funding source | Study funded by local scientific academic fund | |
| Notes | The number of participants in Table 2 (p187) were wrong (paroxetine/placebo: N = 32/32 should be N = 28/29) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Sequence numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Placebo used, but unclear if it was matched |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7/64 (11%) participants dropped out |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Low risk | Baseline balance |
Yang 2002.
| Study characteristics | ||
| Methods | Parallel group Aim: to study effects of antidepressant in treatment of people with post‐stroke depression |
|
| Participants | Country: China Setting: inpatients and outpatients Stroke criteria: recovery phase of stroke (2 to 6 months after ischaemic stroke, and 1.5 to 6 months after haemorrhagic stroke). We included this in the 3 to 6 month group. Clinical diagnosis of stroke (not stated whether confirmation by imaging was needed) Depression: HAMD > 7 Treatment: 64 people, mean age 64 ± 3 years, 40 men Control: 57 people, mean age 63 ± 5 years, 32 men |
|
| Interventions | Treatment: paroxetine 20 mg daily plus stroke treatment and rehabilitation Control: stroke treatment and rehabilitation Duration of treatment: 4 months Duration of follow‐up: 0 |
|
| Outcomes | Death They collected data on HAMD and CSS but did not report these data ADL score: did not state which one, so not used AEs not reported |
|
| Funding source | Source of funding not reported | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 11/121 (9%) dropouts |
| Selective reporting (reporting bias) | High risk | No protocol. The paper stated that ADL data and depression data were collected, but these data were not reported |
| Other bias | Low risk | No baseline differences between groups, no other obvious source of bias |
Yang 2011.
| Study characteristics | ||
| Methods | Aim: to treat early post‐stroke depression | |
| Participants | Country: China Setting: inpatient Stroke: all pathological types, clinical diagnosis plus confirmation of lesion on imaging, no previous psychiatric and psychological disorders, age < 75 years old, stroke onset time < 72 hours, NIHSS score: 4 to 19 Mood: HAMD ≥ 8 Treatment: 20 people, mean age 64 ± 8 years, 8 men Control: 22 people, mean age 64 ± 10 years, 13 men Note inconsistency between abstract (20 in treatment and 22 in control, but in tables of results, there are 22 in treatment and 20 in control). We have used the data from the abstract Excluded: functional psychiatric disorder, functional depression, psychoactive substance and addictive substance induced psychiatric disorders, infectious disease, severe cognitive impairment to affect communication, severe aphasia to affect communication, severe cardiac, pulmonary, hepatic and renal function impairment, previous organic brain disease such as brain tumour, or symptomatic stroke, encephalitis |
|
| Interventions | Treatment: paroxetine 20 mg daily plus usual stroke care Control: usual stroke care Duration of treatment: at least 3 months Duration of follow‐up: 0 |
|
| Outcomes | HAMD score, IL‐1β and IL‐6 level Death AEs not reported |
|
| Funding source | Source of funding: local scientific academic fund | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Case sequence" randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Low risk | No difference in baseline |
Ye 2004.
| Study characteristics | ||
| Methods | Aim: to investigate whether antidepressive therapy is needed for people with post‐stroke depression or not, and the effect of different antidepressive drugs on the rehabilitation of psychological and neurological function after stroke 3 groups: paroxetine, imipramine and control. We are using the paroxetine versus control arm in this review |
|
| Participants | Country: China Setting: inpatient Stroke: all pathological subtypes, clinical diagnosis plus confirmation by imaging (did not state whether a visible lesion was needed to make the diagnosis), no positive psychiatric disorders or family history, clear consciousness, no comprehension problem Mood: inclusion criteria: HAMD score > 21, HAMA scale > 14 Treatment: 30 people, age 58.04 ± 8.28 years, 22 men Control: 30 people, age 59.21 ± 9.52 years, 17 men Exclusion criteria: severe cardiac, hepatic and renal diseases, multiple infarcts or haemorrhage |
|
| Interventions | Treatment: paroxetine 20 mg/day plus acute stroke routine care and rehabilitation Control: acute stroke routine care plus rehabilitation Duration of treatment: 12 weeks Duration of follow‐up (end of treatment to end of study): 0 |
|
| Outcomes | Chinese Neurological Impairment Scale, modified BI, HAMD, HAMA, Therapeutic Effect for Depression and Neurologic Function Death, GI upset Method of recording side effects not stated |
|
| Funding source | Source of funding not stated | |
| Notes | Inconsistent description about the number of recruitment and randomisation between abstract (N = 90) and result part (N = 93) of the text. The number for final analysis is consistent in the text | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Used "number table", but unclear if this was a random number table |
| Allocation concealment (selection bias) | Low risk | The study designer was not involved in assessment and treatment, the assessors did not know the allocation |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The participants were blinded. Not clear if those delivering the treatment were blind, but no placebo used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Only 1 dropped out in paroxetine group |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Other bias | Unclear risk | Different numbers reported to have been recruited and randomised, baseline similar |
Zhao 2011.
| Study characteristics | ||
| Methods | Study type: interventional (clinical trial) Primary purpose: treatment |
|
| Participants | Country: People's Republic of China Setting: inpatient At randomisation number allocated: N = 82: fluoxetine (n = 41); placebo (n = 41) % male: 58.5 Age: mean age 65 ± 12 Subtype of stroke: Ischaemic stroke: 61/82 (74%); haemorrhagic stroke: 21/82 (26%) Severity of stroke: MESSS: fluoxetine 23.2 ± 6.2 (n = 37); placebo 22.8 ± 5.8 (n = 34) Time since stroke onset: within 10 days Inclusion criteria
Exclusion criteria: none Withdrawal criteria: not stated |
|
| Interventions | Experimental:fluoxetine 20 mg daily for 12 weeks Comparator: no fluoxetine |
|
| Outcomes | Outcomes collected at 2nd, 4th and 12 week of treatment and 12 weeks after the end of treatment
|
|
| Funding source | Not available | |
| Notes | Dates study conducted: 2008 to 2010 Declarations of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The participants were randomised into 2 groups (with fluoxetine or without fluoxetine) according to the sequence number and a block randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of high or low |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to permit judgement of high or low |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement of high or low |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate of fluoxetine group vs control group was 4/41 (9.8%) vs 7/41 (17.1%) > 5% loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol available. Insufficient information to permit judgement of high or low |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Zhou 2008.
| Study characteristics | ||
| Methods | Aim: to study effect of early paroxetine on post‐stroke depression and rehabilitation Parallel design Analysis: according to treatment groups |
|
| Participants | Country: China Setting: inpatient Stroke criteria: all stroke, clinical diagnosis plus confirmation by imaging (though not clear if a relevant stroke lesion had to be visible), stroke onset time ≤ 7 days, no obvious cognitive impairment, no obvious aphasia HAMD score < 8 Treatment: 36 people, mean age 63 ± 9.3 years, 16 men Control: 40 people, mean age 61 ± 9.6 years, 19 men Excluded: previous psychiatric disorders, severe hepatic and renal impairment, taking agents with obvious interaction with fluoxetine in recent 1 month |
|
| Interventions | Treatment: fluoxetine 20 mg daily plus acute stroke routine medication Control: acute stroke routine medication Duration of treatment: 8 weeks Duration of follow‐up: 0 |
|
| Outcomes | No raw data provided for any of the following outcomes: diagnosis of depression (CCMD‐3, HAMD, ADL, MESSS) Reported no deaths in either group. Unclear how data on side effects were collected |
|
| Funding source | Source of funding not stated | |
| Notes | − | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts, analysed according to allocated treatment group |
| Selective reporting (reporting bias) | High risk | No protocol, no raw data provided for several of the outcomes |
| Other bias | Low risk | Baseline similar |
ADL: activities of daily living AE: adverse event ALT: Alanine aminotransferase test BDI: Beck Depression Inventory BI: Barthel Index CCMD‐II‐R: Chinese Classification of Mental Disorders, second edition, revised CCMD‐3: Chinese Classification of Mental Disorders‐3 CGI: Clinical Global Impressions Scale CSS: Chinese Stroke Scale CT: computerised tomography CTIMP: Clinical Trial of an Investigational Medical Product DSM: Diagnostic and Statistical Manual of Mental Disorders EEG: electroencephalogram eFGR: estimated glomerular filtration rate FAI: Frenchay Activities Index FAST: Frenchay Aphasia Screening Test FIM: Functional Independence Measure FMMS: Fugl‐Meyer Motor Scale fMRI: functional magnetic resonance imaging GDS: Geriatric Depression Scale GI: gastrointestinal HADS: Hospital Anxiety and Depression Scale HAMA: Hamilton Anxiety scales HAMD/HDRS: Hamilton Depression Rating Scale HSS: Hemispheric Stroke Scale ICD: International Classification of Diseases ICH: intracerebral haemorrhage IL: interleukin ITT: intention‐to‐treat IQR: interquartile range JHFI: Johns Hopkins Functioning Inventory LOCF: last‐observation‐carried‐forward MADRS: Montgomery‐Åsberg Depression Rating Scale MAOI: mono‐amino‐oxidase inhibitor MCA: middle cerebral artery MEP: motor evoked potentials MESSS: Modified Edinburgh‐Scandinavian Stroke Scale MHI‐5: Mental Health Inventory MMSE: Mini‐Mental State Examination MoCA: Montreal Cognitive Assessment MRI: magnetic resonance imaging mRS: modified Rankin score NIHSS: National Institutes of Health Stroke Scale PASE: Physical Activity Scale for the Elderly PICH: primary intracerebral haemorrhage RCT: randomised controlled trial RS: Rankin score SAH: subarachnoid haemorrhage SAS: Zung Self‐rating Anxiety Scale SD: standard deviation SDS: Zung Self‐rating Depression Scale SF‐36: Short Form‐36 SIS: Stroke Impact Scale SSRI: selective serotonin reuptake inhibitors SSS: Scandinavian Stroke Scale TESS: Treatment Emergent Symptom Scale TIA: transient ischaemic attack VAS: visual analogue scale WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12619000573156 | Trial abandoned prior to initiating recruitment due to COVID‐19 pandemic |
| Andersen 1993 | Cross‐over design: double‐blind placebo‐controlled cross‐over protocol as follows: 7 days initial baseline registration, 21 days citalopram or placebo (randomised), 7 days wash‐out, 7 days baseline registration, and cross‐over to second 21‐day treatment period |
| Andersen 2012 | The trial never started |
| Anderson 2002 | The trial never started |
| Anonymous 2012a | Unable to find publication after extensive searching |
| Anonymous 2012b | Unable to find publication after extensive searching |
| Berends 2009 | Mean time from stroke onset to fluoxetine was 39.1 months |
| Bonin Pinto 2019 | Participants were recruited within 2 years (not 1 year) of stroke |
| Chen 2019 | Tandospirone + escitalopram (combination therapy) and escitalopram (monotherapy) in people with vascular depression |
| Choi Kwon 2008 | Participants more than 1 year post‐stroke |
| Finkenzeller 2009 | SSRI plus active intervention (psychotherapy) versus active treatment (psychotherapy) alone. This trial had been included in the original 2012 review but due to the potential interaction between the SSRI and psychotherapy we decided to exclude it in this update |
| Foster 2019 | 2 arms: 1 with SSRI plus exercise and 1 arm with placebo plus exercise |
| Gourab 2015 | Time of stroke onset > 12 months |
| Graffagnino 2002 | Previously listed in 'Studies awaiting classification' (Mead 2012). Unable to access any full publication and we received no response from the author. Given the insufficient information to assess eligibility and, owing to the length of time since the study abstract (2002) was published, we have now excluded this study. CRSREF: 3340767 |
| Ji 2000 | SSRI plus active intervention versus active treatment alone |
| Kitago 2020 | Combined intervention |
| Li 2002 | There is no random component in the sequence generation process |
| Liang 2003 | There is no random component in the sequence generation process. This had been included in the 2012 review but on review of the methodology the review authors decided to exclude this for the update |
| Liu 2004 | SSRI plus active intervention versus active treatment alone |
| Liu 2020 | Wrong comparator |
| Mosarrezaii 2018 | Qu0te: "Patients received numbered cards according to the order of hospitalization. The recipients of the cards with odd and even numbers constituted the case and control group, respectively." Allocation concealment procedure was inadequately concealed |
| NCT01963832 | Study withdrawn (not funded) |
| Robinson 2011 | Ineligible outcomes: prevention of generalised anxiety disorder |
| Sitzer 2002 | Previously listed in 'Studies awaiting classification' (Mead 2012). Unable to access any full publication and we received no response from the author. Given the insufficient information to assess eligibility and, owing to the length of time since the study abstract (2002) was published, we have now excluded this study |
| Sun 2015 | Mean time since onset 19.2 ± 3.5 months. No placebo or usual‐care control group (Prozac, acupuncture, and prozac plus acupuncture) |
| Vogel 2020 | Open‐label single‐group study |
| Xu 2007 | This had been included in the 2012 review but it compares fluoxetine plus wulung capsule versus wulung capsule alone. Wulung capsule is an active comparator so we have therefore excluded this trial for this update |
| Zhou 2003 | There is no random component in the sequence generation process. This trial had been included in the 2012 version of the review but for this update we excluded it |
SSRI: selective serotonin reuptake inhibitor
Characteristics of studies awaiting classification [ordered by study ID]
Guo 2016.
| Methods | Study type: interventional (clinical trial) Actual enrolment: 300 Allocation: randomised Intervention model: parallel assignment Masking: single (outcomes assessor) Primary purpose: prevention |
| Participants | Country: China Setting: inpatient At randomisation numbers allocated: N = 300 Experimental group 1: fluoxetine immediately after enrolment n = 100 Comparator group 1: fluoxetine 7 days after enrolment n = 100 Comparator group 2: no fluoxetine n = 100 % male: unclear Age: Experimental, unclear; Comparator 1, unclear; Comparator 2, unclear Subtype of stroke: unclear Severity of stroke NIHSS score at baseline: unclear Experimental: unclear Comparator 1: unclear Comparator 2: unclear Time from stroke onset: within 1 week after onset of cerebral infarction Inclusion criteria
Exclusion criteria
Withdrawal criteria
|
| Interventions | Experimental: 20 mg of fluoxetine per day for 90 days given immediately after enrolment and conventional therapy of cerebral infarction Comparator 1: 20 mg of fluoxetine a day for 90 days given 7 days after enrolment and conventional therapy of cerebral infarction Comparator 2: no fluoxetine and conventional therapy of cerebral infarction |
| Outcomes | Primary outcome at days 15, 90, and 180
Secondary outcome at days 90 and 180
|
| Notes | ChiCTR‐TRC‐15007658 xuanyi_guo@163.com Baseline demographic and clinical characteristics for each group not presented, but rather the baseline demographic and clinical characteristics for those completing the trial (i.e. a subset of all those randomised at baseline) are presented |
He 2018.
| Methods | Study type: interventional (clinical trial) Actual enrolment: 404 Allocation: randomised Intervention model: parallel assignment Masking: single (outcomes assessor) Primary purpose: prevention |
| Participants | Country: China Setting: inpatient At randomisation numbers allocated: N = 404 Experimental group: fluoxetine n = 202 Comparator group n = 202 % male: 70.5% Age: Experimental: 61.14 ± 10.48; Comparator 62.72 ± 11.86 Subtype of stroke: unclear Severity of stroke NIHSS score at baseline: Experimental: Median 6 (IQR 4, 8) Comparator: Median 5 (IQR 3, 8) Time since stroke onset: mean days, fluoxetine 4.28 ± 1.89; placebo 4.08 ± 2.15 Inclusion criteria
Exclusion criteria
Withdrawal criteria
|
| Interventions | Experimental: 20 mg of fluoxetine a day for 90 days and conventional therapy Comparator: conventional therapy |
| Outcomes |
|
| Notes | ChiCTR‐TRC‐12002078 xuanyi_guo@163.com |
Jurcau 2016.
| Methods | Study type: interventional (clinical trial) Actual enrolment: 89 Allocation: randomised Intervention model: parallel assignment Masking: unclear Primary purpose: treatment |
| Participants | Country: Romania Setting: inpatient At randomisation numbers allocated: N = 89 Experimental group: escitalopram = 43 Comparator group: ?secondary preventive treatment = 46 % male: unclear Age: unclear Subtype of stroke: unclear Severity of stroke: unclear Time since stroke onset: unclear Inclusion criteria: unclear Exclusion criteria: unclear withdrawal criteria: unclear |
| Interventions | Experimental: escitalopram 10 mg/day for 12 weeks Comparator: ?secondary preventive treatment = 46 |
| Outcomes | Outcomes collected at 3, 6 and 12 months post‐stroke
|
| Notes | Does not appear to be a clinical trial register number |
NCT00967408.
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 200 participants Allocation: randomised Intervention model: parallel assignment Masking: quadruple (participant, care provider, investigator, outcomes assessor) Primary purpose: treatment |
| Participants | Country: Italy Setting: inpatient Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: escitalopram and rehabilitation. Escitalopram given 5 mg once a day for the first week, 10 mg once a day from the second to fourth week, and 20 mg daily until the 6th month Comparator: placebo and rehabilitation |
| Outcomes | Primary outcome collected at 2 and 6 months
Secondary outcomes collected at 2 and 6 months:
|
| Notes | clinicaltrials.gov/ct2/show/NCT00967408 Contacted author Prof Cisari; response received; data being analysed |
BDI: Beck Depression Inventory BI: Bathel Index FIM: Functional Independence Measure HAM‐D17: Hamilton Depression Scale ICD‐10: International Statistical Classification of Diseases, 10th revision IQR: interquartile range MMSE: Mini‐Mental State Examination NIHSS: National Institutes of Health Stroke Scale
Characteristics of ongoing studies [ordered by study ID]
ChiCTR1800019467.
| Study name | The effect and mechanism of fluoxetine on the automatic regulation of cerebral blood flow for ischemic stroke |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: Allocation: randomised Intervention model: parallel assignment Masking: unclear Primary purpose: treatment |
| Participants | China Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: 20 mg of fluoxetine daily for 90 days Comparator: conventional therapy |
| Outcomes | Baseline, 30 days after treatment, 90 days after treatment, 180 days after treatment Automatic regulation of cerebral blood flow |
| Starting date | |
| Contact information | |
| Notes |
CTRI/2018/12/016568.
| Study name | An interventional study to look at efficacy of fluoxetine in patients with post‐stroke anxiety |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 60 participants Allocation: randomised Intervention model: parallel assignment Masking: triple (participant, investigator and outcome assessor) Primary purpose: treatment |
| Participants | Country: India Setting: inpatient Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: 20 mg of fluoxetine orally, daily for 12 weeks Comparator: standard care |
| Outcomes | Primary and secondary outcomes at 12 weeks Primary outcome
Secondary outcomes
|
| Starting date | December 2018 |
| Contact information | Dr Deepti Vibha, deeptivibha@gmail.com |
| Notes |
EudraCT 2005‐005266‐37.
| Study name | Influence of escitalopram on the incidence of depression and dementia following acute middle cerebral artery territory infarction. A randomised, placebo‐controlled, double‐blind study |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 60 participants Allocation: randomised Intervention model: parallel assignment Masking: double (detail unclear) Primary purpose: prevention |
| Participants | Country: Germany Setting: inpatient Inclusion criteria
Exclusion criteria
Aiming to recruit 60 participants |
| Interventions | Experimental: escitalopram Comparator: placebo |
| Outcomes | Depression (MADRS) after 180 days Incidence of dementia after 180 days (Clinical Dementia Rating scale) Severity of dementia Zarit Burden Interview Incidence of depression (Depression Visual Analogue Scale) Severity of post‐stroke depression Quality of life (SF‐36) Bayer Activities of Daily Living score NPI |
| Starting date | MHRA approval 7 April 2006; start date not known |
| Contact information | Not available. National Competent Authority is Germany‐BFarm Sponsor Name: Central Institute for Mental Health, Mannheim, Division of Gerontopsychiatry |
| Notes | Details available on EudraCT website www.clinicaltrialsregister.eu/ctr‐search/trial/2005‐005266‐37/DE |
IRCT201112228490N1.
| Study name | Effect of fluoxetine on functional recovery of patients with cerebrovascular accident following middle cerebral artery trunk obstruction: a randomised clinical trial |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 60 participants Allocation: randomised Intervention model: parallel assignment Masking: unclear Primary purpose: treatment |
| Participants | Iran (Islamic Republic of Iran) Inclusion criteria
Exclusion criteria
|
| Interventions | Intervention: fluoxetine, 15 mg oral pill for the first month and 20 mg for the next 2 months Comparator: placebo, 15 mg oral pill for the first month and 20 mg for the next 2 months |
| Outcomes | Primary outcomes collected at discharge, 1 and 3 months
Secondary outcomes collected at discharge
|
| Starting date | 5 April 2012 |
| Contact information | Dr Babak Bakhshayesh Eghbali Poorsina hospital, Guilan University of Medical Sciences bakhshayesh@gums.ac.ir |
| Notes |
IRCT201112228490N1 Contacted 7 February 2019 |
IRCT2012101011062N1.
| Study name | A study of sertraline effect on quality of life in stroke inpatients |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 80 participants Allocation: randomised Intervention model: parallel assignment Masking: unclear Primary purpose: prevention |
| Participants | Iran (Islamic Republic of Iran) Inclusion criteria
Exclusion criteria
Aiming to recruit 80 participants |
| Interventions | Experimental: 3 weeks after stroke sertraline 50 mg a day for 12 months versus Comparator: 3 weeks after stroke a placebo tablet every day |
| Outcomes | Primary outcomes collected at 3 months, 6 months, 9 months
Secondary outcomes collected at 3 months, 6 months, 9 months
|
| Starting date | 28 November 2012. Contacted author for an update on 4 May 2021 but no response received |
| Contact information | Reza Pirzeh, Tabriz University of Medical Sciences, Iran (Islamic Republic of) pirzehr@tbzmed.ac.ir |
| Notes | IRCT2012101011062N1 |
IRCT2017041720258N37.
| Study name | Evaluation of fluoxetine and standard treatment efficacy on change to side effect of stroke of ischaemic strokes in both hemispheres in anterior circulation |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 60 participants Allocation: randomised Intervention model: parallel assignment Masking: unclear Primary purpose: treatment |
| Participants | Islamic Republic of Iran Inclusion criteria
Exclusion criteria
Aiming to recruit 60 participants |
| Interventions | Experimental: 20 milligram fluoxetine and standard treatment (antiplatelets, anticoagulant and statin) Comparator: placebo and standard treatment (antiplatelets, anticoagulant and statin) |
| Outcomes | Primary outcome collected at 1 and 2 months
|
| Starting date | 11 October 2017. Trials register states it's complete but no results are available (email to author on 4 May 2021, no reply) |
| Contact information | Fariba Farokhi, Arak University of Medical Sciences Iran (Islamic Republic of Iran) f.farokhi@arakmu.ac.ir |
| Notes | www.irct.ir/trial/17976 |
IRCT20210307050617N1.
| Study name | The efficacy comparison of fluoxetine and citalopram on motor recovery after ischemic stroke: single‐blind placebo‐controlled randomized clinical trial |
| Methods | 3 arm RCT‐ citalopram, fluoxetine or placebo |
| Participants | Ischaemic stroke, at least 18 years old, hemiparesis or hemiplegia after the first ischaemic stoke in 24 hours. A score greater than 2 NIHSS on the motor items |
| Interventions | Fluoxetine 20 mg daily for 3 months or citalopram 10 mg for first 10 days then 20 mg daily. Placebo‐starch given for 3 months |
| Outcomes | Rate of improvement in motor function |
| Starting date | 22 August 2020 |
| Contact information | sepanta1968@yahoo.com |
| Notes |
NCT02386475.
| Study name | Effect of serotonin and levodopa in ischemic stroke (SELEIS) |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 240 participants Allocation: randomised Intervention model: parallel assignment Masking: single (outcomes assessor) Primary purpose: treatment |
| Participants | Country: Spain Setting: inpatient Inclusion criteria:
Exclusion criteria:
Aiming to recruit 240 participants. |
| Interventions | Placebo comparator: placebo Active comparator: citalopram 20 mg Active comparator: sinemet plus 100 mg Sinemet plus + citalopram group |
| Outcomes | Rankin Scale at 12 months |
| Starting date | 1 January 2015. Study completed 31 October 2019. No results available‐contacted author on 4 May 2021 |
| Contact information | Dolores Cocho mailto:dcocho%40fhag.es?subject=NCT02386475, SELEIS, Effect of Serotonin and Levodopa in Ischemic Stroke |
| Notes | NCT02386475 |
NCT02767999.
| Study name | Resting state MRI connectivity in acute ischemic stroke: serotonin selective reuptake Inhibitor (SSRI) in enhancing motor recovery: a placebo controlled study |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 60 participants Allocation: randomised Intervention model: parallel assignment Masking: double (participant, investigator) Primary purpose: treatment |
| Participants | Country: France Setting: inpatient Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: 20 mg of fluoxetine capsule a day from day 0 to day 90 and have fMRI Comparator: cellulose placebo a day from day 0 to day 90 and have fMRI |
| Outcomes | Primary outcome at 90 days
Secondary outcome at 90 days
|
| Starting date | January 2016 |
| Contact information | Virginie Sattler, Dr: sattler.v@chu‐toulouse.fr François Chollet, MD PhD: chollet.f@chu‐toulouse.fr |
| Notes | NCT02767999 |
NCT02865642.
| Study name | Cortical Ischemic Stroke and Serotonin (CISS) |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 90 participants Allocation: randomised Intervention model: parallel assignment Masking: quadruple (participant, care provider, investigator, outcomes assessor) Primary purpose: supportive care |
| Participants | Country: Switzerland Setting: inpatient Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: escitalopram 5 mg/day at the baseline visit (day 14 (±7) post‐stroke) for 7 days followed by a weekly dosage increase of 5 mg/day till target dose of escitalopram 20 mg/day. Participants remain on escitalopram 20 mg/day until visit 3 (day 90 (±14) post‐stroke) followed by dosage reduction of escitalopram 10 mg/day for 1 week Comparator: placebo 5 mg/day at the baseline visit (day 14 (±7) post‐stroke) for 7 days followed by a weekly dosage of 5 mg/day until target dose of placebo 20 mg/day. Participants remain on placebo 20 mg/day until visit 3 (day 90 (±14) post‐stroke) followed by placebo 10 mg/day for 1 week |
| Outcomes | Primary outcome
Secondary outcomes
Other outcomes
|
| Starting date | August 2016 |
| Contact information | Manuela Pastore‐Wapp manuela.pastore‐wapp@insel.ch |
| Notes | NCT02865642 |
NCT03448159.
| Study name | FLuoxetine Opens Window to improve motor recovery after stroke (FLOW) |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 176 participants Allocation: randomised Intervention model: parallel assignment Intervention model description
Masking: quadruple (participant, care provider, investigator, outcomes assessor) Primary purpose: treatment |
| Participants | Country: Canada Setting: inpatient Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: fluoxetine hydrochloride (Prozac): 10 mg Prozac per day for 3 to 5 weeks and then 20 mg for 12 weeks (the duration of the exercise intervention) Comparator: an over‐encapsulated placebo (identical 'sugar pill'): 10 mg 'sugar pill' a day for 3 to 5 weeks and then 20 mg for 12 weeks (the duration of the exercise intervention) |
| Outcomes | Primary outcomes at 12 weeks
Secondary outcomes at 12 weeks and 6 months
|
| Starting date | 1 November 2018 |
| Contact information | Farrell Leibovitch mailto:farrell%40canadianstroke.ca?subject=NCT03448159, 17‐5134.0, Fluoxetine Opens Window to Improve Motor Recovery After Stroke |
| Notes | NCT03448159 |
NCT03826875.
| Study name | Depression in haemorrhagic stroke |
| Methods | Study type: interventional (clinical trial) Estimated enrolment: 224 participants Allocation: randomised Intervention model: parallel assignment Intervention model description: double‐blinded placebo‐controlled randomised trial Masking: triple (participant, care provider, investigator) Primary purpose: prevention |
| Participants | Country: USA Setting: inpatient Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: fluoxetine 20 mg/day for a period of 1 year Comparator: placebo 20 mg/day for a period of 1 year |
| Outcomes | Primary outcomes at 1 year
Secondary outcomes at 1 year:
|
| Starting date | 1 March 2019 |
| Contact information | Cory M Kelly: kellycm@neurosurgery.washington.edu |
| Notes | NCT03826875 |
TCTR20181216001.
| Study name | Randomized controlled trial of fluoxetine or placebo on quality of life after acute ischemic stroke |
| Methods | Study type: interventional (clinical trial) Allocation: randomised Intervention model: parallel assignment Masking: double blind (no detail) Primary purpose: efficacy |
| Participants | Country: Thailand Setting: inpatient Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: fluoxetine 20 mg once daily for 90 days Comparator: matching placebo once daily for 90 days |
| Outcomes | Primary outcomes at 3 months
Secondary outcomes at 3 months
|
| Starting date | 1 January 2019 |
| Contact information | Sirikanya Lorwatanapongsa: sirikanyalor@yahoo.com |
| Notes | TCTR20181216001 |
BDI: Beck Depression Inventory; BDNF: brain‐derived neurotrophic factor; BI: Barthel Index; CTIMP: Clinical Trial of an Investigational Medicinal Product; DWI: diffusion‐weighted imaging; FLAIR: fluid‐attenuated inversion recovery; FMMS: Fugl Meyr Motor Score; fMRI: functional magnetic resonance imaging; HAM‐A:Hamilton Anxiety Rating Scale; HAM‐D: Hamilton Depression Rating Scale; JTT: Jebsen Taylor Test; MADRS: Montgomery‐Åsberg Depression Rating Scale; MAOI: mono‐amino‐oxidase inhibitor; MCA: middle cerebral artery; MHRA: Medicines and Healthcare products Regulatory Agency MRA: magnetic resonance angiography; MRI: magnetic resonance imaging; mRS: modified Rankin score; NHP: Nottingham Health Profile; NIHSS: National Institute of Health Stroke Scale NPI: Neuropsychiatric Inventory Scale; PHQ‐9: Patient Health Questionnaire; QoL: quality of life; RCT: randomised controlled trial; rTMS: repetitive transcranial magnetic stimulation; SF‐36: Short Form‐36; smRSq: simplified modified Rankin Scale questionnaire; SSRI: selective serotonin reuptake inhibitor; TCD: transcranial Doppler; TIA: transient ischaemic attack;
Differences between protocol and review
Changes to 'Criteria for considering studies for this review'
We did not change the criteria since the last update.
Changes to 'Data collection and analysis'
We included cognition as a secondary outcome.
Changes to Results
We added in new eligible studies, and updated all analyses.
Contributions of authors
Gillian Mead conceived the study, screened references, extracted data, assessed risk of bias, performed the analyses and wrote the first draft of this update.
Lynn Legg searched for studies selected studies for inclusion, collected data, assessed risk of bias, managed studies through the review process, contributed to the final version.
Russel Tilney screened citations, retrieved potentially relevant papers and screened their eligibility, assisted with data extraction, performed risk of bias assessments.
Cheng Fang Hsieh screened citations, retrieved potentially relevant papers and screened their eligibility, assisted with data extraction, performed risk of bias assessments and approved the final version.
Simiao Wu screened citations, retrieved potentially relevant papers and screened their eligibility, assisted with data extraction, performed risk of bias assessments and approved the final version.
Erik Lundström screened citations, retrieved potentially relevant papers and screened their eligibility, assisted with data extraction performed risk of bias assessments and approved the final version.
Xing Hua screened citations, retrieved potentially relevant papers, assisted with data extraction, performed risk of bias assessments and approved the final version.
Linnea Lindgren screened citations, retrieved potentially relevant papers, assisted with data extraction, performed risk of bias assessments and approved the final version
Ann‐Sofie Rudberg screened citations, retrieved potentially relevant papers and screened their eligibility, assisted with data extraction, performed risk of bias assessments and approved the final version.
Mansur Kutlubaev screened citations, retrieved potentially relevant papers and screened their eligibility, assisted with data extraction, performed risk of bias assessments and approved the final version.
Amanda Barugh screened citations, retrieved potentially relevant papers and screened their eligibility, assisted with data extraction, drafted the manuscript for submission, performed risk of bias assessments and approved the final version.
Maree Hackett screened citations, retrieved potentially relevant papers and screened their eligibility, assisted with data extraction, performed risk of bias assessments and approved the final version.
Graeme Hankey conceived the review, provided expertise in relation to analysis methods, and approved the final version of the review.
Martin Dennis provided topic expertise, advised on methods of analysis and approved the final version.
Sources of support
Internal sources
-
National Health and Medical Research Council of Australia, Australia
Maree Hackett: Career Development Fellowship, Population Health (Level 2), APP1141328 (1/1/18‐31/12/21)
External sources
-
Chief Scientist Office, Scotland, UK
The Chief Scientist Office, Scotland, provides infrastructure support for Cochrane Stroke
-
Incentive grant from National Institute of Health Research, UK
£5000 incentive grant to support an honorarium to Lynn Legg
-
NIHR Incentive grant, UK
£7000 to backfill some of Gillian Mead's academic time to enable her to work on this review.
Declarations of interest
Lynn A Legg: none known.
Ann‐Sofie Rudberg: none known.
Xing Hua: none known.
Simiao Wu: none known.
Maree L Hackett: Grants and contracts: Project grant (NHMRC funding for AFFINITY trial), HTA Program (National Institute for Health Research funding for FOCUS), Framework grant (Swedish Research Council funding for EFFECTS); all funding received by the author's institution. Payment for a fellowship: National Health and Medical Research Council (NHMRC), received by the author's institution.
Russel Tilney: none known.
Linnea Lindgren: none known.
Mansur A Kutlubaev: none known.
Cheng‐Fang Hsieh: none known.
Amanda Barugh: none known.
Graeme J Hankey: Grants and contracts: Chief Investigator for the AFFINITY trial, National Health and Medical Research Council of Australia, received by the author's institution. Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events: Discussion about antithrombotic therapy to prevent stroke, Medscape, received by the author. Consulting fees: Consulting on design of a possible phase III trial of a new anticoagulant in atrial fibrillation, Janssen Research and Development, received by the author. Payment for participation on a Data Safety Monitoring Board, Advisory Board, or Guideline Panel: Chair or Member of Data Safety Monitoring Committees, of ACI trials of an immune therapies for Alzheimer's disease, AC Immune, Lausanne, Switzerland, received by the author; Member of Stroke Prevention Initiative, Bayer, received by the author; Other: Associate Editor of Circulation, American Heart Association, received by the author. Published opinions in medical journals, the public press, broadcast and social media relevant to the interventions in the work: Publication, Lancet Neurology, AFFINITY Trial Collaboration. Safety and efficacy of fluoxetine on functional outcome after acute stroke (AFFINITY): a randomised, double‐blind, placebo‐controlled trial. Lancet Neurology 2020; 19(8): 651‐660. doi: 10.1016/S1474‐4422(20)30207‐6. PMID: 32702334; Publication, Stroke. Declaring involvement in eligible studies: Yes, National Health and Medical Research Council of Australia (for AFFINITY trial).
Erik Lundström: Grants and contracts: Funding, STROKE‐Riksförbundet, received by author's institution. Leadership or other fiduciary role in other board, society, committee, or advocacy group: Chief Investigator of the EFFECTS trial, received by author. Declaring involvement in eligible studies: The Swedish Research Council, The Swedish Heart‐Lung Fund, The Swedish Brain Fund, STROKE‐Riksförbundet, The Swedish Medical Society, Konung Gustaf V:s och Drottning Victorias Frimurarstiftelse.
Martin Dennis: Grants and contracts: Grants received to carry out FOCUS trial ‐ and RCT which is included in the review, NIHR, Stroke Association, received by the author's institution
Gillian E Mead: Grants and contracts: Research grants, HTA NIHR, co‐applicant on grants led by Prof Graeme Hankey and Maree Hackett, and Erik Lundstrom; NIHR incentive award for updating this review, both received by the author's institution.
Gillian Mead, Martin Dennis, Maree Hackett, Erik Lundstrom and Graeme Hankey are investigators on the FOCUS trial (Fluoxetine or control under supervision) in the UK, the AFFINITY (Assessment of fluoxetine in stroke recovery) trial in Australia, and the EFFECTs trial in Sweden designed to assess the impact of fluoxetine on disability and dependency after stroke. None of these review authors extracted data from these three trials.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Acler 2009 {published data only}
- Acler M, Avesani A, Fiaschi A, Manganotti P. Serotonergic modulation of brain excitability and motor recovery in patients affected by stroke. A double blind placebo RCT. International Journal of Stroke 2008;3:336. [Google Scholar]
- Acler M, Robol E, Fiaschi A, Manganotti P. A double blind placebo RCT to investigate the effects of serotonergic modulation on brain excitability and motor recovery in stroke patients. Journal of Neurology 2009;256(7):1152-8. [DOI] [PubMed] [Google Scholar]
AFFINITY 2020 {published data only}
- ACTRN12611000774921. Assessment of fluoxetine in stroke recovery (AFFINITY) trial, 2011. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12611000774921 (first received 22 July 2011).
- ACTRN12619000986178. The assessment of fluoxetine in stroke recovery imaging and blood biomarkers sub-study AFFINITY BM. www.anzctr.org.au/Trial/Registration/TrialReview.aspx ?ACTRN=12619000986178 (first received 11 July 2019).
- AFFINITY Trial Collaboration. Safety and efficacy of fluoxetine on functional outcome after acute stroke (AFFINITY): a randomised, double-blind, placebo-controlled trial. Lancet Neurology 2020;19(8):651-60. [DOI] [PubMed] [Google Scholar]
- Hankey G. Assessment oF FluoxetINe In sTroke recoverY (AFFINITY). www.affinitytrial.org/ (accessed 19th February 2019).
Almeida 2006 {published data only}
- Almeida OP, Waterreus A, Hankey GJ. Preventing depression after stroke: results from a randomized placebo-controlled trial. Journal of Clinical Psychiatry 2006;67(7):1104-9. [DOI] [PubMed] [Google Scholar]
Andersen 1994 {published data only}
- Andersen G, Vestergaard K, Lauritzen L. Effective treatment of post-stroke depression with selective serotonin reuptake inhibitors. Journal of Neurology 1994;241:S42. [DOI] [PubMed] [Google Scholar]
- Andersen G, Vestergaard K, Lauritzen L. Effective treatment of post-stroke depression with the selective serotonin reuptake inhibitor citalopram. Stroke 1994;25(6):1099-104. [DOI] [PubMed] [Google Scholar]
- Andersen G, Vestergaard K, Lauritzen L. Post-stroke depression treated with citalopram. Acta Neurologica Scandinavica 1994;89 Suppl 155:20. [Google Scholar]
- Andersen G, Vestergaard K, Lauritzen L. Post-stroke depression treated with citalopram - a selective serotonin reuptake inhibitor. Canadian Journal of Neurological Sciences 1993;20:S115. [Google Scholar]
- Andersen G, Vestergaard K, Lauritzen L. Post-stroke depression treated with citalopram a selective serotonin reuptake inhibitor. In: 7th Scandinavian Meeting on Cerebrovascular Disease. 1993:54.
- Andersen G, Vestergaard K, Lauritzen LU. Effective treatment of depression following apoplexy with citalopram. Ugeskrift for Laeger 1995;157(14):2000-3. [PubMed] [Google Scholar]
- Flicker C, Andersen G, Bayer L. A placebo controlled study of citalopram treatment for post-stroke depression. In: 11th Annual Meeting of the American Association for Geriatric Psychiatry. 1998.
Andersen 2013 {published data only}
- Andersen G. The efficacy of citalopram treatment in acute stroke (TALOS). www.clinicaltrials.gov/ct2/show/NCT01937182 (first received 9 September 2013).
- Damsbo AG, Mortensen JK, Kraglund KL, Johnsen SP, Andersen G, Blauenfeldt RA. Prestroke physical activity and poststroke cognitive performance. Cerebrovascular Diseases 2020;49(6):632-8. [DOI] [PubMed] [Google Scholar]
- Kraglund KL, Mortensen JK, Damsbo AG, Modrau B, Simonsen SA, Iversen, HK, et al. Neuroregeneration and vascular protection by citalopram in acute ischemic stroke (TALOS). Stroke 2018;49(11):2568-76. [DOI] [PubMed] [Google Scholar]
- Kraglund KL, Mortensen JK, Damsbo AG, Modrau B, Simonsen SA, Iversen HK, et al. Neuroregeneration and vascular protection by citalopramin in acute ischemic stroke (TALOS). Stroke 2018;49(11):2568-76. [DOI] [PubMed] [Google Scholar]
- Kraglund KL, Mortensen JK, Grove EL, Johnsen SP, Andersen G. TALOS: a multicenter, randomised, double blind, placebo controlled trial to test the effects of citalopram in patients with acute stroke; protocol. International Journal of Stroke 2015;10:985-87. [DOI] [PubMed] [Google Scholar]
- Kraglund KL, Mortensen JK, Johnsen SP, Andersen G, Grove EL. Antiplatelet effects of citalopram in patients with ischaemic stroke: a randomized, placebo-controlled, double-blind study. Scientific Reports 2019;9(1):200482019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Asadollahi 2018 {published data only}
- Asadollahi M, Ramezani M, Khanmoradi Z, Karimialavijeh E. The efficacy comparison of citalopram, fluoxetine, and placebo on motor recovery after ischemic stroke: a double-blind placebo-controlled randomized controlled trial. Clinical Rehabilitation 2018;32(8):1069-75. [DOI] [PubMed] [Google Scholar]
Bembenek 2020 {published data only}
- Bembenek JP, Niewada M, Klysz B, Mazur A, Kurczych K, Gluszkiewicz M, et al. Fluoxetine for stroke recovery improvement - the doubleblind, randomised placebo-controlled FOCUS-Poland trial. Neurologia i Neurochirurgia Polska 2020;54(6):544-51. [DOI] [PubMed] [Google Scholar]
- Fluoxetine or control under supervision: Poland. Polish Office for Registration of Medicinal Products, Medical Devices and Biocidal Products - EduraCT No: 2014-001335-37 2014.
Birchenall 2019 {published and unpublished data}
- Birchenall J, Térémetz M, Roca P, Lamy JC, Oppenheim C, Maier MA, et al. Individual recovery profiles of manual dexterity, and relation to corticospinal lesion load and excitability after stroke - a longitudinal pilot study. Neurophysiologie Clinique 2019;49(2):149-64. [DOI] [PubMed] [Google Scholar]
- NCT02063425. Evaluation by transcranial magnetic stimulation of the benefit of fluoxetine on motor recovery after stroke (EFLUSTIM). clinicaltrials.gov/ct2/show/NCT02063425 (first received 14 February 2014).
Brown 1998 {published data only}
- Brown KW, Sloan RL, Pentland B. Fluoxetine as a treatment for post-stroke emotionalism. Acta Psychiatrica Scandinavica 1998;98(6):455-8. [DOI] [PubMed] [Google Scholar]
Burns 1999 {published data only}
- Burns A, Russell E, Stratton-Powell H, Tyrell P, O'Neill P, Baldwin R. Sertraline in stroke-associated lability of mood. International Journal of Geriatric Psychiatry 1999;14(8):681-5. [PubMed] [Google Scholar]
Cao 2020 {published data only}
- Cao JX, Liu L, Sun YT, Zeng QH, Wang Y, Chen JC. Effects of the prophylactic use of escitalopram on the prognosis and the plasma copeptin level in patients with acute cerebral infarction. Brazilian Journal of Medical and Biological Research 2020;53(11):e8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao JX, Liu L, Sun YT, Zeng QH, Yang ZD, Chen JC. Escitalopram improves neural functional prognosis and endothelial dysfunction in patients with acute cerebral infarction. Restorative Neurology and Neuroscience 2020;38(5):385-93. [DOI] [PubMed] [Google Scholar]
Chen 2001 {published data only}
- Chen WY, Liu FY, Yang AP. Study of effect of integrative Chinese herbs with fluoxetine on rehabilitation of neurological impairment in patients with post-stroke depression. Journal of Chengdu University of Traditional Chinese Medicine 2001;24(4):20-3. [Google Scholar]
Chen 2002 {published data only}
- Chen W, Wang G-F, Chen X-H, Sheng Y-L, Zhu H. Effects of paroxetine on function recovery in patients with post-stroke depression. Chinese Journal of Clinical Rehabilitation 2002;6(13):2014-5. [Google Scholar]
Chen 2005a {published data only}
- Chen KN. Changes of neurotransmitter in patients with post-stroke depression observed with encephalofluctuography technology. Chinese Journal of Clinical Rehabilitation 2005;9(16):118-9. [Google Scholar]
Chen 2005b {published data only}
- Chen T, Li J, Han M. A study on paroxetine in the treatment for post-stroke depression. Jiangxi Medicine 2005;40(7):382-4. [Google Scholar]
Chen 2015 {published data only}
- Chen Z, Xu X, Wu Y, Huang L. Clinical efficacy of drug intervention in patients with acute depression after stroke. International Journal of Psychiatry 2015;42(5):97-100. [Google Scholar]
Cheng 2003 {published data only}
- Cheng F, Shao G, Bao S. Study of effect on neurologic function rehabilitation in patient with post-stroke depression. Chinese Journal of Clinical Rehabilitation 2003;7(1):108-9. [Google Scholar]
Chollet 2011 {published data only}
- Chollet F, Tardy J, Albucher J-F, Thalamas E, Berard E, Lamy C, et al. Fluoxetine for motor recovery after acute ischaemic stroke (FLAME): a randomised placebo-controlled trial. Lancet Neurology 2011;10(2):123-30. [DOI] [PubMed] [Google Scholar]
Dam 1996 {published data only}
- Dam M, Tonin P, De Boni A, Pizzolato G, Casson S, Ermani M, et al. Effects of fluoxetine and maprotiline on functional recovery in poststroke hemiplegic patients undergoing rehabilitation therapy. Stroke 1996;27(7):1211-4. [DOI] [PubMed] [Google Scholar]
Dike 2019 {published data only}
- Dike F. Pharmacological enhancement of motor function recovery in patients with ischaemic stroke: a trial of fluoxetine. www.pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=967 (last accessed 16 February 2021).
- Dike FO, Ekeh BC, Ogun AS, Ekrikpo EU, Walshak P, Ogunniy AA. Pharmacological enhancement of motor function recovery in patients with ischaemic stroke: a trial of fluoxetine. Journal of Neurology and Stroke 2019;9(1):47-51. [Google Scholar]
EFFECTS 2020 {published data only}
- EFFECTS Trial Collaboration. Safety and efficacy of fluoxetine on functional recovery after acute stroke (EFFECTS): a randomised, double-blind, placebo-controlled trial. Lancet Neurology 2020;19(8):661-9. [DOI] [PubMed] [Google Scholar]
- ISRCTN13020412. Establishing the effect(s) and safety of fluoxetine initiated in the acute phase of stroke. www.isrctn.com/ISRCTN13020412 (first received 19 December 2014).
- Lundström E, Isaksson E, Näsman P, Wester P, Mårtensson B, Norrving B. Correction to: Update on the EFFECTS study of fluoxetine for stroke recovery: a randomised controlled trial in Sweden. Trials 2020;21(388):s13063-020-04327-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundström E, Isaksson E, Näsman P et al. Update on the EFFECTS study of fluoxetine for stroke recovery: a randomised controlled trial in Sweden. Trials 2020;21(233):s13063-020-4124-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundstrom E, Isaksson E, Nasman P, Wester P, Martensson B, Norrving B, et al. Safety and efficacy of fluoxetine on functional recovery after acute stroke (EFFECTS): a randomised, double-blind, placebo-controlled trial. Lancet Neurology 2020;19(8):661‐9. [DOI] [PubMed] [Google Scholar]
Feng 2004 {published data only}
- Feng B-L, Wang Q-C, Zheng-Yuan LI. Influence of Jieyu Huoxue decoction on rehabilitation of patients with depression after cerebral infarction. Journal of Chinese Integrated Medicine 2004;2(3):182-4. [DOI] [PubMed] [Google Scholar]
FOCUS 2019 {published data only}
- Anonymous. The FOCUS (Fluoxetine or Control under Supervision) trial results: effects of a 6 month course of fluoxetine on the Stroke Impact Scale, mood and fatigue in patients with stroke. www.ed.ac.uk/clinical-brain-sciences/research/completed-studies-trials/focus-stroke-trial (accessed 12 02 2021).
- Cook R, Thomas V, Martin R. Does fluoxetine improve recovery after stroke? BMJ 2019;364:1029. [DOI] [PubMed] [Google Scholar]
- Dennis M, Forbes J, Graham C, Hackett M, Hankey GJ, House A, et al. Fluoxetine to improve functional outcomes in patients after acute stroke: the FOCUS RCT. Health Technology Assessment 2020;24(22):1-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Forbes J, Graham C, Hackett ML, Hankey GJ, House A, et al. Fluoxetine and fractures after stroke: exploratory analyses from the FOCUS Trial. Stroke 2019;50(11):3280-2. [DOI] [PubMed] [Google Scholar]
- FOCUS Trial Collaboration. Effects of fluoxetine on functional outcomes after acute stroke (FOCUS): a pragmatic, double-blind, randomised, controlled trial. Lancet 2019;393(10168):265-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham C, Lewis S, Forbes J, Mead G, Hackett ML, Hankey GJ, et al. The FOCUS, AFFINITY and EFFECTS trials studying the effect(s) of fluoxetine in patients with a recent stroke: statistical and health economic analysis plan for the trials and for the individual patient data meta-analysis. Trials 2017;18(1):627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundstrom E, Dennis M, Mead G. The effects of fluoxetine on fracture risk after stroke: Further analyses from the focus trial. European Stroke Journal 2019;4 suppl 1:7142019. [Google Scholar]
- Mead G, Dennis M. Feasibility of reporting results of large randomised controlled trials to participants: experience from the Fluoxetine or Control under Supervision (FOCUS) trial. BMJ Open 2020;10(11):e0404922020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead G. Fluoxetine Or Control Under Supervision (FOCUS) trial: to establish the effect(s) of routine administration of Fluoxetine in patients with a recent stroke. www.isrctn.com/ISRCTN83290762 (first received 23 May 2012).
- Mead GE, Dennis MS, Innes K, MacLeod M, Sandercock PA, House A, et al. A multicentre randomised trial to establish the effect(s) of routine administration of fluoxetine in patients with a recent stroke (Fluoxetine Or Control Under Supervision, FOCUS). In: 21st European Stroke Conference. 2012:Abst OAID 26.
- Mead GE, Graham C, Billot L, Näsman P, Lundström E, Lewis S, on behalf of the FOCUS , AFFINITY and EFFECTS trialists. Update to the FOCUS, AFFINITY and EFFECTS trials studying the effect(s) of fluoxetine in patients with a recent stroke: statistical analysis plan for the trials and for the individual patient data meta-analysis. Trials 2020;21(1):971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead GE, Legg L, Tilney R, Hsieh CF, Wu S, Lundström E, et al. Fluoxetine for stroke recovery: meta-analysis of randomized controlled trials. International Journal of Stroke 2020;15(4):365-76. [DOI] [PubMed] [Google Scholar]
Fruehwald 2003 {published data only}
- Fruehwald S, Gatterbauer E, Rehak P, Baumhackl U. Early fluoxetine treatment of post-stroke depression: a three-month double-blind placebo-controlled study with an open-label long-term follow up. Journal of Neurology 2003;250(3):347-51. [DOI] [PubMed] [Google Scholar]
Gao 2017 {published data only}
- Gao J, Lin M, Zhao J, Bi S, Ni Z, Shang X. Different interventions for post-ischaemic stroke depression in different time periods: a single-blind randomized controlled trial with stratification by time after stroke. Clinical Rehabilitation 2017;31(7):71-81. [DOI] [PubMed] [Google Scholar]
GlaxoSmithKline 1998 {published data only}
- GlaxoSmithKline. An 8-week double-blind placebo controlled parallel group study to assess the efficacy and tolerability of paroxetine in patients suffering from depression following stroke. GSK Clinical Study Register www.gsk clinicalstudyregister.com (accessed 31 August 2012).
Gong 2020 {published data only}
- Gong L, Yang X, Feng Y, Fei Z, Wang M, Qin B, et al. The efficacy of integrative anti-depressive therapy on motor recovery after ischemic stroke: a randomized clinical trial. European Journal of Integrative Medicine 2020;35:101102. [Google Scholar]
Guo 2009 {published data only}
- Guo R-Y, Su L, Wang CX. Effects of Linggui Bafa on the therapeutic effect and quality of life in patients of post-stroke depression. Chinese Acupuncture & Moxibustion 2009;29(10):785-90. [PubMed] [Google Scholar]
He 2004 {published data only}
- He P. Randomized controlled observation on the effect of early application of fluoxetine in preventing depression after stroke. Chinese Journal of Clinical Rehabilitation 2004;8(28):6016-7. [Google Scholar]
He 2005 {published data only}
- He Y, Wang X, Xiao C. Prospective study of effects of paroxetine with mental intervention on depression and anxiety after stroke. Nervous Diseases and Mental Health 2005;5(1):6-13. [Google Scholar]
- Wang X, He Y, Xiao C-L. A clinical trial of paroxetine and psychotherapy in patients with post-stroke depression and anxiety. Chinese Mental Health Journal 2005;19:564-6. [Google Scholar]
He 2016 {published data only}
- ChiCTR-TRC-12002078. Multi-center randomized clinical study of antidepressant treatment (fluoxetine) on secondary prevention of ischemic stroke. www.chictr.org.cn/showprojen.aspx?proj=7471 (first received 3 April 2012).
- Guo Y, He Y, Tang B, Ma K, Cai Z, Zeng S, et al. Effect of using fluoxetine at different time windows on neurological functional prognosis after ischaemic stroke. Restorative Neurology and Neuroscience 2016;34:177-87. [DOI] [PubMed] [Google Scholar]
- He Y, Cai Z, Zeng S, Chen S, Tang B, Liang Y, et al. Effect of fluoxetine on three-year recurrence in acute ischemic stroke: a randomized controlled clinical study. Clinical Neurology and Neurosurgery 2018;168:1-6. [DOI] [PubMed] [Google Scholar]
- He Y-T, Tang B-S, Cai Z-L, Zeng S-L, Jiang X, Guo Yi. Effects of fluoxetine on neural functional prognosis after ischemic stroke: a randomized controlled study in China. Journal of Stroke and Cerebrovascular Diseases 2016;25(4):761-70. [DOI] [PubMed] [Google Scholar]
Hu 2002 {published data only}
- Hu Y, Suo A, Xiang L. The comparative study of the effectiveness of fluoxetine on the stroke patients with depressive symptoms. Shanghai Archives of Psychiatry 2002;14:149-50. [Google Scholar]
Hu 2018 {published data only}
- Hu H, Wang M. Effects of escitalopram on post-stroke depression and cognitive function of patients with neurological function. Hebei Medicine 2018;24(2):325-8. [Google Scholar]
Huang 2002 {published data only}
- Huang X-H. The clinical correlation study and the effect of fluoxetine intervention on poststroke depression. Chinese Journal of Clinical Rehabilitation 2002;6(15):2296-7. [Google Scholar]
Jia 2005 {published data only}
- Jia W. Effect of early intervention on recovery of motor function and recurrent stroke in patients with post-stroke depression. Chinese Journal of Clinical Rehabilitation 2005;9(12):4-5. [Google Scholar]
Kim 2017 {published data only}
- Kim JS, Lee E-J, Chang D-ll, Park J-H, Ahn SH, Cha J-K, et al. Efficacy of early administration of escitalopram on depressive and emotional symptoms and neurological dysfunction after stroke: a multicentre, double-blind, randomised, placebo-controlled study. Lancet Psychiatry 2017;4(1):33-41. [DOI] [PubMed] [Google Scholar]
- Lee EJ, Kim JS, Chang DI, Park JH, Ahn SH, Cha JK, et al. Differences in therapeutic responses and factors affecting post-stroke depression at a later stage according to baseline depression. Journal of Stroke 2018;20(2):258-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EJ, Kim JS, Chang DI, Park JH, Ahn SH, Cha JK, et al. Post-stroke depressive symptoms: varying responses to escitalopram by individual symptoms and lesion location. Journal of Geriatric Psychiatry and Neurology 2020;10:891988720957108. [DOI] [PubMed] [Google Scholar]
- Lee EJ, Oh MS, Kim JS, Chang DI, Park JH, Cha JK, EMOTION investigators. Serotonin transporter gene polymorphisms may be associated with poststroke neurological recovery after escitalopram use. Journal of Neurology, Neurosurgery and Psychiatry 2018;89(3):271-6. [DOI] [PubMed] [Google Scholar]
- NCT01278498. The preventative effect of escitalopram on depression and related emotional disorders in acute stroke patients, 2011. clinicaltrials.gov/ct2/show/NCT01278498 (first received 19 January 2011). [NCT01278498]
Kong 2007 {published data only}
- Kong Y. Fluoxetine for poststroke depression: a randomized placebo controlled clinical trial. Neural Regeneration Research 2007;2(3):162-5. [Google Scholar]
Lai 2006 {published data only}
- Lai J. The effect of using paroxetine to treat post stroke depression. Journal of Guangdong Medical College 2006;24(6):585-6. [Google Scholar]
Li 2004a {published data only}
- Li J, He Q-Y, Han M-F. Recent effect of fluoxetine in improving neurologic impairment and preventing post-stroke depression in the early stage. Chinese Journal of Clinical Rehabilitation 2004;8(7):1208-9. [Google Scholar]
Li 2004b {published data only}
- Li C-M, Jiang X-D, Liao G, Lei J-M, Lan S, Ni F-W. Effect of antidepressant drugs in early period on the recovery of post-stroke depression. Chinese Journal of Clinical Rehabilitation 2004;8(19):3713-5. [Google Scholar]
Li 2005 {published data only}
- Li Y, Wang X, Qian FS. Related factors of post-stroke depression and effect of paroxetine. Shandong Archives of Psychiatry 2005;18(4):209-10. [Google Scholar]
Li 2006 {published data only}
- Li W-Q, Li D-X. The efficacy of citalopram for post-stroke depression and its effects on stroke rehabilitation. International Journal of Cerebrovascular Diseases 2006;14(4):275-8. [Google Scholar]
Li 2007 {published data only}
- Li Z. Clinical efficacy of paroxetine in the treatment of post-stroke depression. Modern Journal of Integrated Traditional Chinese and Western Medicine 2007;16(34):5103-4. [Google Scholar]
Li 2008 {published data only}
- Li L-T, Wang S-H, Ge H-Y, Chen J, Yue S-W, Yu M. The beneficial effects of the herbal medicine free and easy wanderer plus (FEWP) and fluoxetine on post-stroke depression. Journal of Alternative and Complementary Medicine 2008;14(7):841-6. [DOI] [PubMed] [Google Scholar]
Li 2017 {published data only}
- Li J, Wang J, Li Y, Zhang W, Zhao J. Effects of escitalopram oxalate on post-stroke depression, cognition and neurological function. Journal of Hebei Medical University 2017;38(5):589-92. [Google Scholar]
Liu 2006 {published data only}
- Liu Y, Xu R. Effect of citalopram treatment on post-stroke depression and neurological functional rehabilitation. Chinese Journal of Rehabilitation 2006;21(3):174-5. [Google Scholar]
Marquez Romero 2013 {published data only}
- Marquez-Romero JM, Arauz A, Ruiz-Sandoval JL, Cruz-Estrada Ede L, Huerta-Franco MR, Aguayo-Leytte G, et al. Fluoxetine for motor recovery after acute intracerebral hemorrhage (FMRICH): study protocol for a randomized, double-blind, placebo-controlled, multicenter trial. Trials 2013;14:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez-Romero JM, Reyes-Martínez M, Huerta-Franco MR, Ruiz-Franco A, Silos H, Arauz A. Fluoxetine for motor recovery after acute intracerebral hemorrhage, the FMRICH trial. Clinical Neurology and Neurosurgery 2020;190:105656. [DOI] [PubMed] [Google Scholar]
- Marquez-Romero JM, Reyes-Martínez M, Huerta-Franco MR, Ruiz-Franco A, Silos H, Arauz A. Fluoxetine for motor recovery after acute intracerebral hemorrhage, the FMRICH Trial. Correspondence from Marquez-Romero 2018. [DOI] [PubMed]
- Marquez-Romero JM. Fluoxetine for motor recovery after acute intracerebral hemorrhage (FMRICH). www.clinicaltrials.gov/ct2/show/NCT01737541 (first received 29 November 2012).
Meara 1998 {published data only}
- Meara RJ, Thalanany M, Balonwu V, Hobson P. The treatment of depression after stroke with the selective serotonin reuptake inhibitor sertraline. Cerebrovascular Diseases 1998;8 Suppl 4:90. [Google Scholar]
Miao 2004 {published data only}
- Miao S-Y, Shi Y-J. Related factors of post-stroke depression and therapeutical effect of citalopram. Chinese Journal of Clinical Rehabilitation 2004;8(19):3718-9. [Google Scholar]
Murray 2005 {published data only}
- Murray V, Von Arbin M, Bartfai A, Berggren A-L, Landtblom A-M, Lumdmark J, et al. Double-blind comparison of sertraline and placebo in stroke patients with minor depression and less severe major depression. Journal of Clinical Psychiatry 2005;66(6):708-16. [DOI] [PubMed] [Google Scholar]
NCT00177424 {published data only}
- NCT00177424. Setraline for prevention post stroke depression and improving rehabilitation outcomes. clinicaltrials.gov/ct2/show/NCT00177424 (first received 15 September 2005).
NCT01674868 {published data only}
- NCT01674868. Fluoxetine for motor, aphasia, and neglect recovery after ischemic stroke (FLAN). www.clinicaltrials.gov/ct2/show/NCT01674868 (first received 29 August 2012).
NCT02737930 {published data only}
- NCT02737930. Fluoxetine for visual recovery after ischaemic stroke (FLUORESCE). www.clinicaltrials.gov/ct2/show/NCT02737930 (first received 14 April 2016).
Pan 2018 {published data only}
- Pan X-L, Chen H-F, Cheng X, Hu C-C, Wang J-W, Fu Y-M, et al. Effects of paroxetine on motor and cognitive function recovery in patients with non-depressed ischemic stroke: an open randomized controlled study. Brain Impairment;doi: 10.1017/BrImp.2018.6.
Pariente 2001 {published data only}
- Guiraud-Chaumeil B, Pariente J, Albucher J-F, Loubinoux I, Chollet F. Rehabilitation after stroke [Recuperation neurologique post-ischemique]. Bulletin de l'Académie Nationale de Médecine 2002;6:1015-24. [PubMed] [Google Scholar]
- Pariente J, Loubinoux I, Carel C, Albucher JF, Leger A, Manelfe C, et al. Fluoxetine modulates motor performance and cerebral activation of patients recovering from stroke. Annals of Neurology 2001;50(6):718-29. [DOI] [PubMed] [Google Scholar]
Rasmussen 2003 {published data only}
- Rasmussen A, Lunde M, Poulsen D, Sørensen K, Qvitzau S, Bech P. A double-blind placebo controlled study of sertraline in the prevention of depression in stroke patients. European Neuropyschopharmacology 2002;12:231. [DOI] [PubMed] [Google Scholar]
- Rasmussen A, Lunde M, Poulsen DL, Sørensen K, Qvitzau S, Bech P. A double-blind, placebo-controlled study of sertraline in the prevention of depression in stroke patients. Psychosomatics 2003;44(3):216-22. [DOI] [PubMed] [Google Scholar]
- Rasmussen A. Depression and stroke. Nordic Journal of Psychiatry 2001;55(4):288. [Google Scholar]
- Rasmussen A. Prophylactic treatment for post-stroke depression and comorbidity. Journal of Psychosomatic Research 2000;48(3):66. [Google Scholar]
Razazian 2014 {published data only}
- Razazian N, Esmaeili O, Almasi A. Effect of fluoxetine on motor improvement in ischemic stroke patients: a double blind clinical trial study. Zahedan Journal of Research in Medical Sciences 2016;18(7):e75492016. [Google Scholar]
- Razazian N. A survey for assessment of effectiveness of fluoxetine on motor improvement in ischemic stroke patients. www.en.irct.ir/trial/8797 (first received 9 January 2014).
Restifo 2001 {published data only}
- Restifo DA, Lo Prest R, Lanza S, Giuffrida S, D'Aleo G, Rifici Di Bella C, et al. Motor cortex reorganization induced by fluoxetine in poststroke hemiplegic patients undergoing rehabilitation therapy: a study with transcranial magnetic stimulation. Neurorehabilitation and Neural Repair 2001;15(4):284. [Google Scholar]
Robinson 2000a {published data only}
- Jorge RE, Robinson RG, Arndt S, Starkstein S. Mortality and post-stroke depression: a placebo controlled trial of antidepressants. American Journal of Psychiatry 2003;160:1823-9. [DOI] [PubMed] [Google Scholar]
- Narushima K, Kosier JT, Robinson RG. Preventing post-stroke depression: a 12 week double blind randomised treatment trial and 21 month follow-up. Journal of Nervous and Mental Diseases 2002;190:296-303. [DOI] [PubMed] [Google Scholar]
- Robinson RG, Schultz SK, Castillo C, Kopel T, Kosier JT, Newman RM, et al. Nortriptyline versus fluoxetine in the treatment of depression and in short-term recovery after stroke: a placebo-controlled, double-blind study. American Journal of Psychiatry 2000;157(3):351-9. [DOI] [PubMed] [Google Scholar]
Robinson 2000b {published data only}
- Jorge RE, Robinson RG, Arndt S, Starkstein S. Mortality and post-stroke depression: a placebo controlled trial of antidepressants. American Journal of Psychiatry 2003;160:1823-9. [DOI] [PubMed] [Google Scholar]
- Narushima K, Robinson RG. Preventing post-stroke depression: a 12 week double blind randomised treatment trial and 21 month follow-up. Journal of Nervous and Mental Diseases 2002;190:296-303. [DOI] [PubMed] [Google Scholar]
- Robinson RG, Schultz SK, Castillo C, Kopel T, Kosier JT, Newman RM, et al. Nortriptyline versus fluoxetine in the treatment of depression and in short-term recovery after stroke: a placebo-controlled, double-blind study. American Journal of Psychiatry 2000;157(3):351-9. [DOI] [PubMed] [Google Scholar]
Robinson 2008 {published data only}
- Jorge RE, Acion L, Moser D, Adams HP, Robinson RG. Escitalopram and enhancement of cognitive recovery following stroke. Archives of General Psychiatry 2010;67(2):187-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson RG, Arndt S. Incomplete financial disclosure in a study of escitalopram and problem solving therapy for prevention of post-stroke depression. JAMA 2009;301:1023-4. [DOI] [PubMed] [Google Scholar]
- Robinson RG, Jorge RE, Moser DJ, Acion L, Solodkin A, Small SL, et al. Escitalopram and problem-solving therapy for prevention of poststroke depression. JAMA 2008;299(20):2391-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
Savadi Oskouie 2012 {published data only}
- Savadi Oskouie D, Sharifipour E, Sadeghi Bazargani H, Hashemilar M, Nikanfar M, Ghazanfari Amlashi S, et al. Efficacy of citalopram on acute ischemic stroke outcome: a randomized clinical trial. Neurorehabilitation and Neural Repair 2017;31(7):638-47. [DOI] [PubMed] [Google Scholar]
- Savadi Oskouie D. Evaluation of the effect of citalopram on three months functional prognosis of acute ischemic stroke patients: a randomized clinical trial. www.en.irct.ir/trial/1766 (first received 22 April 2012).
Shah 2016 {published data only}
- Shah IA, Asimi RP, Kawoos Y, Wani MA, Wani MA, Dar MA. Effect of fluoxetine on motor recovery after acute haemorrhagic stroke: a randomized trial. Journal of Neurology and Neurophysiology 2016;7(2). [DOI: 10.4172/2155-9562.1000364] [DOI]
Song 2006 {published data only}
- Song J-G. Effects of fluoxetine hydrochloride on depressive symptoms and P300 after cerebral stroke. Chinese Journal of Clinical Rehabilitation 2006;10(14):160-2. [Google Scholar]
Wang 2003 {published data only}
- Wang X, Tan Z, Wu Z, Gao J, Feng M. The effects of anti-depression therapy on post-stroke depression and neurologic rehabilitation in the elderly patients. Chinese Journal of Geriatrics 2003;22(5):270-3. [Google Scholar]
Wang 2009 {published data only}
- Wang X. The efficacy of paroxetine in the treatment of post-stroke depression in 55 cases. Chinese Community Physician (Medical Professional Half-monthly) 2009;11(7):11. [Google Scholar]
Wen 2006 {published data only}
- Wen Z-X. The influence of post-stroke prophylactic anti-depression treatment on nerve functional rehabilitation. Acta Academiae Medicinae Qingdao Universitatis 2006;42(3):253-4. [Google Scholar]
Wiart 2000 {published data only}
- Wiart L, Petit H, Joseph PA, Mazaux JM, Barat M. Fluoxetine in early poststroke depression: a double-blind placebo-controlled study. Stroke 2000;31(8):1829-32. [DOI] [PubMed] [Google Scholar]
Xie 2005 {published data only}
- Xie R, Liu J, Quan H. A prospective random clinical contrast study of treatment with sertraline in elderly patients with post-stroke depression. Chinese Journal of Clinical Neuroscience 2005;13(3):294-7. [Google Scholar]
Xu 2001 {published data only}
- Xu J, Tan J, Ou L. A study on treatment of fluoxetine to depression in early recovery stage of cerebral infarction. Chinese Journal of Rehabilitation Medicine 2001;16(5):281-3. [Google Scholar]
Xu 2006 {published data only}
- Xu J, Wang J, Liu J. Preventive effects of antidepressants on post-stroke depression. Chinese Mental Health Journal 2006;20(3):186-8. [Google Scholar]
Yang 2002 {published data only}
- Yang J, Zhao Y, Bai S. Controlled study on antidepressant treatment of patients with post-stroke depression. Chinese Mental Health Journal 2002;16(12):871-2. [Google Scholar]
Yang 2011 {published data only}
- Yang J. Therapeutic effect of paroxetine on patients with early poststroke depression and the serum interleukins. Chinese Journal of Cerebrovascular Diseases 2011;8(5):235-8. [Google Scholar]
Ye 2004 {published data only}
- Ye L-X, Wang H, Wang Y-D, Zhong L, Liang D-S, Guo Y. Effect of anti-depressive therapy on the rehabilitation of psychological and neurological function after stroke. Chinese Journal of Clinical Rehabilitation 2004;8(31):6826-8. [Google Scholar]
- Ye LX. Effect of paxil and berhomine on post-stroke anxiety-depression and neurological recovery. Chinese Journal of Clinical Rehabilitation 2006;10(6):153-5. [Google Scholar]
Zhao 2011 {published data only}
- Zhao P, Wang J-P. Effects of antidepressants on neurofunctional recovery of post-stroke patients with aphasia. Journal of Dalian Medical University 2011;33(1):55-7. [Google Scholar]
Zhou 2008 {published data only}
- Zhou Z-l, Liang L-Z, Yan Y-X. Preventive effects of fluoxetine on post-stroke depression. Chinese Journal of Modern Applied Pharmacy 2008;25(3):263-4. [Google Scholar]
References to studies excluded from this review
ACTRN12619000573156 {published data only}
- ACTRN12619000573156. FRAMBOISE: Fluoxetine, Recovery And Motor BiOmarkers In StrokE. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=377306 (first received 11 April 2019).
Andersen 1993 {published data only}
- Andersen G, Vestergaard K, Riis JO. Citalopram for post-stroke pathological crying. Lancet 1993;342(8875):837-9. [DOI] [PubMed] [Google Scholar]
Andersen 2012 {published data only}
- Andersen G. Efficacy of escitalopram treatment in acute stroke and the role of specific genotypes in stroke. www.clinicaltrialsregister.eu/ctr-search/search?query=2011-005541-12 (first received 27 February 2012).
- Andersen G. Escitalopram Treatment In Acute Stroke (ESTIAS). www.clinicaltrials.gov/ct2/show/NCT01561092 (first received 22 March 2012).
Anderson 2002 {published data only}
- Anderson C, Hackett M, Carter K, Ni MC. Maximising outcome by overcoming depression in stroke (MOODS) trial. Cerebrovascular Diseases 2002 2002;13 Suppl 3:79. [Google Scholar]
Anonymous 2012a {published data only}
- Anonymous 2012. Stroke and depression. Johns Hopkins Medical Letter: Health After 50 2012;23(11):3. [PubMed] [Google Scholar]
Anonymous 2012b {published data only}
- Anonymous. Drug & Device News. Medical Malpractice Law & Strategy, New York Law Journal Newsletters 2012;30(2):5. [Google Scholar]
Berends 2009 {published data only}
- Berends HI, Nijlant JM, Putten MJ, Movig KL, IJzerman MJ. Single dose of fluoxetine increases muscle activation in chronic stroke patients. Clinical Neuropharmacology 2009;32(1):1-5. [also known as Flu 2006] [PubMed] [Google Scholar]
Bonin Pinto 2019 {published data only}
- Bonin Pinto C, Morales-Quezada L, Toledo Piza PV, Zeng D, Saleh Vélez FG, Ferreira IS, et al. Combining fluoxetine and rTMS in poststroke motor recovery: a placebo-controlled double-blind randomized phase 2 clinical trial. Neurorehabilitation and Neural Repair 2019;33:643-55. [DOI: 10.1177/1545968319860483.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02208466. Effects rTMS combined with fluoxetine on motor recovery in stroke patients. www.clinicaltrials.gov/ct2/show/NCT02208466 (first received 5 August 2014).
Chen 2019 {published data only}
- Chen Ma, Ping L. Effectiveness of paroxetine in the treatment of poststroke depression. Medicine 2018;97(29):1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi Kwon 2008 {published data only}
- Choi-Kwon S, Choi J, Kwon SU, Kang DW, Kim JS. Fluoxetine improves the quality of life in patients with poststroke emotional disturbances. Cerebrovascular Diseases 2008;26(3):266-71. [DOI] [PubMed] [Google Scholar]
Finkenzeller 2009 {published data only}
- Finkenzeller W, Zobel I, Rietz S, Schramm E, Berger M. Interpersonal psychotherapy and pharmacotherapy for post-stroke depression. Feasibility and effectiveness. Der Nervenarzt 2009;80(7):805-12. [DOI] [PubMed] [Google Scholar]
Foster 2019 {published data only}
- Foster E, Yaroslavtseva O, Chundamala J, Leibovitch F, Eng JJ, Ali F, et al. FLOW Trial: fluoxetine to open the critical period time window to improve motor recovery after stroke. International Journal of Stroke 2019;14 Suppl 3:36. [Google Scholar]
Gourab 2015 {published data only}
- Gourab K, Schmit BD, Hornby GT. Increased lower limb spasticity but not strength or function following a single-dose serotonin reuptake inhibitor in chronic stroke. Archives of Physical Medicine and Rehabilitation 2015;96(12):2112-9. [DOI] [PubMed] [Google Scholar]
Graffagnino 2002 {published data only}
- Graffagnino C. Poststroke depression and functional recovery (SADBRAIN). Duke University Medical Centre 2002.
Ji 2000 {published data only}
- Ji QM, Xie LP. Efficacy of fluoxetine in the treatment of 20 patients with depression after stroke. Herald of Medicine 2000;19(4):329. [Google Scholar]
Kitago 2020 {published data only}
- Dose-finding study of selective serotonin reuptake inhibitors to enhance neuroplasticity [Dose finding study but the intervention is a combination of an SSRI and paired associative stimulation, so we can exclude]. Source not provided from searches 2020.
Li 2002 {published data only}
- Li F, Gu DX, Ceng SH, Xu JW. Effect of paroxetine on prognosis of patients with post cerebral infarction depression. Chinese Journal of New Drugs and Clinical Remedies. 2002;21(1):11-3. [Google Scholar]
Liang 2003 {published data only}
- Liang Z, Shuliang T. Clinical efficacy of fluoxetine in treatment of patients with depression after acute stroke. Chinese Journal of Clinical Rehabilitation 2003;7(13):1924-5. [Google Scholar]
Liu 2004 {published data only}
- Liu L-X. Recent effect of drug intervention on post-stroke anxiety. Chinese Journal of Clinical Rehabilitation 2004;8(30):6600-1. [Google Scholar]
Liu 2020 {published data only}
- Liu W, Ding W. Study on the efficacy and mechanism of paroxetine hydrochloride combined with repetitive transcranial magnetic stimulation in the treatment of post-stroke depression. International Journal of Clinical and Experimental Medicine 2020;13(10):7881-8. [Google Scholar]
Mosarrezaii 2018 {published data only}
- Mosarrezaii A, Salmasi BA, Taghavi SA. Studying effect of fluoxetine on improvement of motor performance in patients with ischemic stroke. Journal of Research in Medical and Dental Sciences 2018;6(3):118-22. [Google Scholar]
NCT01963832 {published data only}
- NCT01963832. RCT of a neuroplasticity agent and CI therapy for severe arm paresis after stroke. clinicaltrials.gov/ct2/show/NCT01963832 (first received 16 October 2013).
Robinson 2011 {published data only}
- Robinson RG, Mikami K, Jang M, Jorge RE. Prevention of anxiety disorder after stroke. Journal of Neuropsychiatry and Clinical Neurosciences 2011;23(2):18. [Google Scholar]
Sitzer 2002 {published data only}
- Sitzer M, Huff W, Steckel R. Prevention of poststroke depression after acute ischemic stroke using the selective serotonin reuptake inhibitor sertraline (PreDis-study). Stroke 2002;33(2):651-2. [Google Scholar]
Sun 2015 {published data only}
- Sun YT, Bao YH, Wang SL, Chu JM, Li LP. Efficacy observation on the treatment of post-stroke depression by acupuncture at the acupoints based on ziwuliuzhu and Prozac. Chinese Acupuncture and Moxibustion 2015;355(2):119-22. [PubMed] [Google Scholar]
Vogel 2020 {published data only}
- Vogel AC, Okeng'o K, Chiwanga F, Ismail SS, Buma D, Pothier L. MAMBO: Measuring Ambulation, Motor, and Behavioral Outcomes with post-stroke fluoxetine in Tanzania: protocol of a phase II clinical trial. Journal of the Neurological Sciences 2020;408:116563. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2007 {published data only}
- Xu B, Zhou WY, Zhang SJ. Observation of effect of Wulung capsule in treating post-stroke depression. Chinese Journal of Integrated Traditional and Western Medicine 2007;27(7):640-2. [PubMed] [Google Scholar]
Zhou 2003 {published data only}
- Zhou B. Effects of fluoxetine on neurofunctional recovery of non depressed patients after stroke. Chinese Journal of Clinical Rehabilitation 2003;7(3):374-5. [Google Scholar]
References to studies awaiting assessment
Guo 2016 {published data only}
- Guo Y, He Y, Tang B, Ma K, Cai Z, Zeng S, et al. Effect of using fluoxetine at different time windows on neurological functional prognosis after ischemic stroke. Restorative Neurology and Neuroscience 2016;34(2):177–87. [DOI] [PubMed] [Google Scholar]
- Guo Y. Effect of using fluoxetine at different time windows after ischemic stroke on neurological functional prognosis: a randomized controlled trial. chictr.org.cn/showprojen.aspx?proj=12925 (first received 27 December 2015).
He 2018 {published data only}
- ChiCTR-TRC-12002078. Multi-center randomized clinical study of antidepressant treatment (fluoxetine) on secondary prevention of ischemic stroke. www.chictr.org.cn/showprojen.aspx?proj=7471 (first received 3 April 2012).
- He Y, Cai Z, Zeng S, Chen S, Tang B, Liang Y, et al. Effect of fluoxetine on three-year recurrence in acute ischemic stroke: a randomized controlled clinical study. Clinical Neurology and Neurosurgery 2018;168:1-6. [DOI] [PubMed] [Google Scholar]
Jurcau 2016 {published data only}
- Jurcau A, Simion A. Improved post-ischaemic stroke recovery over 1 year with escitalopram for 3 months. European Journal of Neurology 2016;23:614. [Google Scholar]
NCT00967408 {published data only}
- NCT00967408. Effects of clinical and functional outcome of escitalopram in adult stroke patients. clinicaltrials.gov/ct2/show/NCT00967408 (first received 27 August 2009). [NCT00967408]
References to ongoing studies
ChiCTR1800019467 {published data only}
- ChiCTR1800019467. The effect and mechanism of fluoxetine on the automatic regulation of cerebral blood flow for ischemic stroke. https://www.chictr.org.cn/showprojen.aspx?proj=32801.
CTRI/2018/12/016568 {published data only}
- CTRI/2018/12/016568. An interventional study to look at efficacy of fluoxetine in patients with post-stroke anxiety. http://ctri.nic.in CTRI/2018/12/016568 (first received 10 December 2018).
EudraCT 2005‐005266‐37 {published data only}2005‐005266‐37
- EudraCT 2005-005266-37. Influence of escitalopram on the incidence of depression and dementia following acute middle cerebral artery territory infarction. A randomised placebo-controlled double blind study. www.clinicaltrialsregister.eu/ctr-search/search?query=2005-005266-37 (first received 7 April 2006).
IRCT201112228490N1 {published data only}
- IRCT201112228490N1. Effect of fluoxetine on functional recovery of patients with cerebrovascular accident following middle cerebral artery trunk obstruction: a randomized clinical trial. www.en.irct.ir/trial/8954 (first received 25 January 2012).
IRCT2012101011062N1 {published data only}
- IRCT2012101011062N1. A study of sertraline effect on quality of life in stroke inpatients. www.en.irct.ir/trial/11413 (first received 28 November 2012).
IRCT2017041720258N37 {published data only}
- IRCT2017041720258N37. Evaluation of fluoxetine and standard treatment efficacy on change to side effect of stroke of ischemic strokes in both hemispheres in anterior circulation. www.irct.ir/trial/17976 (first received 11 October 2017).
IRCT20210307050617N1 {published data only}
- IRCT20210307050617N1. The efficacy comparison of fluoxetine and citalopram on motor recovery after ischemic stroke: single-blind placebo-controlled randomized clinical trial. https://en.irct.ir/trial/54896 (first received 27 March 2021).
NCT02386475 {published data only}
- NCT02386475. Effect of serotonin and levodopa in ischemic stroke. www.clinicaltrials.gov/ct2/show/NCT02386475 (first received 12 March 2015).
NCT02767999 {published data only}
- NCT02767999. Serotonin Selective Reuptake Inhibitor (SSRI) effects on cerebral connectivity in acute ischemic stroke (RECONISE). www.clinicaltrials.gov/ct2/show/NCT02767999 (first received 11 May 2016).
NCT02865642 {published data only}
- NCT02865642. Cortical ischemic stroke and serotonin (CISS). www.clinicaltrials.gov/ct2/show/NCT02865642 (first received 12 August 2016).
NCT03448159 {published data only}
- NCT03448159. Fluoxetine Opens Window to improve motor recovery after stroke (FLOW). www.clinicaltrials.gov/ct2/show/NCT03448159 (first received 27 February 2018).
NCT03826875 {published data only}
- NCT03826875. Depression in hemorrhagic stroke. www.clinicaltrials.gov/ct2/show/NCT03826875 (first received 1 February 2019).
TCTR20181216001 {published data only}
- TCTR20181216001. Randomized controlled trial of fluoxetine or placebo on quality of life after acute ischemic stroke. www.thaiclinicaltrials.org/show/TCTR20181216001 (first received 16 December 2018).
Additional references
Allida 2019
- Allida S, Patel K, House A, Hackett ML. Pharmaceutical interventions for emotionalism after stroke. Cochrane Database of Systematic Reviews 2019, Issue 3. Art. No: CD003690. [DOI: 10.1002/14651858.CD003690.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2021
- Deeks JJ, Higgins JP, Altman DG, editors. Chapter 10 : Analysing data and performing metaanalyses. In: Higgins JP , Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al( editor s) . ) , Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021) Cochrane 2021. Available at www.training.cochrane.org/handbook.
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
GBD 2015
- GBD 2015. Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study. Lancet 2016;388(10053):1545–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADE 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
GRADEproGDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime, Inc.) GRADEpro Guideline Development Tool [Software]. McMaster University (developed by Evidence Prime, Inc.), 2015.
Hatano 1976
- Hatano S. Experience from a multicentre stroke register: a preliminary report. Bulletin of the World Health Organization 1976;54(5):541-53. [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook.
Johnson 2016
- Johnson W, Onuma O, Owolabi M, Sachdev S. Stroke: a global response is needed. Bulletin of the World Health Organization 2016;94(9):634-634A. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lang 2004
- Lang UE, Jockers-Scherübl MC, Hellweg R. State of the art of the neurotrophin hypothesis in psychiatric disorders: implications and limitations. Journal of Neural Transmission 2004;111(3):387-411. [DOI] [PubMed] [Google Scholar]
Legg 2019
- Legg LA, Tilney R, Hsieh C, Wu S, Lundström E, Rudberg A, et al. Selective serotonin reuptake inhibitors for stroke recovery. Cochrane Database of Systematic Reviews 2019, Issue 11. Art. No: CD009286. [DOI: 10.1002/14651858.CD009286.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2020
- Li, X, Zhang C. Comparative efficacy of nine antidepressants in treating Chinese patients with post-stroke depression: a network meta-analysis. Journal of Affective Disorders 2020;266:540-8. [DOI] [PubMed] [Google Scholar]
Lim 2009
- Lim CM, Kim SW, Park JY, Kim C, Yoon SH, Lee JK. Fluoxetine affords robust neuroprotection in the postischemic brain via its anti-inflammatory effect. Journal of Neuroscience Research 2009;87(4):1037-45. [DOI] [PubMed] [Google Scholar]
Loubinoux 1999
- Loubinoux I, Boulanouar K, Ranjeva JP, Carel C, Berry I, Rascol O, et al. Cerebral functional magnetic resonance imaging activation modulated by a single dose of the monoamine neurotransmission enhancers fluoxetine and fenozolone during hand sensorimotor tasks. Journal of Cerebral Blood Flow and Metabolism 1999;19(12):1365-75. [DOI] [PubMed] [Google Scholar]
Mantel 1959
- Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. Journal of the National Cancer Institute 1959;22(4):719-48. [PubMed] [Google Scholar]
Mead 2020
- Mead GE, Graham C, Billot L, Näsman P, Lundström E, Lewis S, for FOCUS, AFFINITY and EFFECTS trialists. Update to the FOCUS, AFFINITY and EFFECTS trials studying the effect(s) of fluoxetine in patients with a recent stroke: statistical analysis plan for the trials and for the individual patient data meta-analysis. Trials 2020;21(1):971. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ming 2005
- Ming GL, Song H. Adult neurogenesis in the mammalian central nervous system. Annual Review of Neuroscience 2005;28:223-50. [DOI] [PubMed] [Google Scholar]
Molnar 2008
- Molnar FJ, Hutton B, Fergusson D. Does analysis using “last observation carried forward” introduce bias in dementia research? CMAJ 2008;179(8):751–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
NHS 2021
- NHS. Side effects-selective serotonin reuptake inhibitors (SSRI). www.nhs.uk (accessed 10 August 2021).
Pälvimäki 1994
- Pälvimäki E-P, Laakso A, Kuoppamäki M, Syvälahti E, Hietala J. Up-regulation of beta l-adrenergic receptors in rat brain after chronic citalopram and fluoxetine treatments. Psychopharmacology 1994;115(4):543-6. [DOI] [PubMed] [Google Scholar]
Pinto 2017
- Pinto CB, Saleh Velez FG, Lopes F, Toledo Piza PV, Dipietro L, Wang QM, et al. SSRI and motor recovery in stroke: reestablishment of inhibitory neural network tonus. Frontiers in Neuroscience 2017;11:637. [DOI: 10.3389/fnins.2017.00637] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.4. The Cochrane Collaboration, 2020.
Santarelli 2003
- Santarelli L, Saxe M, Gross C, Surget A, Battaglia F, Dulawa S, et al. Requirement of hippocampal neurogenesis antidepressant treatments and animal models of depressive-like behaviour. Behavioural Pharmacology 2003;301:805-9. [DOI] [PubMed] [Google Scholar]
Schmidt 2007
- Schmidt HD, Duman RS. The role of neurotrophic factors in adult hippocampal neurogenesis, antidepressant treatments and animal models of depressive-like behaviour. Behavioural Pharmacology 2007;18(5-6):391-418. [DOI] [PubMed] [Google Scholar]
Schünemann 2017
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Akl E, Guyatt GH on behalf of the Cochrane GRADEing Methods Group and the Cochrane Statistical Methods Group. Chapter 11: Completing ‘Summary of findings’ tables and grading the confidence in or quality of the evidence. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017). The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook.
Shin 2009
- Shin TK, Kang MS, Lee HY, Seo MS, Kim SG, Kim CD, et al. Fluoxetine and sertraline attenuate postischemic brain injury in mice. Korean Journal of Physiology and Pharmacology 2009;13(3):257-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2017
- Sterne JA, Egger M, Moher D, Boutron I, editor(s). Chapter 10: Addressing reporting biases. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017). The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook.
Taupin 2006
- Taupin P. Adult neurogenesis and neuroplasticity. Restorative Neurology and Neuroscience 2006;24(1):9-15. [PubMed] [Google Scholar]
Wan 2014
- Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Research Methodology 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiltrout 2007
- Wiltrout C, Lang B, Yan Y, Dempsey RJ, Vemuganti R. Repairing brain after stroke: a review on post-ischaemic neurogenesis. Neurochemistry International 2007;50(7-8):1028-41. [DOI] [PubMed] [Google Scholar]
Xie 2019
- Xie Y, Liu PP, Lian YJ, Liu H-B, Kang J-S. The effect of selective serotonin reuptake inhibitors on cognitive function in patients with Alzheimer’s disease and vascular dementia: focusing on fluoxetine with long follow-up periods. Signal Transduction and Targeted Therapy 2019;4:30. [DOI: 10.1038/s41392-019-0064-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yi 2010
- Yi ZM, Liu F, Zhai SD. Fluoxetine for the prophylaxis of post-stroke depression in patients with stroke: a meta-analysis. International Journal of Clinical Practice 2010;64(9):1310-7. [DOI] [PubMed] [Google Scholar]
Zittel 2008
- Zittel S, Weiller C, Liepert J. Citalopram improves dexterity in chronic stroke patients. Neurorehabilitation and Neural Repair 2008;22(3):311-4. [DOI: 10.1177/1545968307312173] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Legg 22019
- Legg LA, Tilney R, Hsieh CF, Wu S, Lundström E, Rudberg AS, et al. Selective serotonin reuptake inhibitors (SSRIs) for stroke recovery. Cochrane Database of Systematic Reviews 2019, Issue 11. Art. No: CD009286. [DOI: 10.1002/14651858.CD009286.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mead 2011
- Mead GE, Hankey GJ, Kutlubaev MA, Lee R, Bailey M, Hackett ML. Selective serotonin reuptake inhibitors (SSRIs) for stroke. Cochrane Database of Systematic Reviews 2011, Issue 10. Art. No: CD009286. [DOI: 10.1002/14651858.CD009286] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mead 2012
- Mead GE, Hsieh CF, Lee R, Kutlubaev MA, Claxton A, Hankey GJ, et al. Selective serotonin reuptake inhibitors (SSRIs) for stroke recovery. Cochrane Database of Systematic Reviews 2012, Issue 11. Art. No: CD009286. [DOI: 10.1002/14651858.CD009286.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


