Abstract
Background:
The syndesmosis ligament complex stabilizes the distal tibiofibular joint while allowing for small amounts of physiologic motion. When injured, malreduction of the syndesmosis is the most important factor that contributes to inferior functional outcomes. Syndesmotic reduction is a dynamic measure, which is not adequately captured by conventional computed tomography (CT). Four-dimensional CT (4DCT) can image joints as they move through range of motion (ROM). The aim of this study was to employ 4DCT to determine in vivo syndesmotic motion with ankle ROM in uninjured ankles.
Methods:
Uninjured ankles were analyzed in patients who had contralateral syndesmotic injuries, as well as a cohort of healthy volunteers with bilateral uninjured ankles. Bilateral ankle 4DCT scans were performed as participants moved their ankles between maximal dorsiflexion and plantarflexion. Multiple measures of syndesmotic width, as well as sagittal translation and fibular rotation, were automatically extracted from 4DCT using a custom program to determine the change in syndesmotic position with ankle ROM.
Results:
Fifty-eight ankles were analyzed. Measures of syndesmotic width decreased by 0.7 to 1.1 mm as the ankle moved from dorsiflexion to plantarflexion (P < .001 for each measure). The fibula externally rotated by 1.2 degrees with ankle ROM (P < .001), but there was no significant motion in the sagittal plane (P = .43). No participants with bilateral uninjured ankles had a side-to-side difference in syndesmotic width of 2 mm or greater.
Conclusion:
4DCT allows accurate, in vivo syndesmotic measurements, which change with ankle ROM, confirming prior work that was limited to biomechanical studies. Side-to-side syndesmotic measurements are consistent within subjects, validating the method of templating syndesmotic reduction off the contralateral ankle, in a consistent ankle position, to achieve anatomic reduction of syndesmotic injury.
Level of Evidence:
Level II, prospective cohort study.
Keywords: 4DCT, dynamic CT, syndesmosis, reduction, kinematics
Introduction
The tibiofibular syndesmosis plays an important role in ankle stability. 11 The syndesmosis primarily resists fibular external rotation and lateral translation.6,11 In addition, the syndesmosis increases joint contact area between the distal tibia and talus and transmits axial loads from the tibia to the fibula throughout the gait cycle. 24 Small but significant amounts of motion are seen at the distal tibiofibular joint throughout ankle range of motion (ROM), as well as in response to loading.2,33 This motion can provide additional ankle stability when accommodating motion of the irregularly shaped talus. 15 In cadaveric and imaging studies, when the ankle moves from dorsiflexion to plantarflexion, there is up to 1.3 mm of anterior fibular translation, 3.0 mm of medial translation, and 3.7 degrees of internal rotation relative to the tibia.15,28,33
Injuries to the syndesmosis are common, occurring in up to 18% of all ankle sprains 24 and in up to one-quarter of ankle fractures. 4 When injured, the historical gold standard for treatment has been reduction of the tibiofibular joint and rigid screw fixation between the tibia and fibula to maintain the reduction. 4 However, due to concerns regarding excessive rigidity and screw breakage or loosening, flexible suture-button devices have been introduced. 37 These flexible devices reduce the rate of malreduction, but malreduction still occurs in up to 20% of flexible cases compared with up to 52% of rigid cases.1,34 Malreduction is the most important predictor of inferior outcomes after injury, leading to chronic pain, stiffness, instability, or arthritis. 41 Efforts to improve reduction, such as direct visualization of the syndesmosis, avoidance of reduction clamps that may introduce overcompression, and intraoperative computed tomography (CT), have demonstrated limited success.8,9,20
Malreduction is commonly judged based on side-to-side differences on bilateral ankle CT.10,30 However, the syndesmosis is a dynamic structure and conventional CT does not capture changes in syndesmotic position with ankle ROM. A CT volume taken at a single nonstandardized, patient-selected ankle position may give inaccurate and potentially misleading results. Four-dimensional CT (4DCT), also known as dynamic CT, is an emerging technology that can image a joint in real time as it moves through ROM and accurately capture changes in syndesmotic position with ankle ROM. 19 Multidetector arrays and fast gantry speeds allow the capture of an entire volume in under 0.3 seconds, which can be repeated to create a moving image. 16
Given the consequences of syndesmotic malreduction, as well as demonstrated motion at the distal tibiofibular joint, it is important to appreciate this motion when treating syndesmotic injuries. Treating reduction as a static measurement rather than a parameter affected by ankle ROM may predispose patients to worse functional outcomes if reduction throughout ROM is not maintained. Therefore, the purpose of this study was to use 4DCT to investigate the in vivo effect of ankle ROM on syndesmotic measurements in uninjured, asymptomatic participants. By first understanding normal syndesmotic motion, we hope to identify reduction and fixation strategies in future study that re-create physiologic motion and subsequently reduce impairment after syndesmotic injury. We hypothesized that in vivo syndesmotic measurements would change significantly throughout ankle ROM and that side-to-side differences would be minimal, as defined as below thresholds used to define malreduction.
Methods
Inclusion Criteria
Participants were gathered from 3 separate studies, though only uninjured ankles from each study were analyzed. In the first study, a subset of patients from a multicenter randomized controlled trial comparing rigid and flexible fixation after syndesmotic injury were recruited to undergo bilateral ankle 4DCT at 12 months after their index surgery (RCT group) (ClinicalTrials.gov identifier NCT02199249). 34 The second study is a prospective cohort study comparing reduction after rigid and flexible fixation currently underway, in which all patients undergo a bilateral ankle 4DCT scan at 3 months after their index surgery (prospective injury group). The last study was a prospective cohort of healthy, adult volunteers who were recruited from our level 1 trauma center and affiliated university to undergo bilateral ankle 4DCT (healthy control group). The contralateral uninjured ankle was analyzed in patients from the RCT and prospective injury groups, and both ankles were used in participants from the healthy control group. All participants were skeletally mature and 18 years of age or older with a unilateral uninjured ankle (bilateral in the healthy control group). Participants were excluded if they had prior lower extremity fractures or known syndesmotic injuries, were nonambulatory or required gait aids, had congenital lower extremity deformities or neuromuscular disease, or were pregnant or attempting to become pregnant. The study was approved by our institutional research ethics review board (REB14-1142 and REB18-2146).
Data Acquisition
Each participant underwent a 4DCT of their bilateral ankles using a GE Medical Systems Revolution CT scanner (General Electric, Boston, MA) at 120 kVp and 70 mA. Imaging was performed from 2017 to 2020. A 140-mm axial scan length with a 300 × 300 mm field of view in the axial plane was used. Axial slice resolution was 0.586 × 0.586 mm with 0.625 mm between axial slices. Participants were instructed to move their ankles freely between maximal comfortable dorsiflexion and plantarflexion continuously with 2 seconds between extremes. Ten imaging time points were captured every 0.9 seconds. The effective radiation dose for the entire scanning protocol was 0.06 mSv, which is well below the radiation exposure of a standard chest x-ray, or roughly equivalent to 1 week of background atmospheric radiation. 25 To ensure the healthy control group represented an asymptomatic population, validated functional outcome measures were administered, including the American Orthopaedic Foot & Ankle Society (AOFAS) Hindfoot Score, Foot and Ankle Ability Measure (FAAM), Olerud and Molander (OM) score, and a visual analog scale (VAS) for pain.
Measurement Process
From CT data, 3-dimensional (3D) models were created of the tibia, fibula, and talus bilaterally for each participant using Mimics software (Materialise, Leuven, Belgium). A custom MATLAB (MathWorks, Natick, MA) program was then used to automatically segment the CT volume and register the 3D model to each time point. A 500 to 2222 Hounsfield Unit intensity threshold was used to segment the imaging volume, followed by a combination of iterative closest point and intensity matching algorithms to register the 3D reference model to each 4DCT time point (Figure 1). The mean root-mean-square error in registration was 0.33 mm. At each time point, the tibiotalar angle was calculated between the long axis of the tibia and the long axis of the talus. The long axis of the tibia was defined as the line between the centroid of the tibia taken at its most proximal aspect and at the level of the incisura, as measured on axial CT slices (Figure 2). The talar long axis was found by calculating the first principal moment of inertia axis. The fibular rotation axis was defined as the tangent line along the medial fibular border at 5 mm below the plafond, as the fibular axis can be defined more reliably at this level.30,39 Syndesmotic measurements were taken 10 mm above the plafond, consistent with other studies, as these measurements can be correlated with radiograph findings and the anterior and posterior tubercles are most prominent at this level. 5 These measurements included anterior (ASD), middle (MSD), and posterior (PSD) syndesmotic distances, which were measured from the most anterior and posterior points of the incisura, as well as the midpoint of the incisura, to the closest corresponding points on the fibula (Figure 3). 30 Tibiofibular clear space (TFCS) was the distance between the most medial fibula and most medial part of the incisura measured perpendicular to the incisura, while the tibiofibular overlap (TFO) was the distance between the most medial fibula and most lateral part of the incisura. 22 Sagittal translation was the distance from the most anterior incisura to the most anterior fibula parallel to the incisura, and fibular rotation was the angle between the fibular axis and the incisura tangent. 30 The syndesmotic area was determined by fitting tangents between the tibia and fibula anteriorly and posteriorly and then finding the area bounded by the tangents. 26 All measurements were automated calculated based off the registered 3D models in MATLAB. After manual reference model creation, the registration, model orientation, and measurement process were fully automated. Therefore, no user input was required to generate syndesmotic measurements, giving complete measurement reproducibility and eliminating error related to subjective landmark selection.
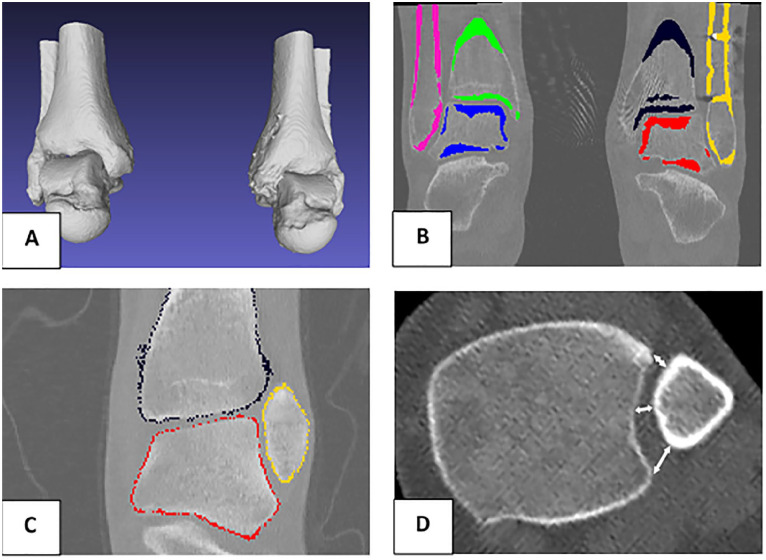
Figure 1.
Automated measurement process. (A) Three-dimensional reference models. (B) Threshold-based segmentation. (C) Reference models registered to 4-dimensional computed tomography data. (D) Automated syndesmosis measurements calculated based on registered models. An automated measurement process calculates multiple measurements at each 4DCT time point.
Figure 2.
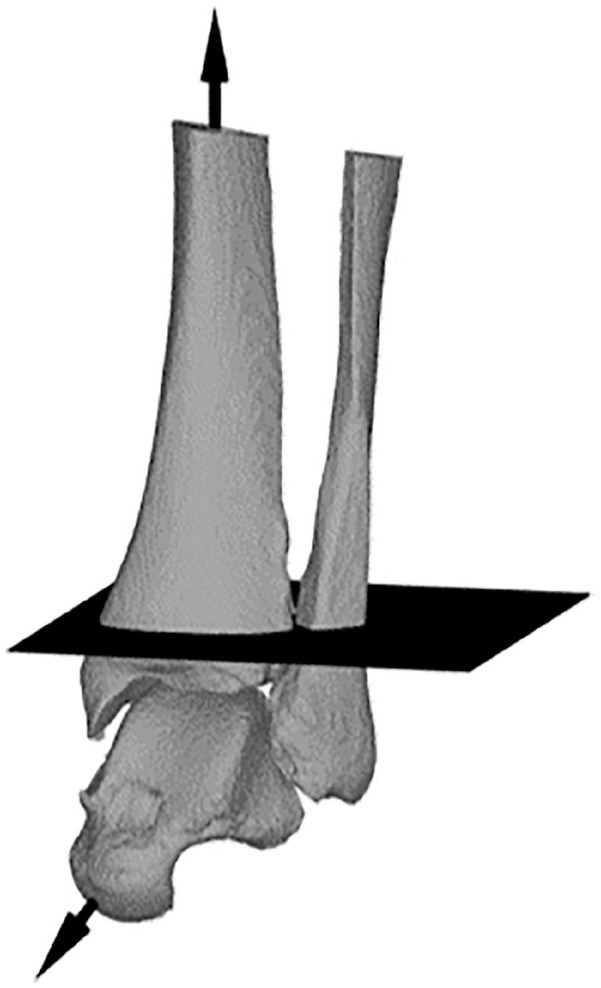
Long axis of the tibia and talar axis. Plane slices through the incisura perpendicular to the tibial axis.
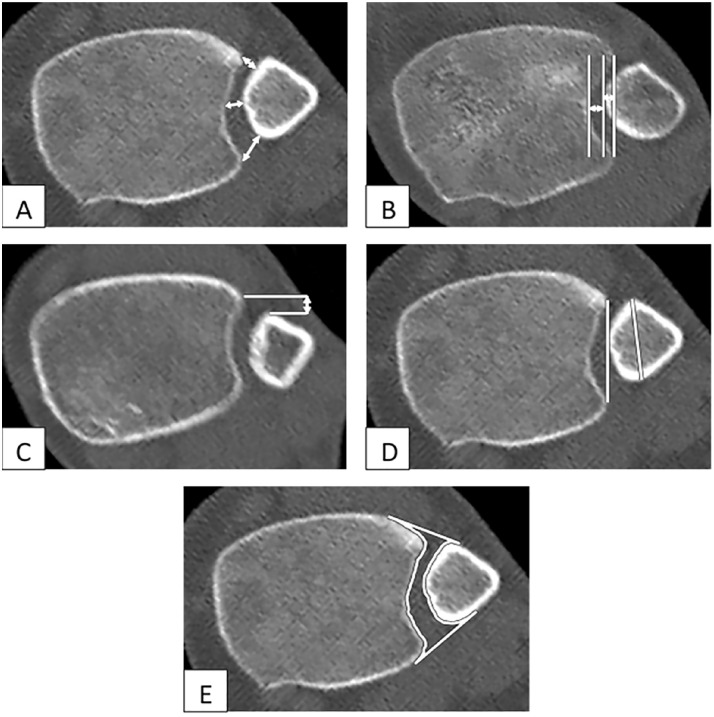
Figure 3.
Syndesmosis measurements generated from 3-dimensional models overlain on 4-dimensional computed tomography data. (A) Anterior, middle, and posterior syndesmosis distances. (B) Tibiofibular clear space and tibiofibular overlap. (C) Sagittal translation. (D) Fibular rotation. (E) Syndesmotic area.
Statistical Analysis
A linear mixed-effects model was used to determine the position of the syndesmosis in the neutral (0 degrees dorsiflexion) ankle position, as well as the syndesmotic motion across ankle ROM. Adjusted r2 values were calculated to determine the model fit, and Shapiro-Wilk tests were used to assess normality. Data were nested within specimens to avoid pseudoreplication within the bilateral control cohort. Side-to-side variability of syndesmotic position and motion was evaluated by comparing the slope and intercept fit to each individual ankle with a linear regression model. P values less than 0.05 were deemed statistically significant.
Results
Demographics
Fifty-eight ankles in 39 different patients were included in the analysis. Thirteen patients came from the RCT group, 7 from the prospective injury group, and 19 from the healthy control group. The healthy control group all had excellent ankle function based on AOFAS, FAAM, OM, and VAS scores. There were 24 males and 15 females. The median age was 31 (range, 18-75) years. The mean maximal dorsiflexion was −2 (range, −20 to 19) degrees, and the mean maximal plantarflexion was 44 (range, 27-61) degrees. There was no difference in baseline characteristics between groups (P > .05 for age, maximal dorsiflexion, and maximal plantarflexion). The adjusted marginal r2 value of the linear mixed-effects models ranged from 0.91 to 0.97, indicating good model fit for each measurement. No significant differences between the 3 patient groups were detected with the numbers available for any measurement (Supplementary Table 1).
Normal Syndesmotic Measurements
The mean ASD in neutral position was 3.3 mm, which decreased by 0.7 mm from dorsiflexion to plantarflexion (P < .001). The MSD was 3.4 mm and decreased by 1.1 mm with plantarflexion (P < .001). The PSD was 6.1 mm and decreased by 0.8 mm with plantarflexion (P < .001) (Table 1). Age did not have a significant impact on syndesmotic position or motion. Males demonstrated less change in PSD with ROM than females (0.6 mm vs 1.0 mm, P = .048), but no differences in neutral position in ASD, MSD, or PSD were detected, nor were there differences in ASD or MSD motion.
Table 1.
Normal Syndesmotic Position in Neutral Dorsiflexion and Motion From Dorsiflexion to Plantarflexion.
|
Position
|
Motion
|
|||
|---|---|---|---|---|
| Mean (SD) | 95% CI | Mean (SD) | 95% CI | |
| ASD, mm | 3.3 (0.9) | 3.0 to 3.6 | −0.7 (0.5) | −0.9 to −0.5 |
| MSD, mm | 3.4 (0.9) | 3.1 to 3.7 | −1.1 (0.5) | −1.2 to −0.9 |
| PSD, mm | 6.1 (1.2) | 5.7 to 6.5 | −0.8 (0.6) | −1.0 to −0.6 |
| TFCS, mm | 3.9 (0.9) | 3.6 to 4.2 | −1.1 (0.5) | −1.3 to −0.9 |
| TFO, mm | −0.3 (1.3) | −0.7 to 0.1 | 1.1 (0.5) | 0.9 to 1.3 |
| Sagittal translation, mm | 0.5 (1.2) | 0.1 to 0.9 | 0.1 (0.6) | −0.1 to 0.3 |
| Fibular rotation, deg | 18.3 (7.0) | 16.1 to 20.6 | −1.2 (1.6) | −1.7 to −0.7 |
| Syndesmotic area, mm2 | 122 (23) | 115 to130 | −26 (11) | −29 to −22 |
Abbreviations: ASD, anterior syndesmotic distance; MSD, middle, syndesmotic distance; PSD, posterior syndesmotic distance; TFCS, tibiofibular clear space; TFO, tibiofibular overlap.
The mean TFCS was 3.9 mm in neutral, which decreased by 1.1 mm during plantarflexion (P < .001). TFO was −0.3 mm, indicating a lack of overlap between the medial fibular border and the lateral border of the incisura. This overlap increased by 1.1 mm with plantarflexion (P < .001). No age- or sex-related differences were found for TFCS and TFO position or motion. An example of each individual ankle’s change in syndesmotic measurement with ankle ROM is shown in Figure 4 for TFCS.
Figure 4.
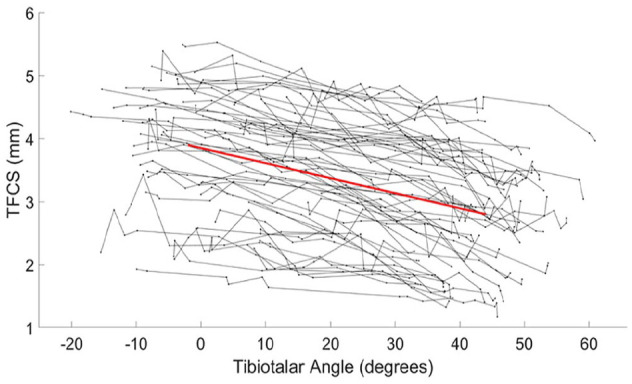
Tibiofibular clear space (TFCS) versus tibiotalar angle plotted for each individual ankle with the overall trendline.
The fibula was situated 0.5 mm posterior to the anterior border of the incisura but did not translate significantly in the sagittal plane with ankle ROM (P = .43). In neutral position, the fibular axis was 18.3 degrees internally rotated relative to the incisura axis and externally rotated 1.2 degrees with plantarflexion (P < .001). Fibular internal rotation was found to increase significantly with age by 0.2 degrees per year (P = .041). No other age- or sex-related changes were significant for sagittal translation or fibular rotation.
The mean syndesmotic area in neutral position was 122 mm2. From dorsiflexion to plantarflexion, the syndesmotic area decreased 26 mm2 (P < .001). Although males had a greater syndesmotic area by 14 mm2, this failed to reach statistical significance (P = .069). There was no difference in change in area between sexes and no age-related differences for area or change in area.
Side-to-Side Variability
The 19 uninjured participants were analyzed to determine side-to-side variability of the syndesmotic measurements for position and motion (Table 2). Using ASD, MSD, PSD, TFCS, or TFO, none of the participants had a side-to-side position difference of 2 mm or greater (Figure 5). One participant was above the 2-mm position threshold for sagittal translation, at 3.1 mm. If a lower threshold of a 1.5 mm side-to-side difference was used, none of the participants would be considered abnormal by ASD, 2 by MSD, 1 by PSD, 0 by TFCS, 1 by TFO, and 3 by sagittal translation. The greatest side-to-side position difference in fibular rotation was 9 degrees. The greatest difference in syndesmotic area was 27 mm2. The side-to-side differences in syndesmotic motion with ankle ROM are depicted in Figure 6.
Table 2.
Side-to-Side Differences in Syndesmotic Position in Neutral Dorsiflexion and Motion From Dorsiflexion to Plantarflexion.
|
Side-to-side position difference
|
Side-to-side motion difference
|
|||
|---|---|---|---|---|
| Mean (SD) | 95% CI | Mean (SD) | 95% CI | |
| ASD, mm | 0.7 (0.4) | 0.5-0.9 | 0.6 (0.5) | 0.3-0.8 |
| MSD, mm | 0.6 (0.6) | 0.3-0.9 | 0.5 (0.5) | 0.3-0.7 |
| PSD, mm | 0.8 (0.4) | 0.5-1.0 | 0.5 (0.5) | 0.2-0.7 |
| TFCS, mm | 0.5 (0.3) | 0.4-0.7 | 0.5 (0.4) | 0.3-0.7 |
| TFO, mm | 0.7 (0.5) | 0.5-0.9 | 0.4 (3) | 0.2-0.6 |
| Sagittal translation, mm | 0.9 (0.8) | 0.5-1.3 | 0.6 (0.5) | 0.3-0.8 |
| Fibular rotation, deg | 3.1 (2.4) | 1.9-4.3 | 2.3 (1.8) | 1.5-3.2 |
| Syndesmotic area, mm2 | 11 (7) | 8-15 | 10 (10) | 5-15 |
Abbreviations: ASD, anterior syndesmotic distance; MSD, middle, syndesmotic distance; PSD, posterior syndesmotic distance; TFCS, tibiofibular clear space; TFO, tibiofibular overlap.
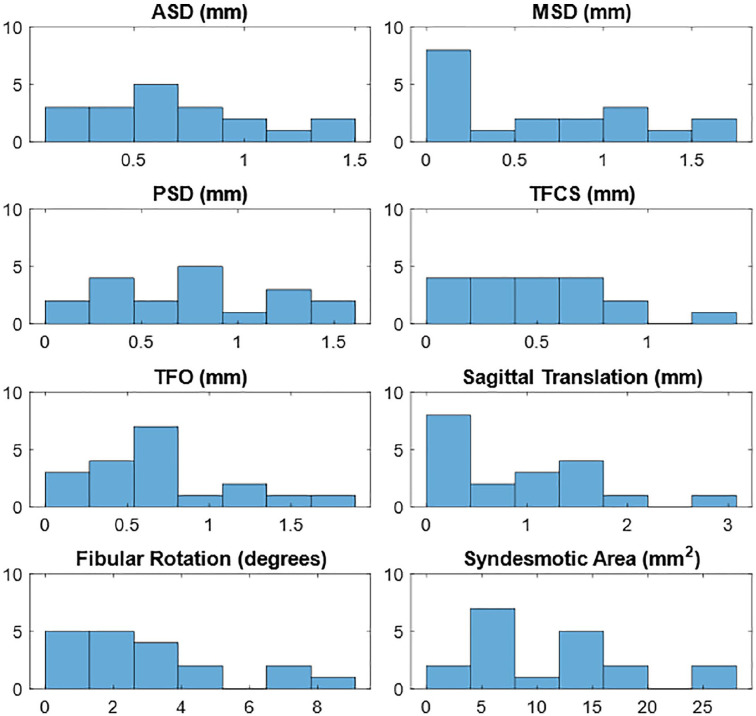
Figure 5.
Distribution of side-to-side differences in syndesmotic position with the ankle in neutral. The y-axis indicates the number of patients, and the x-axis indicates the value for each syndesmotic measurement. ASD, anterior syndesmotic distance; MSD, middle, syndesmotic distance; PSD, posterior syndesmotic distance; TFCS, tibiofibular clear space; TFO, tibiofibular overlap.
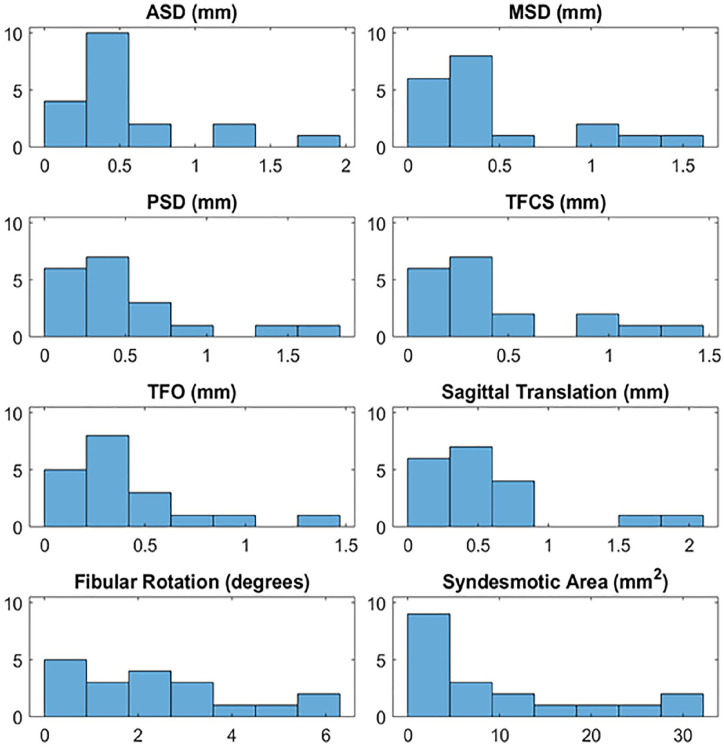
Figure 6.
Distribution of side-to-side differences in syndesmotic motion between dorsiflexion and plantarflexion. The y-axis indicates the number of patients, and the x-axis indicates the value for each syndesmotic measurement. ASD, anterior syndesmotic distance; MSD, middle, syndesmotic distance; PSD, posterior syndesmotic distance; TFCS, tibiofibular clear space; TFO, tibiofibular overlap.
Discussion
Determining whether a syndesmosis is accurately reduced is challenging, especially given the wide variation in normal anatomy and numerous different measures of reduction, which vary in intra- and interrater reliability. Current measures have not accounted for normal syndesmotic motion or the position of the ankle at the time of the measurements when judging reduction, which puts patients at risk of inferior functional outcomes.
Normal Position and Motion
This study shows that commonly used measures of syndesmotic width and fibular rotation vary significantly with ankle ROM under nonweightbearing conditions. These measurements were chosen due to their common use in clinical practice, demonstrated repeatability, and sensitivity in detecting injury.10,23,26,30
The values determined in this study for each syndesmotic measurement at neutral dorsiflexion are comparable to those previously reported.10,26,30 We found slightly less variation in values than these prior studies. This may be due to our calculation of these values from a mixed-effects model incorporating 10 time points per ankle, or perhaps from the resulting standardized ankle position, as position was either not specified in previous studies10,26 or varied due to different splinting positions for hindfoot fractures. 30
In various biomechanical studies, the fibula translates medially 0.8 to 3 mm, anteriorly 0.9 to 1.3 mm, and rotates 0.5 to 3.7 degrees internally with plantarflexion.15,33 Mousavian et al 28 have also investigated the change in syndesmotic measurements through ankle ROM using 4DCT. When investigating 10 uninjured, unilateral ankles, the only significant change was 0.7 mm of posterior translation with plantarflexion, contrary to the prior studies showing anterior translation. 28 The current 4DCT study of 58 uninjured ankles found an in vivo decrease in syndesmotic width of up to 1.1 mm and area by 26 mm2, consistent with existing biomechanical literature, which can be explained by the greater width of the talar dome in dorsiflexion compared with plantarflexion. No change in sagittal translation was detected in the present study, perhaps due to our imaging protocol, which was unloaded and had subjects perform a comfortable ROM. This protocol could potentially lead to submaximal motion, and extremes of motion may not have been captured with the 0.9-second imaging intervals. Differences in methodology may explain discrepancies between our results and biomechanical motion studies. These studies were either cadaveric experiments where the soft tissues were denuded and the ankle was moved passively, or in vivo studies using radiostereometric analysis. In either case, these subjects were imaged in an upright position compared with our supine study. Prior work has also demonstrated that radiographs have poor accuracy for detecting positional changes at the distal tibiofibular joint. 3 Mousavian et al’s 28 findings may also be different due to their method of measuring sagittal translation, based off a tangent line drawn from the anterolateral fibula, which would also be impacted by fibular rotation. Our automated measurement program found 1.2 degrees of fibular external rotation with ankle plantarflexion on average. Some amount of external rotation was seen in 70% of ankles (35/50). While previous studies have shown predominantly internal rotation, external rotation has been reported in some subjects. 15 Estimates of fibular rotation from radiographs are inaccurate, 17 so prior estimates of the change in fibular rotation are based on cadaveric studies using optical or ultrasound-based motion tracking.14,15 Again, it is possible that contributions from intact soft tissue attachments and active muscular contraction could explain why external rotation was found in vivo.
Normal syndesmotic motion has important implications on imaging and fixation of syndesmotic injuries. Previous authors have suggested that rigid fixation of the syndesmosis need not be performed at a specific ankle position. 38 However, these conclusions were based off the restoration of ankle ROM, and not syndesmotic reduction. In addition to this study, Nault et al 29 demonstrated increases in syndesmotic width with ankle plantarflexion, as did Kortekangas et al, 18 who performed intraoperative CT scans and detected 7 malreductions out of 21 cases after flexible fixation. In these cases, open exploration was performed intending to revise the reduction, but each ankle was found to be well reduced under direct inspection and on subsequent CT scans at 0 degrees dorsiflexion. 18 Therefore, ankle position should be standardized when measuring and performing reduction of these injuries, if we wish to obtain an anatomic reduction. When imaging the syndesmosis, a consistent ankle position should be chosen to avoid changes in syndesmotic position resulting from nonstandard ankle position. When reducing a syndesmosis, it is important to ensure that the reduction achieved is appropriate for the ankle position, as the anatomically reduced syndesmotic position will vary depending on ankle position. If a syndesmosis rigidly fixed in dorsiflexion loses normal motion, it may be undercompressed, resulting in abnormal diastasis in plantarflexion compared with uninjured ankles, and the fibular position may be internally rotated in plantarflexion, while rigid fixation in plantarflexion and subsequent loss of motion may produce overcompression of the syndesmosis and excessive external rotation of the fibula when the ankle is dorsiflexed, when compared with uninjured motion. If not accounted for, syndesmotic motion may explain why, even when using intraoperative CT, malreduction rates can remain as high as 38%. 9
Given the demonstrated motion at the syndesmosis, we should seek to restore both position and motion of the syndesmosis to optimize outcomes for patients after injury. While postfixation motion has not been quantified, potential strategies to restore motion include either flexible fixation or removing rigid implants or allowing them to fail. However, loss of reduction or other complications with secondary procedures are possible. 35 Though seemingly small, this syndesmotic motion impacts ankle kinematics and joint contact mechanics. If motion is not restored, the joint contact area is reduced, leading to earlier cartilage degradation, and impingement or instability is possible.21,39
Side-to-Side Variability
Imaging of bilateral ankles demonstrated mild side-to-side variability, as shown previously.10,23 Only 1 subject out of 19 had a single side-to-side measurement difference of 2 mm, a common threshold for malreduction.12,39 Three of 19 (15.8%) had asymmetry in rotational measurements greater than 5 degrees, indicating that wider thresholds should be used when determining rotational malreduction based on the contralateral side. This supports work by Warner et al, 40 who found no functional difference in patients with a mean rotational asymmetry of 5.75 degrees after syndesmotic injury, and Vasarhelyi et al, 39 who proposed 10 to 15 degrees as a cutoff after which AOFAS scores worsened. Similar to position, side-to-side motion demonstrated only mild variability. These findings support the common practice of measuring reduction based on the difference in syndesmotic measurements between the injured and contralateral, uninjured ankle.
Age- and Sex-Related Changes
The only impact of age found was a small increase in fibular internal rotation with increasing age. It is possible that this finding represents a type I error. If not, one potential explanation is that the distal fibular articular cartilage is in closer proximity anteriorly, and may thin with aging, leading to increased internal rotation. If degenerative changes do occur, they are not large enough to detect significant changes in syndesmotic widths. Most studies found no age-related changes in syndesmotic measurements, though increased internal rotation has been previously reported. 32
This study found no difference in position measurements between sexes, though there was a significant difference in PSD motion between males and females. Studies of normal position using various modalities have varying results, but in general show greater measurements of syndesmotic width or sagittal translation in males due to larger joint sizes overall.10,23 Syndesmotic area is highly sensitive to changes in syndesmotic width and was larger in males in the current study, but failed to reach statistical significance (P = .067), indicating that the effect size was too small to detect in our sample. Currently, no separate malreduction cutoffs for males and females exist, though some advocate for this, based on different average joint sizes. 23
Limitations
The study investigated the impact of ankle ROM on syndesmotic position in a supine position. Therefore, the presented data are in a nonweightbearing condition, and it is known that gravity imparts a posterior force on the fibula. Studies have shown that weightbearing leads to 0.4 to 0.6 mm of lateral fibular translation compared with the unloaded state, though they were performed on patients with a history of foot and ankle injury or disease who may not accurately represent the uninjured condition.27,31 These changes to syndesmotic position with weightbearing are smaller than the changes with ankle ROM reported in the current study, as well as previous studies.15,33 Other studies have failed to find significant changes between loaded and unloaded conditions in both in vitro and in vivo experiments.2,6,13 Approximately 30 degrees of ankle ROM is required for normal walking, 40 degrees for ascending stairs, and 55 degrees for descending stairs; therefore, syndesmotic reduction through ankle ROM has important clinical implications for daily, low-impact, low-demand activities.7,36 As the CT protocol captured 4DCT time points at regular intervals, we cannot guarantee that extremes of motion or specific positions were captured for direct comparison. This was overcome with the linear mixed-effects model, which was able to model each syndesmotic measurement as a function of tibiotalar angle and interpolate or extrapolate to a standard position as required, while still accounting for the variation within individual ankle data sets.
Strengths
The strengths of this study include the use of an emerging technology, 4DCT, to accurately measure syndesmotic motion in vivo. Prior work has relied on cadaveric data with denuded soft tissues and passive motion, or imaging modalities that have lower sensitivity and are more prone to error. 4DCT in peripheral extremities has a low radiation dose, less than a chest x-ray in our study, or approximately equivalent to 10 days of background atmospheric radiation. Syndesmotic measurements were calculated 10 times per specimen to model reduction throughout ROM. The automated measurement process achieved subvoxel size registration accuracy and completed measurements automatically, ensuring repeatable and accurate measurements. This process has allowed us to perform the largest study of motion, to our knowledge, and is the first to report on side-to-side motion variation in normal individuals. We also included a substantial cohort of healthy control participants to ensure truly asymptomatic, normal ankles. The developed imaging and measuring process can be applied to future patients, allowing us to study motion after injury and after fixation to determine surgical strategies to restore physiologic motion. Comparisons of motion between rigid and flexible fixation are possible, including the effects of intact, removed, or failed fixation. Additional avenues could be the impact of posterior malleolus fractures or deltoid ligament injuries, with or without fixation or repair.
Conclusion
This study used 4DCT to confirm that there is significant syndesmotic motion during in vivo ankle ROM, including medial translation and external rotation of the fibula with plantarflexion. Syndesmotic position and motion are consistent within subjects; therefore, surgeons may use the contralateral ankle as a valid template for anatomic reduction, provided ankle position is standardized. The quantification of in vivo physiologic motion can be used in future studies to determine which methods of reduction and fixation best re-create this motion.
Supplemental Material
Supplemental material, sj-pdf-1-fai-10.1177_10711007211015204 for Four-Dimensional CT Analysis of Normal Syndesmotic Motion by Murray T. Wong, Charmaine Wiens, Jeremy Lamothe, W. Brent Edwards and Prism S. Schneider in Foot & Ankle International
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors report grants from Arthrex (Naples, FL), the Orthopaedic Trauma Association, AO Trauma North America, and the Workers Compensation Board of Alberta, during the conduct of the study. ICMJE forms for all authors are available online.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: AO Trauma North America, Arthrex, Orthopaedic Trauma Association, Workers’ Compensation Board–Alberta.
ORCID iD: Murray T. Wong, MD, MSc,  https://orcid.org/0000-0003-0837-0121
https://orcid.org/0000-0003-0837-0121
Supplemental Material: Supplementary material is available online with this article.
References
- 1. Andersen MR, Frihagen F, Hellund JC, Madsen JE, Figved W. Randomized trial comparing suture button with single syndesmotic screw for syndesmosis injury. J Bone Joint Surg Am. 2018;100(1):2-12. [DOI] [PubMed] [Google Scholar]
- 2. Beumer A, Valstar ER, Garling EH, et al. Kinematics of the distal tibiofibular syndesmosis: radiostereometry in 11 normal ankles. Acta Orthop Scand. 2003;74(3):337-343. [DOI] [PubMed] [Google Scholar]
- 3. Beumer A, Van Hemert WLW, Niesing R, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004;(423):227-234. [DOI] [PubMed] [Google Scholar]
- 4. Carr JC, Werner BC, Yarboro SR. An update on management of syndesmosis injury: a national US database study. Am J Orthop (Belle Mead NJ). 2016;45(7):E472-E477. [PubMed] [Google Scholar]
- 5. Chen Y, Qiang M, Zhang K, Li H, Dai H. A reliable radiographic measurement for evaluation of normal distal tibiofibular syndesmosis: a multi-detector computed tomography study in adults. J Foot Ankle Res. 2015;8:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Clanton TO, Williams BT, Backus JD, et al. Biomechanical analysis of the individual ligament contributions to syndesmotic stability. Foot Ankle Int. 2017;38(1):66-75. [DOI] [PubMed] [Google Scholar]
- 7. Coetzee JC, Castro MD. Accurate measurement of ankle range of motion after total ankle arthroplasty. Clin Orthop Relat Res. 2004;424:27-31. [DOI] [PubMed] [Google Scholar]
- 8. Cosgrove CT, Spraggs-Hughes AG, Putnam SM, et al. A novel indirect reduction technique in ankle syndesmotic injuries: a cadaveric study. J Orthop Trauma. 2018;32(7): 361-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Davidovitch RI, Weil Y, Karia R, et al. Intraoperative syndesmotic reduction: three-dimensional versus standard fluoroscopic imaging. J Bone Joint Surg Am. 2013;95(20): 1838-1843. [DOI] [PubMed] [Google Scholar]
- 10. Dikos GD, Heisler J, Choplin RH, Weber TG. Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J Orthop Trauma. 2012;26(7):433-438. [DOI] [PubMed] [Google Scholar]
- 11. Ebraheim NA, Taser F, Shafiq Q, Yeasting RA. Anatomical evaluation and clinical importance of the tibiofibular syndesmosis ligaments. Surg Radiol Anat. 2006;28(2):142-149. [DOI] [PubMed] [Google Scholar]
- 12. Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27(10):788-792. [DOI] [PubMed] [Google Scholar]
- 13. Hagemeijer NC, Chang SH, Abdelaziz ME, et al. Range of normal and abnormal syndesmotic measurements using weightbearing CT. Foot Ankle Int. 2019;40(12):1430-1437. [DOI] [PubMed] [Google Scholar]
- 14. Hu WK, Chen DW, Li B, Yang YF, Yu GR. Motion of the distal tibiofibular syndesmosis under different loading patterns: a biomechanical study. J Orthop Surg. 2019;27(2):1-6. [DOI] [PubMed] [Google Scholar]
- 15. Huber T, Schmoelz W, Bölderl A. Motion of the fibula relative to the tibia and its alterations with syndesmosis screws: a cadaver study. Foot Ankle Surg. 2012;18(3):203-209. [DOI] [PubMed] [Google Scholar]
- 16. Hurlock GS, Higashino H, Mochizuki T. History of cardiac computed tomography: single to 320-detector row multislice computed tomography. Int J Cardiovasc Imaging. 2009;25(suppl 1):31-42. [DOI] [PubMed] [Google Scholar]
- 17. Knops SP, Kohn MA, Hansen EN, Matityahu A, Marmor M. Rotational malreduction of the syndesmosis: reliability and accuracy of computed tomography measurement methods. Foot Ankle Int. 2013;34(10):1403-1410. [DOI] [PubMed] [Google Scholar]
- 18. Kortekangas T, Savola O, Flinkkilä T, et al. A prospective randomised study comparing TightRope and syndesmotic screw fixation for accuracy and maintenance of syndesmotic reduction assessed with bilateral computed tomography. Injury. 2015;46(6):1119-1126. [DOI] [PubMed] [Google Scholar]
- 19. Kwong Y, Mel AO, Wheeler G, Troupis JM. Four-dimensional computed tomography (4DCT): a review of the current status and applications. J Med Imaging Radiat Oncol. 2015;59(5):545-554. [DOI] [PubMed] [Google Scholar]
- 20. LaMothe J, Baxter JR, Gilbert S, Murphy CI, Karnovsky SC, Drakos MC. Effect of complete syndesmotic disruption and deltoid injuries and different reduction methods on ankle joint contact mechanics. Foot Ankle Int. 2017;38(6):694-700. [DOI] [PubMed] [Google Scholar]
- 21. Lamothe JM, Baxter JR, Murphy C, Gilbert S, Desandis B, Drakos MC. Three-dimensional analysis of fibular motion after fixation of syndesmotic injuries with a screw or suture-button construct. Foot Ankle Int. 2016;37(12):1350-1356. [DOI] [PubMed] [Google Scholar]
- 22. Lepojärvi S, Niinimäki J, Pakarinen H, Leskelä HV. Rotational dynamics of the normal distal tibiofibular joint with weight-bearing computed tomography. Foot Ankle Int. 2016;37(6):627-635. [DOI] [PubMed] [Google Scholar]
- 23. Lepojärvi S, Pakarinen H, Savola O, Haapea M, Sequeiros RB, Niinimäki J. Posterior translation of the fibula may indicate malreduction: CT study of normal variation in uninjured ankles. J Orthop Trauma. 2014;28(4):205-209. [DOI] [PubMed] [Google Scholar]
- 24. Lin CF, Gross MT, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006;36(6):372-384. [DOI] [PubMed] [Google Scholar]
- 25. Lombard C, Gervaise A, Villani N, et al. The impact of dose reduction in quantitative kinematic CT of ankle joints using a full model-based iterative reconstruction algorithm: a cadaveric study. AJR Am J Roentgenol. 2018;210(2):396-403. [DOI] [PubMed] [Google Scholar]
- 26. Malhotra G, Cameron J, Toolan BC. Diagnosing chronic diastasis of the syndesmosis: a novel measurement using computed tomography. Foot Ankle Int. 2014;35(5):483-488. [DOI] [PubMed] [Google Scholar]
- 27. Malhotra K, Welck M, Cullen N, Singh D, Goldberg AJ. The effects of weight bearing on the distal tibiofibular syndesmosis: a study comparing weight bearing-CT with conventional CT. Foot Ankle Surg. 2019;25(4):511-516. [DOI] [PubMed] [Google Scholar]
- 28. Mousavian A, Shakoor D, Hafezi-Nejad N, et al. Tibiofibular syndesmosis in asymptomatic ankles: initial kinematic analysis using four-dimensional CT. Clin Radiol. 2019;74(7):571.e1-571.e8. [DOI] [PubMed] [Google Scholar]
- 29. Nault ML, Marien M, Hébert-Davies J, et al. MRI quantification of the impact of ankle position on syndesmosis anatomy. Foot Ankle Int. 2017;38(2):215-219. [DOI] [PubMed] [Google Scholar]
- 30. Nault MLL, Hébert-Davies J, Laflamme GYY, Leduc S. CT scan assessment of the syndesmosis: a new reproducible method. J Orthop Trauma. 2013;27(11):638-641. [DOI] [PubMed] [Google Scholar]
- 31. Osgood GM, Shakoor D, Orapin J, et al. Reliability of distal tibio-fibular syndesmotic instability measurements using weightbearing and non-weightbearing cone-beam CT. Foot Ankle Surg. 2019;25(6):771-781. [DOI] [PubMed] [Google Scholar]
- 32. Prakash AA. Syndesmotic stability: is there a radiological normal? A systematic review. Foot Ankle Surg. 2018;24(3): 174-184. [DOI] [PubMed] [Google Scholar]
- 33. Rammelt S, Obruba P. An update on the evaluation and treatment of syndesmotic injuries. Eur J Trauma Emerg Surg. 2015;41(6):601-614. [DOI] [PubMed] [Google Scholar]
- 34. Sanders D, Schneider P, Taylor M, Tieszer C, Lawendy AR. Improved reduction of the tibiofibular syndesmosis with TightRope compared to screw fixation: results of a randomized controlled study. J Orthop Trauma. 2019;3(3): 2473011418S0012. [DOI] [PubMed] [Google Scholar]
- 35. Schepers T, Van Lieshout EMM, de Vries MR, Van der Elst M. Complications of syndesmotic screw removal. Foot Ankle Int. 2011;32(11):1040-1044. [DOI] [PubMed] [Google Scholar]
- 36. Sinitski EH, Hansen AH, Wilken JM. Biomechanics of the ankle-foot system during stair ambulation: implications for design of advanced ankle-foot prostheses. J Biomech. 2012;45(3):588-594. [DOI] [PubMed] [Google Scholar]
- 37. Thornes B, Walsh A, Hislop M, Murray P, O’Brien M. Suture-endobutton fixation of ankle tibio-fibular diastasis: a cadaver study. Foot Ankle Int. 2003;24(2):142-146. [DOI] [PubMed] [Google Scholar]
- 38. Tornetta P, Spoo JE, Reynolds FA, Lee C. Overtightening of the ankle syndesmosis: is it really possible? J Bone Joint Surg Am. 2001;83(4):489-492. [DOI] [PubMed] [Google Scholar]
- 39. Vasarhelyi A, Lubitz J, Gierer P, et al. Detection of fibular torsional deformities after surgery for ankle fractures with a novel CT method. Foot Ankle Int. 2006;27(12):1115-1121. [DOI] [PubMed] [Google Scholar]
- 40. Warner SJ, Fabricant PD, Garner MR, Schottel PC, Helfet DL, Lorich DG. The measurement and clinical importance of syndesmotic reduction after operative fixation of rotational ankle fractures. J Bone Joint Surg Am. 2015;97(23):1935-1944. [DOI] [PubMed] [Google Scholar]
- 41. Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma. 2005;19(2):102-108. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fai-10.1177_10711007211015204 for Four-Dimensional CT Analysis of Normal Syndesmotic Motion by Murray T. Wong, Charmaine Wiens, Jeremy Lamothe, W. Brent Edwards and Prism S. Schneider in Foot & Ankle International