Abstract
Objective:
To determine whether selected features of the built environment can predict weight gain in a large longitudinal cohort of adults.
Methods:
Weight trajectories over a 5-year period were obtained from electronic health records for 115,260 insured patients aged 18–64 years in the Kaiser Permanente Washington health care system. Home addresses were geocoded using ArcGIS. Built environment variables were population, residential unit, and road intersection densities captured using Euclidean-based SmartMaps at 800-meter buffers. Counts of area supermarkets and fast food restaurants were obtained using network-based SmartMaps at 1,600, and 5,000-meter buffers. Property values were a measure of socioeconomic status. Linear mixed effects models tested whether built environment variables at baseline were associated with long-term weight gain, adjusting for sex, age, race/ethnicity, Medicaid insurance, body weight, and residential property values.
Results:
Built environment variables at baseline were associated with differences in baseline obesity prevalence and body mass index but had limited impact on weight trajectories. Mean weight gain for the full cohort was 0.06 kilograms at 1 year (95% CI: 0.03, 0.10); 0.64 kilograms at 3 years (95% CI: 0.59, 0.68), and 0.95 kilograms at 5 years (95% CI: 0.90, 1.00). In adjusted regression models, the top tertile of density metrics and frequency counts were associated with lower weight gain at 5 years follow-up compared to the bottom tertiles, though the mean differences in weight change for each follow-up year (1, 3, and 5) did not exceed 0.5 kilograms.
Conclusion:
Built environment variables that were associated with higher obesity prevalence at baseline had limited independent obesogenic power with respect to weight gain over time. Residential unit density had the strongest negative association with weight gain. Future work on the influence of built environment variables on health should also examine social context, including residential segregation and residential mobility.
Keywords: built environment, geographic information systems, electronic medical records, obesity
INTRODUCTION
Where people live can influence their weight, health, and mental well-being [1]. Studies on health and place have pointed to links between multiple built environment (BE) variables, obesity prevalence, and other health outcomes [1–4]. However, the observed associations have been mixed and not always consistent [1,5]. In general, BE variables were more closely linked to physical activity (PA) measures [1,6,7] than to diet quality [5,8,9]. Whereas the walkability of neighborhoods was consistently linked to lower obesity prevalence [1,10,11], the density of food sources (e.g. fast food restaurants and supermarkets) was not [1,5,8,9]. Furthermore, there is evidence that the collocation of BE features supporting PA and healthy diets, were associated with lower obesity prevalence than any single feature [12].
One question, directly relevant to public policy, was whether residing in a given neighborhood could explain long-term changes in weight status [1,5,6]. In the United States (US) and in other high-income countries, the “obesogenicity” of the BE, in the sense of being associated with or even influencing long-term weight gain, was defined in terms a lack of spatially accessible of supermarkets, grocery stores, and farmers’ markets, as opposed to convenience stores and fast food restaurants [1,5]. Other relevant BE features were green spaces, PA locations, and walkability, as measured, in part, by the connectivity of roads and sidewalks [1,6,11]. Spatial clustering of fast food restaurants around schools was viewed as obesogenic as was higher fast food density in low-income areas [8]. Conversely, neighborhoods that were more walkable [10,13] and closer to parks and trails had lower obesity prevalence [14–16]. The diversity of methods used to characterize individual exposures, including BE exposures, may have contributed to the mixed findings observed in the body of BE and obesity work [5]. The relation between BE variables could be clarified by large-scale longitudinal cohort studies. However, to date, few examples of such longitudinal studies exist [4,11,18–22].
The present study sought to determine whether BE features, measured at baseline, had any influence on adult body weight trajectories at 1, 3, and 5 years of follow-up. Measured weights came from electronic health records (EHR). Primary analyses used linear mixed models to estimate weight gain at each time point, adjusting for demographics and patient residential property values. Secondary analyses mutually adjusted for multiple BE features to determine the combined influence of BE features and the food environment on measured weight trajectories over time.
METHODS
Study population and design
Development of the Moving to Health (M2H) retrospective cohort has been described in detail elsewhere [23,24]. Data on the residential history, measured heights and weights, and health of patients receiving care from Kaiser Permanente Washington (KPW) between 1/1/2005 and 4/30/2017 were extracted from KPW EHR. Patients who were KPW members, aged 18–64 years at baseline and had at least 270 days of continuous enrollment between January 2005 and April 2017 were included. Insurance status was verified at the time of enrollment. Gaps in enrollment of 92 days were allowed. Excluded at baseline were patients with a prior-year cancer diagnosis (omitting non-melanoma skin cancer), patients who had prior-year bariatric surgery, patients who were pregnant or within 3 months after delivery, and those of unknown sex. The King County (KC) address at the baseline weight measure was the baseline address. This analysis was limited to patients who had at least one follow-up weight measured after their baseline weight. We limited the cohort to KPW enrolled patients with a geocodable address and available residential property values; disenrollment from KPW was defined as a gap in enrollment of ≥13 months. A flow chart is shown in Figure 1.
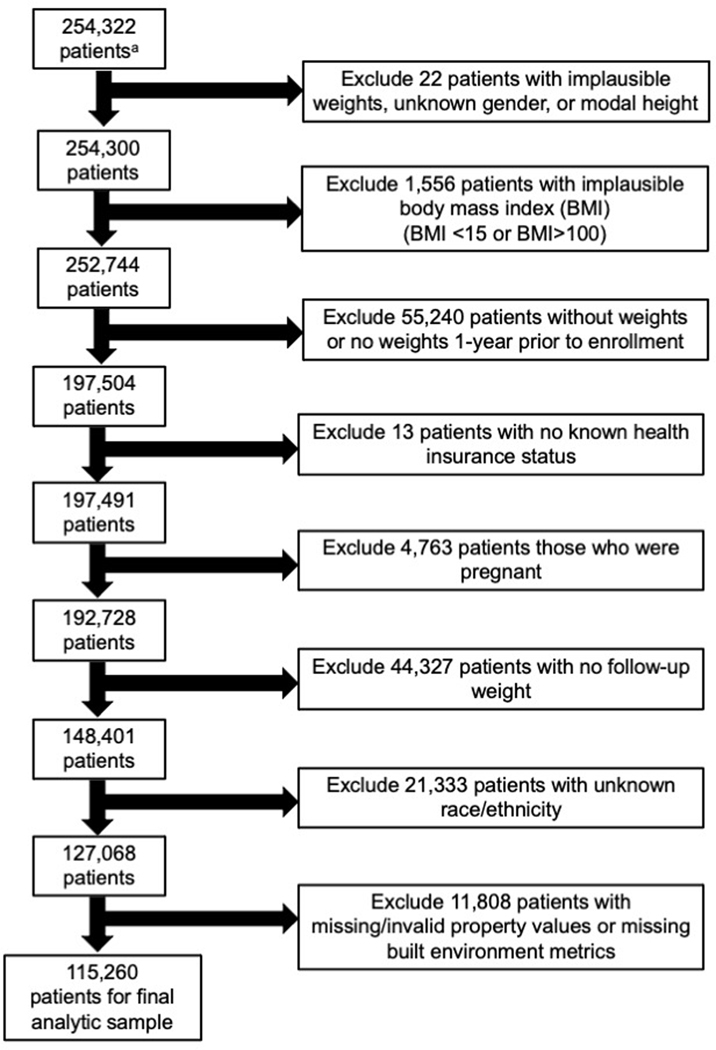
Figure 1.
Patient analytic sample exclusion/inclusion decision flow diagram
aInitial sample of 254,322 were KPW patient members, aged 18–64 at baseline, having at least 270 days of continuous enrollment between 2005 and April 2017 and residing in King County, Washington
Body weight measurement
Clinicians recorded body weight measurements in the EHR during each clinical visit. Observations that clinical expertise indicated as having biologically implausible weight values for adults (<31.75 or >317.52 kg) were excluded. We additionally excluded follow-up weights taken during the pregnancy period (9 months before and 3 months after pregnancy outcome) [23]. Patients were followed for subsequent weight measures from the time of the baseline weight until the end of the study period and were censored if they had a change in residential location (n=48,148), a bariatric surgery (n=312), a cancer diagnosis (n=13,838), disenrolled from KPW (gap in enrollment of ≥13 months) (n=9,461), or had a gap in address data ≥13 months (n=659).
Geocoding patient addresses
The KPW patients’ baseline addresses were geocoded to determine each patient’s baseline BE exposures, which served as the exposures of interest in all cross-sectional and longitudinal analyses. Geocoding, conducted using ArcGIS and KC address point reference data, yielded successful matches for 93.0% of patient addresses. We then searched for a match within the Esri Business Analyst tool using a match threshold of 85 [25]. This enabled us to match an additional 1.5% of patient addresses. Approximately 5.6% of addresses could not be geocoded. These patients were removed from the final analytic sample. The most common reasons for an inability to geocode included, but were not limited to, the use of a post office box as a mailing address and incorrectly written addresses for which the geocoder could not determine the precise location [23]. Once geocoded, the latitude/longitude point was used to determine BE exposures using SmartMaps at fixed buffer and network distances [26].
Built environment exposures
Primary measures of potentially obesogenic BE exposures were residential unit density (derived from KC tax assessor data) and population density (derived from American Community Survey data), which have been used in prior studies as proxies for walkability and have been associated with obesity prevalence [6,27–32]. A recent KC study found that residential unit density was the most predictive BE metric of walking bouts [6]. Moreover, in our sample, residential unit density and population density were highly correlated (r=0.92) indicating that both BE measures may be good proxies for walkability. Street intersection density (from TIGER/Line files) was a measure of walking route connectivity and has been linked to obesity prevalence [33]. These density variables were calculated as units per hectare and averaged within 800 and 1,600 m Euclidian buffers of the home address, representing 10 and 20 minute walking distances, respectively [34]. The food environment was measured using counts of supermarkets and fast food restaurants (from Public Health-Seattle KC food permit addresses) [35]. Fast food restaurants included all quick service restaurants, that is, establishments in which one pays for food first before eating. Counts of these food outlets were measured within a 1,600 m and 5,000 m (accessible within a short drive) network buffer of the home address. Lacking commonly recognized threshold measures of BE characteristics related to health, we operationalized the residential unit, population, and intersection densities by stratifying each continuous measure into tertiles. Residential density was also dichotomized as above and below 18 residential units per hectare, based on well-established thresholds needed to allow for the provision of public transit [36,37]. For the food environment, 1,600 m buffer fast food and supermarket counts were dichotomized using 1 if any fast food restaurant or supermarket was located with the 1,600 m buffer and 0 if otherwise. Fast food restaurant and supermarket counts at 5,000 m buffers were categorized into tertiles. Given the large number of geocoded home locations, BE exposures were measured using SmartMaps, which are continuous rasterized surfaces that provide estimates of neighborhood-level BE variables points within a study area, developed by the University of Washington Urban Form Lab [26,38–40]. More details on the Euclidean- and network-based SmartMaps can found be in the Technical Appendix as well as in prior publications [23,24,26].
Patients baseline BE exposures were matched temporally to their year of entry into the cohort. Yearly data were available for residential density and residential property values. For all other BE exposures, patients were matched to nearest year for which data were available (Supplemental Table 1).
Statistical analysis
Baseline built environment exposures and baseline weight
We conducted cross-sectional analyses to examine the association between baseline BE characteristics and baseline weight in the same year. We regressed baseline weight on each baseline BE predictor, adjusted for the same series of covariates as in our analysis of weight change. Unlike in our primary, longitudinal analyses, we adjusted for spline terms, or a piecewise polynomial function that allows a more flexible fit, of baseline height (instead of baseline weight).
Baseline built environment exposures and weight change
Our primary goal was to estimate the association between baseline BE characteristics with individual weight change independent of socioeconomic status (SES) and demographic characteristics. We modeled weight change, in kilograms, from baseline to 5-years after baseline (primary outcome), as well as change in body weight at 1 and 3 years (secondary outcomes). To estimate the association between each of the baseline BE characteristics and body weight changes over time, we used linear mixed-effect models. Our primary linear mixed-effect models were defined as:
where is the change in weight of person i from baseline to time t (calculated as follow-up weight minus baseline weight), is a vector of person-specific baseline covariates, and is a person-specific random intercept, assumed to have an exponential covariance (given the irregularly spaced follow-up time points). is each built environment variable at baseline for person i at level k of the categorical BE variable (+1 is the number of levels), categorized into tertiles or binary. The functions denote longitudinal changes in weight at different levels of the categorical BE variable. Weight change trajectories were flexibly modeled using natural cubic splines with 5 degrees of freedom (DF) and inflection points at quantiles. These spline terms were interacted with categorical BE variables to allow the weight change trajectories to differ based on BE category. P values were calculated to compare the weight change at the 3rd versus 1st tertile of BE (or between the two categories for binary BE variables).
Models were adjusted for factors that were known or hypothesized to be associated with baseline BE and longitudinal weight change. Our primary model adjusted for sex (male and female), baseline age (nonlinearly via spline terms with 10 DF), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and non-Hispanic Asian), Medicaid (yes, no), and baseline weight (nonlinearly via spline terms with 5 DF, allowing association to differ by gender), and patient residential property values at the tax parcel-level (modeled as inflation-adjusted, year-specific deciles). Patient residential property values were used as a proxy measure for SES since the EHR does not contain traditional measures of SES (e.g. income, education) (see Technical Appendix for more detail). Note that this model, as well as all other models, adjusted for baseline weight, which could itself be impacted by the baseline BE, since each patient resided at their address for an unknown period of time prior to their baseline weight measure. Thus, we estimate the association between baseline BE and weight change, beyond any association between baseline BE and baseline weight.
We also ran three sensitivity analyses to test the robustness of our findings. First, we ran our primary models additionally adjusting for smoking status and comorbidities (diabetes, mental health, and mood disorders). Given that smoking status was missing for approximately 21.4% of our cohort, the sample size for this analysis was smaller. Second, out of concern that our primary model could potentially remove some of the association between the BE and weight change if property values lie on the causal pathway, we ran our primary model without adjustment for property values. Note, however, that in our primary models, we hypothesized that the influence of confounding by SES was larger than the influence of the BE mediated by year-specific property values. Third, to investigate whether our results may have been sensitive to the choice of cut-points used to categorize the continuous BE measures (i.e., tertiles) [41], we additionally ran models for residential density as well as for counts of supermarkets and fast food restaurants as continuous metrics, in which we flexibly modeled the exposure-response function (to allow for non-linearity) by using spline terms with 5 DF.
Mutually adjusted models
As a secondary analysis, we mutually adjusted for other BE characteristics, applying the same set of covariates from our primary model. We focused on associations with residential density and food environment BE characteristics, given the correlation among residential, population, and road intersection densities, with Pearson correlation coefficients ranging from 0.66 to 0.92. Since mutually adjusted models that include BE measures with different buffer sizes can be difficult to interpret, we selected a common buffer size of 1,600 m. Mutually adjusted models of residential density were adjusted for binary fast food and supermarket measures, which were each interacted with spline terms of time since baseline as the primary BE predictor. Mutually adjusted models of each food BE measure were adjusted for residential density by interacting residential density tertiles with spline terms of time, with inflection points as previously described.
RESULTS
Table 1 shows baseline characteristics, median follow-up time, and median number of weight measurements of participants included in the M2H cohort. The majority of patients were female (60.2%), between the ages of 30 to 44 years (30.5%), White (67.2%), had commercial insurance (94.7%), and had a BMI between 18.5 to 24.9 kg/m2 (37.7%). Smokers comprised 10.4% of patients while 4.9% had a diagnosis of diabetes. The median number of weight measurements per patient was 5 with a median of 2 years between each assessment. The median number of weight measurements was generally consistent across sociodemographic characteristics and health but were slightly higher for older patients and those with Medicare, higher BMIs, and a diagnosis of diabetes. In addition, with respect to patient baseline addresses, 78% of were residential, 16.2% were commercial apartments, and 5.8% were condominiums (data not shown).
Table 1.
Baseline characteristics, follow-up time, and number of weight measurements
| Characteristic | n | % | Yrs. Between weights | No. weights |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | |||
| Overall cohort | 115,260 | 100.0 | 2.0 (0.7, 4.5) | 5 (3, 11) |
| Sex | ||||
| Female | 69,384 | 60.2 | 1.9 (0.7, 4.4) | 5 (3, 11) |
| Male | 45,876 | 39.8 | 2.1 (0.7, 4.8) | 5 (3, 10) |
| Age categories (years) | ||||
| 18 to 29 | 26,248 | 22.8 | 1.3 (0.5, 3.1) | 4 (2, 7) |
| 30 to 44 | 35,133 | 30.5 | 1.8 (0.7, 4.4) | 5 (3, 9) |
| 45 to 54 | 28,266 | 24.5 | 3.0 (1.1, 6.8) | 7 (4, 15) |
| 55 to 64 | 25,613 | 22.2 | 2.1 (0.8, 4.3) | 6 (3, 12) |
| Race/ethnicity | ||||
| non-Hispanic White | 77,398 | 67.2 | 2.0 (0.7, 4.6) | 5 (3, 11) |
| non-Hispanic Black | 8,403 | 7.3 | 1.8 (0.6, 4.3) | 5 (3, 11) |
| Hispanic | 7,017 | 6.1 | 1.7 (0.6, 4.0) | 5 (3, 10) |
| non-Hispanic Asian | 17,578 | 15.3 | 2.2 (0.8, 4.7) | 5 (3, 10) |
| Hawai’ian / Pacific Islander | 1,503 | 1.3 | 1.7 (0.6, 3.9) | 5 (3, 9) |
| Native American / Alaskan Native | 1,602 | 1.4 | 1.7 (0.6, 4.1) | 6 (3, 11) |
| Other | 1,759 | 1.5 | 1.8 (0.6, 4.1) | 5 (3, 10) |
| Insurance type | ||||
| Commercial | 109,146 | 94.7 | 2.0 (0.7, 4.6) | 5 (3, 11) |
| Medicaid | 4,109 | 3.6 | 1.5 (0.6, 3.3) | 5 (3, 10) |
| Medicare | 1,273 | 1.1 | 1.8 (0.7, 3.8) | 8 (4, 18) |
| Other | 732 | 0.6 | 0.8 (0.3, 1.8) | 3 (2, 6) |
| BMI categories | ||||
| 15.0 to 18.4 | 1,629 | 1.4 | 1.8 (0.6, 3.8) | 5 (3, 9) |
| 18.5 to 24.9 | 43,396 | 37.7 | 1.9 (0.7, 4.4) | 5 (3, 9) |
| 25.0 to 29.9 | 37,152 | 32.2 | 2.1 (0.7, 4.7) | 5 (3, 11) |
| 30.0 to 34.9 | 18,502 | 16.1 | 2.0 (0.7, 4.7) | 6 (3, 12) |
| 35.0 to 39.9 | 8,211 | 7.1 | 1.9 (0.7, 4.5) | 6 (3, 12) |
| 40.0 or more | 6,370 | 5.5 | 1.9 (0.6, 4.3) | 7 (3, 14) |
| Self-reported smoking status | ||||
| Current, Self-Report | 12,000 | 10.4 | 1.6 (0.5, 3.8) | 5 (3, 10) |
| Former, Self-Report | 16,747 | 14.5 | 1.8 (0.7, 4.1) | 5 (3, 11) |
| Never, Self-Report | 61,867 | 53.7 | 1.8 (0.7, 4.1) | 5 (3, 10) |
| Missing | 24,646 | 21.4 | 3.0 (1.0, 6.3) | 7 (3, 13) |
| Diabetes diagnosis | 5,685 | 4.9 | 1.9 (0.7, 4.3) | 8 (4, 16) |
BMI = body mass index, n = sample size, IQR = interquartile range
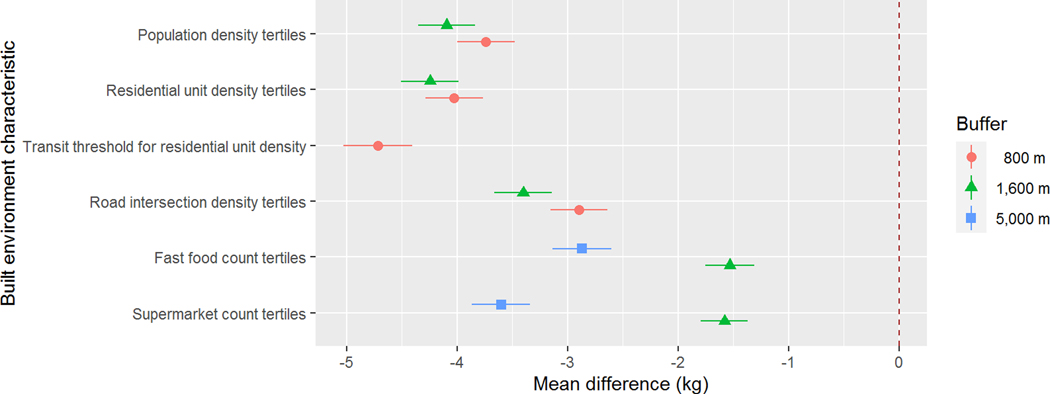
Table 2 and Figure 2 relate baseline BE characteristics to baseline BMI values, obesity prevalence, and weight. Patients in the highest tertile of population density, residential density, and road intersection density within an 800 m buffer from their home had lower mean weights, BMIs, and obesity prevalence when compared to individuals in the lowest tertile. Those with any fast food restaurants or any supermarkets within a 1,600 m radius of home had lower mean weights, BMIs, and obesity prevalence compared to participants with none. At a larger neighborhood scale, patients living with the highest tertile of fast food restaurant or supermarkets counts within 5,000 m from their home had lower mean weights, BMIs, and obesity prevalence compared to those participants in the lowest tertile.
Table 2.
Baseline built environment characteristics in relation to baseline BMI values and obesity prevalence
| Built environment characteristic | n | % | Mean BMI (SD) | Obese % |
|---|---|---|---|---|
| Overall | 115,260 | 100.0 | 27.8 (6.6) | 28.7 |
| Population density tertiles (800 m) | ||||
| Tertile 1 (0.0 to <15.8) | 38,420 | 33.3 | 28.1 (6.6) | 30.9 |
| Tertile 2 (15.8 to <26.0) | 38,420 | 33.3 | 28.3 (6.8) | 31.2 |
| Tertile 3 (26.0 to 129.5) | 38,420 | 33.3 | 27.1 (6.3) | 24.0 |
| Residential unit density tertiles (800 m) | ||||
| Tertile 1 (0.0 to <6.4) | 38,420 | 33.3 | 28.2 (6.6) | 31.1 |
| Tertile 2 (6.4 to <11.5) | 38,420 | 33.3 | 28.3 (6.8) | 31.6 |
| Tertile 3 (11.5 to 123.3) | 38,420 | 33.3 | 27.0 (6.2) | 23.4 |
| Transit threshold for residential unit density (800 m)a | ||||
| 0.0 to <18.0 | 99,360 | 86.2 | 28.0 (6.7) | 30.1 |
| 18.0 to 123.0 | 15,900 | 13.8 | 26.4 (6.0) | 20.0 |
| Road intersection density tertiles (800 m) | ||||
| Tertile 1 (0.0 to <0.5) | 38,416 | 33.3 | 28.2 (6.7) | 31.1 |
| Tertile 2 (0.5 to <0.7) | 38,264 | 33.2 | 28.1 (6.7) | 30.0 |
| Tertile 3 (0.7 to 1.9) | 38,580 | 33.5 | 27.2 (6.3) | 25.1 |
| Fast food count (1,600 m) | ||||
| None | 43,592 | 37.8 | 27.9 (6.5) | 29.5 |
| Any | 71,668 | 62.2 | 27.8 (6.7) | 28.2 |
| Fast food count tertiles (5,000 m) | ||||
| Tertile 1 (0 to <14) | 35,271 | 30.6 | 28.0 (6.5) | 30.0 |
| Tertile 2 (14 to <28) | 41,508 | 36.0 | 28.2 (6.7) | 31.0 |
| Tertile 3 (28 to 99) | 38,481 | 33.4 | 27.3 (6.5) | 25.0 |
| Supermarket count (1,600 m) | ||||
| None | 51,855 | 45.0 | 28.0 (6.6) | 30.1 |
| Any | 63,405 | 55.0 | 27.7 (6.6) | 27.6 |
| Supermarket count tertiles (5,000 m) | ||||
| Tertile 1 (0 to <5) | 33,732 | 29.3 | 28.3 (6.7) | 31.7 |
| Tertile 2 (5 to <9) | 38,450 | 33.4 | 28.3 (6.8) | 31.8 |
| Tertile 3 (9 to 26) | 43,078 | 37.4 | 27.0 (6.2) | 23.6 |
| Property value deciles (tax parcel-level, year-specific) | ||||
| Decile 1 | 11520 | 10.0 | 29.5 (7.8) | 38.6 |
| Decile 2 | 11487 | 10.0 | 28.6 (7.3) | 33.7 |
| Decile 3 | 11465 | 9.9 | 29.0 (7.1) | 35.9 |
| Decile 4 | 11516 | 10.0 | 28.6 (6.9) | 33.9 |
| Decile 5 | 11464 | 9.9 | 28.2 (6.5) | 31.6 |
| Decile 6 | 11561 | 10.0 | 27.7 (6.3) | 28.0 |
| Decile 7 | 11576 | 10.0 | 27.3 (6.1) | 25.2 |
| Decile 8 | 11534 | 10.0 | 27.0 (5.8) | 23.6 |
| Decile 9 | 11566 | 10.0 | 26.4 (5.3) | 20.0 |
| Decile 10 | 11571 | 10.0 | 25.8 (5.0) | 16.7 |
BMI = body mass index
Note: All densities calculated as units per hectare. Population, residential, and road intersection densities based on Euclidean distance. Fast food and supermarket counts based on network-based buffer. Property values are inflation-adjusted to 2017 United States dollars. Values in parentheses for property values deciles represent the midpoint of each decile.
Transit threshold refers to the residential unit density needed to support development of transit systems
Figure 2.
Mean difference in weight at baseline comparing the first and third tertiles of built environment characteristics at different buffer sizes, after adjusting for baseline demographics, height, and year-specific patient property values
Note: All densities are calculated as units per hectare. Models adjust for sex at birth (male and female), baseline age (nonlinearly via spline terms with 10 DF), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, Hawai’ian / Pacific Islander, Native American / Alaskan Native, and Other), Medicaid (yes/no), and baseline height (nonlinearly via spline terms with 5 DF, allowing association to differ by sex at birth), and patient residential property values. Separate models were fit for each BE variable. Models for fast food and supermarket counts at 1,600 m are binary comparisons of any vs. none, not tertiles. The model for transit threshold for residential unit density is also binary at the transit threshold: 18 units/hectare in 800 m.
Table 3 provides the estimated mean weight change at 1, 3, and 5 years from baseline in relation to baseline BE measures, adjusting for baseline socio-demographics and weight. Overall, mean weight change in the sample was 0.06 kg (95% confidence interval (CI): 0.03, 0.10) at 1 year, 0.64 kg (95% CI: 0.59, 0.68) at 3 years and 0.95 kg (95% CI: 0.90, 1.00) at 5 years. At 5 years, compared with patients in the lowest tertile, patients residing in areas with the highest tertile of population density (mean weight change: 0.76 kg, 95% CI: 0.67, 0.86 vs. 1.12 kg, 95% CI: 1.03, 1.20), residential density (mean weight change: 0.75 kg, 95% CI: 0.65, 0.84 vs. 1.05 kg, 95% CI: 0.97, 1.13), and road intersection density within a 800 m buffer from their home (mean weight change: 0.81 kg, 95% CI: 0.72, 0.84 vs. 1.03, 95% CI: 0.72, 0.90) experienced a moderately lower weight gain. Using the binary transit threshold for residential unit density, patients residing in neighborhoods with residential densities above 18 units/hectare in 800 m experienced lower weight gained at 5 years (mean weight change: 0.63 kg, 95% CI: 0.45, 0.80 vs. 0.98, 95% CI: 0.93, 1.04). Likewise, those patients residing in locations with the highest fast food (mean weight change: 0.75 kg, 95% CI: 0.66, 0.84 vs. 1.09, 95% CI: 1.00, 1.17) and supermarkets counts (mean weight change: 0.75 kg, 95% CI: 0.67, 0.84 vs. 1.14, 95% CI: 1.05, 1.23) within a 5,000 m buffer from their home experienced moderately lower weight gain compared to those in the lowest tertile. Patients with any fast food or supermarkets within 1,600 m of their home experienced less weight gain compared with those having none in proximity to their home. Parallel patterns were observed at 1 and 3 years. Sensitivity analyses adjusting for smoking status and comorbidities as well as removing residential property values as a covariate had little influence on model estimates (Supplemental Tables 2 and 3). Additionally, results from continuous BE exposure models were consistent with our primary analysis, indicating that increasing values of residential unit density, fast food count, and supermarket count were associated with lower weight change (Supplemental Figure 1).
Table 3.
Built environment characteristics and their relationship with change in weight (in kilograms) at 1, 3, and 5 years from baseline (mean difference), after adjusting for baseline demographics, weight, and year-specific patient property values at the tax parcel level
| Built environment characteristic | 1 year | 3 year | 5 year | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Wt. Change (95% CI) | P-value | Wt. Change (95% CI) | P-value | Wt. Change (95% CI) | P-value | |
| Overall | 0.06 (0.03, 0.10) | 0.64 (0.59, 0.68) | 0.95 (0.90, 1.00) | |||
|
| ||||||
| Population density tertiles (800 m) | ||||||
| Tertile 1 (0.0 to <15.8) | 0.17 (0.10, 0.23) | 0.75 (0.68, 0.83) | 1.12 (1.03, 1.20) | |||
| Tertile 2 (15.8 to <26.0) | 0.07 (0.00, 0.13) | 0.64 (0.56, 0.71) | 0.94 (0.86, 1.03) | |||
| Tertile 3 (26.0 to 129.5) | −0.06 (−0.12, 0.01) | <0.001 | 0.51 (0.43, 0.59) | <0.001 | 0.76 (0.67, 0.86) | <0.001 |
|
| ||||||
| Residential unit density tertiles (800 m) | ||||||
| Tertile 1 (0.0 to <6.4) | 0.15 (0.09, 0.21) | 0.73 (0.66, 0.81) | 1.05 (0.97, 1.13) | |||
| Tertile 2 (6.4 to <11.5) | 0.11 (0.04, 0.17) | 0.68 (0.61, 0.76) | 1.01 (0.92, 1.09) | |||
| Tertile 3 (11.5 to 123.3) | −0.09 (−0.15, −0.02) | <0.001 | 0.47 (0.39, 0.55) | <0.001 | 0.75 (0.65, 0.84) | <0.001 |
|
| ||||||
| Transit threshold for residential unit density (800 m) | ||||||
| 0.0 to <18.0 | 0.09 (0.05, 0.13) | 0.67 (0.63, 0.72) | 0.98 (0.93, 1.04) | |||
| 18.0 to 123.0 | −0.16 (−0.27, −0.06) | <0.001 | 0.33 (0.19, 0.47) | <0.001 | 0.63 (0.45, 0.80) | <0.001 |
|
| ||||||
| Road intersection density tertiles (800 m) | ||||||
| Tertile 1 (0.0 to <0.5) | 0.11 (0.04, 0.17) | 0.69 (0.62, 0.77) | 1.03 (0.95, 1.11) | |||
| Tertile 2 (0.5 to <0.7) | 0.09 (0.02, 0.15) | 0.70 (0.62, 0.77) | 1.00 (0.91, 1.08) | |||
| Tertile 3 (0.7 to 1.9) | −0.01 (−0.08, 0.05) | 0.009 | 0.52 (0.44, 0.60) | 0.002 | 0.81 (0.72, 0.90) | <0.001 |
|
| ||||||
| Fast food count (1,600 m) | ||||||
| None | 0.13 (0.07, 0.19) | 0.68 (0.61, 0.75) | 1.01 (0.93, 1.09) | |||
| Any | 0.02 (−0.03, 0.07) | 0.006 | 0.61 (0.55, 0.67) | 0.130 | 0.91 (0.84, 0.97) | 0.045 |
|
| ||||||
| Fast food count tertiles (5,000 m) | ||||||
| Tertile 1 (0 to <14) | 0.13 (0.06, 0.19) | 0.74 (0.67, 0.82) | 1.09 (1.00, 1.17) | |||
| Tertile 2 (14 to <28) | 0.10 (0.04, 0.16) | 0.69 (0.61, 0.76) | 0.99 (0.91, 1.07) | |||
| Tertile 3 (28 to 99) | −0.05 (−0.11, 0.02) | <0.001 | 0.47 (0.39, 0.55) | <0.001 | 0.75 (0.66, 0.84) | <0.001 |
|
| ||||||
| Supermarket count (1,600 m) | ||||||
| None | 0.12 (0.07, 0.18) | 0.69 (0.62, 0.75) | 1.01 (0.94, 1.08) | |||
| Any | 0.01 (−0.04, 0.06) | 0.004 | 0.60 (0.53, 0.66) | 0.039 | 0.90 (0.83, 0.97) | 0.025 |
|
| ||||||
| Supermarket count tertiles (5,000 m) | ||||||
| Tertile 1 (0 to <5) | 0.16 (0.09, 0.23) | 0.77 (0.69, 0.85) | 1.14 (1.05, 1.23) | |||
| Tertile 2 (5 to <9) | 0.09 (0.03, 0.15) | 0.67 (0.59, 0.74) | 0.99 (0.90, 1.07) | |||
| Tertile 3 (9 to 26) | −0.05 (−0.11, 0.02) | <0.001 | 0.50 (0.42, 0.57) | <0.001 | 0.75 (0.67, 0.84) | <0.001 |
Wt = weight, CI = confidence interval
Note: All densities are calculated as units per hectare. Population, residential, and road intersection densities based on Euclidean distance. Fast food and supermarket counts based on network-based buffer. Transit threshold refers to the residential unit density needed to support development of transit systems. Models adjust for sex (male and female), baseline age (nonlinearly via spline terms with 10 DF), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, Hawai’ian / Pacific Islander, Native American / Alaska Native, and Other), Medicaid (yes/no), and baseline weight (nonlinearly via spline terms with 5 DF, allowing association to differ by gender), and patient residential property values at the tax parcel level. Separate model fit for each BE variable. Models for fast food and supermarket counts at 1600m are binary comparisons of any vs. none, not tertiles. P-values compare 1, 3, and 5-year weight change between the third and first tertile (or any versus none for binary variables).
Mutually adjusted models
Table 4 provides the estimated mean weight change at 1, 3, and 5 years from baseline mutually adjusting for residential density and binary BE measures of fast food and supermarket counts. When adjusting for residential density, the observed association between fast food count (any versus none within 1,600 m) and 5-year mean weight change were attenuated. For patients with a fast food restaurant in their neighborhood buffer, the mean weight change was 0.97 kg (95% CI: 0.86, 1.08) versus 0.87 kg (95% CI: 0.75, 1.00) for patients without a fast food restaurant. Similarly, for patients with a supermarket in their neighborhood buffer, the mean weight change from baseline to 5 years was 0.96 kg (95% CI: 0.85, 1.07) versus 0.90 kg (95% CI: 0.78, 1.02) for patients without a supermarket. Conversely, the association between residential density and mean weight change at 5 years follow-up between the highest and lowest residential unit density tertiles was robust to adjustment for food environment (mean weight change: 0.78 kg, 95% CI: 0.67, 0.89 vs. 1.24, 95% CI: 1.11, 1.38).
Table 4.
Built environment characteristics and their relationship with change in weight (in kilograms) at 1, 3, and 5 years from baseline (mean difference) comparing the third and first tertile of residential unit density and any vs. no fast food and supermarkets at a 1600 m buffer, after mutually adjusting for baseline BE characteristics and demographics, weight, and property values
| Built environment characteristic | 1 year | 3 year | 5 year | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Wt. Change (95% CI) | P-value | Wt. Change (95% CI) | P-value | Wt. Change (95% CI) | P-value | |
| Residential unit density tertiles (1600 m) | ||||||
| Tertile 1 (0.0 to <5.9) | 0.18 (0.08, 0.28) | 0.84 (0.72, 0.96) | 1.24 (1.11, 1.38) | |||
| Tertile 2 (5.9 to <10.5) | 0.12 (0.03, 0.20) | 0.72 (0.62, 0.82) | 1.00 (0.89, 1.11) | |||
| Tertile 3 (10.5 to 87.4) | −0.06 (−0.14, 0.03) | <0.001 | 0.50 (0.40, 0.60) | <0.001 | 0.78 (0.67, 0.89) | <0.001 |
| Fast food count (1,600 m) | ||||||
| None | 0.10 (0.00, 0.19) | 0.62 (0.51, 0.73) | 0.87 (0.75, 1.00) | |||
| Any | 0.09 (0.01, 0.18) | 0.890 | 0.69 (0.59, 0.79) | 0.170 | 0.97 (0.86, 1.08) | 0.110 |
| Supermarket count (1,600 m) | ||||||
| None | 0.11 (0.02, 0.19) | 0.65 (0.54, 0.76) | 0.90 (0.78, 1.02) | |||
| Any | 0.09 (0.00, 0.17) | 0.710 | 0.68 (0.58, 0.78) | 0.560 | 0.96 (0.85, 1.07) | 0.280 |
Wt = weight, CI = confidence interval
Note: Residential density based on Euclidean distance and calculated as units per hectare. Fast food and supermarket counts based on network-based buffer. Models adjust for sex (male and female), baseline age (nonlinearly via spline terms with 10 DF), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, Hawai’ian / Pacific Islander, Native American / Alaskan Native, and Other), Medicaid (yes/no), and baseline weight (nonlinearly via spline terms with 5 DF, allowing association to differ by gender), and patient residential property values. Separate model fit for each combination of residential unit density and fast food count and residential unit density and supermarket count. Models for fast food and supermarket counts at 1600 m are binary comparisons of any vs. none, not tertiles. P-values compare 1, 3, and 5-year weight change between the third and first tertile (or any versus none for binary variables).
DISCUSSION
Higher population and residential density as well as greater spatial access to supermarkets and fast foods were each associated with lower mean body weights, mean BMI, and obesity prevalence at baseline. Insofar as population and residential densities are proxies for walkability [6], these cross-sectional findings are consistent with prior research [1,4,42–48,8–10,13–17]. We also found that residential, population, and intersection density had comparable effects on obesity prevalence at baseline. It is worth noting that lower BMIs and obesity prevalence were observed only at the highest tertiles of urban form densities suggesting a potential threshold.
Our metrics of the food environment were based on prior published work that also made use of area counts and distances from the home [1,5,8,43]. Supermarkets, grocery stores, fast food restaurants, and convenience stores are the most commonly studied food sources [1,5,8,43]. In multiple published studies, proximity to supermarkets was associated with lower obesity prevalence [1,8,42,43]. By contrast, many studies linked greater spatial access to fast food restaurants to higher obesity prevalence. Still more studies found no relation between multiple aspects of the food environment and obesity [5]. The current finding linking fast food access to lower obesity risk runs counter to prior work finding higher obesity risk, or no relation [1,8,42,43]. However, the finding of lower obesity risk has been reported by some [49].
Where the present analyses departs from most prior cross-sectional work is by making use of long-term trajectories of measured body weight [11,18–22]. Higher residential, population, and intersection densities were associated with lower weight gain over 5 years. Likewise, higher supermarket and fast food counts were also associated with marginally lower weight gain over 5 years. Based on the present analyses, differences in mean weight gain between the highest and lowest groupings of BE variables (densities and counts) were less than 0.5 kg between baseline and year 1, 3, and 5. Nevertheless, even if the impact of the BE on 5-year weight gain seems small, these differences could potentially translate into larger cumulative weight gain over the entire life course.
Mutually adjusted models explored the joint influence of BE urban characteristics and the food environment on weight gain. When accounting for residential density, the lower weight gain associated with greater proximity to supermarkets and fast food restaurants was attenuated to the null. The finding that the food environment no longer had any influence on weight gain, after adjustment for urban characteristics, is consistent with recent longitudinal work and a body of prior work that found no association between supermarket or fast food access and obesity [5,22]. These models further suggest that the observed protective effect of supermarkets on obesity prevalence may be driven by urban form and that these measures are highly correlated. Conversely, the influence of residential density on weight gain was robust to adjusting for food environment variables.
This study had limitations. First, the baseline BE measures cannot take into account variations in the duration of exposure. The duration of residence at each patient’s baseline address prior to inclusion in the study is unknown. We did not explore the impact of any secular changes in the BE and neighborhood foodscapes on patient’s weight history; however, this will be explored in future analyses. Second, residing in a given neighborhood does not necessarily predict full use of that neighborhood’s resources [50]. Some investigators have sought to quantify an individual’s realized experience of the BE using GPS tracking devices to establish activity spaces [51,52]. Unfortunately, the use of large scale geocoded EHR data precluded this option. Third, the study was limited to employed and insured patients and therefore this sample likely excludes individuals with long-term disability and loss of insurance may have removed participants from the study. Therefore, this study’s findings may not be generalizable to other populations within Washington State or outside of the US. Fourth, our evaluation of obesogenic characteristics is primarily focused on a US urban context and it is unclear whether these findings are readily generalizable internationally to other metropolitan centers. Fifth, this study focuses only on the BE influence on weight change in adults, it is unclear if similar influences are present in youth. Sixth, data on residential property values, a key covariate in this analysis may not be readily accessible, useful in areas bereft of open markets or where home sales or rent renewals are infrequent, or predictive of health in all countries.
Future work should more fully consider the underlying social and economic influences on the relation between place and obesity prevalence [53]. The choice of place, as well as the quality of the local food supply, may depend on neighborhood composition, history of racial segregation, and unequal geographic distributions of poverty and wealth [54–56]. We attempted to account for this through patient property values adjustment [57]. In future M2H analysis we will evaluate whether these observed associations vary across demographic (age, sex, race/ethnicity) and SES (residential property values) factors.
More difficult to capture in studies of the BE and obesity is the extent to which residential self-selection may influence observed association between the BE and health. Individuals with the economic resources and privilege to be able to choose where they live often elect to reside in neighborhoods that have more resources and may engage in lifestyles that lower obesity risk [1,58]. Conversely, individuals with fewer resources must make decisions on where to live based on affordability rather than aesthetics, and may be less mobile, which may have implications for both the type and duration of BE exposures as well as health. Evaluating the influence of moving to a new BE on health is a future aim of the M2H study.
In conclusion, our selected BE metrics were strongly associated with obesity prevalence at baseline but had limited influence on body weight gain over a 5-year period. It would appear that those neighborhoods that are commonly described as “obesogenic” might have less obesogenic power than expected. That finding has implications for those obesity prevention policies or programs that are grounded in the assumption that BE-driven interventions will reduce neighborhood obesity prevalence. BE features may not help reverse the obesity epidemic; rather it is socioeconomic, cultural, and behavioral factors that lead to the geographic clustering of people with obesity. It may also be time to replace the concept of obesogenic neighborhoods with “neighborhoods with concentrated obesity.”
Supplementary Material
ACKNOWLEDGEMENTS
This manuscript was supported by three grants from the National Institutes of Health: 1 R01 DK 114196, 5 R01 DK076608, and 4 R00LM012868.
Competing interesting statement: Adam Drewnowski has received grants, honoraria, and consulting fees from numerous food, beverage, and ingredient companies and from other commercial and nonprofit entities with an interest in diet quality and nutrient density of foods. The University of Washington receives research funding from public and private sectors.
Footnotes
All other authors have no conflicts of interest to declare.
REFERENCES
- 1.Drewnowski A, Buszkiewicz J, Aggarwal A, Rose C, Gupta S, Bradshaw A. Obesity and the Built Environment: A Reappraisal. Obesity. 2020;28:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parise I. The built environment and obesity: You are where you live. Aust J Gen Pract. NLM (Medline); 2020;49:226–30. [DOI] [PubMed] [Google Scholar]
- 3.Congdon P. Obesity and urban environments. Int. J. Environ. Res. Public Health. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garfinkel-Castro A, Kim K, Hamidi S, Ewing R. Obesity and the built environment at different urban scales: examining the literature. Nutr Rev. 2017;75:51–61. [DOI] [PubMed] [Google Scholar]
- 5.Wilkins E, Radley D, Morris M, Hobbs M, Christensen A, Marwa WL, et al. A systematic review employing the GeoFERN framework to examine methods, reporting quality and associations between the retail food environment and obesity. Heal. Place 2019. p. 186–99. [DOI] [PubMed] [Google Scholar]
- 6.Mooney SJ, Hurvitz PM, Moudon AV, Zhou C, Dalmat R, Saelens BE. Residential neighborhood features associated with objectively measured walking near home: Revisiting walkability using the Automatic Context Measurement Tool (ACMT). Heal Place. 2020;63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith M, Hosking J, Woodward A, Witten K, MacMillan A, Field A, et al. Systematic literature review of built environment effects on physical activity and active transport - an update and new findings on health equity. Int J Behav Nutr Phys Act. 2017;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lake A, Townshend T, Burgoine T, Buttriss J, Welch A, Kearney J, et al. Obesogenic neighbourhood food environments. In: Buttriss J, Welch A, JM K, SA L-N, editors. Public Heal Nutr Nutr Soc Textb Ser. 2nd ed. 2017. p. 327–38. [Google Scholar]
- 9.Devarajan R, Prabhakaran D, Goenka S. Built environment for physical activity—An urban barometer, surveillance, and monitoring. Obes Rev. 2020;21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCormack G, Blackstaffe A, Nettel-Aguirre A, Csizmadi I, Sandalack B, Uribe F, et al. The Independent Associations between Walk Score® and Neighborhood Socioeconomic Status, Waist Circumference, Waist-To-Hip Ratio and Body Mass Index Among Urban Adults. Int J Environ Res Public Health. 2018;15:1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kowaleski-Jones L, Zick C, Smith KR, Brown B, Hanson H, Fan J. Walkable neighborhoods and obesity: Evaluating effects with a propensity score approach. SSM - Popul Heal. 2018;6:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hobbs M, Griffiths C, Green MA, Jordan H, Saunders J, McKenna J. Neighbourhood typologies and associations with body mass index and obesity: A cross-sectional study. Prev Med (Baltim). 2018;111:351–7. [DOI] [PubMed] [Google Scholar]
- 13.Salvo G, Lashewicz B, Doyle-Baker P, McCormack G. Neighbourhood Built Environment Influences on Physical Activity among Adults: A Systematized Review of Qualitative Evidence. Int J Environ Res Public Health. 2018;15:897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bancroft C, Joshi S, Rundle A, Hutson M, Chong C, Weiss CC, et al. Association of proximity and density of parks and objectively measured physical activity in the United States: A systematic review. Soc. Sci. Med 2015. p. 22–30. [DOI] [PubMed] [Google Scholar]
- 15.Kaczynski AT, Besenyi GM, Stanis SWA, Koohsari MJ, Oestman KB, Bergstrom R, et al. Are park proximity and park features related to park use and park-based physical activity among adults? Variations by multiple socio-demographic characteristics. Int J Behav Nutr Phys Act. 2014;11:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaczynski AT, Koohsari MJ, Stanis SAW, Bergstrom R, Sugiyama T. Association of street connectivity and road traffic speed with park usage and park-based physical activity. Am J Health Promot. 2014;28:197–203. [DOI] [PubMed] [Google Scholar]
- 17.Mayne SL, Auchincloss AH, Michael YL. Impact of policy and built environment changes on obesity-related outcomes: A systematic review of naturally occurring experiments. Obes Rev. 2015;16:362–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drewnowski A, Aggarwal A, Tang W, Moudon A. Residential property values predict prevalent obesity but do not predict 1‐year weight change. Obesity. 2015;23:671–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powell-Wiley T, Moore K, Allen N, Block R, Evenson K, Mujahid M, et al. Associations of Neighborhood Crime and Safety and With Changes in Body Mass Index and Waist Circumference: The Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2017;186:280–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leonard T, Ayers C, Das SR, Neeland IJ, Powell-Wiley TM. Do neighborhoods matter differently for movers and non-movers? Analysis of weight gain in the longitudinal Dallas Heart Study. Heal Place. 2017;44:52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ou S. Are some neighborhoods bad for your waistline? A test of neighborhood exposure effects on BMI. J Health Econ. 2019;63:52–63. [DOI] [PubMed] [Google Scholar]
- 22.Okuyama K, Li X, Abe T, Hamano T, Franks PW, Nabika T, et al. Fast food outlets, physical activity facilities, and obesity among adults: a nationwide longitudinal study from Sweden. Int J Obes. 2020;1–9. [DOI] [PubMed] [Google Scholar]
- 23.Mooney SJ, Bobb JF, Hurvitz PM, Anau J, Theis MK, Drewnowski A, et al. Impact of Built Environments on Body Weight (the Moving to Health Study): Protocol for a Retrospective Longitudinal Observational Study. JMIR Res Protoc. 2020;9:e16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drewnowski A, Arterburn D, Zane J, Aggarwal A, Gupta S, Hurvitz PM, et al. The Moving to Health (M2H) approach to natural experiment research: A paradigm shift for studies on built environment and health. SSM - Popul Heal. 2019;7:100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.ESRI. ArcGIS Desktop: Release 10. Redlands, CA: Environmental Systems Research Institute; 2011. [Google Scholar]
- 26.Hurvitz PM, Moudon AV, Kang B, Saelens BE, Duncan GE. Emerging Technologies for Assessing Physical Activity Behaviors in Space and Time. Front Public Heal. 2014;2:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pouliou T, Elliott SJ. Individual and socio-environmental determinants of overweight and obesity in Urban Canada. Heal Place. 2010;16:389–98. [DOI] [PubMed] [Google Scholar]
- 28.Huang R, Moudon AVA, Cook AJ, Drewnowski A. The spatial clustering of obesity: does the built environment matter? 2015;28:604–12. [DOI] [PubMed] [Google Scholar]
- 29.Sarkar C, Webster C, Gallacher J. Association between adiposity outcomes and residential density: a full-data, cross-sectional analysis of 419 562 UK Biobank adult participants. Lancet Planet Heal. 2017;1:e277–88. [DOI] [PubMed] [Google Scholar]
- 30.Lopez RP. Neighborhood risk factors for obesity. Obesity. 2007;15:2111–9. [DOI] [PubMed] [Google Scholar]
- 31.Lovasi GS, Neckerman KM, Quinn JW, Weiss CC, Rundle A. Effect of individual or neighborhood disadvantage on the association between neighborhood walkability and body mass index. Am J Public Health. 2009;99:279–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rundle A, Field S, Park Y, Freeman L, Weiss CC, Neckerman K. Personal and neighborhood socioeconomic status and indices of neighborhood walk-ability predict body mass index in New York City. Soc Sci Med. 2008;67:1951–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Durand CP, Oluyomi AO, Gabriel KP, Salvo D, Sener IN, Hoelscher DM, et al. The Effect of Light Rail Transit on Physical Activity: Design and Methods of the Travel-Related Activity in Neighborhoods Study. Front Public Heal. 2016;4:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lovasi GS, Grady S, Rundle A. Steps Forward: Review and Recommendations for Research on Walkability, Physical Activity and Cardiovascular Health. Public Health Rev. 2011;33:484–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vernez Moudon A, Drewnowski A, Duncan GE, Hurvitz PM, Saelens BE, Scharnhorst E. Characterizing the food environment: Pitfalls and future directions. Public Health Nutr. 2013;16:1238–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pushkarev B, Zupan J. Public transportation and land use policy. Bloomington: Indiana University Press; 1977. [Google Scholar]
- 37.Frank LD, Pivo G. Impacts of Mixed Use and Density on Utilization of Three Modes of Travel: Single-Occupant Vehicle, Transit, and Walking. Transp Res Rec. 1994;1466:44–52. [Google Scholar]
- 38.Casey JA, Schwartz BS, Stewart WF, Adler NE. Using Electronic Health Records for Population Health Research: A Review of Methods and Applications. Annu Rev Public Health. 2016;37:61–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hurvitz PM, Moudon AV. Home versus nonhome neighborhood: Quantifying differences in exposure to the built environment. Am J Prev Med. 2012;42:411–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee C, Moudon AV, Courbois JYP. Built Environment and Behavior: Spatial Sampling Using Parcel Data. Ann Epidemiol. 2006;16:387–94. [DOI] [PubMed] [Google Scholar]
- 41.Lamb KE, White SR. Categorisation of built environment characteristics: The trouble with tertiles. Int J Behav Nutr Phys Act. 2015;12:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Townshend T, Lake A. Obesogenic environments: Current evidence of the built and food environments. Perspect. Public Health. 2016. p. 38–44. [DOI] [PubMed] [Google Scholar]
- 43.Caspi CE, Sorensen G, Subramanian SVVS, Kawachi I. The local food environment and diet: A systematic review. Heal Place. 2012;18:1172–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rundle AG, Chen Y, Quinn JW, Rahai N, Bartley K, Mooney SJ, et al. Development of a Neighborhood Walkability Index for Studying Neighborhood Physical Activity Contexts in Communities across the U.S. over the Past Three Decades. J Urban Heal. 2019;96:583–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morgan Hughey S, Kaczynski AT, Porter DE, Hibbert J, Turner-McGrievy G, Liu J. Development and testing of a multicomponent obesogenic built environment measure for youth using kernel density estimations. Heal Place. 2019;56:174–83. [DOI] [PubMed] [Google Scholar]
- 46.Martínez-García Trescastro-López, Galiana-Sánchez Pereyra-Zamora. Data Collection Instruments for Obesogenic Environments in Adults: A Scoping Review. Int J Environ Res Public Health. 2019;16:1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barquera S, Hernández-Barrera L, Rothenberg SJ, Cifuentes E. The obesogenic environment around elementary schools: Food and beverage marketing to children in two Mexican cities. BMC Public Health. 2018;18:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jones A, Bentham G, Foster C, M H, Panter J. Tackling obesities: future choices-obesogenic environments-evidence review. London, UK; 2007. [Google Scholar]
- 49.Bader MDM, Schwartz-Soicher O, Jack D, Weiss CC, Richards CA, Quinn JW, et al. More neighborhood retail associated with lower obesity among New York City public high school students. Heal Place. Elsevier Ltd; 2013;23:104–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sharp L, Macrorie R, Turner A. Resource efficiency and the imagined public: Insights from cultural theory. Glob Environ Chang. 2015;34:196–206. [Google Scholar]
- 51.Chaix B. Mobile Sensing in Environmental Health and Neighborhood Research. Annu Rev Public Health. 2018;39:367–84. [DOI] [PubMed] [Google Scholar]
- 52.Kestens Y, Thierry B, Shareck M, Steinmetz-Wood M, Chaix B. Integrating activity spaces in health research: Comparing the VERITAS activity space questionnaire with 7-day GPS tracking and prompted recall. Spat Spatiotemporal Epidemiol. 2018;25:1–9. [DOI] [PubMed] [Google Scholar]
- 53.An R, Sturm R. School and residential neighborhood food environment and diet among California youth. Am J Prev Med. 2012;42:129–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McClure E, Feinstein L, Cordoba E, Douglas C, Emch M, Robinson W, et al. The legacy of redlining in the effect of foreclosures on Detroit residents’ self-rated health. Heal Place. 2019;55:9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017. p. 1453–63. [DOI] [PubMed] [Google Scholar]
- 56.Jacoby SF, Dong B, Beard JH, Wiebe DJ, Morrison CN. The enduring impact of historical and structural racism on urban violence in Philadelphia. Soc Sci Med. 2018;199:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Drewnowski A, Aggarwal A, Cook A, Stewart O, Moudon AV. Geographic disparities in Healthy Eating Index scores (HEI-2005 and 2010) by residential property values: Findings from Seattle Obesity Study (SOS). Prev Med (Baltim). 2016;83:46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Drewnowski A, Aggarwal A, Rehm C. Environments perceived as obesogenic have lower residential property values. Am J Prev Med. 2014;47:260–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.