ABSTRACT.
Poliomyelitis (polio) is a communicable viral disease that mainly affects under-5 children. This study focuses on the impact of women’s empowerment and women’s working status on the uptake of polio vaccination of children in polio-endemic countries, including Pakistan and Afghanistan, and Nigeria, the latter of which has recently been declared polio-free. The polio vaccination status can be divided into no vaccination (NV), incomplete vaccination (IV), and complete vaccination. We used data from the most recent Demographic and Health Surveys (DHS) rounds for this manuscript. Multinomial logistic regression-based estimates suggest that mothers’ working status, empowerment, age, education, father’s education, and household wealth status reduce the risk of NV and IV in the polio-endemic countries (Afghanistan and Pakistan) and Nigeria. In addition, the mothers’ working status, empowerment, age, education, and father’s education increase the child’s healthcare information that helps complete polio vaccination of the child. On the other hand, the children whose mothers work in the agriculture sector or are engaged in a blue-collar job are more likely to remain unvaccinated than women in white-collar jobs. Similarly, mothers engaged in government jobs are more likely to get their children fully vaccinated than unemployed mothers. Thus, as a child’s polio vaccination is strongly dependent on a mother’s working status and empowerment, the focus of public policy on empowering women and promoting their labor force participation may increase polio vaccination uptake, besides adopting other measures to increase immunization.
INTRODUCTION
Contextualizing poliomyelitis.
Poliomyelitis (polio) is a crippling and infectious disease with lifelong socioeconomic costs.1 It is a communicable viral disease that mainly affects children under 5 years. Polio spreads through the fecal–oral route and accumulates in the intestine, from where it can invade the nervous system and paralyze the patient.2
Polio can be of two types: naturally occurring or vaccine-derived. Naturally occurring polio is called wild polio, which is of three types: type 1 (WPV1), type 2 (WPV2), and type 3 (WPV3). Two types of vaccines are widely used to protect against poliomyelitis: oral polio vaccine (OPV) and inactivated poliovirus vaccine (IPV). OPV may contain one, two, or all three types of attenuated vaccine. After WPV2 was eradicated in 2015, the world switched from trivalent OPV (used for all three types of WPV) to bivalent OPV (used for only WPV1 and WPV3). In contrast, IPV protects against all the three types of polioviruses. It differs from OPV because it does not contain a live virus and cannot cause vaccine-derived poliovirus (VDPV). However, IPV does not stop the transmission of the virus. As a result, OPV is often used to contain the outbreak of poliovirus even in those countries that exclusively use IPV as part of their routine immunization program. Countries that use bivalent OPV have added a single dose of IPV to protect against WPV2.3
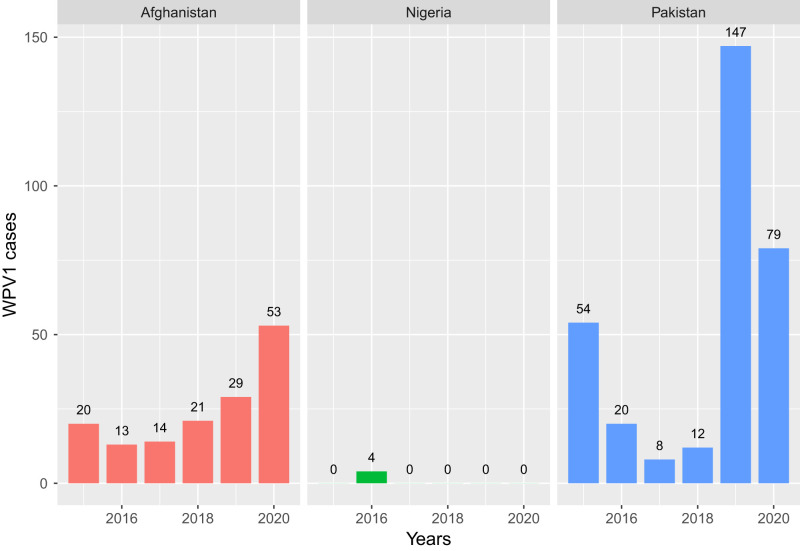
According to WHO, the last case of WPV2 was detected in 1999, and the last case of WPV3 was reported in Nigeria in 2012.2 Both WPV2 and WPV3 have been officially declared as “globally eradicated” in 2015 and 2019, respectively. However, as shown in Figure 1, WPV1 remains active in only two countries: Pakistan and Afghanistan.2
Figure 1.
Recent profile of WPV1 cases in Afghanistan, Pakistan, and Nigeria. Source: GPEI.4 This figure appears in color at www.ajtmh.org.
Role of polio immunization in polio eradication.
Immunization is a proven, cost-effective intervention to reduce morbidity and mortality from vaccine-preventable diseases.4 Each year immunization averts 2.5 million deaths in children younger than 5 years.5 Poliomyelitis affected nearly half a million people each year before the IPV was developed in 1955.6 Ever since the Global Polio Eradication Initiative was launched in 1988, the global incidence of poliomyelitis has dropped by 99%.7 However, there are wide gaps in the polio immunization coverage in Pakistan and Afghanistan. Sreevatsava et al.8 found that IPV coverage among children under 14 weeks in Pakistan was only 39% in 2018, while OPV coverage was only 42% in the same age cohort in 2018 in surveyed areas. In Afghanistan, only 51% of the children received all doses of each antigen though the recommended data of immunization and the recommended interval between two doses were not fully observed.9
Even if WPV2 and WPV3 are globally eradicated, and WPV1 is restricted only to Pakistan and Afghanistan, recent data shows that cVDPV cases are routinely reported from many African countries such as Burkina Faso, Democratic Republic of Congo, Ghana, Nigeria, and Sudan.10 Additionally, insufficient immunization and accessibility issues in Nigeria, especially in the regions marked by violence, such as Borno and Yobe and Lake Chad Basin, allow potential undetected paralytic cases even after Nigeria has been declared wild polio-free.11
Risk factors of incomplete polio immunization coverage.
The existing literature has identified a range of factors behind the failure of Afghanistan and Pakistan to eradicate polio.12,13 In the case of Pakistan, low coverage of routine immunization, insecurity, extensive movement of population, and lack of political commitment have been highlighted as the crucial determinants of incomplete immunization coverage. Pakistan has also witnessed armed attacks on polio vaccination teams.14 In Nigeria, people routinely boycotted polio vaccination as they thought it was unsafe for their children.15 Violence against and kidnapping of polio vaccinators also disrupted antipolio campaigns in Afghanistan and Nigeria.16
Public opinion is swayed against polio initiatives through rumors and hearsay. For example, in Pakistan, there is a perception that vaccination sterilizes the children, making some parents reluctant to get their children vaccinated against polio.17 In contrast, other parents are apprehensive because they think that the polio vaccine is made with religiously prohibited ingredients.18 Another study on Pakistan discovered the widespread public belief that polio immunization drives in Pakistan were a ploy behind which the United States targets terror networks.19
A vast literature has focused on maternal characteristics, which affect the extent of polio immunization drives. Some of the identified factors associated with successful immunization include a mother’s education, economic condition and empowerment,20 a mother’s willingness to immunize their children,21 a mother’s fears about the adverse effects of immunization,22 and the role of better communication between mothers and health providers to allay the fears of mothers about the outcomes of immunization.23 In addition, a mother’s agency and empowerment are some of the critical factors in the success of immunization. The women’s agency, typically measured by their decision-making power, is positively associated with complete immunization in childhood.24 In India, for instance, vaccination of infants was lower in families where women were not empowered.25
Maternal role in the success of immunization: Some theoretical reflections.
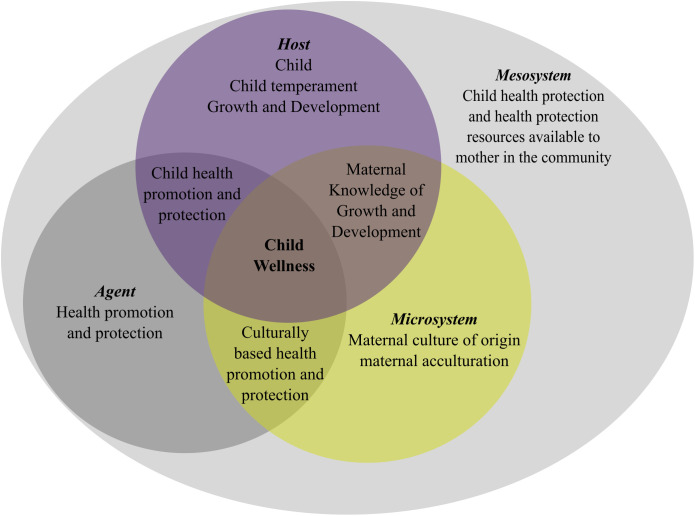
Although risk factors associated with the spread and eradication of poliovirus and the extent of polio immunization have been identified in the literature,12,26–28 all these risk factors interact in a complex way resulting in the gaps in immunization. So, instead of analyzing the risk factors in isolation, a more consistent approach would be to explore the reasons for immunization gaps in a unified theoretical framework. Ecological models of human interaction have been frequently used to understand the complicated health issues.29,30 The ecological model developed by Bronfenbrenner,31 and extended by Reifsnider et al.,32 consists of a set of nested structures corresponding with microsystem, mesosystem, exosystem, and macrosystem which can be used to examine the maternal characteristics to achieve success in immunization campaigns.
At the innermost level of the Bronfenbrenner ecological model32 is the microsystem, which includes both the mother and child. The following ecological levels represent settings that may or may not contain the mother. Still, these settings crucially affect a mother’s parenting style, which, in turn, has a significant impact on a child’s well-being.
The ecological model of high-level child wellness explains the mother’s role in child health. According to this framework, child health promotion and protection are influenced by the interaction of agents (health promotion and protection), host (child), and environment (a wide range of physical, biological, and socioeconomic factors). First, the interaction of the maternal microsystem (immediate setting containing mother and child) with the host is reflected in the maternal characteristics, such as her knowledge of the growth and development of the child. Second, the interaction between the mother’s mesosystem (a group of microsystems formed or extended whenever the mother moves in a new setting) is manifested in the type of informational resources available to facilitate child health promotion and protection activities.
The analog of the agent in this study is immunization, as shown in Figure 2. The interaction of the maternal microsystem with the host is reflected in her knowledge about the healthy growth of the child, which in turn, is based on her education, her understanding of immunization, and her ability to identify the mala fide intentions in the propaganda against immunization, and most importantly her ability to influence household members to ensure complete immunization.
Figure 2.
Ecological model for factors affecting polio immunization. Note: The ecological model is adapted from Reifsnider et al.32 This figure appears in color at www.ajtmh.org.
We test the hypothesis that maternal characteristics affect polio immunization in Afghanistan, Pakistan, and Nigeria. An analysis of these countries is vital because of the close association of these countries with the polio eradication endgame. In addition, Afghanistan and Pakistan are the only polio-endemic countries globally, and the severe issue of immunization gaps still exists in these countries, including Nigeria.
METHODS
Variables.
The outcome variable of our study is the status of polio vaccination which corresponds with incomplete vaccination (IV), no vaccination (NV), and complete vaccination (CV). If a child did not receive any vaccination at all, it is categorized as NV category. If a child received less than four doses of polio vaccination, it is categorized as IV. If a child gets all four vaccinations, it is categorized as CV. We considered a child to have received polio drop if 1) there is a vaccination date on the card, or 2) the mother reports the dose administration, or 3) vaccination is marked on the card. The description of variables is provided in Table 1.
Table 1.
Variable description
| Variables | Categories |
|---|---|
| Vaccination (Outcome variable) | Complete vaccination |
| Incomplete vaccination | |
| No vaccination | |
| Covariates | |
| Maternal empowerment | Not empowered |
| Empowered | |
| Mother’s occupational status | Not working |
| Working | |
| Mother’s current age | 15–24 |
| 25–34 | |
| 35+ | |
| Mother’s highest education level | No education |
| Primary | |
| Secondary | |
| Higher | |
| Mother’s exposure to media | No exposure |
| Exposure | |
| Father’s highest education level | No education |
| Primary | |
| Secondary | |
| Higher | |
| Household wealth quintile | Poorest |
| Poorer | |
| Middle | |
| Richer | |
| Rural/urban residence | Rural |
| Urban |
The reference category for each variable is in bold.
Among the maternal characteristics hypothesized to affect a child’s immunization status, a mother’s empowerment figures prominently. We used three questions from Demographic and Health Surveys (DHS) about women’s say in the decision-making to capture empowerment. The questions included: 1) Who makes decisions related to health? 2) Who makes decisions about the household’s major purchases? 3) Who makes decisions regarding relatives or family visits? If a woman makes the decision alone or with her husband, at least in one of the abovementioned situations, she is placed in the empowered category. Conversely, if a woman does not make any decision alone or with her husband in any category, she is placed in the not empowered category.
Following the previous literature,33 we constructed exposure to media using three indicators: access to newspaper, radio, and TV. A woman has no media exposure if she reports that she does not read newspapers, listens to the radio, or watches TV. However, if she accesses any one or more of the three popular media, she is considered to have media exposure.
Data source.
We used the nationally representative and internationally comparable DHS data for Pakistan (2018), Nigeria (2013), and Afghanistan (2019). A total of 60,118 ever-married women aged 15–49 years were included in the analysis. The sample size was 5,687 for Pakistan, 24,435 for Afghanistan, and 29,996 for Nigeria, respectively. The DHS data has a two-stage cluster design. Sampling weights are applied to ensure the representativeness of data. To account for sampling weights, stratification, and clustering in the sample design, the svy, and svyset commands were applied.
Nations depend on the success of their polio immunization programs, primarily on their routine immunization (RI) systems. However, in many developing countries, certain population groups remain susceptible to vaccine-preventable diseases because of the inadequacies of the RI systems. Consequently, many countries, including Pakistan, Afghanistan, and Nigeria, routinely undertake supplementary immunization activities (SIAs), called mass immunization campaigns, to vaccinate uncovered or underserved population groups against polio. However, the DHS collects the information on polio vaccination provided only by RI systems in Pakistan, Afghanistan, and Nigeria and ignores vaccination information collected through SIAs.34
Statistical methods.
The outcome variable, polio vaccination, has been split into three outcomes: NV, IV and CV. We used a multinomial logistic regression model to estimate the association between maternal characteristics and polio vaccination.
RESULTS
The bivariate association between polio vaccination coverage and a set of correlates depicted in Table 2 shows that except for the mother’s working status in Afghanistan, all variables in the three countries are significant at 95% or higher significance levels. We retained the insignificant factors in Afghanistan’s equation to ensure the comparability of our analyses.
Table 2.
Bivariate association
| Afghanistan: Vaccination | Nigeria: Vaccination | Pakistan: Vaccination | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | IV | CV | P value* | No | IV | CV | P value | No | IV | CV | P value | |
| Maternal empowerment | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | |||
| Not empowered | 20.7 | 51.1 | 28.1 | 0.000 | 36.7 | 44.5 | 18.8 | 0.000 | 6.2 | 33.5 | 60.3 | 0.016 |
| Empowered | 15.2 | 47.7 | 37.1 | – | 17.6 | 49.1 | 33.3 | – | 3.9 | 31.3 | 64.8 | – |
| Total | 17.4 | 49.0 | 33.6 | – | 25.3 | 47.2 | 27.5 | – | 5.0 | 32.4 | 62.6 | – |
| Mother’s current age | ||||||||||||
| 15–24 | 17.4 | 51.2 | 31.5 | 0.010 | 29.5 | 48.9 | 21.7 | 0.000 | 6.0 | 35.1 | 59.0 | 0.022 |
| 25–34 | 18.4 | 47.2 | 34.4 | – | 22.8 | 46.6 | 30.7 | – | 4.2 | 30.7 | 65.1 | – |
| 35+ | 15.5 | 49.5 | 35.0 | – | 24.5 | 46.8 | 28.7 | – | 5.9 | 33.4 | 60.7 | – |
| Total | 17.5 | 48.9 | 33.6 | – | 25.0 | 47.3 | 27.7 | – | 5.0 | 32.4 | 62.7 | – |
| Rural/urban residence | ||||||||||||
| Rural | 18.8 | 49.7 | 31.5 | 0.000 | 31.2 | 49.0 | 19.8 | 0.000 | 5.4 | 33.9 | 60.6 | 0.042 |
| Urban | 12.8 | 46.0 | 41.1 | – | 15.6 | 44.5 | 39.9 | – | 4.1 | 29.1 | 66.8 | – |
| Total | 17.5 | 48.9 | 33.6 | – | 25.0 | 47.3 | 27.7 | – | 5.0 | 32.4 | 62.7 | – |
| Mother’s highest education level | ||||||||||||
| No education | 19.1 | 49.8 | 31.2 | 0.000 | 40.8 | 46.3 | 12.8 | 0.000 | 7.8 | 39.6 | 52.6 | 0.000 |
| Primary | 10.3 | 47.8 | 41.9 | – | 21.2 | 50.2 | 28.6 | – | 3.4 | 26.7 | 69.9 | – |
| Secondary | 9.8 | 39.9 | 50.3 | – | 11.2 | 48.3 | 40.4 | – | 1.7 | 25.5 | 72.8 | – |
| Higher | 5.4 | 47.6 | 47.0 | – | 3.4 | 43.2 | 53.4 | – | 2.5 | 25.3 | 72.1 | – |
| Total | 17.5 | 48.9 | 33.6 | – | 25.0 | 47.3 | 27.7 | – | 5.0 | 32.4 | 62.7 | – |
| Father’s highest education level | ||||||||||||
| No education | 19.5 | 51.4 | 29.1 | 0.000 | 42.6 | 45.4 | 12 | 0.000 | 9.7 | 37.3 | 53.0 | 0.000 |
| Primary | 14.6 | 50.5 | 34.9 | – | 23.8 | 49.4 | 26.8 | – | 4.7 | 36.5 | 58.8 | – |
| Secondary | 14.5 | 43.1 | 42.4 | – | 15.0 | 49.2 | 35.8 | – | 2.5 | 27.4 | 70.1 | – |
| Higher | 13.6 | 43.8 | 42.6 | – | 9.9 | 45.3 | 44.9 | – | 2.8 | 30.1 | 67.1 | – |
| Total | 17.4 | 49.1 | 33.6 | – | 25.1 | 47.3 | 27.7 | – | 5.0 | 32.3 | 62.6 | – |
| Household wealth quintile | ||||||||||||
| Poorest | 21.8 | 51.9 | 26.4 | 0.000 | 40.5 | 46.4 | 13.2 | 0.000 | 9.3 | 42.5 | 48.3 | 0.000 |
| Poorer | 20.0 | 51.1 | 28.9 | – | 33.1 | 50.2 | 16.7 | – | 6.8 | 33.3 | 59.9 | – |
| Middle | 19.2 | 50.8 | 30.1 | – | 24.8 | 48.6 | 26.5 | – | 3.8 | 31.7 | 64.5 | – |
| Richer | 14.4 | 46.7 | 38.9 | – | 15.3 | 48.1 | 36.6 | – | 2.8 | 26.2 | 71.0 | – |
| Richest | 11.5 | 43.5 | 44.9 | – | 6.4 | 42.0 | 51.7 | – | 1.8 | 27.0 | 71.2 | – |
| Total | 17.5 | 48.9 | 33.6 | – | 25.0 | 47.3 | 27.7 | – | 5.0 | 32.4 | 62.7 | – |
| Mother’s occupational status | ||||||||||||
| Not working | 17.4 | 48.2 | 34.4 | 0.014 | 36.3 | 43.9 | 19.8 | – | 4.8 | 32.3 | 62.9 | 0.547 |
| Working | 18.1 | 53.4 | 28.5 | – | 20.2 | 48.7 | 31.1 | – | 6.2 | 32.8 | 61.1 | – |
| Total | 17.5 | 48.9 | 33.6 | – | 25.0 | 47.3 | 27.7 | – | 5.0 | 32.4 | 62.7 | – |
| Mother’s exposure to media | ||||||||||||
| No exposure | 21.9 | 50.9 | 27.2 | 0.000 | 38.0 | 46.5 | 15.5 | 0.000 | 7.7 | 38.5 | 53.9 | 0.000 |
| Exposure | 15.2 | 47.9 | 36.9 | – | 17.2 | 47.7 | 35.1 | – | 3.3 | 28.7 | 68.0 | – |
| Total | 17.5 | 48.9 | 33.6 | – | 25.0 | 47.3 | 27.7 | – | 5.0 | 32.4 | 62.7 | – |
CV = complete vaccination; IV = incomplete vaccination; No = no vaccination.
P value is based on Design-based F.
Table 3 provides the results of the multinomial logistic regression model for the three countries. In this model, CV is used as a reference category. In all three countries, the risk of receiving NV is significantly less among the children whose mothers are empowered than the children whose mothers are not empowered. Similarly, maternal empowerment significantly reduces the risk of IV in Afghanistan (odds ratio [OR] 0.72; 95% CI: 0.62–0.85; P < 0.001), but this association is insignificant for Pakistan and Nigeria.
Table 3.
Multinomial logistic model
| Pakistan | Nigeria | Afghanistan | ||||
|---|---|---|---|---|---|---|
| NV | IV | NV | IV | NV | IV | |
| RRR | RRR | RRR | RRR | RRR | RRR | |
| Maternal empowerment | ||||||
| Not empowered | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Empowered | 0.704* | 0.987 | 0.580*** | 0.906 | 0.582*** | 0.728*** |
| [0.503, 0.986] | [0.810, 1.203] | [0.506, 0.665] | [0.805, 1.019] | [0.443, 0.765] | [0.622, 0.852] | |
| Mother’s occupational status | ||||||
| Not working | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Working | 0.952 | 0.862 | 0.627*** | 0.915 | 1.378* | 1.386*** |
| [0.568, 1.596] | [0.645, 1.152] | [0.542, 0.726] | [0.807, 1.037] | [1.038, 1.830] | [1.152, 1.669] | |
| Mother’s current age | ||||||
| 15–24 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| 25–34 | 0.704* | 0.824* | 0.774*** | 0.808*** | 0.906 | 0.803** |
| [0.502, 0.986] | [0.684, 0.993] | [0.672, 0.892] | [0.724, 0.901] | [0.760, 1.079] | [0.695, 0.929] | |
| 35+ | 0.769 | 0.820 | 0.801** | 0.832** | 0.699*** | 0.779** |
| [0.456, 1.297] | [0.625, 1.077] | [0.678, 0.947] | [0.724, 0.956] | [0.579, 0.843] | [0.665, 0.913] | |
| Rural/urban residence | ||||||
| Rural | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Urban | 1.749* | 1.112 | 0.853 | 0.783*** | 1.116 | 1.139 |
| [1.030, 2.972] | [0.855, 1.447] | [0.681, 1.068] | [0.685, 0.894] | [0.751, 1.660] | [0.929, 1.397] | |
| Mother’s highest education level | ||||||
| No education | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Primary | 0.545 | 0.595*** | 0.496*** | 0.696*** | 0.510*** | 0.812 |
| [0.295, 1.007] | [0.451, 0.785] | [0.412, 0.597] | [0.594, 0.815] | [0.378, 0.687] | [0.652, 1.012] | |
| Secondary | 0.393* | 0.585*** | 0.275*** | 0.562*** | 0.451*** | 0.624** |
| [0.182, 0.846] | [0.438, 0.781] | [0.226, 0.334] | [0.479, 0.659] | [0.291, 0.699] | [0.450, 0.865] | |
| Higher | 0.738 | 0.562** | 0.123*** | 0.524*** | 0.315** | 0.863 |
| [0.305, 1.787] | [0.397, 0.797] | [0.0817, 0.185] | [0.414, 0.664] | [0.141, 0.705] | [0.464, 1.607] | |
| Father’s highest education level | ||||||
| No education | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Primary | 0.609 | 1.064 | 0.554*** | 0.744** | 0.800 | 0.932 |
| [0.368, 1.008] | [0.861, 1.316] | [0.446, 0.689] | [0.613, 0.901] | [0.630, 1.016] | [0.813, 1.068] | |
| Secondary | 0.368*** | 0.797 | 0.512*** | 0.776** | 0.716** | 0.698*** |
| [0.225, 0.602] | [0.634, 1.001] | [0.419, 0.626] | [0.648, 0.928] | [0.570, 0.899] | [0.610, 0.798] | |
| Higher | 0.552 | 1.052 | 0.462*** | 0.733** | 0.908 | 0.796 |
| [0.301, 1.011] | [0.812, 1.364] | [0.347, 0.616] | [0.583, 0.921] | [0.642, 1.285] | [0.615, 1.029] | |
| Household wealth quintile | ||||||
| Poorest | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Poorer | 0.773 | 0.752 | 0.969 | 0.995 | 0.807 | 0.878 |
| [0.446, 1.339] | [0.549, 1.029] | [0.774, 1.213] | [0.822, 1.206] | [0.608, 1.072] | [0.687, 1.123] | |
| Middle | 0.545 | 0.772 | 0.863 | 0.835 | 0.732 | 0.841 |
| [0.292, 1.017] | [0.567, 1.052] | [0.660, 1.127] | [0.677, 1.031] | [0.503, 1.067] | [0.662, 1.069] | |
| Richer | 0.424* | 0.657* | 0.708* | 0.775* | 0.488*** | 0.638*** |
| [0.192, 0.938] | [0.453, 0.953] | [0.523, 0.960] | [0.617, 0.973] | [0.372, 0.641] | [0.509, 0.800] | |
| Richest | 0.304** | 0.747 | 0.394*** | 0.581*** | 0.419*** | 0.565*** |
| [0.124, 0.747] | [0.508, 1.100] | [0.276, 0.563] | [0.456, 0.741] | [0.267, 0.658] | [0.414, 0.771] | |
| Mother’s exposure to media | ||||||
| No exposure | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Exposure | 0.675 | 0.813* | 0.673*** | 0.863* | 0.708*** | 0.843* |
| [0.395, 1.154] | [0.667, 0.993] | [0.572, 0.793] | [0.755, 0.986] | [0.594, 0.842] | [0.734, 0.968] | |
| Observations | 5,687 | – | 17,172 | – | 28,562 | – |
| F | 5.323 | – | 36.89 | – | 7.743 | – |
| p | 8.74e-17 | – | 3.38e-157 | – | 3.24e-30 | – |
IV = incomplete vaccination; Complete vaccination is the reference group in the multinomial logistic model; NV = no vaccination; RRR = relative risk ratio. Exponentiated coefficients; 95% CI in brackets.
P < 0.05; ** P < 0.01; *** P < 0.001.
Mother’s job is associated with a decrease in the risk of NV in Nigeria (OR 0.627; 95% CI: 0.54–0.72; P < 0.001) but counterintuitively, increases that risk in Afghanistan (OR 1.37; 95% CI: 1.03–1.83; P < 0.05). Children of working women are at a higher risk of receiving IV in Afghanistan (OR 1.38; 95% CI: 1.15–1.66; P < 0.001).
The risk of NV or IV generally decreases as the mother’s age increases. Mother’s age above 34 years is associated with a reduced risk of NV in Nigeria (OR 0.801; 95% CI: 0.67–0.94; P < 0.001) and Afghanistan (OR 0.69; 95% CI: 0.57–0.84; P < 0.001). When the mother is 34 years old or above, maternal age significantly reduces the risk of IV in Nigeria and Afghanistan.
Mother’s education is a significant correlate of vaccination, in line with the ecological theoretical model. Higher education of the mother significantly reduces the risk of NV in Nigeria (OR 0.12; 95% CI: 0.08–0.18; P < 0.001) and Afghanistan (OR 0.31; 95% CI: 0.14–0.70; P < 0.01). A mother’s higher education also significantly reduces the risk of IV in Pakistan and Nigeria.
The father’s education is generally a significant protective factor against NV in all three countries. In Nigeria, a father’s higher education significantly reduces the risk of NV and IV. However, in Pakistan and Nigeria, higher education insignificantly reduces the risk of NV and IV.
An increase in the household’s wealth status almost monotonically reduces the risk of NV and IV in all three countries. For example, a household in the richest wealth quantile is 70%, 61%, and 59% less likely to have an unvaccinated child in Pakistan, Nigeria, and Afghanistan, respectively.
Exposure to media plays a crucial role in the complete immunization of a child. Overall, the mother’s exposure to media reduces the risk of NV and IV in all three countries. The mothers who have media exposure significantly reduce the risk of NV in Nigeria and Afghanistan. Whereas mother’s exposure to media also significantly reduces the risk of IV in all three countries.
DISCUSSION
Maternal empowerment is associated with a significantly reduced risk of NV in all three countries and a significantly reduced risk of IV in Nigeria and Afghanistan. Although the mother’s paid job is a protective factor against NV in Nigeria, the paid job of women increases the risk of NV and IV in Afghanistan. A mother’s age exceeding 34 years reduces the risk of NV and IV in Nigeria and Afghanistan. Higher levels of mothers’ and fathers’ education are associated with a significantly reduced risk of NV and IV.
Higher household wealth levels are associated with a reduced risk of NV and IV in all three countries. Geographic location shows a wide diversity concerning the odds of IV. Urban children were at 74.9% higher risk of no polio vaccination in Pakistan but living in urban areas is a protective factor against IV in Nigeria.
Our findings are consistent with a few previous studies that found maternal empowerment associated with a higher likelihood of CV and a significantly smaller likelihood of NV or IV.20,25,35 A mother’s job is also a protection against IV or NV. A mother’s job provides a hedge against financial obstacles associated with IV or NV.36–38 The nature of the job is also a significant predictor of a child’s vaccination status.
Children whose mothers work in the agriculture sector or are engaged in a blue-collar job are more likely to remain unvaccinated than women doing white-collar jobs.39 Similarly, mothers engaged in government jobs are more likely to get their children fully vaccinated than nonworking mothers.40
A mother’s age exceeding 34 years is associated with increased odds for CV. One possible reason is that older women have greater experience of childcare.13 But some studies found that younger women were more likely to have their children vaccinated because they have fewer children and are more self-motivated.13,36,41
The level of education is positively associated with CV. Educated parents have greater knowledge about the best practices of childcare.42–46 A father’s education is important because he is a major decision maker in the house.43,45 The specific knowledge of immunization provided by health workers during their antenatal care (ANC) visits could be translated into CV only by more educated mothers.47,48
Moreover, higher household wealth levels are associated with a reduced risk of NV and IV in all three countries. Mothers who belong to higher wealth quantiles have greater financial autonomy and leverage over their children’s health to provide better healthcare services to their children.48,49
Geographical location shows a wide diversity concerning the odds of IV. Urban children were at 67.5% higher risk of no polio vaccination in Pakistan, whereas living in urban areas was a protective factor against IV in Nigeria. Children in urban areas are expected to have higher chances of CV because they have easier access to health facilities.49,50 In rural areas, mothers of nonvaccinated children were often unaware of the needs of immunization and sources of immunization.51,52 In Pakistan, extremist elements have been engaged in propaganda against polio drives. Though polio workers are mostly attacked during SIAs in Pakistan and Afghanistan,53,54 such attacks create a general atmosphere of fear and mistrust, and may have indirect effects on the vaccination drives undertaken through RI systems. As the urban population in Pakistan has greater exposure to the media, including social media, refusal rates against vaccination are perhaps higher in urban areas.55
CONCLUSION
In polio-endemic countries, completing the basic polio immunization rate remains a big challenge. This study highlights the maternal and demographic characteristics that help to overcome this challenge. Multinomial logistic regression analysis was applied using recent DHS data of Afghanistan, Pakistan, and Nigeria. Nigeria has been declared polio-free recently in June 2020,2 but it provides an interesting case to generate important lessons for Pakistan and Afghanistan.
Since a child’s polio vaccination is strongly dependent on a mother’s working status and empowerment, the governments of the respective countries need to focus on empowering mothers, which would help increase polio vaccination uptake. Additionally, because of the recent security threats to polio workers, polio immunization programs remain unsuccessful. Though polio workers are mostly attacked during SIAs in Pakistan and Afghanistan53,54 (DHS does not collect information about SIAs), such attacks may indirectly and negatively affect the government’s initiative through RI systems. Consequently, there is a reason to believe that women’s empowerment should complement other protective factors such as a safe working environment for health workers. This study, therefore, recommends additional efforts to provide a risk-free working environment to the health workers.
ACKNOWLEDGMENTS
The American Society of Tropical Medicine and Hygiene (ASTMH) assisted with publication expenses.
REFERENCES
- 1. Naqvi AA, Naqvi SBS, Zehra F, Verma AK, Usmani S, Badar S, Ahmad R, Ahmad N, 2018. Estimation of the direct cost of poliomyelitis rehabilitation treatment to Pakistani patients: a 53-year retrospective study. Appl Health Econ Health Policy 16: 871–888. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization , 2020. Poliomyelitis (polio). Available at: https://www.who.int/health-topics/poliomyelitis#tab=tab_1. Accessed March 18, 2021.
- 3. CDC , 2020. Polio Disease and Poliovirus. Available at: https://www.cdc.gov/cpr/polioviruscontainment/diseaseandvirus.htm. Accessed March 18, 2021.
- 4. Brearley L, Eggers R, Steinglass R, Vandelaer J, 2013. Applying an equity lens in the decade of vaccines. Vaccine 31: B103–B107. [DOI] [PubMed] [Google Scholar]
- 5. Bryce J, Black RE, Walker N, Bhutta ZA, Lawn JE, Steketee RW, 2005. Can the world afford to save the lives of 6 million children each year? Lancet 365: 2193–2200. [DOI] [PubMed] [Google Scholar]
- 6. Bhutta ZA, 2011. The last mile in global poliomyelitis eradication. Lancet 378: 549–552. [DOI] [PubMed] [Google Scholar]
- 7. Grassly NC, 2013. The final stages of the global eradication of poliomyelitis. Philos Trans R Soc Lond B Biol Sci 368: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sreevatsava M, Burman AL, Wahdan A, Safdar RM, O’Leary A, Amjad R, Salam A, Quershi M, Ishaq R, Khan J, 2020. Routine immunization coverage in Pakistan: a survey of children under 1 year of age in community-based vaccination areas. Vaccine 38: 4399–4404. [DOI] [PubMed] [Google Scholar]
- 9. Martinez M, Shukla H, Nikulin J, Wadood MZ, Hadler S, Mbaeyi C, Tangermann R, Jorba J, Ehrhardt D, 2017. Progress toward poliomyelitis eradication—Afghanistan, January 2016–June 2017. MMWR Morb Mortal Wkly Rep 66: 854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. GPEI , 2020. Vaccine-Derived Polioviruses. Available at: http://polioeradication.org/polio-today/polio-prevention/the-virus/vaccine-derived-polio-viruses/. Accessed March 18, 2021.
- 11. Kalkowska DA, Franka R, Higgins J, Kovacs SD, Forbi JC, Wassilak SG, Pallansch MA, Thompson KM, 2021. Modeling poliovirus transmission in Borno and Yobe, northeast Nigeria. Risk Anal 41: 289–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Andrade GE, Hussain A, 2018. Polio in Pakistan: political, sociological, and epidemiological factors. Cureus 10: e3502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Khan MT, Zaheer S, Shafique K, 2017. Maternal education, empowerment, economic status and child polio vaccination uptake in Pakistan: a population based cross sectional study. BMJ Open 7: e013853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abimbola S, Malik AU, Mansoor GF, 2013. The final push for polio eradication. PLoS Med 10: e1001529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ghinai I, Willott C, Dadari I, Larson HJ, 2013. Listening to the rumours. Glob Public Health 8: 1138–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Warraich HJ, 2009. Religious opposition to polio vaccination. Emerg Infect Dis 15: 978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hussain RS, McGarvey ST, Fruzzetti LM, 2015. Partition and poliomyelitis. PLoS One 10: e0115628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Khan TM, Sahibzada MUK, 2016. Challenges to health workers and their opinions about parents’ refusal of oral polio vaccination in the Khyber Pakhtoon Khawa (KPK) Province, Pakistan. Vaccine 34: 2074–2081. [DOI] [PubMed] [Google Scholar]
- 19. Khan TM, Chiau LM, 2015. Polio vaccination in Pakistan: by force or by volition? Lancet 386: 1733. [DOI] [PubMed] [Google Scholar]
- 20. Onsomu EO, Abuya BA, Okech IN, Moore D, Collins-McNeil J, 2015. Maternal education and immunization status among children in Kenya. Matern Child Health J 19: 1724–1733. [DOI] [PubMed] [Google Scholar]
- 21. Tozzi AE, Ravà L, Stat D, Pandolfi E, Marino MG, Ugazio AG, 2009. Attitudes towards HPV immunization of Italian mothers of adolescent girls and potential role of health professionals in the immunization program. Vaccine 27: 2625–2629. [DOI] [PubMed] [Google Scholar]
- 22. White GE, Thomson A, 1995. ‘As every good mother should’. Childhood immunization in New Zealand: a qualitative study. Health Soc Care Community 3: 73–82. [Google Scholar]
- 23. Shui I, Kennedy A, Wooten K, Schwartz B, Gust D, 2005. Factors influencing African-American mothers’ concerns about immunization safety: a summary of focus group findings. J Natl Med Assoc 97: 657. [PMC free article] [PubMed] [Google Scholar]
- 24. Thorpe S, VanderEnde K, Peters C, Bardin L, Yount KM, 2016. The influence of women’s empowerment on child immunization coverage in low, lower-middle, and upper-middle income countries: a systematic review of the literature. Matern Child Health J 20: 172–186. [DOI] [PubMed] [Google Scholar]
- 25. Mathew JL, 2012. Inequity in childhood immunization in India: a systematic review. Indian Pediatr 49: 203–223. [DOI] [PubMed] [Google Scholar]
- 26. Khan MU, Ahmad A, Salman S, Ayub M, Aqeel T, Haq N-U, Saleem F, Khan MU, 2017. Muslim scholars’ knowledge, attitudes and perceived barriers towards polio immunization in Pakistan. J Relig Health 56: 635–648. [DOI] [PubMed] [Google Scholar]
- 27. Kennedy J, 2017. How drone strikes and a fake vaccination program have inhibited polio eradication in Pakistan. Int J Health Serv 47: 807–825. [DOI] [PubMed] [Google Scholar]
- 28. Tauil Md C, Sato APS, Waldman EA, 2016. Factors associated with incomplete or delayed vaccination across countries. Vaccine 34: 2635–2643. [DOI] [PubMed] [Google Scholar]
- 29. Richard L, Gauvin L, Raine K, 2011. Ecological models revisited: their uses and evolution in health promotion over two decades. Annu Rev Public Health 32: 307–326. [DOI] [PubMed] [Google Scholar]
- 30. Sallis JF, Owen N, Fisher E, 2015. Ecological models of health behavior. Health Behav 5: 43–64. [Google Scholar]
- 31. Bronfenbrenner U, 1979. The Ecology of Human Development. Cambridge, MA: Harvard University Press. [Google Scholar]
- 32. Reifsnider E, Gallagher M, Forgione B, 2005. Using ecological models in research on health disparities. J Prof Nurs 21: 216–222. [DOI] [PubMed] [Google Scholar]
- 33. Abbas F, Amir-Ud-Din R, 2019. Correlates of C-section in Punjab: a disaggregated analysis at the level of rural-urban residential status and place of delivery. Women Health 59: 997–1014. [DOI] [PubMed] [Google Scholar]
- 34. ICF , 2018. Demographic and Health Surveys Standard Recode Manual for DHS7. Rockville, MD: DHS Program/ICF. [Google Scholar]
- 35. Allendorf K, 2007. Do women’s land rights promote empowerment and child health in Nepal? World Dev 35: 1975–1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Awasthi A, Pandey C, Singh U, Kumar S, Singh T, 2015. Maternal determinants of immunization status of children aged 12–23 months in urban slums of Varanasi, India. Clin Epidemiol Glob Health 3: 110–116. [Google Scholar]
- 37. Mindlin M, Jenkins R, Law C, 2009. Maternal employment and indicators of child health: a systematic review in pre-school children in OECD countries. J Epidemiol Community Health 63: 340–350. [DOI] [PubMed] [Google Scholar]
- 38. Bates AS, Wolinsky FD, 1998. Personal, financial, and structural barriers to immunization in socioeconomically disadvantaged urban children. Pediatrics 101: 591–596. [DOI] [PubMed] [Google Scholar]
- 39. Bbaale E, 2015. Immunization status and child survival in Uganda. African Journal of Economic Review 3: 1–20. [Google Scholar]
- 40. Tagbo BN, Eke CB, Omotowo BI, Onwuasigwe CN, Onyeka EB, Mildred UO, 2014. Vaccination coverage and its determinants in children aged 11–23 months in an urban district of Nigeria. World J Vaccines 4: 175. [Google Scholar]
- 41. Fatiregun AA, Okoro AO, 2012. Maternal determinants of complete child immunization among children aged 12–23 months in a southern district of Nigeria. Vaccine 30: 730–736. [DOI] [PubMed] [Google Scholar]
- 42. Balogun SA, Yusuff HA, Yusuf KQ, Al-Shenqiti AM, Balogun MT, Tettey P, 2017. Maternal education and child immunization: the mediating roles of maternal literacy and socioeconomic status. Pan Afr Med J 26: 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Brugha R, Kevany J, Swan A, 1996. An investigation of the role of fathers in immunization uptake. Int J Epidemiol 25: 840–845. [DOI] [PubMed] [Google Scholar]
- 44. Xeuatvongsa A, Hachiya M, Miyano S, Mizoue T, Kitamura T, 2017. Determination of factors affecting the vaccination status of children aged 12–35 months in Lao People’s Democratic Republic. Heliyon 3: e00265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Johri M, Subramanian S, Sylvestre M-P, Dudeja S, Chandra D, Koné GK, Sharma JK, Pahwa S, 2015. Association between maternal health literacy and child vaccination in India: a cross-sectional study. J Epidemiol Community Health 69: 849–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Phimmasane M, Douangmala S, Koffi P, Reinharz D, Buisson Y, 2010. Factors affecting compliance with measles vaccination in Lao PDR. Vaccine 28: 6723–6729. [DOI] [PubMed] [Google Scholar]
- 47. Streatfield K, Singarimbun M, Diamond I, 1990. Maternal education and child immunization. Demography 27: 447–455. [PubMed] [Google Scholar]
- 48. Oyefara JL, 2014. Mothers’ characteristics and immunization status of under-five children in Ojo Local Government Area, Lagos State, Nigeria. SAGE Open 4: 1–10. [Google Scholar]
- 49. Luqman B, Kolawole OT, 2014. Mothers health seeking behaviour and socio-economic differentials: a factor analysis of full childhood immunization in south-western Nigeria. J Public Health Epidemiol 6: 132–147. [Google Scholar]
- 50. Bugvi AS, Rahat R, Zakar R, Zakar MZ, Fischer F, Nasrullah M, Manawar R, 2014. Factors associated with non-utilization of child immunization in Pakistan: evidence from the Demographic and Health Survey 2006–07. BMC Public Health 14: 232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bonu S, Rani M, Baker TD, 2003. The impact of the national polio immunization campaign on levels and equity in immunization coverage: evidence from rural North India. Soc Sci Med 57: 1807–1819. [DOI] [PubMed] [Google Scholar]
- 52. Pande RP, Yazbeck AS, 2002. Beyond National Averages for Immunization in India: Income, Gender and Regional Inequalities. Washington, DC: World Bank, Health, Nutrition and Population. [Google Scholar]
- 53. Ataullahjan A, Ahsan H, Soofi S, Habib MA, Bhutta ZA, 2021. Eradicating polio in Pakistan: a systematic review of programs and policies. Expert Rev Vaccines 1–18. [DOI] [PubMed] [Google Scholar]
- 54. Verma AA, Jimenez MP, Tangermann RH, Subramanian S, Razak F, 2018. Insecurity, polio vaccination rates, and polio incidence in northwest Pakistan. Proc Natl Acad Sci USA 115: 1593–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Qasim M, 2019. Anti-polio Campaign: 10 Times More Refusal Cases Recorded in Federal Capital. The News. Pakistan.