Abstract
Introduction
The U.S. opioid crisis has been exacerbated by COVID-19 and the spread of synthetic opioids (e.g., fentanyl).
Methods
We model the effectiveness of reduced prescribing, drug rescheduling, prescription monitoring programs (PMPs), tamper-resistant drug reformulation, excess opioid disposal, naloxone availability, syringe exchange, pharmacotherapy, and psychosocial treatment. We measure life years, quality-adjusted life years (QALYs), and opioid-related deaths over five and ten years.
Findings
Under the status quo, our model predicts that approximately 547,000 opioid-related deaths will occur from 2020 to 2024 (range 441,000 - 613,000), rising to 1,220,000 (range 996,000 - 1,383,000) by 2029. Expanding naloxone availability by 30% had the largest effect, averting 25% of opioid deaths. Pharmacotherapy, syringe exchange, psychosocial treatment, and PMPs are uniformly beneficial, reducing opioid-related deaths while leading to gains in life years and QALYs. Reduced prescribing and increasing excess opioid disposal programs would reduce total deaths, but would lead to more heroin deaths in the short term. Drug rescheduling would increase total deaths over five years as some opioid users escalate to heroin, but decrease deaths over ten years. Combined interventions would lead to greater increases in life years, QALYs, and deaths averted, although in many cases the results are subadditive.
Interpretation
Expanded health services for individuals with opioid use disorder combined with PMPs and reduced opioid prescribing would moderately lessen the severity of the opioid crisis over the next decade. Tragically, even with improved public policies, significant morbidity and mortality is inevitable.
Research in Context.
Evidence before this study
Previous studies have modelled the effectiveness of various interventions for controlling the U.S. opioid epidemic, but COVID-19 and the spread of synthetic opioids (e.g., fentanyl) makes prior conclusions less reliable.
Added value of this study
This study updates and extends with new data a previously developed model to assess the effectiveness of the following interventions for controlling the U.S. opioid epidemic, singly and in combinations: reduced opioid prescribing, drug rescheduling, prescription monitoring programs, tamper-resistant opioid reformulation, excess opioid disposal, naloxone availability, syringe exchange, pharmacotherapy for opioid use disorder, and psychosocial treatment. The analysis shows that expanding naloxone availability would have the largest impact; other interventions would have smaller but positive impacts.
Implications of all the available evidence
Expanded health services for individuals with opioid use disorder combined with prescription monitoring programs and reduced opioid prescribing would moderately lessen the severity of the opioid crisis over the next decade. Tragically, even with improved public policies, significant morbidity and mortality is inevitable.
Alt-text: Unlabelled box
1. Background
The quadrupling of U.S. opioid prescribing that began in the mid 1990s [1] initiated an epidemic of opioid misuse and use disorder that has since expanded to include illicitly sourced heroin and fentanyl [2]. Opioids were the major driver of the estimated 71,000 drug overdose deaths in 2019, and a cause of significant morbidity and lost productivity [3], [4], [5]. Opioid overdoses increased significantly in 2020, exacerbated by COVID-19 [6], [7], [8], [9], [10], [11]. The Stanford-Lancet Commission on the North American Opioid Crisis was launched in 2020 to formulate evidence-informed recommendations for reducing opioid-related morbidity and mortality in the U.S. and Canada. The Commission is using dynamic models such as we present here to project the impacts of possible policy options.
The policies examined here have all been proposed in influential circles and/or to some extent implemented. All have at least some evidence of impact [12], [13], [14]. For example, policies aimed at returning U.S. opioid prescribing to levels seen in other developed countries [15] began around 2011. Although prescriptions remain well above historical and international norms, they decreased by 12.4% between 2017 and 2018 alone [16]. Expanding access to the overdose reversal drug naloxone, mandating prescriber enrollment and use of prescription monitoring programs, expanding access to pharmacotherapy (e.g., buprenorphine, naltrexone) and psychosocial treatment for individuals with opioid use disorder, and augmenting syringe exchange programs have also attracted significant policy attention and are therefore worthy of evaluation. Though less prominent in the policy conversation, we also evaluate the potential impact of reformulating more opioids with tamper-resistant features, expanding programs for excess opioid disposal, and more tightly scheduling opioid medications.
In this paper we extend and update with new data a previously developed model [17] to assess the effectiveness of interventions for controlling the U.S. opioid epidemic. The original model, on which two of the present authors collaborated, modelled the years 2016 to 2025, and found that policies that reduce the prescription opioid supply may increase heroin use and reduce quality of life in the short term, but in the long term could generate positive health benefits. The analysis also found that expanded health services for people with opioid use disorder reduced mortality in the short and long term, and that a portfolio of interventions had greater life-saving potential than any single policy. The analysis presented here models the years 2020 to 2029, is updated in light of new evidence, and takes into account two critical developments which occurred after our initial model was published: COVID-19, which has been associated with increased overdose deaths and interruptions in treatment for opioid use disorder [6], [7], [8], [9], [10], [11], and the spread of deadly synthetic opioids (e.g., fentanyl) from east of the Mississippi River to the rest of the U.S. [18]. For each policy alone and in combinations, we project life years, quality-adjusted life years (QALYs), and overdose deaths, over a five- and ten-year time horizon.
2. Methods
2.1. Dynamic Model
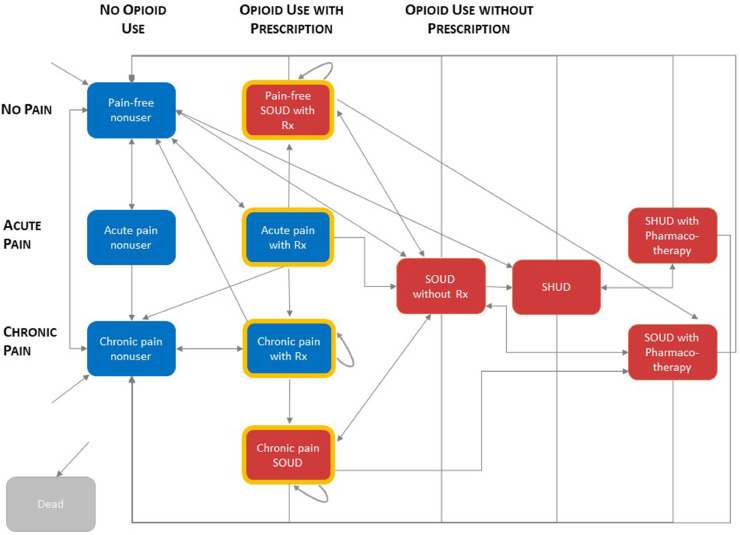
We extend a previously developed dynamic compartmental model of opioid prescribing and opioid use disorder in the U.S. adult population [17]. Figure 1 shows a schematic of the updated model. The model includes three pain states (no pain, acute pain (defined as the first month of pain), and chronic pain (defined as pain lasting longer than one month), three opioid use states (no use, use with a prescription, and use without a prescription), and three use disorder states (no use disorder, severe opioid use disorder (SOUD), and severe heroin use disorder (SHUD)). Additional states reflect pharmacotherapy (e.g., methadone maintenance) for individuals with SOUD and SHUD. We distinguish individuals with SHUD from those with SOUD to reflect the former's greater morbidity and mortality risk, stemming from higher fentanyl exposure and rates of injection use.
Figure 1.
Model schematic. Blue shading indicates no opioid use disorder. Red shading indicates opioid use disorder (either SOUD or SHUD). Yellow border indicates prescription holders. Rx = prescription; SHUD = severe heroin use disorder; SOUD = severe opioid use disorder.
The model is simulated on a monthly basis. In any month, individuals can begin opioid use, either with or without a prescription, and can begin heroin use. The influence of synthetic opioids such as fentanyl is reflected in the mortality rates we assumed. The model assumes that the rate at which pain-free individuals begin opioid use without a prescription is a function of the number of individuals with prescriptions multiplied by the number of individuals without a prescription (similar to a contagion model). Individuals who use opioids can develop opioid use disorder, and individuals with SOUD and SHUD can enter treatment. Individuals with prescriptions may or may not receive a prescription renewal at the end of a given month. At the end of a month with acute pain, an individual may be pain free, or may progress to chronic pain, with or without a prescription. When an individual with acute pain transitions to chronic pain and receives a new prescription, we refer to that as a prescription for transitioning pain. The model assumes that some opioid use is through diverted pills, and that the supply of diverted pills is linearly related to the number of prescriptions in the previous year. Deaths can occur in all health states.
2.2. Model Instantiation
We instantiated the model for the U.S. adult population age 12 and older. Table 1 shows parameter values; sources are provided in Table S1. Compared to the prior analysis [17], mortality rates are higher, reflecting two distinct phenomena. First, the increase in fentanyl and other synthetic opioids has made opioid use more dangerous [8] and, second, COVID-19 has caused widespread emotional strain while making it harder for individuals to enter and to stay in treatment [6,10,11]. Additionally, unlike the prior analysis, the current model allows for development of SHUD in some individuals who do not have prior SOUD. This reflects the reality that even though heroin markets expanded to provide opioids to people with SOUD, once in place they increased the opportunity for individuals to begin their opioid use with heroin [19]. We assumed that, with no incremental intervention, treatment availability would return to pre-COVID levels by June 2022. Because of significant uncertainty in the data regarding opioid use disorder and treatment, we created ten base case parameter sets (Table 2). Each base case was created by changing a single parameter that had significant uncertainty (e.g., mortality from heroin use) and then adjusting other relevant model parameters so that the model projected a plausible future trajectory for the opioid epidemic (Supplemental Figure S1).
Table 1.
Parameter values1
| Parameter | Value2 |
|---|---|
| Demographic data | |
| Total population size, age 12+ | 276,077,200 |
| Chronic pain prevalence (moderate to severe) | 8.6% |
| Acute pain prevalence (moderate to severe) | 2.5% |
| Severe opioid use disorder prevalence | 0.49% |
| Severe heroin use disorder prevalence | 0.36% |
| Rate of maturation into the population, people/month | 234,167 |
| Pain natural history | |
| Acute pain incidence for pain-free nonusers, %/month | 2.5% |
| Chronic pain incidence for pain-free nonusers, %/month | 0.30% |
| Chronic pain subsidence, %/month | 8% |
| Probability that acute pain persists without opioid prescription | 15.0% |
| Probability that acute pain persists with opioid prescription | 14.7% |
| Percent of 12+ population with chronic pain of any severity | 43% |
| Percent of chronic pain population with moderate to severe pain | 20% |
| Percent of 12+ population getting surgery or ED trauma visit | 4% |
| Percent of surgeries resulting in moderate to severe pain | 61% |
| Percent of prescription-holding SOUD population who suffer from chronic pain | 65% |
| Percent of SOUD without Rx and SHUD populations who have with chronic pain | 45% |
| Risk ratio for chronic pain developing during acute pain treatment with vs. without opioids | 0.98 |
| Prescribing behavior | |
| Percent of acute pain patients prescribed opioids | 38% |
| Probability of continued use of opioids for pain that persists from acute | 50% |
| Percent of total population prescribed opioids for chronic pain | 4% |
| Probability of chronic pain sufferer being prescribed opioids, %/month | 7.6% |
| Probability of SOUD individual being prescribed opioids, %/month | 7.6% |
| Probability of opioid prescription renewal for chronic pain patients without SOUD, %/month | 97% |
| Probability of opioid prescription renewal for individuals with SOUD, %/month | 94% |
| Estimated annual decline in opioid prescriptions from 2018-2019 | 8.9% |
| Probability of individuals with iatrogenic SOUD continuing use of opioids after acute pain treatment | 50% |
| Probability that chronic pain opioid user without SOUD wants to get prescription renewed, %/month | 99% |
| Probability that an opioid user is able to get renewal for chronic pain prescription if they choose, %/month | 98% |
| Use Disorder | |
| Probability of developing SHUD for non-opioid users with no pain | 0.002% |
| Probability of iatrogenic SOUD with opioid prescription, %/month | 0.20% |
| Probability of a non-medical user developing SOUD from diverted pills, %/month | 7% |
| Baseline rate of escalation to SHUD from SOUD without Rx, %/month | 4% |
| Probability of escalation to SHUD if there are not diverted pills for SOUD without Rx | 75%-60% |
| SOUD prevalence among population with opioid prescription for chronic pain | 7% |
| Percent of SHUD population who escalated from SOUD | 80% |
| Number of pain-free nonusers a prescription holder diverts opioids to, #/month | 0.01 |
| Proportionality factory relating SOUD without Rx population able to be sustained by diverted pills to lagged number of prescription holders | 0.02 |
| Treatment and desistance | |
| Percent of SOUD population enrolled in pharmacotherapy | 13%-26% |
| Percent of SHUD population enrolled in pharmacotherapy | 16%-32% |
| Rate of SOUD with Rx enrollment in pharmacotherapy, %/month | 0.5%-1% |
| Rate of SOUD without Rx enrollment in pharmacotherapy, %/month | 2%-4% |
| Rate of SHUD enrollment in pharmacotherapy, %/month | 2%-4% |
| Rate of drop out from pharmacotherapy for SOUD, %/month | 5% |
| Rate of drop out from pharmacotherapy for SHUD, %/month | 14% |
| Rate of desistance from SOUD in pharmacotherapy, %/month | 1.0% |
| Baseline rate of desistance from SOUD without pharmacotherapy, %/month | 0.5% |
| Rate of desistance from SHUD in pharmacotherapy, %/month | 0.5% |
| Rate of desistance from SHUD not in pharmacotherapy, %/month | 0.25% |
| Probability of enrollment in pharmacotherapy if there are not diverted pills for SOUD without Rx | 15%-30% |
| Probability of desistance if there are not diverted pills for SOUD without Rx | 10% |
| Mortality | |
| Mortality rate for the general population, %/month | 0.07% |
| Mortality rate for SOUD not in pharmacotherapy %/month | 0.23% |
| Mortality rate for SHUD not in pharmacotherapy %/month | 0.54% |
| Mortality rate for SOUD in pharmacotherapy %/month | 0.13% |
| Mortality rate for SHUD in pharmacotherapy %/month | 0.30% |
| Overdose mortality for person with SHUD, not in pharmacotherapy, %/month | 0.43% |
| Overdose mortality for person with SOUD, not in pharmacotherapy, %/month | 0.15% |
| Infection-related mortality for person with SHUD, not in pharmacotherapy, %/month | 0.03% |
| 1-month relative risk of use disorder-related mortality in vs. out of pharmacotherapy for person with severe use disorder | 0.50 |
| Utility values | |
| Pain-free nonuser | 1 |
| Chronic pain nonuser | 0.85 |
| Acute pain nonuser | 0.88 |
| Acute pain with Rx | 0.94 |
| Chronic pain with Rx | 0.85 |
| SOUD not in pharmacotherapy | 0.83 |
| SOUD in pharmacotherapy | 0.92 |
| SHUD not in pharmacotherapy | 0.80 |
| SHUD in pharmacotherapy | 0.90 |
| Dead | 0 |
Abbreviations: Rx = prescription; SHUD = severe heroin use disorder; SOUD = severe opioid use disorder
Sources for all parameter values are provided in the Supplement.
Where a range is shown for a value, the parameter takes on the first value from January 2020 to December 2020, then the value changes linearly from the first value to the second value over the time period January 2021 to June 2022, and then the parameter has the second value over the remainder of the modeled time horizon.
Table 2.
Base cases
| Base Case | Brief Description | Details |
|---|---|---|
| 1 | Reference case | Values as described in Table 1 |
| 2 | Decreased chance of heroin death | 25% less likely for individual with SHUD to have overdose or infection death |
| 3 | Increased chance of prescription opioid death | 25% more likely for individual with SOUD to have overdose death |
| 4 | Reduced probability of turning to heroin if there are not enough pills to divert | 50% lower chance of individual with SOUD without access to prescription turning to heroin; increased chance of enrolling in pharmacotherapy |
| 5 | Reduced pharmacotherapy effectiveness | No mortality benefit from pharmacotherapy and chance of recovery in pharmacotherapy is reduced by half |
| 6 | Increased chance of individuals with SOUD having a prescription (at start of time horizon) | 25% more individuals with SOUD have a prescription (at start of time horizon) |
| 7 | Decreased chance of iatrogenic SOUD | Likelihood of iatrogenic SOUD is 35% lower |
| 8 | Increased chance of starting heroin from no pain non-use-disorder state | 50% more likely to start heroin from no pain non-use-disorder state |
| 9 | Decreased chance of escalating from SOUD to SHUD regardless of pill supply | 75% less likely to escalate to heroin usage regardless of pill supply |
| 10 | Increased likelihood of diverting opioid prescription to pain-free nonuser | 2x as likely for a prescription holder to divert pills to a pain-free nonuser |
Abbreviations: SHUD = severe heroin use disorder; SOUD = severe opioid use disorder
2.3. Interventions
We considered the following interventions (Table 3): reduced opioid prescribing for acute pain, transitioning pain (pain that persists at the end of the first month of acute pain), and chronic pain (three separate interventions); drug rescheduling; prescription monitoring programs (PMPs); drug reformulation; excess opioid disposal; naloxone availability; syringe exchange; pharmacotherapy for opioid use disorder; and psychosocial treatment for opioid use disorder.
Table 3.
Interventions considered
| Intervention | Assumed Magnitude |
|---|---|
| Reduced Prescribing for Acute Pain | 10% reduction in incidence of prescribing opioids for acute pain |
| Reduced Prescribing for Transitioning Pain | 10% reduction in incidence of prescribing opioids for acute pain that transitions to chronic |
| Reduced Prescribing for Chronic Pain | 10% reduction in incidence of prescribing opioids for chronic pain |
| Drug Rescheduling | 10% reduction in chance of getting prescription renewed |
| Prescription Monitoring Program (PMP) | 15% reduction in incidence of prescribing opioids for acute pain |
| 5% reduction in incidence of prescribing opioids for transitioning pain | |
| 5% reduction in incidence of prescribing opioids for chronic pain | |
| Drug Reformulation | 2.25% reduction in iatrogenic use disorder |
| 2.25% reduction in chance of use disorder via diversion for pain-free non-users | |
| 2.25% reduction in pill-seeking for individuals with SOUD without Rx | |
| Excess Opioid Disposal - Policy 1 | 10% reduction in diversion to pain-free non-users |
| 10% reduction in number of individuals with SOUD without Rx able to be sustained by non-SOUD Rx holders | |
| Excess Opioid Disposal - Policy 2 | 15% reduction in diversion to pain-free non-users |
| 15% reduction in number of individuals with SOUD without Rx able to be sustained by non-SOUD Rx holders | |
| Naloxone Availability - Policy 1 | 5% reduction in overdose mortality |
| Naloxone Availability - Policy 2 | 15% reduction in overdose mortality |
| Naloxone Availability - Policy 3 | 30% reduction in overdose mortality |
| Pharmacotherapy | 25% increased likelihood of entering pharmacotherapy |
| Psychosocial Treatment | 10% increased likelihood of desistance |
| Syringe Exchange | 10% reduction in infection mortality |
Abbreviations: Rx = prescription; SOUD = severe opioid use disorder
Opioid prescribing in the U.S. decreased by 26.0% from 2015 to 2018 [20]. We assumed that prescribing reduction policies would further reduce prescriptions for each type of pain by 10%, which is feasible given that U.S. per capita prescribing is still more than double that of a generation ago.
Drug rescheduling involves moving opioids to more restrictive schedules, as for example was done when hydrocodone combination analgesics were moved from Schedule III to Schedule II [21]. We assumed that further opioid drug rescheduling would lead to a 10% reduction in prescription renewals [17].
PMPs allow prescribers and pharmacists to see whether a patient has multiple prescriptions from other providers, reducing the likelihood of dangerous combinations (e.g., opioids and benzodiazepines) and increasing the chance of detecting “doctor shopping” [22]. Since our original model was published, many states began mandating that prescribers enroll in and use PMPs (e.g., when writing a new opioid prescription), which we assumed would decrease prescriptions for acute, transitioning, and chronic pain by varying amounts, with an average decrease of approximately 8% [23].
Drug reformulation is intended to reduce misuse of opioid medication (e.g., by making pills more difficult to crush for inhalation or injection). We estimated that 5% of current prescriptions have tamper-resistant formulation properties [24] and that such formulations lead to a 45% reduction in misuse [25]. We assumed that an additional 5% of prescriptions could have tamper-resistant formulations. Combined with an estimated 45% reduction in misuse, this leads to 2.25% reduction in iatrogenic use disorder as well as in the chance of developing SOUD via diversion for pain-free non-users and the rate of pill seeking by individuals with SOUD and no prescription.
Excess opioid disposal initiatives comprise “prescription take back days” and secure dropoff sites at pharmacies and clinics. We considered two potential levels of impact, either a 10% or 15% reduction in the supply of pills available for diversion, based on a study of patients who received opioid prescriptions after surgery and education about opioid disposal [26].
The opioid antagonist naloxone will typically reverse the acute effects of opioids (e.g., stopped respiration). We considered three different levels of naloxone availability, leading to a 5%, 15%, or 30% reduction in overdose mortality, based on two nationwide studies [27,28].
Pharmacotherapy involves medications such as methadone, buprenorphine, and naltrexone [29]. We estimated that 13% of individuals with SOUD and 16% of individuals with SHUD currently receive pharmacotherapy, with these numbers increasing to 26% and 32%, respectively, by June 2022 [16,30,31]. We assumed that pharmacotherapy could be scaled up so that individuals with SOUD and SHUD have a 25% increased likelihood of entering pharmacotherapy.
Psychosocial treatment comprises talk therapies (e.g., cognitive-behavioral therapy) and related services (e.g., job counselling). We assumed that expanded access to psychosocial treatment would increase the likelihood of desistance by 10%.
Syringe exchange programs reduce the chance of transmitting infections such as HIV and hepatitis C via shared injection equipment. We assumed that syringe exchange programs could be scaled up to a level that would reduce infection-related mortality among people who inject drugs by 10%.
2.4. Outcomes
For each intervention or intervention combination we assessed opioid-related deaths, life years, and QALYs for all ten base cases, discounted to the present at 3% [32]. We measured all life years and QALYs for all individuals alive in the model during the modeled time horizon as well as future lifetime life years and QALYs for all individuals alive in the model at the end of the time horizon. We report the mean and range for all outcomes over the ten base cases.
2.5. Sensitivity Analysis
All analyses were performed over the ten base cases, which themselves constitute a form of sensitivity analysis. We performed additional one-way sensitivity analyses on heroin overdose mortality, opioid pill overdose mortality, rate of escalation to heroin, level of opioid pill diversion to non-users, quality multipliers for chronic pain with opioid prescription, and probability that individuals with SOUD start pharmacotherapy.
2.6. Role of the Funding Source
The funders had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; nor in the decision to submit the paper for publication.
3. Results
With no additional intervention, our model predicts that approximately 547,000 opioid-related deaths will occur from 2020 to 2024 (range 441,000 - 613,000), rising to 1,220,000 (range 996,000 - 1,383,000) by 2029 (Table S2). These totals reflect a projected baseline increase in the number of individuals with SHUD and the increased mortality associated with illicit opioid use due to fentanyl and other synthetic opioids (Figures S1).
Our analysis assumes that the impact of COVID-19 on treatment availability ends in June 2022. We estimated the overall impact of COVID-19 on deaths by comparing total opioid-related deaths from 2020 until the end of 2022 with and without our assumption about COVID-19 limiting treatment availability. From this analysis, we estimate that COVID-19 will lead to approximately 15,400 more opioid-related deaths (5.2%) than would have occurred otherwise.
3.1. Base Case Analysis
3.1.1. Single Interventions
Table 4 and Table S3 show the five- and ten-year outcomes for all interventions, considered singly. Expanding naloxone availability, pharmacotherapy, psychosocial treatment, syringe exchange, and PMPs are beneficial in both the short and long term, reducing opioid-related deaths while leading to gains in life years and QALYs.
Table 4.
Results for single interventions: difference from the status quo3
| a. Results for single interventions over five years | |||||
|---|---|---|---|---|---|
| Policy | Discounted Net Present LYs in Thousands (%) | Discounted Net Present QALYs in Thousands (%) | Pill Deaths (%) | Heroin Deaths (%) | Total Opioid Deaths (%) |
| Acute Pain Prescribing | 240 (0.004%) | -80 (-0.001%) | -1,100 (-1.2%) | -1,300 (-0.3%) | -2,400 (-0.4%) |
| Prescribing for Transitioning Pain | 50 (0.001%) | 70 (0.001%) | -600 (-0.6%) | 200 (0.0%) | -300 (-0.1%) |
| Chronic Pain Prescribing | 250 (0.004%) | 360 (0.006%) | -3,500 (-3.9%) | 2,300 (0.5%) | -1,200 (-0.2%) |
| Drug Rescheduling | 1,000 (0.016%) | 1,780 (0.029%) | -38,300 (-42.5%) | 49,200 (10.8%) | 10,900 (2.0%) |
| PMP | 520 (0.008%) | 90 (0.001%) | -3,600 (-4.0%) | -700 (-0.1%) | -4,300 (-0.8%) |
| Drug Reformulation | 190 (0.003%) | 250 (0.004%) | -1,700 (-1.8%)* | 100 (0.0%) | -1,600 (-0.3%) |
| Excess Opioid Disposal 10% | 210 (0.003%) | 310 (0.005%) | -3,100 (-3.4%) | 2,000 (0.4%) | -1,100 (-0.2%) |
| Excess Opioid Disposal 15% | 320 (0.005%) | 470 (0.008%) | -4,600 (-5.1%) | 3,000 (0.6%) | -1,700 (-0.3%) |
| Naloxone Availability 5% | 970 (0.015%) | 810 (0.013%) | -4,400 (-4.9%) | -19,000 (-4.2%) | -23,500 (-4.3%) |
| Naloxone Availability 15% | 3,030 (0.048%) | 2,520 (0.040%) | -13,300 (-14.8%) | -57,700 (-12.6%) | -71,000 (-13.0%) |
| Naloxone Availability 30% | 6,440 (0.102%) | 5,350 (0.086%) | -26,800 (-29.7%) | -117,200 (-25.7%) | -144,000 (-26.3%) |
| Pharmacotherapy | 630 (0.010%) | 730 (0.012%) | 400 (0.4%) | -10,600 (-2.3%) | -10,200 (-1.9%) |
| Psychosocial Treatment | 340 (0.005%) | 390 (0.006%) | -400 (-0.4%) | -3,600 (-0.8%) | -4,000 (-0.7%) |
| Syringe Exchange | 110 (0.002%) | 90 (0.001%) | 0 (0.0%) | -2,800 (-0.6%) | -2,800 (-0.5%) |
| b. Results for single interventions over ten years | |||||
| Acute Pain Prescribing | 490 (0.007%) | 180 (0.003%) | -3,000 (-1.7%) | -7,000 (-0.7%) | -9,900 (-0.8%) |
| Prescribing for Transitioning Pain | 120 (0.002%) | 150 (0.002%) | -1,500 (-0.8%) | -700 (-0.1%) | -2,100 (-0.2%) |
| Chronic Pain Prescribing | 620 (0.009%) | 790 (0.012%) | -8,900 (-5.2%) | -1,200 (-0.1%) | -10,100 (-0.8%) |
| Drug Rescheduling | 3,220 (0.048%) | 4,430 (0.067%) | -80,400 (-46.8%) | 43,100 (4.1%) | -37,300 (-3.1%) |
| PMP | 1,100 (0.016%) | 740 (0.011%) | -9,500 (-5.5%) | -11,400 (-1.1%) | -20,800 (-1.7%) |
| Drug Reformulation | 400 (0.006%) | 490 (0.007%) | -3,900 (-2.3%) | -3,700 (-0.4%) | -7,600 (-0.6%) |
| Excess Opioid Disposal 10% | 480 (0.007%) | 630 (0.009%) | -7,400 (-4.3%) | -700 (-0.1%) | -8,100 (-0.7%) |
| Excess Opioid Disposal 15% | 720 (0.011%) | 940 (0.014%) | -11,100 (-6.4%) | -1,000 (-0.1%) | -12,100 (-1.0%) |
| Naloxone Availability 5% | 1,300 (0.019%) | 1,100 (0.016%) | -8,400 (-4.9%) | -39,900 (-3.8%) | -48,300 (-4.0%) |
| Naloxone Availability 15% | 4,060 (0.060%) | 3,410 (0.051%) | -25,400 (-14.8%) | -122,000 (-11.6%) | -147,300 (-12.1%) |
| Naloxone Availability 30% | 8,630 (0.128%) | 7,250 (0.109%) | -50,900 (-29.6%) | -251,100 (-24.0%) | -301,900 (-24.8%) |
| Pharmacotherapy | 970 (0.014%) | 1,130 (0.017%) | 1,200 (0.7%) | -29,200 (-2.8%) | -28,000 (-2.3%) |
| Psychosocial Treatment | 660 (0.010%) | 760 (0.011%) | -800 (-0.5%) | -13,600 (-1.3%) | -14,400 (-1.2%) |
| Syringe Exchange | 150 (0.002%) | 130 (0.002%) | 0 (0.0%) | -5,900 (-0.6%) | -5,900 (-0.5%) |
Abbreviations: LY = life year; PMP = prescription monitoring program; QALY = quality-adjusted life year
Life years and QALYs are rounded to the nearest 10,000. Deaths are rounded to the nearest 100.
Naloxone directly reduces deaths by reversing overdose. Naloxone expansion by 5% would prevent approximately 23,500 deaths over five years (a 4.3% reduction in deaths); with 15% and 30% expansion, this number rises to 71,000 (13.0% reduction) and 144,000 (26.3% reduction), respectively. The number of deaths averted is approximately linear in the level of expansion. Over ten years, these numbers are approximately doubled.
Pharmacotherapy expansion would have a small impact on life years and QALYs, and a larger impact on deaths. Over five years, pharmacotherapy would increase life years by 0.010% and QALYs by 0.012%; over ten years, these values are 0.014% and 0.017%, respectively. Pharmacotherapy would avert 10,200 opioid-related deaths over five years (1.9% reduction) and 28,000 deaths over ten years (2.3% reduction). Although the total number of deaths decreases, the number of deaths involving opioid pills increases slightly. This is because pharmacotherapy reduces the rate of escalation to heroin use, leading to a larger number of pill-using individuals with SOUD than would occur if individuals escalated to SHUD. Although some treated individuals recover and leave the SOUD state, other treated individuals who would have escalated to heroin remain in the SOUD state, and the net number of individuals in the SOUD state is slightly higher when there is increased pharmacotherapy.
Psychosocial treatment expansion is similarly beneficial, slightly increasing life years and QALYs (0.005% and 0.006%, respectively over five years and 0.010% and 0.011% over ten years) and averting a small number of opioid-related deaths. Over five years, 4,000 deaths would be averted (0.7% reduction), with the majority (3,600) among individuals with SHUD; over ten years, these values rise to 14,400 (1.2% reduction) with 13,600 of these among individuals with SHUD.
Syringe exchange would also have a positive but small impact, averting approximately 2,800 deaths over five years (0.5% reduction) and 5,900 deaths over ten years (0.5% reduction). The impact is small because syringe exchange indirectly reduces deaths by reducing the spread of infections such as HIV and hepatitis C that lead to morbidity and mortality.
Mandating PMP use also has a small but positive impact. The total number of opioid deaths decreases over both five and ten years (by 0.8% and 1.7%, respectively), while life years and QALYs increase over both five and ten years (by 0.008% and 0.001%, respectively, over five years, and by 0.016% and 0.011%, respectively, over ten years).
The above interventions have positive effects. Other interventions have mixed effects.
Reduced prescribing for acute pain leads to a gain in life years (0.004% over five years and 0.007% cumulatively over ten years) but a reduction in QALYs (0.001% over five years) because some individuals with acute pain no longer receive pain relief from opioids. However, over ten years, QALYs slightly increase by 0.003%. Reducing acute pain prescribing has a modest effect on reducing deaths (0.4% over five years and 0.8% over ten years). Reduced prescribing for transitioning pain and chronic pain lead to slight increases in both life years and QALYs, with the effect greater for chronic pain prescribing because of the larger number of prescriptions for chronic pain. Reduced prescribing for transitioning pain slightly lowers deaths (0.1% over five years and 0.2% over ten years). Reduced prescribing for chronic pain increases heroin deaths over five years (0.5% increase), but reduces total deaths (0.2% decrease). The short-term increase in heroin deaths occurs when some individuals who cannot access opioid pills escalate to heroin, which is more deadly, particularly when it also includes fentanyl. In the longer term, however, reduced prescribing for chronic pain reduces both pill deaths (5.2% reduction) and heroin deaths (0.1% reduction), with a decrease in total deaths of 0.8%.
Excess opioid disposal has effects similar to that of reduced chronic pain prescribing, and for similar reasons. Heroin deaths increase over five years (by 0.4% and 0.6% for a 10% and 15% expansion, respectively) but decrease over ten years (by 0.1% for both levels of expansion). Total deaths decrease over five and ten years (by 0.2% and 0.3% for a 10% and 15% expansion, respectively, over five years, and by 0.7% and 1.0% over ten years), and both life years and QALYs are gained in the short term and long term.
For drug rescheduling, deaths increase over five years (by 2.0%) due to increases in heroin deaths. This occurs because some individuals switch to heroin, creating more deaths in the short term. Although heroin deaths increase over ten years, the total number of opioid deaths decreases (by 3.1%), because the total number of individuals with use disorder is smaller. Both life years and QALYs are gained in the short term and long term.
Tamper-resistant drug reformulation leads to very small increases in life years and QALYs (0.003% and 0.004% over five years, respectively, and 0.006% and 0.007% over ten years) and a small decrease in total deaths (0.3% over five years and 0.6% over ten years). Significant numbers of prescription opioid deaths are averted, which is partially offset by a smaller increase in the number of heroin deaths in the short term. This is because drug reformulation decreases the supply of opioid pills easily converted to more potent routes of administration, thereby causing some individuals to escalate to heroin use.
3.1.2. Combined Interventions
Table 5 shows results for combinations of interventions. The greatest impact was achieved with 30% naloxone expansion combined with either reductions in all prescribing or with PMPs, leading to approximately 0.1% gains in life years and QALYs and approximately 27% reductions in opioid deaths over five and ten years.
Table 5.
Results for combined interventions: difference from the status quo4 a. Results for combined interventions over five years b. Results for combined interventions over ten years
| Policy | Discounted Net Present LYs in Thousands (%) | Discounted Net Present QALYs in Thousands (%) | Pill Deaths (%) | Heroin Deaths (%) | Total Opioid Deaths (%) |
|---|---|---|---|---|---|
| All Prescribing5 | 550 (0.009%) | 350 (0.006%) | -5,100 (-5.7%) | 1,200 (0.3%) | -3,900 (-0.7%) |
| All Prescribing + Naloxone 5% | 1,500 (0.024%) | 1,140 (0.018%) | -9,300 (-10.3%) | -17,900 (-3.9%) | -27,200 (-5.0%) |
| All Prescribing + Naloxone 15% | 3,510 (0.056%) | 2,820 (0.045%) | -17,700 (-19.6%) | -56,600 (-12.4%) | -74,300 (-13.6%) |
| All Prescribing + Naloxone 30% | 6,860 (0.108%) | 5,590 (0.090%) | -30,300 (-33.6%) | -116,400 (-25.5%) | -146,700 (-26.8%) |
| All Prescribing + SEP | 660 (0.010%) | 440 (0.007%) | -5,100 (-5.7%) | -1,600 (-0.4%) | -6,700 (-1.2%) |
| All Prescribing + Pharmacotherapy | 1,160 (0.018%) | 1,060 (0.017%) | -4,700 (-5.3%) | -9,200 (-2.0%) | -14,000 (-2.6%) |
| All Prescribing + PT | 890 (0.014%) | 730 (0.012%) | -5,400 (-6.0%) | -2,400 (-0.5%) | -7,800 (-1.4%) |
| All Prescribing + Drug Reformulation + Pharmacotherapy + SEP + Naloxone 5% + PT | 2,690 (0.043%) | 2,520 (0.040%) | -10,700 (-11.8%) | -33,900 (-7.4%) | -44,600 (-8.1%) |
| Drug Rescheduling + Naloxone 5% | 1,910 (0.030%) | 2,540 (0.041%) | -40,900 (-45.3%) | 28,100 (6.2%) | -12,800 (-2.3%) |
| Drug Rescheduling + Naloxone 15% | 3,840 (0.061%) | 4,140 (0.067%) | -46,000 (-51.0%) | -14,800 (-3.2%) | -60,800 (-11.1%) |
| Drug Rescheduling + Naloxone 30% | 7,060 (0.112%) | 6,810 (0.109%) | -53,800 (-59.6%) | -80,800 (-17.7%) | -134,500 (-24.6%) |
| Drug Rescheduling + SEP | 1,110 (0.018%) | 1,880 (0.030%) | -38,300 (-42.5%) | 46,100 (10.1%) | 7,800 (1.4%) |
| Drug Rescheduling + Pharmacotherapy | 1,580 (0.025%) | 2,450 (0.039%) | -37,600 (-41.7%) | 38,300 (8.4%) | 700 (0.1%) |
| Drug Rescheduling + PT | 1,300 (0.021%) | 2,120 (0.034%) | -38,400 (-42.6%) | 45,600 (10.0%) | 7,200 (1.3%) |
| PMP + Naloxone 5% | 1,470 (0.023%) | 880 (0.014%) | -7,900 (-8.8%) | -19,700 (-4.3%) | -27,500 (-5.0%) |
| PMP + Naloxone 15% | 3,480 (0.055%) | 2,560 (0.041%) | -16,400 (-18.2%) | -58,200 (-12.8%) | -74,700 (-13.7%) |
| PMP + Naloxone 30% | 6,830 (0.108%) | 5,340 (0.086%) | -29,300 (-32.5%) | -117,700 (-25.8%) | -147,000 (-26.9%) |
| PMP + SEP | 620 (0.010%) | 180 (0.003%) | -3,600 (-4.0%) | -3,500 (-0.8%) | -7,100 (-1.3%) |
| PMP + Pharmacotherapy | 1,130 (0.018%) | 800 (0.013%) | -3,300 (-3.6%) | -11,100 (-2.4%) | -14,300 (-2.6%) |
| PMP + PT | 850 (0.013%) | 470 (0.008%) | -4,000 (-4.4%) | -4,200 (-0.9%) | -8,200 (-1.5%) |
| All Prescribing2 | 1,230 (0.018%) | 1,130 (0.017%) | -13,200 (-7.7%) | -9,100 (-0.9%) | -22,200 (-1.8%) |
| All Prescribing + Naloxone 5% | 2,490 (0.037%) | 2,190 (0.033%) | -20,900 (-12.2%) | -48,600 (-4.6%) | -69,600 (-5.7%) |
| All Prescribing + Naloxone 15% | 5,160 (0.076%) | 4,440 (0.067%) | -36,600 (-21.3%) | -130,000 (-12.4%) | -166,500 (-13.7%) |
| All Prescribing + Naloxone 30% | 9,600 (0.142%) | 8,160 (0.123%) | -60,100 (-35.0%) | -257,900 (-24.6%) | -318,100 (-26.1%) |
| All Prescribing + SEP | 1,380 (0.020%) | 1,250 (0.019%) | -13,200 (-7.7%) | -15,000 (-1.4%) | -28,100 (-2.3%) |
| All Prescribing + Pharmacotherapy | 2,160 (0.032%) | 2,220 (0.033%) | -12,000 (-7.0%) | -37,400 (-3.6%) | -49,400 (-4.0%) |
| All Prescribing + PT | 1,870 (0.028%) | 1,860 (0.028%) | -13,900 (-8.1%) | -22,400 (-2.1%) | -36,300 (-3.0%) |
| All Prescribing + Drug Reformulation + Pharmacotherapy + SEP + Naloxone 5% + PT | 4,490 (0.067%) | 4,510 (0.068%) | -23,800 (-13.9%) | -97,100 (-9.3%) | -120,900 (-9.9%) |
| Drug Rescheduling + Naloxone 5% | 4,400 (0.065%) | 5,420 (0.081%) | -84,900 (-49.4%) | 1,600 (0.1%) | -83,400 (-6.8%) |
| Drug Rescheduling + Naloxone 15% | 6,900 (0.102%) | 7,520 (0.113%) | -94,000 (-54.7%) | -84,000 (-8.0%) | -178,000 (-14.6%) |
| Drug Rescheduling + Naloxone 30% | 11,060 (0.164%) | 11,010 (0.166%) | -107,600 (-62.6%) | -218,500 (-20.9%) | -326,100 (-26.7%) |
| Drug Rescheduling + SEP | 3,370 (0.050%) | 4,550 (0.068%) | -80,400 (-46.8%) | 37,000 (3.5%) | -43,400 (-3.6%) |
| Drug Rescheduling + Pharmacotherapy | 4,080 (0.060%) | 5,410 (0.081%) | -78,600 (-45.7%) | 15,400 (1.5%) | -63,200 (-5.2%) |
| Drug Rescheduling + PT | 3,780 (0.056%) | 5,060 (0.076%) | -80,600 (-46.9%) | 30,800 (2.9%) | -49,800 (-4.1%) |
| PMP + Naloxone 5% | 2,360 (0.035%) | 1,800 (0.027%) | -17,400 (-10.1%) | -50,800 (-4.8%) | -68,300 (-5.6%) |
| PMP + Naloxone 15% | 5,040 (0.075%) | 4,060 (0.061%) | -33,400 (-19.4%) | -132,000 (-12.6%) | -165,400 (-13.6%) |
| PMP + Naloxone 30% | 9,500 (0.141%) | 7,800 (0.117%) | -57,500 (-33.5%) | -259,600 (-24.8%) | -317,200 (-26.0%) |
| PMP + SEP | 1,240 (0.018%) | 860 (0.013%) | -9,500 (-5.5%) | -17,200 (-1.6%) | -26,700 (-2.2%) |
| PMP + Pharmacotherapy | 2,040 (0.030%) | 1,830 (0.028%) | -8,300 (-4.8%) | -39,800 (-3.8%) | -48,100 (-3.9%) |
| PMP + PT | 1,740 (0.026%) | 1,470 (0.022%) | -10,200 (-6.0%) | -24,700 (-2.4%) | -35,000 (-2.9%) |
Abbreviations: LY = life year; PMP = prescription monitoring program; PT = psychosocial treatment; QALY = quality-adjusted life year; SEP = syringe exchange program
Life years and QALYs are rounded to the nearest 1000. Deaths are rounded to the nearest 100.
Reductions in prescribing for acute, transitioning, and chronic pain
If all prescribing were reduced by 10%, a modest impact would be achieved over five years: pill deaths would decrease by 5.7% whereas heroin deaths would increase by 0.3%, leading to a net 3,900 fewer deaths (0.7% reduction). Over ten years, more benefits would accrue, with 22,200 deaths averted (1.8% reduction). Over both time horizons, life years and QALYs increase very slightly. Benefits increase significantly when reductions in prescribing are combined variously with naloxone, syringe exchange, pharmacotherapy, and psychosocial treatment. If prescribing reductions are combined with 30% naloxone expansion, approximately 27% of opioid deaths are averted over both five and ten years, and life years and QALYs increase by approximately 0.1%. Even with 5% naloxone expansion, if prescribing reductions are also combined with drug reformulation, pharmacotherapy, and syringe exchange, 8.1% of deaths (44,600) could be averted over five years, and 9.9% of deaths (120,900) could be averted over ten years. Reductions in prescribing combined with syringe exchange, pharmacotherapy, or psychosocial treatment alone would have only a modest impact, increasing life years and QALYs by less than 0.1% and decreasing deaths by 1.2%-4.0% over five and ten years.
When PMP is combined with naloxone, syringe exchange, pharmacotherapy, or psychosocial treatment, effects are similar to those for reduced prescribing when combined with these interventions: the greatest benefit occurs when PMP is combined with 30% naloxone expansion.
When drug rescheduling is combined with syringe exchange, pharmacotherapy, or psychosocial treatment, total deaths increase over five years due to increases in heroin deaths but decrease over ten years.
In many cases, intervention combinations are less than additive. For example, when pharmacotherapy is combined with reductions in prescribing, drug rescheduling, or PMP, the number of life years and QALYs gained is slightly lower than the sum from the individual interventions and the number of deaths averted is slightly lower. This is because the same death and morbidity cannot be prevented twice.
Synergies occurred when syringe exchange was combined with reductions in prescribing or drug rescheduling: the number of life years, QALYs, and opioid-related deaths for the combined interventions over five years were all higher than the sum of these values for the single interventions. This synergy occurs because, for individuals who escalate to heroin due to reductions in prescribing or drug rescheduling, syringe exchange reduces injection-related deaths, allowing those individuals to live longer and gain life years and QALYs.
3.2. Sensitivity Analyses
In one-way sensitivity analyses (Table S4), results were particularly sensitive to the probability of diversion of pills to non-users. If diversion of pills to non-users is 50% lower than in the base case analyses, reductions in prescribing, drug rescheduling, PMPs, drug reformulation, and excess opioid disposal lead to more deaths than in the base case analyses. This is because more individuals escalate to heroin when fewer pills are available for diversion. If the probability of escalation to heroin is 25% lower than in the base case analyses, then reduced chronic pain prescribing and excess opioid disposal both avert more deaths over five and ten years, whereas drug rescheduling leads to a smaller increase in deaths over five years than in the base case analyses (0.6% vs. 2.0%), and leads to 3.9% of deaths averted over ten years.
4. Discussion
Our analyses show that reduced opioid prescribing combined with PMPs and expanded health services for individuals with opioid use disorder would moderately lessen the severity of the opioid crisis over the next decade. Expansion of naloxone availability had the largest effect: with 30% expansion, approximately 25% of opioid deaths would be averted. Pharmacotherapy, syringe exchange, psychosocial treatment, and PMPs are beneficial across time horizons and outcomes, reducing opioid-related deaths while leading to gains in life years and QALYs. Tamper-resistant reformulation was also beneficial, though the effect was smaller. Reduced prescribing and increasing excess opioid disposal programs would reduce lives lost at five and ten years. Rescheduling drugs would lead to increases in total deaths over five years as some individuals escalate to heroin, but decreases in deaths over ten years. Combined interventions would lead to greater increases in life years, QALYs, and deaths averted. In many cases, the results of combined interventions are subadditive because interventions compete with each other for resources and because success of some interventions (e.g., pharmacotherapy) lowers the need for others (e.g., syringe exchange). Sadly, significant morbidity and mortality occur even if significant policy change is assumed.
Some policies have modest or even negative effects in the short term and a positive effect in the longer term. For example, restrictions on opioid prescribing can lead to some pill-addicted individuals switching to more dangerous illicit opioids. In the first few years, this effect can nearly outweigh decreases in prescription pill deaths. However, the balance shifts over time to the policy being clearly welfare-maximizing because the pool of previously addicted potential switchers grows smaller while the pool of individuals without opioid use disorder who avoid pill addiction grows larger.
One might ask why the U.S. would even consider implementing prescription restricting policies when policies such as syringe exchange and pharmacotherapy expansion can reduce years of life lost immediately and consistently [33]. Epidemics do not generally fade via a public health strategy with no preventive component. Over time, more judicious opioid prescribing is necessary so that fewer individuals develop opioid use disorder in the first place. The most recent UN data shows that while U.S. per capita opioid prescribing has declined by about one third since its peak, it still is the highest in the world and out of step with developed world norms (e.g., more than four-fold that of Italy and France, which have comparable levels of population pain) [34].
Several differences in the findings here versus our prior analysis [17] merit comment. Policies restricting opioid prescribing now appear more beneficial in terms of lives saved. This is because the current model focuses on a later period of time in which population transitions from opioid pill to illicit opioid use disorder have partially occurred already. PMPs produced a much more positive result in this model in part due to this same effect, and also because enrolling in and using PMPs is becoming mandatory. Recent research shows that while PMPs per se have little effect, with mandates they reduce opioid-related morbidity and mortality [23,35]. As more states adopt these requirements, the benefits of these programs should continue to expand.
The other major difference in our model is increased prediction of opioid-related mortality in the age of COVID-19 and synthetic opioids, which was not foreseeable in our prior model. Both the virus and the measures taken to stop its spread can increase anxiety, isolation, and difficulty accessing treatment services [6,7,9,11]. All signs are that COVID-19, combined with increased availability of synthetic opioids will make 2020 the deadliest year in U.S. history in terms of overdose mortality [8]. The former challenge should recede rapidly as vaccines are administered, with positive side effects on opioid-related morbidity and mortality. The latter challenge is more enduring: because the profit margin on fentanyl is so much higher than for heroin, drug traffickers can be expected to expand its availability in the future [36]. New policies to address synthetic drugs are receiving detailed attention within the Stanford-Lancet Commission's ongoing work [37] as well as by the European Monitoring Centre for Drugs and Drug Addiction [38].
Our results are in line with those of other recent studies that have modeled the impact of interventions on the opioid epidemic, but with a narrower focus than we have taken. For example, a study using a dynamic systems model of the U.S. opioid epidemic found that interventions targeting prescription opioid misuse would have a positive but modest effect on their own [39]. Another modelling study also concluded that no single intervention would significantly reduce overdose deaths and prevalence of SOUD, but a combined strategy including reduced prescriptions, reduction in diverted prescriptions, expanded treatment, and expanded naloxone could have a significant impact [40].
Our analysis has several limitations. We attempted to compensate for weaknesses in data on the opioid epidemic by creating ten base cases and performing extensive sensitivity analyses. More refined data about the epidemic and potential interventions could help support more granular estimates of intervention effects. Even with more refined data, many social, political, economic, and other factors that we have not captured (e.g., the emergence of other addictive drugs) could affect the course of the opioid epidemic. Additionally, our analysis focuses on interventions specifically targeted to opioid use disorder but does not capture potential effects of broader public policies (e.g., economic, housing, labor and occupational safety, criminal justice [41]) on the opioid epidemic.
Our findings point to routes to save many thousands of lives. However, it is sobering that even all policies combined cannot prevent substantial further morbidity and mortality. Drug epidemics have their own momentum once a very large population of individuals with use disorder is created by an enormous increase in drug supply, even if that original source of supply is subsequently diminished. Thus, although every effort should be made using the policies studied here to lessen the damage of the epidemic, it should never be forgotten that the best public health policy would have been to have had a stronger regulatory environment in which profit-seeking companies could never have started it in the first place [42].
Countries like the U.S. and Canada with a large population of individuals with opioid use disorder should implement the policies found effective here (e.g., naloxone distribution) to lessen the further toll of the crisis on population morbidity and mortality. Additionally, policymakers in nations other than the U.S. and Canada should take strong preventive action now to regulate opioid manufacturers in a fashion that prevents a spread of the opioid epidemic to their countries [15]
Contributors
IR was responsible for literature search; data collection and verification; model development and methodology; model validation and analysis; and manuscript preparation and revision. KH was responsible for conceptualization, funding acquisition, literature search, data collection, methodology, supervision, and manuscript preparation and revision. MB was responsible for conceptualization, funding acquisition, literature search, data collection, methodology, supervision, and manuscript preparation and revision.
Declaration of Interests
KH is an unpaid scientific advisor to the Foundation for Opioid Response Efforts, a non-profit foundation funding research and services that was created using $100 million from opioid distributors. All other authors declare no competing interests.
Data Sharing Statement
All data used in this analysis are publicly available in the cited sources.
Funding
Grant R37-DA15612 from the National Institute on Drug Abuse, Grant # IIR 17-139 from the US Department of Veterans Affairs, Health Services Research and Development (HSR&D), and a grant from Stanford University School of Medicine to support the Stanford-Lancet Commission on the North American Opioid Crisis. The authors have no conflict of interest to report.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lana.2021.100031.
Appendix. Supplementary materials
References
- 1.Centers for Disease Control and Prevention. CDC guideline for prescribing opioids for chronic pain. 2020. https://www.cdc.gov/drugoverdose/pdf/Guidelines_At-A-Glance-508.pdf (accessed Jun 22 2021).
- 2.Centers for Disease Control and Prevention. Wide-ranging online data for epidemiologic research (WONDER). 2020. https://wonder.cdc.gov/ (accessed Jun 17 2021).
- 3.Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901–906. doi: 10.1097/MLR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burden of Disease Collaborators U.S., Mokdad AH, Ballestros K, et al. The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444–1472. doi: 10.1001/jama.2018.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luo F, Li M, Florence C. State-level economic costs of opioid use disorder and fatal opioid overdose - United States, 2017. MMWR Morb Mortal Wkly Rep. 2021;70(15):541–546. doi: 10.15585/mmwr.mm7015a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alexander GC, Stoller KB, Haffajee RL, Saloner B. An epidemic in the midst of a pandemic: opioid use disorder and COVID-19. Ann Intern Med. 2020;173(1):57–58. doi: 10.7326/M20-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Medical Association. Issue brief: Reports of increases in opioid-related overdose and other concerns during COVID pandemic. 2021. https://www.ama-assn.org/system/files/2020-12/issue-brief-increases-in-opioid-related-overdose.pdf (accessed Jun 23 2021).
- 8.Centers for Disease Control and Prevention. Increase in fatal drug overdoses across the United States driven by synthetic opioids before and during the COVID-19 pandemic. 2020. https://emergency.cdc.gov/han/2020/han00438.asp (accessed Jun 22 2021).
- 9.Katz J, Goodnough A, Sanger-Katz M. NY Times; 2020. In shadow of pandemic, U.S. drug overdose deaths resurge to record. Jul 15. [Google Scholar]
- 10.The Daily Briefing. Fatal drug overdoses hit a record high last year. Covid-19 is making the problem worse. 2020. https://www.advisory.com/daily-briefing/2020/07/17/overdose (accessed Aug 5 2020).
- 11.Wan W, Long H. Cries for help’: Drug overdoses are soaring during the coronavirus pandemic. Washington Post. 2020 Jul 1 [Google Scholar]
- 12.Strang J, Babor T, Caulkins J, Fischer B, Foxcroft D, Humphreys K. Drug policy and the public good: evidence for effective interventions. Lancet. 2012;379(9810):71–83. doi: 10.1016/S0140-6736(11)61674-7. [DOI] [PubMed] [Google Scholar]
- 13.Babor T, Caulkins J, Fischer B, et al. 2nd ed. Oxford University Press; Oxford, UK: 2018. Drug Policy and the Public Good. [Google Scholar]
- 14.National Academies of Sciences Engineering and Medicine . National Academies Press; Washington, DC: 2019. Medications for Opioid Use Disorder Save Lives. [PubMed] [Google Scholar]
- 15.Humphreys K. Avoiding globalisation of the prescription opioid epidemic. Lancet. 2017;390(10093):437–439. doi: 10.1016/S0140-6736(17)31918-9. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Annual surveillance report of drug-related risks and outcomes – United States surveillance special report. 2019. https://www.cdc.gov/drugoverdose/pdf/pubs/2019-cdc-drug-surveillance-report.pdf (accessed Jun 22 2021).
- 17.Pitt AL, Humphreys K, Brandeau ML. Modeling health benefits and harms of public policy responses to the US opioid epidemic. Am J Public Health. 2018;108(10):1394–1400. doi: 10.2105/AJPH.2018.304590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shover CL, Falasinnu TO, Dwyer CL, et al. Steep increases in fentanyl-related mortality west of the Mississippi River: recent evidence from county and state surveillance. Drug Alcohol Depend. 2020;216 doi: 10.1016/j.drugalcdep.2020.108314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quinones S. Bloomsbury Press; New York, NY: 2016. Dreamland: The True Tale of America's Opiate Epidemic. [Google Scholar]
- 20.Centers for Disease Control and Prevention. U.S. opioid dispensing rate maps. 2020. https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html (accessed Jun 22 2021).
- 21.Jones CM, Lurie PG, Throckmorton DC. Effect of US Drug Enforcement Administration's rescheduling of hydrocodone combination analgesic products on opioid analgesic prescribing. JAMA Intern Med. 2016;176(3):399–402. doi: 10.1001/jamainternmed.2015.7799. [DOI] [PubMed] [Google Scholar]
- 22.McDonald DC, Carlson KE. Estimating the prevalence of opioid diversion by "doctor shoppers" in the United States. PLoS One. 2013;8(7):e69241. doi: 10.1371/journal.pone.0069241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dowell D, Zhang K, Noonan RK, Hockenberry JM. Mandatory provider review and pain clinic laws reduce the amounts of opioids prescribed and overdose death rates. Health Aff (Millwood) 2016;35(10):1876–1883. doi: 10.1377/hlthaff.2016.0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Food and Drug Administration. FDA analysis of long-term trends in prescription opioid analgesic products: quantity, sales, and price trends. 2018. https://www.fda.gov/media/111695/download (accessed Jun 22 2021).
- 25.Cicero TJ, Ellis MS. Abuse-deterrent formulations and the prescription opioid abuse epidemic in the United States: lessons learned from OxyContin. JAMA Psychiatry. 2015;72(5):424–430. doi: 10.1001/jamapsychiatry.2014.3043. [DOI] [PubMed] [Google Scholar]
- 26.Hasak JM, Roth Bettlach CL, Santosa KB, Larson EL, Stroud J, Mackinnon SE. Empowering post-surgical patients to improve opioid disposal: a before and after quality improvement study. J Am Coll Surg. 2018;226(3) doi: 10.1016/j.jamcollsurg.2017.11.023. 235-40 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abouk R, Pacula RL, Powell D. Association between state laws facilitating pharmacy distribution of naloxone and risk of fatal overdose. JAMA Intern Med. 2019;179(6):805–811. doi: 10.1001/jamainternmed.2019.0272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McClellan C, Lambdin BH, Ali MM, et al. Opioid-overdose laws association with opioid use and overdose mortality. Addict Behav. 2018;86:90–95. doi: 10.1016/j.addbeh.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 29.Fairley M, Humphreys K, Joyce VR, et al. Cost-effectiveness of treatments for opioid use disorder. JAMA Psychiatry. 2021;31 doi: 10.1001/jamapsychiatry.2021.0247. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Substance Abuse and Mental Health Services Administration. 2018 National Survey on Drug Use and Health: detailed tables. 2019 2019. https://www.samhsa.gov/data/report/2018-nsduh-detailed-tables (accessed Jun 17 2021).
- 31.Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS): 2017. Admissions to and discharges from publicly-funded substance use treatment. 2019. https://www.samhsa.gov/data/report/treatment-episode-data-set-teds-2017-admissions-and-discharges-publicly-funded-substance-use (accessed Jun 17 2021).
- 32.Sanders GD, Neumann PJ, Basu A, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016;316(10):1093–1103. doi: 10.1001/jama.2016.12195. [DOI] [PubMed] [Google Scholar]
- 33.Humphreys K. Reconciling the present and the future in opioid prescription policy: an ethical dilemma. Pain Med. 2018;19(8):1514–1515. doi: 10.1093/pm/pny120. [DOI] [PubMed] [Google Scholar]
- 34.International Narcotics Control Board. Narcotic drugs: estimated world requirements for 2020 and statistics for 2018. 2020. https://www.incb.org/documents/Narcotic-Drugs/Technical-Publications/2019/Narcotic_Drugs_Technical_Publication_2019_web.pdf (accessed Jun 24 2021).
- 35.Buchmueller TC, Carey C. The effect of prescription drug monitoring programs on opioid utilization in Medicare. Amer Econ J: Econ Policy. 2018;10(1):77–112. [Google Scholar]
- 36.Humphreys K. How fentanyl could alter global drug policy. Washington Post. 2018 May 22. [Google Scholar]
- 37.Humphreys K, Shover CL, Andrews CM, et al. Working Paper; 2021. Responding to the opioid crisis in North America and beyond: recommendations of The Stanford-Lancet Commission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.European Monitoring Centre for Drugs and Drug Addiction . Luxembourg: Publications Office of the European Union; 2020. New psychoactive substances: global markets, global threats and the COVID-19 pandemic. An update from the EU Early Warning System (December 2020) [Google Scholar]
- 39.Chen Q, Larochelle MR, Weaver DT, et al. Prevention of prescription opioid misuse and projected overdose deaths in the United States. JAMA Netw Open. 2019;2(2) doi: 10.1001/jamanetworkopen.2018.7621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Homer J, Wakeland W. A dynamic model of the opioid drug epidemic with implications for policy. Am J Drug Alcohol Abuse. 2021;47(1):5–15. doi: 10.1080/00952990.2020.1755677. [DOI] [PubMed] [Google Scholar]
- 41.Bernard CM, Rao IJ, Robison KK, Brandeau ML. Health outcomes and cost-effectiveness of diversion programs for low-level drug offenders: a model-based analysis. PLoS Med. 2020;17(10) doi: 10.1371/journal.pmed.1003239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Humphreys K, Caulkins JP, Felbab-Brown V. Opioids of the masses: stopping an American epidemic from going global. Foreign Affairs. 2018;97:118–129. May-Jun. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.