Katrine M Johannesen
Katrine M Johannesen, MD, PhD
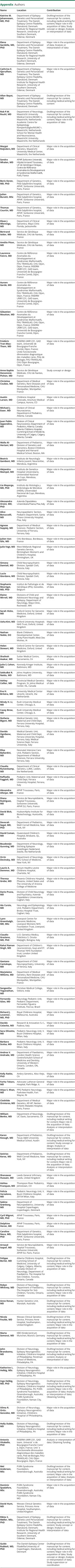
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,✉,
Elena Gardella
Elena Gardella, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Cathrine E Gjerulfsen
Cathrine E Gjerulfsen, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Allan Bayat
Allan Bayat, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Rob PW Rouhl
Rob PW Rouhl, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Margot Reijnders
Margot Reijnders, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Sandra Whalen
Sandra Whalen, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Boris Keren
Boris Keren, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Julien Buratti
Julien Buratti, MSc
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Thomas Courtin
Thomas Courtin, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Klaas J Wierenga
Klaas J Wierenga, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Bertrand Isidor
Bertrand Isidor, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Amélie Piton
Amélie Piton, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Laurence Faivre
Laurence Faivre, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Aurore Garde
Aurore Garde, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Sébastien Moutton
Sébastien Moutton, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Frédéric Tran-Mau-Them
Frédéric Tran-Mau-Them, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Anne-Sophie Denommé-Pichon
Anne-Sophie Denommé-Pichon, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Christine Coubes
Christine Coubes, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Austin Larson
Austin Larson, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Michael J Esser
Michael J Esser, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Juan Pablo Appendino
Juan Pablo Appendino, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Walla Al-Hertani
Walla Al-Hertani, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Beatriz Gamboni
Beatriz Gamboni, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Alejandra Mampel
Alejandra Mampel, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Lía Mayorga
Lía Mayorga, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Alessandro Orsini
Alessandro Orsini, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Alice Bonuccelli
Alice Bonuccelli, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Agnese Suppiej
Agnese Suppiej, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Julien Van-Gils
Julien Van-Gils, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Julie Vogt
Julie Vogt, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Simona Damioli
Simona Damioli, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Lucio Giordano
Lucio Giordano, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Stephanie Moortgat
Stephanie Moortgat, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Elaine Wirrell
Elaine Wirrell, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Sarah Hicks
Sarah Hicks, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Usha Kini
Usha Kini, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Nathan Noble
Nathan Noble, DO
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Helen Stewart
Helen Stewart, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Shailesh Asakar
Shailesh Asakar, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Julie S Cohen
Julie S Cohen, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
SakkuBai R Naidu
SakkuBai R Naidu, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Ashley Collier
Ashley Collier, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Eva H Brilstra
Eva H Brilstra, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Mindy H Li
Mindy H Li, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Casey Brew
Casey Brew, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Stefania Bigoni
Stefania Bigoni, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Davide Ognibene
Davide Ognibene, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Elisa Ballardini
Elisa Ballardini, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Claudia Ruivenkamp
Claudia Ruivenkamp, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Raffaella Faggioli
Raffaella Faggioli, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Alexandra Afenjar
Alexandra Afenjar, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Diana Rodriguez
Diana Rodriguez, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
David Bick
David Bick, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Devorah Segal
Devorah Segal, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
David Coman
David Coman, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Boudewijn Gunning
Boudewijn Gunning, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Orrin Devinsky
Orrin Devinsky, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Laurie A Demmer
Laurie A Demmer, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Theresa Grebe
Theresa Grebe, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Dario Pruna
Dario Pruna, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Ida Cursio
Ida Cursio, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Lynn Greenhalgh
Lynn Greenhalgh, MD, MSc
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Claudio Graziano
Claudio Graziano, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Rahul Raman Singh
Rahul Raman Singh, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Gaetano Cantalupo
Gaetano Cantalupo, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Marjolaine Willems
Marjolaine Willems, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Sangeetha Yoganathan
Sangeetha Yoganathan, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Fernanda Góes
Fernanda Góes, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Richard J Leventer
Richard J Leventer, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Davide Colavito
Davide Colavito, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Sara Olivotto
Sara Olivotto, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Barbara Scelsa
Barbara Scelsa, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Andrea V Andrade
Andrea V Andrade, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Kelly Ratke
Kelly Ratke, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Farha Tokarz
Farha Tokarz, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Atiya S Khan
Atiya S Khan, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Clothilde Ormieres
Clothilde Ormieres, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
William Benko
William Benko, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Karen Keough
Karen Keough, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Sotirios Keros
Sotirios Keros, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Shanawaz Hussain
Shanawaz Hussain, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Ashlea Franques
Ashlea Franques, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Felicia Varsalone
Felicia Varsalone, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Sabine Grønborg
Sabine Grønborg, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Cyril Mignot
Cyril Mignot, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Delphine Heron
Delphine Heron, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Caroline Nava
Caroline Nava, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Arnaud Isapof
Arnaud Isapof, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Felippe Borlot
Felippe Borlot, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Robyn Whitney
Robyn Whitney, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Anne Ronan
Anne Ronan, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Nicola Foulds
Nicola Foulds, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Marta Somorai
Marta Somorai, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
John Brandsema
John Brandsema, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Katherine L Helbig
Katherine L Helbig, MSc
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Ingo Helbig
Ingo Helbig, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Xilma R Ortiz-González
Xilma R Ortiz-González, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Holly Dubbs
Holly Dubbs, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Antonio Vitobello
Antonio Vitobello, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Mel Anderson
Mel Anderson, MSc
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Dominic Spadafore
Dominic Spadafore, MSc
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
David Hunt
David Hunt, MD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Rikke S Møller
Rikke S Møller, MSc, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,
Guido Rubboli
Guido Rubboli, MD, PhD
1From the Department of Epilepsy Genetics and Personalized Treatment (K.M.J., E.G., C.E.G., A.B., R.S.M., G.R.), The Danish Epilepsy Centre Filadelfia, member of ERN EpiCARE, Dianalund; Institute for Regional Health Research (K.M.J., E.G., A.B., R.S.M), University of Southern Denmark, Odense; Department of Neurology (R.P.W.R.), Maastricht University Medical Centre (MUMC+); Academic Centre for Epileptology Kempenhaeghe/MUMC+ (R.P.W.R.), Maastricht; School for Mental Health and Neuroscience (R.P.W.R.), Maastricht University; Department of Clinical Genetics (M.R.), Maastricht University Medical Center, the Netherlands; APHP, Sorbonne Université (S.W.), Hôpital Armand Trousseau, UF de Génétique Clinique, Centre de Référence Anomalies du Développement et Syndromes Malformatifs, Paris, France; Department of Genetics (B.K., J.B., T.C., C.N.), Pitié-Salpêtrière hospital, APHP, Sorbonne Université, Paris, France; Department of Clinical Genomics (K.J.W.), Mayo Clinic Florida, Jacksonville; Service de Génétique Médicale (B.I., A.P., A.-S.D.-P.), CHU de Nantes; Centre de Référence Anomalies du Développement et Syndromes Malformatifs (L.F., A.G., S.M.), FHU TRANSLAD, CHU Dijon; INSERM UMR1231 (L.F., A.G., S.M., F.T.M.-T., A.V.), GAD team, Université de Bourgogne-Franche Comté, Dijon; Unité Fonctionnelle dInnovation diagnostique des maladies rares (F.T.-M.-T., A.V.), Pôle de Biologie, FHU-TRANSLAD, CHU Dijon Bourgogne; Department of Medical Genetics (C.C., M.W.), Rare Diseases and Personalized Medicine, CHU Montpellier, France; Childrens Hospital Colorado (A.L.), Anschutz Medical Campus, Aurora, CO; Division of Clinical Neuroscience (M.J.E., J.P.A.), Department of Pediatrics, Alberta, Canada; Alberta Childrens Hospital (J.P.A., F.B.), Cumming School of Medicine, University of Calgary, Alberta, Canada; Department of Pediatrics (W.A.-H.), Division of Genetics and Genomics, Boston Childrens Hospital and Harvard Medical School, MA; Instituto de Neurología Infanto Juvenil (B.G.), Neuroinfan; Instituto de Genetica-Hospital Universitario (A.M.), Universidad Nacional de Cuyo; Instituto de Histología y Embriología de Mendoza (IHEM) (L.M.), Universidad Nacional de Cuyo, Mendoza, Argentina; Azienda Ospedaliera Universitaria Pisana (A.O.); Neuropaediatric Section (A.B.), Pediatric Department, Santa Chiara University Hospital, Pisa; Department of Medical Sciences- Pediatric Section (A.S.), University of Ferrara, Italy; CHU Bordeaux (J.V.-G.), Bordeaux, France; West Midlands Regional Genetics Service (J.V.), Birmingham Women's and Children's Hospital, Birmingham, UK; Child Neuropsychiatric Division (S.D., L.G.), Spedali Civili, Brescia, Italy; Institut de Pathologie et de Génétique (IPG) (S.M.), Gosselies, Belgium; Divisions of Child and Adolescent Neurology and Epilepsy (E.W.), Department of Neurology, Mayo Clinic, Rochester, MN; Oxford Centre for Genomic Medicine (S.H., H.S.); Oxford University Hospitals NHS Trust (U.K.), United Kingdom; Blank Children's Developmental Center (N.N.), Unity Point Health, West Des Moines, IA; Sutter Medical Centre (S.A.), Sacramento, CA; Kennedy Krieger Institute (J.S.C.); Johns Hopkins University (S.R.N.), Baltimore, MD; Provincial Medical Genetics Program (A.C.), St. Johns Medical Center, NL, Canada; University Medical Center Utrecht (E.H.B.), Utrecht, the Netherlands; Rush University Medical Center (M.H.L., C.B.), Chicago, IL; Medical Genetic Unit (S.B., D.O.), Maternal and Child Department, Ferrara University Hospital; Medical Science Department (D.O.), Ferrara University; Neonatal Intensive Care Unit (E.B.), Pediatric Section, Department of Medical Sciences, Ferrara University, Italy; Department of Clinical Genetics (C.R.), LUMC, Leiden, the Netherlands; Pediatric Unit, Maternal and Child Department (R.F.), Ferrara University Hospital, Italy; APHP Trousseau (A.A., C.M., D.H.); Service de Neuropédiatrie (D.R., A.I.), Hopital Trousseau, Sorbonne Université, APHP.SU, Paris, France; HudsonAlpha Institute for Biotechnology (D.B.), Huntsville, AL; Department of Pediatrics (D.S., S.K.), Weill Cornell Medicine, New York; Queensland Children's Hospital (D.C.), Brisbane, QL, Australia; Department of Neurology (B.G.), Stichting Epilepsie Instellingen Nederland, Zwolle, the Netherlands; Department of Neurology (O.D.), NYU School of Medicine; Atrium Healths Levine Childrens Hospital (L.A.D.), Charlotte, NC; Phoenix Childrens Hospital (T.G.), the University of Arizona College of Medicine; Division of Child Neurology and Psychiatry (D.P.), Azienda Ospedaliero Universitaria; Neurology and Epileptology Unit (I.C.), Pediatric Department, Brotzu Hospital Trust, Cagliari, Italy; Liverpool Centre for Genomic Medicine (L.G., G.R.), Liverpool Womens NHS Foundation Trust, Liverpool, United Kingdom; U.O. Genetica Medica (C.G.), Policlinico S. Orsola-Malpighi, Bologna, Italy; Department of Children's neurosciences (R.R.S.), Guys and ST. Thomas' NHS foundation trust, London United Kingdom; Department of Child Neuropsychiatry (G.C.), University of Verona, Italy; Christian Medical College (S.Y.), Vellore, India; Neurology Pediatric Unit (F.G.), Pediatric Department, Fernandes Figueira Institute, Fiocruz, Brazil; Royal Childrens Hospital (F.J.L.), Melbourne, Australia; Research & Innovation S.r.l. (D.C.), Padova; Pediatric Neurology Unit (S.O., B.S., F.V.), V. Buzzi Childrens Hospital, Milan, Italy; Department of Paediatrics (A.V.A.), London Health Science Centre/Schulich School of Medicine and Dentisty, University of Western Ontario, London, ON, Canada; Ambry Genetics (K.R.), Aliso Viejo, CA; Advocate Lutheran General Hospital (F.T.), Park Ridge, IL; PPG Pediatric Neurology (A.S.K.), Parkview Health, Fort Wayne, IN; Department of Medical Genetics (C.O.), AP-HP, Necker-Enfants Malades Hospital, Paris, France; Department of Neurology (W.B.), UC Davis, Sacramento, CA; Department of Pediatrics (K.K.), Texas A&M University Medical School, Austin; Leeds General Infirmary (S.H,), United Kingdom; Thompson River Pediatrics (A.F.), Johnstown, CO; Department of Neuropediatrics (S.G.), University Hospital Copenhagen, Denmark; Division of Neurology (F.B., R.W.), Department of Paediatrics, The Hospital for Sick Children, Toronto, Ontario, Canada; Hunter Genetics Unit, Waratah, Australia (A.R.); Wessex Clinical Genetics Service, Princess Anne Hospital, Southampton, United Kingdom (N.F., D.H.); KBO-Kinderzentrum München, Munich, Germany (M.S.); Division of Neurology, Epilepsy Neurogenetics Initiative, Childrens Hospital of Philadelphia (J.B., K.L.H., I.H., X.R.O-G, H.D.); Perelman School of Medicine, Philadelphia, PA (J.B.); PURA Syndrome Foundation, Greensborough, Australia (I.H., M.A., D.S.); PURA Syndrome Foundation, Kansas City, MO (I.H., D.S.).
1,*;
the PURA study group1