ABSTRACT
Social distancing, also referred to as physical distancing, means creating a safe distance of at least two meters (six feet) between yourself and others. This is a term popularized during the COVID-19 pandemic, as it is one of the most important measures to prevent the spread of this virus. However, the term ‘social distancing’ can be misleading, as it may imply that individuals should stop socializing. However, socializing in a safe context (i.e. over the phone, video-chat, etc.) is especially important during this time of crisis. Therefore, in this narrative review, we suggest the term ‘distant socializing’ as more apt expression, to promote physical distancing measures while also highlighting the importance of maintaining social bonds. Further, articles discussing the practice, implementation, measurement, and mental health effects of physical distancing are reviewed. Physical distancing is associated with psychiatric symptoms (such as anxiety and depression), suicidal ideation, and domestic violence. Further, unemployment and job insecurity have significantly increased during COVID-19, which may exacerbate these negative mental health effects. Governments, medical institutions, and public health bodies should therefore consider increasing mental health resources both during and after the pandemic, with a specific focus on frontline workers, COVID-19 survivors, and marginalized communities.
KEYWORDS: COVID-19, distant socializing, social distancing, physical distancing, infectious diseases, public health, mental health
Introduction
“Man is by nature a social animal; an individual who is unsocial naturally and not accidentally is either beneath our notice or more than human. Society is something that precedes the individual.” – Aristotle
According to the United States Center for Disease Control (CDC), social distancing is defined as staying ‘at least 6 feet from other people who are not from your household in both indoor and outdoor spaces’ [1]. However, the World Health Organization (WHO) opts for the term ‘physical distancing’ highlighting that, while keeping a distance of at least two meters from each other and avoiding crowded places or groups is important to stop COVID-19 transmission, ‘we can still stay socially connected while physically distant – through video, call, or text’ [2]. This is an important point to highlight, as physical distancing can have significant negative impacts on both individuals and society as a whole. In this article, we aim to examine the inevitable conflict that arises when there is both a need to maintain physical distance to prevent the spread of an infectious agent and a need to nurture social connections to mitigate the negative mental health consequences of a global pandemic. We also suggest the term ‘distant socializing’ as an alternative to social distancing, in order to highlight the need for both physical distancing and social connection during the COVID-19 pandemic, both of which are crucial for maintaining both physical and mental well-being.
Physical distancing is an important measure to prevent the spread of contagious respiratory illnesses. COVID-19 is spread through respiratory droplets and aerosols that are produced when an infected individual coughs, sneezes, and even sings, shouts, or talks. Physical distancing prevents this transmission by creating a distance between individuals that is too great for these viral particles to cross. Maintaining physical distance is shown to effectively reduce the spread of airborne viruses, even in densely populated settings, such as schools, the workplace, theaters, and sporting events [3]. Maintaining physical distance from others is an especially important measure considering that asymptomatic infected individuals can still transmit the COVID-19 virus [4].
Despite the well-established health benefits of physical distancing, many individuals do not adhere to these guidelines. There are several explanations for this: regulations are insufficiently encouraged, or community and public leaders may not model this behavior effectively. However, one of the most likely explanation is that humans, by nature, are social creatures and it is difficult for us to alter our social behaviors, despite the health consequences. Further, socialization has become even more important during the COVID-19 pandemic, when fears and anxieties are heightened. It is therefore crucial to emphasize that physical distancing and social connection are not mutually exclusive. In fact, maintaining social bonds is more important now than ever.
‘Distant socializing,’ is defined. In this review, we first explain what physical distancing means and how it is implemented. The potential mental health consequences of physical distancing are then discussed. Finally, we present the term ‘distant socializing,’ defined as maintaining social bonds at a safe distance to prevent the spread of airborne infectious diseases, as an alternative to ‘physical’ or ‘social’ distancing.
Methodology
Articles of potential interest for this narrative review were identified by searching Scopus, Web of Science, PubMed, Google Scholar, and Research Gate databases using the following search strategy: (‘social distancing’ OR ‘physical distancing’ OR ‘isolation’ OR ‘quarantine’) AND (‘COVID-19’ OR ‘coronavirus’ OR ‘pandemic’). The search was then refined by identyfing articles that discussed the practice, implementation, measurement, and mental health effects of physical distancing. Only articles written in English were considered; there was no restriction on year of publication.
Results
Physical distancing: terminology
Physical distancing and social distancing, according to the US CDC, are interchangeable terms. However, social distancing implies restricting social connections. Physical distancing, on the other hand, is less restrictive, implying only that people maintain a certain physical distance from one another [1,2]. While these terms are used synonymously, we will use the term physical distancing for the remainder of this article.
Physical distancing, quarantine, and self-isolation often used interchangeably by the general public; however, these are three distinct terms (Table 1). Physical distancing is a preventative measure, while quarantine and self-isolation are actions taken by individuals who have been, or may have been, infected. Specifically, those who have tested positive for COVID-19 and/or are showing COVID-19 symptoms engage in self-isolation, while those who may have been exposed, but do not have symptoms or a positive status, are asked to quarantine.
Table 1.
Definitions, indications, and suggestions for social distancing, quarantine, and self-isolation during the COVID-19 pandemic [5–7]
| Physical Distancing | Quarantine | Self-isolation | |
|---|---|---|---|
| Definition | Keeping a defined space between individuals to prevent viral transmission | The act of avoiding contact with all others and staying home; required for individuals who do not have symptoms but may have been exposed to an infectious disease | The act of staying home and/or in an isolation unit, and avoiding all contact with others; required for individuals who have tested positive for an infectious disease or show disease symptoms |
| Application during COVID-19 |
|
|
|
Value of physical distancing
Physical distancing reduces transmission of airborne viruses. Most government authorities and regulatory bodies recommend keeping a distance of two meters from others to prevent the spread of COVID-19 [2,6,7]. This recommendation is based on research conducted in the late 19th century, which found that visible particles containing pathogens could not travel more than two meters [8]. Since then, multiple studies have found that viral particles can actually travel much farther than this, up to eight meters in some studies [9–11]. Despite this, the two-meter rule has remained popular. However, some experts suggest that maintaining a two-meter distance is only effective when also wearing a face mask [12]. Face masks are recommended to prevent an infected individual (the mask wearer) from infecting others in their close proximity. Surgical-grade face masks have proven to be effective in preventing the transmission of COVID-19 from infected to non-infected individuals [13]. Cloth masks are less reliable and their efficacy depends on the material used, number of layers, degree of moisture in the mask, and mask fit, but they are likely useful in crowded spaces where physical distancing is not possible [14].
‘Dynamic physical distancing’ measures may also be employed. This refers to the implementation of varying degrees of physical distancing guidelines depending on the current transmission rate in a region. Specifically, more strict guidelines are enacted when transmission rates are high, to prevent over-burdening the healthcare system; while guidelines are more relaxed when rates are low, thus allowing for increased social contact and opening of select business [15,16]. This is likely to mitigate some of the detrimental economic and mental health effects of physical distancing [16].
Physical distancing is especially important under certain conditions. Firstly, when rates of transmission are very high, physical distancing is critical to prevent our healthcare system from becoming oversaturated with patients and thus only being able to provide care for a fraction of those in need [17]. Further, it is important to implement physical distancing measures in at-risk communities, such as people experiencing homelessness and individuals in nursing homes, who are at much higher risk of serious complications and death from COVID-19 than the general public [18,19]. Finally, lengthy exposure to an infected individual, poor ventilation, and indoor settings (versus outdoor) all increase risk for COVID-19 transmission and therefore physical distancing is especially important in these situations.
Physical distancing is a key factor in preventing the spread of COVID-19, but must also be employed in conjunction with proper hygiene measures. These two mitigation strategies are highlighted in Table 2.
Table 2.
Physical distancing and other hygiene measures to prevent the spread of COVID-19 and other airborne viruses
| Physical Distancing Measures | Hygiene Measures |
|---|---|
|
|
Societal responses to physical distancing
Governments and communities across the globe have had a variety of responses to the COVID-19 pandemic. While some of these responses may be culturally specific, they may also vary based on the specific needs of each country and regional transmission and death rates. Importantly, the vast majority of these responses directly promote physical distancing. Some examples of measures taken include suspension of some, or all, forms of travel in or out of a region; isolation of highly infected regions; closure of educational and religious institutions; and closure of shopping malls, civic centers, restaurants, sports arenas, and other non-essential gathering places.
Importantly, closures of these so-called ‘non-essential’ services need to be coordinated with access to ‘essential services,’ such as healthcare, sanitation services, and grocery stores. This is especially true when considering socially and economically marginalized groups, such as people living in resource-poor settings and overpopulated areas, communities with inadequate access to healthcare services, people with disabilities, and people with serious medical and/or mental illnesses. For example, when considering closing down fast-food restaurants or corner stores (often deemed ‘non-essential’ services), the government must consider if people in the community rely on these places to obtain food and other goods and if they will be able to as easily access a grocery store or pharmacy (i.e.” essential” services). Alternatives must be considered, such as not-for-profit food delivery services and additional resources for online schooling, to ensure that all people have equitable access to essential goods and services. Further, the government should consider providing funding for individuals who have faced unemployment as a result of the pandemic.
Monitoring physical distancing
With the emergence of new technologies, including artificial intelligence software, mobile apps, and drone technology, there are various potential methods for tracking individuals’ movements. Rapid tracking of contacts with infected persons helps public health professionals contain the spread of infection and provides essential data to aid governments in decision making. For example, Google has launched a website to track movements across different geographic sites to assess the impact of social-distancing measures in curbing the spread of COVID-19 [20]. These ‘community mobility reports’ are generated from anonymized location history of Google Maps users and currently cover 131 countries (google.com/covid19/mobility/). Used correctly, this data can inform government policies, such as those regarding safe business hours and delivery services. The Government of Canada has also launched an app that that can be downloaded voluntarily. This tracks users’ movements and alerts a user if they were recently in close contact with another user who reported testing positive for COVID-19.
Mental health effects of physical distancing
Despite the prophylactic benefits of physical distancing, there are also negative psychological consequences, such as increased risks of anger, anxiety, depression, fear, insomnia, loneliness, post-traumatic stress symptoms, or suicidal urges [21]. These symptoms can be largely explained by the direct effect of physical distancing in promoting social isolation. Social isolation has been identified as a risk factor for depressive symptoms, suicide attempts, and low self-esteem, particularly among adolescents [22]. In fact, the prevalence of depression symptoms has increased by 3 to 4 fold since the COVID-19 outbreak [23]. Further, likely due to its effects on the stress response, social isolation increases risk of morbidity and mortality [24].
Physical distancing also has several indirect effects that may also worsen psychological well-being. Firstly, as a result of physical distancing measures, many workplaces have shut down, either temporarily or permanently, putting many out of work. Unemployment is associated with significant psychological effects, including symptoms of depression and anxiety, substance abuse and decreased subjective well-being [25,26]. Further, with the constant uncertainty about future government restrictions, many individuals are facing perceived job insecurity, i.e. concerns about potential involuntary job loss in the future. Perceived job insecurity has psychological effects similar to those unemployment [27]. Further exacerbating this issue, the global economic impact of COVID-19 leads to further financial stress, and this may directly contribute to mental health issues [28–30].
As people are staying home more, in order to comply with physical distancing regulations, rates of domestic violence have dramatically increased. While the data on the true rate of domestic violence during the COVID-19 lockdown are still being collected, numerous countries around that world, such as the United States, Australia, China, and India, report increases in domestic violence as great as 100–200% [31,32]. In fact, it was reported by the United States National Domestic Violence Hotline that many callers have stated that their abusers are using physical distancing measures as an excuse to further restrict their access to support networks [33]. Further, the reduced hours and/or closure of many support services means survivors of domestic violence have an even more difficult time receiving psychological support. Domestic violence disproportionately affects women and children and these groups are more likely to experience long-term negative psychological effects from domestic violence [34]. Domestic violence against women is associated with depression and PTSD, as well as suicidal behavior, sleep disorders, eating disorders, and social dysfunction [35]. Further, women experiencing domestic violence are significantly more likely to have a substance use disorder; and domestic violence can exacerbate psychotic symptoms among individuals diagnosed with a psychotic disorder [35,36]. Childhood abuse is associated with development of depression, anxiety disorders, eating disorders, post-traumatic stress disorder, and substance use disorder in later life [37].
Healthcare workers are also at a heightened risk for the development of mental disorders during the COVID-19 pandemic. Medical workers in Wuhan, China, where the COVID-19 virus was first identified, have described a series of factors contributing to deterioration of mental health, such as inadequate protection against contamination, long work hours, discrimination, isolation, angry and aggressive patients, decreased contact with family, and physical exhaustion [38]. Consequently, healthcare workers report symptoms of stress, anxiety, depression, insomnia, anger, and fear [39]. Further, healthcare workers are at risk for developing post-traumatic stress disorders and burnout syndromes [40].
Historically marginalized groups may also experience more severe psychological effects of the COVID-19 pandemic. This is in large part due to the fact that minority communities are more likely to experience the negative health and socioeconomic effects of the pandemic. In countries such as the United States, Black and Latino individuals are significantly more likely than White people to contract COVID-19, and the mortality rate is twice as high for Black and Latino patients compared to white patients [41]. Further, minority groups are much less likely to have access to healthcare [41]. Latino groups were disproportionately affected by widespread unemployment as a result of the pandemic [42,43]. Minority groups are also more likely to live below the poverty line and therefore experience greater financial insecurity, which is especially burdensome during a time of employment instability [41]. All of these factors – increased disease burden, unemployment, and financial hardship – are associated with poorer mental health outcomes [25–27,44] (Table 3).
Table 3.
Issues that may contribute to decreased mental health during COVID-19
| Potential Issues | Examples |
|---|---|
| Psychological Symptoms [45,46] |
|
| Health Issues [47,48] |
|
| Interpersonal conflict and violence [32,49] |
|
| Financial stress [27,50] |
|
| News and social media [51–53] |
|
Mitigation of mental health problems associated with physical distancing
Clear and effective communication by the media and government can help to reduce fear and anxiety by decreasing the spread of misinformation and providing citizens with coherent guidelines on how to decrease the risk of transmission [54,55]. Further, public health efforts should focus on vulnerable populations, who are not only at heightened risk for contracting COVID-19, but also for experiencing negative mental health effects associated with physical distancing measures. These vulnerable populations include historically marginalized communities (e.g. Black, Latino, and Indigenous communities), economically disadvantaged communities, older adults, essential workers, and women and children (Figure 1).
Figure 1.
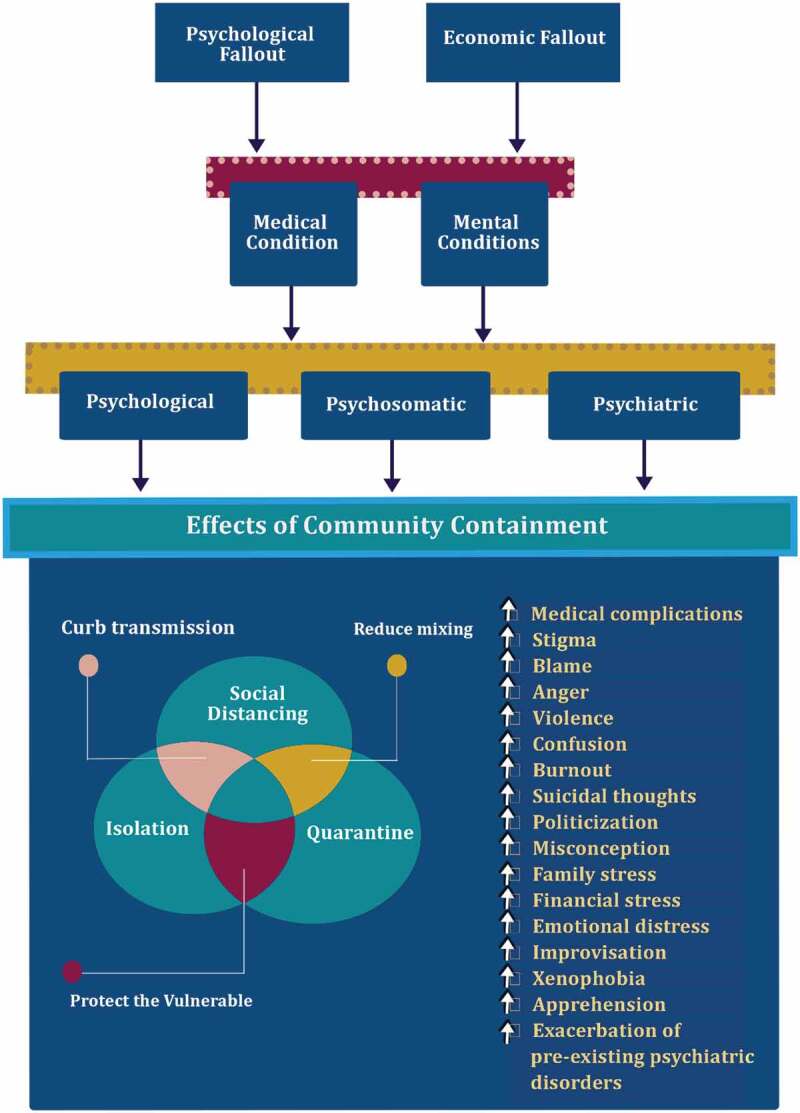
Relationship between COVID-19 physical distancing measures and mental health problems
Efforts should also be taken to address mental health concerns among patients being treated for COVID-19 and their families. For example, hospitals should consider offering training sessions for frontline staff to identify and respond to common psychological symptoms among patients with COVID-19, such as anxiety and depression [56]. Further, healthcare centers should offer psychological counseling and psychiatric services to COVID-19 patients and their family members.
Mental health services should also be offered to healthcare workers, who may also be at an increased risk of mental health issues. A good example of this is the COVID-19 psychological intervention plan developed at the Second Xiangya Hospital in the Hunan Province, China. A psychological intervention team developed online courses for staff to provide information on how to address common psychological problems; and implemented a staff mental health hotline [56]. Further, physically distanced leisure and group activities to decrease stress were provided, and rest areas for staff were created. Finally, psychological counselors regularly visited staff rest areas to provide support [56].
Discussion
The COVID-19 global pandemic has presented novel challenges for people worldwide. In order to prevent the spread of the virus, social distancing measures have been implemented in nearly every country. While this has done much to slow the spread, there have been significant psychological ramifications of these actions. The term ‘social distancing,’ used synonymously with physical distancing, implies that social contact should be limited. However, during a time of such fear and uncertainty, social relationships are more important now than ever. There are many ways in which social connections can be sustained, while also maintaining physical distance, such as via phone calls, video conferencing, or distanced outdoor meetings. Therefore, we have suggested that ‘distant socializing’ is a more appropriate term that does not imply restriction of social contacts, but rather promotes socializing in a safe and appropriate context. By changing the terminology surrounding physical distancing measures, we hope that this will promote a healthier and more sustainable approach to fighting the spread of COVID-19. Further, people may be more likely to adhere to public health guidelines if they understand that doing so must not compromise their social connections.
Physical distancing, along with handwashing and mask wearing, has consistently been shown to reduce the spread of viral particles [57–59]. However, there are many inadvertent consequences of physical distancing that can have significant societal effects. Physical distancing is associated with increased psychiatric symptomatology, suicidal ideation, and domestic violence. Historically marginalized communities and frontline workers are at heightened risk of experiencing psychological distress as a result of physical distancing measures. In order to maintain physical distance, many workplaces have shut down leading to unemployment and job insecurity. This may exacerbate the negative psychological consequences of physical distancing.
In order to mitigate the negative psychological effects of COVID-19, increased access to psychological treatment, such as counseling, should be provided to healthcare workers, and COVID-19 patients and their families. Public health measures to increase mental health information and resources for the general population, particularly historically marginalized populations, should also be considered.
The current review addresses the implementation of physical distancing and the negative mental health effects that physical distancing measures have had on countless individuals. While much data exists on the negative psychological effects of social isolation, the COVID-19 pandemic is
unprecedented and the full burden of this pandemic on mental health cannot yet be fully understood. Further, it is likely that these mental health effects will persist long after the pandemic has ended; therefore, there is still much to be learned about the mental health consequences of physical distancing during COVID-19.
Conclusions
During a global health crisis, such as the COVID-19 pandemic, the vast majority of resources are typically allocated toward drug development and physical health care. Psychiatric and psychosocial issues are often be overlooked. However, the COVID-19 pandemic has taken a toll on the mental health of countless individuals, and these effects may take longer to recover from than the virus itself. Once the pandemic has subsided, attention will need to be focused on treating these emerging mental health issues. In the meantime, when possible, measures to reduce the psychological burden of physical distancing are necessary. One important way to do this is by promoting social contact and human connection. Distant socializing is therefore an important step toward preventing the spread of COVID-19 while promoting mental health.
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the author(s).
References
- [1].Centers for Disease Control and Prevention (CDC) . Social Distancing. cdc.gov.
- [2].World Health Organization . COVID-19: physical distancing. who.int. [Google Scholar]
- [3].Ahmed F, Zviedrite N, Uzicanin A.. Effectiveness of workplace social distancing measures in reducing influenza transmission: a systematic review. BMC Public Health. 2018;18(1):518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bai Y, Yao L, Wei T, et al. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA. 2020;323(14):1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].World Health Organization . Considerations for quarantine of contacts of COVID-19 cases Interim guidance. Geneva; 2020. [Google Scholar]
- [6].Centers for Disease Control and Prevention (CDC) . COVID-19: quarantine vs. Isolation. cdc.gov.
- [7].Government of Canada . Coronavirus disease (COVID-19): prevention and risks. Canada.ca.
- [8].Flugge C. Uber Iufinfection. Z Hyg Infekt. 1987;25:179–224. [Google Scholar]
- [9].Bourouiba L. Turbulent Gas Clouds and respiratory pathogen emissions. JAMA. 2020;(323):1837–1838. [DOI] [PubMed] [Google Scholar]
- [10].Bourouiba L. A Sneeze. N Engl J Med. 2016;375(8):e15. [DOI] [PubMed] [Google Scholar]
- [11].Jones NR, Qureshi ZU, Temple RJ, et al. Two metres or one: what is the evidence for physical distancing in covid-19? BMJ. 2020;370:m3223. [DOI] [PubMed] [Google Scholar]
- [12].Setti L, Passarini F, De Gennaro G, et al. Airborne transmission route of COVID-19: why 2 Meters/6 Feet of inter-personal distance could not be enough. Int J Environ Res Public Health. 2020;17(8):2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Leung NHL, Chu DKW, Shiu EYC, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26(5):676–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Sharma S, Mishra M, Mudgal S. Efficacy of cloth face mask in prevention of novel coronavirus infection transmission: a systematic review and meta-analysis. J Educ Health Promot. 2020;9(1):192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Moyles IR, Heffernan JM, Kong JD. Cost and social distancing dynamics in a mathematical model of COVID-19 with application to Ontario, Canada. R Soc Open Sci. 2021;8(2):201770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Tuite AR, Fisman DN, Greer AL. Mathematical modelling of COVID-19 transmission and mitigation strategies in the population of Ontario, Canada. Can Med Assoc J. 2020;192(19):E497–E505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Patrick K, Stanbrook MB, Laupacis A. Social distancing to combat COVID-19: we are all on the front line. Can Med Assoc J. 2020;192(19):E516–E517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Brown KA, Jones A, Daneman N, et al. Association between nursing home crowding and COVID-19 infection and mortality in Ontario, Canada. JAMA Intern Med. 2021;181(2):229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Richard L, Booth R, Rayner J, et al. Testing, infection and complication rates of COVID-19 among people with a recent history of homelessness in Ontario, Canada: a retrospective cohort study. C Open. 2021;9(1):E1–E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Sprouse W. Google launches ‘Mobility reports’ to monitor social distancing. In: CFO. 2020. [Google Scholar]
- [21].Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hall-Lande JA, Eisenberg ME, Christenson SL, et al. Social isolation, psychological health, and protective factors in adolescence. Adolescence. 2007;42(166):265–286. [PubMed] [Google Scholar]
- [23].Ettman CK, Abdalla SM, Cohen GH, et al. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. 2020;3(9):e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Cruces J, Venero C, Pereda-Péeez I, et al. The effect of psychological stress and social isolation on neuroimmunoendocrine communication. Curr Pharm Des. 2014;20(29):4608–4628. [DOI] [PubMed] [Google Scholar]
- [25].Paul KI, Moser K. Unemployment impairs mental health: meta-analyses. J Vocat Behav. 2009;74(3):264–282. [Google Scholar]
- [26].Unemployment HD. Substance use: a review of the Literature (1990-2010). Curr Drug Abus Rev. 2011;4(1):4–27. [DOI] [PubMed] [Google Scholar]
- [27].Griep Y, Kinnunen U, Nätti J, et al. The effects of unemployment and perceived job insecurity: a comparison of their association with psychological and somatic complaints, self-rated health and life satisfaction. Int Arch Occup Environ Health. 2016;89(1):147–162. [DOI] [PubMed] [Google Scholar]
- [28].Li W, Yang Y, Liu Z-H, et al. Progression of mental health services during the COVID-19 Outbreak in China. Int J Biol Sci. 2020;(16):1732–1738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Shigemura J, Ursano RJ, Morganstein JC, et al. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74(4):281–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Shah K, Kamrai D, Mekala H, et al. Focus on mental health during the Coronavirus (COVID-19) Pandemic: applying learnings from the past outbreaks. Cureus. 2020. March 25. DOI: 10.7759/cureus.7405. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Chandra J NCW launches domestic violence helpline. The Hundu, 10 April 2020, https://www.thehindu.com/news/national/ncw-launches-domestic-violence-helpline/article31312219.ece (2020 Apr 10).
- [32].Usher K, Bhullar N, Durkin J, et al. Family violence and COVID‐19: increased vulnerability and reduced options for support. Int J Ment Health Nurs. 2020;29(4):549–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Godin M. As Cities around the world go on lockdown, victims of domestic violence look for a way out. Time. 2020. March;18. [Google Scholar]
- [34].Alejo K. Long-term physical and mental health effects of domestic violence. Themis Res J Justice Stud Forensic Sci. 2014:82-98. [Google Scholar]
- [35].Howard LM, Trevillion K, Agnew-Davies R. Domestic violence and mental health. Int Rev Psychiatry. 2010;22(5):525–534. [DOI] [PubMed] [Google Scholar]
- [36].Neria Y, Bromet EJ, Carlson GA, et al. Assaultive trauma and illness course in psychotic bipolar disorder: findings from the suffolk county mental health project. Acta Psychiatr Scand. 2005;111(5):380–383. [DOI] [PubMed] [Google Scholar]
- [37].Springer KW, Sheridan J, Kuo D, et al. The long-term health outcomes of childhood abuse. J Gen Intern Med. 2003;18(10):864–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kang L, Li Y, Hu S, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Jones NM, Thompson RR, Dunkel Schetter C, et al. Distress and rumor exposure on social media during a campus lockdown. Proc Natl Acad Sci. 2017;(114):11663–11668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Sood S. Psychological effects of the Coronavirus disease-2019 pandemic. Res Humanit Med Educ. 2020;7:23–26. [Google Scholar]
- [41].Tai DBG, Shah A, Doubeni CA, et al. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2021;72(4):703–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Fairlie R, Couch K, Xu H. The Impacts of COVID-19 on minority unemployment: first evidence from April 2020 CPS microdata. Cambridge, MA, Epub ahead of print May 2020 10.3386/w27246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Couch KA, Fairlie RW, Xu H. Early evidence of the impacts of COVID-19 on minority unemployment. J Public Econ. 2020;192:104287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Prince M, Patel V, Saxena S, et al. No health without mental health. Lancet. 2007;370:859–877. [DOI] [PubMed] [Google Scholar]
- [45].Goyal K, Chauhan P, Chhikara K, et al. Fear of COVID 2019: first suicidal case in India ! Asian J Psychiatr. 2020;49:101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Mamun MA, Griffiths MD. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian J Psychiatr. 2020;51:102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Giannis D, Ziogas IA, Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020;127:104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17–e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].World Health Organization . Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations.
- [50].McKibbin WJ, Fernando R. The Global Macroeconomic Impacts of COVID-19: Seven Scenarios, Canberra, 2020. [Google Scholar]
- [51].White AIR. Historical linkages: epidemic threat, economic risk, and xenophobia. Lancet. 2020;395(10232):1250–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Carbone M, Green JB, Bucci EM, et al. Coronaviruses: facts, myths, and hypotheses. J Thorac Oncol. 2020;15(5):675–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Pennycook G, McPhetres J, Zhang Y, et al. Fighting COVID-19 misinformation on social media: experimental evidence for a scalable accuracy-nudge intervention. Psychol Sci. 2020;31(7):770–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. [DOI] [PubMed] [Google Scholar]
- [55].Torales J, O’Higgins M, Castaldelli-Maia JM, et al. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–320. [DOI] [PubMed] [Google Scholar]
- [56].Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Zivich PN, Gancz AS, Aiello AE. Effect of hand hygiene on infectious diseases in the office workplace: a systematic review. Am J Infect Control. 2018;46(4):448–455. [DOI] [PubMed] [Google Scholar]
- [58].Howard J, Huang A, Li Z, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci. 2021;118(4):e2014564118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Fong MW, Gao H, Wong JY, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings—social distancing measures. Emerg Infect Dis. 2020;26(5):976–984. [DOI] [PMC free article] [PubMed] [Google Scholar]


