Abstract
A lateral mass screw (LMS) is one of the standard anchor screws in posterior cervical fixation. Although the advantage of cervical LMS is that it is easier and safer to place than pedicle screw, it is sometimes difficult for surgeons to confirm the exact point for screw entry and accurate angle in cases of revision surgery. When LMS fixation is performed as revision surgery after cervical laminoplasty or laminectomy, it might be complicated to secure safe placement of the LMSs. We present a simple but practical technique involving a caliper and angle device for revision surgery after cervical laminoplasty for ossification of the posterior longitudinal ligament. In this technique, the distance between the bilateral entry points is ascertained using preoperative CT. Insertion of the screw is guided using the angle device set to 25 degrees. The technique presented here is easy and allows accurate placement of the LMSs in the posterior cervical spine, and is practical even for revision surgery.
Keywords: cervical laminoplasty, lateral mass screw, ossification of posterior longitudinal ligament, revision surgery, subaxial cervical spine
Introduction
A lateral mass screw (LMS) is one of the standard anchor screws in posterior cervical fixation.1,2) There are various techniques for LMS fixation,1,3–9) which are only slightly different from each other in terms of the entry point or screw trajectory. In all the techniques, the important step is safe placement of the screw while maintaining sufficient mechanical strength. The center point of lateral mass (LM) of cervical spine is a crucial anatomical landmark. The trajectory of LMS should be controlled during its placement to avoid any neural or vascular structures. Although intraoperative image guidance is usually helpful for achieving this, it is sometimes difficult for surgeons to confirm the exact point for screw entry in cases of revision surgery. Securing safe placement of the cervical LMSs when LMS fixation is applied as revision surgery after cervical laminoplasty or laminectomy might be even more complicated and difficult than for the primary surgery, since the anatomical landmarks of osseous structures, such as spinous processes and laminae, might be lost. Furthermore, postoperative granulation and adhesion might interfere with exposure of the operative field. While wide exposure of the wound might let surgeons confirm anatomical structure, it is likely to be associated with more postoperative neck pain. In this technical note, we present our simple but practical technique using calipers and our original angle device to safely place the cervical LMSs in revision surgery after cervical laminoplasty for ossification of the posterior longitudinal ligament (OPLL).
Case Report
Surgical technique
To safely place the LMSs during revision surgery after cervical laminoplasty for OPLL, two simple surgical instruments, calipers and our original angle device are used. The caliper is a pair of dividers for detection of the midpoint of the LM (Fig. 1a and 1b). The angle device is a device that is opened at an angle of 25 degrees at its tip and is used for measurement of lateral angulation (Fig. 1c and 1d).10) The sagittal angle was adjusted toward the posterior ridge of the transverse process (Fig. 1e and 1f). The distance between the midpoint of the LMs bilaterally and the angle of the LMS at each cervical level is estimated based on preoperative axial CT images (Fig. 1g). The distance from the lateral gutter to the midpoint of the LM at each cervical level is also estimated based on preoperative axial CT images. The LM is carefully exposed partially toward the outside without excessive dissection (Fig. 1h). The laminar spacers were removed because they might interfere with the procedure of screw placement. The caliper is adjusted on the LMs bilaterally, to identify the entry points of the LMS (Fig. 1i). The exact entry point of the LMS is finally determined while making sure that the midline of each cervical spine is correctly identified. The lateral trajectory of 25 degrees is set using the angle device adjusting the vertical line hanging from the ceiling (Fig. 1j and 1k). The pilot hole is made using a 2-mm-sized diamond drill (Fig. 1l). After the cranial and caudal lateral facets are identified, elevators are carefully inserted in the bilateral facets to adjust the lateral view of fluoroscopy (Fig. 1m). The LMS are finally placed toward the posterior ridge of the transverse process (Fig. 1n and 1o). After ensuring that all the LMSs are accurately placed, the screws and rods are tightly connected (Fig. 1p). Then, autologous bone fragments are grafted onto the decorticated surface of lateral facet joints. The surgical technique presented here has been applied to a total of 16 initial or revision surgeries during the last 5 years.
Fig. 1.
Photographs showing the surgical instruments used: a caliper (a and b) and angle device (c–e). The sagittal angle is adjusted toward the posterior ridge of the transverse process (solid line) (f). Preoperative axial CT images showing the distance between the midpoint of the LMs bilaterally and the angle of the LMS at each cervical level (g). Intraoperative photographs and lateral fluoroscopic images showing the surgical steps and final construct (h–p). (h) Exposure of the LMs on both sides. (i) Identification of the entry point of LMS using a caliper. (j and k) Adjustment of the lateral trajectory. (l) Making the pilot hole using a 2-mm-sized diamond drill. (m–o): The lateral view of fluoroscopy. (p) Final construct. LMs: lateral massses, LMS: lateral mass screw.
Illustrative case
Case 1
A 58-year-old man presented with cervical myelopathy due to cervical OPLL (Fig. 2a). He underwent posterior decompression with C3-4 laminoplasty, and his neurological condition improved in the early period after surgery (Fig. 2b). However, he again demonstrated worsening of cervical myelopathy 3 months after the initial surgery probably due to the local instability of cervical spine after laminoplasty. Because external orthosis using a soft neck collar partially relieved his symptoms. Revision surgery of posterior cervical fixation at C3–5 was performed well without any trouble, and his neurological condition significantly improved postoperatively (Fig. 2c–2e). Cervical CT performed 1 year after the revision surgery showed an osseous bridge of OPLL at the beaked portion of the C3/4 level compared to the cervical CT before surgery (Fig. 2f and 2g).
Fig. 2.
Illustrative Case 1. (a) Preoperative sagittal T2-weighted MR images showing segmental type of OPLL compressing the spinal cord at the C3/4 level. (b) Postoperative sagittal T2-weighted MR images early after the first surgery showing partial posterior decompression of the spinal cord. (c) Postoperative sagittal T2-weighted MR images obtained 1 year after the second surgery showing no recurrence of compression of the spinal cord. (d) Anteroposterior cervical X-ray showing the posterior cervical fixation at C3–5. (e) Lateral cervical X-ray. (f) Sagittal cervical CT images before posterior cervical fixation showing dissociation of the OPLL at the C3/4 level. (g) Sagittal cervical CT images 1 year after posterior cervical fixation showing the osseous bridge of the OPLL at the C3/4 level. OPLL: ossification of the posterior longitudinal ligament.
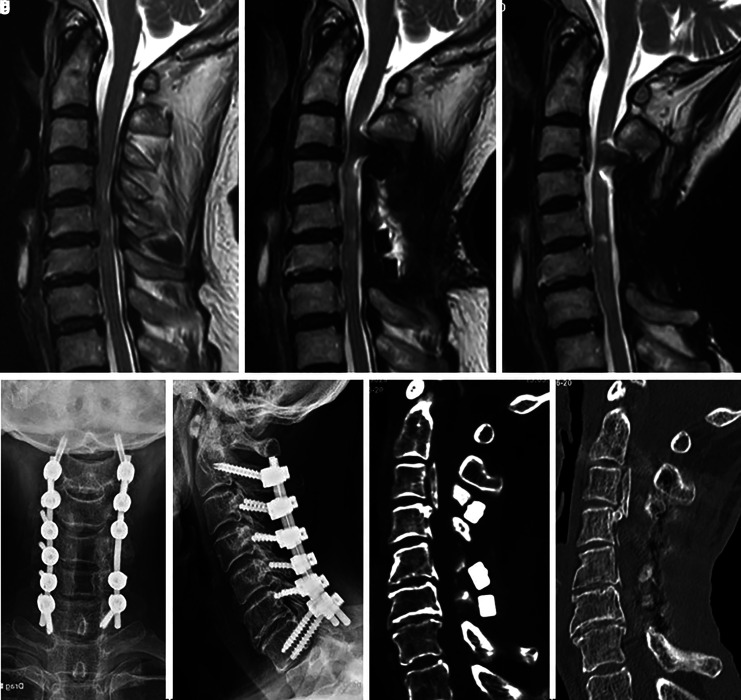
Case 2
A 73-year-old woman presented with cervical myelopathy due to cervical OPLL (Fig. 3a). She underwent posterior decompression with C3–6 laminoplasty, and her neurological condition improved in the early period after surgery (Fig. 3b). However, she subsequently demonstrated worsening of cervical myelopathy 4 months after the initial surgery probably due to the local instability of cervical spine after laminoplasty. Because external orthosis using a soft neck collar partially relieved her symptoms. Long fixation at C2–7 was selected to stabilize the cervical spine sufficiently after C3–6 laminoplasty. Revision surgery of posterior cervical fixation at C2–7 was performed without any trouble, and her neurological condition significantly improved after surgery (Fig. 3c–3e). Cervical CT performed 1 year after the revision surgery showed the osseous bridge of OPLL compared to cervical CT before surgery (Fig. 3f and 3g).
Fig. 3.
Illustrative Case 2. (a) Preoperative sagittal T2-weighted MR images showing segmental type of OPLL compressing the spinal cord at the C3/4/5/6 level. (b) Postoperative sagittal T2-weighted MR images early after the first surgery showing partial decompression of the spinal cord. (c) Postoperative sagittal T2-weighted MR images obtained 1 year after the second surgery showing no recurrence of compression of the spinal cord. (d) Anteroposterior cervical X-ray showing posterior cervical fixation at C2–7. (e) Lateral cervical X-ray. (f) Sagittal cervical CT images before posterior cervical fixation showing dissociation of the OPLL at the C3/4 level. (g) Sagittal images of cervical CT 1 year after posterior cervical fixation showing the osseous bridge of the OPLL at the C3/4 level. OPLL: ossification of the posterior longitudinal ligament.
Discussion
Since the cervical spine is basically mobile, dynamic factors sometimes cause myelopathy, especially in patients with cervical OPLL.11,12) Although posterior decompression, such as cervical laminoplasty or laminectomy, is well performed in the majority of cases of cervical OPLL, cervical arthrodesis is sometimes necessary even after the initial surgery of posterior decompression. Revision surgery of posterior cervical fixation is another option in such situations. For posterior cervical fixation, the LMS, pedicle screw, intralaminar screw, or transarticular screw can be available as anchor screws.1,2,13) Among them, LMS is commonly used as a safer anchor for the cervical spine and is technically easier to place than the pedicle screw.8,9,14) There are various techniques for the safe placement of LMSs (Table 1).1,3,9) Although the techniques differ slightly from each other, they share basic concepts in terms of screw entry and trajectory. Surgeons need to recognize the LM as a rectangle.8) The superior and inferior borders of the LM are formed by the cranial facet joint and caudal facet junction, respectively. The medial border of the LM is the junction between the lamina and lateral facet, and the lateral border of the LM is the lateral edge of the lateral facet. When exposing the lateral border, wide exposure to the outer edge of the LM, which feels like a cliff, is necessary.8,9) This allows surgeons to detect the midpoint of the LM under direct vision. However, recognition of the anatomical structure of the LM might be difficult in cases of revision surgery after cervical laminoplasty or laminectomy, because anatomical osseous landmarks are partially lost. In these cases, use of an intraoperative navigation system is now a practical solution. However, when bony structures, such as the spinous processes, where the reference arc of the navigation system should be placed, have been excised during the initial surgery, we have no choice but to set the reference arc at a location far from the level of vertebral fixation. In such a situation, accuracy of the navigation system cannot be guaranteed. The technique presented here can be applied safely even for the revision surgery not only after cervical laminoplasty for OPLL but also after wide laminectomy.
Table 1. Details of previously reported LMS fixation techniques.
| Technique | Year | Entry point | Lateral angulation | Sagittal angulation |
|---|---|---|---|---|
| Roy-Camille3) | 1989 | Midpoint of the LM | 10° lateral | 90° to the LM surface |
| Louis7) | 1991 | At the intersection of a vertical line 5 mm medial to the lateral edge of the facet joint and a horizontal line 3 mm below the inferior edge of the facet joint line above | Straight ahead, no lateral angulation | 90° to the LM surface |
| Magerl6) | 1991 | 1 mm medial and 1 mm cranial to the midpoint of the LM | 20–30° lateral | Parallel to the adjacent facet joints |
| Anderson5) | 1991 | 1 mm medial to the midpoint of the LM | 10° lateral | 30–40° in a cephalad direction (also parallel to the facet joint) |
| An4) | 1991 | 1 mm medial to the midpoint of the LM | 30° lateral | 15° of cephalad angulation |
| Kim8) | 2012 | 1 mm medial to the midpoint of the LM | 24–30° lateral | Parallel to the angle of the spinous process |
| Riew1) | 2018 | 1 mm medial and 1 mm caudal to the midpoint of the LM | Aim toward the upper and outer corner of the LM | Aim toward the upper and outer corner of the LM |
| Rathinavelu9) | 2020 | 2 mm lateral to the medial border of the LM and 2 mm above the inferior facet joint | Aim toward the upper and outer corner of the LM | Aim toward the upper and outer corner of the LM |
LM: lateral mass, LMS: lateral mass screw.
Avoidance of vertebral artery injury
During the placement of LMSs, there is a potential risk of neural or vascular injury, in particular, iatrogenic injury of the vertebral artery (VA) potentially resulting in catastrophic outcomes.2,15,16) Although Seybold et al.17) have reported a VA injury rate of 5.8% with bi-cortical screw placement in a cadaveric study, the prevalence rate reported in clinical studies is negligible.9,18,19) However, Cho et al. reported a case of VA injury presenting with infarction of the cerebellum and brain stem.20) Kim et al. reported that the rate of transverse foramen violation without VA injury rate is 0.9%, with the highest incidence rate at the level of C6 (54%).21) Hence, iatrogenic injury to the VA during the procedure of LMS fixation cannot be ignored. The transverse foramen is in line with the midpoint of the LM.22) Control of lateral angulation is, therefore, a key procedure to avoid VA injury. Merola et al. have shown that the 20–30 degrees lateral angulation in the Roy-Camille method, Anderson method, and Magerl method is mandatory for preventing neurovascular injury.15) Therefore, there is good evidence that a minimum 20 degrees of lateral angulation of the LMS provides a reliable degree of safety. On the other hand, lateral angulation of the LMS of more than 30 degrees might cause fracture of the LM.10) Hence, we used 25 degrees lateral angulation of the LMS in our technique.10) However, it is difficult to accurately estimate a 25-degree angle intraoperatively, because precision of the angle depends on visual estimation by the surgeon. The angle device presented here is easy to use and practical for obtaining safe control of lateral angulation of the LMS, in order to avoid iatrogenic injury to the VA or LM fracture.
Avoidance of nerve root injury
Sagittal angulation of the LMS is also crucial for avoiding the risk of nerve root injury or facet joint violation.1,17) Excessively long screws might cause impingement of the nerve root exiting above.1) Xu et al. have reported that the potential risk of nerve root injury is higher with the Magerl (95%) and Anderson (90%) techniques than with the An (60%) technique, based on differences in the exit point of the LMS.16) Although a cadaveric study suggested a relatively high incidence of nerve root injury, the actual incidence in clinical studies is quite low (0.6–1.8%).18,23–25) To avoid nerve root injury, the exit point of the LMS should not be located on the cranial side of the transverse process. Hence, we aim toward the posterior ridge of the transverse process under lateral fluoroscopic imaging, as in the An technique (Fig. 1f).18) Additionally, in order to avoid excessively long screws, we recommend the use of 14 mm long screws in Japanese patients to avoid nerve injury.10)
Conclusion
The use of surgical calipers and an angle device enables safe placement of the LMS in revision surgery after posterior decompression and cervical laminoplasty for cervical OPLL. In revision surgery, appropriate determination of the entry point and angle of the LMS without excessive dissection of the LM is desirable. The technique presented here is easy and allows accurate placement of the LMSs in the posterior cervical spine; additionally, it is practical even for revision surgery.
Conflicts of Interest Disclosure
All authors report no conflicts of interest concerning the materials or methods used in this study or the findings specified in this paper. All authors who are members of The Japan Neurosurgical Society (JNS) have registered online Self-reported COI Disclosure Statement Forms through the website for JNS members.
References
- 1).Joaquim AF, Mudo ML, Tan LA, Riew KD: Posterior subaxial cervical spine screw fixation: a review of techniques. Global Spine J 8: 751–760, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Joaquim AF, Tan L, Riew KD: Posterior screw fixation in the subaxial cervical spine: a technique and literature review. J Spine Surg 6: 252–261, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Roy Camille R, Salient G, Mazel C: Internal fixation of the unstable cervical spine by a posterior osteosynthesis with plates and screws, in The Cervical Spine Research Society (ed): The Cervical Spine, ed 2. Philadelphia, JB Lippincott, 1989, pp 390–403 [Google Scholar]
- 4).An HS, Gordin R, Renner K: Anatomic considerations for plate-screw fixation of the cervical spine. Spine (Phila Pa 1976) 16: S548–S551, 1991 [DOI] [PubMed] [Google Scholar]
- 5).Anderson PA, Henley MB, Grady MS, Montesano PX, Winn HR: Posterior cervical arthrodesis with AO reconstruction plates and bone graft. Spine (Phila Pa 1976) 16: S72–S79, 1991 [DOI] [PubMed] [Google Scholar]
- 6).Jeanneret B, Magerl F, Ward EH, Ward JC: Posterior stabilization of the cervical spine with hook plates. Spine (Phila Pa 1976) 16: S56–S63, 1991 [DOI] [PubMed] [Google Scholar]
- 7).Nazarian SM, Louis RP: Posterior internal fixation with screw plates in traumatic lesions of the cervical spine. Spine (Phila Pa 1976) 16: S64–S71, 1991 [DOI] [PubMed] [Google Scholar]
- 8).Kim SH, Seo WD, Kim KH, Yeo HT, Choi GH, Kim DH: Clinical outcome of modified cervical lateral mass screw fixation technique. J Korean Neurosurg Soc 52: 114–119, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Rathinavelu S, Islam A, Shivhare P, Chatterjee S: Lateral mass screw fixation in the cervical spine: introducing a new technique. Asian Spine J Epub 2020 Nov 16. ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Shimokawa N, Fu Y, Tsukazaki Y, Sugino T, Ikeda H, Urano Y: [Lateral mass screw fixation for stabilization of the middle and lower cervical spine: Avoidance and management of complications]. Spinal Surg 23: 6–10, 2009 (Japanese) [Google Scholar]
- 11).Johnson R: Anatomy of the cervical spine and its related structures, in Torg JS.(ed): Athletic Injuries to the Head, Neck, and Face, ed 2. St Louis, MO: Mosby Year Book, 1991, pp 371–383 [Google Scholar]
- 12).Shimokawa N, Sato H, Matsumoto H, Takami T: Review of radiological parameters, imaging characteristics, and their effect on optimal treatment approaches and surgical outcomes for cervical ossification of the posterior longitudinal ligament. Neurospine 16: 506–516, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Shimokawa N, Takami T: Surgical safety of cervical pedicle screw placement with computer navigation system. Neurosurg Rev 40: 251–258, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Mohamed E, Ihab Z, Moaz A, Ayman N, Haitham AE: Lateral mass fixation in subaxial cervical spine: anatomic review. Global Spine J 2: 39–46, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Merola AA, Castro BA, Alongi PR, et al. : Anatomic consideration for standard and modified techniques of cervical lateral mass screw placement. Spine J 2: 430–435, 2002 [DOI] [PubMed] [Google Scholar]
- 16).Xu R, Haman SP, Ebraheim NA, Yeasting RA: The anatomic relation of lateral mass screws to the spinal nerves. A comparison of the Magerl, Anderson, and An techniques. Spine (Phila Pa 1976) 24: 2057–2061, 1999 [DOI] [PubMed] [Google Scholar]
- 17).Seybold EA, Baker JA, Criscitiello AA, Ordway NR, Park CK, Connolly PJ: Characteristics of unicortical and bicortical lateral mass screws in the cervical spine. Spine (Phila Pa 1976) 24: 2397–2403, 1999 [DOI] [PubMed] [Google Scholar]
- 18).Heller JG, Silcox DH, Sutterlin CE: Complications of posterior cervical plating. Spine (Phila Pa 1976) 20: 2442–2448, 1995 [DOI] [PubMed] [Google Scholar]
- 19).Wellman BJ, Follett KA, Traynelis VC: Complications of posterior articular mass plate fixation of the subaxial cervical spine in 43 consecutive patients. Spine (Phila Pa 1976) 23: 193–200, 1998 [DOI] [PubMed] [Google Scholar]
- 20).Cho KH, Shin YS, Yoon SH, Kim SH, Ahn YH, Cho KG: Poor surgical technique in cervical plating leading to vertebral artery injury and brain stem infarction–case report. Surg Neurol 64: 221–225, 2005 [DOI] [PubMed] [Google Scholar]
- 21).Kim HS, Suk KS, Moon SH, et al. : Safety evaluation of freehand lateral mass screw fixation in the subaxial cervical spine: evaluation of 1256 screws. Spine (Phila Pa 1976) 40: 2–5, 2015 [DOI] [PubMed] [Google Scholar]
- 22).Ebraheim NA, Xu R, Yeasting RA: The location of the vertebral artery foramen and its relation to posterior lateral mass screw fixation. Spine (Phila Pa 1976) 21: 1291–1295, 1996 [DOI] [PubMed] [Google Scholar]
- 23).Heller JG, Carlson GD, Abitbol JJ, Garfin SR: Anatomic comparison of the Roy-Camille and Magerl techniques for screw placement in the lower cervical spine. Spine (Phila Pa 1976) 16: S552–S557, 1991 [DOI] [PubMed] [Google Scholar]
- 24).Graham AW, Swank ML, Kinard RE, Lowery GL, Dials BE: Posterior cervical arthrodesis and stabilization with a lateral mass plate. Clinical and computed tomographic evaluation of lateral mass screw placement and associated complications. Spine (Phila Pa 1976) 21: 323–328; discussion 329, 1996 [DOI] [PubMed] [Google Scholar]
- 25).Deen HG, Birch BD, Wharen RE, Reimer R: Lateral mass screw-rod fixation of the cervical spine: a prospective clinical series with 1-year follow-up. Spine J 3: 489–495, 2003 [PubMed] [Google Scholar]