Abstract
Since the COVID-19 pandemic started, countries have enacted a series of non-clinical preventive mechanisms aimed at slowing the rate of spread. However, these mechanisms can be effective only when they are correctly followed and only when individuals believe the risk of COVID-19 is high enough to warrant following them. As risk perceptions decline, individuals are more likely to relax following preventive measures and the rate of spread might increase. This study assesses the determinants of changes in perceptions of COVID-19 risk and the determinants of adherence to preventive measures in Uganda. Logistic regression results show that age, access to information and being supportive of preventive measures strongly predicts keeping higher risk perceptions and adhering to preventive actions. Qualitative results show that risk perceptions are also influenced by economic stress, citizens’ level of confidence in the government, local political climate and the extent of proliferation of misinformation about COVID-19.
Keywords: COVID-19, Risk perception changes, Preventive measures, Uganda
Introduction
In responding to the fast-spreading COVID-19 virus, governments imposed non-clinical pandemic control policies such as social distancing, lockdowns and curfews. Evidence suggests that these measures curtailed the fast spread of the virus [1,2]. However, these measures also were associated with worsening socioeconomic conditions [3] and associated mental health challenges and fatigue [4,5]. Studies around the world have shown that where higher risk perceptions existed, knowledge and attitudes towards prevention and containment were high [6]. However, some section of the population still espouse low-risk perceptions and prevention mechanisms [7].
As the pandemic drags on and prevention policies double down in the more deadly second and third waves, change in risk perceptions will be expected as economic [3] and social anxiety [8] increase. Moreover, the increase in misinformation [9,10] is likely to further negatively affect adherence to prevention strategies. This has been the experience in previous pandemics [11]. While many studies have investigated knowledge, actions and practices (KAP) during the coronavirus pandemic [12], fewer studies have investigated whether perceptions about the pandemic negatively change given the increase in pandemic fatigue [13]. Moreover, changing perceptions might derail the progress made on prevention and curtailing the spread. Developing countries – especially those in which previous pandemics exposed health systems weaknesses-would be at higher risk [14] further underscoring the necessity of positive risk perceptions and prevention.
In this study, we focus on Uganda. We are interested in two main questions. First, we study the correlates of adherence to preventive strategies set by the government. One study in this regard is Amodan et al. [15] who assessed the determinants of adherence to preventive measures in Uganda. Secondly, we assess the correlates of change in risk perceptions of COVID-19. Using an internet survey, we qualitatively and quantitatively highlight the extent of mostly negative perception changes and adherence to preventive strategies. We find that access to information, local political aand economic situations influence how people perceive the risk of COVID-19 and their patterns of adhering to preventive actions. We find some indication of misinformation proliferation, but also notice that experience of previous epidemics provides individuals with reference points to build trust in the health system. Section 2 provides a brief background of COVID-19 in Uganda and methods and data analysis strategy are in Section 3. We provide results in Section 4, elaborate on them in discussion Section 5 and conclude with Section 6.
COVID-19 in Uganda
Uganda registered her first COVID-19 case on 21 March 2020 and by January 2021 had registered close to 40,000 cases and over 320 deaths. To curtail the spread, the country implemented lockdown and social distancing strategies from March 2020[16]. Though the country's case burden remains and is predicted to remain low [17], the economic effects have been deeply regressive. In rural Uganda, non-farm income declined by 60 percent [18] and increasing food insecurity was recorded among a greater share of the population [19]. While knowledge, attitudes and practices about COVID-19 were higher among Ugandans[12], some cohorts of the population registered various harmful misconceptions [20] that might affect adherence to prevention strategies. In 2020, Uganda also had election campaigns for the January 2021 general elections and individuals were more likely to renege on standard prevention mechanisms during campaign events. The country, therefore, presented an appropriate opportunity to study adherence and perceptions changes that would be very useful for other countries. Moreover, Uganda has had several outbreaks of haemorrhagic fevers in the last two decades [21], which were successfully handled before they became full-fledged epidemics [22]. It is argued that Uganda's model of pandemic response can be helpful to other countries of low resource settings [23].
Methods
Data
The study, therefore, sought to establish four key issues; namely (1) the extent of adherence to preventive strategies, (2) determinants of adherence to prevention strategies, (3) extent of negative changes in risk perceptions between March when the first case was recorded and July 2020, three months into the pandemic in the country and (4) determinants of perception changes. In one dimension, we contribute to research elaborating on adherence to prevention mechanisms in Uganda [12]. However, this goes further to assess the extent to which individuals change perceptions from higher risk to lower risk perceptions.
To study these questions, we used a self-administered public opinion survey conducted in Uganda. The survey was run online on the Survey Monkey platform and circulated on Twitter, Facebook and WhatsApp between 6th and 15th July 2020. As an incentive for participation, respondents were entered into a raffle draw to win internet bundles. Altogether, 1353 individuals responded. In this analysis, we use 1195 observations for which all the relevant information was present.
Analysis
Our main analysis deduces from two main questions. To assess the extent of change in perceptions, respondents answered the following question. “How much do you fear the COVID−19 disease now (July) compared to how you felt in March” The responses were 1 = “I fear COVID−19 less now (July) than I did in March” and 0 = “I fear COVID−19 more now (July) than I did in March”. Individuals responding that they feared the diseases less in July than they did in March 2020 would then provide a proxy reduced risk aversion and hence a negative change in perceptions regarding the risk posed by COVID-19. To establish the level of adherence to prevention strategies imposed by the governments, we asked respondents the question “How serious are you about following COVID -19 rules like physical distancing and wearing a mask?” The question had four responses categorised as 1= very relaxed, 2 = somewhat relaxed, 3= somewhat serious and 4 = very serious. At the analysis level, we recorded the responses to this question into a dummy variable corresponding to 1= seriously following COVID-19 rules and 0= otherwise (relaxed about following the rules). Since both questions were binary outcomes, we implemented two separate logistic regressions of the following form.
Where was a binary outcome (ie. a) fear of COVID-19 to capture a change in risk perceptions between March and July 2020 and b)adhrence to preventive mechanisms) for individual i. is a vector of covariates and is the error term. In the two logistic regressions, we control for age, gender, education level, household expenditure, and information access, employment status represented by two dummy variables for formal sector and self-employment and a dummy of working from home. We also control for the perception of how helpful presidential COVID-19 addresses on television were, relief support from the government, level of approval of lockdown and curfew prevention mechanisms. We also include regional dummies to account for geographical variation. We report 95% confidence intervals and robust standard errors. Summary results are in Supplementary Tables 1 and 2 for the two outcomes respectively.
The questionnaire also provided space for individuals to give reasons why they responded as they did concerning their perceptions of COVID-19 fear/ risk. We extracted this qualitative data and using simple thematic analysis, we analyse it to accompany quantitative analysis.
Results
Descriptive and qualitative results
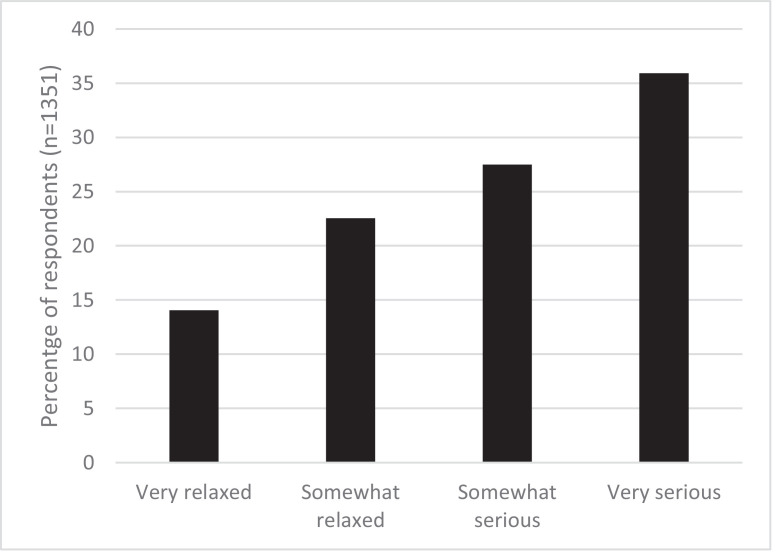
First, we show the results of adherence to COVID-19 prevention strategies. The strategies assessed in this study were social distancing and masque-wearing. Fig. 1 below shows the descriptive results of how seriously people considered preventive measures. We found that just over 63% of the respondents self-reported that they were seriously adhering to COVID-19 regulations. A large proportion of respondents (36.6%) reported that they were not adhering to these regulations, indicating they were either very relaxed or somewhat relaxed.
Fig. 1.
Adherence to COVID-19 preventive mechanisms (social distancing and masque-wearing).
Secondly, we assessed the prevalence of perception changes. Out of 1323 individuals who responded to the question, 85% feared COVID-19 less in July than they did in March 2020. While not all the perception change is a true reflection of an increase in risk loving and less prevention, it is a very close proxy. The question provided an option for respondents to give a reason why they felt the way they did in regards to fear of COVID-19. About 8.5% (102 respondents) provided this additional qualitative data. Incorporating this qualitative data, we confirm that a change in perceptions is most likely negative and makes individuals feel less COVID-19 risk. We coded each of the 102 qualitative responses on how much they were negative (less preventive behavior) neutral or positive (more preventive behavior) perception changes. Sixty-one percent had negative perception changes compared to only 10 percent whose perceptions were more positive, more risk-averse and hence predictive of higher prevention actions.
Looking into the qualitative reasons why individuals changed perceptions, with a few selected and informative quotations from the respondents, we highlight some of them. First, COVID-19 in Uganda was associated with sharp declines in living standards, income losses and increasing food insecurity [18,19]. It therefore seems the dire economic situation was more prominent in individuals’ risk assessment than the risk of the disease. One respondent put it:
“I don't fear it anymore. The current situation has proven that we need to coexist with it because people are dying from mental illnesses, police brutality, lack of food and access to health care services instead.” Female respondent – 18–25 years
The statement by this respondent also pointed to an important theme of the politics of pandemic response and how that affected how individuals think about the pandemic. In some countries, governments have used the pandemic as a toll for increased marginalization of some sub-groups [24]. In Uganda, the pandemic response would not be separated from the politics of a very heated election season. Military and police brutality were observed with military and police enforcing regulations [25,26] including the November 2020 events in which at least 50 individuals lost their lives [27]. Several respondents, therefore, felt that the risk associated with militarised pandemic response was possibly higher than of the disease itself. One male, aged between 26 and 34 years inferred that:
“I fear the local defence unit (LDU) more than COVID-19.”
Agreeing with another male in the same age group who also commented that
“I fear hunger, poverty and death by LDU more than COVID-19″ Male, 26–34 years
However, while some individuals might have become apathetic due to the militarisation of the pandemic response, others were equally dispirited by the politicisation of response, especially concerning corruption and misuse of pandemic resources. Two male respondents between 26 and 34 years had this to say.
“COVID -19 is no more - it's a business venture for the people that depend on pandemic economics.”
“I now don't even fear COVID -19 at all. A lot has caused apathy because of the mismanagement of resources and repugnant directives that have impoverished us the more.”
A female respondent between 35 and 44 years also intimated that:
“I know COVID -19 exists but the Ugandan government is taking undue advantage of it.”
Corruption in Uganda's health sector [28] and in general is well documented [29]. The low expectation of pandemic management from a financial governance perspective, therefore, gives individuals less belief that the pandemic itself is dangerous if it can be used for economic gain.
The other reason for the negative perception changes is the relatively low case numbers in Uganda and Africa at large. Low COVID-19 mortality and morbidity have increasingly become a puzzle [30,31]. The outcome of this in individual prevention behavior and practices is that individuals and policymakers might develop complacency in pandemic management strategies. Because many individuals would not have encountered COVID-19 casualties in their social networks, their behaviour towards prevention would have regressed. We find this to be the case among some people in our sample. One young female respondent said:
“Am not scared anymore because I don't see anyone dying, or no one in Uganda coming out to say how it all was, usually there are people among the many who will come out to speak sincerely and tell people to keep safe.” Female respondent, 18–25 years
This respondent agreed with another, who said:
“I don't fear it all coz I don't believe in its existence anymore in Uganda, after all, I heard from the victims said to be positive not being sick at all.” Male respondent, 26–34 years
At worst, the effect of such complacency has been the flourishing of misinformation and fake news about the actual existence of the disease or those whom it affects. One respondent said:
“This COVID-19 thing or disease is a scam. People die every day of other diseases, but no one has died of COVID-19. It is just one of the ploys they use to make Ugandans poorer.” Male respondent, 35–44 years.
Another one added:
“I don't fear COVID-19; I am very convinced that it might even be a hoax.” Female respondent, 26–34 years.
However, not all perception change is negative. We observed positive perception change in about 10% of those who provided additional qualitative statements. This was close to the general question on perception change in which 14 percent indicated that they feared COVID-19 more in July than they did in March. Two key themes seem to influence positive perception changes that induce more behavior that is protective. The first is confidence in the health system, especially regarding its experience with handling previous viral diseases such as Ebola and Marburg virus outbreaks [22]. The success in handling previous Ebola and Marburg viruses not only provided best practices for other low resource countries [32] but also should potentially lay the ground for management of current and future pandemic outbreaks [33]. Some individuals felt confident that COVID-19 was and would continue to be handled successfully. One respondent commented:
“On the contrary, I have not approached COVID-19 with any level of fear either before or now; I do appreciate that it's a disease whose prevention and precautions experts have made known to us. I have learned to live with the disease rather than fear” Male respondent, 35–44 years.
While another added:
“We have faced many epidemics before and I knew this would also pass, I don't fear COVID-19″ Female respondent, >45 years.
Another respondent pointed to the communication from local scientists about the possible broader effects of COVID-19.
“I still do (fear COVID-19) considering the research shared by Makerere University on its effects on organs like lungs.” Female respondent, 35–44 years.
The second theme is continued vigilance with self-protection. Individuals who did not negatively change their perception also showed more adherence to self-protective preventive behavior. One respondent wrote:
“I don't fear COVID-19 but I have made sure I use my masque where necessary. I have sanitised my hands where necessary and made sure I am always clean, my environment is clean and my entire household is very clean all the time and I make sure I avoid crowds and I wash my hands all the time with clean water and clean soap.” Female respondent, 35–44 years.
These qualitative results reveal a couple of things. First, there is some substantial misinformation in developing countries about COVID-19. While this study does not seek to establish the level of misinformation, other studies in countries like Uganda find high levels of misinformation [34,35]. There is a high likelihood that such misinformation is increasing risky behavior and non-adherence to preventive strategies. Secondly, we learn that political and socio-economic reasons are likely to increase pandemic apathy. This is more so in countries like Uganda that are characterized by reduced civic space, electoral seasons and pre-existing high levels of corruption and less government trust. However, we also note that there are still some islands of hope for individuals’ faith in the health system, especially building on experiences from the previous management of viral haemorrhagic fevers.
Logistic regression results
We report results from two logistic regression models in Table 1 . Odds ratios are presented with 95% confidence intervals.
Table 1.
Logistic regression results.
| (1) | (2) | |||
|---|---|---|---|---|
| Fear COVID-19 less | Adherence to COVID-19 prevention | |||
| VARIABLES | Odds ratio | 95% CI | Odds ratio | 95% CI |
| Age group | ||||
| 26–34 | 0.644 | (0.349 - 1.187) | 1.408* | (0.960 - 2.067) |
| 35–44 | 0.469⁎⁎ | (0.229 - 0.961) | 1.902⁎⁎ | (1.165 - 3.104) |
| >=45 | 0.327⁎⁎⁎ | (0.159 - 0.672) | 2.569⁎⁎⁎ | (1.387 - 4.758) |
| Gender (1=female, 0=Male) | 0.917 | (0.615 - 1.368) | 1.352⁎⁎ | (1.002 - 1.824) |
| Education level (1= Secondary and above) | 0.973 | (0.612 - 1.549) | 0.956 | (0.675 - 1.354) |
| Household Monthly expenditure (in UgX) Household Monthly expenditure (in UgX) (base >200,000 | ||||
| 201,000 - 800,000 | 1.069 | (0.645 - 1.772) | 0.814 | (0.570 - 1.163) |
| 801,000 - 2000,000 | 0.905 | (0.478 - 1.715) | 0.809 | (0.507 - 1.292) |
| >=2001,000 | 0.939 | (0.438 - 2.011) | 1.072 | (0.609 - 1.889) |
| COVID News intensity | ||||
| About once a week | 0.427 | (0.084 - 2.165) | 0.717 | (0.346 - 1.488) |
| A few times a week | 0.427 | (0.097 - 1.881) | 1.131 | (0.627 - 2.038) |
| Daily | 0.217⁎⁎ | (0.053 - 0.882) | 2.066⁎⁎⁎ | (1.211 - 3.524) |
| Several times a day | 0.205⁎⁎ | (0.049 - 0.854) | 1.783⁎⁎ | (1.039 - 3.060) |
| Uses social media | 1.168 | (0.690 - 1.976) | 0.850 | (0.537 - 1.345) |
| Uses traditional media | 0.587* | (0.332 - 1.039) | 1.058 | (0.740 - 1.512) |
| Job type (base: not employed) | ||||
| Formal sector | 1.505* | (0.937 - 2.416) | 1.077 | (0.758 - 1.528) |
| Informal sector | 1.046 | (0.552 - 1.981) | 1.140 | (0.703 - 1.849) |
| Self employed | 1.070 | (0.629 - 1.819) | 1.158 | (0.778 - 1.726) |
| Job loss | 0.880 | (0.600 - 1.289) | 0.949 | (0.726 - 1.240) |
| Presidential addresses | 0.429 | (0.131 - 1.406) | 1.460 | (0.872 - 2.445) |
| Received food aid | 0.944 | (0.600 - 1.484) | 0.888 | (0.635 - 1.241) |
| Approval of lockdown policy (base: strongly disapprove) | ||||
| Disapprove | 2.899 | (0.814 - 10.325) | 0.925 | (0.465 - 1.839) |
| Not sure | 2.794 | (0.795 - 9.818) | 1.649 | (0.813 - 3.347) |
| Approve | 1.371 | (0.520 - 3.616) | 2.143⁎⁎ | (1.167 - 3.936) |
| Strong approve | 0.937 | (0.368 - 2.385) | 2.242⁎⁎⁎ | (1.226 - 4.099) |
| Approval of curfew measures (base: strongly disapprove) | ||||
| Disapprove | 0.805 | (0.372 - 1.742) | 1.687⁎⁎⁎ | (1.174 - 2.424) |
| Not sure | 0.203⁎⁎⁎ | (0.088 - 0.468) | 2.779⁎⁎⁎ | (1.628 - 4.742) |
| Approve | 0.331⁎⁎⁎ | (0.157 - 0.695) | 3.612⁎⁎⁎ | (2.361 - 5.527) |
| Strong approve | 0.201⁎⁎⁎ | (0.096 - 0.421) | 6.109⁎⁎⁎ | (3.745 - 9.967) |
| Central Uganda | 1.695 | (0.516 - 5.572) | 1.256 | (0.492 - 3.211) |
| Eastern Uganda | 3.065* | (0.941 - 9.980) | 1.008 | (0.417 - 2.441) |
| Kampala, Wakisoor Mukono | 3.035⁎⁎ | (1.051 - 8.766) | 0.813 | (0.375 - 1.764) |
| Northern Uganda | 3.409* | (0.972 - 11.961) | 1.450 | (0.523 - 4.023) |
| Western Uganda | 1.831 | (0.590 - 5.682) | 0.743 | (0.309 - 1.789) |
| Constant | 101.619⁎⁎⁎ | (12.952 - 797.308) | 0.151⁎⁎⁎ | (0.044 - 0.516) |
| Observations | 1177 | 1181 | ||
| Mean VIF | 4.26 | 4.24 | ||
| Pseudo R-squared | 0.167 | 0.159 | ||
95% confidence intervals in parentheses with robust standard errors.
p < 0.01,.
p < 0.05,.
p < 0.1.
Correlates of changing (negatively) perceptions about COVID-19 risk
First, we highlight the correlates of a likely negative change in perceptions about COVID-19 between March and July 2020. Older individuals were less likely to change their perception of COVID-19 seriousness between March and July 2020. Respondents between 35 and 44 years had 53 percent fewer odds (OR 0.469; 95% CI 0.229–0.961) while those higher than 45 years had 67 percent fews odds (OR 0.327; 95% CI 0.159–0.672) of changing perceptions on COVID-19 risk compared to the younger 18-25 years age group.
Secondly, receiving COVID-19 related news decreased the odds of changing perceptions. This was especially true for individuals receiving more of their news from traditional news platforms such as television, radio and newspapers. Individuals receiving COVID-19 related news at least daily had close to 80% fewer odds of changing their perceptions (OR 0.217; 95% CI 0.053–0.882) as were those receiving news several times a day (OR 0.205; 95% CI 0.049 - 0.854). Receiving news through traditional news channels was associated with more than 40% fewer odds of negatively altering their perceptions (OR 0.587; 95% CI 0.332–1.039). Regarding the influence of economically challenging preventive strategies such as lockdown and curfew policies, individuals approving curfew measures were less likely to change perceptions. Compared to those who strongly disapproved of curfew measures, odds of changing perception reduced along the measures’ approval trajectory. Specifically, those indifferent about curfew measures had 80% lower odds (OR 0.203; 95% CI 0.088–0.468), those in approval had 67% lower odds (OR 0.331; 95% CI 0.157–0.695) and those who strongly approved of the measures had about 80% lower odds (OR 0.201; 95% CI 0.096–0.421) of changing perceptions.
One key factor that increased the odds of changing perception – employment in the formal sector. Employment in the formal sector, compared with not having a job, was associated with more than 50% higher odds of negatively changing perceptions (OR 1.505; 95% CI 0.937–2.416). Across the regions, higher odds of perception changes were observed in Eastern and Northern regions and areas in and around the capital, Kampala.
Correlates of following prevention regulations
Model 2 reports results of correlates of following COVID-19 preventive measures. Specifically, the preventive measures assessed were practising social distancing and regularly using facemasks. As with changing perceptions of COVID-19 risk, older individuals were more likely to adhere to preventive measures than younger individuals. Compared to younger individuals between 18 and 25 years, individuals between 26 and 34 years, 35 and 44 years and those above 45 years had 1.4 (OR 1.408; 95% CI 0.960–2.067), 1.9 (OR 1.902; 95% CI 1.165–3.104) and over 2.5 times (OR 2.569; 95% CI1.387–4.758) respectively higher odds of adhering to preventive measures. Women were more than 35 percent (OR 1.352; 95% CI 1.002–1.824) more likely to adhere to preventive measures than men.
Compared to individuals who listened to news only about once a week, those who listened to or watched the news at least daily or several times a day were twice (OR 2.066; 95% CI 1.211–3.524) and 78 percent (OR 1.783; 95% CI 1.039–3.060) more likely to adhere to preventive measures. Individuals who approved and those who strongly approved of lockdown measures were more than 2.1 times (OR 2.143; 95% CI 1.167–3.936) and more than 2.2 times (OR 2.242; 95% CI 1.226–4.099) more likely to adhere to preventive behavior. Approving of curfew measures (which followed lockdown) was associated with higher odds on adherence to preventive behavior. The odds of adhering to preventive actions increased from 60% (OR 1.687; 95% CI 1.174–2.424) for individuals who disapproved of curfew measures to more than six times higher (OR 6.109; 95% CI 3.745–9.967) for individuals who strongly approved of curfew.
Discussion
This paper contributes to the broader literature of COVID-19 prevention and in particular contributes to studies in Uganda documenting how the country has dealt with the pandemic, especially regarding risk perceptions and adherence to prevention mechanisms.
We find that age, being a woman, listening to news and approving of pandemic response mechanisms were correlated with reducing the odds of changing risk perceptions and adhering to preventive practices. In general, people tended to reduce their fear and hence their risk perception of COVID-19 over time. Only 15 percent of the respondents feared the disease more in July than they did in March. This is a rather worrying finding because lower risk perceptions are strongly associated with continued adherence to preventive measures [[45], [46]] and even vaccine acceptance [[47], [48]]. However, we do not find many factors associated with an increase in lower risk perceptions.
The findings on the age and behavior of older people are not at all surprising. While developing countries like Uganda generally have younger populations, older people are more at risk of COVID-19. Older people are therefore more likely to consider the disease deadly than younger people and therefore maintain risk-averse behavior rather than relax their perception of risk. Older people are also more likely to continue adhering to prevention behavior than younger people.
The results regarding employment corroborate the evidence of job and income losses across the country [18]. Moreover, our qualitative evidence also shows that economic pressures associated with the side effects of lockdown policies were imposed detrimental effects on households than the immediate risk of COVID-19. Therefore income and employment security were key in people's response and risk perception [36].
In principle, one would expect no differences between men and women. However, we observe that women were more likely to adhere to prevention behavior compared to men, similar to another study in Uganda [15] despite men believing they were more at risk than women [20]. We advance two hypotheses to explain this gender-based difference. First, possibly due to the nature of men's occupations and level of involvement, it is logical for them to believe they are more at risk than women [20]. Men are the main breadwinners for their households and often take on more risky occupations and activities than women. These activities are likely to affect their ability to adhere to social distancing and other preventive measures. Secondly, men often have poor health-seeking behavior [37] which might also influence their risk perceptions and COVID-19 prevention behavior. Our findings, in this case, resonate with those in Pakistan, where it was also found that men generally had lower COVID-19 risk perception than women [38].
We further observe that individuals who consume more news, especially traditional news media like radio, television or newspapers are more likely to take COVID-19 more seriously. Access to news remains a challenge in developing countries. While radio stations have increased in countries like Uganda, radio ownership remains at less than 60 percent of the population and less than 20 percent own a television [39]. Moreover, equity in access to news remains a challenge with more skewness to urban residents and men. However, a larger proportion of the population lives in rural areas, which might also be underserved with health facilities. This might imply that a prolonged pandemic might unevenly affect rural, underserved and unconnected communities.
Suffice to mention that we do not find a significant correlation between receiving news from social media and perception of COVID-19 seriousness. In our sample, 84% received news from a social media platform, so we could rule out the hypothesis that social media penetration was higher than average among survey respondents, likely because the survey was primarily distributed through Twitter, WhatsApp and Facebook. However, we find a negative correlation between social media and changing perspectives about COVID seriousness. Though the correlation is not statistically significant, it suggests that receiving news from social media might discourage people from taking COVID-19 seriously. This is in line with the recent literature on misinformation in pandemics, especially through social media [40]. Moreover, government public health organizations are more likely to transmit COVID-19 related information on traditional media platforms [41] which could explain the strong positive association.
Approving of lockdown restrictions is likely associated with the socioeconomic class as poor people are more likely to be affected than richer people [42]. We, therefore, think whereas poor people might also consider the disease serious, their precarious socioeconomic conditions cannot allow them to stay without work for extended periods to strictly observe lockdown and social distancing measures. Moreover, in developing countries like Uganda, this vulnerability is worsened by a large informal sector and the absence of unemployment insurance.
Limitations
One key limitation of our work is our internet sampling strategy that might limit the generalisability of the results. Generally, internet-based surveys have become increasingly important during the COVID-19 pandemic [43]. However, they might not be precisely representative due to low internet penetration rates in developing countries because of low internet penetration and subscription. Respondents are therefore more likely to be male, urban and more educated than the average population [44]. We, therefore, limit our interpretation to an online population rather than the general population.
Conclusion
In this study, we utilize an internet survey to shed more light on the extent of changing perception regarding the risk of COVID-19 in Uganda. We found that about 85% of the sample feared COVID-19 more in March than in July 2020 (or feared COVID-19 less in July 2020 than they did in March 2020). We further found that just about 63% of the sample were either somewhat seriously or very seriously following prevention recommendations such as regularly using facemasks and social distancing. Epidemiologists have predicted that, due to some advantages such as younger populations and warmer weather, African countries like Uganda might be spared a full-blown pandemic [31]. However, complacency associated with relaxing risk perceptions and associated preventive measures could be very dangerous. We found that being an older individual, receiving COVID-19 related news especially from traditional media platforms, and approving prevention policies such as lockdowns and curfews, were predictive of maintaining preventive behavior and higher COVID-19 risk perception. However, these results should be read with the caveat that internet surveys are less representative of the average population.
Funding
The authors have received no funding for this work.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: DR B Gyampoh
References
- 1.Chaudhry R., Dranitsaris G., Mubashir T., Bartoszko J., Riazi S. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. EClinicalMedicine. 2020;25 doi: 10.1016/j.eclinm.2020.100464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maier B.F., Brockmann D. Effective containment explains subexponential growth in recent confirmed COVID-19 cases in China. Science. 2020;368(6492):742–746. doi: 10.1126/science.abb4557. (80-) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egger D., Miguel E., Warren S., Shenoy A. Falling living standards during the COVID-19 Crisis: quantitative evidence from nine developing countries. Sci. Adv. 2021;(April) doi: 10.1126/sciadv.abe0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morgul E., Bener A., Atak M., et al. COVID-19 pandemic and psychological fatigue in Turkey. Int. J. Soc. Psychiatry. 2020:1–8. doi: 10.1177/0020764020941889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brewer G., Stratton K. Living with chronic fatigue syndrome during lockdown and a global pandemic. Fatigue Biomed. Heal Behav. 2020;8(3):144–155. doi: 10.1080/21641846.2020.1827503. [DOI] [Google Scholar]
- 6.Dryhurst S., Schneider C.R., Kerr J., et al. Risk perceptions of COVID-19 around the world. J. Risk Res. 2020;23(7–8):994–1006. doi: 10.1080/13669877.2020.1758193. [DOI] [Google Scholar]
- 7.Wise T., Zbozinek T.D., Michelini G., Hagan C.C., Mobbs D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. R. Soc. Open Sci. 2020;7(9) doi: 10.1098/rsos.200742rsos200742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ozili P. COVID-19 in Africa: socio-economic impact, policy response and opportunities. Int. J. Soc. Soc. Policy. 2020 doi: 10.1108/IJSSP-05-2020-0171. [DOI] [Google Scholar]
- 9.Teovanović P., Lukić P., Zupan Z., Lazić A., Ninković M., Žeželj I. Irrational beliefs differentially predict adherence to guidelines and pseudoscientific practices during the COVID-19 pandemic. Appl. Cogn. Psychol. 2020:1–11. doi: 10.1002/acp.3770. (November) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brainard J., Hunter P.R. Misinformation making a disease outbreak worse: outcomes compared for influenza, monkeypox, and norovirus. Simulation. 2020;96(4):365–374. doi: 10.1177/0037549719885021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vinck P., Pham P.N., Bindu K.K., Bedford J., Nilles E.J. Institutional trust and misinformation in the response to the 2018–19 Ebola outbreak in North Kivu, DR Congo: a population-based survey. Lancet Infect Dis. 2019;19(5):529–536. doi: 10.1016/S1473-3099(19)30063-5. [DOI] [PubMed] [Google Scholar]
- 12.Usman I.M., Ssempijja F., Ssebuufu R., et al. Community drivers affecting adherence to WHO guidelines against COVID-19 amongst rural ugandan market vendors. Front. Public Heal. 2020;8(July) doi: 10.3389/fpubh.2020.00340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rypdal K., Bianchi F.M., Rypdal M. Intervention fatigue is the primary cause of strong secondary waves in the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2020;17(24):1–17. doi: 10.3390/ijerph17249592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kieny M., Evans D.B., Schmets G., Kadandale S. Health-system resilience: reflections on the Ebola crisis in western Africa. Bull. World Heal Organ. 2014;92(850) doi: 10.2471/BLT.14.149278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amodan B.O., Bulage L., Katana E., et al. Level and determinants of adherence to COVID-19 preventive measures in the first stage of the outbreak in Uganda. Int. J. Environ. Res Public Health. 2020;17(23):1–14. doi: 10.3390/ijerph17238810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Migisha R., Kwesiga B., Mirembe B.B., et al. Early cases of SARS-CoV-2 infection in Uganda: epidemiology and lessons learned from risk-based testing approaches–March-April 2020. Glob. Health. 2020;16(1):1–9. doi: 10.1186/s12992-020-00643-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bell D., Hansen K.S., Kiragga A.N., Kambugu A., Kissa J., Mbonye A.K. Predicting the impact of COVID-19 and the potential impact of the public health response on disease burden in Uganda. Am. J. Trop. Med. Hyg. 2020;103(3):1191–1197. doi: 10.4269/ajtmh.20-0546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mahmud M., Riley E. Household response to an extreme shock: evidence on the immediate impact of the COVID-19 lockdown on economic outcomes and well-being in rural Uganda. World Dev. 2020;140 doi: 10.1016/j.worlddev.2020.105318. 2020March. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kansiime M.K., Tambo J.A., Mugambi I., Bundi M., Kara A., Owuor C. COVID-19 implications on household income and food security in Kenya and Uganda: findings from a rapid assessment. World Dev. 2021;137 doi: 10.1016/j.worlddev.2020.105199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kasozi K.I., MacLeod E., Ssempijja F., et al. Misconceptions on COVID-19 risk among ugandan men: results from a rapid exploratory survey, April 2020. Front. Public Heal. 2020;8(July):1–10. doi: 10.3389/fpubh.2020.00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mbonye A., Wamala J., Kaboyo W., Tugumizemo V., Aceng J., Makumbi I. Repeated outbreaks of viral hemorrhagic fevers in Uganda. Afr. Health Sci. 2012;12(4):579–583. doi: 10.4314/ahs.v12i4.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aceng J.R., Ario A.R., Muruta A.N., et al. Uganda ’ s experience in Ebola virus disease outbreak preparedness, 2018–2019. Glob. Health. 2020;16(24):1–12. doi: 10.1186/s12992-020-00548-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarki A.M., Ezeh A., Stranges S. Uganda as a role model for pandemic containment in Africa. Am. J. Public Health. 2020;110(12):1800–1802. doi: 10.2105/AJPH.2020.305948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Forester S., O'Brien C. Antidemocratic and exclusionary practices: COVID-19 and the continuum of violence. Polit. Gend. 2020;16(4):1150–1157. doi: 10.1017/S1743923X2000046X. [DOI] [Google Scholar]
- 25.Parker M., MacGregor H., Akello G. COVID-19, public authority and enforcement. Med. Anthropol. Cross Cult. Stud. Heal Illn. 2020;39(8):666–670. doi: 10.1080/01459740.2020.1822833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parkes J., Datzberger S., Howell C., et al. Young People, inequality and violence during the COVID-19 lockdown in Uganda. London; 2020. https://osf.io/preprints/socarxiv/2p6hx/.
- 27.Bagala A. Death toll from riots rises to 50. Daily Monit. 2020;24 https://www.monitor.co.ug/uganda/special-reports/death-toll-from-riots-rises-to-50–3208320. Published November. [Google Scholar]
- 28.Sekalala S.R., Kirya M.T. Challenges in multi-level health governance: corruption in the global fund's operations in Uganda and Zambia. Hague J. Rule Law. 2015;7(1):141–151. doi: 10.1007/s40803-015-0010-x. [DOI] [Google Scholar]
- 29.Tangri R., Mwenda A.M. Elite corruption and politics in Uganda. Commonw. Comp. Polit. 2008;46(2):177–194. doi: 10.1080/14662040802005336. [DOI] [Google Scholar]
- 30.Diop B.Z., Ngom M., Pougué Biyong C., Pougué Biyong J.N. The relatively young and rural population may limit the spread and severity of COVID-19 in Africa: a modelling study. BMJ Glob. Heal. 2020;5(5) doi: 10.1136/bmjgh-2020-002699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Njenga M.K., Dawa J., Nanyingi M., et al. Why is there low morbidity and mortality of COVID-19 in Africa? Am. J. Trop. Med. Hyg. 2020;103(2):564–569. doi: 10.4269/ajtmh.20-0474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Osewe P., Mensah J. What can we learn from Uganda on fighting deadly disease outbreaks? World Bank Blogs. 2014 https://blogs.worldbank.org/health/what-can-we-learn-uganda-fighting-deadly-disease-outbreaks PublishedAccessed February 5, 2021. [Google Scholar]
- 33.Lumu I. COVID-19 response in sub-saharan Africa: lessons from Uganda. Disaster Med. Public Health Prep. 2020;14(3):e46–e48. doi: 10.1017/dmp.2020.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nsoesie E.O., Cesare N., Müller M., Ozonoff Al. COVID-19 misinformation spread in eight countries: exponential growth modeling study. J. Med. Internet Res. 2020;22(12) doi: 10.2196/24425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Islam A.K.M.N., Laato S., Talukder S., Sutinen E. Misinformation sharing and social media fatigue during COVID-19: an affordance and cognitive load perspective. Technol. Forecast. Soc. Change. 2020;159(July) doi: 10.1016/j.techfore.2020.120201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haider N., Osman A.Y., Gadzekpo A., et al. Lockdown measures in response to COVID-19 in nine sub-Saharan African countries. BMJ Glob. Heal. 2020;5(10):1–10. doi: 10.1136/bmjgh-2020-003319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Galdas P.M., Cheater F., Marshall P. Men and health help-seeking behaviour: literature review. J. Adv. Nurs. 2005;49(6):616–623. doi: 10.1111/j.1365-2648.2004.03331.x. [DOI] [PubMed] [Google Scholar]
- 38.Ahmad I., Saleem S., Bilal A., Jamshed A., Ahmad J., Ahmad A. COVID-19 risk perception and coping mechanisms : does gender make a difference ? Int. J. Disaster Risk Reduct. 2021;55(January) doi: 10.1016/j.ijdrr.2021.102096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.UBOS I.C.F. Kampala and Rockville Maryland; 2018. Uganda Demographic and Health Survey 2016. [Google Scholar]
- 40.Rochwerg B., Parke R., Murthy S., et al. Misinformation during the coronavirus disease 2019 outbreak. Crit. Care Exp. 2020;2(4):e0098. doi: 10.1097/cce.0000000000000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van der Meer T.G.L.A., Jin Y. Seeking formula for misinformation treatment in public health crises: the effects of corrective information type and source. Health Commun. 2020;35(5):560–575. doi: 10.1080/10410236.2019.1573295. [DOI] [PubMed] [Google Scholar]
- 42.Teachout M., Zipfel C. The economic impact of COVID-19 lockdowns in sub- Saharan Africa. 2020;(May). https://www.theigc.org/wp-content/uploads/2020/05/Teachout-and-Zipfel-2020-policy-brief-.pdf.
- 43.Ali S.H., Foreman J., Capasso A., Jones A.M., Tozan Y., Diclemente R.J. Social media as a recruitment platform for a nationwide online survey of COVID-19 knowledge, beliefs, and practices in the United States: methodology and feasibility analysis. BMC Med. Res. Methodol. 2020;20(1):1–11. doi: 10.1186/s12874-020-01011-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rosenzweig L.R., Bergquist P., Pham K.H., Rampazzo F., Mildenberger M. Survey sampling in the global south using facebook advertisements. Unpubl. Work Pap. 2020:1–24. https://static1.squarespace.com/static/5410fc5ae4b0b9bdbd0cde82/t/5f201d340708bc5116d036cd/1595940154387/Facebook_sampling_public.pdf [Google Scholar]
- 45.Tesfaw Aragaw, Arage Getachew, Tashome Fentaw, Taklual Wubet, Seid Tigist, Belay Emaway, Mehiret Gashaw. Community risk perception and barriers for the practice of COVID-19 prevention measures in Northwest Ethiopia: A qualitative study. PLoS ONE. 2021;16(9) doi: 10.1371/journal.pone.0257897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Albrecht Rebecca, Jarecki Jana B, Meier Dominik S, Rieskamp Jörg. Risk preferences and risk perception affect the acceptance of digital contact tracing. Humanities and Social Sciences Communications. 2021;18(195) doi: 10.1057/s41599-021-00856-0. [DOI] [Google Scholar]
- 47.Du Min, Tao Liyuan, Liu Jue. The Association Between Risk Perception and COVID-19 Vaccine Hesitancy for Children Among Reproductive Women in China: An Online Survey. Frontiers in Medicine. 2021;8(September) doi: 10.3389/fmed.2021.741298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mahmud Sultan, Mohsin Md, Khan Ijaz Ahmed, Mian Ashraf Uddin, Zaman Miah Akib. Knowledge, beliefs, attitudes and perceived risk about COVID-19 vaccine and determinants of COVID-19 vaccine acceptance in Bangladesh. PLoS ONE. 2021;16(9) doi: 10.1371/journal.pone.0257096. [DOI] [PMC free article] [PubMed] [Google Scholar]