Abstract
Rationale
Registered nurses are struggling on the front line to manage patients with COVID-19 and other illnesses, placing them at increased risks for severe perceived stress. Although perceived stress has often been considered a significant risk factor for impaired quality of life among registered nurses, having resilience has been generally shown to be associated with better quality of life.
Purpose
This study aimed to investigate the mediating effects of resilience on the relationship between perceived stress and quality of life in Jordanian clinical registered nurses during the COVID-19 pandemic.
Methods
The study used a cross-sectional correlational design with an online survey and adhered to the STROBE guideline for cross-sectional studies. A total of 550 registered nurses working in 6 hospitals were conveniently selected. Data were collected via a demographic questionnaire, the Perceived Stress Scale (PSS), the Connor-Davidson Resilience Scale (CD-RISC), and the WHOQOL scale. Descriptive, Pearson correlation, t-test, one-way ANOVA, and hierarchical linear regression analyses were used to analyze the data.
Results
The results indicated that resilience was negatively correlated with perceived stress and quality of life. Further, resilience was found to play a partial mediating role in the relationship between perceived stress and quality of life. Therefore, the results partially supported our study hypotheses.
Conclusion
Health policy makers and administrators in Jordan should be aware of the importance of assessing and improving nurses’ resilience to decrease devastating effects of stress on quality of life.
Keywords: Resilience, Stress, Quality of life, Registered nurse, Pandemics
Resilience, Stress, Quality of life, Registered nurse, Pandemics.
1. Introduction
The Coronavirus Disease 2019 (COVID-19) was first reported in Wuhan, China in December 2019 and has since then spread rapidly across the world. In Jordan, the first case of COVID-19 was reported on March 2nd, 2020, and by November 18th, 2020, the total number of confirmed cases in Jordan had reached 163,926, with 1,969 deaths [1]. Facing this critical situation, healthcare providers, especially nurses working in clinical settings, have been struggling to manage patients with COVID-19 and other illnesses [2, 3].
Many nurses struggle with strict guidelines, long working hours, insufficient personal protective equipment (PPE), and inadequate training about infection control measures, which places them at an increased risk of becoming infected and transmitting the disease to their family members. Therefore, nurses may face several challenges and suffer from high levels of perceived stress [4, 5, 6], which adversely impacts their quality of life [7, 8]. Quality of life is an important indicator in determining whether nurses have been able to cope successfully with challenges during stressful events and emergencies. Impaired quality of life can disrupt nurses’ efficiency in providing high-quality care and services and adequate psychological support to patients [9].
Although perceived stress is considered a significant risk factor for psychopathology associated with low quality of life among nurses, having resilience has been shown to prevent the development of psychopathology [10, 11]. Therefore, the implementation of early psychological interventions aimed at developing resilience as a coping mechanism among nurses is important [12]. Resilience helps nurses deal with stress, maintain professionalism in various job situations, and deal with issues related to excessive workloads, staffing shortages, and general healthcare deficiencies [13]. Resilience has also been found to protect nurses against stress, depression, and emotional exhaustion that could compromise their quality of life and the quality of their provided care [14, 15, 16]. The literatures shows that level of education, work experience, age, and gender are significantly associated with nurses' resilience [17, 18]. Hence, enhancing nurses' resilience levels, with taking in consideration the nurses’ demographic and professional characteristics, is crucial for allowing them to provide high-quality care and deal effectively with adverse events in healthcare settings during the COVID-19 pandemic [19].
According to the transactional theory of stress (TTS) [20], coping strategies play a mediating role in the relationship between perceived stress and health outcomes. Resilience is commonly defined as a coping ability to tolerate adversity and bounce back from adverse circumstances [21]. Accordingly, resilience is expected to mediate the relationship between perceived stress and quality of life. However, little is known about the mediating role of resilience in the relationship between perceived stress and quality of life among clinical registered nurses during critical situations, such as the COVID-19 pandemic, in Jordan. Thus, this study aimed to investigate the influence of perceived stress on quality of life, and the mediating effects of resilience on the relationship between perceived stress and quality of life in clinical registered nurses in Jordan during the COVID-19 pandemic.
1.1. Theoretical framework
In applying the transactional theory of stress (TTS) [20] to understand stress experienced by nurses during the COVID-19 pandemic, the role of appraisal of a stressful situation and individuals' variations in response to the same stressors are emphasized. According to the TTS, stress refers to the individual's relationship with environments which the individual views as taxing or exceeding their resources and threatening their health [20].
On a daily basis, nurses encounter different types of stressors in the workplace [22], and these stressors are appraised as either being benign or a threat [23]. Based on the TTS [20], stress responses are caused by individuals' subjective evaluation or interpretation (i.e., cognitive appraisal) of stressors, which explains the variations in the ways people respond to the same stressors and the coping resources they use. Cognitive appraisal, which refers to how individuals, such as nurses, evaluate an experienced event and perceive it to influence their goals and well-being, is a core component of the TTS and includes primary and secondary appraisal of stressors [20]. Primary appraisal involves appraising the relevance of an event to one's well-being as being either irrelevant, benign positive, or stressful (i.e., challenging, threatening, or harmful). Meanwhile, secondary appraisal refers to the nurse's evaluation of the coping resources available to manage events appraised as stressful [20]. The lack of effective coping resources can trigger emotional, physical, and social reactions, eventually impairing health outcomes, work performance, and quality of life [7, 8].
Coping is defined as cognitive and behavioral efforts used to manage stressful situations [20]. Resilience is a coping ability associated with positive emotions that may have adaptive benefits during stressful experiences [24]. Thus, high resilience is proposed to better enable nurses to easily overcome stressful situations [23], develop other efficient coping strategies, and adapt cognitively to changing situations [25, 26].
Recently, more research focus has been placed on stress and coping among nurses. However, the concept of resilience as a coping strategy among nurses has only recently emerged. Additionally, previous studies which have explored stress and coping among nurses have lacked theoretical backgrounds. Therefore, the current study will use Lazarus and Folkman's transactional model to explain the mediating role of resilience as a coping strategy in the relationship between perceived stress and quality of life among registered nurses. We hypothesize that: 1) there is a negative association between perceived stress and resilience, 2) there is a positive association between resilience and quality of life, 3) there is a negative association between perceived stress and quality of life, and 4) resilience mediates the relationship between perceived stress and quality of life.
2. Methods
2.1. Design, sample, and settings
The study used a cross-sectional correlational design with an online survey and adhered to the STROBE guideline for cross-sectional studies. Convenience sampling was used to recruit registered nurses who were authorized to take care of COVID-19 patients and who were working in any of 8 selected hospitals in Jordan (2 private hospitals, 2 public hospitals, 2 military hospitals, and 2 university hospitals) located in the three biggest cities in Jordan (Amman, Irbid, and Al-zarqa). Nurses were considered eligible if they had completed bachelor's degree in nursing, were working full-time with inpatients, and had at least 6 months of clinical experience. Nurses who were doing internships or any other training or volunteer work and nurses working in the outpatient clinics were excluded.
2.2. Sample size
A priori of power analysis by G∗Power was used to calculate the required sample size. Assuming α of 0.05, power of 0.95 (generally required largest sample size), effect size of 0.075 (medium effect size [27], and a maximum of 9 tested predictors (the main study independent variables and demographic variables), the resulting required sample size was 324. Considering low response rate due to using an online survey method and the busy schedule of nurses during the pandemic, we expected that the response rate would be low. Considering an expected response rate of 50%, 324 participants should be added, yielding the final total sample size of 648.
2.3. Instruments
The study data were collected using an Arabic online self-administered questionnaire. The questionnaire consisted of four parts: sociodemographic data, the Connor-Davidson Resilience Scale (CD-RISC), the Perceived Stress Scale (PSS), and the World Health Organization Quality of Life- BREF scale (The WHOQOL-BREF).
2.3.1. The socio-demographic data
The first section of the questionnaire was developed by the researchers and included questions related to the participants’ sociodemographic and professional characteristics. These characteristics included gender, age, marital status, parental status, level of education, years of experience, hospital type, and work shift pattern.
2.3.2. The Connor-Davidson Resilience Scale (CD-RISC)
The CD-RISC (Kathryn, Connor, Jonathan, & Davidson, 2003) is a self-rating scale used to assess resilience. The CD-RISC consists of 25 items scored on a five-point Likert scale ranging from 0-4 as follows: “not true at all” (0), “rarely true” (1), “sometimes true” (2), “often true” (3), and “true nearly all of the time” (4). The total possible score ranges from 0 to 100, with higher scores indicating higher resilience. The CD-RISC has demonstrated good reliability (α = .88 and .89), test-retest reliability (.87), and convergent and divergent validity [28, 29]. A Cronbach's alpha of 0.91 was reported for this scale among a sample of Arab adults [30].
2.3.3. The Perceived Stress Scale (PSS)
The Perceived Stress Scale (PSS) (Cohen, Kamarck, & Mermelstein, 1983) is one of the most popular instruments for assessing the perception of stress. The scale consists of 10 items which assess the degree to which situations in one's life are appraised as stressful. The items are rated on a 5-point Likert scale ranging from 0 (never) to 4 (very often). The total possible score ranges from 0 to 40, with higher scores indicating higher levels of perceived stress [31]. The PSS has been validated for use among college students. In the original study, the scale had internal consistency coefficients ranging from .84 to 36 and test-retest reliability of .85 [31]. The Arabic version of the PSS showed adequate psychometric qualities among the Jordanian general population. The exploratory factor analysis revealed two factors with eigenvalues greater than 1.0 (45.0% of the variance); the Cronbach's alpha coefficients were 0.74 for Factor 1, 0.77 for Factor 2, and 0.80 for the whole scale [32].
2.3.4. The WHOQOL-BREF
The WHOQOL-BREF (The WHOQOL Group, 1998) is a 26-item scale, derived from the original 100-item WHOQOL-100 scale. The scale items cover four domains related to QOL: physical health, psychological health, social relationships, and environment. An additional two items which measure overall QOL and general health are included. The items are rated on a 5-point Likert scale, with higher scores indicating higher QOL. Based on the scoring guidelines, the scores of the items in each domain are summed to obtain the domain score. The raw domain scores for the WHOQOL-BREF are transformed to scores ranging from 4 to 20. The scores are then linearly transformed to a 0–100 scale. The Arabic version of the WHOQOL-BREF has previously been used in a study among nurses [33]. The psychometric properties of the Arabic version of the WHOQOL-BREF were tested among a general Arab population, and the results indicated acceptable validity and reliability, with Cronbach's α of ≥.70 [34].
2.4. Data collection procedure
The study data were collected through an online survey using Google Forms (Free Online Surveys). After obtaining approval from the institutional review board (IRB) at Jordan University of Science and Technology, the principle investigator contacted nursing managers working in different public, private, military, and university hospitals inviting them to ask their registered nurses to participate in the study. Nurses who agreed to participate were sent the survey link through email or WhatsApp, based on their preference. The electronic consent form was included on the front page of the online survey and an “I accept” button provided participants access into the survey. A reminder was sent to nurses who had still not completed the survey after one week of receiving the link. The study data were collected from May 17th, 2020 to August 15th, 2020.
2.5. Ethical consideration
Approval was obtained from the IRB at Jordan University of Science and Technology. The questionnaires were coded, and the participants were assured that all data would be kept anonymous and confidential and used for research purposes only. Permission to use the selected scales was obtained from the original authors.
2.6. Data analysis
Data analysis was conducted using the IBM SPSS statistics software (version 25.20). Descriptive analysis, including means, standard deviations, frequencies, and percentages, was used to describe the study variables. The statistical assumption of normality for the continuous variables was assessed using the Kolmogorov-Smirnov test and visual histograms. Levene's test of equal variance was used for testing the homogeneity of variance statistical assumptions for the measured concepts and continuous variables.
The independent samples t-test and one-way ANOVA were used to assess the statistical significance of the mean differences in the nurses' perceptions of quality of life and perceived stress across the levels of measured binary and multi-level categorical demographic and professional characteristics. Pearson's correlation coefficient (r) test was used to assess the associations between the metric variables. The scale's reliability was assessed using the Cronbach's alpha test of internal consistency.
The study hypotheses representing the correlations between the study variables (i.e. resilience, perceived stress, and quality of life) and the mediating effect of resilience were tested using hierarchical multiple regression analysis. A variable is defined as a mediator when it meets the following conditions: (a) the independent variables are strongly correlated with the dependent variables; (b) the independent variables are associated with the mediator; and (c) the independent variables and the mediator are correlated with the dependent variables [35]. Within the correlation framework, a 3-step regression analysis was performed to test the mediating effects, as per many previous studies. In the present study, perceived stress was first regressed on resilience, and then quality of life was regressed on resilience. Finally, quality of life was regressed on resilience and perceived stress. The separate coefficients for each regression equation were examined.
There are three possible ways of interpreting the results of regression coefficient examination. First, when the coefficient of the first step is insignificant, mediating effects analysis is ended. Second, when the coefficients of the first and second step are significant and the coefficient for the independent variable (resilience) in the third step is insignificant, this indicates a significant full mediating effect. Third, when the coefficient of the first step and the second step are significant, and the coefficient for the independent variable (perceived stress) in the third step is less than the result of the second step, this represents a significant partial mediating effect [35].
3. Results
3.1. Sociodemographic and professional characteristics
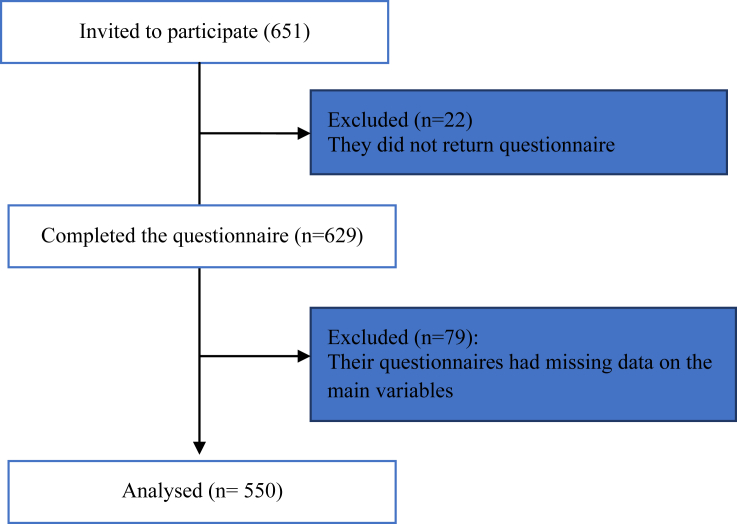
Table 1 presents the characteristics of the study sample. Of 650 surveys sent to registered nurses, 550 surveys were completed and submitted, with a response rate of 85% (see Figure 1). Most of the participants were female, married, and working two shifts (day and night shift). The mean age of the participants was 29.61 years. Additionally, most of the participants held a bachelor's degree in nursing. The mean number of years of nursing experience among the participants was 6.85 years.
Table 1.
The demographic and professional characteristics of nurses (N = 550).
| Variable | Categories | Frequency (%) | Mean (SD) |
|---|---|---|---|
| Gender | |||
| Male | 171 (31.1) | ||
| Female | 379 (68.9) | ||
| Marital status | |||
| Single | 208 (37.8) | ||
| Married | 342 (62.2) | ||
| Educational level | |||
| Bachelor's degree | 471 (86) | ||
| Master's degree | 79 (14) | ||
| Hospital type | |||
| Private | 94 (17.1) | ||
| University | 232 (42.2) | ||
| Public | 83 (15.1) | ||
| Military | 141 (25.6) | ||
| Shift pattern | |||
| Two Shifts (Day/Night) | 132 (24) | ||
| Three Shifts (ABC) | 418 (76) | ||
| Age | 29.61 (5.24) | ||
| Nursing experience | 6.85 (4.95) | ||
| Number of children | 1.16 (1.4) | ||
Figure 1.
Flow diagram demonstrating inclusion and exclusion of participants.
3.2. Description of perceived stress, resilience and quality of life
The basic descriptive statistics of perceived stress, resilience, and quality of life are shown in Table 2. The mean score for perceived stress was 19.50, the mean score for resilience was 61.57, and the mean score for quality of life was 52.46. The domain of satisfaction with environment had the lowest mean score in comparison to the other domains, whilst the domain of psychological satisfaction had the highest mean score.
Table 2.
Descriptive analysis of quality of life, perceived stress, and resilience (N = 550).
| Variable | M (SD) | Possible Range | Chronbach's α |
|---|---|---|---|
| Quality of life | 52.46 (9.45) | 0-80 points | .91 |
| Perceived stress | 19.50 (5.22) | 0-40 points | .662 |
| Resilience | 61.57 (17.43) | 0-100 points | .96 |
3.3. Quality of life and sociodemographic and professional characteristics
Table 3 shows the bivariate analysis results for the association between quality of life and the selected sociodemographic and professional categorical characteristics. The Pearson's correlation coefficient (r), the independent samples t-test, and one-way ANOVA were used. The findings showed that quality of life level differed significantly according to educational level (p < .001) and hospital type (p < .001). Further, quality of life correlated significantly with nursing experience (p < .01).
Table 3.
The relationship between sample characteristics, resilience and quality of life (N = 550).
| Variables | Resilience |
Quality of Life |
|||||
|---|---|---|---|---|---|---|---|
| M(SD) | t, F, or r | p | M(SD) | t, F, or r | p | ||
| Gender | Male | 61 (18.8) | t = -.447 | 0.655 | 52.40 (9.92) | t = -.086 | 0.932 |
| Female | 61.8 | 52.48 (9.25) | |||||
| Marital status | Single | 62.5 (18.6) | t = .949 | 0.343 | 52.14 (9.43) | t = 0.62 | 0.726 |
| Married | 61.0 (16.7) | 52.64 (9.47) | |||||
| Educational level | Bachelor's | 61.0 (17.97) | t = -2.28 | 0.024 | 52.34 (9.44) | t = -3.63 | .000 |
| Master's | 64.9 (13.37) | 55.99 (8.95) | |||||
| Hospital type | Private | 57.9 (17.4) | F = 2.95 | 0.032 | 55.43 (9.91) | F = 5.54 | 0.001 |
| University | 60.8 (16.6) | 52.63 (9.29) | |||||
| Public | 63.9 (18.9) | 50.64 (9.55) | |||||
| Military | 63.9 (5.17) | 53.87 (9.22) | |||||
| Shift pattern | 2 shifts (Day/Night) | 63.7 (17.5) | t = 1.58 | 0.115 | 53.02 (9.35) | t = .79 | 0.433 |
| 3 shifts (ABC) | 60.9 (17.4) | 52.28 (9.49) | |||||
| Experience | r = .06 | .169 | r = .114 | .008 | |||
| Age | r = -.005 | .91 | r = .062 | 0.146 | |||
| Number of children | r = .04 | .354 | r = .028 | .517 | |||
3.4. Resilience and sociodemographic and professional characteristics
Table 3 also shows the bivariate analysis results for the association between psychological resilience and the selected demographic and professional characteristics. The findings showed that psychological resilience differed significantly according to educational level (p < .05) and hospital type (p < .05). Meanwhile, the variables gender, age, marital status, number of children, work experience, and work shift pattern were not found to be significantly associated with psychological resilience.
3.5. Mediating effect of resilience
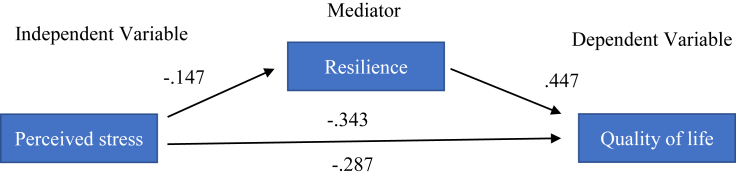
Table 4 displays the analysis of the mediating effect of psychological resilience on the relationship between perceived stress and quality of life. The mediating variable was resilience, the predictor was resilience, and the dependent variable was quality of life.
Table 4.
Mediating effect of resilience on perceived stress and quality of life (N = 550).
| Steps | Description | IV | DV | Beta | p-value |
|---|---|---|---|---|---|
| 1 | Direct effect of perceived stress on resilience | Resilience | Stress | -.147 | .001 |
| 2 | Direct effect of resilience on quality of life | Resilience | QoL | 0.447 | .00 |
| 3 | Direct effect of perceived stress on quality of life | Stress | QoL | -0.343 | .00 |
| 4 | Indirect effect of perceived stress on quality of life | Stress & | QoL | -0.287 | .00 |
| Resilience | QoL | 0.409 | .00 |
QoL: Quality of life.
Four hierarchal multiple regression analysis tests were conducted to examine the mediating effect of psychological resilience. In the first test (Model-1), psychological resilience was regressed on perceived stress. Because educational level and hospital type could impact psychological resilience, they were controlled using a hierarchical multiple regression by entering them into the first block of the equation. Perceived stress was entered into the second block. The findings of the first step showed psychological resilience to be significantly regressed on perceived stress (beta = -.147, p = .001). In the second step, quality of life was regressed on resilience. Since educational level, hospital type, and work experience correlated significantly with quality of life, they were controlled by entering them in the first block of the equation, and psychological resilience was entered into the second block. The findings of the second step showed that quality of life was significantly regressed on psychological resilience (beta = .447, p < .001). In the third step, quality of life was regressed on perceived stress, after controlling for educational level, hospital type, and work experience (as we did in the first and second steps). The findings of the third step showed that quality of life was significantly regressed on perceived stress (beta = -.343, p < .001). In the fourth step, quality of life was regressed on perceived stress, with psychological resilience as the mediator. The variables educational level, hospital type, and work experience were controlled by entering them in the first block, as they were found to be significantly associated with quality of life. Resilience and perceived stress were entered into the second block. Quality of life was significantly regressed on resilience (beta = .409, p < .001) and perceived stress (β = -.287, p < .001), respectively.
The effect of perceived stress on quality of life declined by about .056 from model 1 to model 4 (beta = -.343 in Model-1 to a beta of -0.287 in model-4). This suggested that after considering the joint effect of psychological resilience, the impact of perceived stress on quality of life had declined but remained negatively significant. Thus, adding psychological resilience in model 4 had partially buffered the effect of perceived stress on quality of life. In conclusion, the analysis showed that psychological resilience partially mediates the association between perceived stress and quality of life among registered nurses (Figure 2).
Figure 2.
The mediating Model of Resilience.
4. Discussion
The current study explored the mediating role of psychological resilience in the relationship between perceived stress and quality of life among registered nurses working in clinical settings during the COVID-19 pandemic. The results indicated that psychological resilience was negatively correlated with perceived stress and quality of life. Further, psychological resilience was found to play a partial mediating role in the relationship between perceived stress and quality of life. Therefore, the results partially supported our study hypotheses.
As a result of their exposure to multiple stressors, nurses who work on the front line during pandemics such as the COVID-19 pandemic are susceptible to high levels of stress [5]. Perceived stress experienced during the COVID-19 pandemic may have detrimental impacts on psychosocial health and quality of life among registered nurses. The current study found that perceived stress not only directly affects the QOL of registered nurses during the COVID-19 pandemic, but it also indirectly affects their QOL through psychological resilience.
Our finding regarding the direct relationship between perceived stress and QOL is similar to the findings of previous studies, which have indicated a negative relationship between perceived stress and QOL among registered nurses from different countries [7, 8, 36, 37]. It has been reported that during the COVID-19 pandemic, registered nurses have encountered various stressors which they have appraised as exceeding or taxing their coping resources and ultimately jeopardizing their quality of life (4,5,6,7,8). According to Lazarus and Folkman (1984), perceived stress results in the triggering of emotional, physical, and social reactions. If these reactions last for a long time and are not coped with effectively, they can lead to poor health outcomes and threaten health and quality of life [20].
Our findings also indicated that perceived stress indirectly affects quality of life through the mediation of psychological resilience. Whilst the present study is the first to examine the mediating role of perceived stress on the relationship between resilience and quality of life among registered nurses, previous studies have examined the mediating role of stress and other health outcomes. For example, Liu et al. (2019) found that resilience partially mediated the relationship between negative life events, known as stressors, and depression among Chinese adolescents [38]. Also, Shi et al. (2015) reported that resilience functioned as a partial mediator in the relationship between stress and life satisfaction among Chinese medical students [39].
Further, our findings showed that registered nurses' psychological resilience is a buffering mediator between perceived stress and quality of life. According to the TTS [20], a coping mechanism, as a mediator between perceived stress and quality of life and health, is described as a personal effort to manage these challenges and demands appraised as taxing or exceeding the resources of the person. Psychological resilience is often described as a coping mechanism that helps individuals respond effectively to stressors faced in daily life, allowing them to overcome their struggles by focusing on the real problem and how to deal with it effectively instead of being distracted by these stressors [40], Previous studies have revealed that when faced with demanding situations, nurses with good resilience experience less stress and are able to overcome the stressful situation more easily than nurses with low resilience [41, 42, 43]. Rutter (2002) proposed that resilient people are optimistic about their ability to successfully overcome and control the challenges they encounter in their daily life. Several studies have shown that resilience-based therapy is effective in allowing individuals to overcome stress [44]. Psychological resilience may buffer the detrimental impacts of perceived stress on health and quality of life by enhancing people's ability to overcome challenges and adversities and cope with struggles and stressors [37, 45].
Although our findings showed that perceived stress can affect QOL through the mediation of psychological resilience, the mediation was partial and the mediation effect ratios were only 28.0%, suggesting that other variables may play a mediating role in the relationship between perceived stress and QOL. The results partially supported our hypotheses, since resilience as a coping mechanism partially mediated the relationship between perceived stress and quality of life. This partial mediation showed that other factors, such as other coping mechanisms, may play a mediating role in the relationship between resilience and quality of life. According to Lazarus and Folkman (2018), many coping mechanisms mediate the relationship between perceived stress and quality of life, including problem-focused and emotion-focused coping mechanisms [20]. Huang et al. (2020) found that nurses in China had relied on problem-focused coping methods during the outbreak of COVID-19 [46]. Thus, it is expected that Jordanian registered nurses may use other coping mechanisms besides resilience during the COVID-19 outbreak. Yang et al. (2018) found that social support and psychological resilience played the role of mediators between perceived stress and life satisfaction among Chinese people with substance use disorder [47]. Thus, the mediating role of other coping mechanisms besides psychological resilience, such as social support, in the relationship between perceived stress and quality of life among registered nurses should be explored in future research.
4.1. Limitations
Although the results of this study address a gap in the literature, there are limitations to our study that should be taken into consideration in future research. Firstly, the use of a cross-sectional study design did not allow for understanding the causal relationships between the variables. Secondly, there are many confounding factors, such as other coping strategies, which were not included and examined in our study design, therefore limiting the internal validity. Thirdly, convenience sampling was used to recruit participants, which may have resulted in findings that may not necessarily be representative of nurses in Jordan and may therefore threaten the external validity. However, the generalizability was improved by recruiting registered nurses who were working in any of 8 selected hospitals in Jordan (2 private hospitals, 2 public hospitals, 2 military hospitals, and 2 university hospitals) located in the three biggest cities in Jordan. Fourthly, the study data were collected using self-report questionnaires, which may have led to response bias and therefore negatively impacted the internal validity.
It is recommended that longitudinal studies or randomized controlled trials (RCT) are conducted to further confirm our results. Our study is largely based on quantitative methods. Qualitative or mixed-model methods should be considered to explore the interrelationships between psychological resilience, perceived stress, and quality of life. Further, whilst only psychological resilience as a mediating variable was included and examined in our study to explore the relationship between resilience and quality of life, other factors, such as social support, may also mediate this relationship among registered nurses. Thus, future research should consider other factors which may mediate the relationship between resilience and quality of life. Finally, it is recommended that future studies use probability sampling methods in order to increase the representativeness of the sample.
4.2. Implications
In the 21st century, healthcare systems worldwide are seeking to deliver high-quality care, improve patient satisfaction, and decrease nurse turnover. However, this cannot be achieved if nurses have low quality of life. Understanding the determinants of low quality of life among nurses, such as perceived stress and psychological resilience, will be useful for the development of effective holistic programs aimed at improving registered nurses’ quality of life [48].
The findings of our study showed perceived stress and psychological resilience to have significant effects on quality of life among registered nurses working during the COVID-19 pandemic. Thus, it is essential that decision-makers in healthcare settings or hospitals in Jordan are aware of the importance of providing nurses with psychological support through the development and implementation of resilience-based stress reduction programs. In turn, this may improve the QOL of nurses working during the COVID-19 pandemic. Further, continuous development departments in healthcare settings in Jordan should organize educational workshops aimed at strengthening the psychological resilience of nurses. This will contribute to the improvement of nurses’ work environments and the effective achievement of organizational goals. Further, this will create optimistic work environments and guarantee the personal safety of nurses, thereby enabling them to continue providing the highest quality of patient care during their battle against the pandemic.
As with regards to nursing education institutions, the findings of this study shed light on the importance of integrating resilience-based stress reduction programs in the nursing curricula in Jordan. This will help nursing students strengthen their psychological resilience before entering the work environment. Further, nursing faculties and administrators in Jordan should be proactive in addressing nursing students’ stress and hence poor quality of life. Nursing students are the future of the nursing profession. If nursing faculties do not take reasonable and realistic steps to help students manage the overwhelming demands of their roles, the nursing profession could fail to thrive [49]. With the nursing profession in Jordan facing continuous pressure to recruit nurses and reduce nurse turnover, nursing faculties and administrators should work to reduce stress among nurses through resilience-based stress reduction programs, as stress is a major cause of nurse turnover.
5. Conclusion
Despite the limitations noted above, this study is the first to explore the mediating effect of psychological resilience in the relationship between perceived stress and quality of life among registered nurses working in clinical settings during the COVID-19 pandemic. The findings partially supported our hypothesized model, indicating that psychological resilience partially mediated the relationship between perceived stress and quality of life. Thus, perceived stress and resilience should be valued as important components for the improvement of nurses' quality of life. Our results serve to increase policy makers' awareness of the importance of assessing and improving nurses’ resilience and managing their stress through the development and implementation of effective resilience-based programs.
Declarations
Author contribution statement
Hossam AlHawatmeh and Rahaf Alsholol: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Heyam Dalky: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Nahla Al-Ali and Raya Albataineh: Analyzed and interpreted the data; Wrote the paper.
Funding statement
This work was supported by Jordan University of Science and Technology (IRB# 20200330).
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors thank the participating hospitals, head nurses, and nurse participants for their assistance, as well as Jordan University of Science and Technology for funding the study.
References
- 1.Group T.W. The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc. Sci. Med. 1998;46(12):1569–1585. doi: 10.1016/s0277-9536(98)00009-4. [DOI] [PubMed] [Google Scholar]
- 2.Smith G.D., Ng F., Li W.H. COVID-19: emerging compassion, courage and resilience in the face of misinformation and adversity. J. Clin. Nurs. 2020;29(9-10):1425–1428. doi: 10.1111/jocn.15231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . World Health Organization; Geneva: 2019. Coronavirus Disease 2019 (COVID-19) Situation Report – 82.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200411-sitrep-82-covid-19.pdf?sfvrsn=74a5d15_2 [internet] [cited 2020 Jun 2]. Available from: [Google Scholar]
- 4.Braquehais M.D., Vargas-Cáceres S., Gómez-Durán E., Nieva G., Valero S., Casas M., Bruguera E. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. QJM: Int. J. Med. 2020;113(9):613–617. doi: 10.1093/qjmed/hcaa207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., Wang J. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maben J., Bridges J. Covid-19: supporting nurses' psychological and mental health. J. Clin. Nurs. 2020;29(15-16):2742–2750. doi: 10.1111/jocn.15307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sarafis P., Rousaki E., Tsounis A., Malliarou M., Lahana L., Bamidis P., Niakas D., Papastavrou E. The impact of occupational stress on nurses’ caring behaviors and their health related quality of life. BMC Nurs. 2016;15(1):56. doi: 10.1186/s12912-016-0178-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silva A.M., Guimarães L.A. Occupational stress and quality of life in nursing. Paidéia (Ribeirão Preto) 2016;26(63):63–70. [Google Scholar]
- 9.Stojanov J., Malobabic M., Stanojevic G., Stevic M., Milosevic V., Stojanov A. Quality of sleep and health-related quality of life among health care professionals treating patients with coronavirus disease-19. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020942800. 20764020942800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Babanataj R., Mazdarani S., Hesamzadeh A., Gorji M.H., Cherati J.Y. Resilience training: effects on occupational stress and resilience of critical care nurses. Int. J. Nurs. Pract. 2019;25(1) doi: 10.1111/ijn.12697. [DOI] [PubMed] [Google Scholar]
- 11.Khamisa N., Oldenburg B., Peltzer K., Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int. J. Environ. Res. Pub. Heal. 2015;12(1):652–666. doi: 10.3390/ijerph120100652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmadi B., Mosadeghrad A.M., Karami B. Effectiveness of resilience education on quality of working life among nursing personnel: a randomized controlled study. Payesh (Health Monitor) 2019;18(3):279–289. [Google Scholar]
- 13.Hart P.L., Brannan J.D., De Chesnay M. Resilience in nurses: an integrative review. J. Nurs. Manag. 2014;22(6):720–734. doi: 10.1111/j.1365-2834.2012.01485.x. [DOI] [PubMed] [Google Scholar]
- 14.Guo Y.F., Luo Y.H., Lam L., Cross W., Plummer V., Zhang J.P. Burnout and its association with resilience in nurses: a cross-sectional study. J. Clin. Nurs. 2018;27(1-2):441–449. doi: 10.1111/jocn.13952. [DOI] [PubMed] [Google Scholar]
- 15.Magtibay D.L., Chesak S.S., Coughlin K., Sood A. Decreasing stress and burnout in nurses: efficacy of blended learning with stress management and resilience training program. J. Nurs. Adm. 2017;47(7/8):391–395. doi: 10.1097/NNA.0000000000000501. [DOI] [PubMed] [Google Scholar]
- 16.Zou G., Shen X., Tian X., Liu C., Li G., Kong L., Li P. Correlates of psychological distress, burnout, and resilience among Chinese female nurses. Ind. Health. 2016;54(5):389–395. doi: 10.2486/indhealth.2015-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Afshari D., Nourollahi-Darabad M., Chinisaz N. Demographic predictors of resilience among nurses during the COVID-19 pandemic. Work. 2021;68(2):297–303. doi: 10.3233/WOR-203376. [DOI] [PubMed] [Google Scholar]
- 18.Alameddine M., Bou-Karroum K., Ghalayini W., Abiad F. Resilience of nurses at the epicenter of the COVID-19 pandemic in Lebanon. Int. J. Nurs. Sci. 2021;8(4):432–438. doi: 10.1016/j.ijnss.2021.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aburn G., Gott M., Hoare K. What is resilience? An integrative review of the empirical literature. J. Adv. Nurs. 2016;72(5):980–1000. doi: 10.1111/jan.12888. [DOI] [PubMed] [Google Scholar]
- 20.Lazarus R.S., Folkman S. Springer publishing company; 1984 Mar 15. Stress, Appraisal, and Coping. [Google Scholar]
- 21.Earvolino-Ramirez M. Resilience: a concept analysis. Nurs. Forum. 2007;42(2):73–82. doi: 10.1111/j.1744-6198.2007.00070.x. [DOI] [PubMed] [Google Scholar]
- 22.López-López I.M., Gómez-Urquiza J.L., Cañadas G.R., De la Fuente E.I., Albendín-García L., Cañadas-De la Fuente G.A. Prevalence of burnout in mental health nurses and related factors: a systematic review and meta-analysis. Int. J. Ment. Health Nurs. 2019;28(5):1035–1044. doi: 10.1111/inm.12606. [DOI] [PubMed] [Google Scholar]
- 23.Salek Ebrahimi L., Mousavi S.E., Gharraee B., Mohammadi Bytamar J., Saberi Isfeedvajani M. Cognitive errors and psychological resilience in patients with social anxiety and obsessive-compulsive disorder: a cross-sectional study. Hosp. Pract. Res. 2019;4(1):25–30. [Google Scholar]
- 24.Shilpa S., Srimathi N.L. Role of resilience on perceived stress among pre university and under graduate students. Int. J. Ind. Psychol. 2015;2(2):141–149. [Google Scholar]
- 25.Lim M.L., Lim D., Gwee X., Nyunt M.S., Kumar R., Ng T.P. Resilience, stressful life events, and depressive symptomatology among older Chinese adults. Aging Ment. Health. 2015;19(11):1005–1014. doi: 10.1080/13607863.2014.995591. [DOI] [PubMed] [Google Scholar]
- 26.Shatté A., Perlman A., Smith B., Lynch W.D. The positive effect of resilience on stress and business outcomes in difficult work environments. J. Occup. Environ. Med. 2017;59(2):135. doi: 10.1097/JOM.0000000000000914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Green S.B. How many subjects does it take to do a regression analysis. Multivariate Behav. Res. 1991;26(3):499–510. doi: 10.1207/s15327906mbr2603_7. [DOI] [PubMed] [Google Scholar]
- 28.Connor K.M., Davidson J.R. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 29.Gucciardi D.F., Jackson B., Coulter T.J., Mallett C.J. The Connor-Davidson Resilience Scale (CD-RISC): dimensionality and age-related measurement invariance with Australian cricketers. Psychol Sport Exerc. 2011;12(4):423–433. [Google Scholar]
- 30.Kimhi S., Eshel Y., Marciano H., Adini B. Distress and resilience in the days of COVID-19: comparing two ethnicities. Int. J. Environ. Res. Public Health. 2020;17(11):3956. doi: 10.3390/ijerph17113956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 32.Almadi T., Cathers I., Mansour A.M., Chow C.M. An Arabic version of the perceived stress scale: translation and validation study. Int. J. Nurs. Stud. 2012;49(1):84–89. doi: 10.1016/j.ijnurstu.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 33.Aboshaiqah A.E., Cruz J.P. Quality of life and its predictors among nursing students in Saudi Arabia. J Holist Nurs. 2019;37(2):200–208. doi: 10.1177/0898010118784147. [DOI] [PubMed] [Google Scholar]
- 34.Ju Ohaeri, Awadalla A.W. The reliability and validity of the short version of the WHO Quality of Life Instrument in an Arab general population. Ann. Saudi. Med. 2009;29(2):98–104. doi: 10.4103/0256-4947.51790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bennett J.A. Mediator and moderator variables in nursing research: conceptual and statistical differences. Res. Nurs. Health. 2000;23(5):415–420. doi: 10.1002/1098-240x(200010)23:5<415::aid-nur8>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 36.Kim W.J., Lee K.H., Yoon B.H., Lee J.H., Kim M.D., Jung Y.E., Soh M.J., Lee S.Y. Occupational stress and quality of life in mental health welfare center workers. Mood and Emotion. 2020;18(1):28–36. [Google Scholar]
- 37.Tseng H.M., Shih W.M., Shen Y.C., Ho L.H., Wu C.F. Work stress, resilience, and professional quality of life among nurses caring for mass burn casualty patients after Formosa color dust explosion. J. Burn. Care Res. 2018;39(5):798–804. doi: 10.1093/jbcr/irx053. [DOI] [PubMed] [Google Scholar]
- 38.Liu W.J., Zhou L., Wang X.Q., Yang B.X., Wang Y., Jiang J.F. Mediating role of resilience in relationship between negative life events and depression among Chinese adolescents. Arch. Psychiatr. Nurs. 2019;33(6):116–122. doi: 10.1016/j.apnu.2019.10.004. [DOI] [PubMed] [Google Scholar]
- 39.Shi M., Wang X., Bian Y., Wang L. The mediating role of resilience in the relationship between stress and life satisfaction among Chinese medical students: a cross-sectional study. BMC Med. Educ. 2015;15(1):16. doi: 10.1186/s12909-015-0297-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Foster K., Cuzzillo C., Furness T. Strengthening mental health nurses' resilience through a workplace resilience programme: a qualitative inquiry. J. Psychiatr. Ment. Health. Nurs. 2018;25(5-6):338–348. doi: 10.1111/jpm.12467. [DOI] [PubMed] [Google Scholar]
- 41.Smith G.D., Yang F. Stress, resilience and psychological well-being in Chinese undergraduate nursing students. Nurse Educ. Today. 2017;49:90–95. doi: 10.1016/j.nedt.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 42.Elqerenawi A.Y., Thabet A.A., Vostanis P. Job stressors, coping and resilience among nurses in Gaza strip. Clin. Experim. Psychol. 2017;3(3):1–8. [Google Scholar]
- 43.Sam P.R., Lee P. Do stress and resilience among undergraduate nursing students exist? Amarjeet Kaur Sandhu. 2020;12(1):146–149. [Google Scholar]
- 44.Badu E., O’Brien A.P., Mitchell R., Rubin M., James C., McNeil K., Nguyen K., Giles M. Workplace stress and resilience in the Australian nursing workforce: a comprehensive integrative review. Int. J. Ment. Health Nurs. 2020;29(1):5–34. doi: 10.1111/inm.12662. [DOI] [PubMed] [Google Scholar]
- 45.Gerami Nejad N., Hosseini M., Mousavi Mirzaei S.M., Ghorbani Moghaddam Z. Association between resilience and professional quality of life among nurses working in intensive care units. Iran J. Nurs. 2019;31(116):49–60. [Google Scholar]
- 46.Huang L., Lei W., Xu F., Liu H., Yu L. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: a comparative study. PLoS One. 2020;15(8) doi: 10.1371/journal.pone.0237303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang C., Xia M., Han M., Liang Y. Social support and resilience as mediators between stress and life satisfaction among people with substance use disorder in China. Front. Psychiatry. 2018;9:436. doi: 10.3389/fpsyt.2018.00436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kelbiso L., Belay A., Woldie M. Determinants of quality of work life among nurses working in Hawassa town public health facilities, South Ethiopia: a cross-sectional study. Nurs. Res. Pract. 2017;2017:1–11. doi: 10.1155/2017/5181676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shin S., Hwang E. The effects of clinical practice stress and resilience on nursing students' academic burnout. Korean J. Med. Educ. 2020;22(2):115–121. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.